Abstract
Objective
Health informatics has growing importance in clinical practice with successive General Medical Council recommendations. However, prior data suggest that undergraduate medical education largely neglects this area. An up-to-date, UK-wide view of health informatics training in medical schools is required.
Design
An online survey was developed using current guidance and recommendations of UK professional bodies.
Participants and Setting
Senior academic staff and health informatics educators at all 34 UK medical schools were invited to complete the survey.
Main outcome measures
Quantitative and qualitative data regarding health informatics in the undergraduate medical curriculum.
Results
A total of 26/34 (76%) of UK medical schools responded and 23 provided full information. Aspects most frequently mentioned were literature searching and research governance. Seventeen per cent of respondents felt there was little or no HI training, although clinical record keeping was addressed by all medical schools. Pedagogies used to teach health informatics were self-directed learning (78%) to lecture based (70%), seminars (70%), informal teaching in clinical settings (57%) and problem-based learning (22%). Health informatics was usually integrated vertically and horizontally across the curriculum (76%). Assessment and updates of the health informatics curriculum are limited (57 and 41%, respectively). Thirty-two per cent of respondents reported a low level of confidence among students to use health informatics as doctors. In the most up-to-date survey of health informatics teaching in UK medical schools, there are three major findings. First, the proportion of health informatics in the medical undergraduate curriculum is low. Second, there was variation in content, pedagogy and timing across medical schools. Third, health informatics is rarely assessed and course content is not regularly updated.
Conclusions
There is a role for national guidelines and further research in this area of the curriculum which is rapidly gaining in prominence.
Keywords: medical informatics, medical education
Introduction
Health informatics and its role in clinical practice are not new,1–4 but with new NHS targets to move to paperless working and the Wachter review of NHS information technology underway, there is renewed focus.5,6 Health informatics can be defined as ‘the knowledge, skills and tools which enable information to be collected, managed, used and shared safely to support the delivery of healthcare and promote health’.7
Clinical tasks are increasingly completed using computerised tools and automation. Technical advances generate new forms of data to inform clinical decision-making, from next-generation sequencing to wearable sensors. Healthcare organisations must extract value from data collected in clinical work. Training must prepare clinicians to ensure that best quality data are created at the clinical workface and to be intelligent users of statistics and analytics generated by the ‘big data’ revolution.8
A framework for health informatics education for health professionals was set out by the NHS Information Authority in 1999, and detailed learning outcomes for different professional groups were organised into eight themes: communication, knowledge management, data quality and management, confidentiality and security, secondary uses of clinical data and information, clinical and service audit, working clinical systems and telemedicine and telecare.9 The American Health Informatics Management Association defined five areas of health informatics that health professional education should address: literacy and skills, electronic health records, privacy and confidentiality, information and data technical aspects and security, basic computer literacy.9,10 The UK’s General Medical Council core curriculum for medical students includes health informatics competencies (Box 1).11
Box 1.
General Medical Council outcomes for doctors, the doctor as practitioner.10
| Use information effectively in a medical context. |
| a. Keep accurate, legible and complete clinical records |
| b. Make effective use of computers and other information systems, including storing and retrieving information |
| c. Keep to the requirements of confidentiality and data protection legislation and codes of practice in all dealings with information |
| d. Access information sources and use the information in relation to patient care, health promotion, advice and information to patients, and research and education |
| e. Apply the principles, method and knowledge of health informatics to medical practice. |
Despite strong guidance from professional bodies12,13 to incorporate health informatics into training and clinical practice, data from 2004 suggest that UK medical schools were not adequately training students in health informatics.1,2 More recent data are lacking. We therefore conducted a survey of UK medical schools to provide current data on the state of health informatics education, exploring whether health informatics teaching has been enhanced or updated based on new guidance and materials.
Our study had three aims:
To investigate which aspects of health informatics were addressed in UK medical school curricula in 2015/16
To identify pedagogies used for health informatics education
To explore awareness of medical educators about health informatics at their institution.
