Abstract
BACKGROUND:
Female sexual dysfunction (FSD) in Indian women is often overlooked due to cultural beliefs and considered as social taboos. Sexuality is an important and integral part of life. There are many causes of sexual dysfunction, but the prevalence of FSD in endometriotic patients is still underdiagnosed.
MATERIALS AND METHODS:
Study design - Cross-sectional observational study conducted at tertiary care center, from June 2015 to March 2016. Sample size - Fifty-one patients in reproductive age group (18–47 years) who were diagnosed with endometriosis on diagnostic laparoscopy were included. Methods - FSD was assessed with a detailed 19-item female sexual function index questionnaire. All six domains of sexual dysfunction, i.e., desire, arousal, lubrication, orgasm, satisfaction, and pain were studied. Exclusion - Patients with other gynecological, medical or surgical history were excluded.
RESULTS:
Out of 51 patients with endometriosis, 47.06% of patients had sexual dysfunction. With the increase in staging of endometriosis, sexual dysfunction prevalence is also rising. FSD was 100% in patients with severe endometriosis as compared to 33.33% in minimal endometriosis.
CONCLUSION:
Every individual deserves good sexual life. The sexual dysfunction associated with endometriosis should also be taken into consideration while managing these patients.
KEY WORDS: Endometriosis, female sexual dysfunction, female sexual function index, pain
INTRODUCTION
Sexual dysfunction is defined as difficulty experienced by an individual or a couple during any stage of a normal sexual activity, including physical pleasure, desire, preference, arousal, or orgasm.[1] There are various causes for sexual dysfunction, but endometriosis is one of the most important and least understood factors in terms of sexuality. Endometriosis, especially deep infiltrating lesions can hamper the quality of sexual life. Apart from dyspareunia, these patients can be depressed or frustrated due to pain and endometriosis-associated infertility, leading to sexual pain disorder and desire-arousal disorder. There are many studies on symptomology, medical or surgical management of endometriosis but less literature on female sexual dysfunction (FSD) associated with endometriosis.
MATERIALS AND METHODS
This is a cross-sectional study conducted at tertiary care center, from June 2015 to March 2016.
Inclusion criteria
Patients in reproductive age group (18–47 years) who were diagnosed with endometriosis on diagnostic laparoscopy were included. All these patients underwent diagnostic laparoscopy for infertility workup except two where it was done for chronic pelvic pain. These patients were classified as minimal, mild, moderate, and severe endometriosis based on Revised American Society for Reproductive Medicine Classification, 1997.
Methods
FSD was assessed with a detailed 19-item female sexual function index (FSFI) questionnaire. Oral informed consent was taken from patients included in the study. FSFI pro forma was given to patients according to their preferred language (Hindi, English, and Gujarati). Pro forma was pilot tested for cultural appropriateness and linguistic accuracy. Illiterate women were interviewed personally. All six domains of sexual dysfunction, i.e., desire, arousal, lubrication, orgasm, satisfaction, and pain were studied. In addition to prevalence of FSD among patients with endometriosis, association between psychological factors and sexual dysfunction was also studied as both are interrelated.
Exclusion criteria
Patients with other gynecological, medical, or surgical history were excluded from this study.
Female sexual function index
It is a 19-item questionnaire, which acts as brief, multidimensional self-report instrument for assessing different domains of female sexual function.[2] It provides scores on six domains of sexual function: desire, arousal, lubrication, orgasm, satisfaction, and pain, as well as a total score.[3] Response to each question relates to previous 4 weeks sexual activity and are scored from 0 (no sexual activity), 1 (indicative of dysfunction) to 5 (suggestive of normal sexual activity). Individual domain scores are obtained by adding the scores of the individual questions that comprise the domain and multiplying the sum by the domain factor provided in the FSFI for each domain. The total score is obtained by adding scores of all domains. The score varies from 2 (minimum) to 36 (maximum). A score ≤26.55 is classified as FSD, as obtained from a validation study.
