Abstract
Hepatobiliary and pancreatic (HBP) cancers are associated with high cancer-related death rates. Surgery aiming for complete tumor resection (R0) remains the cornerstone of the treatment for HBP cancers. The current progress in the adjuvant treatment is quite slow, with gemcitabine chemotherapy available only for pancreatic ductal adenocarcinoma (PDA). In the advanced and metastatic setting, only two targeted drugs have been approved by the Food & Drug Administration (FDA), which are sorafenib for hepatocellular carcinoma and erlotinib for PDA. It is a pity that multiple Phase III randomized control trials testing the efficacy of targeted agents have negative results. Failure in the development of effective drugs probably reflects the poor understanding of genome-wide alterations and molecular mechanisms orchestrating therapeutic resistance and recurrence. In the post-ENCODE (Encyclopedia of DNA Elements) era, cancer is referred to as a highly heterogeneous and systemic disease of the genome. The unprecedented potential of next-generation sequencing (NGS) technologies to accurately identify genetic and genomic variations has attracted major research and clinical interest. The applications of NGS include targeted NGS with potential clinical implications, while whole-exome and whole-genome sequencing focus on the discovery of both novel cancer driver genes and therapeutic targets. These advances dictate new designs for clinical trials to validate biomarkers and drugs. This review discusses the findings of available NGS studies on HBP cancers and the limitations of genome sequencing analysis to translate genome-based biomarkers and drugs into patient care in the clinic.
Keywords: next-generation sequencing (NGS), clinical implications, hepatobiliary and pancreatic (HBP) cancers
1. Introduction
The integration of next-generation sequencing (NGS) technologies [1] and systems biology methods into the ENCODE project (Encyclopedia of DNA Elements) [2,3] has revolutionized biomedical research. New knowledge on non-coding genome functionality and genome-wide sequence variation have changed researchers’ thinking in the way health and disease are affected. A tremendous patient-centric research has began to transform medicine from an inexact science into precision medicine [4]. Genome-based directions in cancer research are urgently needed [5], as survival remains poor [6,7] either for the more advanced stages of major cancer types or even in some early and localized aggressive cancers.
Hepatobiliary and pancreatic (HBP) adenocarcinomas are considered to be among the most aggressive cancer types, as reflected by the clinical evidence of dismal prognosis [6,7]. High expectations for overcoming substantial therapeutic resistance, recurrence and cancer-related deaths rise from NGS applications. Accuracy, dropping costs, and speed have led to an explosion of NGS use in biomedical research over the past decade [8]. Accumulating evidence from early NGS studies provides promising results for identifying extensive genetic and genomic heterogeneity [9,10], which in turn suggests the need for the development of genome-based robust biomarkers and effective targeted drugs to improve personalized cancer medicine. However, multiple challenges have emerged, including the questionable validity of bioinformatics and the large sample sizes required to achieve statistical significance in the discovery of both novel cancer driver genes and therapeutic targets.
This review discusses the advances of modern surgery and oncology and, at the same time, describes the hurdles in improving oncological outcomes of HBP cancers. These tumors have been very difficult to effectively treat and are associated with high therapeutic resistance and relapse rates. Furthermore, we elaborate on the potential and limitations of NGS analysis to develop a biomarker-based patient selection system for more effective therapies, either with available targeted drugs or by discovering new agents targeting novel druggable mutations.
A search of the published literature was conducted in the PubMed database, using the following algorithm: (targeted OR tNGS OR whole-exome OR WES OR whole-genome OR WGS) AND next-generation sequencing AND (hepatocellular carcinoma OR hepatocellular cancer OR liver cancer OR cholangiocarcinoma OR bile duct cancer OR gallbladder cancer OR pancreatic cancer OR pancreatic adenocarcinoma).
2. Clinical Standards
The main cancer types comprising the HBP cancer group are the hepatocellular carcinoma (HCC), the intrahepatic and extrahepatic bile duct cholangiocarcinoma (ICC and ECC), gallbladder cancer (GBC), and the pancreatic ductal adenocarcinoma (PDA). Although incidence rates are relatively low for HBP cancers, mortality rates are very high, indicating the aggressiveness of these tumors. More specifically, primary liver cancers stand for 39,230 and 782,451 cancer cases annually in the US and worldwide, respectively, while they are responsible for 27,170 and 745,533 deaths in those areas. Similarly, 53,070 and 337,872 patients are diagnosed with pancreatic cancer each year in the US and globally, while 41,780 and 330,391 people die, respectively [6,7,11].
Sadly, screening is available only for patients at high risk for HCC. This group includes patients with hepatic cirrhosis, mainly due to hepatitis B or C, alcoholic and non-alcoholic fatty liver disease (NAFLD), as well as hepatitis B carriers, even without cirrhosis. The screening process includes the use of ultrasonography every six months. The combination with Alpha-fetoprotein (AFP) is not recommended, as the 6%–8% gain in the detection rate does not counterbalance the increase in false positive results, ultimately leading to an approximately 80% increase in the cost of each small HCC diagnosed (EASL–EORTC clinical practice guidelines 2012) [12].
Advances in cancer imaging have led to more accurate diagnosis of HBP cancers so that, unlike many other cancers, imaging remains the primary method for diagnosing and staging HBP cancers, and resection of those tumors usually does not require a biopsy. For example, diagnosis of PDA requires the use of Multi-Detector Computed Tomography (MDCT) angiography and the acquisition of thin, axial sections using a dual-phase pancreatic protocol [13]. The diagnosis of HCC requires the employment of a triple-phase CT (or MRI—Magnetic Resonance Imaging) scan with intravenous contrast and the presence of the radiological hallmark for HCC, i.e., contrast uptake in the arterial phase and washout in the venous/late phase. Non-invasive diagnosis is established by one imaging technique in nodules above 2 cm, showing the HCC radiological hallmark and two coincidental techniques with nodules of 1–2 cm in diameter in suboptimal settings (CT, MRI) [12,14]. The only indications for conducting a pre-surgery biopsy are for hepatic tumors that fail to produce the radiological hallmark of HCC (core biopsy is preferred over FNA—fine-needle aspiration), and always before starting a chemotherapy regimen. This last category includes borderline pancreatic adenocarcinomas that require neo-adjuvant treatment, and unresectable and metastatic tumors. Finally, diagnosis of biliary tract tumors is similarly based on imaging and, sometimes, on biopsy performed during the investigation of a hepatic mass.
Pre-surgery staging of HBP cancers aims at defining the resectability of the tumor and is based upon history and physical examination along with a number of imaging and laboratory studies, dependable on the specific type of cancer. For instance, the staging process of PDA additionally employs the use of chest imaging (CT preferred over X-rays), endoscopic ultrasound (EUS), MRI/magnetic resonance cholangiopancreatography (MRCP)/endoscopic retrograde cholangiopancreatography (ERCP), and liver function tests. FNA cytology during the EUS is performed when clinically indicated [15,16,17,18]. Staging of HCC consists of a hepatitis panel, serum levels of bilirubin, transaminases, alkaline phosphatase, albumin, creatinine and AFP, calculation of blood urea nitrogen (BUN) and international normalized ratio (INR), a complete blood count, a chest CT, and a bone scan if clinically indicated [19,20,21]. Moreover, preoperative volumetric assessment of total liver volume (TLV) and functional liver remnant (FLR) is mandatory in order to assess the minimum FLR (40% in chronic liver disease) that can sustain proper liver function. In addition, many centers, mainly in Asia, use the percentage of Indocyanine Green Clearance in 15 min (ICGR15, %) which is a very good marker of hepatic functional reserve and provides more information versus estimation of FLR alone [22]. Staging of biliary tract tumors includes CT or MRI scans with intravenous contrast, a chest CT, liver function tests, serum carcinoembryonic antigen (CEA), cancer antigen 19–9 (CA 19–9), and AFP levels, a hepatitis panel, biopsy and esophagogastroduodenoscopy, and colonoscopy, in the case of ICC. All decisions about resectability should be discussed at multidisciplinary oncologic meetings [23,24].
Complete surgical resection (R0, AJCC/UICC) [25,26], when feasible, remains the only potentially curative option for treating HBP cancers. Thus, the primary treatment option for resectable HCC tumors is the partial hepatectomy [27,28]. Furthermore, patients meeting the United Network for Organ Sharing (UNOS) [29] criteria can undergo a liver transplantation, addressing both the issues of HCC and possible underlying chronic liver disease. For GBC, a cholesystectomy must be followed by en bloc hepatectomy (removal of segments IVb and V) and regional lymphadenectomy with or without bile duct excision, except for T1a tumors incidentally found on pathologic review after cholesystectomy, for which observation is advised [30]. Lymph node excision is also advised after resection of ICC for accurate post-operative staging [31]. Lastly, the type of surgical procedure executed for resectable pancreatic tumors depends on the location and tumor-node-metastasis (TNM) status of the PDA. The procedures include the pancreatoduodenectomy (Whipple procedure) and the distal pancreatectomy with splenectomy, often en bloc [23,24,32].
2.1. Modern Adjuvant and Neoadjuvant Treatment
In contrast to the majority of cancers adjuvant therapy of any kind is not advised in the case of HCC [24,33,34,35]. Adjuvant treatment of GBC includes fluoropyrimidine chemoradiation (except T1a or T1b, N0) and fluoropyrimidine- or gemcitabine-based chemotherapy, although observation is not ill-advised [36,37]. Adjuvant therapy for ICC depends on the post-resection status, as to the presence of residual disease. After R0 resection, fluoropyrimidine- or gemcitabine-based chemotherapy is advised equally to simple observation or participation in a clinical trial. R1 resection or regional node involvement requires chemotherapy (fluoropyrimidine- or gemcitabine-based) or fluoropyrimidine chemoradiation. Lastly, R2 resection calls for one of the following: combination therapy with gemcitabine and cisplatin, a chemotherapy regimen as above, participation in a clinical trial, or locoregional therapy, always with the best possible supportive care [36,37,38,39]. In ECC patients, adjuvant treatment again is based on the post-resection status. For R0 resections with negative regional nodes or for in situ carcinomas, the patient can simply be observed or undergo an adjuvant treatment regimen among fluoropyrimidine chemoradiation, fluoropyrimidine- or gemcitabine-based chemotherapy or participate in a clinical trial. After R1 or R2 resection, it is advised that patients further be subjected to chemoradiation followed by chemotherapy. As for regional lymph node involvement, adjuvant treatment consists of chemotherapy alone [36,37,38].
PDAs are staged preoperatively as resectable, borderline resectable and unresectable, based on tumor contact with specific blood vessels [13]. Borderline resectable PDA is the only HBP cancer for which neo-adjuvant systemic treatment is advised, followed by imaging studies to assess respectability. Acceptable neoadjuvant regimens include FOLFIRINOX, gemcitabine plus albumin bound paclitaxel, and chemoradiation (fluoropyrimidine- or gemcitabine-based), alone or after chemotherapy [40,41,42,43,44]. Adjuvant treatment depends on whether the patient received neoadjuvant therapy or not. In the latter case, recommendations regarding adjuvant treatment include participation in a clinical trial, chemoradiation (fluoropyrimidine- or gemcitabine-based) preceded and followed by chemotherapy (gemcitabine or 5-FU/leucovorin or continuous infusion of 5-FU), or chemotherapy alone [45,46,47,48]. On the other hand, patients who received prior neoadjuvant treatment are advised to consider additional chemotherapy. In general, due to the lack of large scale randomized controlled trials (RCTs) about adjuvant and neoadjuvant treatment options against HBP cancers, patients are encouraged to participate in clinical trials [23,24].
Treatment of unresectable and metastatic HBP carcinomas is mainly based on systemic chemotherapy. In HCC, treatment options for intrahepatic unresectable disease include locoregional therapy (trans-arterial chemoembolization), systemic targeted therapy with sorafenib in advanced HCCs with macrovascular invasion, or some other chemotherapy regimen. Metastatic HCCs are also treated with sorafenib [49,50,51,52]. Sorafenib is an inhibitor of several tyrosine protein kinases, such as vascular endothelial growth factor receptors (VEGFR), platelet-derived growth factor receptor (PDGFR), and Raf family kinases (more avidly C-Raf than BRAF) [53,54]. It is indicated for the treatment of advanced renal cell carcinoma, advanced hepatocellular carcinoma, and radioactive iodine-resistant advanced thyroid carcinoma, without biomarker-based patient selection [51,54,55,56]. It is currently the first of only two targeted drugs used against HBP cancers, the other being erlotinib. Treatment for unresectable and metastatic biliary tract cancers consists of combination therapy with gemcitabine and cisplatin, or another chemotherapy regimen based on gemcitabine or fluoropyrimidine. Unresectable, non-metastatic bile duct tumors can also be treated with fluoropyrimidine chemoradiation [37,38,39].
Management of unresectable and metastatic PDAs depends upon the patient performance status (PS). If PS is good, therapeutic options include the FOLFIRINOX regimen, gemcitabine alone, combined with albumin-bound paclitaxel or with erlotinib, or another gemcitabine-based combination therapy. In the case that PS is poor, there is only the option of gemcitabine monotherapy and palliative care. Erlotinib hydrochloride is a drug approved for the treatment of non-small cell lung cancer (NSCLC) and advanced pancreatic cancer. It is a tyrosine kinase inhibitor, which acts on the epidermal growth factor receptor (EGFR) and is the second targeted therapy against HBP cancers, along with sorafenib. Patients with locally advanced, unresectable tumors can also be treated with chemoradiation (fluoropyrimidine- or gemcitabine-based), preferably after a course of chemotherapy [40,41,57,58,59,60,61]. All patients with unresectable and metastatic HBP cancers must be provided with the best possible supportive care and are encouraged to participate in clinical trials [23,24].
2.2. Limitations of Current Therapeutic Interventions
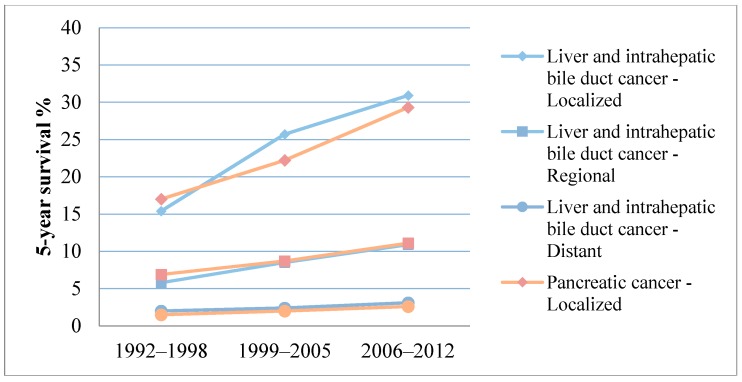
Despite all this progress in the diagnosis and treatment of HBP cancers, 5-year survival rates (5-YSR) remain disappointing, even for early, localized tumors, as we can see in Table 1 [7,62]. Even though some improvement can be seen over the past two decades, particularly for early stage tumors, all stages of HBP cancer still feature very poor survival (Figure 1) [7,63,64]. For instance, combined 5-YSR for localized liver, intrahepatic bile duct, and pancreatic cancer is about 30%, which is minimal when compared to 5-YSR of over 90% for localized breast and colorectal cancer [6,7]. Nevertheless, specialized, high-volume HBP centers have recently reported improved 5-YSR of 45%–56% for HCC [22,65]. These numbers can be explained by the very high rates of tumor recurrence after complete resection that range from 54% for HCC [65] to 81% for PDA [48]. Because the majority of recurrences after hepatic resection (66%) [65] are limited to the liver, overall recurrence rates are as low as less than 20% after liver transplantation [66]. Recurrence rates in further detail are demonstrated in Table 2 [48,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80]. HCC incidence can be decreased either by mass vaccination programs against hepatitis B virus or by adequate antiviral treatment.
Table 1.
