Abstract
Background:
Lumbar disc herniation is a major cause of back pain and sciatica. The surgical management of lumbar disc prolapse has evolved from exploratory laminectomy to percutaneous endoscopic discectomy. Percutaneous endoscopic discectomy is the least invasive procedure for lumbar disc prolapse. The aim of this study was to analyze the clinical outcome, quality of life, neurologic function, and complications.
Materials and Methods:
One hundred patients with lumbar disc prolapse who were treated with percutaneous endoscopic discectomy from May 2012 to January 2014 were included in this retrospective study. Clinical followup was done at 1 month, 3 months, 6 months, 1 year, and at yearly interval thereafter. The outcome was assessed using modified Macnab's criteria, visual analog scale, and Oswestry Disability Index.
Results:
The mean followup period was 2 years (range 18 months - 3 years). Transforaminal approach was used in 84 patients, interlaminar approach in seven patients, and combined approach in nine patients. An excellent outcome was noted in ninety patients, good outcome in six patients, fair result in two patients, and poor result in two patients. Minor complications were seen in three patients, and two patients had recurrent disc prolapse. Mean hospital stay was 1.6 days.
Conclusions:
Percutaneous endoscopic lumbar discectomy is a safe and effective procedure in lumbar disc prolapse. It has the advantage that it can be performed on a day care basis under local anesthesia with shorter length of hospitalization and early return to work thus improving the quality of life earlier. The low complication rate makes it the future of disc surgery. Transforaminal approach alone is sufficient in majority of cases, although 16% of cases required either percutaneous interlaminar approach or combined approach. The procedure definitely has a learning curve, but it is acceptable with adequate preparations.
Keywords: Endoscopic discectomy, lumbar discectomy, percutaneous discectomy, transforaminal discectomy, lumbar disc
MeSH terms: Disc, herniated, endoscopy, lumbar vertebrae, minimally invasive surgical procedure
INTRODUCTION
Low back and sciatic pain have been one of the most common and disabling spinal disorders recorded in medical history.1 Lumbar disc herniation is a major cause of back pain and sciatica. The surgical management of lumbar disc prolapse has evolved from exploratory laminectomy to percutaneous endoscopic discectomy. Mixter and Bar first published results of laminectomy and discectomy for lumbar disc prolapse.2 Yasargil and Caspar started the use of microscopes for posterior discectomy which limited the skin incision and lead to less muscle and epidural scarring.3,4 Patients had less postoperative pain, early rehabilitation, and early return to work. Due to these advantages, microdiscectomy became the gold standard in disc surgery. Hijikata (1975) independently experimented with mechanical nucleotomy via a 2.6-mm-od cannula that was inserted into the center of the intervertebral disc via a posterolateral access. He reported a satisfactory postoperative outcome in 64% of patients.5 Kambin and Schaffer (1988) used arthroscope for visualization and excision of the disc.6 Yeung developed rigid working channel endoscope for percutaneous endoscopic lumbar discectomy (PELD).7 The advantage of a percutaneous endoscopic discectomy is that the disc is approached posterolaterally through the triangle of Kambin without the need for bone or facet resection thus preserving spinal stability. There is less damage to muscular and ligamentous structures allowing for faster rehabilitation, shorter hospital stay, and earlier return to function.8 Although many studies have shown the efficacy of PELD with good clinical outcome, the percutaneous approach poses challenges to surgeons and the PELD, the learning curve is usually perceived to be steep. Major complications such as nerve root injury, dural tear, haematoma, visceral injury, vascular injury, and infection may occur, possibly resulting from lack of skilled surgical techniques during the learning period.9 The purpose of this study was to report the results of PELD by a single surgeon who had not been previously exposed to this procedure.
