Abstract
AIM:
The goal was to compare the effects of three different sperm preparation media on sperm motility, viability, and DNA integrity of semen samples from normozoospermic men.
METHODS:
A total of 15 normozoospermic males were included in the study. The semen analysis (SA) was performed in accordance with the WHO guidelines (2010). After SA, each sample was divided into three aliquots, and swim-up was performed with three different sperm preparation media (Sperm Preparation Media, Origio, Denmark; Ham's F10, Biochrome, Berlin, Germany; and VitaSperm™, Innovative Biotech, Iran). Sperm motility, viability, and DNA fragmentation were evaluated at 0, 1, 2, and 24 h after swim-up.
RESULTS:
There were no significant differences, at any time intervals, in the total sperm motility between the different sperm preparation media. However, the rate of progressive motility was significantly higher in spermatozoa prepared using the media from Origio in comparison with VitaSperm™ (P = 0.03), whereas no significant difference was found against Ham's F10 medium. No significant differences in sperm viability were seen between the media products. However, 1 h after swim-up, the extent of sperm DNA fragmentation was lower in the medium from Origio versus VitaSperm™ (P = 0.02).
CONCLUSIONS:
The data showed that the quality of medium for preparation of semen samples from normozoospermic men significantly affects the performance of spermatozoa in assisted conception programs.
KEY WORDS: DNA fragmentation, sperm motility, sperm preparation media, sperm viability
INTRODUCTION
The need for assisted reproduction technology (ART) procedures for the establishment of pregnancies has steadily increased worldwide. Around 7% of all annual births are thought to be established by ART, which corresponds to 1 million treatments.[1] Therefore, it is of vital importance that an efficient sperm preparation technique used for retrieval of high-quality spermatozoa contributes to the creations of high-quality embryos, with high implantation potential.[2] The main goal with the sperm preparation is to yield highly motile spermatozoa with good morphology and low DNA fragmentation rates, criteria that support the subsequent development of high-quality embryos. The sperm DNA integrity affects fertilization,[3] embryo development, pregnancy outcome,[4,5] miscarriage rates,[2] and abnormalities in the offspring[5] after both in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI). In animals, development of cancer and shorter lifespan in their offspring are related to the injection of spermatozoa with high DNA fragmentation rates.[6,7]
The recovery of a good proportion of high-quality spermatozoa depends on the quality of the semen sample, the sperm preparation method, time and storage temperature of the prepared sperm suspension.[8,9,10] The choice of sperm preparation medium also interferes with the recovery of high-quality spermatozoa, which affects the treatment outcome.[11] An effective sperm preparation method yields a high number of motile spermatozoa with good morphology and quality, which may convert more complex treatment, such as ICSI, into more simple techniques of IVF or intrauterine insemination (IUI) for a more natural and cost-effective treatments. It is also important to evaluate the integrity of sperm DNA after the sperm preparation technique since morphologically normal spermatozoa still may have DNA damage.[12,13] Currently, there are several techniques for detection of sperm DNA fragmentation. The sperm chromatin dispersion (SCD) assay evaluates DNA fragmentation and has the same predictive values such as the sperm chromatin structure assay (SCSA) and TdT-mediated dUTP-biotin nick end labeling (TUNEL).[14] In addition, this assay is easy, rapid, accurate, and not requiring sophisticated instruments. The aim of this study was to compare the effects of three different sperm preparation media on viability, motility, and DNA integrity of spermatozoa after preparation of normozoospermic samples.
METHODS
Patients
This case study involved 15 normozoospermic specimens from men undergoing infertility. This study was done from July 2014 to February 2015. All the patients signed the consent form. This study was approved by the Institutional Review Board.
