Abstract
Background:
Open fractures of tibia have posed great difficulty in managing both the soft tissue and the skeletal components of the injured limb. Gustilo Anderson III B open tibial fractures are more difficult to manage than I, II, and III A fractures. Stable skeletal fixation with immediate soft tissue cover has been the key to the successful outcome in treating open tibial fractures, in particular, Gustilo Anderson III B types. If the length of the open wound is larger and if the exposed surface of tibial fracture and tibial shaft is greater, then the management becomes still more difficult.
Materials and Methods:
Thirty six Gustilo Anderson III B open tibial fractures managed between June 2002 and December 2013 with “fix and shift” technique were retrospectively reviewed. All the 36 patients managed by this technique had open wounds measuring >5 cm (post debridement). Under fix and shift technique, stable fixation involved primary external fixator application or primary intramedullary nailing of the tibial fracture and immediate soft tissue cover involved septocutaneous shift, i.e., shifting of fasciocutaneous segments based on septocutaneous perforators.
Results:
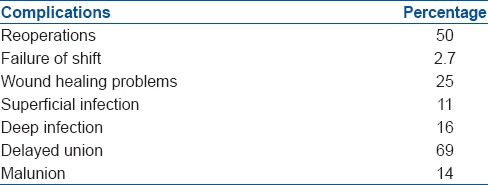
Primary fracture union rate was 50% and reoperation rate (bone stimulating procedures) was 50%. Overall fracture union rate was 100%. The rate of malunion was 14% and deep infection was 16%. Failure of septocutaneous shift was 2.7%. There was no incidence of amputation.
Conclusion:
Management of Gustilo Anderson III B open tibial fractures with “fix and shift” technique has resulted in better outcome in terms of skeletal factors (primary fracture union, overall union, and time for union and malunion) and soft tissue factors (wound healing, flap failure, access to secondary procedures, and esthetic appearance) when compared to standard methods adopted earlier. Hence, “fix and shift” could be recommended as one of the treatment modalities for open III B tibial fractures.
Keywords: External fixation, interlocking nail, open fractures, septocutaneous shift, tibial fractures
MeSH terms: Tibial fractures, open fractures, nailing, intramedullary, surgical flaps
INTRODUCTION
Various methods have been employed in stabilizing open tibial fractures, in particular, Gustilo Anderson III B types.1,2,3,4 Primary external fixator application5,6,7,8 has been used over a long period of time with great success. This form of fixation is of choice6 while dealing with open tibial fractures with a lot of contamination, segmental bone loss, segmental comminution, and crushing of surrounding musculotendinous units. Primary unreamed nailing8,9 was used in the recent past but has been out of favor currently. Primary reamed nailing5,6,10,11,12,13 has been used with greater success than unreamed nailing for all types of open tibial fractures including III B types. Reamed nailing has been the procedure of choice in open tibial fractures with lesser contamination and lesser comminution.6
Soft tissue injuries have been managed by different methods. The list includes primary suturing,14 fasciocutaneous flaps,15,16,17,18,19 sural flaps,20 propeller flaps,16,21 adipofascial flaps,22 pedicled muscle flaps,17,18,19,23,24 free perforator,25,26 and free muscle flaps.23,25,26 Various other techniques that are rarely used are bipedicled fasciocutaneous flaps,27 multiple relaxing incisions;28 Taylor spatial frame for acute deformation to close open wound and delayed correction;29,30 negative pressure wounds therapy31 in the 1st week followed by flap or Split Skin Graft (SSG), tissue expanders for converting III B to III A open fractures, and free fibular osteoseptocutaneous flap graft.32,33 Although the above said fasciocutaneous and muscle flaps are advantageous in managing small to medium sized soft tissue defects, their role in managing open defects with skin wounds >10 cm is questionable. Each of these techniques has some disadvantage while managing open tibial fractures while dealing with greater soft tissue defects. This includes flap tip necrosis,34 limited excursion of flap,35 donor site morbidity, esthetic appeal, etc., Septocutaneous shift comes handy in situations where the soft tissue defect is larger and where soft tissue cover is needed immediately.
Septocutaneous shift is performed by shifting the septo-fasciocutaneous composite segment based on multiple septocutaneous perforators36,37 of the leg which are neither skeletonized nor rotated. The perforators are never dissected and only the interperforator fascia is divided. This results in greater mobilization of fasciocutaneous segment. This shift can be performed immediately following skeletal fixation and the exposed fracture or the skeleton can be covered with the septocutaneous segment (flap). The resulting raw area following the shift is covered with split skin grafting after a week.
"Fix and shift" technique of managing open tibial fracture involves primary external fixator or primary reamed nailing to stabilize the fracture and septocutaneous shift for covering the soft tissue defect.
MATERIALS AND METHODS
Two hundred and forty three patients with 245 open tibial fractures were managed between June 2002 and December 2013. Forty two Gustilo Anderson III B fractures from this group were treated by fix and shift technique. The results of 36 patients with complete followup were analyzed and are discussed here. Followup of patients ranged from a minimum of 6 months to a maximum of 29 months.
The patients, on admission, were resuscitated by Advanced Trauma Life Support protocol. Intravenous antibiotics were administered within 3 h of admission. Neurovascular assessment was carefully done and recorded along with the description of the fracture and the other injuries. External fixator was used to fix fractures with significant contamination, muscle crushing, segmental bone loss, and/or segmental comminution. Primary reamed nailing was the choice for fractures with minimal contamination. Those patients who underwent septocutaneous shift and who had complete followup were taken up for analysis in this article.
The inclusion criteria for performing septocutaneous shift were an oval shaped open wound with the length of the wound (parallel to the long axis of tibia) greater than the breadth of the same wound. Age was not a contraindication as this technique was used in children, adults, and elderly people. Any breach of the posterior compartment of the leg like lacerations over the calf and extensive bruising or necrosis of the skin over calf were considered as contraindications to this technique. Skeletal and soft tissue procedures were performed by the author himself. The study was approved by ethical committee.
