Abstract
Background and Objectives:
Pseudomonas aeruginosa (PA) is one of the most important causes of nosocomial infections and has an intrinsic resistance to many antibiotics. Among all the resistance-nodulation-division (RND) pumps of P. aeruginosa, MexAB-OprM is the first efflux pump found to target multiple classes of antibiotics. This study was aimed to evaluate the expression level of genes expressing MexAB-OprM in clinical isolates of P. aeruginosa.
Materials and Methods:
In this study, 45 P. aeruginosa strains were isolated from patients admitted to Children’s Medical Center Hospital, an Iranian referral hospital. Disk diffusion and Minimum Inhibitory Concentration (MIC) methods were used for determination of the patterns of resistance to antibiotics. Real-time PCR was used to investigate the expression level of genes of MexAB-OprM efflux pump.
Results:
Among 45 resistant PA isolates, the frequency of genes overexpression was as follows: MexA (n=25, 55.5%), MexB (n=24, 53.3%) and OprM (n=16, 35.5%). In addition, in 28 strains (62%) overexpression was observed in one of the studied three genes of MexAB-OprM efflux pump.
Conclusion:
In our study 28 isolates (62%) had increased expression level of efflux pumps genes, MexAB-OprM. Although the efflux pumps play important roles in increasing the resistance towards different antibiotics but the role of other agents and mechanisms in evolution of resistance should not be ignored. Since the concomitant overproduction of other Mex efflux systems might have additive effects on antibiotic resistance, the co-expressing of a multicomponent efflux pump is recommended. On the other hand, the concomitant overproduction of two Mex pumps might have additive effects on resistance to antibiotic. Therefore co-expressing of Mex efflux systems is recommended.
Keywords: Pseudomonas aeruginosa, Efflux pump, Real-time PCR
INTRODUCTION
Emergence of bacterial resistance to many different antibiotics is considered as a great concern in human health. Pseudomonas aeruginosa (PA) has been recognized as one of the significant pathogens of nosocomial infections (1). Key mechanism of antibiotic resistance in P. aeruginosa is the expulsion of antibiotics through multidrug resistance (MDR) efflux systems belonging to the resistance-nodulation-division (RND) family (2). MexAB-OprM, MexCD-OprJ, MexEF-OprN, MexXY, MexJK and MexVW contribute the most significantly to antibiotic resistance (3) and play an important role in intrinsic and acquired multidrug resistance (2). Resistance of P. aeruginosa to multiple antibiotics is largely attributable to expression of the MexAB-OprM efflux pump (4). Among all the RND pumps of PA, Mex-AB-OprM was the first efflux pump found to target multiple classes of antibiotics including β-lactam (carboxypenicillins, aztreonam, extended-spectrum cephalosporins, penems, the carbapenems such as meropenem and panipenem except imipenem and biapenem); fluoroquinolones, tetracyclines, chloramphenicol, macrolides, novobiocin, trimethoprim and sulfonamides (5, 6).
The MexAB-OprM efflux pump belongs to the superfamily of ribonucleoproteins and consists of an inner membrane (MexB), a periplasmic membrane fusion protein (MexA) and a channel-forming outer membrane protein, OprM (7).
In this study, we investigated the role of Mex-AB-OprM efflux pump. Transcription level of efflux pump genes MexA, MexB, OprM, MexR and AmpC were analyzed using Real-time PCR.
MATERIALS AND METHODS
Bacterial strains.
P. aeruginosa strains were isolated from patients of Children’s Hospital Medical Center during 6 months (March and August 2012). All bacterial isolates were identified at microbiology lab using standard biochemical identification methods (8). A total of 45 samples were collected from various clinical specimens such as urine (n=21), exudates (n=11), eye (n=2), ear (n=2), CSF (n=2), blood (n=2), trachea (n=2) and lung secretions (n=3). P.aeruginosa PAO1 strain which has entirely sequenced genome was used as the reference wild type strain throughout the study.
Antimicrobial susceptibility tests.
