Abstract
Phaeohyphomycosis is a rare mycotic infection caused by various heterogenous groups of phaeoid (dematiaceous) fungi involving the skin and subcutaneous tissue. Common clinical manifestations are subcutaneous abscesses or cystic swellings. Here, we report a case of subcutaneous phaeohyphomycosis presenting as multiple asymptomatic cystic swellings over the hands and feet without any predisposing factors. Histopathology showed granulomatous inflammation and special stain with Grocott's methanamine silver stain revealed broad pigmented hyphae. Culture showed black-colored colonies identified as Exophiala jeanselmi. The patient was treated with surgical excision of the lesions.
Keywords: E. jeanselmi, multiple cystic swellings, phaeohyphomycosis
Introduction
Phaeohyphomycosis is a group of mycotic infections caused by dematiaceous fungi (pigmented) that contain melanin in their cell walls. Melanin is a known virulence factor in these fungi, and it acts by scavenging free radicals produced by phagocytic cells in the oxidative process, which would kill most organisms, and also prevents their action on the plasma membrane by binding to hydrolytic enzymes.[1] The formation of fungal appressorium, which helps in fungal penetration into the host cell is also influenced by the melanin.[1] All these actions explain the pathogenic potential of dematiaceous fungi even in an immunocompetent host. The fungus is present in host tissues as brownish hyphae, pseudohyphae, yeast cells, or combination of these forms.[2] These organisms are widespread in the environment, being found in soil, wood, and decomposing plant debris. They are distributed worldwide and are more common in tropical and subtropical climates. The major etiologic agents of phaeohyphomycosis are species of Bipolaris, Exophiala, Curvularia, Chaetomium, Phoma, Exserohilum, and Wangiella.[3] It is a rare infection mostly involving the skin and subcutis, and rarely involving the paranasal sinuses, eyes, central nervous system, lymph nodes, and bone.[4] The clinical presentation ranges from solitary cutaneous nodules to deep subcutaneous abscesses.[5] The subcutaneous infections typically occur on the exposed areas of the body, especially the extremities, fingers, wrists, knees, or ankles, resulting from traumatic inoculation.[3] Histopathological examination (HPE) and culture is important in the diagnosis of phaeohyphomycosis. We report this case for its uncommon clinical presentation with multiple cystic swellings on both the feet and right hand in an immunocompetent individual.
Case Report
A 35-year-old male agriculturist presented with multiple asymptomatic swellings on the dorsum of right hand, both feet, and ankle region of 6 months’ duration. History of occasional yellowish discharge was present. There was no history of trauma, fever or intake of medication, and any other underlying systemic disease.
Cutaneous examination revealed multiple skin-colored, nontender, firm-to-soft, cystic swellings approximately 3 cm in diameter present on the ankle region and feet. Multiple swellings were coalesced to form a large fluctuant mass measuring 8–10 cm, present on the dorsum of right hand [Figure 1]. There was no lymphadenopathy. A differential diagnosis of multiple abscesses, calcinosis cutis, and deep fungal infection were considered.
Figure 1.

8 × 10 cm confluent nodular swelling over the dorsum of the hand
Routine investigations were normal. While performing an excisional biopsy, there was purulent discharge from the biopsy site, and hence all the lesions were incised [Figure 2]. Pus was sent for Gram stain and culture. Cyst material was sent for HPE Gram stain was negative for bacteria and on culture with Sabouraud's dextrose agar, pigmented fungi were identified and lactophenol cotton blue showed Exophiala jeanselmi species [Figure 3]. Cyst material for HPE showed multiple granulomas and Grocott's methanamine silver (GMS) stain showed broad brownish filaments [Figures 4 and 5].
Figure 2.

Multiple cystic swellings over the feet
Figure 3.