The fractured limb was examined under anesthesia to assess the extent of the injury. The open wound was measured and the perforators on the medial and lateral aspect of the leg were localized with handheld Doppler machine without contaminating the wound. Following wound debridement (including postdebridement measurement) and skeletal fixation, a deep longitudinal incision up to the deep fascia was made on the midcalf region. Sural nerve and lesser saphenous vein were protected if encountered. The incision was extended both proximally and distally. While extending the incision distally, due care was taken to protect tendo Achilles by stopping short the incision proximal to the Tendon. Blunt dissection was carried out underneath deep fascia on either side up to their respective septae. The medial septum on the medial side separates tibia from posterior compartment of the leg [Figure 1]. The skin and fascia of the medial half of the calf were shifted pivoting on the septum to cover the anterior open wound. If the shift of this fasciocutaneous unit was found to be inadequate, then the interperforator-septal-fascia was divided by sharp dissection [Figure 2] after carefully identifying and protecting the perforators on the septum either by direct vision or by loupe. This division was done as close to the base of the septum as possible. This division gives greater excursion for the septo-fasciocutaneous unit to cover the anterior defect. Utmost care was taken to ensure that the perforators were neither severed nor skeletonized. Similar dissection was done on the lateral side. The lateral intermuscular septum separates peroneal compartment from superficial posterior compartment. This septum was also mobilized by incising interperforator-septal-fascia which helped in shifting the lateral septocutaneous unit. The lateral unit moves lesser than the medial unit because the lateral unit is still anchored by the intermuscular septum dividing anterior compartment from peroneal compartment. This septum was further mobilized by releasing interperforator-septal-fascia for augmenting the shift of the lateral septocutaneous unit. The lateral septocutaneous unit in conjunction with medial one closes the skin defect anteriorly. The surgical wound that followed the above said posterior incision was covered with split skin grafting after 1 week.
Figure 1.
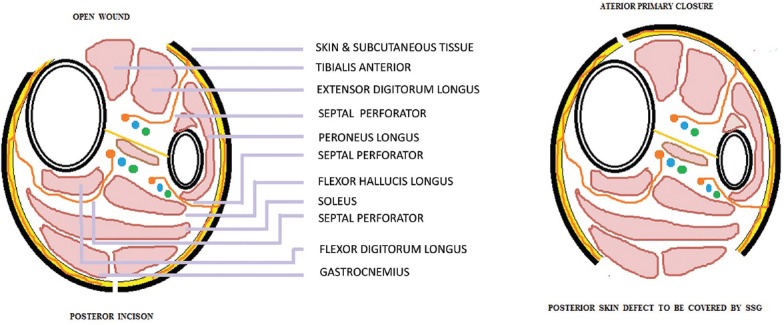
Schematic diagram showing the septocutaneous perforators of the leg in the cross-sectional plane
Figure 2.
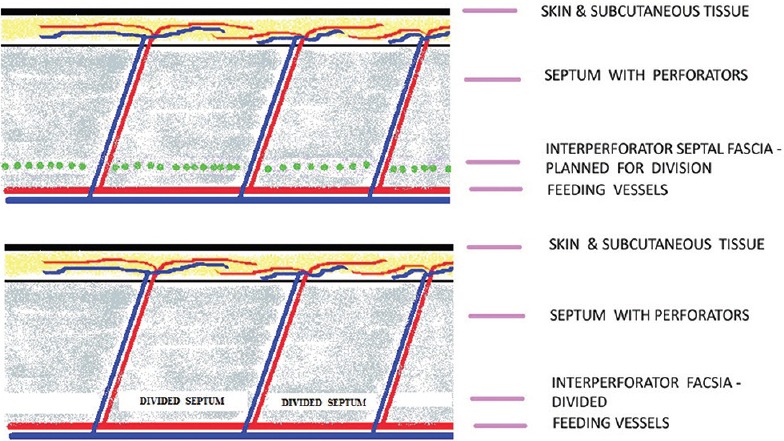
Schematic diagram showing the division of interperforator-septal-fascia
Nonweight bearing mobilization was advised for patients with external fixators once their soft tissue healing was complete. Patients who had a stable fixation without any bone loss were managed with fixator removal, AK plaster cast after the completion of soft tissue healing. Patients who underwent bone grafting while on external fixator were allowed to weight bear after fixator removal but with plaster cast. Patients who were managed by reamed nailing following fixator removal were allowed to weight bear immediately after nailing. Patients who were subjected to reamed nailing and bone grafting after the removal of fixator were mobilized initially without weight bearing. They were allowed to weight bear once the radiographs showed signs of bone healing. Those patients who were managed by primary reamed nailing were allowed to weight bear once the soft tissue healing was complete.
RESULTS
Of the total of 115 Gustilo Anderson III B fractures [Table 1], 36 patients with 36 fractures remained under complete followup. The age of the patients varied from 11 years to 70 years. Of these 36 fractures, 5 were in the proximal third of tibia [Figure 3], 13 in the middle third [Figure 4], three were segmental fractures [Figures 5 and 6], 15 in the distal third [Figure 7] and one in pediatric age group [Figure 8]. Nine fractures (25%) belonged to C3.3 category (2 of 41C3.3, 4 of 42C3.3, and 3 of 43C3.3) indicating significant segmental multifragmented nature of the fractures [Table 2].
Table 1.
Types of fractures
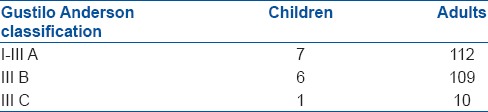
Figure 3.
(a) Clinical photograph (preoperative) of 70 years old lady showing Gustilo Anderson III B open proximal third tibial fracture (b) Preoperative x-ray anteroposterior view showing fracture proximal tibia (c) Clinical photograph showing external fixator in situ with fasciocutaneous skin flap (d) Postoperative X-ray showing external fixator (e) Clinical photograph showing wound healing after removal of external fixator (f) Clinical photograph showing exposure of nonunion site for bone grafting, secondary nailing also done (g) Clinical photograph showing range of motion and healed wounds (h) X-ray anteroposterior and lateral views of leg bones showing fracture union
Figure 4.
