Abstract
Spontaneous osteonecrosis of the knee (SONK) is a feared condition of unknown cause, in its classic form appearing in the medial femoral condyle in middle-aged or elderly subjects. Diagnosis with radiography is notoriously difficult with a long latency before typical changes appear. Magnetic resonance imaging (MRI) is regarded as a diagnostic tool with the possibility to give an earlier diagnosis with improved chances for treatment. However, also with MRI there may be an initial diagnostic blind spot before typical changes appear. Little is known about the temporal evolution of the MRI changes. In the current case report, a case of SONK is reported where serial imaging with MRI was performed, from initial symptoms to eventual resolution after almost three years.
Keywords: Osteonecrosis, knee, magnetic resonance imaging (MRI)
Introduction
Osteonecrosis or avascular necrosis is the end stage of multiple pathological pathways leading to impaired intraosseous circulation, resulting in infarction of bone. Osteonecrotic lesions are usually painful although “silent” forms have been described (1) and often lead to secondary osteoarthritic changes if they occur in the subchondral bone with subsequent collapse of the joint surface (2). Osteonecrosis of the knee is also strongly associated with an increased risk of joint arthroplasty (2).
Today, osteonecrosis of the knee is often discussed in terms of three separate conditions (3): (i) spontaneous osteonecrosis of the knee (SONK), the subject of the current case report, usually affecting a single condyle in middle-aged or older patients; (ii) secondary osteonecrosis from a known cause, such as corticosteroid treatment or sickle-cell anemia, more often affecting younger patients, with multifocal and sometimes asymptomatic “silent” lesions; and (iii) post-arthroscopy osteonecrosis, characterized by increasing knee pain and positive magnetic resonance imaging (MRI) findings after arthroscopic surgery (4).
The etiology of SONK is unknown, but two main theories have been advanced: vascular (5,6) and traumatic, resulting from a microfracture perhaps in association with low bone mineral density (7). SONK can lead to subchondral collapse and secondary osteoarthritis often requiring knee surgery (2). The prognosis of the disease, has been shown to depend on the size of the lesion (8).
The onset of SONK is classically an acute onset of pain without a significant predisposing trauma. Some patients, however, describe a more gradual increase of symptoms. The most common finding on physical examination is localized tenderness over the medial femoral condyle. Initial radiographs may be negative, especially if the symptoms are of short duration, and the diagnosis is therefore often missed at this stage (8,9). With time, radiography shows a characteristic half-moon-shaped sclerosis with a radiolucent center adjacent to the joint surface (10), followed by a joint surface impression. MRI can diagnose SONK in the pre-radiographic stage (11), with increased potential for treatment to prevent joint surface collapse.
Proper treatment depends on a high degree of clinical suspicion and prompt imaging with radiography as well as MRI. With negative radiography and diagnostic MRI prognosis is better with the primary treatment objective to preserve joint congruence, and avoid a dismal prognosis with arthroplasty as the outcome. MRI may be used to monitor treatment, but the MRI appearance from onset to resolution has not previously been documented in serial imaging.
The purpose of the current report was to describe the MRI findings in a case of SONK imaged repeatedly during 2.5 years.
Case report
A 55-year-old man presented with gradually worsening throbbing pain in the medial half of the knee, which changed into a stabbing pain with weight bearing. He had no prior health complaints, was not on any medication, did not smoke, and practiced moderate exercise with jogging 5 km twice a week. Physical examination was unremarkable with only mild swelling and effusion. Three weeks earlier he had walked a lot on hard surfaces and also been in a minor car accident without obvious knee trauma. MRI showed non-specific bone marrow edema (Fig. 1). All MR examinations were performed on a 1.5 T Achieva scanner (Philips, Best, The Netherlands) with a standard knee protocol (Table 1).
