Abstract
Introduction
Older minority groups are more likely to have poor AED adherence. We describe adherence to antiepileptic drugs (AEDs) among older Americans with epilepsy.
Methods
In retrospective analyses of 2008–2010 Medicare claims for a 5% random sample of beneficiaries augmented by minority representation, epilepsy cases in 2009 were those with ≥1 claim with ICD-9 345.x or ≥2 with 780.3x, and ≥1 AED. New onset cases had no such claims or AEDs in the year before the 2009 index event. We calculated the Proportion of Days Covered (PDC) (days with ≥1 AED over total follow-up days) and used logistic regression to estimate associations of non-adherence (PDC <0.8) with minority group adjusting for covariates.
Results
Of 36,912 epilepsy cases (19.2% White, 62.5% African American (AA), 11.3% Hispanic, 5.0% Asian and 2% American Indian/Alaskan Native), 31.8 % were non-adherent (range: 24.1% Whites to 34.3% AAs). Of 3,706 new onset cases, 37% were non-adherent (range: 28.7% Whites to 40.5% AAs). In adjusted analyses, associations with minority group were significant among prevalent cases, and for AA and Asians vs. Whites among new cases. Among other findings, beneficiaries from high poverty ZIP codes were more likely to be non-adherent than their counterparts, and those in cost-sharing drug benefit phases were less likely than those in deductible phases.
Conclusion
About a third of older adults with epilepsy have poor AED adherence; minorities are more likely than Whites. Investigations of reasons for non-adherence, and interventions to promote adherence, are needed with particular attention to the effect of cost-sharing and poverty.
Keywords: epilepsy, adherence, Medicare, older adults, Part D coverage
1. Introduction
Antiepileptic drugs (AEDs) are the foundation of epilepsy treatment. AEDs help patients to maintain seizure control and limit negative clinical outcomes associated with epilepsy [1]. AED effectiveness is minimized if prescribed regimens are not followed [2]. Adherence is the degree to which patients’ drug taking is consistent with instructions provided by health professionals [3]. Nonadherence to AEDs is associated with the development of pharmacoresistance, higher risk of seizures, fractures, and head injuries, increased medical resource utilization and costs, impaired quality of life, and increased mortality [2, 4–7].
Previous studies have reported that 20–60% of adults with epilepsy are non-adherent to their prescribed AED therapy [6, 8, 9]. Some demographic groups may be more likely to have poor adherence and suffer its consequences. For example, minorities and older adults are more likely to be non-adherent to AEDs than their counterparts [2, 10]. Among adults 65 years old and older with epilepsy in a VA population, about 50% had poor adherence to their AED treatment [11]. Additionally, among adults 65 years and older in a managed care population with epilepsy about 40% had poor adherence to AEDs [12]. This is concerning given the importance of adequate AED treatment to prevent seizures and the high incidence of epilepsy in the older age groups [13]. The poor adherence found in older adults may be due to the sensitivity to AED side effects, personal factors such as the existence of multiple comorbid conditions and associated polypharmacy, and economic reasons such as drug affordability. There is evidence that adherence varies by AED, with older drugs like phenytoin, commonly prescribed in older adults, being associated with lower adherence [6, 11, 12]. The degree to which older adults from minority groups adhere to their AED treatment, however, is currently unclear.
The purpose of this study was to characterize the adherence to AED treatment in diverse cohort of older adults with epilepsy. We identified epilepsy cases among Medicare beneficiaries with part D plans, to date the largest population of older Americans for which adherence has been reported. We further examined whether adherence varied across the demographic groups of older Medicare beneficiaries, namely African Americans, Hispanics, Asians, American Indian/Alaskan Native (AI/AN) and Whites. We also examined if differences in adherence were explained by differences in AED prescribed, personal characteristics, comorbid conditions, socioeconomic factors, and Medicare Part D benefit characteristics.
2. Materials and Methods
This study, reviewed and approved by the Institutional Review Board of the University of Alabama at Birmingham, consists of a retrospective analysis of 2008–2010 administrative claims from the Center for Medicare and Medicaid Services of a 5% random sample of Medicare beneficiaries 66 and older in 2008 augmented with sample of beneficiaries of the same age who were African American, Hispanic, Asian and AI/AN and had administrative claims for seizures and epilepsy. Race/ethnicity was defined as in the Medicare data set based on the Research Triangle Institute (RTI) Race Code, an enhanced race/ethnicity designation based on first and last name algorithms [14].
2.1 Epilepsy case identification
Medicare beneficiaries with a claim-based epilepsy diagnosis in 2009 were defined as those who had the following: i) at least one claim (inpatient, outpatient or physician visit) with International Classification of Disease- version 9 (ICD-9) codes 345.xx, or at least two claims 780.3x that were 30 days apart; and ii) at least one prescription of 60 days or more for AEDs in 2009. Epilepsy identifying algorithms like this were found to have a positive predictive value of 94% among older veterans [15]. Among these identified epilepsy cases, we considered those beneficiaries who had at least one year of follow-up from the 2009 index event (first claim with epilepsy or seizure diagnosis code). The follow-up was characterized by coverage for Medicare Part A (hospital insurance), B (coverage for outpatient and physician visits), and D (prescription drug coverage), and no participation in managed care plans, for the entire year or until death if death occurred within the year. Following these criteria, we identified 36,912 beneficiaries with epilepsy.
