Abstract
Background:
Cyclops syndrome is characterized by loss of terminal knee extension due to proliferative fibrous nodule formation in the intercondylar notch. This complication occurs in the early postoperative period after anterior cruciate ligament reconstruction (ACLR). The pathogenesis of Cyclops syndrome is not well understood.
Hypothesis:
Persistent hamstring contracture after ACLR is associated with an increased risk of subsequent Cyclops syndrome.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
The files of 45 patients who underwent arthroscopic debridement of a Cyclops lesion after ACLR were analyzed. Recorded data included demographic information and technical details of surgery. Preoperative magnetic resonance images were also analyzed, and patients with femoral bone bruising were identified. Passive and active range of motion were recorded in all patients preoperatively and at 3 and 6 weeks after surgery to address the Cyclops lesion. Passive extension deficit was evaluated in comparison with the contralateral limb and classified as secondary to hamstring contracture when contracture was observed and palpated in the prone position and when the extension deficit was reversed after exercises performed to fatigue the hamstrings. A control group was selected using a random numbers table among our entire ACLR cohort. Statistical analysis was performed to analyze differences between the 2 groups.
Results:
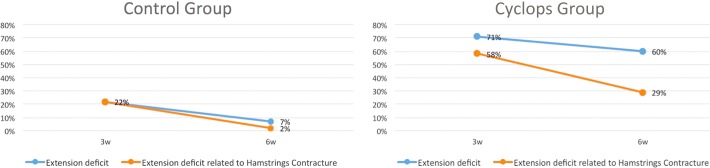
There was no significant difference between the groups with regard to age at ACLR, sex distribution, time from injury to surgery (P > .05), proportion of professional athletes, presence of femoral bone bruise, or technical aspects of surgery. The overall extension deficit incidence was significantly higher in the Cyclops group at 3 weeks (Cyclops, 71%; control, 22%) (P < .001) and at 6 weeks (Cyclops, 60%; control, 7%) (P < .001). The extension deficit related to hamstring contracture was significantly higher in the Cyclops group at 3 weeks (Cyclops, 58%; control, 22%) (P < .001) and at 6 weeks (Cyclops, 29%; control, 2%) (P < .001).
Conclusion:
The Cyclops lesion is associated with a persistent hamstring contracture at 3 and 6 weeks after ACLR.
Keywords: Cyclops syndrome, hamstring contracture, knee extension deficit, rehabilitation, anterior cruciate ligament, knee
Cyclops syndrome is characterized by loss of terminal knee extension due to proliferative fibrous nodule formation in the intercondylar notch after anterior cruciate ligament reconstruction (ACLR).7,23 It is 1 of the 4 described types of arthrofibrosis.18 A critical size seems necessary to result in observable disability.11 However, when it does occur, the functional consequences are often severe enough to warrant reoperation. In the first description of this type of lesion, Jackson and Schaefer7 stated that “Cyclops appeared in those patients who failed to regain extension early,” and more recently, a possible correlation between Cyclops syndrome and an extension deficit due to a reflex hamstring contracture after anterior cruciate ligament (ACL) surgery has been hypothesized but not clearly demonstrated.19
The purpose of this study was to analyze the correlation between immediate postoperative reflex hamstring contracture and the development of a Cyclops lesion after ACLR. Our hypothesis is that there is an association between a persistent hamstrings contracture at the early phase of ACLR and the Cyclops syndrome.
Methods
The case notes of 45 patients who underwent an arthroscopic arthrolysis for Cyclops syndrome after a primary ACLR between 2010 and 2014 were retrospectively reviewed. Both surgeries (ACLR and Cyclops) were performed by the senior author (B.S.C.). The exclusion criteria were a first surgery other than primary ACLR (all revisions were excluded) and cases with a final diagnosis other than Cyclops syndrome. To test our hypothesis, we compared our Cyclops cohort (n = 45) with a random control group taken from our ACLR universe of 2089 patients operated on in the same time period.