Antimicrobial susceptibility tests were performed using disk diffusion and minimum inhibitory concentration (MIC) methods. Antibiotics used in this study were chosen randomly from different antibiotic classes that were used mostly in this hospital. Antibiotics used in the disk diffusion method were cephalothin (30 μg), cefepime (30 μg), ceftazidime (30 μg), ciprofloxacin (5 μg) (flouroquionolones), meropenem (10 μg), imipenem (10 μg) (carbapenems), piperacillin/tazobactam (10/100 μg) (β-lactams), gentamicin (10 μg) and amikacin (30 μg) (aminoglycosides). All antibiotic disk were purchased from Mast Company (UK).
Determination of MICs for each antibacterial agent was performed by micro broth dilution method. Antibiotics used in this study were cefuroxime, ceftazidim, cefazolin, ceftriaxone (cephems), meropenem (carbapenems), amikacin, tobramycin (aminoglycosides), aztreonam (monobactam), ampicillin, piperacillin (penicillins), colistin (lipopeptides), gatifloxacin, nalidixic acid (flouroquionolones), piperacillin-tazobactam, tazobactam (β-lactams) (Mast, UK).
Isolation of total RNA and cDNA synthesis for RT-PCR.
Total RNA was extracted using RNA extraction kit (Fermentas, Lithuania), and converted into cDNA using the cDNA synthesis kit (Fermentas, Lithuania) according to the manufacturer’s instruction and the quality and purity of the RNA obtained was evaluated using spectrophotometer.
PCR reaction.
The final optimized PCR reaction consisted of 1 μl of each primer (10pmol) (Table 1), 0.5 μl dNTP (10mM), 0.5 μl MgCl (100mM), 0.2 μl (1 unit) Taq DNA polymerase (Metabion, Germany), 2.5 μl PCR buffer (10X), and 0.5 μl of DNA template (100μg/ml) in total volume of 25 μl with double distilled water. The cycling program was adjusted as follows: initial denaturation at 94 °C for 5 min followed by 30 cycles of 94 °C for 45 sec, 50–72 °C (45 sec), 72 °C (1 min) and a final extension at 72 °C for 10 min (9).
Table 1.
Primers used in PCR and real-time PCR
| Genes | Primers (5′-3′) | PCR product size (bp) | Reference |
|---|---|---|---|
| MexA | F: 5′acctacgaggccgactaccaga-3′ R: 5′- gttggtcaccagggcgccttc-3′ |
179 | 24 |
| MexB | F: 5′- gtgttcggctcgcagtactc-3′ R: 5′- aaccgtcgggattgaccttg-3′ |
244 | 30 |
| OprM | F: 5′- ccatgagccgccaactgtc-3′ R: 5′- cctggaacgccgtctggat-3′ |
205 | 31 |
| AmpC | F: 5′- ggtgcagaaggaccaggcacagat-3′ R: 5′- cgatgctcgggttggaatagaggc-3′ |
97 | 26 |
Real-time PCR reaction.
Real-time quantification of cDNA was carried out on an ABI step one detection system (Applied Biosystems, UK) using the SYBR green PCR master mix. Real-time PCR was used to investigate the expression level of each gene in MexAB-OprM efflux pump to expression each of these genes of separately measured by relative quantitation Real-time PCR. The optimized reaction consisted of master mix (10X), 1 μl of each primer (10 pmol), and 0.5 μl of template DNA (100 μg/ml) in a total volume of 20 μl.
Relative expression values (R) were determined using the ΔΔCt method. P. aeruginosa strain PAO1 was used as a standard strain for normalization of relative mRNA levels.
AmpC gene was considered as a housekeeping gene and all gene expressions were compared with AmpC gene expression. The assay was performed three times for each sample and the mean of three obtained quantities was considered as quantity. Expressions of all genes were calculated using the 2 −ΔΔCt method (fold). Cycle of threshold (C t ) was considered as the average threshold cycle number from three independent experiments.
