Abstract
Case series
Patient: Male, 77 • Male, 57 • Male, 73
Final Diagnosis: Coronary chronic total occlusion
Symptoms: Angina pectoris
Medication: —
Clinical Procedure: Percutaneous coronary intervention of coronary chronic total occlusions
Specialty: Cardiology
Objective:
Unusual setting of medical care
Background:
During antegrade dissection re-entry (ADR) of chronic total occlusions (CTO), the first-generation Stingray catheter requires the use of large-bore guides (sheathless 7.5 Fr or 8 Fr), which increases the risk for access site-related complications and compromises radial approaches. Smaller guiding sizes necessitate long guidewires (e.g., 300 cm) or guidewire extensions for catheter advancement or removal. However, friction between guides and the Stingray catheter can result in unstable guidewire position or unintentional removal. Furthermore, failure to deliver the catheter at the distal re-entry zone is a common problem. To overcome issues of deliverability and reduce the need for pre-dilatations, with its inherent risk of creating subintimal hematomas, the Stingray low-profile (LP) balloon catheter was developed.
Case Report:
We describe 3 cases of successful application of the novel Stingray LP catheter during ADR. In all cases, 7 Fr guiding catheters were successfully used in combination with the device. The lower profile facilitated a good exchange and delivery of the device, without the need for balloon pre-dilatations in 2 cases. This resulted in a limited subintimal plane, enabling a smooth puncture into the true lumen. One case presented with extreme levels of calcification and tortuosity, resulting in a high degree of friction, despite the lower catheter profile. No in-hospital coronary or access site-related complications occurred.
Conclusions:
This case report illustrates the feasibility of the Stingray LP catheter for the treatment of CTOs via the ADR technique. The lower profile of the catheter potentially increases the deliverability, safety, and exchangeability of the device.
MeSH Keywords: Atherosclerosis, Coronary Artery Disease, Coronary Occlusion, Percutaneous Coronary Intervention
Background
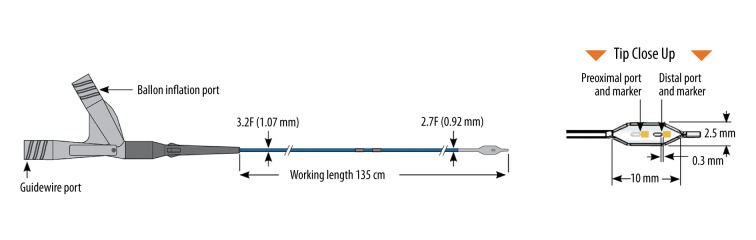
Antegrade dissection and re-entry (ADR) is a commonly applied technique for the percutaneous coronary intervention (PCI) of coronary chronic total occlusions (CTO) [1–4]. In the majority of cases, re-entry into the distal true lumen is accomplished via use of the Stingray catheter and guidewire (Boston Scientific), after either the CrossBoss catheter (Boston Scientific) or a knuckled guidewire (although less preferred, as it is less controllable and might result in an overly large subintimal space) has successfully traversed the subintimal space up to the distal re-entry zone. The Stingray catheter is a self-orienting, flat, small balloon, which has a ‘wing-like’ structure in order to accommodate to the vessel wall architecture upon inflation within the subintimal space. The catheter has 2 contralateral exit ports, which are used to puncture towards the true lumen, and 1 straight exit port. The balloon shaft is coated with a hydrophilic coating to facilitate smooth device delivery (Figure 1) [1,5–7].
Figure 1.
Construction of the Stingray low-profile balloon catheter. No alterations were made to the original Stingray balloon design (Image provided courtesy of Boston Scientific. © 2016 Boston Scientific Corporation or its affiliates. All rights reserved).
Performing ADR during CTO-PCI requires an 8Fr guiding catheter to allow for trapping of a 190-cm-long intracoronary guide-wire (with a regular 2.5–3.0 mm balloon) at the moment of advancement or removal of the first-generation Stingray catheter. The use of smaller guides (6 or 7 Fr radial or femoral approaches) obliges the operator to use 300-cm guidewires or guidewire extensions to advance or remove the Stingray catheter. However, friction between the guides and the Stingray catheter might result in unintentional guidewire removal or unstable intracoronary guidewire position, the latter being key during a controlled re-entry procedure. In addition, ADR performed via radial access requires the use of sheathless 7.5 Fr guides or customized devices.
