Abstract
Background:
Ulnar collateral ligament (UCL) tears have become common, and UCL reconstruction (UCLR) is currently the preferred surgical treatment method for treating UCL tears.
Purpose/Hypothesis:
The purpose of this study was to review the literature surrounding UCL repair and determine the viability of new repair techniques for treatment of UCL tears. We hypothesized that UCL repair techniques will provide comparable results to UCLR for treatment of UCL tears.
Study Design:
Systematic review and meta-analysis; Level of evidence, 4.
Methods:
A systematic review was registered with PROSPERO and performed with PRISMA guidelines using 3 publicly available free databases. Biomechanical and clinical outcome investigations reporting on UCL repair with levels of evidence 1 through 4 were eligible for inclusion. Descriptive statistics were calculated for each study and parameter/variable analyzed.
Results:
Of the 46 studies eligible, 4 studies (3 clinical and 1 biomechanical) were included. There were 92 patients (n = 92 elbows; 61 males [62.3%]; mean age, 21.9 ± 4.7 years) included in the clinical studies, with a mean follow-up of 49 ± 14.4 months. Eighty-six percent of repairs performed were on the dominant elbow, and 38% were in college athletes. Most UCL repairs (66.3%) were performed via suture anchors. After UCL repair, 87.0% of patients were able to return to sport. Overall, 94.9% of patients scored excellent/good on the Andrews-Carson score. Patients who were able to return to sport after UCL repair did so within 6 months after surgery. Biomechanically, when UCL repair was compared with the modified Jobe technique, the repair group showed significantly less gap formation than the reconstruction group.
Conclusion:
In patients for whom repair is properly indicated, UCL repair provides similar return-to-sport rates and clinical outcomes with shorter return-to-sport timing after repair compared with UCL reconstruction. Future outcome studies evaluating UCL repair with internal bracing are necessary before recommending this technique.
Keywords: ulnar collateral ligament (UCL), repair, ulnar collateral ligament reconstruction (UCLR), Tommy John, baseball, pitcher
The ulnar collateral ligament (UCL) is the primary restraint to valgus force at the elbow.26,27 While the UCL does not play a large role in elbow stability during activities of daily living, the UCL comes under tremendous stress, approaching that of failure, each time a baseball pitcher throws a pitch.23,24,26 Contributions from surrounding osseous and muscular/tendinous structures help prevent UCL tears with each pitch. However, with increasing workload placed on the elbow from repetitive pitching, more and more pitchers of recent have suffered UCL tears.5,13,15,18,20 Often, treatment for UCL tears initially involves a period of rest followed by structured rehabilitation and a return to throwing program.1,16 If patients are unable to return to sport (RTS) and wish to continue to pitch, surgical treatment is a viable option. Surgical treatment options include UCL repair or UCL reconstruction.4,10,16
UCL repair was initially described as a treatment option for UCL tears in 1992, but the results were suboptimal, with an RTS rate of 71.4%.7 Ulnar collateral ligament reconstruction (UCLR), first described by Dr Frank Jobe in 1986, has since become the gold standard for treatment of UCL tears in overhead athletes who wish to RTS.21 While this procedure has undergone many modifications, results after UCLR have been encouraging, with RTS rates ranging from 66.7% to 97% based on the athlete’s level of competition and surgical technique.3,5,8,13,14,28,31 Regarding these modifications, a recent survey study found most Major League Baseball (MLB) team orthopaedic surgeons perform UCLR using the docking technique with a palmaris longus autograft.17 UCL repair obviates the need for a graft harvest, thereby decreasing graft site issues such as wound infections, postoperative weakness, erroneous graft harvest, or damage to surrounding neurovascular structures.
Although athletes have seen good results after UCLR, new UCL repair techniques, in the proper patient, may also offer similar results with some added benefits, including shorter rehabilitation times.11 Therefore, the purpose of this study was to critically review the literature surrounding UCL repair and determine the viability of new repair techniques for treatment of UCL tears compared with historic techniques. The authors hypothesize that new UCL repair techniques will provide comparable results to UCLR for treatment of UCL tears.