Methods
Survey design
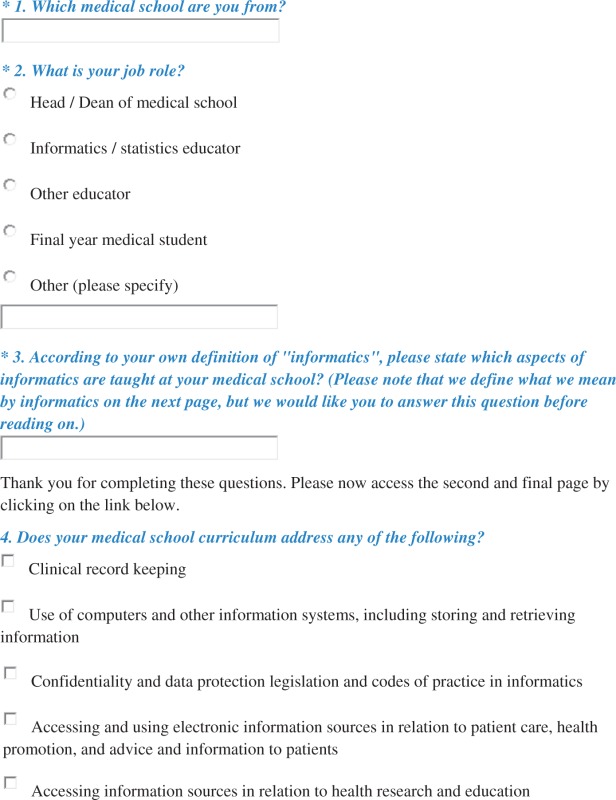
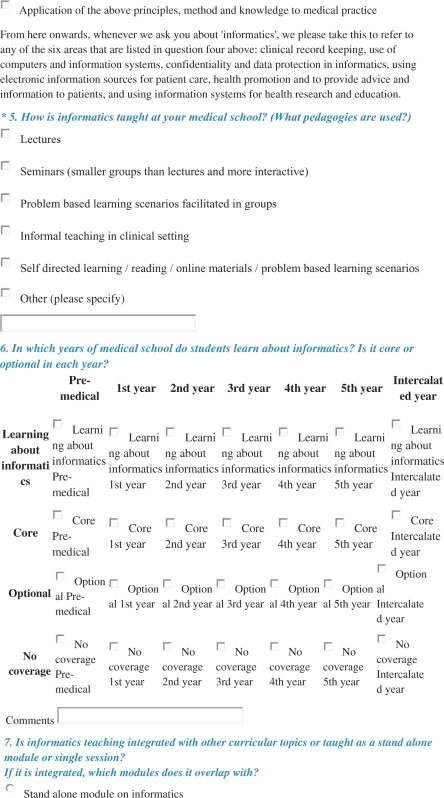
Informed by General Medical Council guidance on health informatics competencies for doctors,11 published analysis of health informatics learning needs2 and discussions with leading academics in health informatics, an online survey was developed (Appendix 1) and piloted by two researchers.
Study population
Senior academic staff and health informatics educators at UK medical schools were surveyed.
Recruitment
Relevant educators (medical, health informatics or data science) were identified at each of the 34 UK medical schools14 via their websites, phone calls to medical school administration offices and contacts of the authors. An email was sent to each educator to invite them to participate. Reminder emails were sent to those who had not responded after two weeks and then again two weeks before the end of the three-month survey period.
Analysis
The percentage of medical schools represented was calculated. For multiple choice questions, descriptive quantitative results were calculated. Qualitative responses were downloaded and read by all authors. The Health and Social Care Information Centre health informatics theme15 framework was used to categorise responses about health informatics teaching, allowing exploration of frequency of responses related to each theme and variation between responses.
Ethical approval
The project had ethical approval from University College London Research Ethics Committee, Project ID: 7979/002.
Results
Participant characteristics
Responses were received from 26/34 (76%) of UK medical schools. Basic information was provided by 30 respondents (four medical schools provided two separate responses), and 23 respondents provided full information. Eight respondents (27%) were head or dean of the medical school, seven (23%) were ‘Informatics/Statistics educator’ and 15 (50%) had varying roles, e.g. Deputy Dean, Phase One Director.