The real-time PCR apparatus was programmed as follows: initial denaturation at 95 °C (15 min) followed by 40 cycles of 95 °C (15 sec), 61 °C (15 sec), 71 °C (20 sec) and melt curve at 61 °C (1 min) and 95 °C for 15 sec. To obtain reproducibility of the reaction, the quantification of standards was run in triplicate. AmpC gene was considered as a housekeeping gene and the results were compared with gene expression in a susceptible PA reference strain. Primer dimers and other artifacts were evaluated by melting curve analysis. To confirm that specific amplification had occurred, melting curves of each amplicon were assessed. Relative expression values (R) were determined using the ΔΔCt method. P. aeruginosa strain PAO1 was used as a standard strain for normalization of relative mRNA levels.
Real-time PCR efficiencies were acquired by amplification of a standardized dilution series of the template cDNA and were determined for each gene as the slope of a linear regression model. PCR efficiency was determined by measuring the CT Ct to a specific threshold for a serial dilution of cDNA. The corresponding real-time PCR efficiencies were then calculated according to the equation: E = (10−1/slope−1) × 100 (10–12).
RESULTS
Demographic data.
Totally, 45 strains of P. aeruginosa were isolated from patients aged 2 months to 12 years who were referred to Children’s Medical Center Hospital, Tehran, Iran. The majority of isolates were collected from patients hospitalized in PICU (n=18, 39%), NICU (n=5, 11%) followed by emergency ward (n=3, 7%), nephrology (n=3, 7%), surgery (n=5, 11%), neurology (n=3, 7%), urology (n=5, 11%) and infectious ward (n=3, 7%). Most of the strains were isolated from male children aged 10–15 months.
Antibacterial susceptibility testing.
The most antibiotic resistance based on CLSI reference guidelines for disk diffusion method was detected for cephalothin (n=41, 92%) whereas MICs should the following frequencies for antibiotic resistance: cefuroxime (n=41, 91%), ceftazidime (n=42, 93%), amikacin (n=38, 84.5%), cefazolin (n=40, 89%), aztreonam (n=42, 93%), piperacillin (n=39, 86.5%), tazobactam (n=41, 91%) and piperacillin-tazobactam (n=42, 93%). Antibiotics such as colistin (15%), ceftriaxone (33%) and tobramycin (22%) showed the highest susceptibility rates against the isolates (Table 2).
Table 2.
Pattern of determined antibiotic resistance among P. aeruginosa strains using disk diffusion and MIC methods
| Antibiotics | Disk diffusion results | ||
|---|---|---|---|
|
| |||
| Resistant (%) | Intermediate (%) | Sensitive (%) | |
| Cephalothin | 41 (92) | 1 (1) | 3 (7) |
| Cefepime | 27 (60) | 3 (7) | 15 (33) |
| Ciprofloxacin | 14 (32) | 8 (17) | 23 (51) |
| Meropenem | 15 (34) | 6 (12.6) | 24 (53.3) |
| Ceftazidim | 24 (55) | 5 (10) | 16 (35) |
| Piperacillin/tazobactam | 10 (26) | 8 (14) | 27 (60) |
| Imipenem | 12 (28) | 2 (3) | 31 (69) |
| Gentamicin | 35 (78) | 5 (11) | 5 (11) |
| Antibiotics | MIC results | ||
|---|---|---|---|
|
| |||
| Resistant (%) | Intermediate (%) | Sensitive (%) | |
| Cefuroxime | 41 (91) | 4 (9) | 0 |
| Cetriaxone | 15 (33) | 10 (11.2) | 25 (55.5) |
| Ceftazidim | 25 (56) | 3 (7) | 17 (38) |
| Piperacillin | 39 (86.5) | 5 (11) | 1 (2.5) |
| Meropenem | 16 (35) | 10 (23) | 19 (42) |
| Colistin | 7 (15) | 10 (23) | 28 (62) |
| Amikacin | 38 (84.5) | 5 (11) | 2 (4.5) |
| Gatifloxacin | 40 (89) | 4 (9) | 1 (2) |
| Cefazolin | 40 (89) | 5 (11) | 0 |
| Nalidixic acid | 41 (91) | 4 (9) | 0 |
| Aztreonam | 42 (93) | 3 (7) | 0 |
| Piperacillin/tazobactam | 12 (27) | 5 (11) | 28 (62) |
| Ampicillin | 35 (78) | 4 (9) | 6 (13) |
| Tazobactam | 41 (91) | 1 (2) | 3 (7) |
| Tobramycin | 10 (22) | 10 (22) | 25 (56) |
PCR and Real-time PCR.