Methods
A systematic review was conducted according to PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines using a PRISMA checklist.22 Systematic review registration was performed using the PROSPERO international prospective register of systematic reviews (registration number 42016035808). Two reviewers independently conducted the search on February 25, 2016 using the following databases: Medline, Cochrane Central Register of Controlled Trials, SportDiscus, and CINAHL. The electronic search citation algorithm utilized was ((((ulnar collateral ligament) AND repair) AND elbow) NOT hand). English-language clinical studies of levels 1 through 4 evidence (2011 update by the Oxford Centre for Evidence-Based Medicine29) were eligible. Biomechanical studies were also eligible for inclusion. Medical conference abstracts were ineligible for inclusion. All references within included studies were cross-referenced for inclusion if missed by the initial search. Duplicate subject publications within separate unique studies were not reported twice. The study with longer duration follow-up or greater number of subjects was retained for inclusion. Level 5 evidence reviews, letters to the editor, imaging studies, studies looking at UCLR, and studies evaluating lateral collateral ligament repair and/or reconstruction were excluded.
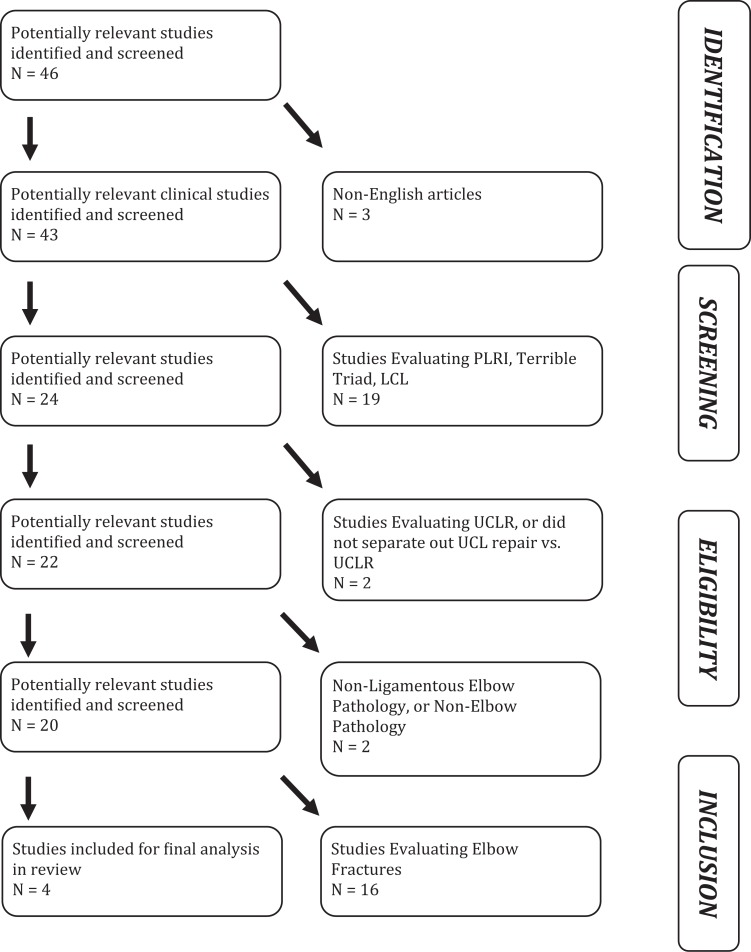
A total of 46 studies were located, and, after implementation of the exclusion criteria, 4 studies were included in the final analysis: 1 biomechanical study and 3 clinical studies. Patient demographics, including age, sex, handedness, sport, and position, were recorded. Clinical outcomes, including RTS rates and Andrews-Carson outcome score, were recorded. Complications were also recorded. For biomechanical studies, surgical technique, maximum torque at failure, torsional stiffness, and gap formation were recorded.
Statistical Analysis
Study descriptive statistics were calculated. Continuous variable data were reported as mean ± SD. Weighted means and standard deviations were calculated for all subject and surgical parameters. Categorical variable data were reported as frequencies with percentages.
Results
A total of 4 studies (3 clinical and 1 biomechanical) were included in this review (Figure 1). Of these studies, 3 (75%) had no conflicts of interest.
Figure 1.
Systematic review search algorithm according to PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines. After application of all exclusion criteria, 4 studies were identified for inclusion and further analysis. LCL, lateral collateral ligament; PLRI, posterolateral rotary instability; UCLR, ulnar collateral ligament reconstruction.