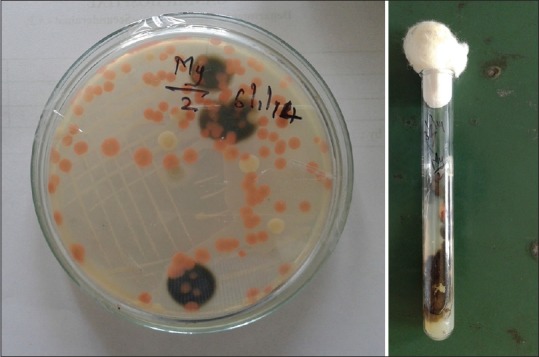
Pigmented fungi on Sabouraud's dextrose agar
Figure 4.
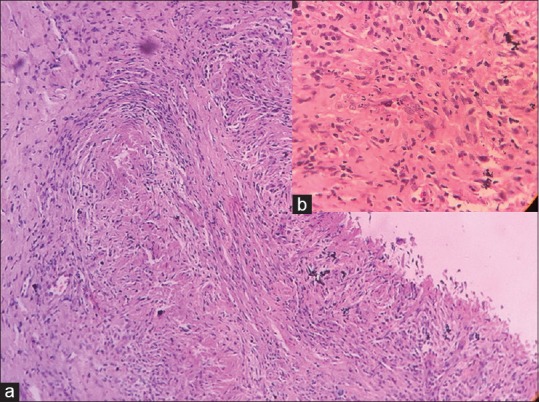
(a) (H and E, ×10) Granuloma in the dermis composed of epithelioid cells, lymphocytes, and fibroblasts. (b) (H and E, ×100) closer view
Figure 5.
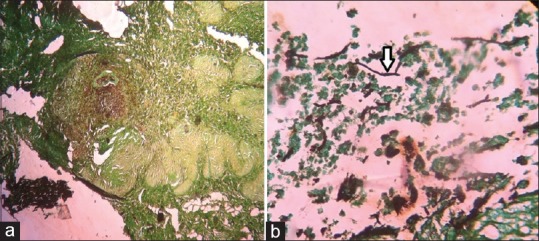
(a) Granulomas with pigmented fungal growth (scanner view – GMS) (b) Pigmented fungal filaments (High power view – GMS)
The patient was treated by surgical excision of the lesions without any antifungal therapy.
Discussion
The infections caused by dematiaceous (melanized) fungi are grouped into three classes that include phaeohyphomycosis, chromoblastomycois, and eumycotic mycetoma.[3] Phaeohyphomycosis represents a broad range of primary and opportunistic mycoses classified into four clinical forms, which includes superficial, cutaneous, subcutaneous, systemic, and disseminated forms (brain, eye, central nervous system, peritoneum, bones). Subcutaneous infections mostly occur on the limbs, fingers, wrist, knees, or ankles. The immune status of the host plays a major role in the clinical presentation which could range from papulonodules, verrucous, hyperkeratotic, or ulcerated plaques, cysts, abscesses, pyogranuloma, nonhealing ulcers, or sinuses.
Subcutaneous phaeohyphomycosis is a rare infection, however, the number of cases appears to be increasing in recent years as the number of immunocompromised patients also have increased.[6] However, our case showed that immunocompromised state is not a necessary prerequisite for phaeohyphomycosis. Infection usually occurs through traumatic inoculation of the skin and subcutaneous tissue[7] with contaminated matter, with majority of lesions occurring on the feet and legs of outdoor workers, as observed in this patient. The age of patients ranges from 3 to 60 years. Males are more commonly affected because of their outdoor occupation. It is more common in tropical and subtropical climates.