Among these 36,912 cases, we defined 8,787 probable new cases who had a clean period of 365 days before the index event, i.e., a period with i) continuous coverage with Part A, B, and D, ii) no claims for epilepsy or seizures, and iii) no prescriptions for AED drugs typically prescribed exclusively for epilepsy, namely Carbamazepine, Ethosuximide, Felbamate, Levetiracetam, Methsuximide, Phenytoin, Oxcarbazepine, and Tiagabine. Of the probable new cases, 3,706 were those who did not have any AED in the clean period (possible new cases).
2.2 Main Outcome
To determine adherence we considered any AED prescription filled by the population with epilepsy identified above. We measured adherence by calculating the Proportion of Days Covered (PDC) which is defined as the ratio of days with at least one AED prescription over the total days of follow-up. The total days of follow-up were defined as the length of time from the start of the first AED to the end of the follow-up period. Using the available data on the start date of prescriptions and the number of days the prescriptions were for, we calculated the number of days with at least one AED as the period from the start of the first AED to the last AED in the follow-up excluding any days in between with no AED prescriptions. Non-adherence was defined as a PDC < 0.80 [9].
2.3 Analysis
We examined the following characteristics of epilepsy cases: 1) individual factors: age at diagnosis, gender, number of comorbid conditions; 2) neurology visits i.e., having at least one claim for a visit with a neurologist or neurosurgeon in the 45 days before to the 60 days period post the 2009 epilepsy index event; 3) Part D Coverage: Part D benefit phase for the drug prescribed before the first observed AED prescription; 4) socio-economic factors: being eligible for Part D Low Income Subsidy (LIS), ZIP code level indicators of poverty; and 5) geography: US region of residence (Northeast, West, Midwest, and South). Comorbid conditions were identified in the one-year before the epilepsy index event using algorithms based on the Charlson Comorbidity score.[16] In 2009–2010, the Part D phases were, in order of occurrence, as follows: 1) Deductible in which beneficiaries pay the full cost of the drug; 2) Copayment/Coinsurance in which beneficiaries pay a copayment or co-insurance for covered prescription drugs until they reached a set level of out-of-pocket costs; 3) Coverage Gap (donut hole) in which beneficiaries, depending on the plans, paid the full cost of prescription drugs; and 4) Catastrophic Coverage in which Medicare covered most of prescription drug cost. ZIP code level information on poverty was obtained from the 2010 Census. We created an indicator for high poverty corresponding to ZIP codes where >20% of households lived below 100% of the Federal Poverty Line. We compared characteristics across prevalent, probable and possible new cases, and compared cases to a cohort of Medicare beneficiaries from the 5% random sample who may or may not have epilepsy and who had a one-year follow-up similar to the epilepsy cases but defined starting from a random date in 2009.
We tested for differences in non-adherence by minority group using logistic regression models adjusting for the characteristics described above. In addition, we adjusted for the type of AED taken by including a binary indicator for enzyme-inducing (EI) AEDs (phenytoin, carbamazepine, phenobarbital and primidone, and the corresponding brand name drugs) versus all other AEDs.
3. Results
Of the 36,912 prevalent cases of epilepsy included in this analysis, 19.2% were White, 62.5% African American, 11.3% Hispanic, 5.0% Asian, and 2.0% AI/AN (Table 1). The majority of the cases were female (61.6%), live in the south (50.3%), and were eligible for the Part D Low Income Subsidy (82.0%). A higher proportion of cases were ages 65–74 (41.5%) compared to the older age categories. Nearly half (46.0%) had 4 or more comorbidities in the year before the epilepsy diagnosis, and a third (36.3%) saw a neurologist close to diagnosis.
Table 1.