Clinical Studies
Three studies, all level 4 evidence, reported on UCL repair.2,7,30 Of the 92 patients (92 elbows) there were 61 (62.3%) males and 31 (33.7%) females, with a mean age of 21.9 ± 4.7 years (range, 14.8-38 years). The mean follow-up was 49 ± 14.4 months, with 86% of UCL repairs performed on the dominant elbow. One study mentioned UCL tear location.30 All patients in this study had proximal or distal UCL tears. No midsubstance tears were included. The mean duration of symptoms before surgery was 12.3 ± 5.9 months, and the mean duration of non-operative treatment was 3.1 ± 0.7 months. The majority of athletes were college (38%) or high school (32.6%) level, and most participated in baseball (66.3%) (Table 1).
TABLE 1.
Breakdown of Patients Who Underwent UCL Repair (N = 92) by Activity Level and Sporta
| n (%) | |
|---|---|
| Athletic level | |
| Professional | 10 (10.9) |
| College | 35 (38.0) |
| High school | 30 (32.6) |
| Recreational | 17 (18.5) |
| Sport | |
| Baseball | 61 (66.3) |
| Softball | 12 (13.1) |
| Gymnastics | 6 (6.6) |
| Cheerleading | 6 (6.6) |
| Tennis | 2 (2.2) |
| Basketball | 2 (2.2) |
| Snow skiing | 1 (1.0) |
| Baton twirling | 1 (1.0) |
| Calf roping | 1 (1.0) |
aUCL, ulnar collateral ligament.
There were 3 types of repairs that were performed in the included studies. These techniques included repair via suture anchors (61 patients; 66.3%), direct repair without graft augmentation (17 patients; 18.5%), and repair via drill holes (14 patients; 15.2%). Complications occurred in 12.0% of patients. These complications included transient ulnar neuropraxia in 6 patients, arthrofibrosis in 1 patient, stitch abscess in 1 patient, superficial wound infection requiring debridement in 1 patient, and failure of the repair in 2 patients. Complication rates in UCLR have been reported between 5.3% and 10.5%.13,14,31
The mean RTS rate after UCL repair was 87.0%, with the majority of included patients participating at the college and high school level. Overall, 94.9% of patients who underwent UCL repair scored excellent/good on the Andrews-Carson score (Table 2). The Conway score was used in 1 study, and 50% of patients scored excellent while 22% scored good, 14% scored fair, and 14% scored poor.
TABLE 2.
Clinical Outcomes Using the Andrews-Carson Score for Patients Who Underwent UCL Repaira
| Andrews-Carson Scoreb | No. of Patients |
|---|---|
| Subjective | |
| Excellent | 67 |
| Good | 7 |
| Fair | 2 |
| Poor | 2 |
| Objective | |
| Excellent | 72 |
| Good | 3 |
| Fair | 2 |
| Poor | 1 |
| Overall | |
| Excellent | 69 |
| Good | 5 |
| Fair | 3 |
| Poor | 1 |
aUCL, ulnar collateral ligament.
bOne study did not report the breakdown of the Andrews-Carson score, so the individual numbers will not total 92 here but rather 78.
Biomechanical Study
There was only 1 biomechanical study in the literature that evaluated UCL repair, and thus was included in this review.12 Dugas et al12 compared a novel repair technique that was augmented with internal bracing to the modified Jobe technique in 9 matched pairs of cadaveric arms. Their repair technique involved 1 drill hole in the ulna and 1 in the medial epicondyle. A 3.5-mm knotless SwiveLock (Arthrex Inc) anchor loaded with 2-mm FiberTape (Arthrex Inc) and a size 0 nonabsorbable suture was oriented such that the tape was as close to the native UCL attachment as possible and then placed in the ulnar hole. The suture was then used to repair the UCL to its insertion on the ulna. After this, the split in the UCL was repaired with simple 2-0 sutures. To fix the internal brace proximally, the free ends of the FiberTape suture were loaded into a second 3.5-mm SwiveLock anchor, and with the joint reduced, the anchor was advanced to match the tension of the underlying tissue and the screw advanced into the hole. Finally, size 0 absorbable suture was used to suture the FiberTape and native UCL together.12
The authors12 then compared the repaired UCL augmented with the FiberTape internal brace with those elbows reconstructed with the modified Jobe technique using an Arthrex MTS 858 Mini Bionix II axial-torsional materials testing machine (MTS System Corp). The elbows in the repair group failed from ulnar screw pullout (44.4%), humeral shaft/ supracondylar fracture (33.4%), and epicondyle screw pullout (22.2%). The elbows in the reconstruction group failed from intrasubstance tears (33.3%), ulnar tunnel fracture (33.4%), and humeral shaft/supracondylar fracture (33.3%). On testing, the repair group showed significantly less gap formation than the reconstruction group. Furthermore, there was no difference between the repair and reconstruction groups for the maximum torque at failure, torsional stiffness, or gap formation during the failure test.