Five-year survival rates for hepatobiliary and pancreatic (HBP) cancers.
| Cancer Type | Localized | Regional | Distant | Unstaged | Overall |
|---|---|---|---|---|---|
| Liver and intahepatic bile duct cancer | 30.9% [7] | 10.9% [7] | 3.1% [7] | 6.1% [7] | 17.5% [7] |
| Intrahepatic bile duct cancer | 15% [62] | 6% [62] | 2% [62] | N/A | N/A |
| Extrahepatic bile duct cancer | 30% [62] | 24% [62] | 2% [62] | N/A | N/A |
| Pancreatic cancer | 29.3% [7] | 11.1% [7] | 2.6% [7] | 4.9% [7] | 7.7% [7] |
N/A: Not available.
Figure 1.
Five-year survival rates for hepatobiliary and pancreatic (HBP) cancers by stage from 1992 to 2012 [7,63,64].
Table 2.
Recurrence rates of hepatobiliary and pancreatic (HBP) cancers after surgical resection, in Phase III randomized controlled trials (RCTs) or retrospective studies.
| Type of Cancer | Treatment | Recurrence Rate (%) |
|---|---|---|
| HCC | Hepatectomy | 51% [67]; 54% [65]; 63% [68] |
| HCC | OLT | 7.6% [69]; 15.3% [66]; 18.3% [70] |
| PDA | Pancreatectomy and adjuvant chemotherapy | 75%–85% [71]; 81%–93% (Phase III RCT) [48] |
| ICC | Resection | 62.2% [72]; 70% [73] |
| Mixed HCC-CC/ICC Hilar/ICC | OLT | 60% [74]; 38% [75] |
| ECC | ||
| Distal | Resection | 39% [76] |
| Hilar | Resection, OLT | 53% [77]; 68% [78]; After OLT: 20% [79] |
| GBC | Resection, resection and adjuvant chemotherapy | 66% [78]; 81.4% [80] |
HCC: hepatocellular carcinoma; OLT: orthotopic liver tranplantation; PDA: pancreatic ductal adenocarcinoma; ICC: intrahepatic bile duct cholangiocarcinoma; HCC-CC: hepatocellular cholangiocarcinoma; ECC: extrahepatic bile duct cholangiocarcinoma; GBC: gallbladder cancer.
High recurrence and low survival rates have led to a very large number of clinical trials concerning systemic treatment of HBP cancers, and medical interest has focused on the development of new targeted drugs. Targeted therapy is the most recent major modality of treatment for cancer, along with cytotoxic chemotherapy and hormonal therapy. Targeted drugs block tumor growth by interfering with specific molecules vital to carcinogenesis, rather than harming all rapidly dividing cells, thus causing fewer and less intense adverse effects compared to chemotherapy. Sadly, only approximately 20 Phase III randomized controlled trials (RCTs) on targeted drugs against HBP cancers have reached completion. Until now nearly all completed Phase III RCTs for HBP tumors feature negative or not statistically significant results, as we can see in Table 3 and Table 4 [81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99]. By contrast, two studies have reported promising results. The RESORCE trial, which examines regorafenib as a second line treatment after sorafenib, has featured a significantly increased overall survival of 10.6 months versus 7.8 months for the placebo (hazard ratio—HR = 0.62 [95% confidence interval—CI, 0.50–0.78]; p < 0.001) on the preliminary report [100]. A second and most impressive example is a study by Lee JH et al. that evaluates the efficacy of autologous cytokine-induced killer cells in the adjuvant setting after a complete resection of HCC, that featured a significant overall survival benefit (HR = 0.21 [95% CI, 0.06–0.75]; p = 0.008), although it has not yet achieved FDA approval and has not been included in current guidelines [23,24,89].
Table 3.
Completed Phase III RCTs on targeted drugs for hepatocellular and bile duct cancers.
| N | Setting | Intervention | Results | Reference/Clinicaltrials.gov Identifier |
|---|---|---|---|---|
| 1114 | Adjuvant HCC | Sorafenib vs. Placebo | RFS HR = 0.940; [95% CI, 0.780–1134]; one-sided p = 0.26 | STORM trial [81] |
| 1075 | Advanced HCC First-line | Sunitinib vs. Sorafenib | Terminated based on a higher incidence of serious adverse events in the sunitinib and on failure to demonstrate superiority or non-inferiority to sorafenib | NCT00699374 |
| 1035 | Advanced HCC First-line | Linifanib vs. Sorafenib | OS HR = 1.046; [95% CI, 0.896–1.221] | [82] |
| 870 | Intermediate Unresectable HCC | Brivanib vs. Placebo after TACE | HR = 0.90 [95% CI, 0.66–1.23]; log-rank p = 0.5280 | [83] |
| 720 | Advanced HCC First-line | Sorafenib + Erlotinib vs. Sorafenib + Placebo | OS 9.5 vs. 8.5 months, HR = 0.929; p = 0.408 | SEARCH trial [84] |
| 635 | Advanced HCC Second-line | ADI-PEG 20 vs. Placebo | OS 7.8 vs. 7.4 months; HR = 1.022 [95% CI, 0.847–1.233]; p = 0.884 PFS 2.6 vs. 2.6 months; HR = 1.175 [95% CI, 0.964–1.432]; p = 0.075 |
[85] |
| 565 | Advanced HCC Second-line | Ramucirumab vs. Placebo after Sorafenib | 9.2 vs. 7.6 months; HR = 0.87 [95% CI, 0.72–1.05]; p = 0.14 HR = 0.674; p = 0.0059 with baseline AFP ≥ 400 ng/mL |
REACH trial [86] |
| 420 | Advanced HCC | Tamoxifen + SOC vs. SOC alone | OS 4.8 [95% CI, 3.6–6] vs. 4.0 months [95% CI, 3.5–4.5] | [87] |
| 395 | Advanced HCC Second-line | Brivanib vs. Placebo | OS 9.4 vs. 8.2 months; HR = 0.89 [95.8% CI, 0.69–1.15]; p = 0.3307 | BRISK PS trial [88] |
| 230 | Adjuvant HCC | CIK vs. Placebo | RFS 44.0 vs. 30.0 months; HR = 0.63; [95% CI, 0.43–0.94]; p = 0.010 OS HR = 0.21 [95% CI, 0.06–0.75]; p = 0.008 |
[89] |
| 124 * | Advanced BDC | Cis/Gem + Cediranib vs. Cis/Gem + Placebo | PFS HR = 0.93 [95% CI, 0.65–1.35]; p = 0.72 | ABC-03 trial [90] |
Bile duct cancer (BDC); hazard ratio (HR); hepatocellular carcinoma (HCC); overall survival (OS); progression-free survival (PFS); recurrence-free survival (RFS); standard of care (SOC); trans-arterial chemoembolization (TACE); * Phase 2/3 RCT.
Table 4.
Completed Phase III RCTs on targeted drugs for pancreatic ductal adenocarcinoma.
| N | Setting | Intervention | Results | Reference |
|---|---|---|---|---|
| 1062 | Advanced PDA First-line | Arm I: Chemotherapy alone Arm II: Chemotherapy with sequential GV1001 (telomerase peptide vaccine) Arm III: Chemotherapy with concurrent GV1001 |
Sequential chemoimmunotherapy group OS HR = 1.19 [98.25% CI, 0.97–1.48]; p = 0.05 Concurrent chemoimmunotherapy group OS HR = 1.05 [98.25% CI, 0.85–1.29]; p = 0.64 |
TeloVac trial [91] |
| 745 | Locally Advanced PDA First-line | Gemcitabine + Cetuximab vs. Gemcitabine alone | OS HR = 1.06 [95% CI, 0.91–1.23]; p = 0.23, one-sided | Southwest Oncology Group-directed intergroup trial S0205 [92] |
| 722 | Adjuvant PDA | Algenpantucel-L (HAPa) Immunotherapy + SOC vs. SOC alone | Study completed No statistically significant difference on preliminary report OS 27.3 vs. 30.4 months |
IMPRESS trial [93] |
| 688 | Advanced PDA First-line | Gemcitabine + Tipifarnib (R115777) vs. Gemcitabine + Placebo | OS HR = 1.03 [95% CI, 0.86–1.23]; stratified log-rank p = 0.75 | [94] |
| 632 | Advanced PDA First-line | Gemcitabine + AG-013736 (Axitinib) vs. Gemcitabine + Placebo | OS HR = 1.014 [95% CI, 0.786–1.309]; p = 0.5436 | [95] |
| 602 | Advanced PDA First-line | Gemcitabine + Bevacizumab vs. Gemcitabine plus Placebo | OS HR = 1.044 [95% CI, 0.88 to 1.24]; p = 0.95 | CALGB 80303 trial [96] |
| 160 * | Metastatic PDA First-line |
Rigosertib (ON 01910.Na) + Gemcitabine vs. Gemcitabine alone | OS HR = 1.24 [95% CI, 0.85–1.81] | [97] |
| 154 | Advanced PDA First-line | G17DT immunogen vs. Placebo | Mortality HR = 0.75 [95% CI, 0.51–1.10]; p = 0.138 | [98] |
| 153 * | Advanced PDA First-line | Elpamotide + Gemcitabine vs. Placebo + Gemcitabine | OS HR = 0.87 [95% CI, 0.486–1.557]; Harrington-Fleming p-value = 0.918; log-rank p-value = 0.897 |
[99] |
Hazard ratio (HR); overall survival (OS); pancreatic ductal adenocarcinoma (PDA); * Phase 2/3 RCT.
2.3. Underway Phase III RCTs
Approximately 20 Phase III RCTs on targeted drugs are underway but only four are using biomarker-based patient selection. The REACH-2 trial investigates the effects of ramucirumab as second line treatment after sorafenib on patients with advanced HCC and elevated baseline AFP ≥ 400 ng/mL, after observing favorable effects of ramucirumab only on patients of this subgroup in the REACH trial, while the overall cohort of the study was negative [86,101]. The METIV-HCC trial uses tivantinib as second line treatment of MET-high, inoperable HCC tumors, after correlation with longer time to progression on a Phase II clinical trial [102,103]. The third trial (NCT02395016) uses nimotumumab in addition to gemcitabine on patients with K-RAS wild-type, advanced PDA. Lastly, the POLO trial examines the effects of olaparib on patients with germline BRCA1/2 mutated PDA, who have shown no progression on first line platinum-based chemotherapy [104].
It becomes obvious that, despite the great interest in targeted therapy on behalf of pharmaceutical companies, most large-scale RCTs with hundreds of patients enrolled end up with negative results. This underlines the urgent need for an early drug development strategy, in order to predict drug efficacy and the capability of FDA approval [105]. The recent evidence on substantial genetic and genomic tumor heterogeneity by NGS has shifted biomedical interest to the research for the development of robust biomarkers and effective targeted drug discovery.
3. NEXT-Generation Sequencing and Tumor Heterogeneity
The advent and rapid progress of NGS technologies over the past decade has revolutionized biomedical research [1]. The unprecedented potential provided by NGS for accurate identification of genomic alterations (GAs) underlying common and rare diseases, has led to a tremendous effort in moving forward from current medicine as an inexact science and building the foundations of genomics-based precision medicine [4,8,106,107].
Particularly in cancer, definitive evidence for extensive genetic tumor heterogeneity [9] and validity of NGS technologies by a recent international consensus panel [108] have resulted in an explosion in NGS use on patient-derived sample analysis. Early after the introduction of NGS, fresh frozen sample collection and storage in biobanks was the standard procedure. However, this approach is time and resource consuming and is limited by the obligatory prospective design of clinical studies and the lack of long-term patient follow-up data. Technical developments have recently allowed the DNA/RNA extraction from formalin-fixed paraffin-embedded (FFPE) for NGS analysis, including targeted next-generation sequencing (tNGS), whole-exome sequencing (WES), and whole-genome sequencing (WGS), with similar accuracy as fresh frozen tissue sample NGS analysis [109,110].
Although clonal evolution and tumor heterogeneity have been proposed by Nowell in 1976 [111], evidence on genetic and genomic variation has emerged in the last two decades [112]. This tumor diversity can be crucial for developing more effective, personalized treatments for HBP cancers, to overcome current substantial therapeutic resistance and high recurrence rates of these tumors. For example, large-scale Phase III RCTs with a recruited population of over 1000 patients, testing the efficacy of targeted drugs (i.e., sorafenib in the adjuvant setting of HCC [81], linifanib as the first line in advanced HCC [82]) were negative. The failure of these studies to meet their endpoints can be explained by the empirical approach without either understanding the molecular landscape underlying therapeutic resistance or using biomarker-based patient selection for recruitment. Recent advances in NGS can overcome these limitations by implementing tNGS, WES, and WGS in new designs of clinical trials.
3.1. Targeted Next-Generation Sequencing
Over the past few years, the ability of NGS application on FFPE samples has led to the routine use of tNGS in public and private laboratories for screening a panel of genes to identify alterations matched to available targeted drugs [113,114]. Apart from decision-making on selecting an agent from the available FDA-approved list, tNGS provides the potential for performing new-design clinical trials, including umbrella and basket studies. For any specific cancer type (i.e., pancreatic cancer), the identification of subgroups of patients with similar druggable GAs could predict the positivity of umbrella clinical trials at an early stage. By contrast, basket design studies are performed to assess the clinical utility of specific targeted drugs on several different cancer types with similar GAs [105], such as transtuzumab for HER2-positive breast and gastric cancer [115]. However, tNGS has limited or no potential to identify novel cancer driver genes and therapeutic targets to overcome drug resistance.
Twenty targeted NGS studies were eligible for inclusion in the present review, studying HCC (Table 5) [116,117,118,119,120,121], biliary tract cancer (BTC) (Table 6) [122,123,124,125,126,127,128,129], and PDA (Table 7) [130,131,132,133,134,135].
Table 5.
Targeted next-generation sequencing studies on hepatocellular carcinoma.
| N | Findings | Clinical Implications | Reference |
|---|---|---|---|
| 9 tNGS; 1 WES | Mutations were observed in TP53 and CTNNB1 genes in 5/9 tumors | Larger studies are required | [116] |
| 12 | TP53 mutations in 5/12 patients, RUNX1 in 3/12 and other less frequent mutations | Larger studies required | [117] |
| 14 (advanced-metastatic) | Mutations identified in several well-known genes and pathways | Larger studies required | [118] |
| 45 patients (pts) treated with sorafenib (tNGS and CN assay; 6 CR, 39 non-CR) |
FGFR mutations in 5/45 FGF19 copy number gain was detected more frequently among CR cases (2/6 vs. 2/39; p = 0.024) |
Larger studies are required to evaluate potential clinical utility of CN gain for FGF19 as a predictive biomarker to sorafenib | [119] |
| 46 pts treated with sorafenib | Average number of detected oncogene mutations differed significantly between the PD and non-PD groups (p = 0.0446) | Targeted sequencing could predict response to sorafenib | [120] |
| 104 | Most frequent mutations: TERT (65%, associated with HCV infection), TP53 (38%, associated with HBV infection), CTNNB1 (30%, associated with absence of HBV infection) |
TERT promoter mutations are related to poor prognosis Results may influence diagnostic and therapeutic strategies |
[121] |
Complete response (CR); copy number (CN); progressive disease (PD); targeted next-generation sequencing (tNGS); whole-exome sequencing (WES).
Table 6.