Characteristics of Medicare beneficiaries with epilepsy and in a random sample, 2009
| Prevalent epilepsy cases | New epilepsy cases | Medicare beneficiaries’ random sample | ||
|---|---|---|---|---|
|
| ||||
| N = 36,912 | Probable N = 8,787 |
Possible N = 3,706 |
N = 633,710 | |
| White | 19.2 | 21.3 | 18.0 | 87.0 |
| African American | 62.5 | 58.4 | 61.2 | 7.8 |
| Hispanic | 11.3 | 12.0 | 12.3 | 2.4 |
| Asian | 5.0 | 6.1 | 6.6 | 2.4 |
| AI/AN | 2.0 | 2.2 | 2.0 | 0.4 |
| Female | 61.6 | 66.3 | 64.9 | 69.1 |
| Age in 2009 | ||||
| 65–74 | 41.5 | 39.4 | 34.9 | 38.4 |
| 75–84 | 36.1 | 36.4 | 37.3 | 36.1 |
| 85+ | 22.4 | 24.1 | 27.8 | 26.0 |
| Comorbid conditions | ||||
| 0 | 8.3 | 5.1 | 3.7 | 41.6 |
| 1–3 | 45.7 | 42.6 | 41.0 | 39.3 |
| 4+ | 46.0 | 52.3 | 55.3 | 19.1 |
| Neurologist close to diagnosis | 36.3 | 54.9 | 72.8 | 5.3 |
| LISa eligible | 82.0 | 79.9 | 77.2 | 33.5 |
| Medicare/Medicaid | 69.6 | 68.1 | 65.5 | 29.5 |
| Medicare Part D Phaseb | ||||
| Deductible | 19.3 | 14.4 | 17.0 | 16.8 |
| Copay/coinsurance | 59.2 | 58.3 | 60.4 | 58.0 |
| Coverage gap (donut hole) | 13.8 | 17.6 | 15.2 | 9.0 |
| Catastrophic | 5.1 | 6.4 | 4.2 | 3.6 |
| No Phase | 2.6 | 3.3 | 3.3 | 12.7 |
| Region of residencec | ||||
| South | 50.2 | 48.9 | 49.2 | 38.8 |
| West | 13.3 | 15.3 | 15.1 | 16.0 |
| Mid West | 17.7 | 17.1 | 17.0 | 25.9 |
| North East | 18.7 | 18.8 | 18.8 | 19.4 |
AI/AN = American Indian/Alaskan Native;
LIS = Part D Low Income Subsidy;
2009 Part D benefit phase for the drug before the first AED in 2009 for epilepsy cases or first drug post pseudo diagnosis for comparison group;
South = DE, DC, FL, GA, MD, NC, SC, VA, WV, AL, KY, MS, TN, AR, LA, OK, TX; West = AZ, CO, ID, NM, MT, UT, NV, WY, AK, CA, HI, OR, WA; Midwest = IN, IL, MI, OH, WI, IA, NE, KS, ND, MN, SD, MO; Northeast = CT, ME, MA, NH, RI, VT, NJ, NY, PA
Of the new cases (8787 probable new cases and 3706 possible new cases) in 2009, the demographic distribution was similar to prevalent cases except higher proportions of the new cases had 4 or more comorbidities (probable cases 52.3% and possible cases 55.3%) and saw a neurologist (probable cases 54.9% and possible cases 72.8%). Because of our study design, a random sample of Medicare beneficiaries on Part D with similar follow-up time had fewer African American (7.8%), Hispanic (2.4%), Asian (2.4%) and AI/AN (0.4%) beneficiaries (Table 1). This sample also had fewer beneficiaries with high comorbidity (19.1%), with neurology visits (13.2%).
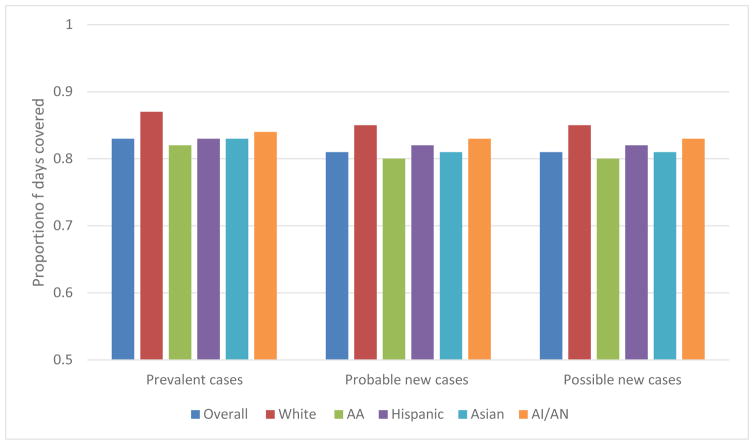
The mean PDC overall was 0.83 for prevalent epilepsy cases, and 0.81 for probable and possible new cases, with the highest PDC for Whites and the lowest for African Americans across all cases (Figure 1). Among prevalent cases, 31.8 % were non-adherent, from 24.1% for Whites to 34.3% for African Americans (Table 2). Additionally, a higher proportion of prevalent cases who were on non-enzyme-inducing (non-EI) AEDs (34.0%) were non-adherent compared to 30.6% of those on EI-AEDs (30.6%). Adherence varied by AED. Among the most common AEDs, non-adherence was highest for those on Pregabalin (31.9%) and Levetiracetam (31.8%) and lowest for those on Lamotrigine (24.6%) and Carbamazepine (25.4%). This was somewhat similar across minority groups except for AI/AN for whom non-adherence was lowest for those on Pregabalin (23.5%).
Figure 1.
Mean Proportion of Days Covered by Racial/Ethnic Group for Prevalent, and Probable and Possible New Epilepsy Cases among older Medicare Beneficiaries, 2009
Table 2.