Thus, downsizing would also help in femoral operations (avoiding large-bore 8 Fr sheaths) with its inherent increased bleeding risk, as well for radial operations, allowing for a conventional 7 Fr radial procedure. Furthermore, reduced friction between gears will result in a more stable guidewire position. Moreover, upscaling from 7 to 8 Fr is not needed when an operator wants to switch from one strategy to another (e.g., antegrade wiring to ADR). Finally, failure to successfully deliver the Stingray catheter also remains a problem when applying the ADR technique. Several angiographic characteristics, such as a high plaque load, heavy calcification, and proximal or lesion tortuosity, can restrict the deliverability of the device.
The new 7 Fr guiding catheter-compatible Low Profile (LP) Stingray catheter was developed to improve the deliverability of the Stingray catheter, guiding catheter compatibility, and reduce the overall risk for access site-related bleeding because of large-bore guiding catheter diameters. Compared to the original Stingray, both the proximal and distal outer shaft diameters have been reduced from 3.7 Fr (0.048”) to 3.2 Fr (0.042”) and 2.9 Fr (0.038”) to 2.7 Fr (0.036”), respectively. In addition, the inner shaft diameter was changed from 0.018” to 0.017” in the new LP version. The SurModics hydrophilic coating was replaced by a Boston Scientific Z-Glide hydrophilic coating on the distal 9.8” (25 cm) and silicon coating on the balloon. No changes were made in the balloon design (Figure 1). We report our initial experience with the new Stingray LP catheter.
Case Report
Case #1
A 77-year-old man with known hypertension, hypercholesterolemia, and peripheral vascular disease presented with Canadian Cardiovascular Society (CCS) class II angina despite maximal medical therapy. Diagnostic angiography demonstrated mild inferior and anterolateral hypokinesia and a CTO of the proximal circumflex (CX) artery, with retrograde collateralization from the right coronary artery (RCA). The proximal CTO cap was tapered, and neither visible calcification nor any tortuosity within the CTO body were found (Figure 2A). Proximal to the CTO, a difficult take-off was present due to a 45° bend (Figure 2B).
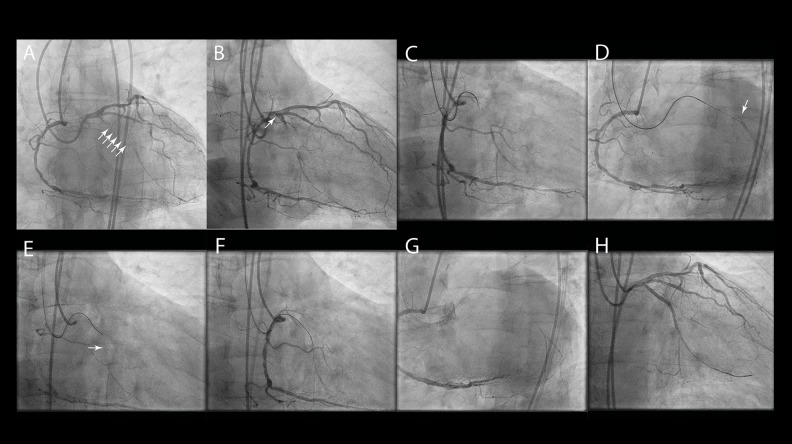
Figure 2.
Case #1. (A) Dual-catheter injection demonstrated a long CTO lesion length (arrows). (B) Difficult take-off due to proximal 45° bend (arrow). (C) Proximal CTO cap was tackled using a Fielder XT-A guidewire and a Corsair microcatheter (Asahi Intecc Co.). (D) Retrograde contrast injection showed the misplaced guidewire. (E) The Stingray LP catheter could be advanced up to the distal target re-entry zone (arrow). (F) Stingray puncture successfully performed using Stingray guidewire. (G) The Stingray guidewire was exchanged for a Pilot 200 (Abbott Vascular) guidewire (‘Stick-and-Swap technique’). (H) The CX was successfully stented.