MATERIALS AND METHODS
One hundred patients with lumbar disc prolapse treated with percutaneous endoscopic discectomy between May 2012 and January 2014 were included in the study. This was a retrospective study with a mean followup period of two years to assess the clinical outcome, quality of life, neurologic function and complications of PELD. The indications for surgery were patients with lumbar disc prolapse with failed conservative treatment of 6 weeks duration, patients with disc prolapse with neurologic deficit, and patients with Cauda equina syndrome. The duration of symptoms ranged from 1 day to 2 years. All patients had preoperative X-rays and magnetic resonance imaging (MRI) scans of lumbosacral spine, and clinical findings were correlated with MRI pictures. Patients with no neurologic deficit (three patients) or minor neurologic deficits (91 patients) were operated after 6 weeks of failed conservative treatment. Patients with major neurologic deficits such as foot drop (three patients), paraparesis (one patient), or Cauda equina syndrome (two patients) were operated immediately. Patients with lumbar canal stenosis, instability, and previous open surgery at the same level were excluded from the study.
Operative procedure
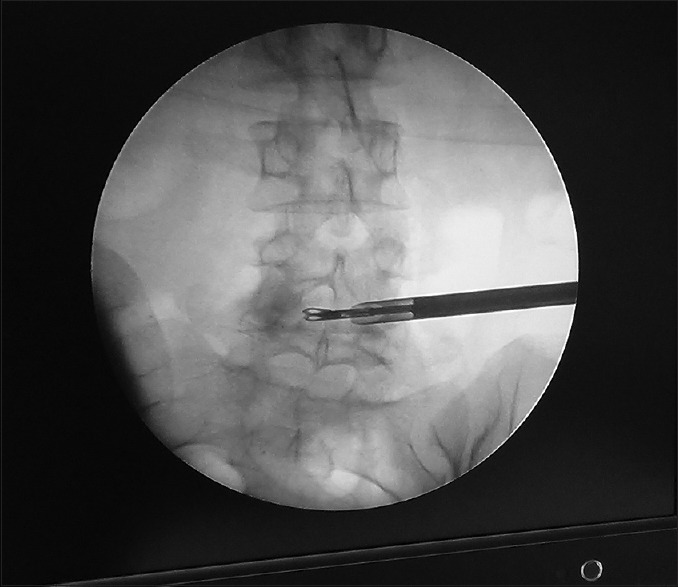
Preoperatively, all patients received 1.5 g of ceftriaxone and sulbactam and 500 mg of amikacin intravenously as antibiotic prophylaxis. The patients were placed prone on a radiolucent operative table. All procedures were done under local anesthesia with continuous monitoring of oxygen saturation, heart rate, and blood pressure. It is important to look for hypoxia, bradycardia, and hypotension due to drug action or pain induced vagal stimulation. For relaxation and comfort of the patient, sedation with intravenous (IV) midazolam (1–2 mg) and fentanyl (100–200 mg) was administered by the anesthetist initially. Subsequent doses of midazolam and fentanyl were given as needed, depending on patient's tolerance to pain. Twenty patients (20%) were uneasy during the operation and required nitrous oxide by mask or propofol infusion. Parts are initially painted with povidone iodine and allowed to dry. Parts were again painted with povidone iodine and draping was done wide enough for a lateral entry point. The skin, subcutaneous tissue, fascia, and muscle layers were infiltrated with 1% lidocaine. Skin entry point was made about 10–14 cm lateral to the posterior midline. An 18 gauge aspiration needle (21-inch length) was inserted such that the needle tip was positioned at the medial pedicular line in the anteroposterior (AP) projection [Figure 1] and on the posterior vertebral borderline in the lateral projection [Figure 2]. The needle was then advanced to the midline in the AP projection.
Figure 1.