The best annealing temperature was obtained at 61 °C. The results of real-time PCR for the genes of MexAB-OprM efflux pump have been shown in Table 3. According to the results of antibiotic resistance via disk diffusion method, overexpression of MexAB-OprM genes was associated to the resistance towards cephalosporin while via MIC method overexpression of MexAB-OprM was seen in those showing resistance towards special antibiotics especially fluoroquinolones, cephalosporin and beta lactams.
Table 3.
The expression of MexAB-OprM efflux pump genes in P. aeruginosa strains isolated from children
| Patients | Gender | Age (Months) | Expression level (folds) | |||
|---|---|---|---|---|---|---|
|
| ||||||
| AmpC (Ct) | MexA | MexB | OprM | |||
| A1 | F | 20 | 27.9 | 9.2 | 8.7 | 6.4 |
| F1 | M | 12 | 25.7 | 4.8 | 5 | 3.3 |
| A2 | M | 11 | 27.6 | 9.6 | 10.8 | 5.4 |
| E1 | M | 5 | 28.3 | 12 | 14 | 9.3 |
| C1 | F | 9 | 27.9 | 9.1 | 10.5 | 6.3 |
| A3 | F | 10.5 | 27.6 | 8.2 | 7.3 | 5.3 |
| G1 | M | 15 | 26.1 | 3.7 | 3.5 | 3 |
| D1 | M | 10 | 28.0 | 8.6 | 5.3 | 5.8 |
| H1 | M | 8 | 25.3 | 3.9 | 1.3 | 2.4 |
| A4 | M | 65 | 26.1 | 4.2 | 5.1 | 3.2 |
| E2 | F | 6 | 25.1 | 5.5 | 6.8 | 5.2 |
| D2 | F | 10 | 24.9 | 2.7 | 3 | 2.2 |
| A5 | M | 14 | 26 | 3.8 | 4.1 | 1.8 |
| C2 | F | 10 | 24.5 | 2.2 | 2.7 | 1.7 |
| A6 | M | 12 | 25.4 | 3.3 | 3.1 | 1.6 |
| A7 | M | 16 | 27.9 | 7.5 | 8.6 | 3.1 |
| E3 | F | 4 | 25.2 | 2.7 | 2.6 | 1.9 |
| A8 | M | 50 | 22.1 | 1.8 | 1.9 | 1.5 |
| A9 | F | 11 | 27.1 | 5.1 | 4.4 | 2.1 |
| H2 | M | 15 | 27.16 | 2.7 | 5.1 | 1.1 |
| A10 | M | 15 | 28 | 11.3 | 5 | 1 |
| B1 | F | 53 | 27.1 | 2.8 | 5.7 | 1 |
| D3 | M | 14 | 27.1 | 4.4 | 4.3 | 3 |
| A11 | F | 74 | 28.1 | 11.1 | 7.1 | 2.3 |
| G2 | M | 10 | 25.3 | 2.7 | 3.9 | 1.2 |
| A12 | F | 7 | 24.2 | 1.9 | 2.7 | 1.4 |
| H3 | M | 12 | 2 | 2.1 | 2.2 | 1.7 |
| B2 | M | 11 | 22.5 | 2 | 2.1 | 1.6 |