Targeted next-generation sequencing studies on biliary tract cancers.
| N | Findings | Clinical Implications | Reference |
|---|---|---|---|
| 11 (3 ICC, 8 ECC) | Molecular heterogeneity was identified between ICC and ECC | This molecular classification could potentially provide personalized therapeutic implications | [122] |
| 28 | In 71% of cases, at least one potentially actionable alteration was found in known genes | Identification of these novel gene fusions (FGFR2-KIAA1598, FGFR2-BICC1, FGFR2-TACC3, and RABGAP1L-NTRK1) provides potential for personalized treatment | [123] |
| 40 (15 ECC, 10 ICC, 14 GBC, 1 AVC) | More (TP53) or less (NRAS, KRAS, ERBB215, PIK3CA) frequently mutated genes were identified | This is another study confirming the potential utility for umbrella studies | [124] |
| 41 (Diffusely infiltrating type CCA; 24 ERCP bile samples, 17 tumor samples) | tNGS on bile samples was feasible and comparable to tumor tNGS Diffusely infiltrating type CCA was genetically distinct from mass-forming type CCA |
Encouraging results provide ground for larger studies to evaluate the reliability of TS on bile samples | [125] |
| 41 (32 ICC, 9 GBC, WES in 2) | Comparison of ICC with GBC revealed these two types are genetically distinct | Further investigation of chromatin remodeling could lead to the development of novel therapies | [126] |
| 75 (55 ICC, 20 ECC; 26 surgical resections, 49 biopsies) | Genetic aberrations were significantly different between ICC and ECC | TS could identify mutated genes-based subgroups of patients with potential prognostic and therapeutic relevance | [127] |
| 153 (70 ICC, 57 ECC, 26 GBC) |
IDH1/2 and BAP1 mutations were characteristic of ICC, while KRAS and TP53 were more frequent in ECC and GBC Potentially actionable mutations were identified in 104/153 (68%) |
Clinical utility of molecular classification identified by this study requires evaluation by clinical trials | [128] |
| 554 (412 ICCs, 57 ECCs and 85 GBCs) | Most frequently mutated genes: ICC: TP53, CDKN2A/B, KRAS, ARID1A, IDH1 ECC: KRAS, TP53, CDKN2A/B, SMAD4 GBC: TP53, CDKN2A/B, ARID1A, ERBB2 |
In the ICC group, TP53, KRAS and FGFR2 mutations can be used as prognostic markers Identification of FGFR mutations in ICC patients could predict therapeutic response to FGFR inhibitors (BGJ398, pazopanib, dovitinib, TAS-120) tNGS can be utilized for clinical benefit and for designing umbrella and basket studies |
[129] |
Cholangiocarcinoma (CCA); extrahepatic cholangiocarcinoma (ECC); gallbladder cancer (GBC); intrahepatic cholangiocarcinoma (ICC); whole-exome sequencing (WES); targeted sequencing (TS).
Table 7.
Targeted next-generation sequencing studies on intraductal papillary mucinous neoplasms of the pancreas and pancreatic ductal adenocarcinomas.
| N | Findings | Clinical Implications | Reference |
|---|---|---|---|
| 11 (oncocytic subtype IPMN; 11 TS, 2 WGS) | Typical oncocytic subtype IPMNs did not have KRAS or GNAS mutations and only one had both RNF43 and PIK3R1 mutations; ARHGAP26, ASXL1, EPHA8, and ERBB4 genes were mutated in more than one sample | Larger studies are required to explore the genetic profile and biologic behavior of the oncocytic subtype of IPMN | [130] |
| 23 (IPMN) | Identification of distinct mechanisms for the development of cancer in patients with IPMN using tNGS | Potential stratification and surveillance of patients based on the risk for pancreatic cancer | [131] |
| TS on FNA samples from 29 pts (25 PDA, 4 AVC) | Most frequent mutations identified: KRAS (93%), TP53 (72%), SMAD4 (31%), and GNAS (10%) Feasibility, reliability and concordance of FNA as compared to tumor samples for tNGS analysis |
FNA-based tNGS analysis enables biomarker-based patient selection for clinical trials | [132] |
| 30 (PDA) | Substantial mutational heterogeneity (73%) | tNGS shapes the development of targeted therapy for pancreatic cancer | [133] |
| 52 (48 IPMNs, 4 ITPNs) | GNAS was mutated in 38/48 (79%) IPMNs, KRAS in 24/48 (50%) both in 18/48 (37.5%); Other mutations were less frequent | Identification of mutations in cyst fluid could enhance diagnosis and prognostic stratification of pancreatic cystic neoplasms | [134] |
| 76 (PDA) | 22 candidate cases have been identified (14 KRAS wild-type, 5 HER2 amplifications, 2 mutations in BRCA2 and 1 ATM mutation) | The availability of drugs targeting these mutated or amplified genes (cetuximab, transtuzumab) enables basket design of clinical trials | [135] |
Fine-needle aspiration (FNA); intraductal papillary mucinous neoplasm (IPMN); intraductal tubulopapillary neoplasm (ITPN); pancreatic ductal adenocarcinoma (PDA); patients (pts); targeted sequencing (TS); whole-genome sequencing (WGS).
Genetic heterogeneity between different cancer types was confirmed by the identification of distinct mutations in cancer driver genes, specific to each cancer. In a large study by Kawai-Kitahata et al. [121], the most frequently mutated gene in HCC tumors was TERT in 65% of the cases, and its mutational status was associated with HCV infection. tNGS studies also revealed potential utility in predicting HCC response to sorafenib [119,120]. Moreover, tNGS highlighted the genetic distinction between the different types of BTC [122,126,127,128]. One of the most frequently mutated and promising genes in BTC was ARID1A, mostly altered in ICC and GBC [129]. In addition, in ICC patients, identification of FGFR mutations may be of predictive value as to the therapeutic response to FGFR inhibitors, such as pazopanib and dovitinib [129]. Implementing tNGS in clinical trials for various cancer types could enhance predictive biomarker identification for improving drug efficacy [136]. Notably, a significant portion of BTC patients, ranging from 68% to 71%, carried potentially actionable gene alterations [123,128]. Concerning PDA, substantial mutational heterogeneity was discovered [133] and KRAS was the most commonly mutated gene [132]. A significant number of cases featured potentially targetable genes, such as HER2 amplifications that are targeted by transtuzumab and wild-type KRAS, which could be an indication for administration of cetuximab, as in colorectal cancer [135].
Recent technical developments allowing NGS analysis on small amounts of tissue have enabled targeted sequencing of FNA samples in the diagnostic and neo-adjuvant setting broadening the clinical implications of NGS [137,138,139]. A recent study showed that tNGS could be performed on FNA samples with reliability comparable to that of conventional tumor samples, in order to achieve pre-treatment biomarker-based patient selection for clinical trials [132].
3.2. Whole-Exome and Whole-Genome Sequencing
Following the ENCODE project that explored the functionality of human genome [2], the exome (protein-coding area), accounting for 1.5% of the genome, can accurately be sequenced by WES. The remaining, non-coding genome that accounts for 98.5%, can only be sequenced by WGS.
Particularly in cancer, progress in NGS analysis of clinical samples is much faster for WES studies than for WGS, for which bioinformatics analysis on big data is highly complex and has not yet been standardized [108]. For example, the continuously dropping cost and the potential for identifying novel cancer driver genes has led to the largest WES study available, which has analyzed 4742 humans tumors for point mutations in the exome [9]. On the contrary, the largest WGS study available has analyzed 300 tumors [10]. Despite its complexity and much higher cost, WGS is essential for identifying large structural genome changes, such as copy number alterations (CNAs) and chromosomal rearrangements that have a critical role in cancer diagnosis and therapy. Moreover, based on the functionality of most of the non-coding genome (~80%), another strength of WGS is the ability to identify non-coding sequence variations. When WGS is coupled with RNA-sequencing (RNA-seq) and chromatin immunoprecipitation sequencing (ChIP-Seq), their combination provides the potential for transcriptome analysis and the future development of next-generation drugs that disrupt transcriptional biocircuits [140]. Despite the advances in WGS, many challenges have to be overcome, including high costs and a lack of bioinformatics standardization.
WES studies on HBP cancers, summarized in Table 8 [141,142,143,144,145,146,147,148,149,150,151,152,153,154,155], are consistent with the extensive genetic tumor heterogeneity identified by the largest WES study available on 21 other cancer types by Lawrence et al [9]. Fifteen WES studies were deemed eligible for inclusion in this review. Frequently mutated genes were KRAS in PDAs [146,151], chromatin regulation genes, and especially ARID1A in PDAs and HCCs [142,145,148,150,151,155] and TERT in 68% of HCCs [155]. Many genes and genomic alterations (GAs) with possible diagnostic, prognostic, and therapeutic significance were identified, including ten novel genes [143,149] and a recurrent novel fusion (FGFR2-PPHLN1) in 16% of ICCs [152]. Interestingly, a significant portion of HBP patients approximate a 30% share targetable or potentially targetable mutations in known genes [144,152,154], such as FGFR, which can be targeted by FGFR inhibitors [152] and ARID1A, which will be discussed in further detail below.
Table 8.
Whole-exome sequencing studies on hepatobiliary and pancreatic cancers.
| Cancer Type | N | Findings | Clinical Implications | Reference |
|---|---|---|---|---|
| HB | 6 | 21 mutated genes, including mutations in the WNT pathway | Larger studies are required to explore the mutational background of HB | [141] |
| HCC (HBV positive) | 10 (110 samples, including PVTTs and intrahepatic metastases) |
ARID1A was mutated in 14 of 110 samples (13%) ARID1A loss-of-function mutations may be crucial for HCC invasion and metastasis |
ARID1A is a potential novel biomarker for treatment and prognosis | [142] † |
| NAFLD-related HCC | 10 (11 samples, WES, TS, CNV studies) | 12 genes were frequently mutated including novel genes (FGA, SYNE1) | Larger studies are required to confirm the validity of novel genes | [143] |
| PDA (acinar differentiation) | 23 | Potentially targetable mutations in well-known genes (BRCA2, PALB2, ATM, BAP1, BRAF and JAK1) were identified in 1/3 of patients | This study supports the conduction of umbrella studies | [144] |
| HCC | 24 WES (NGS); 125 CNA in total with CGH array analysis |
New recurrent mutations in ARID1A, RPS6KA3, NFE2L2 and IRF2
Inactivation of chromatin remodelers was frequent and was associated with alcohol Wnt/b-catenin pathway promotes tumorigenesis through both oxidative stress metabolism and MAPK pathways |
Association of environmental risk factors with specific gene mutations could improve screening and early diagnosis | [145] |
| PDA from VLTSs (≥10 years) | 35 (8 WES, 27 TS) | Frequently mutated genes were identified (KRAS, TP53, RNF43, CDKN2A, and SMAD4) Combined WES and TS data showed no significant difference between VLTSs and patients unselected for survival |
Validity of these data must be investigated by larger studies | [146] |
| FLC | 78 (48 WES + TES, 58 whole-transcriptome, 41 SNP arrays) | Identification of 3 molecular classes: proliferation with altered mTOR pathway, inflammation with altered cytokine production genes and unannotated | Larger studies are required to confirm the validity of the developed prognostic 8-gene expression signature (PEAR1, KRTAP, KLRD1, OSBPL8, RPL32, SLC26A11, RGS11 and RAPGEF1) | [147] |
| HCC | 87 | Substantial genetic heterogeneity NFE2L2-KEAP1 and MLL pathways were recurrently mutated |
Further larger WES studies are needed for completing the cancer driver genes catalog and developing individualized therapy | [148] |
| PDA | 99 with early stage (I and II; WES and CNA) | Substantial genetic heterogeneity 8 novel mutated genes: EPC1 and ARID2 (chromatin modification), ATM (DNA damage repair), ZIM2, MAP2K4, NALCN, SLC16A4 and MAGEA6 |
The novel mutated genes identified could potentially be used as therapeutic targets but validation is required by larger studies | [149] |
| PDA | 101 (24 WES and 77 TS) | Mutated chromatin regulating genes MLL, MLL2, MLL3, ARID1A were associated with improved survival Detection of ctDNA was associated with predictable recurrence 6.5 months before occurrence |
These genes may have prognostic significance and ctDNA could potentially be used as a biomarker to predict recurrence | [150] |
| PDA | 109 | Identification of multiple novel mutated genes in PDA, with select genes harboring prognostic significance KRAS mutations were observed in >90% of cases ARID1A was a marker of poorer outcome RBM10 mutation was associated with longer survival BRAF and PIK3CA mutations expand the spectrum of oncogenic drivers |
PDA is a complex cancer and WES can provide insight on pathogenesis, diagnosis and therapeutic management of these tumors | [151] |
| ICC | 135 (7 fresh frozen samples, 107 FFPE, 21 FFPE mixed HCC-ICC; WES in 8, WGS in 1) | Chromosomal translocation t(10;12)(q26;q12) leads to FGFR2–PPHLN1 fusion; it is successfully inhibited by a selective FGFR2 inhibitor in vitro | Novel fusion event (FGFR2–PPHLN1) could provide therapeutic benefit Most CCA patients harbor potentially targetable molecular alterations |
[152] |
| HCC | 231 (WES and CNA) | Mutated RB1 was a predictor of recurrence and poor survival after HCC resection | RB1 mutations could be used as a prognostic molecular biomarker for resectable HCC | [153] |
| HCC | 243 | 28% of the tumors featured genetic alterations targeted by FDA-approved drugs and 3 groups of genes were associated with risk factors: CTNNB1 (alcohol), TP53 (HBV) and AXINI | Association of environmental risk factors with specific genes provides new potential for HCC prevention and early-stage diagnosis | [154] |
| HCC | 503 (452 WES) * | TERT alterations were identified in 68% of the patients AXIN1 was more frequently mutated in HBV-positive and ARID1A in non-virus cases Druggable kinase alterations were rarely found (<2%) |
Mutations in genes coding for metabolic enzymes, chromatin remodelers and mTOR pathway could provide diagnostic and therapeutic potential | [155] ‡ |
Comparative genomic hybridization (CGH); copy-number alteration (CNA); fibrolamellar hepatocellular carcinoma (FLC); formalin-fixed paraffin-embedded (FFPE); hepatoblastoma (HB); hepatocellular carcinoma (HCC); intrahepatic cholangiocarcinoma (ICC); pancreatic ductal adenocarcinoma (PDA); single nucleotide polymorphism (SNP); targeted sequencing (TS); very long-term survivor (VLTS); whole-exome sequencing (WES); * 22 cases of WGS are included in Table 9; † WES analysis was performed on the Illumina Genome Analyzer II platform, which is no longer available for order on the official Illumina website; ‡ WES analysis was performed on the SureSelect Human All Exon V3 or V4 platform from Agilent Technologies.
WGS studies provide powerful potential for the assessment of both the genetic and genomic heterogeneity, including CNAs and chromosomal rearrangements. Ten WGS reports on HBP cancers were included in our review, and their findings are outlined in Table 9 [10,155,156,157,158,159,160,161,162,163,164]. Recurrent mutations were identified in chromatin regulators and particularly ARID1A and ARID2 in HCCs and PDAs [160,163,164] and in the TERT [10,155,160,162] and TERT promoter locus [163] in all kinds of HBP cancers. A number of cancer-related genes were highlighted, including well-known genes, as well as five novel genes [10,164]. Environmental risk factors, and especially viral hepatitis and alcohol, were associated with specific mutated genes in primary liver cancer, shaping potential clinical benefit [10,159,161,163]. Furthermore, one study compared the WGS analyses of two multicentric HCCs and concluded that the nodes originated from distinct, independent mutations [160].
Table 9.