Understanding of health informatics
An open question about aspects of taught informatics had 30 respondents (100%). Responses showed that understanding of the term ‘informatics’ was mainly related to the seven domains of health informatics outlined by the Health and Social Care Information Centre14 but extended to include bioinformatics (Table 1). Aspects of health informatics most frequently mentioned were literature searching and research governance.
Table 1.
Responses organised according to seven health informatics themes most relevant to clinicians15 and related to bioinformatics.
| Domain of health informatics | Responses from participants (direct quotations) |
|---|---|
| Protection of individuals and organisations | ‘Privacy of records’ ‘Data protection and research governance’ ‘Use of information technology in healthcare’ ‘Data collection, data use, and research ethics’ ‘Digital professionalism/capabilities’ ‘Clinical audit and the relevant information gathering… electronic prescribing… patient electronic records’ ‘Work effectively within the legal and professional constraints that relate to person-identifiable information’ ‘Confidentiality and ethics, information governance’ ‘Use of Data in research’ ‘Information Governance’ |
| Data, information and knowledge | ‘Literature searching, use of databases, literature review, critical appraisal, access to EBM resources’ ‘Database searching; generic training available for various software’ ‘Medline and EBM’ ‘Literature searching and critical appraisal’ ‘Information filtering in relation to research and scholarship’ ‘Tools such as Endnote, and how to effectively search online, etc.’ ‘How to source reliable information’ ‘Decision support’ ‘Systematic literature review, critical review’ ‘Handling/processing data using Excel…. SSC [in] clinical trial/study design and analysis’ ‘Statistics and epidemiology/statistics’ |
| Communication and information transfer | ‘Use computers, computing, information and information technology effectively in a medical context’ ‘Medical records, uses of clinical data for other purposes – research, audit’ ‘Functions and importance of CIS in healthcare for patient care (long term conditions, patient pathways, communication)’ |
| Health and care records | ‘Good record keeping’ ‘Systems and process around information gathering, management, interpretation and application’ ‘Evidence Based Medicine and Clinical Guidelines… best practice in notetaking’ |
| The language of health: clinical coding and terminology | ‘How to record data’ ‘Importance of clinical data quality (coding, etc.)’ |
| Clinical systems and applications | ‘Use of HNS computer systems’ ‘Use of databases in medicine, retrieval of information, use of HNS computer systems’ ‘Use of clinical Information Systems’ |
| eHealth: the future direction of clinical care | ‘E-health’ ‘Telemedicine’ ‘Big data’ ‘Role of digital technology in Medicine, including social media training, effective digital handover’ ‘New ways of delivering care underpinned by technology’ |
| Bioinformatics | ‘Bioinformatics, informatics of genomic and genetic data’ ‘Sequence analysis, gene and protein expression, elementary systems biology’ ‘Genetics, epigenetics’ |
Coverage of health informatics topics
In response to an open question about which aspects of health informatics are taught, some respondents said ‘very little’ (n = 3, 10%) or ‘none’ (n = 2, 7%). Conversely, where health informatics is not recognised in the curriculum, it may be because it is so well integrated across the curriculum:
Eh? That’s like asking what aspects of ‘Communication’ or ‘Physiology’ are taught. Not sure how to respond to such a broad question
None that is badged as informatics (Respondent's role: Lead for medical education)
Respondents were asked whether they addressed five areas of health informatics outlined by the GMC11 and 22 (73%) responded. The majority address all five areas (Table 2), including 100% addressing clinical record keeping.
Table 2.