Recorded data included the age at first (ACLR) and second (Cyclops) surgery, the time period between ACL rupture and the ACLR, the type and level of sports in which the patient was involved, as well as all surgical technical details: type of graft, meniscal tears, and associated extra-articular tenodesis. The data from the preoperative magnetic resonance images were also analyzed, and patients with femoral bone bruising were identified.9
The clinical files after the ACLR were analyzed regarding clinical examination at 3 weeks, 6 weeks, and just before the Cyclops surgery. We registered both passive and active range of motion, and all patients were examined in prone and supine positions. Passive extension deficit was evaluated in comparison with the contralateral limb. Any extension deficit asymmetry greater than 5° was considered.
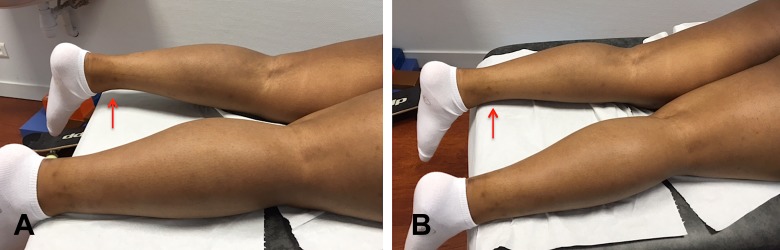
This extension deficit was classified as related to hamstring contracture when:
observation and palpation of the hamstring muscle belly in the prone position revealed a contracture;
extension deficit was improved after repeated flexion against resistance in the prone position (to obtain hamstring muscle fatigue and stunning) resulting in restoration of passive full extension symmetrical to the contralateral side (see Figure 1 and the Video Supplement).
Figure 1.
Typical extension deficit related to hamstring contracture. (A) The extension deficit can be observed in the prone position. (B) This extension deficit is reversed after resistance exercises to obtain hamstring fatigue. Arrows indicate extension deficit as visualized by the distance between the exam table and the anterior aspect of the ankle.
Once passive full extension was achieved, we required the patient to turn supine to access his or her quadriceps function through inspection and palpation, asking the patient to fully extend the knee on the bench and comparing the quadriceps contraction between both knees by symmetric palpation.
Control Group
A control group of similar size (n = 45) was selected among our entire ACLR cohort of 2089 patients without Cyclops syndrome. We used a random numbers table generated by Microsoft Excel for Windows 2013, according to Monte Carlo calculations.
Surgical Procedure
Our standard ACLR surgical technique includes high, fat pad–sparing, arthroscopic portals; full arthroscopic examination; and ACL remnant preservation. In rare cases when this was not possible (related to a poor ACL remnant), we performed an ACLR using a bone–patellar tendon–bone (BPTB) graft.4 The tibial tunnel is drilled in close to full extension to avoid missing any preoperative Cyclops due to the retraction of the ACL stump, particularly the classic bell-hammer posterolateral remnant.9 A shaver is passed through the tibial tunnel and into the remnant so that the remnant is hollowed out for passage of the graft. At the end of the ACLR, a full arthroscopic evaluation was made to check for presence or absence of graft impingement. All knees achieved full extension at the end of the procedure, and this was again clinically confirmed by the senior surgeon (B.S.C.) before the patient left the hospital. All patients were operated on under general anesthesia, without any nerve block, but with a hamstring donor site naropeine injection.1
Statistical Analysis
We analyzed the conditions of applicability of parametric tests on the numeric data: age and delay from ACL injury to ACL surgery. Normality of data was tested using the Kolmogorov-Smirnov test, which showed that the variables do not follow a normal distribution (P age = .029 and P delay < .001). For these reasons, we used the Mann-Whitney test (a nonparametric test) to compare the 2 independent samples.
For the remaining variables (all nominal), the chi-square test was used to analyze the association between the 2 groups. The Wilcoxon test was used to analyze the difference between the 2 clinical observations (at 3 and 6 weeks). All statistical tests were performed using the software SPSS Statistics Version 22 (IBM Corp).
Results
Both groups were similar (P > .05) regarding age at ACLR, sex distribution, and delay from ACL injury to ACLR surgery (Table 1). There was also a similar proportion between the 2 groups of professional athletes, presence of femoral bone bruise, type of graft (hamstring tendon [HT] or BPTB), extra-articular tenodesis, and meniscus suture. All patients had full extension before the ACLR except for 2 patients in the control group and 1 patient in the Cyclops group, all due to a bucket-handle meniscal tear.