Semen analysis
The semen samples, according to the WHO guidelines,[15] met the inclusion criteria. Khalili et al. chamber was used for determination of the sperm count and motility characteristics.[16] The following criteria were applied for evaluation of sperm motility: Rapidly progressive spermatozoa were considered as Grade a. Grade b spermatozoa were slowly progressive, Grades c and d were dedicated to no progressive motility and immotile spermatozoa, respectively. Morphology was evaluated using Papanicolaou method.[9] Three culture media were selected: (a) Sperm Preparation Media (Origio, Måløv, Denmark), (b) Ham's F10 (Biochrome, Berlin, Germany) supplemented with 5 mg/ml human serum albumin, and (c) Sperm Washing Medium (VitaSperm™ Innovative Biotech, Tehran, Iran), where 5 mg/ml HSA was added. Sperm motility, viability, and DNA fragmentation index (DFI) were evaluated at 0, 1, 2, and 24 h after preparation. Sperm viability and DFI were assessed after staining with eosin-nigrosin, and the SCD technique, respectively.
Sperm preparation
The samples were prepared by direct swim-up method. Briefly, 1.2 ml of each culture media was placed into a sterile conical tube, after which 1 ml of the semen was slowly placed under the medium at the bottom of the tube. The swim-up was performed at 37°C in an incubator at 45° angle for 45 min. Thereafter, 1 ml of the upper layer was removed, and 2 ml of the same sperm preparation media was added to the test tube. After centrifugation at 400 g for 7 min, the pellet was resuspended in 0.5 ml preincubated media, the tubes closed tightly, and the sperm suspension analyzed at the aforementioned time intervals.
Sperm chromatin dispersion test
The SCD test was performed according to Fernández et al.[17] Glass slides were coated with 0.65% (w/v) agarose and 70 μl of a low-melting 1% (w/v) agarose was mixed with 30 μl of the sperm suspension. Thereafter, 50 μl of this mixture was placed on the precoated glass slides and kept at 4°C for 4 min. Next, the slides were placed in a denaturation solution (0.08 M HCL) for 7 min at room temperature (RT) in the dark. These slides were placed in 0.4M Tris, 2-mercaptoethanol containing 1% (w/v) sodium dodecyl sulfate (SDS) and 50 mM ethylenediaminetetraacetic acid (EDTA) (pH 7.5), for 10 min at RT. After incubation, the slides were placed in a lysing solution (0.4M Tris, 2M NaCl, and 1% [w/v] SDS, pH 7.5) for 15 min and were finally washed in a Tris-borate-EDTA buffer (0.09 M Tris-borate and 0.002 M EDTA, pH 7.5) for 2 min at RT. The slides were dehydrated in ascending ethanols (70%, 90%, and 100% [v/v]) for 2 min and left to dry at RT.
For staining the slides, Wright's stain was mixed with a phosphate buffer solution at a ratio of 1:1. This mixture was layered on the slides placed in running water until the excess stains washed away and left to dry at RT. The DNA fragmentation rate was related to the halo around the sperm head and categorized into four groups: (a) Big halo, when the halo size was more than the minor diameter of core width (without DNA fragmentation), (b) small halo, with size smaller than one-third of the minor diameter of core width, (c) medium halo size was considered between large and small halos, and (d) no halo. Large- and medium-sized halos have no DNA fragmentation while small size halos or no halos have a fragmented DNA [Figure 1].
Figure 1.
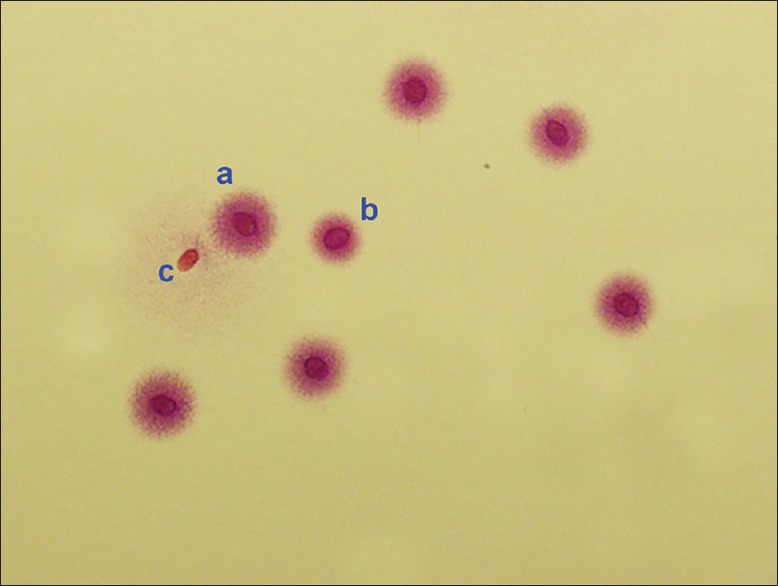
Sperm chromatin dispersion test. (a) A big halo represents no DNA fragmentation, (b) a medium halo represents no DNA fragmentation, and (c) no halo indicates spermatozoa with DNA fragmentation
Statistical analysis
The data are shown as mean ± standard deviation and median (minimum–maximum). The Shapiro test was used for evaluating normal distribution of data. One-way analysis of variance followed by Tukey as a posttest and Kruskal–Wallis test was applied to compare sperm parameters between media at one time point. All hypotheses were considered two-tailed, and P < 0.05 was considered statistically significant.