Whole-genome sequencing studies on hepatobiliary and pancreatic cancers.
| Cancer Type | N | Findings | Clinical Implications | Reference |
|---|---|---|---|---|
| PDA | 3 | KRAS signaling pathway was the most heavily impacted pathway | Larger WGS studies are required for assessing clinical utility | [156] |
| HCC with pulmonary metastasis | 4 | Somatic SNVs, SVs and CNAs were similar between primary and metastatic tumors | Larger studies with multiple biopsies are required to investigate similarities and differences between primary and metastatic tumors | [157] |
| FLC | 10 | Few coding, somatic mutations, no recurrent SVs Molecular differentiation from HCC |
This study supports further research on the DNAJB1-PRKACA fusion protein for potential diagnostic and therapeutic clinical implementation | [158] |
| HCC | 22 * |
TERT alterations were identified in 68% of the patients AXIN1 was more frequently mutated in HBV-positive and ARID1A in non-virus cases Druggable kinase alterations were rarely found (<2%) |
Mutations in genes coding for metabolic enzymes, chromatin remodelers and mTOR pathway could provide diagnostic and therapeutic potential | [155] |
| HBV-related HCC | 22 (WGS and RNA seq.) | Mutations, including non-coding alterations and SVs and virus integrations can create diverse transcriptomic aberrations | Integrative analysis of WGS and RNA-Seq is crucial for understanding the importance of comprehensive GA identification, shaping new diagnostic and therapeutic avenues | [159] |
| HCC | 27 (25 HBV- or HCV-related) | In the two multicentric tumors, WGS analysis suggested origins from independent mutations Chromatin regulation genes (ARID1A, ARID1B, ARID2, MLL, MLL3) were mutated in approximately 50% of the tumors Frequent integration of HBV DNA in TERT locus |
GAs and carcinogenesis can be influenced by the etiological background (viral hepatitis) Further elucidation on the molecular background of HCC is required to achieve significant clinical benefit |
[160] |
| HCC | 42 (WGS, WES and whole-transcriptome seq.) | More (TP53, CTNNB1 and AXIN1) or less (BAP1 and IDH1) frequent mutations and a novel deletion in CTNNB1 were identified; LAMA2 was a predictor of recurrence and poor survival | Identification of GAs and virus-associated genomic changes provide new predictive and therapeutic potential | [161] |
| HCC | 88 (81 HBV positive) | HBV integration is more frequent in the tumors (86.4%) than in adjacent liver tissues (30.7%) Recurrent HBV integration in TERT, MLL4 and CCNE1 genes, with upregulated gene expression |
The number of HBV integrations is associated with survival and could have prognostic significance | [162] |
| HCC/LCB | 90 (30 LCB, 60 HCC) | LCBs feature recurrent mutations in TERT promoter, chromatin regulators (BAP1, PBRM1 and ARID2), a synapse organization gene (PCLO), IDH genes and KRAS
KRAS and IDH mutations were more frequent in hepatitis-negative LCBs and are associated with poor disease-free survival |
Chronic hepatitis has a major impact on the mutational status of liver cancer | [163] |
| PDA | 100 (WGS and CNV analysis) | Identification of altered genes (TP53, SMAD4, CDKN2A, ARID1A and ROBO2), novel gene mutations (KDM6A and PREX2) and frequent targetable gene mutations (ERBB2, MET, FGFR1, CDK6, PIK3R3 and PIK3CA) | KDM6A and PREX2 are potential biomarkers and therapeutic targets | [164] |
| HCC, ICC | 300 (268 HCC, 24 ICC, 8 combined HCC/ICC) | Mutations related to liver carcinogenesis and recurrently mutated coding and noncoding regions were identified Known (CDKN2A, CCND1, APC, and TERT) and novel (ASH1L, NCOR1, and MACROD2) cancer-related genes were identified in SV analysis |
WGS is crucial for detection of cancer driver genes Association of risk factors (smoking, HCV, HBV, alcohol) with specific mutations can predict tumorigenesis and provide prognostic potential |
[10] |
Copy number alteration (CNA); fibrolamellar carcinoma (FLC); genomic alterations (GA); hepatocellular carcinoma (HCC); intrahepatic cholangiocarcinoma (ICC); liver cancer displaying biliary phenotype (LCB); pancreatic ductal adenocarcinoma (PDA); single nucleotide variation (SNV); structural variation (SV); whole-exome sequencing (WES); whole-genome sequencing (WGS); * 452 cases of WES are included in Table 5A.
3.3. Confirmation of Known Cancer Driver Genes by NGS Supporting Clinical Implications
Our review deemed two genes as noteworthy: TERT and ARID1A. TERT alterations were discovered mainly in HCC patients with tNGS [121], WES [155], and WGS [10,155,160,162,163]. On the other hand, ARID1A aberrations were uncovered in all types of HBP cancer by tNGS [129], WES [142,145,150,151,155], and WGS [155,160,164].
Telomerase reverse transcriptase (abbreviated to TERT, hTRT, or hTERT in humans) is a telomerase enzyme catalytic subunit, along with the telomerase RNA component (hTR or TERC). Telomerase is expressed, and telomere length is maintained in human germ cells and the vast majority of primary human cancers (~90%), deterring apoptosis [165,166]. Many cancers also exhibit mutations in the TERT promoter locus, which increase transcriptional activation of this gene [167]. Regulation of TERT and telomerase activity is achieved through a large number of mechanisms and complexes, including the mTOR pathway [166]. Therefore, TERT has been an important target for anticancer treatment, especially immunotherapy, in the past twenty years with mostly unfavorable results [167], despite the successful targeting of telomerase-positive tumor cells in in vitro and in mouse model studies [168].
The ARID1A gene in humans encodes the AT-rich interactive domain-containing protein 1A [169]. This protein is a member of the SWI/SNF family of proteins that are believed to regulate the transcription of certain genes by altering the chromatin structure [170,171,172]. The SWI/SNF complex has also been implicated with DNA repair mechanisms [173]. Several sequencing studies have identified SWI/SNF as a tumor suppressor in a number of diverse malignancies [174,175,176,177,178]. A meta-analysis of 24 whole-exome sequencing studies reported SWI/SNF to be mutated in approximately 20% of human malignancies and ARID1A to be the most commonly mutated gene of the complex [179]. ARID1A has commonly been found mutated in gastric cancer [180], ovarian clear cell carcinoma [178], hepatocellular carcinoma [160], and pancreatic cancer [164,175].
ARID1A is a promising potential target for future therapies. A recent study on ovarian clear cell carcinoma has demonstrated a synthetic lethality between ARID1A mutation and targeted inhibition of enhancer of zeste homolog 2 (EZH2) methyltransferase through upregulation of PIK3IP1, which is a negative regulator of PI3K [181,182]. Furthermore, EZH2 inhibition (EZH2i) has been shown to block tumor formation driven by SNF5 (member of the SWI/SNF complex) inactivation in rhabdoid tumors [183]. EZH2i was also found to alter the response to etoposide in patients with non-small-cell lung cancer, dependent on the mutational status of BRG1 (another member of the SWI/SNF complex) [184]. These findings suggest that targeted EZH2i is a compelling strategy against cancers with mutated SWI/SNF complex and EZH2 inhibitors are currently under clinical development with promising preclinical results [185]. Lastly, another study has identified ARID1B, an ARID1A homolog, as the most essential gene for the survival of ARID1A-mutant cancer cells. The loss of ARID1B in cells with silencing ARID1A mutations impairs cell proliferation, making it a potential therapeutic target in ARID1A-deficient tumors [186].
3.4. Inter-Patient Heterogeneity and Personalized Therapeutic Approach
The evidence of tumor heterogeneity and the clinical challenge of interpatient variation-based personalized treatment could most likely be enabled by WES and WGS studies [9,187]. Two international, large projects, The Cancer Genome Atlas (TCGA) [188] and the International Cancer Genome Consortium (ICGC) [189], aiming at completing the cancer driver genes and mutations catalogue for 50 cancer types using NGS platforms, have already identified many novel genes involved in tumorigenesis. The largest WES study available was conducted by Lawrence et al. [9] spanning 21 tumor types, including 12 from (TCGA) and 14 from non-TCGA projects at the Broad Institute, with some overlapping tumor types. Based on extensive tumor heterogeneity, Lawrence et al. recommend strict criteria for reporting novel cancer genes, such as strong statistical significance (p < 0.01), suggesting large numbers (>500) of tumor samples [9]. Therefore, the novel genes identified by WES (Table 8) and WGS (Table 9) with possible clinical utility as biomarkers or novel therapeutic targets [149,164] require confirmation by larger studies.
4. Future Perspectives
Despite intensive research effort, relapse rates of HBP cancers remain substantially high. There has been slow progress in the development of effective systemic therapies. Only a few therapeutic options are available, including sorafenib approved only for advanced-metastatic HCC, gemcitabine in the adjuvant and metastatic setting of PDA, and erlotinib for locally advanced or metastatic PDA. Moreover, recent, large-scale, negative Phase III RCTs testing the efficacy of targeted drugs (Table 3 and Table 4) suggest the urgent need to shift from inexact medicine to understanding and precisely targeting molecular mechanisms underlying therapeutic resistance. Conventional single biopsy-based NGS studies, by enabling the identification of novel cancer driver genes and druggable mutations, shape a new avenue in the development of more effective systemic therapeutic interventions. Based on the discovery of novel actionable alterations by NGS, the concept of an early drug-development strategy could significantly broaden the list of approved targeted drugs. Given the considerable interpatient heterogeneity, this approach could improve primary therapeutic decision-making. One of the greatest challenges will be the translation of cancer genome sequencing discoveries into patient care [190].
However, accumulating evidence of intratumor heterogeneity (ITH) of the primary cancer [191,192] and the dynamics of genomic subclones according to the principles of Darwinian evolution [193] limit the expectations for overcoming primary and particularly acquired therapeutic resistance with the simple concept of single-biopsy NGS analysis. Breakthrough methods of NGS applications, including multi-regional biopsies for genome sequencing to identify ITH and repeated NGS of plasma circulating cell-free DNA or circulating tumor DNA (cfDNA, ctDNA) can identify dynamic emergence of distinct subclones. By comparing the GA landscape of the primary tumor to that of circulating genomic subclones (CGS) and the relapsed tumors in individual patients, we could develop biomarkers to predict and monitor disease relapse [194]. Furthermore, an early targeting of the identified resistant subclones could overcome therapeutic resistance, prolonging time to recurrence or even preventing metastatic relapse [140].
5. Conclusions
The validity of NGS technologies to identify tumor heterogeneity-associated therapeutic resistance and relapse gives rise to high expectations for translating these advances into patient-centric trials and clinical benefit. In the medium term, tNGS enables the conduction of umbrella and basket clinical trials. The identification of mutated or amplified gene-based patient subgroups and the subsequent tumor-guided treatment with targeted drugs from the list of available FDA-approved agents, matching these specific genetic alterations, could improve personalized patient care.
By contrast, the discovery of novel therapeutic targets by WES and WGS studies raises much higher expectations to substantially broaden the targeted drugs catalogue with a long-term perspective. However, this concept requires evaluation and confirmation by appropriately designed large-scale clinical trials. Therefore, tNGS, WES, and WGS could enable the development of robust biomarkers for tailored treatment.
In summary, translational NGS research represents a top prospect for faster progress than any other available technology to achieve precision oncology.
Author Contributions
All authors have contributed to this article. In particular, the first, second and corresponding author have designed the study and completed the writing of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Shendure J., Ji H. Next-generation DNA sequencing. Nat. Biotechnol. 2008;26:1135–1145. doi: 10.1038/nbt1486. [DOI] [PubMed] [Google Scholar]
- 2.Consortium E.P. An integrated encyclopedia of DNA elements in the human genome. Nature. 2012;489:57–74. doi: 10.1038/nature11247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stamatoyannopoulos J.A. What does our genome encode? Genome Res. 2012;22:1602–1611. doi: 10.1101/gr.146506.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aronson S.J., Rehm H.L. Building the foundation for genomics in precision medicine. Nature. 2015;526:336–342. doi: 10.1038/nature15816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vogelstein B., Papadopoulos N., Velculescu V.E., Zhou S., Diaz L.A., Jr., Kinzler K.W. Cancer genome landscapes. Science. 2013;339:1546–1558. doi: 10.1126/science.1235122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2016. CA Cancer. 2016;66:7–30. doi: 10.3322/caac.21332. [DOI] [PubMed] [Google Scholar]
- 7.Howlader N., Noone A., Krapcho M., Miller D., Bishop K., Altekruse S., Kosary C., Yu M., Ruhl J., Tatalovich Z., et al. SEER Cancer Statistics Review, 1975–2013. [(accessed on 18 October 2016)]; Available online: https://seer.cancer.gov/csr/1975_2013/
- 8.Ku C.S., Roukos D.H. From next-generation sequencing to nanopore sequencing technology: Paving the way to personalized genomic medicine. Expert Rev. Med. Dev. 2013;10:1–6. doi: 10.1586/erd.12.63. [DOI] [PubMed] [Google Scholar]
- 9.Lawrence M.S., Stojanov P., Mermel C.H., Robinson J.T., Garraway L.A., Golub T.R., Meyerson M., Gabriel S.B., Lander E.S., Getz G. Discovery and saturation analysis of cancer genes across 21 tumour types. Nature. 2014;505:495–501. doi: 10.1038/nature12912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fujimoto A., Furuta M., Totoki Y., Tsunoda T., Kato M., Shiraishi Y., Tanaka H., Taniguchi H., Kawakami Y., Ueno M., et al. Whole-genome mutational landscape and characterization of noncoding and structural mutations in liver cancer. Nat. Genet. 2016;48:500–509. doi: 10.1038/ng.3547. [DOI] [PubMed] [Google Scholar]
- 11.Ferlay J., Soerjomataram I., Dikshit R., Eser S., Mathers C., Rebelo M., Parkin D.M., Forman D., Bray F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer. 2015;136:359–386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 12.European Association For The Study Of The Liver. European Organisation For Research and Treatment Of Cancer EASL-EORTC clinical practice guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2012;56:908–943. doi: 10.1016/j.jhep.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 13.Al-Hawary M.M., Francis I.R., Chari S.T., Fishman E.K., Hough D.M., Lu D.S., Macari M., Megibow A.J., Miller F.H., Mortele K.J., et al. Pancreatic ductal adenocarcinoma radiology reporting template: Consensus statement of the society of abdominal radiology and the american pancreatic association. Gastroenterology. 2014;146:291–304. doi: 10.1053/j.gastro.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 14.Bruix J., Sherman M. American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: An update. Hepatology. 2011;53:1020–1022. doi: 10.1002/hep.24199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brugge W.R., de Witt J., Klapman J.B., Ashfaq R., Shidham V., Chhieng D., Kwon R., Baloch Z., Zarka M., Staerkel G. Techniques for cytologic sampling of pancreatic and bile duct lesions: The Papanicolaou Society of Cytopathology Guidelines. CytoJournal. 2014;11:2. doi: 10.4103/1742-6413.133311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li J.H., He R., Li Y.M., Cao G., Ma Q.Y., Yang W.B. Endoscopic ultrasonography for tumor node staging and vascular invasion in pancreatic cancer: A meta-analysis. Dig. Surg. 2014;31:297–305. doi: 10.1159/000368089. [DOI] [PubMed] [Google Scholar]
- 17.Nawaz H., Fan C.Y., Kloke J., Khalid A., McGrath K., Landsittel D., Papachristou G.I. Performance characteristics of endoscopic ultrasound in the staging of pancreatic cancer: A meta-analysis. J. Pancreas. 2013;14:484–497. doi: 10.6092/1590-8577/1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Callery M.P., Chang K.J., Fishman E.K., Talamonti M.S., William Traverso L., Linehan D.C. Pretreatment assessment of resectable and borderline resectable pancreatic cancer: Expert consensus statement. Ann. Surg. Oncol. 2009;16:1727–1733. doi: 10.1245/s10434-009-0408-6. [DOI] [PubMed] [Google Scholar]
- 19.Natsuizaka M., Omura T., Akaike T., Kuwata Y., Yamazaki K., Sato T., Karino Y., Toyota J., Suga T., Asaka M. Clinical features of hepatocellular carcinoma with extrahepatic metastases. J. Gastroenterol. Hepatol. 2005;20:1781–1787. doi: 10.1111/j.1440-1746.2005.03919.x. [DOI] [PubMed] [Google Scholar]
- 20.Kamath P.S., Wiesner R.H., Malinchoc M., Kremers W., Therneau T.M., Kosberg C.L., d’Amico G., Dickson E.R., Kim W.R. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464–470. doi: 10.1053/jhep.2001.22172. [DOI] [PubMed] [Google Scholar]
- 21.Johnson P.J., Berhane S., Kagebayashi C., Satomura S., Teng M., Reeves H.L., O’Beirne J., Fox R., Skowronska A., Palmer D., et al. Assessment of liver function in patients with hepatocellular carcinoma: A new evidence-based approach-the ALBI grade. J. Clin. Oncol. 2015;33:550–558. doi: 10.1200/JCO.2014.57.9151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Torzilli G., Belghiti J., Kokudo N., Takayama T., Capussotti L., Nuzzo G., Vauthey J.N., Choti M.A., de Santibanes E., Donadon M., et al. A snapshot of the effective indications and results of surgery for hepatocellular carcinoma in tertiary referral centers: Is it adherent to the EASL/AASLD recommendations?: An observational study of the HCC East-West study group. Ann. Surg. 2013;257:929–937. doi: 10.1097/SLA.0b013e31828329b8. [DOI] [PubMed] [Google Scholar]
- 23.NCCN Clinical Practice Guidelines in Oncology. Pancreatic Adenocarcinoma, Version 2. 2016. [(accessed on 5 October 2016)]. Available online: https://www.nccn.org/professionals/physician_gls/f_guidelines.asp.