| A13 | F | 20 | 28.1 | 1 | 1.5 | 0.6 |
| B3 | M | 12 | 26.0 | 1.8 | 1.2 | 1 |
| H4 | F | 8 | 25.1 | 1.5 | 1.4 | 0.8 |
| D4 | M | 5 | 2 | 1.2 | 1 | 0.5 |
| A14 | M | 24 | 24.9 | 1.6 | 1.3 | 0.7 |
| A15 | F | 6 | 27.5 | 1 | 1.2 | 0.8 |
| H5 | M | 7 | 26.9 | 0.8 | 0.6 | 0.5 |
| F2 | F | 14 | 27.1 | 0.5 | 1 | 0.9 |
| E4 | M | 10 | 28.6 | 0.2 | 0.5 | 0.1 |
| D5 | F | 6 | 26.5 | 1.2 | 0.8 | 1 |
| A16 | M | 5 | 24.1 | 1.4 | 1.1 | 0.8 |
| E5 | M | 11 | 27.5 | 1 | 0.9 | 0.2 |
| G3 | F | 10 | 28.3 | 0.5 | 1 | 0.8 |
| B3 | M | 18 | 26.8 | 0.7 | 1.2 | 1.5 |
| A17 | F | 12 | 25.9 | 1.3 | 0.8 | 1 |
| F3 | M | 15 | 27.9 | 0.9 | 0.5 | 0.6 |
| A18 | M | 30 | 28.7 | 0.4 | 0.2 | 0.2 |
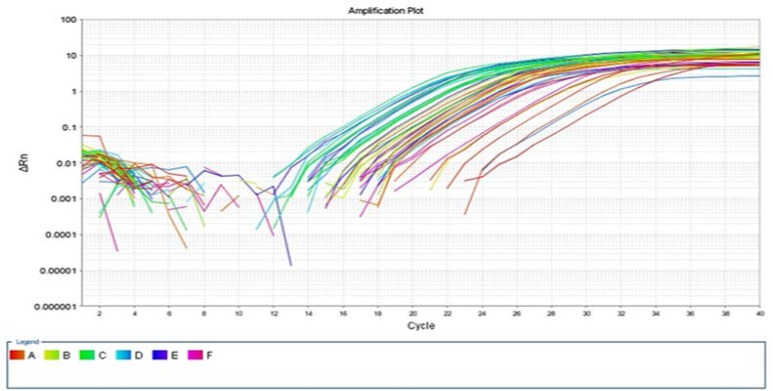
The reproducibility of the expression levels of each gene was measured three times. Different expression of MexAB-OprM genes was observed (Fig. 1). P. aeruginosa clinical isolates demonstrated increased level of MexA (≥ 2 folds), MexB (from 2.2 to 12.0 folds), OprM (≥ 2 folds) and AmpC (≥ 10 folds) at transcriptional mRNA level, respectively.
Fig. 1.
Confirmation of specific amplifications during real-time
PCR on MexAB-OprM genes of efflux pump
Among 45 resistant isolates, overexpression of MexA gene was observed in 25 isolates (55.5%), MexB in 24 isolates (53.3%) and OprM in 16 isolates (35.5%). In 28 isolates (62%), overexpression was observed in one of the three genes of MexAB-OprM efflux pump.
The ratio values obtained for each of the four genes in samples showed that the expression levels of MexA gene (n=25, 89%) was between 1.8 and 11.7 (mean= 6.7), MexB (n=24, 85%) between 1.3 and 14 (mean= 7.6) and OprM gene (n=16, 57%) between 1 and 9 (mean= 5).
Primer dimers and other artifacts were evaluated by melting curve analysis. To confirm that specific amplification (Fig. 1) had occurred, the melting curves of each amplicon were assessed.