TABLE 1.
Characteristics of Control and Cyclops Groupsa
| Variables | Control Group (n = 45) | Cyclops Group (n = 45) | Statistic |
|---|---|---|---|
| Age at ACL reconstruction (min-max), y | 31 (14-55) | 27 (13-48) | z = −1.311; P = .190 (ns) |
| Sex | 34 male, 11 female | 33 male, 12 female | χ2 = 0.058; P = .809 (ns) |
| Delay from ACL injury to surgery (min-max), mo | 3.64 (0.1-23.7) | 3.7 (0.5-22) | z = −1.178; P = .239 (ns) |
| Professional athletes, n | 3 | 5 | χ2 = 0.549; P = .459 (ns) |
| Femoral bone bruise, n | 5 | 9 | χ2 = 1.353; P = .245 (ns) |
| Type of graft | |||
| HT | 33 | 36 | χ2 = 0.559; P = .455 (ns) |
| BPTB | 12 | 9 | |
| Extra-articular tenodesis | 10 | 14 | χ2 = 0.909; P = .340 (ns) |
| Meniscus suture | 20 | 20 | χ2 = 0.000; P > .999 (ns) |
aACL, anterior cruciate ligament; BPTB, bone–patellar tendon–bone; HT, hamstring tendon; min-max, minimum-maximum; ns, nonsignificant.
There were 3 professional athletes in the control group (2 rugby players and 1 basketball player) and 5 in the Cyclops group (3 rugby players, 1 hockey player, and 1 gymnast).
We found a significant difference between the 2 groups in the incidence of extension deficit at both 3 and 6 weeks (P < .001) (Table 2). Extension deficit at 3 weeks occurred at an incidence of 71% in the Cyclops group and 22% in the control group. At 6 weeks, this difference was also significant: 60% had an extension deficit in the Cyclops group compared with 7% in the control group (P < .001).
TABLE 2.
Incidence of Extension Deficit and Hamstrings Contracture in Control and Cyclops Groups
| Extension Deficit | Control Group (n = 45) | Cyclops Group (n = 45) | Statistic |
|---|---|---|---|
| Extension deficit at 3 wk | 10 in 45 (22%) | 32 in 45 (71%) | χ2 = 21.6; P = 3.3 × 10−6a |
| Extension deficit related to hamstrings contracture at 3 wk | 10 in 45 (22%) | 26 in 45 (58%) | χ2 = 11.8; P = .0006a |
| Extension deficit at 6 wk | 3 in 45 (7%) | 27 in 45 (60%) | χ2 = 28.8; P = 8.02 ×10−8a |
| Extension deficit related to hamstrings contracture at 6 wk | 1 in 45 (2%) | 13 in 45 (29%) | χ2 = 12.2; P = .0005a |
aStatistically significant.
A significant difference was also found in the incidence of extension deficit related to hamstring contracture at 3 and 6 weeks (P < .001). Hamstring contracture was reported in 58% of the Cyclops group and in 24% of the control group (P < .001). At 6 weeks, a hamstring contracture was observed in 29% of the Cyclops group and 2% of the control group (P < .001) (Figure 2).
Figure 2.
Evolution of extension deficit and hamstrings contracture at 3 and 6 weeks in the control and Cyclops group.
The secondary Cyclops surgeries were performed at a mean of 11 months (range, 5-31 months) after the primary ACLR. Thirteen patients (20%) also underwent additional procedures besides the Cyclops lesion resection. Ten patients underwent a notchplasty, 1 had a trochlear osteochondral lesion debridement, and 2 other patients had a screw removal. There was a good clinical result in 93% (42 of 45) of patients. All of these 42 patients became asymptomatic and had full range of motion. Three other patients were not satisfied: 1 had septic arthritis after the Cyclops surgery and 2 others reported persistent anterior knee pain.