Bilateral femoral access was obtained with 45-cm-long 7 and 6 Fr sheaths for the RCA and left main coronary arteries, respectively. The RCA was engaged with a Judkins Right guide, and the left main using an AL2 guide. Simultaneous catheter injection showed a long CTO (28 mm) (Figure 2A), resulting in a Japanese CTO (J-CTO) score of 2 [8]. Based on the hybrid algorithm [7], a primary ADR strategy was appropriate. With the help of a Corsair microcatheter (Asahi Intecc), a knuckled Fielder XT-A wire (Asahi Intecc) was used to tackle the CTO (Figure 2C). However, retrograde injection showed an inaccurate guidewire position for ADR (Figure 2D), necessitating redirection of the wire. Although it is advised to switch quickly from the knuckle to the CrossBoss catheter after dissection, the knuckle size was limited and controllable, allowing us to reach the distal CTO cap easily without use of the CrossBoss device. The Stingray LP could be advanced easily in the subintimal lumen up to the distal target re-entry zone, without the need for balloon dilatations (Figure 2E). The Stingray guidewire was used to puncture towards the distal true lumen, after which we switched to a Pilot 200 wire (Abbott Vascular), which was advanced as distally as possible (Figure 2F, 2G). Subsequently, the Stingray LP was smoothly removed using a 2.5×15 mm Emerge trapping balloon (Boston Scientific), which was inflated up to 16 atm. The procedure was finished after predilating and stenting the CTO lesion with an Emerge 2.0×12 mm balloon (12 atm) (Boston Scientific) and 2 drug-eluting stents (2.5×30 mm Orsiro (Biotronik) and 2.25×20 mm Cre8 (Alvimedica). No complications occurred during the patient’s hospital stay, and follow-up revealed complete resolution of angina (Figure 2H).
Case #2
A 57-year-old man, known to have hypertension, hypercholesterolemia, obesity, familial hereditary, chronic kidney disease, peripheral vascular disease, and previous coronary artery bypass graft surgery, presented with CCS class II angina. Diagnostic angiography showed total occlusion of the native circulation, with CTOs in the proximal left anterior descending artery (LAD), proximal CX and proximal RCA, and occluded saphenous vein grafts on both the right posterior descen-dens and first marginal branch, but a patent left mammary graft on the LAD (Figure 3A). Severe hypokinesia of the postero-basal segment was noted. The patient was referred for CTO-PCI of the CX after demonstration of viability in the lateral wall (magnetic resonance imaging). Contrast injection demonstrated a high burden of calcification, a tapered stump, a long lesion length, and proximal tortuosity, corresponding to a J-CTO score of 3 (Figure 3A). As there were no appropriate interventional collaterals or proximal cap ambiguity, a primary ADR strategy was preferred according to the hybrid algorithm.
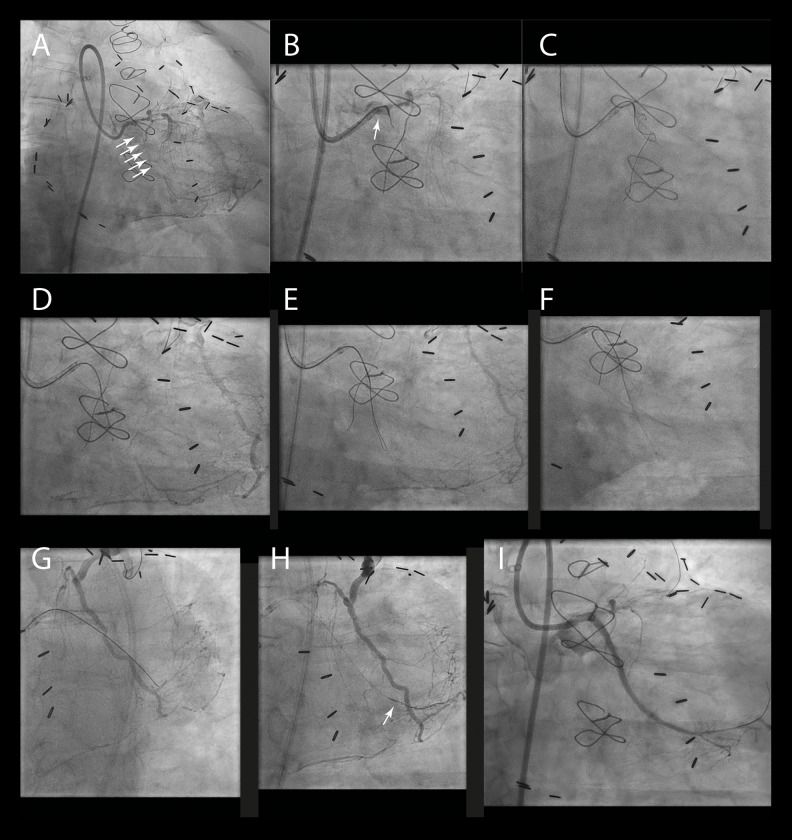
Figure 3.