Discussion
Over the past several years, the number of UCL tears sustained by athletes of all levels of play, especially college and high school baseball pitchers, has increased dramatically.3,5,15,19 UCLR has become the gold standard for treatment of these injuries based largely on 1 study from over 20 years ago that showed better outcomes in patients who underwent UCLR than UCL repair.7 Our study showed that patients who underwent UCL repair had an RTS rate of over 87%. Furthermore, the biomechanical evidence of a novel technique showed significantly less gapping on the medial side of the elbow with an augmented UCL repair compared with the modified Jobe technique.
With the recent increase in the number of UCL injuries sustained by professional, collegiate, high school, and recreational athletes, there have been several studies that have attempted to determine the ideal reconstruction method for UCLR.5,13,14,28,31 No clinical study to date has shown dramatically better results for one UCLR technique over another. Unfortunately, none of these studies have directly compared results of UCLR with UCL repair. The RTS rate after UCLR has largely been cited at >80%, with higher rates seen in collegiate athletes (95.5%) than professional athletes (86.4%).14 Historic results of UCL repair in MLB players have shown an RTS rate of 50%.7 However, recent evidence has shown the RTS after UCL repair in nonprofessional athletes to be between 94.4% and 96.7%.2,30 Furthermore, the timing for RTS in all these athletes after UCL repair has been less than 6 months.2,30 This is in stark contrast to the greater than 12 months that is required for RTS after UCLR.5,13,15,28 Hence, it seems that UCL repair may be a viable treatment option for high school and collegiate athletes, specifically those with UCL tears at the proximal or distal end of the ligament, who wish to RTS. Those who have midsubstance tears seem less likely to benefit from a repair over a reconstruction.
Unfortunately, no clinical studies have directly compared the new techniques for UCL repair with modern UCLR techniques. One biomechanical study did compare the modified Jobe technique for UCLR with a UCL repair technique augmented with an internal brace.12 This recent study showed very encouraging results, with decreased medial gapping present in the repair group compared with the reconstruction group. Although this technique has not yet been tested in overhead athletes, the biomechanical results are encouraging. This technique must be tested in overhead athletes to allow conclusions regarding RTS rates and performance to be made. Interestingly, the shorter duration of postoperative rehabilitation after repair may make this surgery a more attractive option to both professional and nonprofessional athletes moving forward. However, the decision to proceed with a repair or reconstruction is ultimately left to the treating physician and athlete. It is still unclear what the results of modern UCL repair techniques in professional athletes will be as none of the patients included in the 2 recent UCL repair studies have been professional athletes; specifically, no MLB pitchers were included.2,30 As MLB pitchers are the group of athletes who receive the most attention with regard to UCL tears, despite the fact that more UCLRs are performed in collegiate and high school athletes, it is necessary to evaluate these new techniques in this elite patient population.5,14,19 It may be that UCL repair is not suited for these patients, but current studies are necessary to determine whether this is true.
One very important issue that has arisen in the past few years is repeat UCL tears in patients who have already undergone UCLR.6,9,25,32 The revision rate after UCLR has been cited at approximately 15%, and the results after revision UCLR have not been as encouraging as those after primary UCLR, with a shorter career, lower RTS rate, and inferior performance on RTS seen after revision UCLR.9,25,32 However, in these revision cases, the index surgery has been a reconstructed UCL, not a repaired UCL. Therefore, it is unknown whether athletes would perform better, both from an RTS rate and performance perspective, after a revision UCLR from a repaired UCL versus a revision UCLR from an initially reconstructed UCL. The 2 patients who underwent a revision UCLR after their UCL repair had no complications or issues after surgery and were able to RTS at competitive levels.30 Since a UCL repair does not require as much dissection and bony work as a standard UCLR does, it makes sense that a revision surgery after a UCL repair may be technically less demanding and not as traumatic to the elbow as a revision after a standard UCLR. Future studies are necessary to both evaluate the performance results after UCL repair with internal bracing as well as results after revision UCLR in patients whose index procedure was a UCL repair compared with a UCLR.