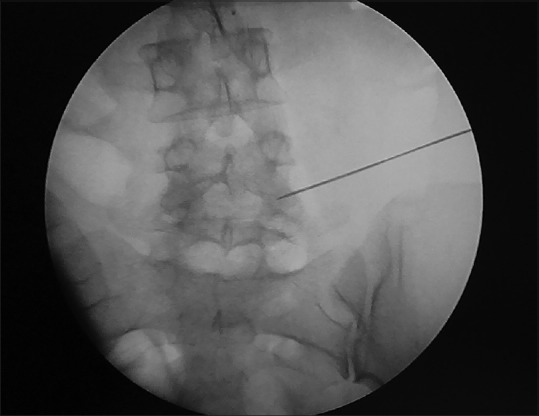
Endoscopic view showing insertion of needle in AP view
Figure 2.

Endoscopic view showing insertion of needle in lateral view
The stylet is removed and discogram was done using methylene blue, normal saline and radiocontrast medium mixed in the ratio of 1:2:2. Discogram reproduced the pain to confirm the pathologic level and methylene blue stains the disc blue, helping in removal. A guidewire was passed into the disc space and the needle was removed. Skin was incised at the entry point for 7 mm in length. Using another needle, the track of the guidewire up to the annulus was infiltrated with local anesthetic. A dilator was inserted over the guidewire into the disc space. The annulus was infiltrated with local anesthetic using the side channel. Once the dilator was inside the disc space at the desired level, guidewire was removed. Operation sheath was then advanced over the dilator. The dilator was removed and endoscope (GORE System from KARL STORZ GmbH and Co. KG Tuttlingen, Germany) was inserted. The disc was directly visualized and removed [Figures 3 and 4]. Initially, all in technique was used. If there is difficulty in removing the disc, then half in half out technique was used. Bleeding was controlled by increasing the pressure of fluid or by bipolar cautery. The surgery was considered to be over when a large blood stained disc fragment is removed with brisk epidural bleeding or removal of multiple disc fragments with visualization of epidural fat or nerve root and complete relief from leg pain. If there was difficulty in removing the fragment, interlaminar approach is used using the same endoscope. Once discectomy was complete, endoscope and sheath are removed. Skin was closed with a single suture.
Figure 3.
Endoscopic view showing endoscope and disc forceps in the disc space
Figure 4.
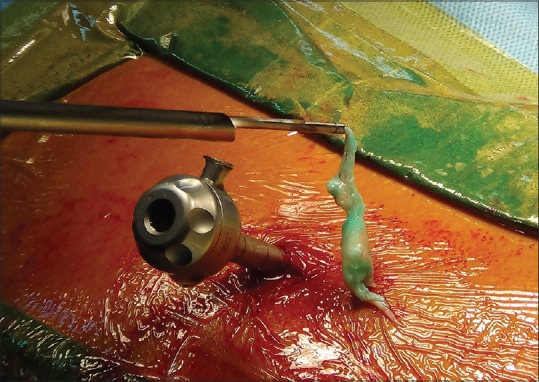
Peroperative photograph showing removal of extruded disc fragment
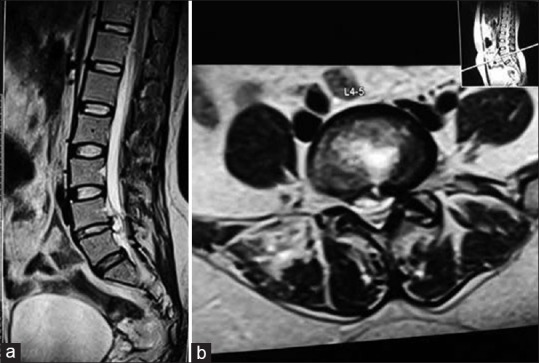
The patient was monitored in the post operative ward for one hour after the surgery. Patient was allowed to walk afterwards. A postoperative MRI scan was done within few hours after surgery to assess decompression and disc excision [Figures 5 and 6]. Followup MRI was done only in patients with recurrence of sciatica. Patient was discharged the same day or next day depending on comfort level. Skin suture was removed after a week. As a protocol, all patients were advised to take rest at home for a period of 1 month. However, at followup, patients with sedentary work revealed that they started working as early as 2 days after surgery. Followup was done at 1 month, 3 months, 6 months, 1 year, and then yearly after the surgery. At followup, patient was assessed regarding his symptoms, neurologic status, visual analog scale (VAS), and Oswestry Disability Index (ODI). A modified Macnab's criteria were used for grading the results. Excellent-no pain/restriction of activity and being able to do all activities; good-occasional pain with relief of presenting symptoms and returning to work with some modification; fair-some improved functional capacity but still handicapped or unemployed and poor results – having objective symptoms of root involvement or repeat surgery at the index level. The results were reviewed by the author himself and not by an independent reviewer. The ODI domains are the following: Pain intensity, personal care, lifting, walking, sitting, standing, sleeping, sex life, social life, and traveling. Each section contains six statements that are scored from zero (minimum degree of difficulty in that activity) to five (maximum degree of difficulty). If more than one statement is marked in each section, the highest score should be taken. The total score is obtained by summing up the scores of all sections, giving a maximum of fifty points. The final score is expressed as a percentage with the following formula: (total score/(5 × number of questions answered) × 100%.10
Figure 5.