(a) Clinical photograph (preoperative) of a 45 years old male showing Gustilo Anderson III B middle third tibial fracture (b) X-ray of leg bones anteroposterior view showing fracture middle 1/3rd tibia (c) Clinical photograph showing external fixator in situ with fasciocutaneous skin flap (d) X-ray of leg bones anteroposterior view showing external fixator in situ (e) Clinical photograph showing healing by fascio-septo-cutaneous shift while in external fixator (f) Clinical photograph showing healed wound after removal of external fixator (g) X-ray of leg bones anteroposterior and lateral views after removal of external fixator showing gap nonunion (h) Peroperative photograph showing plating and bone grafting (i) X-ray of leg bones anteroposterior and lateral views showing bone grafting and plating (j) Clinical photograph after plating showing well healed wounds (k) X-ray of leg bones anteroposterior and lateral views showing fracture union after plate removal (l) Clinical photograph in standing position showing healed wounds
Figure 5.
(a) Clinical photograph (preoperative) of a 29 years old male showing Gustilo Anderson III B segmental tibial fracture (b) Preoperative x-ray of leg bones anteroposterior and lateral views showing segmental fracture tibia (c) Clinical photograph showing external fixator in situ (d) X-ray of leg bones anteroposterior view showing external fixator in situ (e) Clinical photograph showing exposure of nonunion site for the bone grafting and nailing (f) Clinical photograph showing septo cutaneous shift (g) Clinical photograph showing final soft tissue healing (h) X-ray of leg bones anteroposterior and lateral views showing fracture union and nail in situ
Figure 6.
(a) Clinical photograph (preoperative) of a 20 years old male showing Gustilo Anderson III B segmental tibial fracture (b) Preoperative x-ray of leg bones anteroposterior view showing segmental fracture of tibia (c) X-ray of leg bones anteroposterior and lateral views showing external fixator in situ (d)Clinical photograph showing external fixator in situ (e) X-ray of leg bones anteroposterior and lateral views showing fracture union following secondary nailing (f) Clinical photograph showing flexion of knee (g) Clinical photograph showing extension of knee (h) Clinical photograph showing standing position (anterior) (i) Clinical photograph showing standing position (posterior)
Figure 7.
(a) Clinical photograph (preoperative) of a 33 years old male showing Gustilo Anderson III B distal third tibial fracture (b) Preoperative x-ray of leg bones anteroposterior view showing distal third tibial fracture (c) Clinical photograph showing external fixator and medial wound (d) Clinical photograph showing septo cutenaeous shift (e) Clinical photograph showing soft tissue healing (anteromedial) (f) Clinical photograph showing soft tissue healing (posterolateral) (g) X-ray of leg bones anteroposterior and lateral views showing fracture union following secondary nailing
Figure 8.
(a) Clinical photograph (preoperative) of 11 years old boy showing Gustilo Anderson grade III B middle third tibial fracture (b) Preoperative x-ray of leg bones anteroposterior and lateral views showing fracture both bone legs middle 1/3 (c) Clinical photograph showing external fixator in situ (d) X-ray of leg bones anteroposterior and lateral views showing fracture union (e) Clinical photograph showing soft tissue healing in external fixator (f) Clinical photograph showing septo cutaneous shift (g) Clinical photograph showing soft tissue healing (anteromedial)
Table 2.
Clinical details of the patients
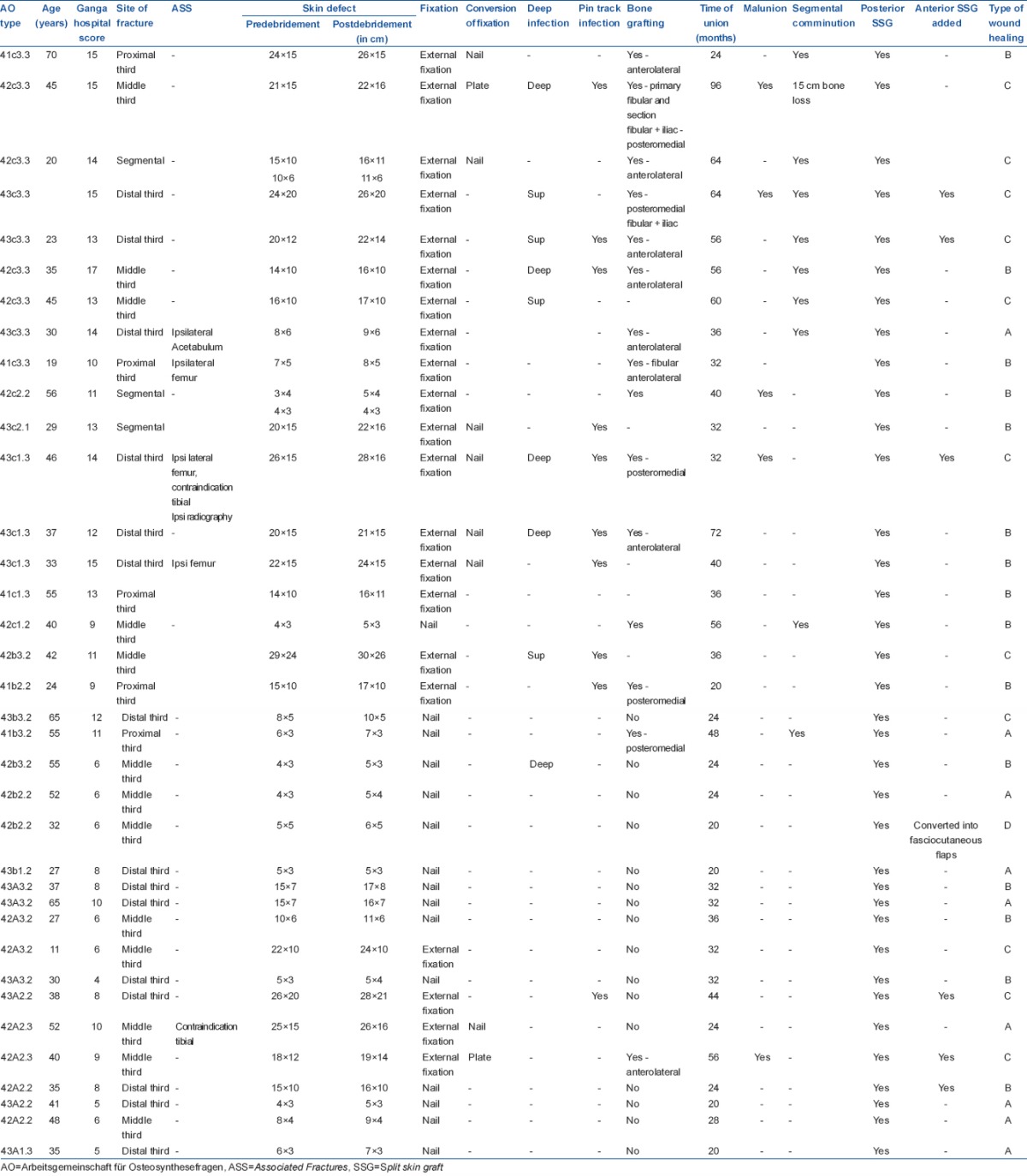
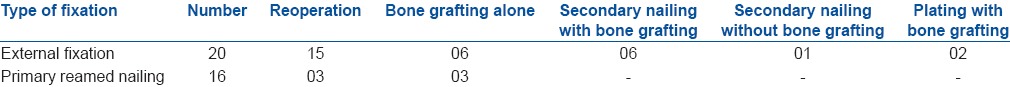
Eighteen patients (50%) achieved primary bone union, [36% (13/36) in nailing group and 14% (5/36) in fixator group]. The average time to union for all 36 fractures was 38 weeks. The fractures in the external fixator group united at an average of 46 weeks and those in primary nailing group took 29 weeks to unite. The fractures categorized as “AO-C3.3” united at an average of 54 weeks. The rate of malunion was 14% and delayed union was 69%. Bone grafting was performed in 17 patients (47%). Fourteen of external fixator group and three of nailing group underwent bone grafting. Bone grafting and/or change of fixation were considered as reoperations6 the rate of which was 50% in total - 42% (15/36) in external fixator group and 8% (3/36) in nailing group [Tables 3 and 4].