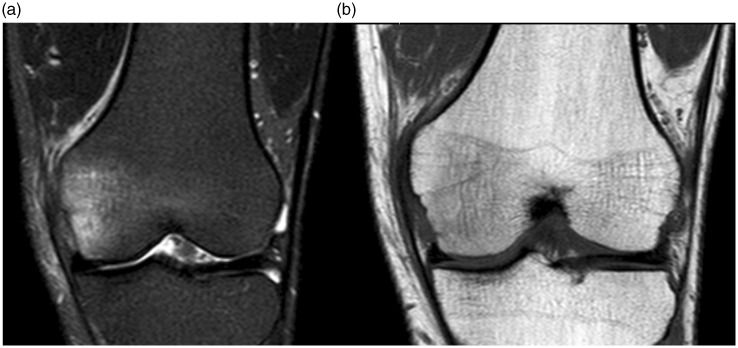
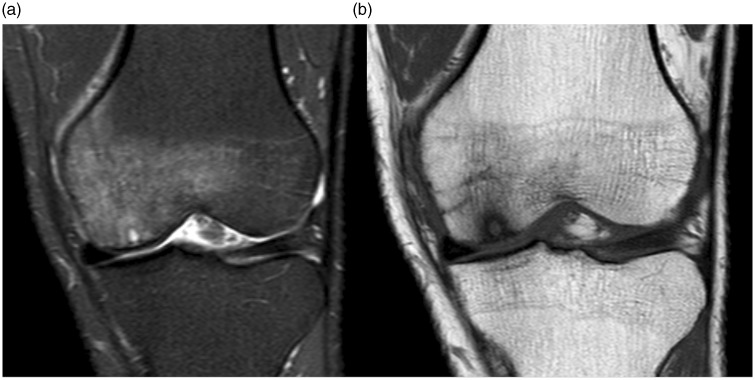
Fig. 1.
MRI at presentation, three weeks after symptom onset. (a) Coronal STIR and (b) coronal T1W images. There was bone marrow edema mostly in the medial half of the medial femoral condyle, otherwise milder and more diffuse in the rest of the condyle, with an appearance more suggestive of contusion than of osteonecrosis. No specific trauma preceded the symptoms, however, the patient had been walking a lot on hard surfaces three weeks earlier.
Table 1.
Standard protocol for knee MRI. The coronal STIR sequence was exchanged for the coronal PD SPAIR sequence in the two last examinations.
| Scan sequence | Scan plane | TR | TE | Section thickness (mm) | Gap (mm) |
|---|---|---|---|---|---|
| TSE T1W | Coronal | 560 | 17 | 3 | 0.6 |
| STIR | Coronal | 3912 | 30 | 3 | 0.6 |
| PD | Sagittal | 4500 | 30 | 3 | 0.3 |
| PD SPAIR | Axial | 3423 | 30 | 3 | 0.3 |
| PD SPAIR | Coronal | 3500 | 30 | 3 | 0.3 |
PD, proton density; SPAIR, spectral attenuated inversion recovery; STIR, short tau inversion recovery; T1W, T1-weighted; TE, echo time; TR, repetition time; TSE, turbo spin-echo.
At follow-up MRI after three weeks (Fig. 2) the bone marrow edema had increased both in intensity and extension, and was suggestive of osteonecrosis. A small subchondral sclerosis had also appeared in the medial femoral condyle on T1-weighted (T1W) imaging. Radiography was unremarkable. Combined, the two MRI studies were, however, interpreted as a possible insufficiency fracture. Treatment was now started with non-steroidal anti-inflammatory drugs (NSAID) and protected weight bearing.