(a) Preoperative magnetic resonance imaging T2WI mid sagittal section showing large disc at L4 L5 level (b) Preoperative magnetic resonance imaging T2WI axial section showing large central disc
Figure 6.
(a) Postoperative magnetic resonance imaging T2WI sagittal section showing decompression at L4 L5 level (b) Postoperative magnetic resonance imaging T2WI axial section showing decompression
RESULTS
The mean age of patients was 40.29 years (range 15–84 years). There were 67 males and 33 females. There were 12 disc protrusions, 81 extrusions, and 7 sequestrated discs. Forty six patients had right-sided radiculopathy, 44 patients had left-sided radiculopathy, eight patients had bilateral sciatica, and two patients had Cauda equina syndrome. The straight leg raising test was positive in 97 patients and negative in three patients. The neurologic deficit was present in 97 patients and absent in three patients. There were fifty patients with L4–L5 disc prolapse, 29 patients with L5-S1 disc prolapse, five patients with L3–L4 disc prolapse, one patient with L2–L3 disc prolapse, one patient with L1–L2 disc prolapse, and 14 patients with two level disc prolapse. The mean operative time was 45 min (range 15 min–3 h). The duration of surgery was long in the initial few cases and in patients who required combined or bilateral approach. This is partly due to learning curve. Transforaminal approach was used in 84 patients, interlaminar approach in seven patients, and combined approach in nine patients. Three patients had bilateral decompressions. Four patients had symptoms on the contralateral side of disc prolapse and were treated from the side of disc prolapse and had complete relief. The mean hospitalization was 1.6 days (range 6 h–5 days). Hospital stay was more in some patients due to insurance clearance and not related to procedure. The mean followup period was 2 years (range 18 months-3 years). All patients who were working preoperatively returned to work. The mean time to return to work was 36 days (range 2–100 days). Two patients with Cauda equina syndrome recovered completely. Another patient with L2–L3 disc prolapse presented with Grade I power of both lower limbs also recovered completely in 3 months. There were three patients with unilateral foot drop of which two recovered to Grade IV power and one did not recover. This patient had gross wasting of muscles before surgery and was warned about nonrecovery of foot drop. However, he had relief from back and leg pain and returned to his work. All other patients recovered from their motor deficits completely at 6 months. Of the one hundred patients, excellent outcome was noted in ninety patients, good outcome in six patients, fair result in two patients, and poor result in two patients. The mean VAS reduced drastically from 8.2 preoperatively to 1.8 postoperatively (P < 0.001). ODI also showed marked improvement from a preoperative 54% to a postoperative 8% (P < 0.001). For statistical analysis of both VAS and ODI, Student's paired t-test was used and found to be highly significant.