Discussion
The most important finding of this study is that, in the early phase of ACLR, the majority of extension deficits are related to hamstring contracture and that these deficits are associated with an increased incidence of Cyclops syndrome. Our data demonstrate that, at both 3 and 6 weeks, the Cyclops group had a significantly higher incidence of extension deficit and hamstrings contracture than the control group. In the control group, extension deficit related to hamstrings contracture was reported in 24% of patients at 3 weeks, but this number dropped to 2% at 6 weeks. This suggests that the persistence of hamstrings contracture between 3 and 6 weeks after ACLR is an early predictive factor for Cyclops syndrome.
It was previously reported that femoral bone bruising is a risk factors for motion impairement.15 In the current study, femoral bone bruising was slightly more prevalent in the Cyclops group than in the control group, but this difference was not significant. Femoral bone bruising was present in 5 patients in the control group. Two of these patients had reported hamstrings contracture at 3 weeks but none at 6 weeks. Femoral bone bruising was also present in 9 patients in the Cyclops group. Three of these patients had reported hamstrings contracture at 3 weeks. All of these patients still had this deficit at 6 weeks. These findings suggest that the persistence, between 3 and 6 weeks, of a hamstrings contracture might be more relevant than femoral bone bruising. Contrary to a previous study,19 we found no relation to the graft choice (HT vs BPTB) or extra-articular tenodesis.
Our overall incidence (2.1%) of Cyclops syndrome is in line with the current literature. Wang and Ao23 observed 48 (15%) cases of Cyclops lesions in 311 second-look arthroscopies for internal fixation device removal, whereas only 1.93% had extension loss. Delincé et al2 described 23 patients (35%) with hypertrophic tissue in the anterior part of the knee in 65 consecutive second-look arthroscopies for hardware removal. The authors found different shapes and locations of scar tissue under the notch roof and reported “smaller nodules generally situated far more anteriorly in the knee can be discovered in asymptomatic patients.” Other second-look arthroscopy series, like that of Muellner et al,12 report a 17.6% incidence, but only half of Cyclops lesions were symptomatic.
Postoperative extension deficit after ACLR results from preoperative, intraoperative, and postoperative factors. Intraoperative factors, such as inadequate tibial tunnel placement, can cause impingement of the graft and loss of extension. With better understanding of the ACL function and anatomy, we acknowledge that the vast majority of patients with extension deficits have no recognizable technical flaw. Since all knees in our cohort achieved full extension at the end of surgery, failure to regain full extension might be due to an acquired condition after surgery, and that leads our attention to postoperative factors.
Full knee extension after ACL rupture or reconstruction depends on passive and active factors. A passive knee block to extension might occur with a meniscal tear, loose body, important hemarthrosis, or bell-hammer ACL tear. We had no such findings among our Cyclops patients. It is possible that those patients who cannot overcome a hamstrings contracture between 3 and 6 weeks are more likely to develop Cyclops syndrome.
Many extension deficits are related to an active mechanism. Most surgeons postpone ACLR until there is full range of motion. This might be a simplistic perspective that does not recognize the importance of full muscle control in ACLR. Quadriceps, hamstring, and soleus muscles are involved in active knee extension. These are antagonist muscles and an involuntary hamstrings contracture (triggered by pain or effusion) may go together with a selective quadricipital “shutdown.”16 Central activation deficits have been recognized to be responsible for quadriceps muscle weakness after knee injures affecting the injured as well as the noninjured leg.5,7,22,23 Rice et al16,17 have done extensive research on this topic and call it “arthrogenic muscle inhibition.” Even 20 mL of effusion can cause quadriceps inhibition in the vastus medialis and the vastus lateralis in otherwise healthy individuals during jogging.21 This arthrogenic muscle response, also seen in the soleus musculature after joint effusion, was found to be regulated by both pre- and postsynaptic control mechanisms.14
Muscular co-contraction is operationally defined as activation of both the agonist and antagonist muscle groups crossing the same joint. An antagonistic co-contraction of hamstring musculature seems to be a component of all functional movements, possibly to maintain dynamic knee stability and protect against excessive joint loads.3,19 Despite its potential stabilizing role, it has an increased metabolic cost and can impair performance.8,25 There are reports on an inverse relation between quadriceps weakness and hamstrings recruitment in total knee arthroplasty but there is no evidence on the effect of hamstrings contraction on the incidence of Cyclops syndrome after ACLR.25
The knee extension deficit at 4 weeks has been shown to be related to extension loss at 12 weeks after ACLR, supporting that, whatever the reason, there is a “therapeutic time window” in which we must obtain nearly normal knee extension.13,15 Our physiopathology hypothesis is that a hamstrings contracture will cause a flexion posture after ACLR. This extension deficit, dynamic and reducible in the first weeks, will prevent closure of the intercondylar notch (which was shown to be narrower in patients with ACL rupture19) and allow local organization of postoperative hemarthrosis. This process might evolve as reported in contained hematomas, from immature to mature connective tissue, the latter with collagenous fibers.20,23 Since 2015, the senior author (B.S.C.) has changed the early postoperative protocol after ACL reconstruction. Patients presenting with an extension deficit related to hamstring contracture are educated and strongly encouraged not only to perform exercises to reverse the extension deficit but also to actively contract their quadriceps in order to regain enduring full active extension (Video Supplement). Our Cyclops rate has decreased dramatically (0.1% in 2015), but we cannot draw any conclusion based on these data, and specific studies are required to demonstrate the effectiveness of this early postoperative care.