RESULTS
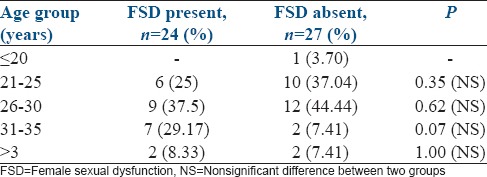
The mean age of patients was 28.51 ± 5.15 years, and mean duration of marriage was 6.29 ± 3.94 years. Table 1 shows age wise distribution. The prevalence of FSD was 47.06%.
Table 1.
Age-wise distribution of female sexual dysfunction
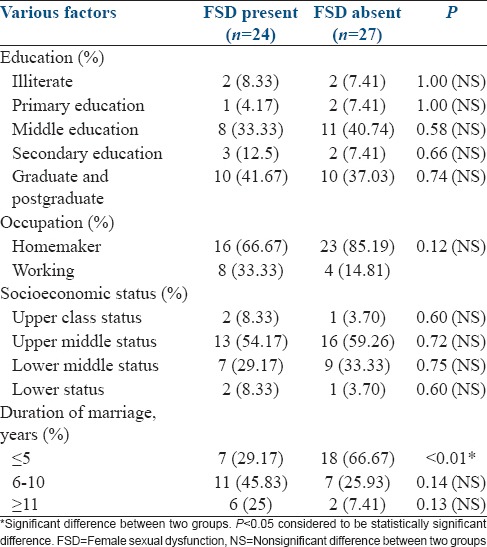
Various demographic factors such as patient's education, occupation, socioeconomic status, and duration of marriage were studied [Table 2].
Table 2.
Various demographic factors and female sexual dysfunction
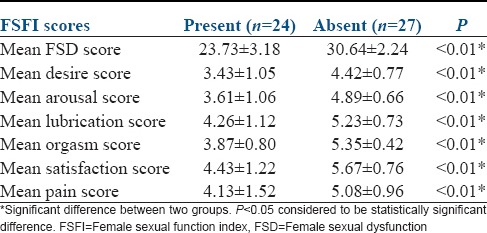
All domains of sexual function were studied along with their mean score [Table 3]. The minimum FSFI score in the study was 13.9 and maximum score being 35.1.
Table 3.
Female sexual function index scoring along with 6 domains score
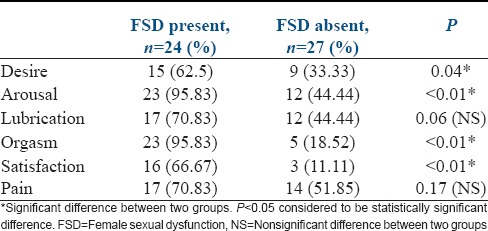
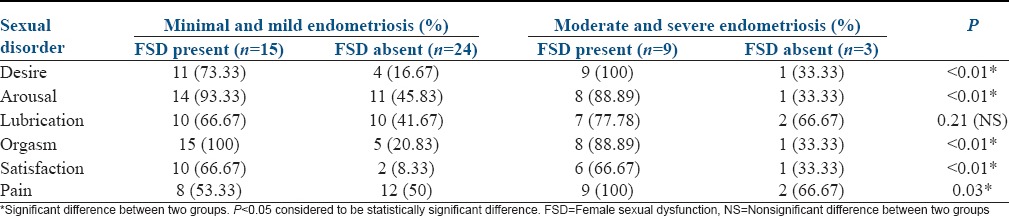
The various types of sexual dysfunction were also studied and compared between patients with FSD and those with no FSD [Table 4]. Patients with endometriosis most commonly had arousal and orgasm dysfunction.
Table 4.
Type of sexual dysfunction in patients with female sexual dysfunction and patients with no female sexual dysfunction
There were 24 patients who were present with FSD. According to the staging of endometriosis, sexual function was studied in these patients [Table 5].
Table 5.