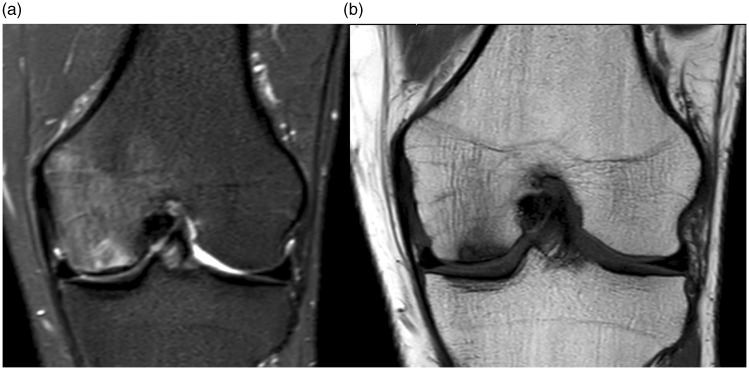
Fig. 2.
MRI three weeks after presentation. (a) Coronal STIR and (b) coronal T1W images. Increase of bone marrow edema both in intensity and extension, with the edema on sagittal images (not shown) now centered around the weight bearing area of the medial femoral condyle, suggestive of osteonecrosis.
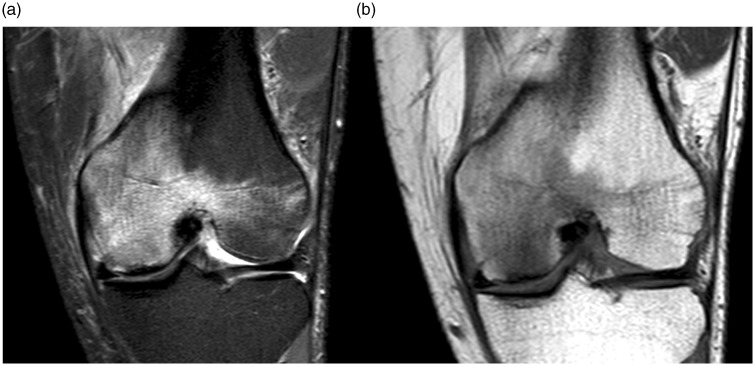
MRI at three months showed unaltered distribution but further progression of signal intensity of the bone marrow edema (Fig. 3). Knee pain was reduced to 20% of the previous pain intensity by the patient’s own assessment. Pain and swelling, however, increased with weight bearing, the patient had difficulties in driving a car due to the knee pain, and there was a mild effusion. Treatment with physiotherapy was started and protected weight bearing continued.
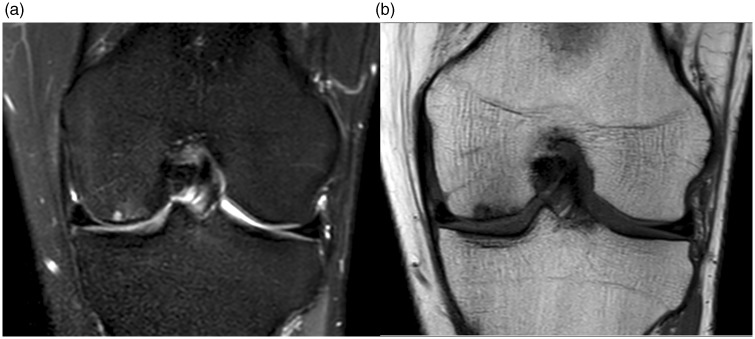
Fig. 3.
MRI at three months. (a) Coronal STIR, (b) coronal T1W, (c) sagittal PD-weighted images. Further progression of signal intensity of the bone marrow edema on a STIR sequence with stable distribution. On the sagittal T1W images a double sclerotic line (arrow) could be seen in the subchondral weight-bearing area.
At five months, MRI showed subtotal regression of the bone marrow edema (Fig. 4). The findings were now interpreted as osteonecrosis. Treatment with a bisphosphonate (alendronic acid 70 mg orally/week) was started, with continued protected weight bearing.
Fig. 4.
MRI at five months. (a) Coronal STIR and (b) coronal T1W images. Subtotal regression of the bone marrow edema on coronal STIR images. The subchondral double line was still present on sagittal T1W images (not shown), and a small cystic area with minimal impression and flattening of the joint surface on the weight-bearing area of the medial femoral condyle had appeared (arrows). The findings were now interpreted as osteonecrosis.