DISCUSSION
P. aeruginosa is one of the most important causes of nosocomial infections due to the presence of various resistant elements (11). During last decades, the emergency of multidrug resistant P. aeruginosa has been observed worldwide. In this study, 28–35% of studied P. aeruginosa isolates were resistant to carbapenems which was in accordance with previous studies (13, 14). High frequency of cephalosporin resistance was also observed among P. aeruginosa isolates similar to the other reports (14, 15). Among all isolates, resistance to piperacillin/tazobactam was low (26–27%) which was in agreement with our previous report (13) and was higher than Ghazi et al. report (16). In this study colistin showed 15% resistance which can be suggested as an effective antibiotic for treatment of PA infections. This finding is similar to the results of study performed by Alekshun et al. in US (17).
At present, the efflux pump has been recognized as one of the significant complexes involved in resistance to most of the classes of antibiotics (11, 18, 19). It has been reported that the prevalence of efflux pump overexpression in clinical P. aeruginosa strains of ranged from 14–75% (20, 21). There are rare reports on prevalence of efflux pump overexpression in our country (22, 23) and there is no investigation on PA strains isolated from children. In the present study the increased expression level of MexAB-OprM genes of efflux pump simultaneously was 25% which was relatively more than Dumas et al. findings in Switzerland (11) and Mesaros et al. in Belgium (24).
In this study, 28 of 45 patients (62%) showed an increased expression level of efflux pumps Mex-AB-OprM genes that was similar to the studies reported more than 50% overexpression level of these genes (24–27). In Arabestani et al. study all the isolates (n=31; 100%) showed overexpression of efflux pump MexAB-OprM genes (23). According to Aghazadeh et al. report, overexpression of mexA was 74% among the isolates (28).
Since the concomitant overproduction of two Mex pumps might have additive effects on being resistant to antibiotics (29) evaluating the co-expression of multi-component efflux pumps other than MexAB-OprM is recommended.
CONCLUSION
Development of novel antibiotics that can bypass the effects of efflux pumps is still a challenging task. Further studies on involved mechanisms and structure-function association of bacterial efflux systems as well as the interactions between the pumps and other resistance mechanisms are highly recommended.
ACKNOWLEDGEMENT
This study was Sahar Yaslianifard’s postgraduate thesis. This study was supported by a grant (grant number: 92-01-88-21861) from Tehran University of Medical Sciences to Dr. Setraeh Mamishi.
REFERENCES
- 1. Akama H, Matsuura T, Kashiwagi S, Yoneyama H, Narita S, Tsukihara T, et al. Crystal structure of the membrane fusion protein, MexA, of the multidrug transporter in Pseudomonas aeruginosa. J Biol Chem 2004; 279: 25939– 25942. [DOI] [PubMed] [Google Scholar]
- 2. Schaible B, Taylor CT, Schaffer K. Hypoxia increases antibiotic resistance in Pseudomonas aeruginosa through altering the composition of multidrug efflux pumps. Antimicrob Agents Chemother 2012; 56: 2114– 2118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Poonsuk K, Tribuddharat C, Chuanchuen R. Simultaneous overexpression of multidrug efflux pumps in Pseudomonas aeruginosa non-cystic fibrosis clinical isolates. Can J Microbiol 2014; 60: 437– 443. [DOI] [PubMed] [Google Scholar]
- 4. Yoneyama H, Maseda H, Kamiguchi H, Nakae T. Function of the membrane fusion protein, MexA, of the MexA, B-OprM efflux pump in Pseudomonas aeruginosa without an anchoring membrane. J Biol Chem 2000; 275: 4628– 4634. [DOI] [PubMed] [Google Scholar]