Minor complications were seen in three patients. One patient had a dural puncture and postspinal headache which settled uneventfully. One patient had an accidental intrathecal injection of urograffin during epidurography for interlaminar approach. He was treated with anticonvulsants (sodium valproate) and observation. He did not have any long term complications. After this complication, urograffin was replaced by iopamidol. One patient with two level disc prolapse had transient weakness of L1 root and recovered completely in 6 weeks. There were no cases of discitis, root damage, hematoma, vascular injury, facet injury, abdominal organ injury, and wound infection. No patient required catheterization, blood transfusion, or IV fluids. Two patients had recurrent symptoms at 5 months and 6 months after surgery. Repeat MRI scan done showed recurrent disc prolapse at the same level and same side. Both patients were treated with microdiscectomy as the patients opted for open surgery. These patients had excellent relief from symptoms after microlumbar discectomy.
DISCUSSION
Conventional open surgery was considered to be the “gold standard” for treating herniated intervertebral disc. With the use of microlumbar discectomy, there was a significant reduction in morbidity of open surgery.3,4 Microlumbar discectomy has definitive advantages over open surgery in terms of hospital stay, blood loss, postoperative pain and epidural fibrosis. However, the disadvantages of open surgery are still present with microlumbar discectomy. These disadvantages include retraction and denervation of paraspinal muscles, postoperative pain, blood loss, bone resection, and scarring. Microdiscectomy is associated with significant intraoperative and postoperative complications.11 Long term complications of microlumbar discectomy include recurrence, epidural fibrosis and spinal instability which are a challenge even for an experienced spinal surgeon. In many cases, it is the beginning of a failed back surgery syndrome.11 Results of microlumbar discectomy in recurrent disc prolapse are not good when compared to primary cases.12 Due to these limitations of microdiscectomy, microendoscopic discectomy was introduced. Jhala and Mistry (2010) reported results of microendoscopic discectomy in one hundred patients with overall 91% good-to-excellent results. They had a dural tear in seven patients, root injury in one patient, recurrence in four patients, discitis in four patients, and facet removal in five patients. Four patients had to be reoperated. Overall 91% of their patients had good-to-excellent results.13 Kaushal and Sen (2014) reported satisfactory results in 90% patients using posterior endoscopic discectomy out of three hundred cases. They reported dural tears and discitis in five patients each, nerve root injury in two patients. However, they had excluded first fifty patients due to learning curve.14 Kulkarni et al. (2014) reported the results of microendoscopic discectomy in 188 patients. They reported 5% dural tear, 2.1% residual disc herniation, 1.5% recurrence, wrong level 0.5%, and 0.5% infection rate.15
Endoscopic discectomy via a percutaneous transforaminal posterolateral approach is an alternative technique used to treat lumbar disc herniations.15 Advances in instrumentation now allow for a “working channel” through which various tools can be passed under direct endoscopic visualization for the safe removal of disc material. The advantages of this technique include no bone resection, low morbidity, small scar (0.5–1 cm), no blood loss, no requirement for IV fluids, no requirement for catheterization, short hospital stay, very low complication rates, rapid recovery and return to work, and reduced cost.16,17,18,19,20,21 As the surgery is done under local anesthesia, it can be done even in patients who are not fit for general anaesthesia. If transforaminal approach is not possible due to high iliac crest, percutaneous interlaminar approach is done using the same system.22
In this study, seven patients required percutaneous interlaminar approach and nine patients required combined transforaminal and interlaminar approach. Patients with L5-S1 disc prolapse with high iliac crest were treated with the interlaminar approach. Combined approach was used in cases when the fragment could not be removed with the transforaminal approach. This indicates that 16% of cases were not suitable for transforaminal approach alone. This high percentage is partly due to learning curve. It is not possible to perform transforaminal discectomy in all cases. However, with experience and techniques such as foraminoplasty, transiliac approach, it is possible to perform more number of cases with transforaminal approach. In the author's series, dural puncture was seen in one patient due to injury by the discectomy forceps. As it is a closed space, and small sized tear, no intervention was needed. The incidence of dural tear is low because dural sac is not exposed routinely. The rate of nerve root injury again is low because surgery is done under local anesthesia. Awake patient will never allow the surgeon to cause permanent root damage. In this study only one patient had transient root weakness which recovered completely in 6 weeks.