Case #2. (A) Contrast injection of the left main and the patent LAD graft showed a long, heavily calcified CTO lesion of the proximal CX, with a tapered proximal cap and a steep 90° bend proximal to the CTO lesion (arrows). (B) Puncture of the proximal CTO cap was performed using a balloon-trapped Corsair (Asahi Intecc Co.) microcatheter (arrow). (C) A controlled dissection was created by knuckling of the Fielder XT-A guidewire (Asahi Intecc Co.). (D) The CrossBoss catheter could not advance at the height of the CTO body due to heavy calcification. (E) The Fielder XT-A guidewire was knuckled further down to overcome the calcification. (F) To limit the size of the distal target zone, the CrossBoss catheter was used to cross the last part. (G) Multiple balloon inflations were required to overcome the friction, needed to successfully deliver the Stingray LP catheter. (H) Successful ‘stick-and-swap’ re-entry was performed using the Stingray and Pilot 200 (Abbott Vascular) guidewires (arrow). (I) The native CX was stented without any complications.
Bifemoral access was used, with 45-cm-long 6 and 7 Fr sheaths. A 6 Fr IMA and a 7 Fr XB3.75 guide was used to engage the left mammary graft and left main, respectively. Due to the extreme level of proximal cap calcification and steep proximal angulation, proximal cap preparation was needed using a balloon-trapped microcatheter (Figure 3B). Subsequently, knuckling of a Fielder XT-A guidewire resulted in a controlled dissection (Figure 3C). Then, the CrossBoss catheter was used to further advance down the CTO body. Unfortunately, the CrossBoss stalled in the CTO body (Figure 3D). In order to progress with the CrossBoss catheter, the Fielder wire was knuckled ahead of the CrossBoss (Figure 3E). To minimize the subintimal space at the distal re-entry site, the last part was tackled with the CrossBoss alone (Figure 3F). Prior to Stingray LP delivery, pre-dilatation was needed with a 2.5×15 mm Emerge balloon, due to the high degree of calcification in the CTO body. Next, the Stingray LP catheter was delivered, albeit with a high degree of friction (Figure 3G). Afterwards, the true lumen was re-entered using the Stingray guidewire, after which we switched to the Pilot 200 wire (Figure 3H). After lesion predilatation, 2 Synergy II (Boston Scientific) stents (maximum diameter and total length of 3.5 mm and 56 mm, respectively) were implanted. The native CX blood flow was restored and complete resolution of angina was achieved, without any complications (Figure 3I).
Case #3
A 73-year-old man without relevant medical history presented himself with silent ischemia on cycloergometry. Coronarography showed two-vessel disease, with a significant 60% stenotic lesion of the proximal LAD and a mid-RCA CTO, with good retrograde collateral flow from LAD septal perforators (Figure 4A). Left ventriculography demonstrated mild hypokinesia of the postero-basal segment and a left ventricular ejection fraction of 70%. A percutaneous revascularization strategy was favored over surgical intervention, given a Syntax score of 14 and the personal preference of the patient. CTO lesion analysis showed the presence of a blunt proximal cap, calcification, and a long lesion length, but no tortuosity or proximal cap ambiguity (Figure 4A). A previous antegrade wiring attempt performed by a non-CTO operator failed. Thus, the J-CTO lesion complexity score was 4.