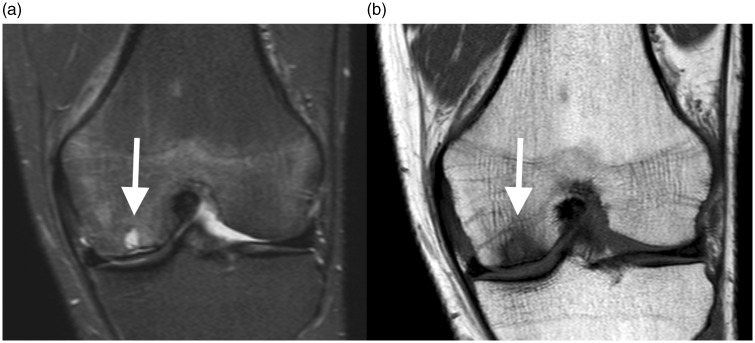
MRI at seven months (Fig. 5) showed slight progression of the subchondral cystic area and reappearance of a discrete bone marrow edema. The clinical findings were stable. At ten months, MRI showed further slight progression of the bone marrow edema, but with filling out of the cyst (Fig. 6). The bisphosphonate treatment was now changed to zoledronic acid (5 mg intravenously/6 months). At the clinical visit at one year follow-up, there was no change in clinical findings.
Fig. 5.
MRI at seven months. (a) Coronal STIR and (b) coronal T1W images. Slight progression of the subchondral cystic area and reappearance of a discrete bone marrow edema.
Fig. 6.
MRI at ten months. (a) Coronal STIR and (b) coronal T1W images. Further slight progression of bone marrow edema, with filling out of the cyst, discernible on T1W images.
At one year and three months a minimal subchondral lucency had appeared at radiography (Fig. 7), while MRI (Fig. 8) showed further healing of the cyst. There was still mild knee pain, which increased with weight bearing and flexion of the knee. On physical examination, there was some swelling and effusion. Treatment was continued with zoledronic acid (total treatment time with bisphosphonates 1.5 years) and protected weight bearing.
Fig. 7.
Radiography at one year and three months. Minimal subchondral lucency with preserved joint congruency and joint space width.
Fig. 8.
MRI at one year and three months. (a) Coronal STIR and (b) coronal T1W images. Unchanged bone marrow edema on STIR images and further filling out of the cyst on T1W images.
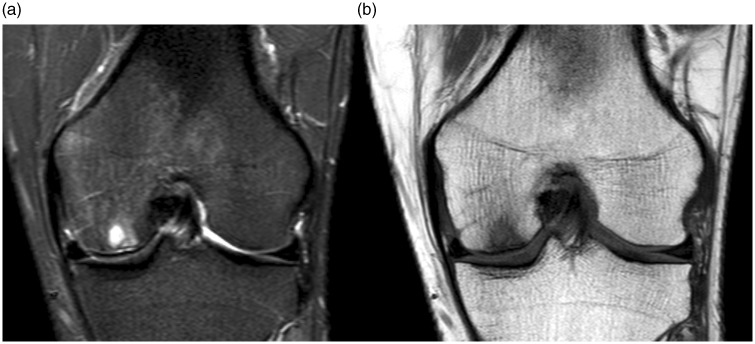
At one year and nine months, MRI showed minimal remaining subchondral edema (Fig. 9). The pain was reduced but moderate muscular atrophy had developed. The final MRI at two years and six months (Fig. 10) showed further healing, also at radiography.
Fig. 9.
MRI at one year and nine months. (a) Coronal fat-suppressed PD-weighted and (b) coronal T1W images. Minimal remaining subchondral edema on fat-suppressed PD-weighted images with mildly irregular trabecular structure at the location of the former cyst.
Fig. 10.