Yeung and Tsou (2002) described results of posterolateral disc excision in 307 patients with minimal followup period of 1 year. They reported satisfactory result rate in 89.7% and poor results in 10.3 patients. The complications were deep infection in two, thrombophlebitis in two, dysesthesia in six, and dural tear in one patient.23
Chae et al. (2009) reported 94.77% satisfactory results with percutaneous endoscopic discectomy in 153 patients with difficult, noncontained lumbar disc herniations.24 In author's series, overall good-to-excellent result is 96% which is consistent with the literature. The complication rate is extremely low. No patient had wound infection which is consistent with very low infection rate with transforaminal endoscopic disc surgery as reported in the literature (0.1–0.65%).23,25 Low infection rate is due to minimal damage to normal tissue, less bleeding, short operative time, continuous saline irrigation, and surgical technique. In our study, the recurrence rate is 2% which is comparable what is reported in the literature (3–7%). The overall complication rate in the present study was statistically compared with the complication rate of microendoscopic discectomy using Chi-square test. The complication rate in the authors series was significantly less than that of microendoscopic discectomy (MED) series by Jhala and Mistry (P < 0.01). However, when compared with the complication rate reported by Kulkarni et al., lower complication rate was not statistically significant (P < 0.1). However, randomized controlled studies with a large number of patients are needed to confirm lower complication rates.
Few randomized control studies have shown that the results of microdiscectomy and endoscopic discectomy are the same, but the endoscopic surgery has the advantages of short hospital stay, low morbidity, and rapid recovery.16,17,18 The main disadvantage of percutaneous endoscopic discectomy is a long learning curve. The author had no experience in endoscopic procedures before starting this study. The author had studied all the available literature, attended workshop, and live surgery before starting this study. Long operating time in the initial cases need for alternate or additional approach as highlighted in this study is due to learning curve. However, the learning curve is not long as it was presumed earlier. If the technique of PELD is studied and executed well in properly selected cases, then excellent results can be obtained. As mentioned earlier, cases with canal stenosis were not considered for PELD as the author was well versed with foraminoplasty at the beginning. Ahn et al. (2015) recommended practicing transforaminal epidural block before venturing into PELD, which enables beginners to develop the stable learning curve.9
There is a long standing debate between microendoscopic discectomy and percutaneous discectomy. Hence, far the existing literature is not conclusive of favoring one procedure over the other.26,27 However, PELD techniques are slowly and steadily gaining more prominence. The posterolateral approach does not violate the spinal canal which is responsible for long term unsatisfactory results with open surgery. Ruetten et al. (2008) reported prospective randomized control study of microdiscectomy and endoscopic discectomy in 178 patients. The final outcome was similar in both groups (96% satisfactory results).28 However, endoscopic procedure has significant advantages over microdiscectomy in terms of operative time, cost, rehabilitation, back pain, scarring, easier revision, complications, and training of assistants. Gibson et al. (2012) did extensive review of literature regarding the results of transforaminal endoscopic disc surgery versus microlumbar discectomy and concluded that results of transforaminal endoscopic surgery are equal or better than microdiscectomy.29 They concluded that it is only a matter of time before transforaminal surgery is widely practiced and accepted as gold standard.29
This study has some limitations. First, it is a retrospective study, and the results are reviewed by the author himself. Second, it includes the entire spectrum of lumbar disc herniation including L1–L2 and L2–L3 levels, two level disc prolapse and cases with Cauda equina syndrome which can influence the final outcome.