Table 3.
The type of fixation with numbers
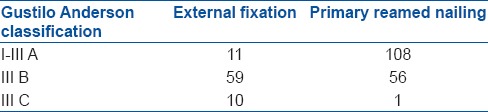
Table 4.
Type of fixation and further procedures
Twenty (56%) of these fractures were fixed by external fixator and 16 (44%) fractures by reamed intramedullary nailing [Table 3]. All the patients with open wounds >20 cm were fixed with external fixator. Among the 10–20 cm group, five underwent external fixation and five underwent nailing [Table 5]. Among the <10 cm group, eleven were treated by nailing and two by external fixation. In retrospect, it can be concluded that wounds >10 cm in length had severe contamination with or without bone loss and were better treated by an external fixator.
Table 5.
The number of fractures with their respective wound length groups

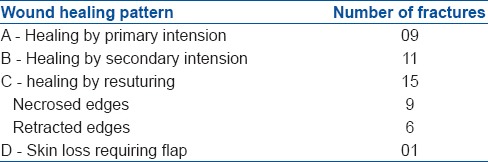
All of the 36 patients needed split skin grafting over the release incision site. Six (16%) of these patients needed SSG on the anterolateral aspect of the leg in addition to posterior SSG, which was a preplanned step. In these six cases, the shaft of tibia was covered by posteromedial septocutaneous shift and the anterolateral muscles were allowed to remain open to be covered by SSG later. Posterior and anterior SSG were performed simultaneously after 1 week. Wound healing of the septocutaneous units on the anterior aspect of the leg was assessed on the basis of classification suggested by Rajasekaran et al.14 (9-A, 11-B, 15-C, and 1-D) [Table 6]. Patients (41%) of the “C” group included 16% of the anterior SSG patients also. Hence, the actual “C” type healing occurred only in 25% of the patients.
Table 6.
The number of fractures with their respective wound healing pattern
Complications [Table 7] of septocutaneous shift were “failure” of the shift (1/36–2.7%) and “wound edge necrosis” requiring resuturing (9/36). This edge necrosis was closer to the fracture site only in four cases which was managed by resuturing. In five of the cases, the edge necrosis was away from the fracture site. The soft tissue procedures to solve the above said complications were not classified as reoperations.6 Superficial infection occurred in four patients (11%) and deep infection occurred in five patients (14%). Pin tract infection occurred in 10/36 (27%). One patient developed chronic osteomyelitis of tibia. Malunion (defined by Larsen et al.13 as varus or valgus >5°, internal or external rotation >15°, and ante or retro curvation >5°) occurred in 5/36 (14%) fractures. None of these 36 patients ended up in amputation.
Table 7.
Complications
DISCUSSION
Forty seven percent (17/36) had Ganga hospital score38 scores of above 11/16. These data indicate that the fractures included in this study were severe open fractures according to guidelines laid down by BOAST39 (British Orthopaedic Association and British Association of Plastic, Reconstructive and Aesthetic Surgeons Standard for Trauma). Even though the severity of the injury was very high, they were successfully managed by “fix and shift” technique which is a relatively easier technique as compared to previous methods.
In the current study, external fixation was used in preference to unreamed nailing because this group of patients had significant contamination or severe musculotendinous unit injury or bone loss or segmental comminution of bone who formed the “high risk” group according to Bhandari et al.6 Bhandari et al.6 had reported that unreamed nail did not significantly alter the risk of nonunion and deep infection when compared to external fixation for III B fractures. All the twenty patients who had an external fixation in the current study had contamination in the form of intramedullary deposition of dust and sand at the tibial fracture site. Unreamed nail would have increased the incidence of deep infection. Giannoudis et al.5 reported 2.7% implant (pin) breakage with external fixation for I to III B fractures. In the current study, among the external fixator group, although there were incidences of pin loosening (27%), there was no incidence of pin breakage.