RESULTS
There were no significant differences in progressive motility between the different sperm preparation media after swim-up at 0, 1, and 24 h. However, the rate of progressive motility was significantly higher in spermatozoa prepared by Sperm Preparation Media, when compared to VitaSperm™ (68.3 ± 11.5 vs. 58 ± 9.8, P = 0.03) [Figure 2]. There were insignificant differences in motility or viability between the different groups [Tables 1 and 2]. In addition, there was no difference in the percentage of normal morphology between Sperm Preparation Media, VitaSperm™, and Ham's F10 after swim-up (15.9 ± 2.1, 16.4 ± 3.2, and 15.8 ± 2.3, respectively). The sperm DFI increased significantly 1 h after swim-up in VitaSperm™ versus Sperm Preparation Media (3 ± 2.7 vs. 1.1 ± 0.8, P = 0.02); however, there was insignificant difference in comparison to Ham's F10 (1.7 ± 1.1). However, the DFI increased significantly over time in the VitaSperm™ medium versus other two media [Figure 3].
Figure 2.
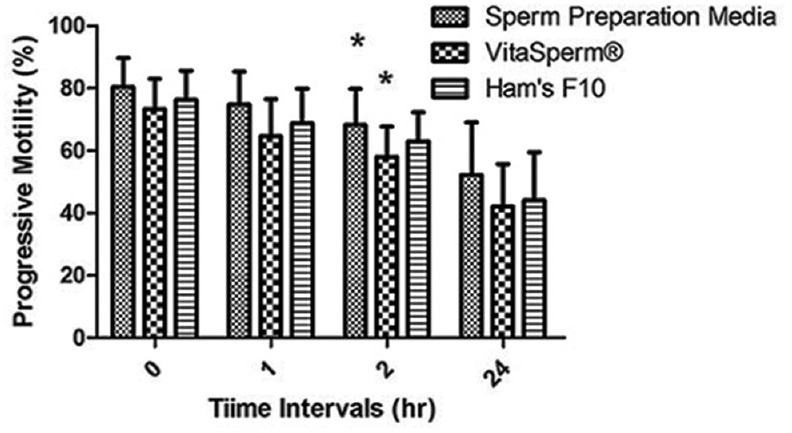
The percentage of progressively motile spermatozoa after swim-up. *P = 0.03
Table 1.
Total number of motile sperm (%) at different time intervals after swim-up
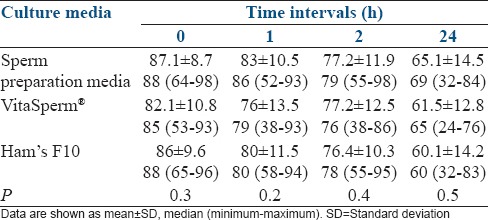
Table 2.
Sperm viability rates (%) at different time intervals after swim-up using eosin-nigrosin stain
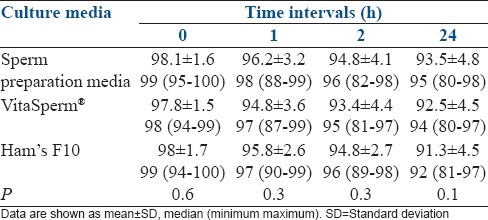
Figure 3.