Female sexual dysfunction in accordance to endometriosis stage
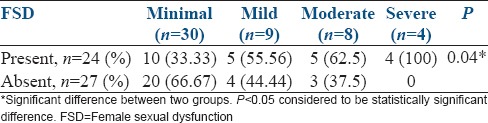
Various domains of sexual dysfunction were compared between patients with minimal and mild endometriosis versus patients with moderate and severe lesions [Table 6]. With the increase in staging of endometriosis, sexual dysfunction prevalence is also rising. This may be due to severe pelvic pain associated with deep infiltrating lesions in severe endometriosis. Due to pain, these patients can develop depression or frustration resulting in decreased desire, arousal, and even interpersonal conflicts, leading to sexual dysfunction. Apart from pain, infertility associated with endometriosis also adds on stress to their life. Patients with minimal and mild endometriosis most commonly had orgasm dysfunction whereas patients with moderate and severe endometriosis most commonly had desire and pain dysfunction.
Table 6.
Comparison of various domains of female sexual dysfunction in two groups
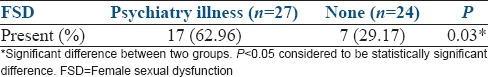
Effects of psychological factors such as anxiety, depression, stress, and interpersonal conflicts in endometriotic patients on their sexual life were also studied [Table 7].
Table 7.
Effect of psychology on sexual function
Data analysis
All collected data entered into the SPSS V20 (IBM) and analysis has been conducted. Continuous data are expressed as mean ± standard deviation form while noncontinuous data are countable and are expressed as percentages or numbers. All continuous data follow Normal distribution and nonnormal distribution both. Independent t-test and Mann–Whitney tests have been used to calculate statistically significant value, i.e., is P value.
For noncontinuous data, Chi-square and Fisher exact test have been used for carrying out the statistically significant value, i.e. P value.
DISCUSSION
Sexuality is a complex process, coordinated by the neurologic, vascular, and endocrine systems.[4] The factors affecting sexuality are often interlinked. FSD is common in women with endometriosis, especially for those with severe pelvic pain and advanced stages of endometriosis.[5] In our study too, FSD was 100% in patients with severe endometriosis as compared to 33.33% in minimal endometriosis. Endometriosis is a chronic condition where endometrial glands and stroma are present outside of the uterus.[5] The number of cases of endometriosis are rising over the past 15–20 years.[6] This enormous increase may be due to the introduction of laparoscopy for the direct confirmation of the presence of endometrial tissue in the abdomen.[7] The prevalence of endometriosis is 5%–15% of women in reproductive age group, but its true prevalence is unknown.[6]
Endometriosis is commonly present as chronic pelvic pain and infertility. About 25% of women may have no symptoms, but many are presented with dysmenorrhea and dyspareunia[8] which can have both social and psychological effects.[9] The amount of pain perceived, correlates poorly with the stage of endometriosis, with some having little or no pain despite having extensive endometriosis or endometriosis with scarring, while other may have severe pain even though they have only a few small areas of endometriosis.[10] However, more than half of women with endometriosis experience dyspareunia during their entire sexual lives, especially those involving uterosacral ligament.[11]
Dyspareunia associated with endometriosis can lead to reduction of self-esteem and a negative effect on relationships with partners.[5] Infertility and depression, which are highly prevalent in these women, may act as confounding factor for FSD.[12] In our study also, most of the patients (48) were infertile, out of which 27 patients were having psychological disturbances such as stress, depression, anxiety, and interpersonal conflicts. The presence of these psychological disturbances had a significant impact on the quality of sexual life.
A study by Verit et al. showed that sexual dysfunction was present in 67.8% of women with chronic pelvic pain.[13] Another study in Brazil reported that women with chronic pelvic pain due to endometriosis, 39.3% had sexual dysfunction.[14] There was decreased in the frequency of sexual intercourse, presence of vaginismus, sexual aversion, and reduced expression of sensuality. Ferrero et al. found that women with endometriosis experienced higher prevalence of deep dyspareunia than controls (60.6% of the sample compared with 34.9% of controls). Women with endometriosis involving uterosacral ligaments had higher prevalence of sexual dysfunction than those with endometriosis in other sites.[11] In our study too, prevalence of FSD among patients with endometriosis was 47.03%.