- 5. Masuda N, Sakagawa E, Ohya S, Gotoh N, Tsujimoto H, Nishino T. Substrate specificities of MexAB-OprM, MexCD-OprJ, and MexXY-oprM efflux pumps in Pseudomonas aeruginosa. Antimicrob Agents Chemother 2000; 44: 3322– 3327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Choudhury D, Ghose A, Dhar Chanda D, Das Talukdar A, Dutta Choudhury M, Paul D, et al. Premature termination of MexR leads to overexpression of Mex-AB-OprM efflux pump in Pseudomonas aeruginosa in a tertiary referral hospital in India. PLoS One 2016; 11: e0149156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wu CM, Cao JL, Zheng MH, Ou Y, Zhang L, Zhu XQ, et al. Effect and mechanism of andrographolide on the recovery of Pseudomonas aeruginosa susceptibility to several antibiotics. J Int Med Res 2008; 36: 178– 186. [DOI] [PubMed] [Google Scholar]
- 8. Garcia LS, Isenberg H. (2010). Clinical Microbiology Procedures Handbook. 3rd ed ASM Press; Washington DC. [Google Scholar]
- 9. Yaslianifard S, Mobarez AM, Fatolahzadeh B, Feizabadi MM. Colonization of hospital water systems by Legionella pneumophila, Pseudomonas aeroginosa, and Acinetobacter in ICU wards of Tehran hospitals. Indian J Pathol Microbiol 2012; 55: 352– 356. [DOI] [PubMed] [Google Scholar]
- 10. Xavier DE, Picão RC, Girardello R, Fehlberg LC, Gales AC. Efflux pumps expression and its association with porin down-regulation and beta-lactamase production among Pseudomonas aeruginosa causing bloodstream infections in Brazil. BMC Microbiol 2010; 10: 217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dumas JL, van Delden C, Perron K, Köhler T. Analysis of antibiotic resistance gene expression in Pseudomonas aeruginosa by quantitative real-time-PCR. FEMS Microbiol Lett 2006; 254: 217– 225. [DOI] [PubMed] [Google Scholar]
- 12. Quale J, Bratu S, Gupta J, Landman D. Interplay of efflux system, ampC, and oprD expression in carbapenem resistance of Pseudomonas aeruginosa clinical isolates. Antimicrob Agents Chemother 2006; 50: 1633– 1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pourakbari B, Movahedi Z, Mahmoudi S, Sabouni F, Ashtiani MT, Sadeghi RH, et al. Genotypic characteristics of Pseudomonas aeruginosa strains circulating in the tertiary referral children’s medical hospital in Tehran, Iran. Br J Biomed Sci 2012; 69: 169– 172. [PubMed] [Google Scholar]
- 14. Movahedi Z, Pourakbari B, Mahmoudi S, Sabouni F, Ashtiani Haghi MT, Hosseinpour Sadeghi R, et al. Pseudomonas aeruginosa infection among cystic fibrosis and ICU patients in the referral children medical hospital in Tehran, Iran. J Prev Med Hyg 2013; 54: 24– 28. [PMC free article] [PubMed] [Google Scholar]
- 15. Pourakbari B, Sadr A, Ashtiani MT, Mamishi S, Dehghani M, Mahmoudi S, et al. Five-year evaluation of the antimicrobial susceptibility patterns of bacteria causing bloodstream infections in Iran. J Infect Dev Ctries 2012; 6: 120– 125. [DOI] [PubMed] [Google Scholar]
- 16. Ghazi M, Khanbabaee G, Fallah F, Kazemi B, Mahmoudi S, Navidnia M, et al. Emergence of Pseudomonas aeruginosa cross-infection in children with cystic fibrosis attending an Iranian referral pediatric center. Iran J Microbiol 2012; 4: 124– 129. [PMC free article] [PubMed] [Google Scholar]
- 17. Alekshun MN, Levy SB. Molecular mechanisms of antibacterial multidrug resistance. Cell 2007; 128: 1037– 1050. [DOI] [PubMed] [Google Scholar]
- 18. Richards MJ, Edwards JR, Culver DH, Gaynes RP. Nosocomial infections in pediatric intensive care units in the United States. Pediatrics 1999; 103: e39. [DOI] [PubMed] [Google Scholar]