The most common etiological agents of subcutaneous phaeohyphomycosis are E. jeanselmi followed by E. dermatitidis.[3] The genus Exophiala is widely distributed in the environment and may cause infections in both immunocompromised (human immunodeficiency virus patients, transplant recipients, debilitating chronic diseases, diabetes, and immunosuppressive therapy) and rarely, in immunocompetent persons. E. jeanselmi usually causes mild cutaneous and subcutaneous infections which are often localized and solitary (phaeohypomycotic cyst).[8] Even in severely immunosuppressed patients Exophiala infection often tends to stay localized.[5]
Common clinical presentation is solitary subcutaneous cyst or abscess, firm to fluctuant, usually sparing the overlying skin. The common site of involvement is upper and lower limbs over the fingers, wrist, knees, or ankles, and less frequently on the face, neck, and scalp. All dematiaceous fungi are similar in morphology and can be differentiated only by culture.
According to Sharma et al.[3] who reviewed the literature on phaeohyphomycosis, 23 patients with subcutaneous phaeohyphomycosis have been reported from India predominantly involving the extremities and very few cases with dissemination. In a study by Murayama et al.,[9] 54 cases of phaeohyphomycosis due to E. jeanselmi were reviewed, however, they failed to identify any underlying disease in 31 cases. Our patient also showed that there was no underlying disease predisposing to phaeohyphomycosis, as reported by Murayama et al.
Our case report highlights the fact that any subcutaneous soft swellings must also be considered under differential diagnosis for fungal infections as they may be mistaken for lipoma, fibroma, epidermal cyst, or foreign body reaction. Surgical excision of the lesion with or without antifungal agents (itraconazole, ketaconazole, amphotericin B) has been widely used in treatment of subcutaneous phaeohyphomycosis.
The present case presented with multiple lesions, and all the lesions were excised. Surgical excision of lesions showed no relapse even after 6 months without any antifungal therapy. Patient is still under follow-up.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We thank Dr. Gajendra Jyothi Lakshmi, Associate Professor, Department of Microbiology, Gandhi medical college, Hyderabad, for the support.
References
- 1.Jacobson ES. Pathogenic roles for fungal melanins. Clin Microbiol Rev. 2000;13:708–17. doi: 10.1128/cmr.13.4.708-717.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kwon Chung KJ, Bennett JE. Phaeohyphomycosis. Med Mycology. Pennsylvania: Lea and Febiger; 1992. [Google Scholar]
- 3.Rinaldi MG. Phaeohyphomycosis. Dermatol Clin. 1996;14:147–53. doi: 10.1016/s0733-8635(05)70335-1. [DOI] [PubMed] [Google Scholar]
- 4.Sharma NL, Mahajan V, Sharma RC, Sharma A. Subcutaneous Phaeohyphomycosis in India: A case report and review. Int J Dermatol. 2002;41:16–20. doi: 10.1046/j.1365-4362.2002.01337.x. [DOI] [PubMed] [Google Scholar]
- 5.Rajendran C, Khaitan BK, Mittal R, Ramam M, Bhardwaj M, Datta KK. Phaeohyphomycosis caused by Exophiala spinifera in India. Med Mycol. 2003;41:437–41. doi: 10.1080/1369378031000153820. [DOI] [PubMed] [Google Scholar]
- 6.Mishra D, Singal M, Rodha MS, Subramanian A. Subcutaneous Phaeohyphomycosis of Foot in an Immunocompetent Host. J Lab Physicians. 2011;3:122–4. doi: 10.4103/0974-2727.86848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manoharan M, Shanmugam N, Veeriyan S. A Rare Case of a Subcutaneous Phaeomycotic Cyst with a Brief Review of Literature. Malays J Med Sci. 2011;18:78–81. [PMC free article] [PubMed] [Google Scholar]
- 8.Madke B, Khopkar U. Pheohyphomycotic cyst. Indian Dermatol Online J. 2015;6:223–5. doi: 10.4103/2229-5178.156429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murayama N, Takimoto R, Kawai M, Hiruma M, Takamori K, Nishimura K. A case of subcutaneous phaeohyphomycotic cyst due to Exophiala jeanselmei complicated with systemic lupus erythematous. Mycoses. 2003;46:145–8. doi: 10.1046/j.1439-0507.2003.00853.x. [DOI] [PubMed] [Google Scholar]