There was statically no significant difference found in the prevalence of FSD in accordance to factors such as socioeconomic status, literacy rate, and age. These findings are supported by a similar study by Jia et al.[15]
CONCLUSION
Sexuality is an integral part of one's personality, which get adversely affected by the presence of endometriosis. With the increase in stage of endometriosis, the prevalence of FSD also rises. It is important to address this problem, and it requires the participation of both gynecologist and psychiatrist along with patient and patient's spouse to solve the problem.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Nolen-Hoeksema S. Abnormal Psychology. New York: McGraw-Hill; 2014. pp. 366–7. [Google Scholar]
- 2.Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The female sexual function index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 3.Meston CM. Validation of the female sexual function index (FSFI) in women with female orgasmic disorder and in women with hypoactive sexual desire disorder. J Sex Marital Ther. 2003;29:39–46. doi: 10.1080/713847100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bachmann GA, Phillips NA. Sexual dysfunction. In: Steege JF, Metzger DA, Levy BS, editors. Chronic Pelvic Pain: An Integrated Approach. Philadelphia: Saunders; 1998. pp. 77–90. [Google Scholar]
- 5.Denny E, Mann CH. Endometriosis-associated dyspareunia: The impact on women's lives. J Fam Plann Reprod Health Care. 2007;33:189–93. doi: 10.1783/147118907781004831. [DOI] [PubMed] [Google Scholar]
- 6.Danewood M, Kresch AJ, Metzger D, Begany T. Current approaches to endometriosis. Patient Care. 1997;31:34–43. [Google Scholar]
- 7.Campbell C, Monga A. Gynaecology by Ten Teachers. 17th ed. London, UK: Edward Arnold; 2000. [Google Scholar]
- 8.Bulletti C, Coccia ME, Battistoni S, Borini A. Endometriosis and infertility. J Assist Reprod Genet. 2010;27:441–7. doi: 10.1007/s10815-010-9436-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Culley L, Law C, Hudson N, Denny E, Mitchell H, Baumgarten M, et al. The social and psychological impact of endometriosis on women's lives: A critical narrative review. Hum Reprod Update. 2013;19:625–39. doi: 10.1093/humupd/dmt027. [DOI] [PubMed] [Google Scholar]
- 10.Stratton P, Berkley KJ. Chronic pelvic pain and endometriosis: Translational evidence of the relationship and implications. Hum Reprod Update. 2011;17:327–46. doi: 10.1093/humupd/dmq050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferrero S, Esposito F, Abbamonte LH, Anserini P, Remorgida V, Ragni N. Quality of sex life in women with endometriosis and deep dyspareunia. Fertil Steril. 2005;83:573–9. doi: 10.1016/j.fertnstert.2004.07.973. [DOI] [PubMed] [Google Scholar]
- 12.ter Kuile MM, Weijenborg PT, Spinhoven P. Sexual functioning in women with chronic pelvic pain: The role of anxiety and depression. J Sex Med. 2010;7:1901–10. doi: 10.1111/j.1743-6109.2009.01414.x. [DOI] [PubMed] [Google Scholar]
- 13.Verit FF, Verit A, Yeni E. The prevalence of sexual dysfunction and associated risk factors in women with chronic pelvic pain: A cross-sectional study. Arch Gynecol Obstet. 2006;274:297–302. doi: 10.1007/s00404-006-0178-3. [DOI] [PubMed] [Google Scholar]
- 14.Tripoli TM, Sato H, Sartori MG, de Araujo FF, Girão MJ, Schor E. Evaluation of quality of life and sexual satisfaction in women suffering from chronic pelvic pain with or without endometriosis. J Sex Med. 2011;8:497–503. doi: 10.1111/j.1743-6109.2010.01976.x. [DOI] [PubMed] [Google Scholar]
- 15.Jia SZ, Leng JH, Sun PR, Lang JH. Prevalence and associated factors of female sexual dysfunction in women with endometriosis. Obstet Gynecol. 2013;121:601–6. doi: 10.1097/AOG.0b013e3182835777. [DOI] [PubMed] [Google Scholar]