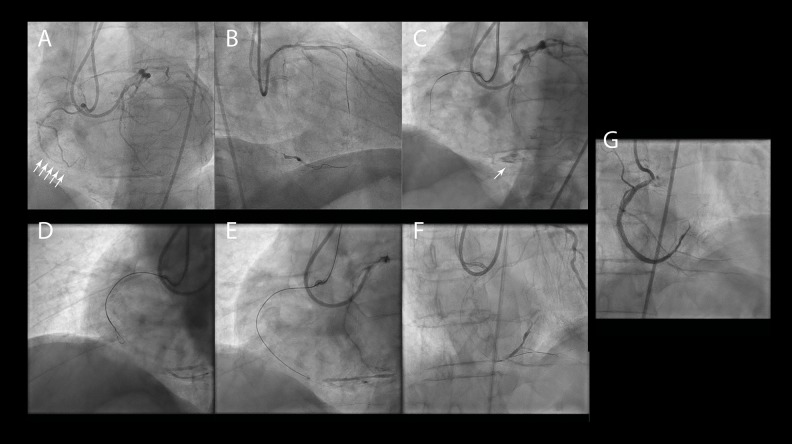
Figure 4.
Case #3. (A) Dual injection demonstrated a long, calcified CTO lesion in the mid-RCA, with a blunt proximal cap and collaterals from the LAD (arrows). (B) An initial retrograde wiring attempt failed despite the use of multiple guidewires in combination with the Corsair microcatheter (Asahi Intecc Co.). (C) Retrograde contrast injection showed a distal contained perforation without clinical consequences (arrow). A switch to an ADR strategy was made. (D) Knuckled Pilot 200 guidewire to advance further down the subintimal space. (E) The CrossBoss followed up to the distal target zone. (F) Stingray re-entry was performed using the Stingray LP catheter and guidewire. (G) The RCA was successfully stented after lesion pre-dilatations.
For this second attempt, a primary retrograde wiring strategy was chosen via the septal collaterals. Access was obtained using a radial, sheathless, 7.5 Fr Asahi guiding and a 7 Fr 45-cm-long femoral sheath. XB4.0 and AL0.75 guides were used to engage the left main and RCA, respectively. Despite multiple guidewires and the use of the Corsair microcatheter, collateral crossing was not possible (Figure 4B). Unfortunately, in the attempt to cross the distal part of the septal collateral, a contained perforation was created, but this did not lead to tamponade or any need for intervention (Figure 4C). A switch to an ADR strategy was then made according to the hybrid algorithm. A Pilot 200 was knuckled and advanced into the subintimal space (Figure 4D), followed by the CrossBoss catheter (Figure 4E). Subsequently, the CrossBoss was exchanged for the Stingray LP using the trapping technique (as before), which could be brought up to the distal crux without the need for any pre-dilatations. Stingray re-entry was performed using the Stingray guidewire and stick-and-swap technique (i.e., Stingray guidewire exchanged for the Pilot 200 wire) (Figure 4F). After lesion predilatation, the blood flow was fully restored without complications by using 3 Cre8 drug-eluting stents (maximum diameter and total length of 3.5 mm and 104, respectively) (Figure 4G). The LAD lesion was treated successfully in a second procedure.
Discussion
The smaller size of the balloon catheter allows for the use of 7 Fr guiding catheters, which decreases the risk for access site-related bleeding complications and provides additional opportunities to work via a radial approach, without the use of 300-cm guidewires or wire extensions. A more stable guide-wire position in the coronary artery promotes a more secure advancement and removal of the Stingray catheter, which is crucial during a re-entry procedure. Although this potential has not yet been studied in a large cohort of patients, our cases illustrate good deliverability of the Stingray LP when used in combination with 7 Fr guiding catheters.
Failure to deliver the Stingray catheter up to the distal re-entry zone remains a problem when applying the ADR technique. The availability of a lower profile Stingray catheter should result in reduced predilatation of the subintimal space, in some cases even without preparation of the subintimal space with CrossBoss.