Proportion (%) of non-adherence to AEDs among older adults with epilepsy, overall, by race/ethnicity, and by AED (2009)
| White | AA | Hispanic | Asian | AI/AN | Overall | |
|---|---|---|---|---|---|---|
|
Prevalent cases (N = 36,912)
| ||||||
| Overall | 24.1 | 34.3 | 31.5 | 30.6 | 31.9 | 31.8 |
| By type of AED | ||||||
| EI-AED | 22.4 | 33.1 | 30.4 | 29.3 | 30.6 | 30.6 |
| Non EI AED | 26.7 | 36.7 | 33.7 | 32.3 | 35.2 | 34.0 |
| By specific AEDs (most common) | ||||||
| Phenytoin | 22.7 | 33.7 | 31.4 | 29.9 | 32.3 | 31.4 |
| Levetiracetam | 23.9 | 34.6 | 28.8 | 29.5 | 26.2 | 31.8 |
| Divalproex | 26.0 | 33.0 | 31.3 | 34.9 | 28.7 | 31.5 |
| Lamotrigine | 21.5 | 26.1 | 25.7 | 22.3 | 34.2 | 24.6 |
| Gabapentin | 24.8 | 32.1 | 32.4 | 29.8 | 29.0 | 30.6 |
| Carbamazepine | 19.6 | 27.5 | 26.7 | 22.0 | 27.8 | 25.4 |
|
| ||||||
|
Probable new epilepsy cases (N = 8,787)
| ||||||
| Pregabalin | 24.7 | 34.6 | 30.0 | 37.5 | 23.5 | 31.9 |
| Overall | 28.5 | 38.8 | 33.9 | 35.5 | 35.6 | 35.8 |
| By type of AED | ||||||
| EI-AED | 28.4 | 39.4 | 32.7 | 34.3 | 33.3 | 36.0 |
| Non EI AED | 28.5 | 38.6 | 34.4 | 35.9 | 36.7 | 35.6 |
| By specific AEDs (most common) | ||||||
| Phenytoin | 32.3 | 40.6 | 32.5 | 33.3 | 35.7 | 37.9 |
| Levetiracetam | 27.4 | 41.7 | 34.9 | 33.9 | 32.4 | 37.6 |
| Divalproex | 28.6 | 37.0 | 32.2 | 37.2 | 33.3 | 34.7 |
| Lamotrigine | 26.6 | 31.6 | 30.8 | 24.1 | 21.4 | 29.0 |
| Gabapentin | 34.4 | 38.0 | 39.9 | 34.7 | 36.9 | 37.3 |
| Carbamazepine | 38.2 | 41.8 | 39.3 | 35.7 | 75.0 | 41.0 |
| Pregabalin | 33.0 | 43.3 | 31.2 | 43.8 | 20.0 | 38.4 |
|
| ||||||
| Possible new cases of epilepsy (N = 3,706) | ||||||
|
| ||||||
| Overall | 28.7 | 40.5 | 31.8 | 37.1 | 35.6 | 37.0 |
| By type of AED | ||||||
| EI-AED | 32.0 | 41.0 | 29.8 | 40.3 | 37.1 | 38.1 |
| Non EI AED | 26.7 | 40.0 | 33.3 | 35.7 | 34.2 | 36.1 |
| By specific AEDs (most common) | ||||||
| Phenytoin | 33.7 | 40.7 | 29.2 | 35.1 | 35.5 | 38.0 |
| Levetiracetam | 27.0 | 40.8 | 34.7 | 34.0 | 31.8 | 37.0 |
| Divalproex | 35.6 | 39.4 | 25.0 | 43.3 | 45.5 | 37.3 |
| Lamotrigine | 35.9 | 26.2 | 40.9 | 30.0 | 0 | 31.3 |
| Gabapentin | 25.5 | 43.0 | 38.6 | 38.5 | 44.4 | 39.5 |
| Carbamazepine | 23.8 | 42.5 | 38.1 | 33.3 | 50.0 | 38.1 |
| Pregabalin | 35.7 | 50.0 | 41.2 | 50.0 | 0.0 | 44.8 |
AI/AN = American Indian/Alaskan Native;
Among probable new cases, 35.8 % were non-adherent, from 28.5% for Whites to 38.8% for African Americans (Table 2). The percentage non-adherent was similar for those on EI-AEDs (36.0%) and non EI-AEDs (35.6%). For the most common AEDs, non-adherence for probable new cases was highest for those on Carbamazepine (41.0%) and lowest for those on Lamotrigine (29.0%). There were some differences across minority groups, for example the highest percentage of non-adherence was for Pregabablin (43.3%) among African Americans, and for Gabapentin (39.9%) among Hispanics (Table 2).
Among possible new cases, 37.0 % were non-adherent, from 28.7% for Whites to 40.5% for African Americans (Table 2). The percentage non-adherent was higher for those on EI-AEDs (38.1%) compared to those on non-EI-AEDs (36.1%). Across the most common AEDs, non-adherence among possible new cases was greatest for those on Pregabalin (44.8%) and lowest for those on Lamotrigine (31.3%). These percentages were similar across minority groups, with a few exceptions among Asians and AI/AN.