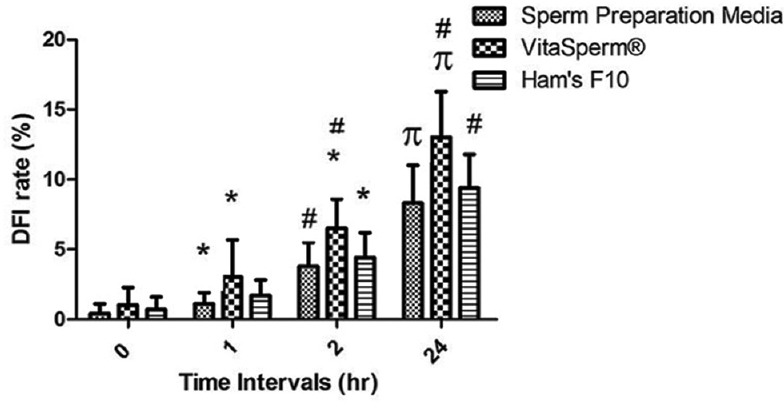
The rate of sperm DNA fragmentation index after swim-up of normozoospermic samples in different sperm preparation media at different time intervals. *P < 0.05, #P < 0.01, πP < 0.001
DISCUSSION
The quality of the prepared sperm suspension affects the outcome of all types of inseminations, whether it is for IUI, IVF, or ICSI. After sperm preparation, the recovery of motile spermatozoa affects the decision of which method would be the most suitable and efficient for the couple. If there is a high recovery of highly motile spermatozoa with good morphology and low DFI, the prepared sperm suspension is suitable for more physiological methods, such as IUI or IVF. Whereas, borderline or male factor samples might be more suitable for ICSI. The handling of the semen sample, choice of sperm preparation method, and storage temperature of the prepared sperm suspension affect the recovery rates of sperm, their fertilization ability, the integrity of the sperm DNA, their ability to support embryo development and the implantation rate.[3,4,5,9] The effects of different sperm preparation techniques on sperm parameter values and the DNA integrity have been evaluated in several studies.[8,18,19,20] It seems that the yield of morphologically normal spermatozoa with good chromatin stability is obtained after preparation of the semen sample by high-density gradient centrifugation in comparison with conventional swim-up and glass wool filtration methods.[19]
In this study, we evaluated the efficacy of three different sperm preparation media on motility, viability, and DNA integrity of human spermatozoa at different time intervals after sperm preparation. Our data showed that the nature of the sperm preparation medium affects sperm motility and the DNA integrity of the prepared spermatozoa. Depending on the quality, the storage temperature, and the incubation time of the sperm suspension, as well as the preparation medium, the level of sperm DNA fragmentation varies.[9,10] Oxidative stress and lipid peroxidation have been suggested to affect sperm motility[21,22] by inducing damages to the axoneme and depletion of intracellular adenosine triphosphate, which reduces the sperm motility.[23,24,25] It is thought that the main product of oxidative stress, 8-hydroxy, 2′deoxyguanosine, also causes most of the damage to the sperm DNA.[26] The extent of sperm DNA fragmentation could be used as a sperm quality marker, which predicts the fertilization capability of the prepared spermatozoa. The main causes to sperm DNA fragmentation are thought to be related to failure in the chromatin remodeling during spermiogenesis or an increase in reactive oxygen species (ROS) levels due to oxidative stress.[27] However, the impact of sperm DNA fragmentation on fertilization has still not been confirmed.[5,28] However, a defect in sperm chromatin stability might affect the sperm cells’ ability to penetrate the rigid zona pellucida.[3,29]
The SCD test is based on the halo formation of dispersed DNA loops after acid denaturation, where spermatozoa with a high DNA fragmentation rate do not create a halo.[9] It has been shown that the SCD gives similar results to that of both the SCSA and the TUNEL assay and that it can be used as a prognostic tool for sperm DNA fragmentation rate.[14]
Oxidative stress in subnormal specimens is induced by other types of contaminating cells, immature and bad morphology spermatozoa, as well as the sperm wash method.[8,15,30,31,32,33] We, therefore, used normozoospermic samples for this study, to reduce potential sources of oxidative stress to spermatozoa and for accurate interpretation of the results.[9,34] The method of choice for preparation of semen may affect the production of ROS, thereby inducing oxidative stress.[35] However, Younglai et al. showed that there was no significant difference in DNA fragmentation rate in spermatozoa prepared by direct swim-up from the semen sample or after prewash of the semen sample.[36] In this study, all samples were prepared by the direct swim-up method; thus, the findings should only be related to the quality of the sperm preparation media. Formation of free radicals and oxidative stress also seem to play a physiological role in sperm capacitation and fusion between the spermatozoa and the oocyte.[30] Antioxidants, such as ascorbic acid and tocopherols, seem to prevent the detrimental effects that ROS have on sperm motility and DNA fragmentation.[34,37] The inclusion of antioxidants in sperm preparation media might, therefore, reduce the detrimental effect that ROS have on sperm during the preparation procedure.