CONCLUSIONS
PELD is a safe and effective procedure in lumbar disc prolapse. The result of PELD is equal to open lumbar microdiscectomy or MED in properly selected patients, with a low complication rate. It has the advantage that it can be performed on a day care basis under local anesthesia with shorter length of hospitalization and early return to work thus improving the quality of life earlier.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kambin P, editor. Arthroscopic and Endoscopic Spinal Surgery. 2nd ed. Totowa, New Jersey: Humana Press; 2005. History of surgical management of herniated lumbar discs from cauterization to arthroscopic and endoscopic spine surgery; pp. 1–27. [Google Scholar]
- 2.Mixter WJ, Barr J. Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med. 1934;211:208–15. [Google Scholar]
- 3.Yasargil MG. Microsurgical operation for herniated lumbar disc. In: Wullenweber R, Brock M, Hamer J, Klinger M, Spoerri O, editors. Advances in Neurosurgery. Berlin: Springer-Verlag; 1977. p. 81. [Google Scholar]
- 4.Caspar W. A new surgical procedure for lumbar disc herniation causing less tissue damage through microsurgical approach. In: Wullenweber R, Brock M, Hamer J, Klinger M, Spoerri O, editors. Advances in Neurosurgery. Berlin: Springer-Verlag; 1977. pp. 74–7. [Google Scholar]
- 5.Hijikata S. Percutaneous nucleotomy. A new concept technique and 12 years’ experience. Clin Orthop Relat Res. 1989;238:9–23. [PubMed] [Google Scholar]
- 6.Kambin P, Schaffer JL. Percutaneous lumbar discectomy. Review of 100 patients and current practice. Clin Orthop Relat Res. 1989;238:24–34. [PubMed] [Google Scholar]
- 7.Yeung AT. Minimally Invasive Disc Surgery with the Yeung Endoscopic Spine System (YESS) Surg Technol Int. 1999;8:267–77. [PubMed] [Google Scholar]
- 8.Peng CW, Yeo W, Tan SB. Percutaneous endoscopic lumbar discectomy: Clinical and quality of life outcomes with a minimum 2 year followup. J Orthop Surg Res. 2009;4:20. doi: 10.1186/1749-799X-4-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahn SS, Kim SH, Kim DW. Learning curve of percutaneous endoscopic lumbar discectomy based on the period (Early vs. Late) and technique (in-and-out vs. in-and-out-and-in): A retrospective comparative study. J Korean Neurosurg Soc. 2015;58:539–46. doi: 10.3340/jkns.2015.58.6.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Longo UG, Loppini M, Denaro L, Maffulli N, Denaro V. Rating scales for low back pain. Br Med Bull. 2010;94:81–144. doi: 10.1093/bmb/ldp052. [DOI] [PubMed] [Google Scholar]
- 11.Kraemer R, Wild A, Haak H, Herdmann J, Krauspe R, Kraemer J. Classification and management of early complications in open lumbar microdiscectomy. Eur Spine J. 2003;12:239–46. doi: 10.1007/s00586-002-0466-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Acharya KN, Nathan TS, Kumar JR, Menon KV. Primary and revision lumbar discectomy: A three-year review from one center. Indian J Orthop. 2008;42:178–81. doi: 10.4103/0019-5413.40254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jhala A, Mistry M. Endoscopic lumbar discectomy: Experience of first 100 cases. Indian J Orthop. 2010;44:184–90. doi: 10.4103/0019-5413.62051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaushal M, Sen R. Posterior endoscopic discectomy: Results in 300 patients. Indian J Orthop. 2012;46:81–5. doi: 10.4103/0019-5413.91640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kulkarni AG, Bassi A, Dhruv A. Microendoscopic lumbar discectomy: Technique and results of 188 cases. Indian J Orthop. 2014;48:81–7. doi: 10.4103/0019-5413.125511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mayer HM, Brock M. Percutaneous endoscopic discectomy: Surgical technique and preliminary results compared to microsurgical discectomy. J Neurosurg. 1993;78:216–25. doi: 10.3171/jns.1993.78.2.0216. [DOI] [PubMed] [Google Scholar]