In logistic regression models, racial/ethnic differences in adherence were significant after adjusting for confounders (Table 3). Among prevalent cases, minorities were more likely to be non-adherent to AEDs than Whites. Similarly, among probable new cases, minorities were more likely to be non/adherent to AEDs: for AI/AN, the association was of similar magnitude but was not statistically significant. Among possible new cases, African Americans and Asians were significantly more likely to be non-adherent to AEDs compared to Whites.
Table 3.
Logistic regression on likelihood of NON-ADHERENCE (PDC <0.80) among epilepsy cases (Prevalent N = 36912; Possible N = 8,787, Probable N = 3706), 2009
| Prevalent cases | Probable cases | Possible cases | |
|---|---|---|---|
|
| |||
| OR (CI) | OR (CI) | OR (CI) | |
| Race/ethnicity (ref White) | |||
| African American | 1.56 (1.46–1.68) | 1.56 (1.37–1.77) | 1.63 (1.32–2.00) |
| Hispanic | 1.40 (1.28–1.54) | 1.27 (1.07–1.52) | 1.15 (0.87–1.52) |
| Asian | 1.41 (1.25–1.54) | 1.41 (1.14–1.74) | 1.42 (1.02–1.97) |
| AI/AN | 1.38 (1.16–1.65) | 1.31 (0.94–1.82) | 1.19 (0.70–2.03) |
| Type of AED | |||
| EI-AED vs Non EI AEDs (ref) | 0.85 (0.81–0.89) | 0.95 (0.86–1.05) | 1.00 (0.87–1.15) |
| Gender (ref Male) | |||
| Female | 1.04 (1.00–1.10) | 1.01 (0.91–1.11) | 1.06 (0.91–1.23) |
| Age in 2009 (ref 65–74) | |||
| 75–84 | 1.02 (0.97–1.08) | 0.95 (0.86–1.06) | 0.84 (0.72–0.99) |
| 85+ | 1.08 (1.02–1.15) | 0.90 (0.80–1.01) | 0.80 (0.67–0.96) |
| Comorbid conditions (ref None) | |||
| 1–3 | 1.09 (1.00–1.19) | 1.13 (0.90–1.40) | 1.18 (0.80–1.73) |
| 4+ | 1.31 (1.20–1.44) | 1.23 (0.99–1.53) | 1.16 (0.79–1.71) |
| Seen neurologist close to diagnosis (ref No neurologist) | 1.14 (1.09–1.20) | 1.12 (1.02–1.23) | 0.95 (0.81–1.11) |
| LISa eligible (ref Not eligible) | 0.89 (0.83–0.95) | 0.86 (0.76–0.99) | 0.95 (0.78–1.15) |
| Part D Coverage Phaseb (ref Deductible) | |||
| Copay/coinsurance | 0.84 (0.78–0.89) | 0.86 (0.75–0.98) | 0.74 (0.61–0.89) |
| Coverage gap (donut hole) | 0.79 (0.73–0.86) | 0.80 (0.68–0.94) | 0.64 (0.50–0.82) |
| Catastrophic coverage | 0.72 (0.65–0.81) | 0.87 (0.70–1.08) | 0.74 (0.51–1.07) |
| No phase | 0.80 (0.69–0.94) | 1.03 (0.78–1.38) | 0.96 (0.62–1.47) |
| Region of residence (ref Northeast) | |||
| Other than northeast | 1.20 (1.13–1.27) | 1.35 (1.20–1.52) | 1.23 (1.02–1.47) |
| ZIP code area | |||
| High Povertyc | 1.16 (1.11–1.22) | 1.13 (1.03–1.24) | 1.01 (0.87–1.16) |
|
| |||
| Number of observations used | 35,410 | 8,406 | 3,562 |
AI/AN = American Indian/Alaskan Native;
Low Income Subsidy;
Coverage phase for the drug prescribed before the first observed AED;
20% or more households below the Federal Poverty Line
Among prevalent cases, several factors were associated with non-adherence (Table 3). Beneficiaries more likely to be non-adherent were older than 85, had more than four comorbid conditions, had at least one neurologist visit, were from regions other than the northeast, and lived in high poverty ZIP code areas. Beneficiaries were less likely to be non-adherent if they were taking EI AEDs, were eligible for Part D LIS, or were in the part D benefit phases other than the deductible (copayment/coinsurance, donut hole, catastrophic coverage). Similar results were found among new probable cases, except there was no association of non-adherence with EI AEDs, age, number of comorbid conditions, and being in certain phases of the Part D benefit plan. Among new probable cases in addition, older age was associated with a lower likelihood of non-adherence, while seen a neurologist, being LIS eligible, or leaving in high poverty ZIP codes were not associated with it.