Primary reamed nailing was performed when the limb had minimal contamination and did not have segmental bone loss or segmental comminution. This is supported by the fact that Court-Brown and Keating et al.,10,11,12 Bhandari et al.,6 Giannoudis et al.,5 and Larsen et al.13 had suggested reamed nailing for III B open tibial fractures. Giannoudis et al.5 reported 3% implant breakage with reamed nailing for I to III B fractures. In the current study, there was no incidence of implant breakage following reamed nailing. Larsen et al.13 had reported lower rates of secondary operations and malunion with reamed nailing as compared to unreamed nailing. In the current study, reamed nailing group had only three cases of reoperation. These reoperations were bone grafting. Keating et al.12 reported 23% exchange nailing in IIIB fractures which were nil in the current study. In the current study, there was no incidence of nail (implant) failure.
The primary bone union was achieved in 50% of the cases in this study, whereas it was 66% in the study by Gopal et al.23 The possible reason for this is the “severity” of the fracture which is indicated by the number of C3.3 fractures. The incidence of C3.3 fracture pattern was 25% in the current study as compared to only 3% in the study by Gopal et al. Gopal reported average time for fracture union as 25 and 30 weeks for internal and external fixation groups which in the current study has been reported as 29 and 46 weeks. Here again, the results of both studies are comparable even though the severity of fracture pattern is greater in the current study. Keating et al.12 reported 43 weeks as the mean time to union in the reamed nailing group which was 29 weeks in the current study. This reiterates the fact that reamed nailing for less contaminated open III B fractures under fix and shift technique results in speedy union. In the study by Giannoudis et al.,5 the rate of overall bone union was 94% in the external fixator group and 97% in the reamed nail group both of which was 100% in the current study. The rate of malunion among the reamed nailing group was reported as 7% by Keating and as 2.7% in the current study. These data show that the results of reamed nailing as the modality of fixation in less contaminated open IIIB tibial fractures under fix and shift technique are comparable or even better to the studies quoted above.
In many studies related to III B fractures, bone grafting at 8 weeks has been included in the treatment protocol itself.6 Obremsky,40,41 following a survey of 379 trauma surgeons stated that although variations existed, majority favored bone grafting between 4 and 8 weeks for segmental bone defects. In the current study, bone grafting was done at or after 8 weeks and after good healing of soft tissues. In the current study, the rate of bone grafting was 47% in total (39% in external fixator group and 8% in the nailed group). However, Gopal et al.23 reported 27% bone grafting (20% - external fixator group and 7% - internal fixation group) for III B and C fractures. Thirty nine percent of bone grafting under the external fixator group in the current study is due to the incidence of 25% of C3.3 fracture pattern which was only 3% under the study by Gopal et al. Giannoudis et al.5 reported 46% bone grafting under external fixator group which was only 39% in the current study under the same group. Keating et al.12 reported 26% and Giannoudis et al.5 reported 15% bone grafting following reamed nailing of III B fractures which was only 8% in the current study under reamed nail group. These data show that the rate of bone grafting under fix and shift technique is lesser when compared to the studies quoted above. Ten out of 15 patients underwent bone grafting through the anterolateral skin segment and five through posteromedial skin segment. Tibial fracture site can be reached through both of these skin segments comfortably [Figures 4 and 6]. Secondary procedures and reoperations, which are difficult through fasciocutaneous or muscle or free flaps,18 are much easier to perform under fix and shift technique. In addition to lesser incidence of bone grafting, the secondary procedure of bone grafting itself becomes much safer to perform keeping the condition of skin in mind. Ten out of 15 patients underwent bone grafting through the anterolateral skin segment and five through posteromedial skin segment. Tibial fracture site can be reached through both of these skin segments comfortably [Figures 4 and 6]. Secondary procedures and reoperations are difficult through fasciocutaneous, muscle or free flaps.18
Bone stimulating procedures (secondary fixations and bone grafting) have been termed as “reoperations” by Bhandari et al.6 Under fix and shift technique, the overall reoperation rate is 50% which is 42% under external fixator group and 8% under reamed nailing group. Overall reoperation rate is 34% under the study by Gopal which again shows that the higher reoperation rate in the current study is due to the increased number of C3.3 fractures. Under external fixator group, Giannoudis et al.5 reported 68.5% reoperation rate which is only 42% in the current study. Under reamed nailing group, Giannoudis et al.5 reported 31.6% reoperation rate which is only 8% in the current study.
Considering infection, deep infection rate was reported as 14% in the current study as compared to 9.5% by Gopal et al.23 Under the external fixator group, the current study reports 11% deep infection rate as compared to 16.2% reported by Giannoudis et al.5 Under the reamed nailing group, the current study reports 2.7% deep infection rate as compared to 6.4% reported by Giannoudis et al.5 Rajasekaran et al.38 had reported infection rate of 39.2% in group III (Glagow Coma Scale GHS – 11–16) and the infection rate for similar group in the current study was 22%. The rate of chronic pin track infection was reported as 32.2% by Giannoudis,5 37% by Gopal et al.,23 and 27% in the current study. These data show that the rate of deep infection is comparable or better when compared to similar studies.
Malunion rate (Larsen et al.13) was 11% under external fixator group and 2.7% under reamed nail group under fix and shift technique. Giannoudis et al.5 reported malunion rates of 20% under external fixator group and 6% under reamed nail group. Fix and shift technique has resulted in lower incidence of malunion as compared to previous studies.