CONCLUSIONS
The quality of the sperm preparation media affects the sperm recovery of high-quality spermatozoa which subsequently may influence the ART outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The present study was supported by the Research and Clinical Center for Infertility, Shahid Sadughi University of Medical Sciences, Yazd, Iran. The authors would like to thank Dr. Mojgan Aboulghasemi, who helped us with her experience in this study.
REFERENCES
- 1.International Committee for Monitoring Assisted Reproductive. de Mouzon J, Lancaster P, Nygren KG, Sullivan E, Zegers-Hochschild F, et al. World collaborative report on assisted reproductive technology, 2002. Hum Reprod. 2009;24:2310–20. doi: 10.1093/humrep/dep098. [DOI] [PubMed] [Google Scholar]
- 2.Zini A, Boman JM, Belzile E, Ciampi A. Sperm DNA damage is associated with an increased risk of pregnancy loss after IVF and ICSI: Systematic review and meta-analysis. Hum Reprod. 2008;23:2663–8. doi: 10.1093/humrep/den321. [DOI] [PubMed] [Google Scholar]
- 3.Tavalaee M, Razavi S, Nasr-Esfahani MH. Influence of sperm chromatin anomalies on assisted reproductive technology outcome. Fertil Steril. 2009;91:1119–26. doi: 10.1016/j.fertnstert.2008.01.063. [DOI] [PubMed] [Google Scholar]
- 4.Collins JA, Barnhart KT, Schlegel PN. Do sperm DNA integrity tests predict pregnancy with in vitro fertilization? Fertil Steril. 2008;89:823–31. doi: 10.1016/j.fertnstert.2007.04.055. [DOI] [PubMed] [Google Scholar]
- 5.Aitken RJ, De Iuliis GN, McLachlan RI. Biological and clinical significance of DNA damage in the male germ line. Int J Androl. 2009;32:46–56. doi: 10.1111/j.1365-2605.2008.00943.x. [DOI] [PubMed] [Google Scholar]
- 6.Fernández-Gonzalez R, Moreira PN, Pérez-Crespo M, Sánchez-Martín M, Ramirez MA, Pericuesta E, et al. Long-term effects of mouse intracytoplasmic sperm injection with DNA-fragmented sperm on health and behavior of adult offspring. Biol Reprod. 2008;78:761–72. doi: 10.1095/biolreprod.107.065623. [DOI] [PubMed] [Google Scholar]
- 7.Pérez-Crespo M, Moreira P, Pintado B, Gutiérrez-Adán A. Factors from damaged sperm affect its DNA integrity and its ability to promote embryo implantation in mice. J Androl. 2008;29:47–54. doi: 10.2164/jandrol.107.003194. [DOI] [PubMed] [Google Scholar]
- 8.Twigg J, Irvine DS, Houston P, Fulton N, Michael L, Aitken RJ. Iatrogenic DNA damage induced in human spermatozoa during sperm preparation: Protective significance of seminal plasma. Mol Hum Reprod. 1998;4:439–45. doi: 10.1093/molehr/4.5.439. [DOI] [PubMed] [Google Scholar]
- 9.Nabi A, Khalili MA, Halvaei I, Roodbari F. Prolonged incubation of processed human spermatozoa will increase DNA fragmentation. Andrologia. 2014;46:374–9. doi: 10.1111/and.12088. [DOI] [PubMed] [Google Scholar]
- 10.Zhang XD, Chen MY, Gao Y, Han W, Liu DY, Huang GN. The effects of different sperm preparation methods and incubation time on the sperm DNA fragmentation. Hum Fertil (Camb) 2011;14:187–91. doi: 10.3109/14647273.2011.604817. [DOI] [PubMed] [Google Scholar]
- 11.Mortimer D. Sperm preparation techniques and iatrogenic failures of in-vitro fertilization. Hum Reprod. 1991;6:173–6. doi: 10.1093/oxfordjournals.humrep.a137300. [DOI] [PubMed] [Google Scholar]