- 19. Chen HY, Yuan M, Livermore DM. Mechanisms of resistance to beta-lactam antibiotics amongst Pseudomonas aeruginosa isolates collected in the UK in 1993. J Med Microbiol 1995; 43: 300– 309. [DOI] [PubMed] [Google Scholar]
- 20. Aeschlimann JR. The role of multidrug efflux pumps in the antibiotic resistance of Pseudomonas aeruginosa and other gram-negative bacteria. Insights from the society of infectious diseases pharmacists. Pharmacotherapy 2003; 23: 916– 924. [DOI] [PubMed] [Google Scholar]
- 21. Vatcheva-Dobrevska R, Mulet X, Ivanov I, Zamorano L, Dobreva E, Velinov T, et al. Molecular epidemiology and multidrug resistance mechanisms of Pseudomonas aeruginosa isolates from Bulgarian hospitals. Microb Drug Resist 2013; 19: 355– 361. [DOI] [PubMed] [Google Scholar]
- 22. Adabi M, Talebi-Taher M, Arbabi L, Afshar M, Fathizadeh S, Minaeian S, et al. Spread of efflux pump over-expressing-mediated fluoroquinolone resistance and multidrug resistance in Pseudomonas aeruginosa by using an efflux pump inhibitor. Infect Chemother 2015; 47: 98– 104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Arabestani MR, Rajabpour M, Yousefi Mashouf R, Alikhani MY, Mousavi SM. Expression of effulux pump MexAB-OprM and OprD of Pseudomonas aeruginosa strains isolated from clinical samples using qRT-PCR. Arch Iran Med 2015; 18: 102– 108. [PubMed] [Google Scholar]
- 24. Mesaros N, Glupczynski Y, Avrain L, Caceres NE, Tulkens PM, Van Bambeke F. A combined phenotypic and genotypic method for the detection of Mex efflux pumps in Pseudomonas aeruginosa. J Antimicrob Chemother 2007; 59: 378– 386. [DOI] [PubMed] [Google Scholar]
- 25. Llanes C, Hocquet D, Vogne C, Benali-Baitich D, Neuwirth C, Plésiat P. Clinical strains of Pseudomonas aeruginosa overproducing MexAB-OprM and MexXY efflux pumps simultaneously. Antimicrob Agents Chemother 2004; 48: 1797– 1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tomás M, Doumith M, Warner M, Turton JF, Beceiro A, Bou G, et al. Efflux pumps, OprD porin, AmpC beta-lactamase, and multiresistance in Pseudomonas aeruginosa isolates from cystic fibrosis patients. Antimicrob Agents Chemother 2010; 54: 2219– 2224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ziha-Zarifi I, Llanes C, Köhler T, Pechere JC, Plesiat P. In Vivo emergence of multidrug-resistant mutants of Pseudomonas aeruginosa overexpressing the active efflux system MexA-MexB-OprM. Antimicrob Agents Chemother 1999; 43: 287– 291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Aghazadeh M, Hojabri Z, Mahdian R, Nahaei MR, Rahmati M, Hojabri T, et al. Role of efflux pumps: MexAB-OprM and MexXY (-OprA), AmpC cephalosporinase and OprD porin in non-metallo-β-lactamase producing Pseudomonas aeruginosa isolated from cystic fibrosis and burn patients. Infect Genet Evol 2014; 24: 187– 192. [DOI] [PubMed] [Google Scholar]
- 29. Lee A, Mao W, Warren MS, Mistry A, Hoshino K, Okumura R, et al. Interplay between efflux pumps may provide either additive or multiplicative effects on drug resistance. J Bacteriol 2000; 182: 3142– 3150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Yoneda K, Chikumi H, Murata T, Gotoh N, Yamamoto H, Fujiwara H, et al. Measurement of Pseudomonas aeruginosa multidrug efflux pumps by quantitative real-time polymerase chain reaction. FEMS Microbiol Lett 2005; 243: 125– 131. [DOI] [PubMed] [Google Scholar]
- 31. Savli H, Karadenizli A, Kolayli F, Gundes S, Ozbek U, Vahaboglu H. Expression stability of six housekeeping genes: A proposal for resistance gene quantification studies of Pseudomonas aeruginosa by real-time quantitative RT-PCR. J Med Microbiol 2003; 52: 403– 408. [DOI] [PubMed] [Google Scholar]