- 24.NCCN Clinical Practice Guidelines in Oncology. Hepatobiliary Cancers, Version 2. 2016. [(accessed on 5 October 2016)]. Available online: https://www.nccn.org/professionals/physician_gls/f_guidelines.asp.
- 25.American Cancer Society . Manual for Staging of Cancer. American Joint Committee; Chicago, IL, USA: 1977. American Joint Committee on Cancer Staging and End Results Reporting. [Google Scholar]
- 26.Hermanek P., Sobin L.H. UICC International Union against Cancer. 4th, Fully Revised ed. Springer; Berlin/Heidelberg, Germany: 1987. TNM Classification of Malignant Tumours. [Google Scholar]
- 27.Bruix J., Llovet J.M. Prognostic prediction and treatment strategy in hepatocellular carcinoma. Hepatology. 2002;35:519–524. doi: 10.1053/jhep.2002.32089. [DOI] [PubMed] [Google Scholar]
- 28.Truty M.J., Vauthey J.N. Surgical resection of high-risk hepatocellular carcinoma: Patient selection, preoperative considerations, and operative technique. Ann. Surg. Oncol. 2010;17:1219–1225. doi: 10.1245/s10434-010-0976-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mazzaferro V., Regalia E., Doci R., Andreola S., Pulvirenti A., Bozzetti F., Montalto F., Ammatuna M., Morabito A., Gennari L. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N. Engl. J. Med. 1996;334:693–699. doi: 10.1056/NEJM199603143341104. [DOI] [PubMed] [Google Scholar]
- 30.D’Angelica M., Dalal K.M., de Matteo R.P., Fong Y., Blumgart L.H., Jarnagin W.R. Analysis of the extent of resection for adenocarcinoma of the gallbladder. Ann. Surg. Oncol. 2009;16:806–816. doi: 10.1245/s10434-008-0189-3. [DOI] [PubMed] [Google Scholar]
- 31.De Jong M.C., Nathan H., Sotiropoulos G.C., Paul A., Alexandrescu S., Marques H., Pulitano C., Barroso E., Clary B.M., Aldrighetti L., et al. Intrahepatic cholangiocarcinoma: An international multi-institutional analysis of prognostic factors and lymph node assessment. J. Clin. Oncol. 2011;29:3140–3145. doi: 10.1200/JCO.2011.35.6519. [DOI] [PubMed] [Google Scholar]
- 32.Nakeeb A., Lillemoe K.D., Grosfeld J.L. Surgical techniques for pancreatic cancer. Minerva Chir. 2004;59:151–163. [PubMed] [Google Scholar]
- 33.Verslype C., Rosmorduc O., Rougier P., Group E.G.W. Hepatocellular carcinoma: ESMO-ESDO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2012;23:41–48. doi: 10.1093/annonc/mds225. [DOI] [PubMed] [Google Scholar]
- 34.Ono T., Yamanoi A., Nazmy El Assal O., Kohno H., Nagasue N. Adjuvant chemotherapy after resection of hepatocellular carcinoma causes deterioration of long-term prognosis in cirrhotic patients: Metaanalysis of three randomized controlled trials. Cancer. 2001;91:2378–2385. doi: 10.1002/1097-0142(20010615)91:12<2378::AID-CNCR1271>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 35.Samuel M., Chow P.K., Chan Shih-Yen E., Machin D., Soo K.C. Neoadjuvant and adjuvant therapy for surgical resection of hepatocellular carcinoma. Cochrane Database Syst. Rev. 2009;1:CD001199. doi: 10.1002/14651858.CD001199.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Horgan A.M., Amir E., Walter T., Knox J.J. Adjuvant therapy in the treatment of biliary tract cancer: A systematic review and meta-analysis. J. Clin. Oncol. 2012;30:1934–1940. doi: 10.1200/JCO.2011.40.5381. [DOI] [PubMed] [Google Scholar]
- 37.Macdonald O.K., Crane C.H. Palliative and postoperative radiotherapy in biliary tract cancer. Surg. Oncol. Clin. N. Am. 2002;11:941–954. doi: 10.1016/S1055-3207(02)00038-8. [DOI] [PubMed] [Google Scholar]
- 38.Hezel A.F., Zhu A.X. Systemic therapy for biliary tract cancers. Oncologist. 2008;13:415–423. doi: 10.1634/theoncologist.2007-0252. [DOI] [PubMed] [Google Scholar]
- 39.Valle J., Wasan H., Palmer D.H., Cunningham D., Anthoney A., Maraveyas A., Madhusudan S., Iveson T., Hughes S., Pereira S.P., et al. Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N. Engl. J. Med. 2010;362:1273–1281. doi: 10.1056/NEJMoa0908721. [DOI] [PubMed] [Google Scholar]
- 40.Conroy T., Desseigne F., Ychou M., Bouche O., Guimbaud R., Becouarn Y., Adenis A., Raoul J.L., Gourgou-Bourgade S., de la Fouchardiere C., et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N. Engl. J. Med. 2011;364:1817–1825. doi: 10.1056/NEJMoa1011923. [DOI] [PubMed] [Google Scholar]
- 41.Von Hoff D.D., Ervin T., Arena F.P., Chiorean E.G., Infante J., Moore M., Seay T., Tjulandin S.A., Ma W.W., Saleh M.N., et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N. Engl. J. Med. 2013;369:1691–1703. doi: 10.1056/NEJMoa1304369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Le Scodan R., Mornex F., Girard N., Mercier C., Valette P.J., Ychou M., Bibeau F., Roy P., Scoazec J.Y., Partensky C. Preoperative chemoradiation in potentially resectable pancreatic adenocarcinoma: Feasibility, treatment effect evaluation and prognostic factors, analysis of the SFRO-FFCD 9704 trial and literature review. Ann. Oncol. 2009;20:1387–1396. doi: 10.1093/annonc/mdp015. [DOI] [PubMed] [Google Scholar]
- 43.Evans D.B., Varadhachary G.R., Crane C.H., Sun C.C., Lee J.E., Pisters P.W., Vauthey J.N., Wang H., Cleary K.R., Staerkel G.A., et al. Preoperative gemcitabine-based chemoradiation for patients with resectable adenocarcinoma of the pancreatic head. J. Clin. Oncol. 2008;26:3496–3502. doi: 10.1200/JCO.2007.15.8634. [DOI] [PubMed] [Google Scholar]
- 44.Varadhachary G.R., Wolff R.A., Crane C.H., Sun C.C., Lee J.E., Pisters P.W., Vauthey J.N., Abdalla E., Wang H., Staerkel G.A., et al. Preoperative gemcitabine and cisplatin followed by gemcitabine-based chemoradiation for resectable adenocarcinoma of the pancreatic head. J. Clin. Oncol. 2008;26:3487–3495. doi: 10.1200/JCO.2007.15.8642. [DOI] [PubMed] [Google Scholar]
- 45.Regine W.F., Winter K.A., Abrams R.A., Safran H., Hoffman J.P., Konski A., Benson A.B., Macdonald J.S., Kudrimoti M.R., Fromm M.L., et al. Fluorouracil vs. gemcitabine chemotherapy before and after fluorouracil-based chemoradiation following resection of pancreatic adenocarcinoma: A randomized controlled trial. JAMA. 2008;299:1019–1026. doi: 10.1001/jama.299.9.1019. [DOI] [PubMed] [Google Scholar]
- 46.Neoptolemos J.P., Stocken D.D., Bassi C., Ghaneh P., Cunningham D., Goldstein D., Padbury R., Moore M.J., Gallinger S., Mariette C., et al. Adjuvant chemotherapy with fluorouracil plus folinic acid vs. gemcitabine following pancreatic cancer resection: A randomized controlled trial. JAMA. 2010;304:1073–1081. doi: 10.1001/jama.2010.1275. [DOI] [PubMed] [Google Scholar]
- 47.Van Laethem J.L., Hammel P., Mornex F., Azria D., van Tienhoven G., Vergauwe P., Peeters M., Polus M., Praet M., Mauer M., et al. Adjuvant gemcitabine alone versus gemcitabine-based chemoradiotherapy after curative resection for pancreatic cancer: A randomized EORTC-40013–22012/FFCD-9203/GERCOR phase II study. J. Clin. Oncol. 2010;28:4450–4456. doi: 10.1200/JCO.2010.30.3446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Oettle H., Neuhaus P., Hochhaus A., Hartmann J.T., Gellert K., Ridwelski K., Niedergethmann M., Zulke C., Fahlke J., Arning M.B., et al. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: The CONKO-001 randomized trial. JAMA. 2013;310:1473–1481. doi: 10.1001/jama.2013.279201. [DOI] [PubMed] [Google Scholar]
- 49.Lo C.M., Ngan H., Tso W.K., Liu C.L., Lam C.M., Poon R.T., Fan S.T., Wong J. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology. 2002;35:1164–1171. doi: 10.1053/jhep.2002.33156. [DOI] [PubMed] [Google Scholar]
- 50.Llovet J.M., Real M.I., Montana X., Planas R., Coll S., Aponte J., Ayuso C., Sala M., Muchart J., Sola R., et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: A randomised controlled trial. Lancet. 2002;359:1734–1739. doi: 10.1016/S0140-6736(02)08649-X. [DOI] [PubMed] [Google Scholar]
- 51.Llovet J.M., Ricci S., Mazzaferro V., Hilgard P., Gane E., Blanc J.F., de Oliveira A.C., Santoro A., Raoul J.L., Forner A., et al. Sorafenib in advanced hepatocellular carcinoma. N. Engl. J. Med. 2008;359:378–390. doi: 10.1056/NEJMoa0708857. [DOI] [PubMed] [Google Scholar]
- 52.Cheng A.L., Kang Y.K., Chen Z., Tsao C.J., Qin S., Kim J.S., Luo R., Feng J., Ye S., Yang T.S., et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: A phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009;10:25–34. doi: 10.1016/S1470-2045(08)70285-7. [DOI] [PubMed] [Google Scholar]
- 53.Wilhelm S.M., Adnane L., Newell P., Villanueva A., Llovet J.M., Lynch M. Preclinical overview of sorafenib, a multikinase inhibitor that targets both Raf and VEGF and PDGF receptor tyrosine kinase signaling. Mol. Cancer Ther. 2008;7:3129–3140. doi: 10.1158/1535-7163.MCT-08-0013. [DOI] [PubMed] [Google Scholar]
- 54.Keating G.M., Santoro A. Sorafenib: A review of its use in advanced hepatocellular carcinoma. Drugs. 2009;69:223–240. doi: 10.2165/00003495-200969020-00006. [DOI] [PubMed] [Google Scholar]
- 55.Escudier B., Eisen T., Stadler W.M., Szczylik C., Oudard S., Siebels M., Negrier S., Chevreau C., Solska E., Desai A.A., et al. Sorafenib in advanced clear-cell renal-cell carcinoma. N. Engl. J. Med. 2007;356:125–134. doi: 10.1056/NEJMoa060655. [DOI] [PubMed] [Google Scholar]
- 56.Brose M.S., Nutting C.M., Jarzab B., Elisei R., Siena S., Bastholt L., de la Fouchardiere C., Pacini F., Paschke R., Shong Y.K., et al. Sorafenib in radioactive iodine-refractory, locally advanced or metastatic differentiated thyroid cancer: A randomised, double-blind, phase 3 trial. Lancet. 2014;384:319–328. doi: 10.1016/S0140-6736(14)60421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Moore M.J., Goldstein D., Hamm J., Figer A., Hecht J.R., Gallinger S., Au H.J., Murawa P., Walde D., Wolff R.A., et al. Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: A phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J. Clin. Oncol. 2007;25:1960–1966. doi: 10.1200/JCO.2006.07.9525. [DOI] [PubMed] [Google Scholar]
- 58.Fabian M.A., Biggs W.H., 3rd, Treiber D.K., Atteridge C.E., Azimioara M.D., Benedetti M.G., Carter T.A., Ciceri P., Edeen P.T., Floyd M., et al. A small molecule-kinase interaction map for clinical kinase inhibitors. Nat. Biotechnol. 2005;23:329–336. doi: 10.1038/nbt1068. [DOI] [PubMed] [Google Scholar]
- 59.Mosquera C., Maglic D., Zervos E.E. Molecular targeted therapy for pancreatic adenocarcinoma: A review of completed and ongoing late phase clinical trials. Cancer Genet. 2016;209:567–581. doi: 10.1016/j.cancergen.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 60.Huguet F., Hammel P., Vernerey D., Goldstein D., Laethem J.L.V., Glimelius B., Spry N., Paget-Bailly S., Bonnetain F., Louvet C. Impact of chemoradiotherapy (CRT) on local control and time without treatment in patients with locally advanced pancreatic cancer (LAPC) included in the international phase III LAP 07 study. Pancreatology. 2014;14:6. [Google Scholar]
- 61.Hammel P., Huguet F., van Laethem J.L., Goldstein D., Glimelius B., Artru P., Borbath I., Bouche O., Shannon J., Andre T., et al. Effect of Chemoradiotherapy vs. Chemotherapy on Survival in Patients with Locally Advanced Pancreatic Cancer Controlled after 4 Months of Gemcitabine with or without Erlotinib: The LAP07 Randomized Clinical Trial. JAMA. 2016;315:1844–1853. doi: 10.1001/jama.2016.4324. [DOI] [PubMed] [Google Scholar]
- 62.American Cancer Society Survival Statistics for Bile Duct Cancers. [(accessed on 14 September 2016)]. Available online: http://www.cancer.org/cancer/bileductcancer/detailedguide/bile-duct-cancer-survival-by-stage.