- 12.Gandini L, Lombardo F, Paoli D, Caruso F, Eleuteri P, Leter G, et al. Full-term pregnancies achieved with ICSI despite high levels of sperm chromatin damage. Hum Reprod. 2004;19:1409–17. doi: 10.1093/humrep/deh233. [DOI] [PubMed] [Google Scholar]
- 13.Avendaño C, Oehninger S. DNA fragmentation in morphologically normal spermatozoa: How much should we be concerned in the ICSI era? J Androl. 2011;32:356–63. doi: 10.2164/jandrol.110.012005. [DOI] [PubMed] [Google Scholar]
- 14.Chohan KR, Griffin JT, Lafromboise M, De Jonge CJ, Carrell DT. Comparison of chromatin assays for DNA fragmentation evaluation in human sperm. J Androl. 2006;27:53–9. doi: 10.2164/jandrol.05068. [DOI] [PubMed] [Google Scholar]
- 15.WHO. WHO Laboratory Manual for the Examination and Processing of Human Semen. 5th ed. Switzerland: Cambridge University Press; 2010. [Google Scholar]
- 16.Khalili MA, Mojibian M, Sultan AM. Role of oocyte morphology on fertilization and embryo formation in assisted reproductive techniques. Middle East Fertility Society J. 2005:10. [Google Scholar]
- 17.Fernández JL, Muriel L, Rivero MT, Goyanes V, Vazquez R, Alvarez JG. The sperm chromatin dispersion test: A simple method for the determination of sperm DNA fragmentation. J Androl. 2003;24:59–66. [PubMed] [Google Scholar]
- 18.Kaewnoonual N, Chiamchanya Ch, Visutakul P, Manochantr S, Chaiya J, Tor-Udom P. Comparative study of semen quality between pre-washed and post-washed with 3 sperm preparation media. Thammasat Med J. 2010;8:292–300. [Google Scholar]
- 19.Hammadeh ME, Kühnen A, Amer AS, Rosenbaum P, Schmidt W. Comparison of sperm preparation methods: Effect on chromatin and morphology recovery rates and their consequences on the clinical outcome after in vitro fertilization embryo transfer. Int J Androl. 2001;24:360–8. doi: 10.1046/j.1365-2605.2001.0317a.x. [DOI] [PubMed] [Google Scholar]
- 20.Sharma RK, Seifarth K, Garlak D, Agarwal A. Comparison of three sperm preparation media. Int J Fertil Womens Med. 1998;44:163–7. [PubMed] [Google Scholar]
- 21.Aitken RJ, Curry BJ. Redox regulation of human sperm function: From the physiological control of sperm capacitation to the etiology of infertility and DNA damage in the germ line. Antioxid Redox Signal. 2011;14:367–81. doi: 10.1089/ars.2010.3186. [DOI] [PubMed] [Google Scholar]
- 22.Aitken RJ, Gibb Z, Mitchell LA, Lambourne SR, Connaughton HS, De Iuliis GN. Sperm motility is lost in vitro as a consequence of mitochondrial free radical production and the generation of electrophilic aldehydes but can be significantly rescued by the presence of nucleophilic thiols. Biol Reprod. 2012;87:110. doi: 10.1095/biolreprod.112.102020. [DOI] [PubMed] [Google Scholar]
- 23.de Lamirande E, Gagnon C. Reactive oxygen species and human spermatozoa. II. Depletion of adenosine triphosphate plays an important role in the inhibition of sperm motility. J Androl. 1992;13:379–86. [PubMed] [Google Scholar]
- 24.De Lamirande E, Gagnon C. Reactive oxygen species and human spermatozoa: I. Effects on the motility of intact spermatozoa and on sperm axonemes. J Androl. 1992;13:368–78. [PubMed] [Google Scholar]