Limitations
As this study was a review of the literature, it is subject to all limitations of the studies that were included. Despite an exhaustive search, it is possible that some studies were missed. Also, repair techniques varied among studies, and this could have introduced heterogeneity and bias into the results. Furthermore, the new internal bracing surgical technique has only been tested in the laboratory setting, so the results may not be translatable to overhead athletes.
Conclusion
In properly indicated patients, UCL repair provides similar RTS rates and clinical outcomes with shorter timing to RTS after repair compared with UCLR. Future outcome studies evaluating UCL repair with internal bracing are necessary before recommending this technique.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: B.R.B. receives research support from Arthrex Inc, CONMED Linvatec, DJ Orthopaedics, Ossur, Smith & Nephew, and Tornier. N.N.V. receives research support from Arthrex Inc, Arthrosurface, DJ Orthopaedics, Smith & Nephew, Athletico, ConMed Linvatec, Miomed, and Mitek; has stock or stock options in Cymedica, Minivasive, and Omeros; is a paid consultant for Minivasive, Orthospace, and Smith & Nephew; and receives royalties from Smith & Nephew. C.A.B. has stock or stock options in Cresco Lab and is an unpaid consultant for The Foundry. A.A.R. receives research support from DJO, Ossur, Smith & Nephew, and Arthrex Inc and receives IP royalties and is a paid consultant for Arthrex Inc.
References
- 1. Andrews JR, Jost PW, Cain EL. The ulnar collateral ligament procedure revisited: the procedure we use. Sports Health. 2012;4:438–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Argo D, Trenhaile SW, Savoie FH, 3rd, Field LD. Operative treatment of ulnar collateral ligament insufficiency of the elbow in female athletes. Am J Sports Med. 2006;34:431–437. [DOI] [PubMed] [Google Scholar]
- 3. Azar FM, Andrews JR, Wilk KE, Groh D. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med. 2000;28:16–23. [DOI] [PubMed] [Google Scholar]
- 4. Bruce JR, Andrews JR. Ulnar collateral ligament injuries in the throwing athlete. J Am Acad Orthop Surg. 2014;22:315–325. [DOI] [PubMed] [Google Scholar]
- 5. Cain EL, Jr, Andrews JR, Dugas JR, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38:2426–2434. [DOI] [PubMed] [Google Scholar]
- 6. Conte SA, Fleisig GS, Dines JS, et al. Prevalence of ulnar collateral ligament surgery in professional baseball players. Am J Sports Med. 2015;43:1764–1769. [DOI] [PubMed] [Google Scholar]
- 7. Conway JE, Jobe FW, Glousman RE, Pink M. Medial instability of the elbow in throwing athletes. Treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am. 1992;74:67–83. [PubMed] [Google Scholar]
- 8. Dines JS, ElAttrache NS, Conway JE, Smith W, Ahmad CS. Clinical outcomes of the DANE TJ technique to treat ulnar collateral ligament insufficiency of the elbow. Am J Sports Med. 2007;35:2039–2044. [DOI] [PubMed] [Google Scholar]
- 9. Dines JS, Yocum LA, Frank JB, ElAttrache NS, Gambardella RA, Jobe FW. Revision surgery for failed elbow medial collateral ligament reconstruction. Am J Sports Med. 2008;36:1061–1065. [DOI] [PubMed] [Google Scholar]
- 10. Dugas J, Chronister J, Cain EL, Jr, Andrews JR. Ulnar collateral ligament in the overhead athlete: a current review. Sports Med Arthrosc. 2014;22:169–182. [DOI] [PubMed] [Google Scholar]
- 11. Dugas JR. Ulnar collateral ligament repair: an old idea with a new wrinkle. Am J Orthop (Belle Mead NJ). 2016;45:124–127. [PubMed] [Google Scholar]
- 12. Dugas JR, Walters BL, Beason DP, Fleisig GS, Chronister JE. Biomechanical comparison of ulnar collateral ligament repair with internal bracing versus modified Jobe reconstruction. Am J Sports Med. 2016;44:735–741. [DOI] [PubMed] [Google Scholar]