Although fasciocutaneous,17 sural,20 propeller,16,21 and adipofascial22 flaps have been commonly employed for the closure of skin defects,15,16 Hallock25 reported 30% complications with fasciocutaneous flaps and Almedia20 reported 25% complications and 4.5% failure with sural artery flaps, whereas the current article reports only 19% complications and 2.7% failure with septocutaneous shift. Panse et al.35 stated that perforator and fasciocutaneous flaps can cover only limited skin defects and if the length of the perforator flap is more than one-third of the length of the leg then this flap had 6 times more chance to necrosis. The current study has shown that 14 open wounds >20 cm and ten wounds between 10 and 20 cm have been successfully managed by septocutaneous shift which would have been very difficult with fasciocutaneous and pedicled perforator flaps. The most common complication of venous congestion following propeller perforator flaps21 is not encountered with septocutaneous shift.
Pedicled muscle flaps such as gastrocnemius,23 hemisoleus,23 and peroneus brevis24 have been used frequently. These flaps provide some difficulty in approaching the bone for secondary procedures18,26 and can cover only limited defects. Hallock25 had reported 27% complication with pedicled muscle flaps. Although Chan et al.18 and Nanchahal19 favored muscle flaps to improve bone union, Nanchahal19 agreed that skin grafted muscle flaps are less resilient even to minor trauma. Septocutaneous shift can tolerate secondary procedures much better than muscle flaps41 (15/36 underwent bone grafting through shifted flap). Free muscle and free perforator flaps have been used cover large skin defects over leg.25 The surgical time, donor site morbidity, and failure rate are much less with septocutaneous shift than with free flaps for covering large defects. The complication rate with free flaps is 39% as reported by Hallock.25 According to Parrett et al.42 there has been a decreasing trend toward free flaps. Secondary refinement procedures like liposuction and debulking of free flaps for esthetic appearance are needed with free perforator flaps.43 Hui-Chou et al.43 reported 32 refinement procedures in seventy flaps. In comparison with the above-said observations, septocutaneous shift did not have any donor site morbidity and did not need any refinement procedure. Fix and flap technique5,23 reported by Gopal et al. suggested pedicled or free muscle flaps to cover soft tissue defects in III B tibial fractures. Gopal et al.23 had reported 3.5% muscle flap failure. The current study reports 2.7% of septocutaneous shift failure.
The distribution of septocutaneous perforators and their perforasomes has been defined well by Saint-Cyr et al.37 They had described three clusters of posterior tibial artery septocutaneous perforators at 4–9 cm, 13–18 cm, and 21–26 cm from intermalleolar line. Septocutaneous perforators from posterior tibial artery traverse between soleus and flexor digitorum longus. Anterior tibial artery perforators are largest at 21–26 cm from intermalleolar line and smallest at distal level. Septocutaneous perforators from anterior tibial artery traverse between peroneus longus and extensor digitorum longus. The peroneal septocutaneous perforators predominate at 13–18 cm from intermalleolar line. Septocutaneous perforators from peroneal artery traverse between peroneus brevis and flexor hallucis longus. To conclude perforators from anterior and posterior tibial arteries predominate at 4–9 cm level, those from peroneal and posterior tibial arteries at 13–18 cm level and those from anterior and posterior tibial arteries at 21–26 cm level. The incision on the posterior calf for the septocutaneous shift lies between posterior tibial and peroneal artery territories. Rubino et al.44 have stated that harvesting a flap based on a single perforator produces “hyper perfusion” of this perforator. The septocutaneous shift is an indirect way of harvesting a flap which is based on two or three perforators and their perforasomes, the number of the perforators being directly proportional to the length of the posterior incision. Hence, the fasciocutaneous skin segment obtained by performing septocutaneous shift has augmented blood supply due to hyperperfusion of the involved perforators.
In the current study, septocutaneous shift was raised immediately following skeletal fixation (within 13 h in 27 cases and within 24 h in 9 cases). This is supported by the fact suggested by D’Alleyrand et al.45 that timing of flap cover was a significant predictor of flap-related complications in III B fractures. Their inference was that the delay beyond 1 week was associated with a daily increase in the infection rate of 16%. Immediate or very early flap cover was also suggested by Giannoudis et al.,5 Gopal et al.,23 and Soni et al.46
CONCLUSION
Gustilo Anderson III B open tibial fractures with “fix and shift” technique has resulted in better outcome in terms of skeletal factors (primary fracture union, overall union, and time for union and malunion) and soft tissue factors (wound healing, flap failure, access to secondary procedures, and esthetic appearance) when compared to standard methods adopted earlier. Hence, “fix and shift” could be recommended as one of the treatment modalities for open III B tibial fractures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: Retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453–8. [PubMed] [Google Scholar]