- 25.Tsunoda S, Kawano N, Miyado K, Kimura N, Fujii J. Impaired fertilizing ability of superoxide dismutase 1-deficient mouse sperm during in vitro fertilization. Biol Reprod. 2012;87:121. doi: 10.1095/biolreprod.112.102129. [DOI] [PubMed] [Google Scholar]
- 26.Santiso R, Tamayo M, Gosálvez J, Meseguer M, Garrido N, Fernández JL. Simultaneous determination in situ of DNA fragmentation and 8-oxoguanine in human sperm. Fertil Steril. 2010;93:314–8. doi: 10.1016/j.fertnstert.2009.07.969. [DOI] [PubMed] [Google Scholar]
- 27.Fernández JL, de la Calle JFV, Tamayo M, Cajigal D, Agarwal A, Gosalvez J. Sperm DNA integrity and male infertility: Current perspectives. Arch Med Sci. 2009;5:S55–62. [Google Scholar]
- 28.Aitken RJ, Gordon E, Harkiss D, Twigg JP, Milne P, Jennings Z, et al. Relative impact of oxidative stress on the functional competence and genomic integrity of human spermatozoa. Biol Reprod. 1998;59:1037–46. doi: 10.1095/biolreprod59.5.1037. [DOI] [PubMed] [Google Scholar]
- 29.Kumar D, Upadhya D, Uppangala S, Salian SR, Kalthur G, Adiga SK. Nuclear DNA fragmentation negatively affects zona binding competence of Y bearing mouse spermatozoa. J Assist Reprod Genet. 2013;30:1611–5. doi: 10.1007/s10815-013-0123-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aitken RJ, Smith TB, Jobling MS, Baker MA, De Iuliis GN. Oxidative stress and male reproductive health. Asian J Androl. 2014;16:31–8. doi: 10.4103/1008-682X.122203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shannon P, Curson B. Kinetics of the aromatic L-amino acid oxidase from dead bovine spermatozoa and the effect of catalase on fertility of diluted bovine semen stored at 5 degrees C and ambient temperatures. J Reprod Fertil. 1982;64:463–7. doi: 10.1530/jrf.0.0640463. [DOI] [PubMed] [Google Scholar]
- 32.Walczak-Jedrzejowska R, Wolski JK, Slowikowska-Hilczer J. The role of oxidative stress and antioxidants in male fertility. Cent European J Urol. 2013;66:60–7. doi: 10.5173/ceju.2013.01.art19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Agarwal A, Virk G, Ong C, du Plessis SS. Effect of oxidative stress on male reproduction. World J Mens Health. 2014;32:1–17. doi: 10.5534/wjmh.2014.32.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fanaei H, Khayat S, Halvaei I, Ramezani V, Azizi Y, Kasaeian A, et al. Effects of ascorbic acid on sperm motility, viability, acrosome reaction and DNA integrity in teratozoospermic samples. Iran J Reprod Med. 2014;12:103–10. [PMC free article] [PubMed] [Google Scholar]
- 35.Griveau JF, Le Lannou D. Effects of antioxidants on human sperm preparation techniques. Int J Androl. 1994;17:225–31. doi: 10.1111/j.1365-2605.1994.tb01247.x. [DOI] [PubMed] [Google Scholar]
- 36.Younglai EV, Holt D, Brown P, Jurisicova A, Casper RF. Sperm swim-up techniques and DNA fragmentation. Hum Reprod. 2001;16:1950–3. doi: 10.1093/humrep/16.9.1950. [DOI] [PubMed] [Google Scholar]
- 37.Talebi AR, Mangoli E, Nahangi H, Anvari M, Pourentezari M, Halvaei I. Vitamin C attenuates detrimental effects of diabetes mellitus on sperm parameters, chromatin quality and rate of apoptosis in mice. Eur J Obstet Gynecol Reprod Biol. 2014;181:32–6. doi: 10.1016/j.ejogrb.2014.07.007. [DOI] [PubMed] [Google Scholar]