The limitations of this study include the fact that there is no measurement tool to objectively evaluate hamstring contracture. In addition, a causal relation between hamstring contracture and Cyclops lesions cannot be stated because, theoretically, a causal model needs to fulfill all Bradford-Hill criteria,6 which is impossible in a retrospective study. Nevertheless, a strong correlation is demonstrated. The results of this study demonstrate a positive relation between the published evidence on quadriceps function, hamstrings contracture, and the reported problems on ACLR when there is no full resolution of the extension deficit.3,10,12,16,24
Conclusion
Cyclops syndrome is correlated with an extension deficit at 3 and 6 weeks after ACL reconstruction. A persistent hamstring contracture in an early phase seems predictive for Cyclops syndrome.
Supplementary Material
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: B.S.C. is a paid consultant, receives royalties, receives research support, and has made presentations for Arthrex. M.T. is a paid consultant, receives research support, and has made presentations for Arthrex.
Ethical approval for this study was obtained from Centre Orthopédique Santy (approval number 2016-16).
A Video Supplement for this article is available at http://journals.sagepub.com/doi/suppl/10.1177/2325967116684121.
References
- 1. Bushnell BD, Sakryd G, Noonan TJ. Hamstring donor-site block: evaluation of pain control after anterior cruciate ligament reconstruction. Arthroscopy. 2010;26:894–900. [DOI] [PubMed] [Google Scholar]
- 2. Delincé P, Krallis P, Descamps PY, Fabeck L, Hardy D. Different aspects of the cyclops lesion following anterior cruciate ligament reconstruction: a multifactorial etiopathogenesis. Arthroscopy. 1998;14:869–876. [DOI] [PubMed] [Google Scholar]
- 3. Ford KR, van den Bogert J, Myer GD, Shapiro R, Hewett TE. The effects of age and skill level on knee musculature co-contraction during functional activities: a systematic review. Br J Sports Med. 2008;42:561–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Garofalo R, Mouhsine E, Chambat P, Siegrist O. Anatomic anterior cruciate ligament reconstruction: the two-incision technique. Knee Surg Sports Traumatol Arthrosc. 2006;14:510–516. [DOI] [PubMed] [Google Scholar]
- 5. Hart JM, Pietrosimone B, Hertel J, Ingersoll CD. Quadriceps activation following knee injuries: a systematic review. J Athl Train. 2010;45:87–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hill AB. The environment and disease: association or causation? Proc R Soc Med. 1965;58:295–300. [PMC free article] [PubMed] [Google Scholar]
- 7. Jackson DW, Schaefer RK. Cyclops syndrome: loss of extension following intra-articular anterior cruciate ligament reconstruction. Arthroscopy. 1990;6:171–178. [DOI] [PubMed] [Google Scholar]
- 8. Knarr BA, Zeni JA, Higginson JS. Comparison of electromyography and joint moment as indicators of co-contraction. J Electromyogr Kinesiol. 2012;22:607–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lefevre N, Naouri JF, Bohu Y, Klouche S, Herman S. Sensitivity and specificity of bell-hammer tear as an indirect sign of partial anterior cruciate ligament rupture on magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc. 2014;22:1112–1118. [DOI] [PubMed] [Google Scholar]