- 2.Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: A new classification of type III open fractures. J Trauma. 1984;24:742–6. doi: 10.1097/00005373-198408000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Horn BD, Rettig ME. Interobserver reliability in the Gustilo and Anderson classification of open fractures. J Orthop Trauma. 1993;7:357–60. doi: 10.1097/00005131-199308000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Brumback RJ, Jones AL. Interobserver agreement in the classification of open fractures of the tibia. The results of a survey of two hundred and forty-five orthopaedic surgeons. J Bone Joint Surg Am. 1994;76:1162–6. doi: 10.2106/00004623-199408000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Giannoudis PV, Papakostidis C, Roberts C. A review of the management of open fractures of the tibia and femur. J Bone Joint Surg Br. 2006;88:281–9. doi: 10.1302/0301-620X.88B3.16465. [DOI] [PubMed] [Google Scholar]
- 6.Bhandari M, Guyatt GH, Swiontkowski MF, Schemitsch EH. Treatment of open fractures of the shaft of the tibia. A systematic overview and meta-analysis. J Bone Joint Surg Br. 2000;82-B:62–8. doi: 10.1302/0301-620x.83b1.10986. [DOI] [PubMed] [Google Scholar]
- 7.Rao P, Schaverien MV, Stewart KJ. Soft tissue management of children's open tibial fractures – A review of seventy children over twenty years. Ann R Coll Surg Engl. 2010;92:320–5. doi: 10.1308/003588410X12664192075017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Henley MB, Chapman JR, Agel J, Harvey EJ, Whorton AM, Swiontkowski MF. Treatment of type II, IIIA, and IIIB open fractures of the tibial shaft: A prospective comparison of unreamed interlocking intramedullary nails and half-pin external fixators. J Orthop Trauma. 1998;12:1–7. doi: 10.1097/00005131-199801000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Tornetta P, 3rd, Bergman M, Watnik N, Berkowitz G, Steuer J. Treatment of grade-IIIb open tibial fractures. A prospective randomised comparison of external fixation and non-reamed locked nailing. J Bone Joint Surg Br. 1994;76:13–9. [PubMed] [Google Scholar]
- 10.Court-Brown CM. Reamed intramedullary tibial nailing: An overview and analysis of 1106 cases. J Orthop Trauma. 2004;18:96–101. doi: 10.1097/00005131-200402000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Court-Brown CM, McQueen MM, Quaba AA, Christie J. Locked intramedullary nailing of open tibial fractures. J Bone Joint Surg Br. 1991;73:959–64. doi: 10.1302/0301-620X.73B6.1955445. [DOI] [PubMed] [Google Scholar]
- 12.Keating JF, Blachut PA, O’Brien PJ, Court-Brown CM. Reamed nailing of Gustilo grade-IIIB tibial fractures. J Bone Joint Surg Br. 2000;82:1113–6. doi: 10.1302/0301-620x.82b8.10566. [DOI] [PubMed] [Google Scholar]
- 13.Larsen LB, Madsen JE, Høiness PR, Øvre S. Should insertion of intramedullary nails for tibial fractures be with or without reaming? A prospective, randomized study with 3.8 years’ followup. J Orthop Trauma. 2004;18:144–9. doi: 10.1097/00005131-200403000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Rajasekaran S, Dheenadhayalan J, Babu JN, Sundararajan SR, Venkatramani H, Sabapathy SR. Immediate primary skin closure in type-III A and B open fractures: Results after a minimum of five years. J Bone Joint Surg Br. 2009;91:217–24. doi: 10.1302/0301-620X.91B2.21228. [DOI] [PubMed] [Google Scholar]
- 15.Kamath JB, Shetty MS, Joshua TV, Kumar A, Harshvardhan, Naik DM. Soft tissue coverage in open fractures of tibia. Indian J Orthop. 2012;46:462–9. doi: 10.4103/0019-5413.97265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hallock GG. Evidence-based medicine: Lower extremity acute trauma. Plast Reconstr Surg. 2013;132:1733–41. doi: 10.1097/PRS.0b013e3182a80925. [DOI] [PubMed] [Google Scholar]
- 17.Varey AH, Khan U. Soft-tissue reconstruction of open fractures of the lower limb: Muscle versus fasciocutaneous flaps. Plast Reconstr Surg. 2013;131:448e. doi: 10.1097/PRS.0b013e31827c723b. [DOI] [PubMed] [Google Scholar]
- 18.Chan JK, Harry L, Williams G, Nanchahal J. Soft-tissue reconstruction of open fractures of the lower limb: Muscle versus fasciocutaneous flaps. Plast Reconstr Surg. 2012;130:284e–95e. doi: 10.1097/PRS.0b013e3182589e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nanchahal J. Reply: Soft-tissue reconstruction of open fractures of the lower limb: Muscle versus fasciocutaneous flaps. Plast Reconstr Surg. 2013;131:448e–9e. doi: 10.1097/PRS.0b013e31827c728f. [DOI] [PubMed] [Google Scholar]
- 20.Almeida MF, da Costa PR, Okawa RY. Reverse-flow island sural flap. Plast Reconstr Surg. 2002;109:583–91. doi: 10.1097/00006534-200202000-00027. [DOI] [PubMed] [Google Scholar]
- 21.Georgescu AV. Propeller perforator flaps in distal lower leg: Evolution and clinical applications. Arch Plast Surg. 2012;39:94–105. doi: 10.5999/aps.2012.39.2.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Verhelle N, Vranckx J, Van den Hof B, Heymans O. Bone exposure in the leg: Is a free muscle flap mandatory? Plast Reconstr Surg. 2005;116:170–7. doi: 10.1097/01.prs.0000169698.89331.0b. [DOI] [PubMed] [Google Scholar]
- 23.Gopal S, Majumder S, Batchelor AG, Knight SL, De Boer P, Smith RM. Fix and flap: The radical orthopaedic and plastic treatment of severe open fractures of the tibia. J Bone Joint Surg Br. 2000;82:959–66. doi: 10.1302/0301-620x.82b7.10482. [DOI] [PubMed] [Google Scholar]
- 24.Bajantri B, Bharathi R, Ramkumar S, Latheef L, Dhane S, Sabapathy SR. Experience with peroneus brevis muscle flaps for reconstruction of distal leg and ankle defects. Indian J Plast Surg. 2013;46:48–54. doi: 10.4103/0970-0358.113706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hallock GG. Utility of both muscle and fascia flaps in severe lower extremity trauma. J Trauma. 2000;48:913–7. doi: 10.1097/00005373-200005000-00016. [DOI] [PubMed] [Google Scholar]