Proportion of respondents who stated that each health informatics area10 is covered in their curriculum.
| Area of health informatics | Respondents who stated that this area is addressed in their curriculum |
|---|---|
| Clinical record keeping | 100% (22/22) |
| Use of computers and other information systems, including storing and retrieving information | 77% (17/22) |
| Confidentiality and data protection legislation and codes of practice in informatics | 77% (17/22) |
| Accessing and using electronic information sources in relation to patient care, health promotion, and advice and information to patients | 82% (18/22) |
| Accessing information sources in relation to health research and education | 91% (20/22) |
| Application of the above principles, method and knowledge to medical practice | 73% (16/22) |
Pedagogies
Of 23 respondents, 78% (18/23) said self-directed learning is used in health informatics education, 70% (16/23) said lectures, 70% (16/23) seminars, 57% (13/23) informal teaching in clinical settings and 22% (5/23) problem-based learning sessions.
health informatics education is mainly integrated with other teaching topics and taught across all years of undergraduate training. Of 21 respondents, 76% (16/21) said that informatics teaching is integrated with other curricular topics. Four respondents said informatics teaching is delivered in stand-alone sessions (19%, 4/21) and one said health informatics comprises a stand-alone module (5%, 1/21).
Respondents commented on integration of health informatics education:
Our training is focused on the effective use of information in a clinical context as part of clinical practice and as such is embedded in practice rather than being identified as a stand-alone topic. (Respondent's role: Dean of medical school)
There is limited formal teaching on informatics but by virtue of clinical exposure students will see informatics in action and become familiar with its use.
Timing of health informatics teaching in medical curriculum
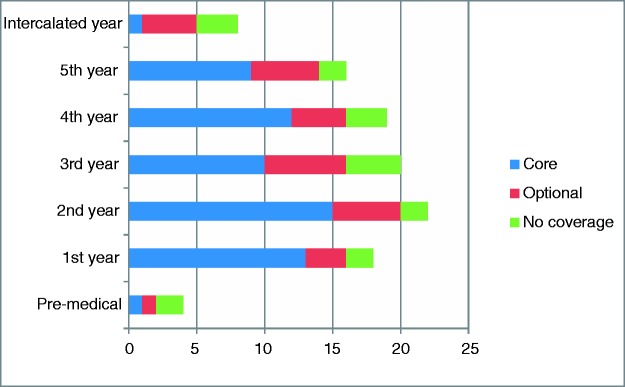
Twenty-one participants answered a question about when health informatics is taught. Health informatics is most commonly taught in second-year core curriculum (15/21, 71%). In every year group, health informatics teaching is more common in core than optional teaching (Figure 1).
Figure 1.
Core and optional HI teaching by year group. x-axis: number of respondents who said that teaching takes place in this year group, y-axis – year group.
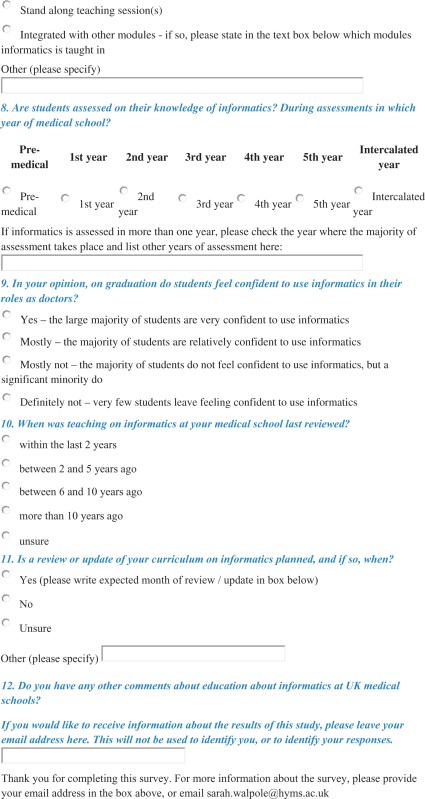
Assessment of health informatics knowledge and competence
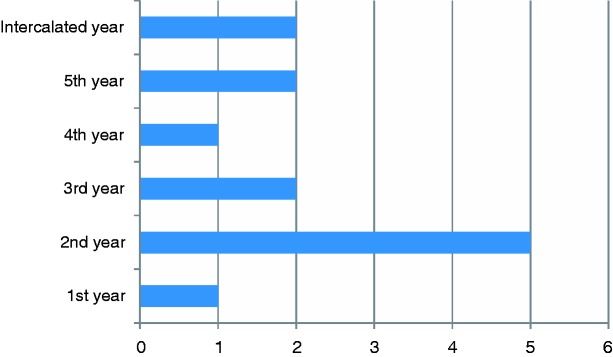
Just over half of respondents (57%, 13/23) said that there was some assessment of health informatics. Most commonly this is during second year (Figure 2).