4. Discussion
In this diverse cohort of older epilepsy cases among Medicare beneficiaries, about a third had less than ideal adherence to antiepileptic drugs. Non-adherence was more prevalent in patients with new onset of epilepsy, i.e., those cases who did not have epilepsy- or seizure-related medical encounters for a least one year before the first event we identified in 2009. Minority groups, in particular African Americans, were more likely to have poor adherence. These differences were significant after accounting for several factors that affect prescription-taking behaviors such as economic constraints. For example, we found a consistent association of poor adherence with being in the deductible Part D benefit phase in which beneficiaries may pay the full cost of their drugs out of pocket, or with being from high poverty ZIP code areas.
Previous studies reported that 20–60% of adult patients with epilepsy are non-adherent to their prescribed AED therapy.[6, 8, 9] Non-adherence to AEDs may be especially problematic in the older population. Older patients are at heightened risk for adverse drug effects that could contribute to AED non-adherence [12]. In a Medicaid population, non-adherence was higher among patients 65 and older (about 32% non-adherent) than among those younger than 65 (about 25% non–adherent) [2]. Similarly, we showed that about 30% of older Medicare beneficiaries on Part D plans with epilepsy were non-adherent. However, as age increased, we found that prevalent cases were more likely to be non-adherent, while probable new cases were less likely. It may be that when new onset epilepsy occurs at a later age, patients are more attentive to AED adherence, as opposed to when epilepsy occurs at a younger age and patients are acclimated to living with epilepsy. The degree of non-adherence in our population was lower than that found in the VA older population, where nearly half of the cases had poor AED adherence [11]. Understanding why there is poor adherence especially among newer cases of epilepsy, and how to prevent it, warrants further investigation.
Differences in adherence across racial/ethnic groups have been reported for younger epilepsy populations [2, 10, 17]. We found that African Americans, Hispanics, AI/AN, and Asians were more likely to be non-adherent than Whites. These results were similar across new cases except for some groups like AI/AN, although this may be due to small sample sizes. Differences remained significant after adjusting for a number of factors that may confound the adherence-race association, for example socioeconomic factors. While this is not a phenomenon confined to epilepsy, racial/ethnic disparities in epilepsy are unsettling [18–20]. African Americans have a high incidence of epilepsy in this age group [21], and, if not treated appropriately, are vulnerable to the consequences of this condition. Therefore, a closer look at the epilepsy treatment of minorities, and whether suboptimal adherence leads to worse outcomes, is warranted.
Adherence across AEDs varies. Similar to other chronic conditions, adherence in epilepsy has been shown to be higher among patients on once daily treatment regimens due to lower pill burden and less regimen complexity compared to those requiring two or more daily doses [22]. Across a number of studies, drugs such as gabapentin, which are taken more than once a day, were associated with lower adherence [6, 11, 12, 23]. Our results are in line with these studies, with the highest adherence being associated with lamotrigine; however, adherence for the other most common AEDs were similar. Overall, among the prevalent cases, we found that beneficiaries taking EI-AEDs were more likely to be adherent than those taking non-EI-AEDs which may have more complex regimens. This result was not significant among potential new cases of epilepsy. Thus, rather than explained by the complexity of the regimen, other factors may explain our results. Among prevalent cases, tolerance to an enzyme-inducing older AED that they may have been effectively taking for a long time may explain the better adherence. On the contrary, these drugs may not be tolerated as well by those starting them at this older age.
Socio-economic factors have a considerable impact on adherence. This is in line with findings by many others on the effect of socio-economic status and medication cost [24, 25]. The benefit phase in which beneficiaries fall right before filling an AED prescription is important as it identifies beneficiaries who were already on a cost-sharing phase when filling the AED prescription. These beneficiaries were less likely to be non-adherent that those who were in the deductible phase, where they paid the full cost of the prescription. Thus, the cost of AEDs is important for full adherence, as also demonstrated by the effect of living in ZIP code areas with high poverty. Paying attention to socioeconomic factors in epilepsy treatment is thus fundamental to ensure optimal outcomes.
Limitations are the common ones related to using administrative claims databases. While claims can be used for research, they are generated for administrative and reimbursement purposes. Therefore, the accuracy of the information must be considered with restraint. Prescription drug claims histories may reflect complex and often erratic patterns of use over time [26]. Medication adherence can be overestimated as claims only measure filled prescriptions and not all medications dispensed are taken by the patient [26]. If this is the case, we may have overestimated the true adherence of this population. Also some cases may have other insurance coverage for their prescriptions which may result in not having all prescription records in the present data. Moreover, some patients may not need new prescriptions if doses are lowered and prescriptions extended. In this case, we may have underestimated the true adherence.
Adherence to AEDs is very important for seizure control. It has been estimated that non-adherence increases seizures by 21% [4] and it is associated with a risk of death 3-fold higher [2]. Non-adherence to AED regimens increases the cost of epilepsy care [1]. Among Medicaid beneficiaries, non-adherent patients had higher number of hospitalizations inpatient days and emergency department visits and an additional cost per quarter of $4,623 for non-adherent patients compared with adherent counterparts [27]. Additionally, re-establishing control of seizures is more expensive than maintenance therapy because it entails additional medical encounters, laboratory studies, and higher medication dosages [28]. Therefore, ensuring adherence to AED treatment is not only important to ensure the quality of life of those older adults affected by epilepsy, but also to control cost of care. In this older large and diverse population of older Americans with epilepsy, adherence to AEDs, although higher than that reported in other studies of older adults, is sub-optimal for a considerable proportion of cases, and especially for some minority groups and for those who may have new onset of epilepsy in this later phase of life. Given the consequences of poor AED adherence on the outcomes of people with epilepsy, further investigations are needed to further understanding how to improve adherence across groups of older adults, paying particular attention to the role that the ability to pay for drugs may have on epilepsy treatment.