- 63.Horner M., Ries L., Krapcho M., Neyman N., Aminou R., Howlader N., Altekruse S., Feuer E., Huang L., Mariotto A., et al. SEER Cancer Statistics Review, 1975–2006. [(accessed on 18 October 2016)]; Available online: https://seer.cancer.gov/csr/1975_2006/
- 64.Ries L., Eisner M., Kosary C., Hankey B., Miller B., Clegg L., Edwards B. SEER Cancer Statistics Review, 1973–1999. [(accessed on 18 October 2016)]; Available online: https://seer.cancer.gov/csr/1973_1999/
- 65.Tabrizian P., Jibara G., Shrager B., Schwartz M., Roayaie S. Recurrence of hepatocellular cancer after resection: Patterns, treatments, and prognosis. Ann. Surg. 2015;261:947–955. doi: 10.1097/SLA.0000000000000710. [DOI] [PubMed] [Google Scholar]
- 66.Leung J.Y., Zhu A.X., Gordon F.D., Pratt D.S., Mithoefer A., Garrigan K., Terella A., Hertl M., Cosimi A.B., Chung R.T. Liver transplantation outcomes for early-stage hepatocellular carcinoma: Results of a multicenter study. Liver Transplant. 2004;10:1343–1354. doi: 10.1002/lt.20311. [DOI] [PubMed] [Google Scholar]
- 67.Shah S.A., Cleary S.P., Wei A.C., Yang I., Taylor B.R., Hemming A.W., Langer B., Grant D.R., Greig P.D., Gallinger S. Recurrence after liver resection for hepatocellular carcinoma: Risk factors, treatment, and outcomes. Surgery. 2007;141:330–339. doi: 10.1016/j.surg.2006.06.028. [DOI] [PubMed] [Google Scholar]
- 68.Lang H., Sotiropoulos G.C., Brokalaki E.I., Schmitz K.J., Bertona C., Meyer G., Frilling A., Paul A., Malago M., Broelsch C.E. Survival and recurrence rates after resection for hepatocellular carcinoma in noncirrhotic livers. J. Am. Coll. Surg. 2007;205:27–36. doi: 10.1016/j.jamcollsurg.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 69.Yoo H.Y., Patt C.H., Geschwind J.F., Thuluvath P.J. The outcome of liver transplantation in patients with hepatocellular carcinoma in the United States between 1988 and 2001: 5-Year survival has improved significantly with time. J. Clin. Oncol. 2003;21:4329–4335. doi: 10.1200/JCO.2003.11.137. [DOI] [PubMed] [Google Scholar]
- 70.Roayaie S., Schwartz J.D., Sung M.W., Emre S.H., Miller C.M., Gondolesi G.E., Krieger N.R., Schwartz M.E. Recurrence of hepatocellular carcinoma after liver transplant: Patterns and prognosis. Liver Transplant. 2004;10:534–540. doi: 10.1002/lt.20128. [DOI] [PubMed] [Google Scholar]
- 71.Sugiura T., Uesaka K., Mihara K., Sasaki K., Kanemoto H., Mizuno T., Okamura Y. Margin status, recurrence pattern, and prognosis after resection of pancreatic cancer. Surgery. 2013;154:1078–1086. doi: 10.1016/j.surg.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 72.Endo I., Gonen M., Yopp A.C., Dalal K.M., Zhou Q., Klimstra D., d’Angelica M., deMatteo R.P., Fong Y., Schwartz L., et al. Intrahepatic cholangiocarcinoma: Rising frequency, improved survival, and determinants of outcome after resection. Ann. Surg. 2008;248:84–96. doi: 10.1097/SLA.0b013e318176c4d3. [DOI] [PubMed] [Google Scholar]
- 73.Tamandl D., Herberger B., Gruenberger B., Puhalla H., Klinger M., Gruenberger T. Influence of hepatic resection margin on recurrence and survival in intrahepatic cholangiocarcinoma. Ann. Surg. Oncol. 2008;15:2787–2794. doi: 10.1245/s10434-008-0081-1. [DOI] [PubMed] [Google Scholar]
- 74.Sapisochin G., Fidelman N., Roberts J.P., Yao F.Y. Mixed hepatocellular cholangiocarcinoma and intrahepatic cholangiocarcinoma in patients undergoing transplantation for hepatocellular carcinoma. Liver Transplant. 2011;17:934–942. doi: 10.1002/lt.22307. [DOI] [PubMed] [Google Scholar]
- 75.Hong J.C., Petrowsky H., Kaldas F.M., Farmer D.G., Durazo F.A., Finn R.S., Saab S., Han S.H., Lee P., Markovic D., et al. Predictive index for tumor recurrence after liver transplantation for locally advanced intrahepatic and hilar cholangiocarcinoma. J. Am. Coll. Surg. 2011;212:514–520. doi: 10.1016/j.jamcollsurg.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 76.Woo S.M., Ryu J.K., Lee S.H., Yoo J.W., Park J.K., Kim Y.T., Jang J.Y., Kim S.W., Kang G.H., Yoon Y.B. Recurrence and prognostic factors of ampullary carcinoma after radical resection: Comparison with distal extrahepatic cholangiocarcinoma. Ann. Surg. Oncol. 2007;14:3195–3201. doi: 10.1245/s10434-007-9537-y. [DOI] [PubMed] [Google Scholar]
- 77.Kobayashi A., Miwa S., Nakata T., Miyagawa S. Disease recurrence patterns after R0 resection of hilar cholangiocarcinoma. Br. J. Surg. 2010;97:56–64. doi: 10.1002/bjs.6788. [DOI] [PubMed] [Google Scholar]
- 78.Jarnagin W.R., Ruo L., Little S.A., Klimstra D., d’Angelica M., de Matteo R.P., Wagman R., Blumgart L.H., Fong Y. Patterns of initial disease recurrence after resection of gallbladder carcinoma and hilar cholangiocarcinoma: Implications for adjuvant therapeutic strategies. Cancer. 2003;98:1689–1700. doi: 10.1002/cncr.11699. [DOI] [PubMed] [Google Scholar]
- 79.Gores G.J., Darwish Murad S., Heimbach J.K., Rosen C.B. Liver transplantation for perihilar cholangiocarcinoma. J. Dig. Dis. 2013;31:126–129. doi: 10.1159/000347207. [DOI] [PubMed] [Google Scholar]
- 80.Takada T., Amano H., Yasuda H., Nimura Y., Matsushiro T., Kato H., Nagakawa T., Nakayama T., Study Group of Surgical Adjuvant Therapy for Carcinomas of the Pancreas and Biliary Tract Is postoperative adjuvant chemotherapy useful for gallbladder carcinoma? A phase III multicenter prospective randomized controlled trial in patients with resected pancreaticobiliary carcinoma. Cancer. 2002;95:1685–1695. doi: 10.1002/cncr.10831. [DOI] [PubMed] [Google Scholar]
- 81.Bruix J., Takayama T., Mazzaferro V., Chau G.Y., Yang J., Kudo M., Cai J., Poon R.T., Han K.H., Tak W.Y., et al. Adjuvant sorafenib for hepatocellular carcinoma after resection or ablation (STORM): A phase 3, randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2015;16:1344–1354. doi: 10.1016/S1470-2045(15)00198-9. [DOI] [PubMed] [Google Scholar]
- 82.Cainap C., Qin S., Huang W.T., Chung I.J., Pan H., Cheng Y., Kudo M., Kang Y.K., Chen P.J., Toh H.C., et al. Linifanib versus Sorafenib in patients with advanced hepatocellular carcinoma: Results of a randomized phase III trial. J. Clin. Oncol. 2015;33:172–179. doi: 10.1200/JCO.2013.54.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kudo M., Han G., Finn R.S., Poon R.T., Blanc J.F., Yan L., Yang J., Lu L., Tak W.Y., Yu X., et al. Brivanib as adjuvant therapy to transarterial chemoembolization in patients with hepatocellular carcinoma: A randomized phase III trial. Hepatology. 2014;60:1697–1707. doi: 10.1002/hep.27290. [DOI] [PubMed] [Google Scholar]
- 84.Zhu A.X., Rosmorduc O., Evans T.R., Ross P.J., Santoro A., Carrilho F.J., Bruix J., Qin S., Thuluvath P.J., Llovet J.M., et al. SEARCH: A phase III, randomized, double-blind, placebo-controlled trial of sorafenib plus erlotinib in patients with advanced hepatocellular carcinoma. J. Clin. Oncol. 2015;33:559–566. doi: 10.1200/JCO.2013.53.7746. [DOI] [PubMed] [Google Scholar]
- 85.Abou-Alfa G.K., Qin S., Ryoo B.-Y., Lu S.-N., Yen C.-J., Feng Y.-H., Lim H.Y., Izzo F., Colombo M., Sarker D., et al. Phase III randomized study of second line ADI-peg 20 (A) plus best supportive care versus placebo (P) plus best supportive care in patients (pts) with advanced hepatocellular carcinoma (HCC); Proceedings of the 2016 ASCO Annual Meeting; Chicago, IL, USA. 2016; [DOI] [PubMed] [Google Scholar]
- 86.Zhu A.X., Park J.O., Ryoo B.Y., Yen C.J., Poon R., Pastorelli D., Blanc J.F., Chung H.C., Baron A.D., Pfiffer T.E., et al. Ramucirumab versus placebo as second-line treatment in patients with advanced hepatocellular carcinoma following first-line therapy with sorafenib (REACH): A randomised, double-blind, multicentre, phase 3 trial. Lancet Oncol. 2015;16:859–870. doi: 10.1016/S1470-2045(15)00050-9. [DOI] [PubMed] [Google Scholar]
- 87.Barbare J.C., Bouche O., Bonnetain F., Raoul J.L., Rougier P., Abergel A., Boige V., Denis B., Blanchi A., Pariente A., et al. Randomized controlled trial of tamoxifen in advanced hepatocellular carcinoma. J. Clin. Oncol. 2005;23:4338–4346. doi: 10.1200/JCO.2005.05.470. [DOI] [PubMed] [Google Scholar]
- 88.Llovet J.M., Decaens T., Raoul J.L., Boucher E., Kudo M., Chang C., Kang Y.K., Assenat E., Lim H.Y., Boige V., et al. Brivanib in patients with advanced hepatocellular carcinoma who were intolerant to sorafenib or for whom sorafenib failed: Results from the randomized phase III BRISK-PS study. J. Clin. Oncol. 2013;31:3509–3516. doi: 10.1200/JCO.2012.47.3009. [DOI] [PubMed] [Google Scholar]
- 89.Lee J.H., Lee J.H., Lim Y.S., Yeon J.E., Song T.J., Yu S.J., Gwak G.Y., Kim K.M., Kim Y.J., Lee J.W., et al. Adjuvant immunotherapy with autologous cytokine-induced killer cells for hepatocellular carcinoma. Gastroenterology. 2015;148:1383–1391. doi: 10.1053/j.gastro.2015.02.055. [DOI] [PubMed] [Google Scholar]
- 90.Valle J.W., Wasan H., Lopes A., Backen A.C., Palmer D.H., Morris K., Duggan M., Cunningham D., Anthoney D.A., Corrie P., et al. Cediranib or placebo in combination with cisplatin and gemcitabine chemotherapy for patients with advanced biliary tract cancer (ABC-03): A randomised phase 2 trial. Lancet Oncol. 2015;16:967–978. doi: 10.1016/S1470-2045(15)00139-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Middleton G., Silcocks P., Cox T., Valle J., Wadsley J., Propper D., Coxon F., Ross P., Madhusudan S., Roques T., et al. Gemcitabine and capecitabine with or without telomerase peptide vaccine GV1001 in patients with locally advanced or metastatic pancreatic cancer (TeloVac): An open-label, randomised, phase 3 trial. Lancet Oncol. 2014;15:829–840. doi: 10.1016/S1470-2045(14)70236-0. [DOI] [PubMed] [Google Scholar]
- 92.Philip P.A., Benedetti J., Corless C.L., Wong R., O’Reilly E.M., Flynn P.J., Rowland K.M., Atkins J.N., Mirtsching B.C., Rivkin S.E., et al. Phase III study comparing gemcitabine plus cetuximab versus gemcitabine in patients with advanced pancreatic adenocarcinoma: Southwest Oncology Group-directed intergroup trial S0205. J. Clin. Oncol. 2010;28:3605–3610. doi: 10.1200/JCO.2009.25.7550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Biotechnology Events. [(accessed on 23 September 2016)]. Available online: http://www.biotechnologyevents.com/node/8843.