MRI at two years and six months. (a) Coronal fat-suppressed PD-weighted and (b) coronal T1W images. Further healing on fat-suppressed PD-weighted images with disappearance of bone marrow edema with remaining small subchondral irregularities, preserved joint surfaces and cartilage.
Discussion
The current case report describes serial imaging with MRI in a patient with SONK, with gradual onset and slowly worsening pain changing into stabbing pain on weight bearing, different from the sudden onset often associated with SONK (9). There was a delay of five months before a diagnosis of SONK was made. However, more gradual or silent onset has been described (1), and in the current case, intensive and frequent walking during one week might be suspected as the cause of microtrauma to the femoral condyle leading to SONK.
The first MRI after three weeks was inconclusive, and only after six weeks could a mild subchondral sclerosis be seen on the T1W images. Often, there is a diagnostic window where MRI may be negative (12), and it has been suggested that this “diagnostic window” may last up to six weeks (13). In the current case, there was initial quick resolution of the widespread bone marrow edema, but changes remained even after 2.5 years. At the last follow-up, there were only minimal radiographic changes, presumably indicating a good prognosis (9,14).
There are several differential diagnoses for painful bone marrow edema on MRI other than SONK. As in the current case, post-traumatic bone marrow edema can be suspected, such as bone contusion, microfracture, stress fracture, or other stress-related bone marrow edema (15). Other differential diagnoses are bone marrow edema syndrome, osteochondritis dissecans, or Sudeck atrophy, while other more obvious differential diagnoses are osteoarthritis, tumor-related bone marrow edema, and postoperative changes (15).
To the authors’ knowledge, this is the first report of serial imaging with MRI in SONK. The evolution of findings in the current case is similar to previously reported follow-up imaging such as in one report (16) where a subchondral cyst had developed at nine months, similar to the appearance of the current case at five months. In another study (17), initially mild findings such as in the current report eight months later had progressed into an impression fracture in the femoral condyle, illustrating the importance of not neglecting early mild changes. Previous studies have reported on the characteristic appearance of SONK on MRI, with bone marrow edema of high intensity on water-sensitive sequences such as short tau inversion recovery (STIR) or fat-suppressed T2 or proton density (PD)-weighted sequences, with focal or diffuse T1 hypointensity in the subchondral area, most commonly in the medial femoral condyle (18). On T1W sequences the necrotic focus is shown as a low signal area often with a surrounding area of intermediate signal intensity, corresponding to the bone marrow edema seen on water-sensitive sequences. Often there is a serpiginous dark line at the margin of the necrotic area, delineating it from the area of bone marrow edema. Ramnath and Kattapuram (18) suggested that a linear component parallel with the joint surface corresponds to an underlying insufficiency fracture plane and also reported that a severe bone marrow edema with an extension greater than two-thirds of the area of the condyle or plateau, both of which were present in the current case, was a prevalent feature.
Treatment with protected weight bearing is a standard treatment to avoid collapse of the subchondral bone in osteonecrosis before healing is complete (3). The beneficial effects of bisphosphonate treatment have been shown in several series, e.g. (14) resulting in less osteoarthritis and less bone collapse compared with untreated series (9), thereby reducing the need for knee arthroplasty.
Based on the evolution of findings the authors of the current report recommend diagnosis and staging with radiography and MRI after onset and repeated after two months if negative with remaining symptoms, repeat imaging if worsening symptoms despite treatment, and final imaging with MRI and possibly radiography 2–3 years after onset for prognostic evaluation, unless worsening symptoms have prompted an earlier intervention.