- 13. Erickson BJ, Bach BR, Jr, Cohen MS, et al. Ulnar collateral ligament reconstruction: the Rush experience. Orthop J Sports Med. 2016;4:2325967115626876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Erickson BJ, Chalmers PN, Bush-Joseph CA, Verma NN, Romeo AA. Ulnar collateral ligament reconstruction of the elbow: a systematic review of the literature. Orthop J Sports Med. 2015;3:2325967115618914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Erickson BJ, Gupta AK, Harris JD, et al. Rate of return to pitching and performance after Tommy John surgery in Major League Baseball pitchers. Am J Sports Med. 2014;42:536–543. [DOI] [PubMed] [Google Scholar]
- 16. Erickson BJ, Harris JD, Chalmers PN, et al. Ulnar collateral ligament reconstruction: anatomy, indications, techniques, and outcomes. Sports Health. 2015;7:511–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Erickson BJ, Harris JD, Fillingham YA, et al. Treatment of ulnar collateral ligament injuries and superior labral tears by Major League Baseball team physicians. Arthroscopy. 2016;32:1271–1276. [DOI] [PubMed] [Google Scholar]
- 18. Erickson BJ, Harris JD, Tetreault M, Bush-Joseph C, Cohen M, Romeo AA. Is Tommy John surgery performed more frequently in Major League Baseball pitchers from warm weather areas? Orthop J Sports Med. 2014;2:2325967114553916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Erickson BJ, Nwachukwu BU, Rosas S, et al. Trends in medial ulnar collateral ligament reconstruction in the United States: a retrospective review of a large private-payer database from 2007 to 2011. Am J Sports Med. 2015;43:1770–1774. [DOI] [PubMed] [Google Scholar]
- 20. Fleisig GS, Andrews JR, Cutter GR, et al. Risk of serious injury for young baseball pitchers: a 10-year prospective study. Am J Sports Med. 2011;39:253–257. [DOI] [PubMed] [Google Scholar]
- 21. Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg Am. 1986;68:1158–1163. [PubMed] [Google Scholar]
- 22. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62: e1–e34. [DOI] [PubMed] [Google Scholar]
- 23. Loftice J, Fleisig GS, Zheng N, Andrews JR. Biomechanics of the elbow in sports. Clin Sports Med. 2004;23:519–530, vii–viii. [DOI] [PubMed] [Google Scholar]
- 24. Lyman S, Fleisig GS, Andrews JR, Osinski ED. Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med. 2002;30:463–468. [DOI] [PubMed] [Google Scholar]
- 25. Marshall NE, Keller RA, Lynch JR, Bey MJ, Moutzouros V. Pitching performance and longevity after revision ulnar collateral ligament reconstruction in Major League Baseball pitchers. Am J Sports Med. 2015;43:1051–1056. [DOI] [PubMed] [Google Scholar]
- 26. Morrey BF. Applied anatomy and biomechanics of the elbow joint. Instr Course Lect. 1986;35:59–68. [PubMed] [Google Scholar]
- 27. Morrey BF, An KN. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med. 1983;11:315–319. [DOI] [PubMed] [Google Scholar]
- 28. O’Brien DF, O’Hagan T, Stewart R, et al. Outcomes for ulnar collateral ligament reconstruction: a retrospective review using the KJOC assessment score with two-year follow-up in an overhead throwing population. J Shoulder Elbow Surg. 2015;24:934–940. [DOI] [PubMed] [Google Scholar]
- 29. Oxford Centre for Evidence-based Medicine. Levels of evidence (March 2009). http://www.cebm.net/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/. Accessed April 16, 2016.
- 30. Savoie FH, 3rd, Trenhaile SW, Roberts J, Field LD, Ramsey JR. Primary repair of ulnar collateral ligament injuries of the elbow in young athletes: a case series of injuries to the proximal and distal ends of the ligament. Am J Sports Med. 2008;36:1066–1072. [DOI] [PubMed] [Google Scholar]
- 31. Vitale MA, Ahmad CS. The outcome of elbow ulnar collateral ligament reconstruction in overhead athletes: a systematic review. Am J Sports Med. 2008;36:1193–1205. [DOI] [PubMed] [Google Scholar]
- 32. Wilson AT, Pidgeon TS, Morrell NT, DaSilva MF. Trends in revision elbow ulnar collateral ligament reconstruction in professional baseball pitchers. J Hand Surg Am. 2015;40:2249–2254. [DOI] [PubMed] [Google Scholar]