- 10. McGinnis K, Snyder-Mackler L, Flowers P, Zeni J. Dynamic joint stiffness and co-contraction in subjects after total knee arthroplasty. Clin Biomech (Bristol, Avon). 2013;28:205–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. McMahon PJ, Dettling JR, Yocum LA, Glousman RE. The cyclops lesion: a cause of diminished knee extension after rupture of the anterior cruciate ligament. Arthroscopy. 1999;15:757–761. [DOI] [PubMed] [Google Scholar]
- 12. Muellner T, Kdolsky R, Grossschmidt K, Schabus R, Kwasny O, Plenk H. Cyclops and cyclopoid formation after anterior cruciate ligament reconstruction: clinical and histomorphological differences. Knee Surg Sports Traumatol Arthrosc. 1999;7:284–289. [DOI] [PubMed] [Google Scholar]
- 13. Noll S, Garrison JC, Bothwell J, Conway JE. Knee extension range of motion at 4 weeks is related to knee extension loss at 12 weeks after anterior cruciate ligament reconstruction. Orthop J Sports Med. 2015;3:2325967115583632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Palmieri RM, Tom JA, Edwards JE, et al. Arthrogenic muscle response induced by an experimental knee joint effusion is mediated by pre- and post-synaptic spinal mechanisms. J Electromyogr Kinesiol. 2004;14:631–640. [DOI] [PubMed] [Google Scholar]
- 15. Quelard B, Sonnery-Cottet B, Zayni R, Ogassawara R, Prost T, Chambat P. Preoperative factors correlating with prolonged range of motion deficit after anterior cruciate ligament reconstruction. Am J Sports Med. 2010;38:2034–2039. [DOI] [PubMed] [Google Scholar]
- 16. Rice DA, McNair PJ. Quadriceps arthrogenic muscle inhibition: neural mechanisms and treatment perspectives. Semin Arthritis Rheum. 2010;40:250–256. [DOI] [PubMed] [Google Scholar]
- 17. Rice DA, McNair PJ, Lewis GN, Dalbeth N. Quadriceps arthrogenic muscle inhibition: the effects of experimental knee joint effusion on motor cortex excitability. Arthritis Res Ther. 2014;16:502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shelbourne KD, Patel DV, Martini DJ. Classification and management of arthrofibrosis of the knee after anterior cruciate ligament reconstruction. Am J Sports Med. 1996;24:857–862. [DOI] [PubMed] [Google Scholar]
- 19. Sonnery-Cottet B, Lavoie F, Ogassawara R, et al. Clinical and operative characteristics of cyclops syndrome after double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2010;26:1483–1488. [DOI] [PubMed] [Google Scholar]
- 20. Takasugi S, Ueda S, Matsumoto K. Chronological changes in spontaneous intracerebral hematoma—an experimental and clinical study. Stroke. 1985;16:651–658. [DOI] [PubMed] [Google Scholar]
- 21. Torry MR, Decker MJ, Millett PJ, Steadman JR, Sterett WI. The effects of knee joint effusion on quadriceps electromyography during jogging. J Sports Sci Med. 2005;4:1–8. [PMC free article] [PubMed] [Google Scholar]
- 22. Urbach D, Awiszus F. Impaired ability of voluntary quadriceps activation bilaterally interferes with function testing after knee injuries. A twitch interpolation study. Int J Sports Med. 2002;23:231–236. [DOI] [PubMed] [Google Scholar]
- 23. Wang J, Ao Y. Analysis of different kinds of cyclops lesions with or without extension loss. Arthroscopy. 2009;25:626–631. [DOI] [PubMed] [Google Scholar]
- 24. Yoshida Y, Mizner RL, Snyder-Mackler L. Association between long-term quadriceps weakness and early walking muscle co-contraction after total knee arthroplasty. Knee. 2013;20:426–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zeni JA, Rudolph K, Higginson JS. Alterations in quadriceps and hamstrings coordination in persons with medial compartment knee osteoarthritis. J Electromyogr Kinesiol. 2010;20:148–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.