Our cases demonstrate how the use of the new low-profile Stingray catheter can facilitate CTO-PCI when applying ADR. Although case 2 showed that a high degree of friction was encountered upon bringing the Stingray LP down, this CTO lesion was characterized by an extreme degree of calcification and a steep proximal angle, limiting support and pushability. As illustrated by the other cases, the lower profile of the Stingray LP allowed for a smooth delivery of the device, without the need for balloon pre-dilatations, even in the presence of a difficult take-off, mild calcification, and long lesion lengths. Avoiding the need for predilatation in the subintimal space is safer and limits the size of the subintimal plane, which enhances the odds for a successful puncture. A large subintimal space allows the Stingray catheter to float, even upon inflation, thereby potentially increasing the distance towards the intimal wall and reducing the support and consequently penetration force when performing the puncture. Furthermore, the lower profile allows for smooth exchanges in the 7 Fr guiding catheter when applying the balloon-trapping technique with conventional 190 cm guidewires and no use of guidewires extensions. No switch to 8 Fr guiding catheters was needed.
Conclusions
In summary, this report demonstrates the feasibility of the new Stingray LP catheter in 7 Fr guiding catheters as part of the ADR strategy for CTO-PCI and illustrates the potential benefits of improved deliverability, exchangeability, and safety, as well as providing opportunities to work via radial access.
Abbreviations
- CTO
chronic total occlusion;
- PCI
percutaneous coronary intervention;
- CX
circumflex artery;
- RCA
right coronary artery;
- CCS
Canadian Cardiovascular Society;
- LAD
left anterior descending artery;
- ADR
antegrade dissection and re-entry;
- LP
low-profile.
Footnotes
Statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethics standards.
References:
- 1.Michael TT, Papayannis AC, Banerjee S, Brilakis ES. Subintimal dissection/reentry strategies in coronary chronic total occlusion interventions. Circ Cardiovasc Interv. 2012;5(5):729–38. doi: 10.1161/CIRCINTERVENTIONS.112.969808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whitlow PL, Burke MN, Lombardi WL, et al. Use of a novel crossing and re-entry system in coronary chronic total occlusions that have failed standard crossing techniques: results of the FAST-CTOs (Facilitated Antegrade Steering Technique in Chronic Total Occlusions) trial. JACC Cardiovasc Interv. 2012;5(4):393–401. doi: 10.1016/j.jcin.2012.01.014. [DOI] [PubMed] [Google Scholar]
- 3.Christopoulos G, Karmpaliotis D, Alaswad K, et al. Application and outcomes of a hybrid approach to chronic total occlusion percutaneous coronary intervention in a contemporary multicenter US registry. Int J Cardiol. 2015;198:222–28. doi: 10.1016/j.ijcard.2015.06.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maeremans J, Walsh S, Knaapen P, et al. The hybrid algorithm for treating chronic total occlusions in Europe: The RECHARGE Registry. J Am Coll Cardiol. 2016;68:1958–70. doi: 10.1016/j.jacc.2016.08.034. [DOI] [PubMed] [Google Scholar]
- 5.Werner GS. The BridgePoint devices to facilitate recanalization of chronic total coronary occlusions through controlled subintimal reentry. Expert Rev Med Devices. 2011;8:23–29. doi: 10.1586/erd.10.76. [DOI] [PubMed] [Google Scholar]
- 6.Werner GS, Schofer J, Sievert H, et al. Multicentre experience with the BridgePoint devices to facilitate recanalisation of chronic total coronary occlusions through controlled subintimal re-entry. EuroIntervention. 2011;7:192–200. doi: 10.4244/EIJV7I2A33. [DOI] [PubMed] [Google Scholar]
- 7.Brilakis ES, Grantham JA, Rinfret S, et al. A percutaneous treatment algorithm for crossing coronary chronic total occlusions. JACC Cardiovasc Interv. 2012;5(4):367–79. doi: 10.1016/j.jcin.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 8.Morino Y, Abe M, Morimoto T, et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. 2011;4(2):213–21. doi: 10.1016/j.jcin.2010.09.024. [DOI] [PubMed] [Google Scholar]