Highlights.
About a third of diverse older adults with epilepsy had poor adherence to antiepileptic drugs
Minority groups were more likely to have poor adherence
Poor adherence was also associated with drug cost sharing and poverty
Acknowledgments
Authors are grateful to Aquila Brown-Galvan, Nancy Cohen, Kay Clements for administrative support, medical coding, and clinical input.
Statistical analyses were performed by Chen Dai and Lucia Juarez in the Division of Preventive Medicine, University of Alabama at Birmingham under the supervision of Drs. Pisu and Richman who had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding
This work was supported by the National Institute of Neurological Disease and Stroke (1R01NS080898-01).
Footnotes
Conflict of Interest Disclosures
Dr. Szaflarski received funding from UCB Biosciences, Compumedics Neuroscan Inc., SAGE Therapeutics Inc.; had consulting activity for SAGE Therapeutics Inc., Biomedical Systems Inc., Elite Medical Experts LLC
Dr. Faught has received research support from Brain Sentinel, Eisai, and UCB Pharma, has served on Data Monitoring Boards for Eisai, Lundbeck, SAGE, and SK Life Science, and has received consultation fees from Aprecia, Supernus, Sunovion, and UCB Pharma
Drs. Pisu, Richman, Piper, Martin, Funkhouser, Mr. Dai, and Ms. Juarez, report nothing to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Faught E. Adherence to antiepilepsy drug therapy. Epilepsy Behav. 2012;25:297–302. doi: 10.1016/j.yebeh.2012.08.027. [DOI] [PubMed] [Google Scholar]
- 2.Faught E, Duh MS, Weiner JR, Guerin A, Cunnington MC. Nonadherence to antiepileptic drugs and increased mortality: findings from the RANSOM Study. Neurology. 2008;71:1572–8. doi: 10.1212/01.wnl.0000319693.10338.b9. [DOI] [PubMed] [Google Scholar]
- 3.Paschal AM, Rush SE, Sadler T. Factors associated with medication adherence in patients with epilepsy and recommendations for improvement. Epilepsy Behav. 2014;31:346–50. doi: 10.1016/j.yebeh.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 4.Manjunath R, Davis KL, Candrilli SD, Ettinger A. Association of antiepileptic drug nonadherence with risk of seizures in adults with epilepsy. Epilepsy and Behavior. 2009;14:372–378. doi: 10.1016/j.yebeh.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 5.Modi AC, Wu YP, Rausch JR, Peugh JL, Glauser TA. Antiepileptic drug nonadherence predicts pediatric epilepsy seizure outcomes. Neurology. 2014;83:2085–90. doi: 10.1212/WNL.0000000000001023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davis KL, Candrilli SD, Edin HM. Prevalence and cost of nonadherence with antiepileptic drugs in an adult managed care population. Epilepsia. 2008;49:446–454. doi: 10.1111/j.1528-1167.2007.01414.x. [DOI] [PubMed] [Google Scholar]
- 7.Shallcross AJ, Becker DA, Singh A, Friedman D, Jurd R, French JA, Devinsky O, Spruill TM. Psychosocial factors associated with medication adherence in ethnically and socioeconomically diverse patients with epilepsy. Epilepsy Behav. 2015;46:242–5. doi: 10.1016/j.yebeh.2015.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jones RM, Butler JA, Thomas VA, Peveler RC, Prevett M. Adherence to treatment in patients with epilepsy: associations with seizure control and illness beliefs. Seizure. 2006;15:504–8. doi: 10.1016/j.seizure.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 9.Goodman MJ, Durkin M, Forlenza J, Ye X, Brixner DI. Assessing adherence-based quality measures in epilepsy. Int J Qual Health Care. 2012;24:293–300. doi: 10.1093/intqhc/mzs017. [DOI] [PubMed] [Google Scholar]
- 10.Bautista RE, Graham C, Mukardamwala S. Health disparities in medication adherence between African-Americans and Caucasians with epilepsy. Epilepsy Behav. 2011;22:495–8. doi: 10.1016/j.yebeh.2011.07.032. [DOI] [PubMed] [Google Scholar]
- 11.Zeber J, Copeland LA, Pugh MJ. Variation in antiepileptic drug adherence among older patients with new-onset epilepsy. The Annals of Pharmacotherapy. 2010;44:1896–1904. doi: 10.1345/aph.1P385. [DOI] [PubMed] [Google Scholar]