- 26.Yazar S, Lin CH, Lin YT, Ulusal AE, Wei FC. Outcome comparison between free muscle and free fasciocutaneous flaps for reconstruction of distal third and ankle traumatic open tibial fractures. Plast Reconstr Surg. 2006;117:2468–75. doi: 10.1097/01.prs.0000224304.56885.c2. [DOI] [PubMed] [Google Scholar]
- 27.Hallock GG. Bipedicled fasciocutaneous flaps in the lower extremity. Ann Plast Surg. 1992;29:397–401. doi: 10.1097/00000637-199211000-00003. [DOI] [PubMed] [Google Scholar]
- 28.DiStasio AJ, 2nd, Dugdale TW, Deafenbaugh MK. Multiple relaxing skin incisions in orthopaedic lower extremity trauma. J Orthop Trauma. 1993;7:270–4. doi: 10.1097/00005131-199306000-00012. [DOI] [PubMed] [Google Scholar]
- 29.Sharma H, Nunn T. Conversion of open tibial IIIb to IIIa fractures using intentional temporary deformation and the Taylor spatial frame. Strategies Trauma Limb Reconstr. 2013;8:133–40. doi: 10.1007/s11751-013-0160-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lahoti O, Findlay I, Shetty S, Abhishetty N. Intentional deformation and closure of soft tissue defect in open tibial fractures with a taylor spatial frame – A simple technique. J Orthop Trauma. 2013;27:451–6. doi: 10.1097/BOT.0b013e318284727a. [DOI] [PubMed] [Google Scholar]
- 31.Blum ML, Esser M, Richardson M, Paul E, Rosenfeldt FL. Negative pressure wound therapy reduces deep infection rate in open tibial fractures. J Orthop Trauma. 2012;26:499–505. doi: 10.1097/BOT.0b013e31824133e3. [DOI] [PubMed] [Google Scholar]
- 32.Formby P, Flint J, Gordon WT, Fleming M, Andersen RC. Use of a continuous external tissue expander in the conversion of a type IIIB fracture to a type IIIA fracture. Orthopedics. 2013;36:e249–51. doi: 10.3928/01477447-20130122-31. [DOI] [PubMed] [Google Scholar]
- 33.Zhen P, Hu YY, Luo ZJ, Liu XY, Lu H, Li XS. One-stage treatment and reconstruction of Gustilo type III open tibial shaft fractures with a vascularized fibular osteoseptocutaneous flap graft. J Orthop Trauma. 2010;24:745–51. doi: 10.1097/BOT.0b013e3181d88a07. [DOI] [PubMed] [Google Scholar]
- 34.Petrisor B, Anderson S, Court-Brown CM. Infection after reamed intramedullary nailing of the tibia: A case series review. J Orthop Trauma. 2005;19:437–41. doi: 10.1097/01.bot.0000161542.93624.8d. [DOI] [PubMed] [Google Scholar]
- 35.Panse NS, Bhatt YC, Tandale MS. What is safe limit of the perforator flap in lower extremity reconstruction? Do we have answers yet. Plast Surg Int 2011. 2011:349357. doi: 10.1155/2011/349357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schaverien M, Saint-Cyr M. Perforators of the lower leg: Analysis of perforator locations and clinical application for pedicled perforator flaps. Plast Reconstr Surg. 2008;122:161–70. doi: 10.1097/PRS.0b013e3181774386. [DOI] [PubMed] [Google Scholar]
- 37.Saint-Cyr M, Wong C, Schaverien M, Mojallal A, Rohrich RJ. The perforasome theory: Vascular anatomy and clinical implications. Plast Reconstr Surg. 2009;124:1529–44. doi: 10.1097/PRS.0b013e3181b98a6c. [DOI] [PubMed] [Google Scholar]
- 38.Rajasekaran S, Naresh Babu J, Dheenadhayalan J, Shetty AP, Sundararajan SR, Kumar M, et al. A score for predicting salvage and outcome in Gustilo type-IIIA and type-IIIB open tibial fractures. J Bone Joint Surg Br. 2006;88:1351–60. doi: 10.1302/0301-620X.88B10.17631. [DOI] [PubMed] [Google Scholar]
- 39.BOAST (British Orthopaedic Association and British Association of Plastic, Reconstructive and Aesthetic Surgeons Standard for Trauma) 4: The management of severe open lower limb fratures. British Orthopaedic Association and British Association of Plastic, Reconstructive and Aesthetic Surgeons Standard for Trauma – 2009 [Google Scholar]
- 40.Obremskey W, Molina C, Collinge C, Nana A, Tornetta P, 3rd, Sagi C, et al. Current practice in the management of open fractures among orthopaedic trauma surgeons. Part A: Initial management. A survey of orthopaedic trauma surgeons. J Orthop Trauma. 2014;28:e198–202. doi: 10.1097/BOT.0000000000000033. [DOI] [PubMed] [Google Scholar]
- 41.Obremskey W, Molina C, Collinge C, Tornetta P, 3rd, Sagi C, Schmidt A, et al. Current practice in the management of open fractures among orthopaedic trauma surgeons. Part B: Management of segmental long bone defects. A survey of orthopaedic trauma association members. J Orthop Trauma. 2014;28:e203–7. doi: 10.1097/BOT.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 42.Parrett BM, Matros E, Pribaz JJ, Orgill DP. Lower extremity trauma: Trends in the management of soft-tissue reconstruction of open tibia-fibula fractures. Plast Reconstr Surg. 2006;117:1315–22. doi: 10.1097/01.prs.0000204959.18136.36. [DOI] [PubMed] [Google Scholar]
- 43.Hui-Chou HG, Sulek J, Bluebond-Langner R, Rodriguez ED. Secondary refinements of free perforator flaps for lower extremity reconstruction. Plast Reconstr Surg. 2011;127:248–57. doi: 10.1097/PRS.0b013e3181f95b67. [DOI] [PubMed] [Google Scholar]
- 44.Rubino C, Coscia V, Cavazzuti AM, Canu V. Haemodynamic enhancement in perforator flaps: The inversion phenomenon and its clinical significance. A study of the relation of blood velocity and flow between pedicle and perforator vessels in perforator flaps. J Plast Reconstr Aesthet Surg. 2006;59:636–43. doi: 10.1016/j.bjps.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 45.D’Alleyrand JC, Manson TT, Dancy L, Castillo RC, Bertumen JB, Meskey T, et al. Is time to flap coverage of open tibial fractures an independent predictor of flap-related complications? J Orthop Trauma. 2014;28:288–93. doi: 10.1097/BOT.0000000000000001. [DOI] [PubMed] [Google Scholar]
- 46.Soni A, Tzafetta K, Knight S, Giannoudis PV. Gustilo IIIC fractures in the lower limb: Our 15-year experience. J Bone Joint Surg Br. 2012;94:698–703. doi: 10.1302/0301-620X.94B5.27948. [DOI] [PubMed] [Google Scholar]