- 17.Hermantin FU, Peters T, Quartararo L, Kambin P. A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy. J Bone Joint Surg Am. 1999;81:958–65. doi: 10.2106/00004623-199907000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Lee DY, Shim CS, Ahn Y, Choi YG, Kim HJ, Lee SH. Comparison of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for recurrent disc herniation. J Korean Neurosurg Soc. 2009;46:515–21. doi: 10.3340/jkns.2009.46.6.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ahn Y, Lee SH, Lee JH, Kim JU, Liu WC. Transforaminal percutaneous endoscopic lumbar discectomy for upper lumbar disc herniation: Clinical outcome, prognostic factors, and technical consideration. Acta Neurochir (Wien) 2009;151:199–206. doi: 10.1007/s00701-009-0204-x. [DOI] [PubMed] [Google Scholar]
- 20.Hoogland T, van den Brekel-Dijkstra K, Schubert M, Miklitz B. Endoscopic transforaminal discectomy for recurrent lumbar disc herniation: A prospective, cohort evaluation of 262 consecutive cases. Spine (Phila Pa 1976) 2008;33:973–8. doi: 10.1097/BRS.0b013e31816c8ade. [DOI] [PubMed] [Google Scholar]
- 21.Lee S, Kim SK, Lee SH, Kim WJ, Choi WC, Choi G, et al. Percutaneous endoscopic lumbar discectomy for migrated disc herniation: Classification of disc migration and surgical approaches. Eur Spine J. 2007;16:431–7. doi: 10.1007/s00586-006-0219-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Choi G, Lee SH, Raiturker PP, Lee S, Chae YS. Percutaneous endoscopic interlaminar discectomy for intracanalicular disc herniations at L5-S1 using a rigid working channel endoscope. Neurosurgery. 2006;58(1 Suppl):ONS59–68. doi: 10.1227/01.neu.0000192713.95921.4a. [DOI] [PubMed] [Google Scholar]
- 23.Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: Surgical technique, outcome, and complications in 307 consecutive cases. Spine (Phila Pa 1976) 2002;27:722–31. doi: 10.1097/00007632-200204010-00009. [DOI] [PubMed] [Google Scholar]
- 24.Chae KH, Ju CI, Lee SM, Kim BW, Kim SY, Kim HS. Strategies for noncontained lumbar disc herniation by an endoscopic approach: Transforaminal suprapedicular approach, semi-rigid flexible curved probe, and 3-dimensional reconstruction CT with discogram. J Korean Neurosurg Soc. 2009;46:312–6. doi: 10.3340/jkns.2009.46.4.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Choi KB, Lee CD, Lee SH. Pyogenic spondylodiscitis after percutaneous endoscopic lumbar discectomy. J Korean Neurosurg Soc. 2010;48:455–60. doi: 10.3340/jkns.2010.48.5.455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sinkemani A, Hong X, Gao ZX, Zhuang SY, Jiang ZL, Zhang SD, et al. Outcomes of microendoscopic discectomy and percutaneous transforaminal endoscopic discectomy for the treatment of lumbar disc herniation: A comparative retrospective study. Asian Spine J. 2015;9:833–40. doi: 10.4184/asj.2015.9.6.833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li M, Yang H, Yang Q. Full-endoscopic technique discectomy versus microendoscopic discectomy for the surgical treatment of lumbar disc herniation. Pain Physician. 2015;18:359–63. [PubMed] [Google Scholar]
- 28.Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: A prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008;33:931–9. doi: 10.1097/BRS.0b013e31816c8af7. [DOI] [PubMed] [Google Scholar]
- 29.Gibson JN, Cowie JG, Iprenburg M. Transforaminal endoscopic spinal surgery: The future ‘gold standard’ for discectomy? – A review. Surgeon. 2012;10:290–6. doi: 10.1016/j.surge.2012.05.001. [DOI] [PubMed] [Google Scholar]