- 12.Ettinger A, Manjunath R, Candrilli SD, Davis KL. Prevalence and cost of nonadherence to antiepileptic drugs in elderly patients with epilepsy. Epilepsy and Behavior. 2009;14:324–329. doi: 10.1016/j.yebeh.2008.10.021. [DOI] [PubMed] [Google Scholar]
- 13.Brodie MJ, Elder AT, Kwan P. Epilepsy in later life. Lancet Neurol. 2009;8:1019–30. doi: 10.1016/S1474-4422(09)70240-6. [DOI] [PubMed] [Google Scholar]
- 14.Eicheldinger C, Bonito A. More accurate racial and ethnic codes for Medicare administrative data. Health Care Financ Rev. 2008;29:27–42. [PMC free article] [PubMed] [Google Scholar]
- 15.Pugh MJ, Van Cott AC, Cramer JA, Knoefel J, Amuan ME, Tabares J, Ramsay RE, Berlowitz DR Team TiGERT. Trends in antiepileptic drug prescribing for older patients with new-onset epilepsy: 2000–2004. Neurology. 2008;70:2171–2178. doi: 10.1212/01.wnl.0000313157.15089.e6. [DOI] [PubMed] [Google Scholar]
- 16.Wilchesky M, Tamblyn RM, Huang A. Validation of diagnostic codes within medical services claims. J Clin Epidemiol. 2004;57:131–41. doi: 10.1016/S0895-4356(03)00246-4. [DOI] [PubMed] [Google Scholar]
- 17.Davis KL, Candrilli SD, Edin HM. Prevalence and cost of nonadherence with antiepileptic drugs in an adult managed care population. Epilepsia. 2008;49:446–54. doi: 10.1111/j.1528-1167.2007.01414.x. [DOI] [PubMed] [Google Scholar]
- 18.Gerber BS, Cho YI, Arozullah AM, Lee SY. Racial differences in medication adherence: A cross-sectional study of Medicare enrollees. Am J Geriatr Pharmacother. 2010;8:136–45. doi: 10.1016/j.amjopharm.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krousel-Wood MA, Muntner P, Islam T, Morisky DE, Webber LS. Barriers to and determinants of medication adherence in hypertension management: perspective of the cohort study of medication adherence among older adults. Med Clin North Am. 2009;93:753–69. doi: 10.1016/j.mcna.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saha S, Freeman M, Toure J, Tippens KM, Weeks C, Ibrahim S. Racial and ethnic disparities in the VA health care system: a systematic review. J Gen Intern Med. 2008;23:654–71. doi: 10.1007/s11606-008-0521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Faught E, Richman J, Martin R, Funkhouser E, Foushee R, Kratt P, Kim Y, Clements K, Cohen N, Adoboe D, Knowlton R, Pisu M. Incidence and prevalence of epilepsy among older U.S. Medicare beneficiaries. Neurology. 2012;78:448–53. doi: 10.1212/WNL.0b013e3182477edc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Buck D, Jacoby A, Baker GA, Chadwick DW. Factors influencing compliance with antiepileptic drug regimes. Seizure. 1997;6:87–93. doi: 10.1016/s1059-1311(97)80060-x. [DOI] [PubMed] [Google Scholar]
- 23.Arif H, Buchsbaum R, Pierro J, Whalen M, Sims J, Resor SR, Jr, Bazil CW, Hirsch LJ. Comparative effectiveness of 10 antiepileptic drugs in older adults with epilepsy. Arch Neurol. 2010;67:408–15. doi: 10.1001/archneurol.2010.49. [DOI] [PubMed] [Google Scholar]
- 24.Wheeler DC, Waller LA, Elliott JO. Modeling epilepsy disparities among ethnic groups in Philadelphia, PA. Stat Med. 2008;27:4069–85. doi: 10.1002/sim.3261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chin RF, Neville BG, Peckham C, Wade A, Bedford H, Scott RC, Group NC. Socioeconomic deprivation independent of ethnicity increases status epilepticus risk. Epilepsia. 2009;50:1022–9. doi: 10.1111/j.1528-1167.2008.01796.x. [DOI] [PubMed] [Google Scholar]
- 26.Crystal S, Akincigil A, Bilder S, Walkup JT. Studying prescription drug use and outcomes with medicaid claims data: strengths, limitations, and strategies. Med Care. 2007;45:S58–65. doi: 10.1097/MLR.0b013e31805371bf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Faught RE, Weiner JR, Guerin A, Cunnington MC, Duh MS. Impact of nonadherence to antiepileptic drugs on health care utilization and costs: Findings from the RANSOM study. Epilepsia. 2009;50:501–509. doi: 10.1111/j.1528-1167.2008.01794.x. [DOI] [PubMed] [Google Scholar]
- 28.Zachry WM, 3rd, Doan QD, Smith BJ, Clewell JD, Griffith JM. Direct medical costs for patients seeking emergency care for losses of epilepsy control in a U.S. managed care setting. Epilepsy Behav. 2009;16:268–73. doi: 10.1016/j.yebeh.2009.07.042. [DOI] [PubMed] [Google Scholar]