- 94.Van Cutsem E., van de Velde H., Karasek P., Oettle H., Vervenne W.L., Szawlowski A., Schoffski P., Post S., Verslype C., Neumann H., et al. Phase III trial of gemcitabine plus tipifarnib compared with gemcitabine plus placebo in advanced pancreatic cancer. J. Clin. Oncol. 2004;22:1430–1438. doi: 10.1200/JCO.2004.10.112. [DOI] [PubMed] [Google Scholar]
- 95.Ioka T., Okusaka T., Ohkawa S., Boku N., Sawaki A., Fujii Y., Kamei Y., Takahashi S., Namazu K., Umeyama Y., et al. Efficacy and safety of axitinib in combination with gemcitabine in advanced pancreatic cancer: Subgroup analyses by region, including Japan, from the global randomized Phase III trial. Jpn. J. Clin. Oncol. 2015;45:439–448. doi: 10.1093/jjco/hyv011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kindler H.L., Niedzwiecki D., Hollis D., Sutherland S., Schrag D., Hurwitz H., Innocenti F., Mulcahy M.F., O’Reilly E., Wozniak T.F., et al. Gemcitabine plus bevacizumab compared with gemcitabine plus placebo in patients with advanced pancreatic cancer: Phase III trial of the Cancer and Leukemia Group B (CALGB 80303) J. Clin. Oncol. 2010;28:3617–3622. doi: 10.1200/JCO.2010.28.1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.O’Neil B.H., Scott A.J., Ma W.W., Cohen S.J., Aisner D.L., Menter A.R., Tejani M.A., Cho J.K., Granfortuna J., Coveler A.L., et al. A phase II/III randomized study to compare the efficacy and safety of rigosertib plus gemcitabine versus gemcitabine alone in patients with previously untreated metastatic pancreatic cancer. Ann. Oncol. 2016;27:1180. doi: 10.1093/annonc/mdw095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gilliam A.D., Broome P., Topuzov E.G., Garin A.M., Pulay I., Humphreys J., Whitehead A., Takhar A., Rowlands B.J., Beckingham I.J. An international multicenter randomized controlled trial of G17DT in patients with pancreatic cancer. Pancreas. 2012;41:374–379. doi: 10.1097/MPA.0b013e31822ade7e. [DOI] [PubMed] [Google Scholar]
- 99.Yamaue H., Tsunoda T., Tani M., Miyazawa M., Yamao K., Mizuno N., Okusaka T., Ueno H., Boku N., Fukutomi A., et al. Randomized phase II/III clinical trial of elpamotide for patients with advanced pancreatic cancer: PEGASUS-PC Study. Cancer Sci. 2015;106:883–890. doi: 10.1111/cas.12674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bruix J., Merle P., Granito A., Huang Y.-H., Bodoky G., Yokosuka O., Rosmorduc O., Breder V., Gerolami R., Masi G., et al. Efficacy and safety of regorafenib versus placebo in patients with hepatocellular carcinoma (HCC) progressing on sorafenib: Results of the international, randomized phase 3 RESORCE trial; Proceedings of ESMO 18th World Congress of Gastrointestinal Cancer; Barcelona, Spain. 29 June–2 July 2016. [Google Scholar]
- 101.Zhu A.X., Galle P.R., Kudo M., Finn R.S., Yang L., Abada P., Chang S.-C., Llovet J.M. A randomized, double-blind, placebo-controlled phase III study of ramucirumab versus placebo as second-line treatment in patients with hepatocellular carcinoma and elevated baseline alpha-fetoprotein following first-line sorafenib (REACH-2); Proceedings of the 2016 Gastrointestinal Cancers Symposium; San Francisco, CA, USA. 21–23 January 2016. [Google Scholar]
- 102.Santoro A., Rimassa L., Borbath I., Daniele B., Salvagni S., van Laethem J.L., van Vlierberghe H., Trojan J., Kolligs F.T., Weiss A., et al. Tivantinib for second-line treatment of advanced hepatocellular carcinoma: A randomised, placebo-controlled phase 2 study. Lancet Oncol. 2013;14:55–63. doi: 10.1016/S1470-2045(12)70490-4. [DOI] [PubMed] [Google Scholar]
- 103.Santoro A., Porta C., Rimassa L., Borbath I., Daniele B., Finn R.S., Raoul J.L., He R., Trojan J., Peck-Radosavljevic M., et al. A Phase 3 Placebo-Controlled Trial with Tivantinib (ARQ 197), in Patients with Second-Line, MET-High, Inoperable Hepatocellular Carcinoma; Proceedings of the International Liver Cancer Association 9th Annual Conference; Paris, France. 4–6 September 2015. [Google Scholar]
- 104.Golan T., Oh D.-Y., Reni M., Macarulla T.M., Tortora G., Hall M.J., Reinacher-Schick A.C., Borg C., Hochhauser D., Walter T., et al. A randomized phase III trial of olaparib maintenance monotherapy in patients (pts) with metastatic pancreatic cancer (mPC) who have a germline BRCA1/2 mutation (gBRCAm); Proceedings of 2016 ASCO Annual Meeting; Chicago, IL, USA. 3–7 June 2016. [Google Scholar]
- 105.Biankin A.V., Piantadosi S., Hollingsworth S.J. Patient-centric trials for therapeutic development in precision oncology. Nature. 2015;526:361–370. doi: 10.1038/nature15819. [DOI] [PubMed] [Google Scholar]
- 106.Mirnezami R., Nicholson J., Darzi A. Preparing for precision medicine. N. Engl. J. Med. 2012;366:489–491. doi: 10.1056/NEJMp1114866. [DOI] [PubMed] [Google Scholar]
- 107.Roukos D.H., Ku C.S. Clinical cancer genome and precision medicine. Ann. Surg. Oncol. 2012;19:3646–3650. doi: 10.1245/s10434-012-2542-9. [DOI] [PubMed] [Google Scholar]
- 108.Swanton C., Soria J.C., Bardelli A., Biankin A., Caldas C., Chandarlapaty S., de Koning L., Dive C., Feunteun J., Leung S.Y., et al. Consensus on precision medicine for metastatic cancers: A report from the MAP conference. Ann. Oncol. 2016;27:1443–1448. doi: 10.1093/annonc/mdw192. [DOI] [PubMed] [Google Scholar]
- 109.Van Allen E.M., Wagle N., Stojanov P., Perrin D.L., Cibulskis K., Marlow S., Jane-Valbuena J., Friedrich D.C., Kryukov G., Carter S.L., et al. Whole-exome sequencing and clinical interpretation of formalin-fixed, paraffin-embedded tumor samples to guide precision cancer medicine. Nat. Med. 2014;20:682–688. doi: 10.1038/nm.3559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Munchel S., Hoang Y., Zhao Y., Cottrell J., Klotzle B., Godwin A.K., Koestler D., Beyerlein P., Fan J.B., Bibikova M., et al. Targeted or whole genome sequencing of formalin fixed tissue samples: Potential applications in cancer genomics. Oncotarget. 2015;6:25943–25961. doi: 10.18632/oncotarget.4671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Nowell P.C. The clonal evolution of tumor cell populations. Science. 1976;194:23–28. doi: 10.1126/science.959840. [DOI] [PubMed] [Google Scholar]
- 112.Klein C.A. Selection and adaptation during metastatic cancer progression. Nature. 2013;501:365–372. doi: 10.1038/nature12628. [DOI] [PubMed] [Google Scholar]
- 113.Mafficini A., Amato E., Fassan M., Simbolo M., Antonello D., Vicentini C., Scardoni M., Bersani S., Gottardi M., Rusev B., et al. Reporting tumor molecular heterogeneity in histopathological diagnosis. PLoS ONE. 2014;9:104979. doi: 10.1371/journal.pone.0104979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Froyen G., Broekmans A., Hillen F., Pat K., Achten R., Mebis J., Rummens J.L., Willemse J., Maes B. Validation and Application of a Custom-Designed Targeted Next-Generation Sequencing Panel for the Diagnostic Mutational Profiling of Solid Tumors. PLoS ONE. 2016;11:0154038. doi: 10.1371/journal.pone.0154038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Roukos D.H. Trastuzumab and beyond: sequencing cancer genomes and predicting molecular networks. Pharmacogenom. J. 2011;11:81–92. doi: 10.1038/tpj.2010.81. [DOI] [PubMed] [Google Scholar]
- 116.Hirotsu Y., Zheng T.H., Amemiya K., Mochizuki H., Guleng B., Omata M. Targeted and exome sequencing identified somatic mutations in hepatocellular carcinoma. Hepatol. Res. 2016;46:1145–1151. doi: 10.1111/hepr.12663. [DOI] [PubMed] [Google Scholar]
- 117.Lu J., Yin J., Dong R., Yang T., Yuan L., Zang L., Xu C., Peng B., Zhao J., Du X. Targeted sequencing of cancer-associated genes in hepatocellular carcinoma using next generation sequencing. Mol. Med. Rep. 2015;12:4678–4682. doi: 10.3892/mmr.2015.3952. [DOI] [PubMed] [Google Scholar]
- 118.Janku F., Kaseb A.O., Tsimberidou A.M., Wolff R.A., Kurzrock R. Identification of novel therapeutic targets in the PI3K/AKT/mTOR pathway in hepatocellular carcinoma using targeted next generation sequencing. Oncotarget. 2014;5:3012–3022. doi: 10.18632/oncotarget.1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kaibori M., Sakai K., Ishizaki M., Matsushima H., de Velasco M.A., Matsui K., Iida H., Kitade H., Kwon A.H., Nagano H., et al. Increased FGF19 copy number is frequently detected in hepatocellular carcinoma with a complete response after sorafenib treatment. Oncotarget. 2016;31:49091–49098. doi: 10.18632/oncotarget.10077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Sakai K., Takeda H., Nishijima N., Orito E., Joko K., Uchida Y., Izumi N., Nishio K., Osaki Y. Targeted DNA and RNA sequencing of fine-needle biopsy FFPE specimens in patients with unresectable hepatocellular carcinoma treated with sorafenib. Oncotarget. 2015;6:21636–21644. doi: 10.18632/oncotarget.4270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kawai-Kitahata F., Asahina Y., Tanaka S., Kakinuma S., Murakawa M., Nitta S., Watanabe T., Otani S., Taniguchi M., Goto F., et al. Comprehensive analyses of mutations and hepatitis B virus integration in hepatocellular carcinoma with clinicopathological features. J. Gastroenterol. 2016;51:473–486. doi: 10.1007/s00535-015-1126-4. [DOI] [PubMed] [Google Scholar]
- 122.Putra J., de Abreu F.B., Peterson J.D., Pipas J.M., Mody K., Amos C.I., Tsongalis G.J., Suriawinata A.A. Molecular profiling of intrahepatic and extrahepatic cholangiocarcinoma using next generation sequencing. Exp. Mol. Pathol. 2015;99:240–244. doi: 10.1016/j.yexmp.2015.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ross J.S., Wang K., Gay L., Al-Rohil R., Rand J.V., Jones D.M., Lee H.J., Sheehan C.E., Otto G.A., Palmer G., et al. New routes to targeted therapy of intrahepatic cholangiocarcinomas revealed by next-generation sequencing. Oncologist. 2014;19:235–242. doi: 10.1634/theoncologist.2013-0352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Yoo K.H., Kim N.K., Kwon W.I., Lee C., Kim S.Y., Jang J., Ahn J., Kang M., Jang H., Kim S.T., et al. Genomic Alterations in Biliary Tract Cancer Using Targeted Sequencing. Transl. Oncol. 2016;9:173–178. doi: 10.1016/j.tranon.2016.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lee C.H., Wang H.E., Seo S.Y., Kim S.H., Kim I.H., Kim S.W., Lee S.T., Kim D.G., Han M.K., Lee S.O. Cancer related gene alterations can be detected with next-generation sequencing analysis of bile in diffusely infiltrating type cholangiocarcinoma. Exp. Mol. Pathol. 2016;101:150–156. doi: 10.1016/j.yexmp.2016.07.010. [DOI] [PubMed] [Google Scholar]
- 126.Jiao Y., Pawlik T.M., Anders R.A., Selaru F.M., Streppel M.M., Lucas D.J., Niknafs N., Guthrie V.B., Maitra A., Argani P., et al. Exome sequencing identifies frequent inactivating mutations in BAP1, ARID1A and PBRM1 in intrahepatic cholangiocarcinomas. Nat. Genet. 2013;45:1470–1473. doi: 10.1038/ng.2813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Churi C.R., Shroff R., Wang Y., Rashid A., Kang H.C., Weatherly J., Zuo M., Zinner R., Hong D., Meric-Bernstam F., et al. Mutation profiling in cholangiocarcinoma: Prognostic and therapeutic implications. PLoS ONE. 2014;9:115383. doi: 10.1371/journal.pone.0115383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Simbolo M., Fassan M., Ruzzenente A., Mafficini A., Wood L.D., Corbo V., Melisi D., Malleo G., Vicentini C., Malpeli G., et al. Multigene mutational profiling of cholangiocarcinomas identifies actionable molecular subgroups. Oncotarget. 2014;5:2839–2852. doi: 10.18632/oncotarget.1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Javle M., Bekaii-Saab T., Jain A., Wang Y., Kelley R.K., Wang K., Kang H.C., Catenacci D., Ali S., Krishnan S., et al. Biliary cancer: Utility of next-generation sequencing for clinical management. Cancer. 2016;122:3838–3847. doi: 10.1002/cncr.30254. [DOI] [PubMed] [Google Scholar]
- 130.Basturk O., Tan M., Bhanot U., Allen P., Adsay V., Scott S.N., Shah R., Berger M.F., Askan G., Dikoglu E., et al. The oncocytic subtype is genetically distinct from other pancreatic intraductal papillary mucinous neoplasm subtypes. Modern Pathol. 2016;29:1058–1069. doi: 10.1038/modpathol.2016.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Pea A., Yu J., Rezaee N., Luchini C., He J., dal Molin M., Griffin J.F., Fedor H., Fesharakizadeh S., Salvia R., et al. Targeted DNA Sequencing Reveals Patterns of Local Progression in the Pancreatic Remnant Following Resection of Intraductal Papillary Mucinous Neoplasm (IPMN) of the Pancreas. Ann. Surg. 2016 doi: 10.1097/SLA.0000000000001817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Gleeson F.C., Kerr S.E., Kipp B.R., Voss J.S., Minot D.M., Tu Z.J., Henry M.R., Graham R.P., Vasmatzis G., Cheville J.C., et al. Targeted next generation sequencing of endoscopic ultrasound acquired cytology from ampullary and pancreatic adenocarcinoma has the potential to aid patient stratification for optimal therapy selection. Oncotarget. 2016;7:54526–54536. doi: 10.18632/oncotarget.9440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wright G.P., Chesla D.W., Chung M.H. Using next-generation sequencing to determine potential molecularly guided therapy options for patients with resectable pancreatic adenocarcinoma. Am. J. Surg. 2016;211:506–511. doi: 10.1016/j.amjsurg.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 134.Amato E., Molin M.D., Mafficini A., Yu J., Malleo G., Rusev B., Fassan M., Antonello D., Sadakari Y., Castelli P., et al. Targeted next-generation sequencing of cancer genes dissects the molecular profiles of intraductal papillary neoplasms of the pancreas. J. Pathol. 2014;233:217–227. doi: 10.1002/path.4344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Chantrill L.A., Nagrial A.M., Watson C., Johns A.L., Martyn-Smith M., Simpson S., Mead S., Jones M.D., Samra J.S., Gill A.J., et al. Precision Medicine for Advanced Pancreas Cancer: The Individualized Molecular Pancreatic Cancer Therapy (IMPaCT) Trial. Clin. Cancer Res. 2015;21:2029–2037. doi: 10.1158/1078-0432.CCR-15-0426. [DOI] [PubMed] [Google Scholar]
- 136.Le Tourneau C., Delord J.P., Goncalves A., Gavoille C., Dubot C., Isambert N., Campone M., Tredan O., Massiani M.A., Mauborgne C., et al. Molecularly targeted therapy based on tumour molecular profiling versus conventional therapy for advanced cancer (SHIVA): A multicentre, open-label, proof-of-concept, randomised, controlled phase 2 trial. Lancet Oncol. 2015;16:1324–1334. doi: 10.1016/S1470-2045(15)00188-6. [DOI] [PubMed] [Google Scholar]
- 137.Valero V., 3rd, Saunders T.J., He J., Weiss M.J., Cameron J.L., Dholakia A., Wild A.T., Shin E.J., Khashab M.A., O’Broin-Lennon A.M., et al. Reliable Detection of Somatic Mutations in Fine Needle Aspirates of Pancreatic Cancer with Next-generation Sequencing: Implications for Surgical Management. Ann. Surg. 2016;263:153–161. doi: 10.1097/SLA.0000000000001156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.De Biase D., Visani M., Baccarini P., Polifemo A.M., Maimone A., Fornelli A., Giuliani A., Zanini N., Fabbri C., Pession A., et al. Next generation sequencing improves the accuracy of KRAS mutation analysis in endoscopic ultrasound fine needle aspiration pancreatic lesions. PLoS ONE. 2014;9:87651. doi: 10.1371/journal.pone.0087651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Sibinga Mulder B.G., Mieog J.S., Handgraaf H.J., Farina Sarasqueta A., Vasen H.F., Potjer T.P., Swijnenburg R.J., Luelmo S.A., Feshtali S., Inderson A., et al. Targeted next-generation sequencing of FNA-derived DNA in pancreatic cancer. J. Clin. Pathol. 2016 doi: 10.1136/jclinpath-2016-203928. [DOI] [PubMed] [Google Scholar]
- 140.Roukos D.H. Crossroad between linear and nonlinear transcription concepts in the discovery of next-generation sequencing systems-based anticancer therapies. Drug Discov. Today. 2016;21:663–673. doi: 10.1016/j.drudis.2016.02.008. [DOI] [PubMed] [Google Scholar]