In conclusion, the current case report demonstrates the timeline with appearance and disappearance of bone marrow edema in a case of SONK, followed by cyst formation and eventual healing. Treatment with protected weight bearing and bisphosphonates was, in this case, believed to have contributed to a favorable outcome.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Bradway JK, Morrey BF. The natural history of the silent hip in bilateral atraumatic osteonecrosis. J Arthroplasty 1993; 8: 383–387. [DOI] [PubMed] [Google Scholar]
- 2.Juréus J, Lindstrand A, Geijer M, et al. The natural course of spontaneous osteonecrosis of the knee (SPONK). A 1- to 27-year follow-up of 40 patients. Acta Orthop 2013; 84: 410–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zywiel MG, McGrath MS, Seyler TM, et al. Osteonecrosis of the knee: a review of three disorders. Orthop Clin North Am 2009; 40: 193–211. [DOI] [PubMed] [Google Scholar]
- 4.Kraenzlin ME, Graf C, Meier C, et al. Possible beneficial effect of bisphosphonates in osteonecrosis of the knee. Knee Surgery, Sport Traumatol Arthrosc 2010; 18: 1638–1644. [DOI] [PubMed] [Google Scholar]
- 5.Kantor H. Bone marrow pressure in osteonecrosis of the femoral condyle (Ahlback’s disease). Arch Orthop Trauma Surg 1987; 106: 349–352. [DOI] [PubMed] [Google Scholar]
- 6.Jones JP. Fat embolism, intravascular coagulation, and osteonecrosis. Clin Orthop Relat Res 1993, pp. 294–308. [PubMed] [Google Scholar]
- 7.Akamatsu Y, Mitsugi N, Hayashi T, et al. Low bone mineral density is associated with the onset of spontaneous osteonecrosis of the knee. Acta Orthop 2012; 83: 249–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lotke PA, Abend JA, Ecker ML. The treatment of osteonecrosis of the medial femoral condyle. Clin Orthop Relat Res 1982, pp. 109–116. [PubMed] [Google Scholar]
- 9.Al-Rowaih A, Lindstrand A, Björkengren A, et al. Osteonecrosis of the knee. Diagnosis and outcome in 40 patients. Acta Orthop Scand 1991; 62: 19–23. [DOI] [PubMed] [Google Scholar]
- 10.Lotke PA, Ecker ML. Osteonecrosis of the knee. J Bone Jt Surg Am 1988; 70: 470–473. [PubMed] [Google Scholar]
- 11.Koshino T. The treatment of spontaneous osteonecrosis of the knee by high tibial osteotomy with and without bone-grafting or drilling of the lesion. J Bone Jt Surg [Am] 1982; 64: 47–58. [PubMed] [Google Scholar]
- 12.Johnson TC, Evans JA, Gilley JA, et al. Osteonecrosis of the knee after arthroscopic surgery for meniscal tears and chondral lesions. Arthroscopy 2000; 16: 254–261. [DOI] [PubMed] [Google Scholar]
- 13.Pape D, Hoffmann A, Kohn D. [Femoral osteonecrosis - Ahlbaeck’s disease]. In German. Radiologe 2012;52:1023–1029. [DOI] [PubMed]
- 14.Juréus J, Lindstrand A, Geijer M, et al. Treatment of spontaneous osteonecrosis of the knee (SPONK) by a bisphosphonate. Acta Orthop 2012; 83: 511–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hofmann S, Kramer J, Vakil-Adli A, et al. Painful bone marrow edema of the knee: differential diagnosis and therapeutic concepts. Orthop Clin North Am 2004; 35: 321–333, ix. [DOI] [PubMed] [Google Scholar]
- 16.Jordan RW, Aparajit P, Docker C, et al. The importance of early diagnosis in spontaneous osteonecrosis of the knee - A case series with six year follow-up. Knee 2016; 23: 702–707. [DOI] [PubMed] [Google Scholar]
- 17.Viana SL, Machado BB, Mendlovitz PS. MRI of subchondral fractures: a review. Skeletal Radiol 2014; 43: 1515–1527. [DOI] [PubMed] [Google Scholar]
- 18.Ramnath RR, Kattapuram SV. MR appearance of SONK-like subchondral abnormalities in the adult knee: SONK redefined. Skeletal Radiol 2004; 33: 575–581. [DOI] [PubMed] [Google Scholar]