- 141.Jia D., Dong R., Jing Y., Xu D., Wang Q., Chen L., Li Q., Huang Y., Zhang Y., Zhang Z., et al. Exome sequencing of hepatoblastoma reveals novel mutations and cancer genes in the Wnt pathway and ubiquitin ligase complex. Hepatology. 2014;60:1686–1696. doi: 10.1002/hep.27243. [DOI] [PubMed] [Google Scholar]
- 142.Huang J., Deng Q., Wang Q., Li K.Y., Dai J.H., Li N., Zhu Z.D., Zhou B., Liu X.Y., Liu R.F., et al. Exome sequencing of hepatitis B virus-associated hepatocellular carcinoma. Nat. Genet. 2012;44:1117–1121. doi: 10.1038/ng.2391. [DOI] [PubMed] [Google Scholar]
- 143.Ki Kim S., Ueda Y., Hatano E., Kakiuchi N., Takeda H., Goto T., Shimizu T., Yoshida K., Ikura Y., Shiraishi Y., et al. TERT promoter mutations and chromosome 8p loss are characteristic of nonalcoholic fatty liver disease-related hepatocellular carcinoma. Int. J. Cancer. 2016;139:2512–2518. doi: 10.1002/ijc.30379. [DOI] [PubMed] [Google Scholar]
- 144.Jiao Y., Yonescu R., Offerhaus G.J., Klimstra D.S., Maitra A., Eshleman J.R., Herman J.G., Poh W., Pelosof L., Wolfgang C.L., et al. Whole-exome sequencing of pancreatic neoplasms with acinar differentiation. J. Pathol. 2014;232:428–435. doi: 10.1002/path.4310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Guichard C., Amaddeo G., Imbeaud S., Ladeiro Y., Pelletier L., Maad I.B., Calderaro J., Bioulac-Sage P., Letexier M., Degos F., et al. Integrated analysis of somatic mutations and focal copy-number changes identifies key genes and pathways in hepatocellular carcinoma. Nat. Genet. 2012;44:694–698. doi: 10.1038/ng.2256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Dal Molin M., Zhang M., de Wilde R.F., Ottenhof N.A., Rezaee N., Wolfgang C.L., Blackford A., Vogelstein B., Kinzler K.W., Papadopoulos N., et al. Very Long-term Survival Following Resection for Pancreatic Cancer Is Not Explained by Commonly Mutated Genes: Results of Whole-Exome Sequencing Analysis. Clin. Cancer Res. 2015;21:1944–1950. doi: 10.1158/1078-0432.CCR-14-2600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Cornella H., Alsinet C., Sayols S., Zhang Z., Hao K., Cabellos L., Hoshida Y., Villanueva A., Thung S., Ward S.C., et al. Unique genomic profile of fibrolamellar hepatocellular carcinoma. Gastroenterology. 2015;148:806–810. doi: 10.1053/j.gastro.2014.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Cleary S.P., Jeck W.R., Zhao X., Chen K., Selitsky S.R., Savich G.L., Tan T.X., Wu M.C., Getz G., Lawrence M.S., et al. Identification of driver genes in hepatocellular carcinoma by exome sequencing. Hepatology. 2013;58:1693–1702. doi: 10.1002/hep.26540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Biankin A.V., Waddell N., Kassahn K.S., Gingras M.C., Muthuswamy L.B., Johns A.L., Miller D.K., Wilson P.J., Patch A.M., Wu J., et al. Pancreatic cancer genomes reveal aberrations in axon guidance pathway genes. Nature. 2012;491:399–405. doi: 10.1038/nature11547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Sausen M., Phallen J., Adleff V., Jones S., Leary R.J., Barrett M.T., Anagnostou V., Parpart-Li S., Murphy D., Kay Li Q., et al. Clinical implications of genomic alterations in the tumour and circulation of pancreatic cancer patients. Nat. Commun. 2015;6:7686. doi: 10.1038/ncomms8686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Witkiewicz A.K., McMillan E.A., Balaji U., Baek G., Lin W.C., Mansour J., Mollaee M., Wagner K.U., Koduru P., Yopp A., et al. Whole-exome sequencing of pancreatic cancer defines genetic diversity and therapeutic targets. Nat. Commun. 2015;6:6744. doi: 10.1038/ncomms7744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Sia D., Losic B., Moeini A., Cabellos L., Hao K., Revill K., Bonal D., Miltiadous O., Zhang Z., Hoshida Y., et al. Massive parallel sequencing uncovers actionable FGFR2-PPHLN1 fusion and ARAF mutations in intrahepatic cholangiocarcinoma. Nat. Commun. 2015;6:6087. doi: 10.1038/ncomms7087. [DOI] [PubMed] [Google Scholar]
- 153.Ahn S.M., Jang S.J., Shim J.H., Kim D., Hong S.M., Sung C.O., Baek D., Haq F., Ansari A.A., Lee S.Y., et al. Genomic portrait of resectable hepatocellular carcinomas: Implications of RB1 and FGF19 aberrations for patient stratification. Hepatology. 2014;60:1972–1982. doi: 10.1002/hep.27198. [DOI] [PubMed] [Google Scholar]
- 154.Schulze K., Imbeaud S., Letouze E., Alexandrov L.B., Calderaro J., Rebouissou S., Couchy G., Meiller C., Shinde J., Soysouvanh F., et al. Exome sequencing of hepatocellular carcinomas identifies new mutational signatures and potential therapeutic targets. Nat. Genet. 2015;47:505–511. doi: 10.1038/ng.3252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Totoki Y., Tatsuno K., Covington K.R., Ueda H., Creighton C.J., Kato M., Tsuji S., Donehower L.A., Slagle B.L., Nakamura H., et al. Trans-ancestry mutational landscape of hepatocellular carcinoma genomes. Nat. Genet. 2014;46:1267–1273. doi: 10.1038/ng.3126. [DOI] [PubMed] [Google Scholar]
- 156.Liang W.S., Craig D.W., Carpten J., Borad M.J., Demeure M.J., Weiss G.J., Izatt T., Sinari S., Christoforides A., Aldrich J., et al. Genome-wide characterization of pancreatic adenocarcinoma patients using next generation sequencing. PLoS ONE. 2012;7:43192. doi: 10.1371/journal.pone.0043192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Ouyang L., Lee J., Park C.K., Mao M., Shi Y., Gong Z., Zheng H., Li Y., Zhao Y., Wang G., et al. Whole-genome sequencing of matched primary and metastatic hepatocellular carcinomas. BMC Med. Genom. 2014;7:2. doi: 10.1186/1755-8794-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Darcy D.G., Chiaroni-Clarke R., Murphy J.M., Honeyman J.N., Bhanot U., LaQuaglia M.P., Simon S.M. The genomic landscape of fibrolamellar hepatocellular carcinoma: Whole genome sequencing of ten patients. Oncotarget. 2015;6:755–770. doi: 10.18632/oncotarget.2712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Shiraishi Y., Fujimoto A., Furuta M., Tanaka H., Chiba K., Boroevich K.A., Abe T., Kawakami Y., Ueno M., Gotoh K., et al. Integrated analysis of whole genome and transcriptome sequencing reveals diverse transcriptomic aberrations driven by somatic genomic changes in liver cancers. PLoS ONE. 2014;9:114263. doi: 10.1371/journal.pone.0114263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Fujimoto A., Totoki Y., Abe T., Boroevich K.A., Hosoda F., Nguyen H.H., Aoki M., Hosono N., Kubo M., Miya F., et al. Whole-genome sequencing of liver cancers identifies etiological influences on mutation patterns and recurrent mutations in chromatin regulators. Nat. Genet. 2012;44:760–764. doi: 10.1038/ng.2291. [DOI] [PubMed] [Google Scholar]
- 161.Jhunjhunwala S., Jiang Z., Stawiski E.W., Gnad F., Liu J., Mayba O., Du P., Diao J., Johnson S., Wong K.F., et al. Diverse modes of genomic alteration in hepatocellular carcinoma. Genome Biol. 2014;15:36. doi: 10.1186/s13059-014-0436-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Sung W.K., Zheng H., Li S., Chen R., Liu X., Li Y., Lee N.P., Lee W.H., Ariyaratne P.N., Tennakoon C., et al. Genome-wide survey of recurrent HBV integration in hepatocellular carcinoma. Nat. Genet. 2012;44:765–769. doi: 10.1038/ng.2295. [DOI] [PubMed] [Google Scholar]
- 163.Fujimoto A., Furuta M., Shiraishi Y., Gotoh K., Kawakami Y., Arihiro K., Nakamura T., Ueno M., Ariizumi S., Nguyen H.H., et al. Whole-genome mutational landscape of liver cancers displaying biliary phenotype reveals hepatitis impact and molecular diversity. Nat. Commun. 2015;6:6120. doi: 10.1038/ncomms7120. [DOI] [PubMed] [Google Scholar]
- 164.Waddell N., Pajic M., Patch A.M., Chang D.K., Kassahn K.S., Bailey P., Johns A.L., Miller D., Nones K., Quek K., et al. Whole genomes redefine the mutational landscape of pancreatic cancer. Nature. 2015;518:495–501. doi: 10.1038/nature14169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Kim N.W., Piatyszek M.A., Prowse K.R., Harley C.B., West M.D., Ho P.L., Coviello G.M., Wright W.E., Weinrich S.L., Shay J.W. Specific association of human telomerase activity with immortal cells and cancer. Science. 1994;266:2011–2015. doi: 10.1126/science.7605428. [DOI] [PubMed] [Google Scholar]
- 166.Sundin T., Hentosh P. InTERTesting association between telomerase, mTOR and phytochemicals. Expert Rev. Mol. Med. 2012;14:8. doi: 10.1017/erm.2012.1. [DOI] [PubMed] [Google Scholar]
- 167.Zanetti M. A second chance for telomerase reverse transcriptase in anticancer immunotherapy. Nat. Rev. 2016 doi: 10.1038/nrclinonc.2016.67. [DOI] [PubMed] [Google Scholar]
- 168.Rosenberg S.A. A new era for cancer immunotherapy based on the genes that encode cancer antigens. Immunity. 1999;10:281–287. doi: 10.1016/S1074-7613(00)80028-X. [DOI] [PubMed] [Google Scholar]
- 169.Dallas P.B., Pacchione S., Wilsker D., Bowrin V., Kobayashi R., Moran E. The human SWI-SNF complex protein p270 is an ARID family member with non-sequence-specific DNA binding activity. Mol. Cell. Biol. 2000;20:3137–3146. doi: 10.1128/MCB.20.9.3137-3146.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Hu G., Schones D.E., Cui K., Ybarra R., Northrup D., Tang Q., Gattinoni L., Restifo N.P., Huang S., Zhao K. Regulation of nucleosome landscape and transcription factor targeting at tissue-specific enhancers by BRG1. Genome Res. 2011;21:1650–1658. doi: 10.1101/gr.121145.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Kassabov S.R., Zhang B., Persinger J., Bartholomew B. SWI/SNF unwraps, slides, and rewraps the nucleosome. Mol. Cell. 2003;11:391–403. doi: 10.1016/S1097-2765(03)00039-X. [DOI] [PubMed] [Google Scholar]
- 172.Tolstorukov M.Y., Sansam C.G., Lu P., Koellhoffer E.C., Helming K.C., Alver B.H., Tillman E.J., Evans J.A., Wilson B.G., Park P.J., et al. Swi/Snf chromatin remodeling/tumor suppressor complex establishes nucleosome occupancy at target promoters. Proc. Natl. Acad. Sci. USA. 2013;110:10165–10170. doi: 10.1073/pnas.1302209110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Watanabe R., Ui A., Kanno S., Ogiwara H., Nagase T., Kohno T., Yasui A. SWI/SNF factors required for cellular resistance to DNA damage include ARID1A and ARID1B and show interdependent protein stability. Cancer Res. 2014;74:2465–2475. doi: 10.1158/0008-5472.CAN-13-3608. [DOI] [PubMed] [Google Scholar]
- 174.Li M., Zhao H., Zhang X., Wood L.D., Anders R.A., Choti M.A., Pawlik T.M., Daniel H.D., Kannangai R., Offerhaus G.J., et al. Inactivating mutations of the chromatin remodeling gene ARID2 in hepatocellular carcinoma. Nat. Genet. 2011;43:828–829. doi: 10.1038/ng.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Shain A.H., Giacomini C.P., Matsukuma K., Karikari C.A., Bashyam M.D., Hidalgo M., Maitra A., Pollack J.R. Convergent structural alterations define SWItch/Sucrose NonFermentable (SWI/SNF) chromatin remodeler as a central tumor suppressive complex in pancreatic cancer. Proc. Natl. Acad. Sci. USA. 2012;109:252–259. doi: 10.1073/pnas.1114817109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Varela I., Tarpey P., Raine K., Huang D., Ong C.K., Stephens P., Davies H., Jones D., Lin M.L., Teague J., et al. Exome sequencing identifies frequent mutation of the SWI/SNF complex gene PBRM1 in renal carcinoma. Nature. 2011;469:539–542. doi: 10.1038/nature09639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Versteege I., Sevenet N., Lange J., Rousseau-Merck M.F., Ambros P., Handgretinger R., Aurias A., Delattre O. Truncating mutations of hSNF5/INI1 in aggressive paediatric cancer. Nature. 1998;394:203–206. doi: 10.1038/28212. [DOI] [PubMed] [Google Scholar]
- 178.Wiegand K.C., Shah S.P., Al-Agha O.M., Zhao Y., Tse K., Zeng T., Senz J., McConechy M.K., Anglesio M.S., Kalloger S.E., et al. ARID1A mutations in endometriosis-associated ovarian carcinomas. N. Engl. J. Med. 2010;363:1532–4153. doi: 10.1056/NEJMoa1008433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Shain A.H., Pollack J.R. The spectrum of SWI/SNF mutations, ubiquitous in human cancers. PLoS ONE. 2013;8:55119. doi: 10.1371/journal.pone.0055119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Wang K., Kan J., Yuen S.T., Shi S.T., Chu K.M., Law S., Chan T.L., Kan Z., Chan A.S., Tsui W.Y., et al. Exome sequencing identifies frequent mutation of ARID1A in molecular subtypes of gastric cancer. Nat. Genet. 2011;43:1219–1223. doi: 10.1038/ng.982. [DOI] [PubMed] [Google Scholar]
- 181.Bitler B.G., Aird K.M., Garipov A., Li H., Amatangelo M., Kossenkov A.V., Schultz D.C., Liu Q., Shih Ie M., Conejo-Garcia J.R., et al. Synthetic lethality by targeting EZH2 methyltransferase activity in ARID1A-mutated cancers. Nat. Med. 2015;21:231–238. doi: 10.1038/nm.3799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.He X., Zhu Z., Johnson C., Stoops J., Eaker A.E., Bowen W., de Frances M.C. PIK3IP1, a negative regulator of PI3K, suppresses the development of hepatocellular carcinoma. Cancer Res. 2008;68:5591–5598. doi: 10.1158/0008-5472.CAN-08-0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Wilson B.G., Wang X., Shen X., McKenna E.S., Lemieux M.E., Cho Y.J., Koellhoffer E.C., Pomeroy S.L., Orkin S.H., Roberts C.W. Epigenetic antagonism between polycomb and SWI/SNF complexes during oncogenic transformation. Cancer Cell. 2010;18:316–328. doi: 10.1016/j.ccr.2010.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Fillmore C.M., Xu C., Desai P.T., Berry J.M., Rowbotham S.P., Lin Y.J., Zhang H., Marquez V.E., Hammerman P.S., Wong K.K., et al. EZH2 inhibition sensitizes BRG1 and EGFR mutant lung tumours to TopoII inhibitors. Nature. 2015;520:239–242. doi: 10.1038/nature14122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Kim K.H., Roberts C.W. Targeting EZH2 in cancer. Nat. Med. 2016;22:128–134. doi: 10.1038/nm.4036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Helming K.C., Wang X., Wilson B.G., Vazquez F., Haswell J.R., Manchester H.E., Kim Y., Kryukov G.V., Ghandi M., Aguirre A.J., et al. ARID1B is a specific vulnerability in ARID1A-mutant cancers. Nat. Med. 2014;20:251–254. doi: 10.1038/nm.3480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Schulze K., Nault J.C., Villanueva A. Genetic profiling of hepatocellular carcinoma using next-generation sequencing. J. Hepatol. 2016;65:1031–1042. doi: 10.1016/j.jhep.2016.05.035. [DOI] [PubMed] [Google Scholar]
- 188.The Cancer Genome Atlas National Cancer Institute, National Human Genome Research Institute. [(accessed on 1 October 2016)]; Available online: https://cancergenome.nih.gov/
- 189.International Cancer Genome Consortium. [(accessed on 1 October 2016)]. Available online: http://icgc.org/
- 190.Roychowdhury S., Chinnaiyan A.M. Translating cancer genomes and transcriptomes for precision oncology. CA Cancer J. Clin. 2016;66:75–88. doi: 10.3322/caac.21329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Xue R., Li R., Guo H., Guo L., Su Z., Ni X., Qi L., Zhang T., Li Q., Zhang Z., et al. Variable Intra-Tumor Genomic Heterogeneity of Multiple Lesions in Patients With Hepatocellular Carcinoma. Gastroenterology. 2016;150:998–1008. doi: 10.1053/j.gastro.2015.12.033. [DOI] [PubMed] [Google Scholar]
- 192.Gao Q., Wang Z.C., Duan M., Lin Y.H., Zhou X.Y., Worthley D.L., Wang X.Y., Niu G., Xia Y., Deng M., et al. Cell Culture System for Analysis of Genetic Heterogeneity Within Hepatocellular Carcinomas and Response to Pharmacologic Agents. Gastroenterology. 2016 doi: 10.1053/j.gastro.2016.09.008. accepted. [DOI] [PubMed] [Google Scholar]
- 193.Eirew P., Steif A., Khattra J., Ha G., Yap D., Farahani H., Gelmon K., Chia S., Mar C., Wan A., et al. Dynamics of genomic clones in breast cancer patient xenografts at single-cell resolution. Nature. 2015;518:422–426. doi: 10.1038/nature13952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Murtaza M., Dawson S.J., Tsui D.W., Gale D., Forshew T., Piskorz A.M., Parkinson C., Chin S.F., Kingsbury Z., Wong A.S., et al. Non-invasive analysis of acquired resistance to cancer therapy by sequencing of plasma DNA. Nature. 2013;497:108–112. doi: 10.1038/nature12065. [DOI] [PubMed] [Google Scholar]