Figure 2.
Assessment of HI by year group. x-axis: number of respondents who said that assessment takes place in this year group, y-axis – year group.
Updating the informatics curriculum
Forty-one per cent (9/22) of respondents said there had been a review of health informatics in their curriculum within the last two years, but 9% (2/22) said it had been over 10 years since the last review. Fifty per cent (11/22) said a curriculum review is planned.
Challenges
Nineteen respondents answered the question ‘In your opinion, on graduation, do students feel confident to use informatics in their role of doctors?’ Three (16%) said ‘yes’, 10 (53%) said ‘mostly’ and the remainder 32% (6/19) said ‘mostly no’.
There was a low expectation regarding the extent of current health informatics teaching:
IMHO [in my humble opinion], the majority of UK medical schools have very limited awareness of, and lack capacity to teach, the broader range of health informatics topics that the students need to know. (Respondent's role: Professor of Digital Healthcare)
It was very noticeable in a recent survey of public health teaching in medical schools (Lyon et al) that informatics was very poorly covered. (Respondent's role: Head of public health / informatics education)
One respondent commented that terminology may be a barrier to engaging students in health informatics education: ‘Students do not connect to the term informatics, it has to relate to their future career as a doctor’.
Practical challenges were raised. For example, one participant said ‘trust IT security often makes this problematic’, another commented that a centralised IT training and access system would be an improvement on the current system of training in each individual healthcare centre.
Discussion
In the most up-to-date survey of health informatics teaching in UK medical schools, there are three major findings. First, the proportion of health informatics in the medical undergraduate curriculum is low and does not meet national standards. Second, there was considerable variation in content, pedagogy and timing across medical schools. Third, health informatics is rarely assessed and the course content is not regularly updated.
There are gaps in the health informatics education that UK undergraduate medical students receive, as in other countries. The International Medical Informatics Association recommend that medical students receive 40 hours of training in health informatics, and a survey in Germany found that students receive between 4 and 30 hours.16 Research in the USA found that medical students do not feel confident to understand and use health informatics appropriately.4 A study in China found that undergraduate medical health informatics education is insufficient.17
Of the five areas of health informatics in which all doctors should be competent,10 only one is taught in all medical schools represented in this survey. Only 73% of respondents said that teaching about the application of health informatics to medical practice is provided. The majority of schools teach health informatics integrated with other topics. Qualitative responses suggest that this can result in students or staff lacking awareness that health informatics education is taking place, and graduates may not be able to discuss core health informatics concepts and domains.
A range of pedagogies are used to teach health informatics, including lectures and small group seminars. Self-directed learning is the most common pedagogy used. Notably, only 57% said that health informatics teaching takes place in clinical settings, but this may represent under-reporting. Research in Germany also found that a range of pedagogies are used to teach health informatics.16 While no evidence supports one pedagogy above another, using a range of pedagogies is considered the optimal way to teach health informatics.9 This also provides opportunity to evaluate the effectiveness of different pedagogies for health informatics education.
Only 19% of respondents said that there is stand-alone teaching on health informatics; most schools integrate health informatics teaching. A challenge is achieving integration but ensuring visibility of health informatics education in the curriculum. Educators highlighted that use of health informatics is frequent in training (for example in accessing online patient records), but there may be a lack of explicit health informatics teaching and awareness among students. The majority of health informatics teaching is in the core curriculum. health informatics teaching and assessment most commonly takes place in second year; however, there is wide variation in practice. Given the importance of good record-keeping and growing use of ‘big data’, health informatics should be taught across the curriculum.
In a large minority of schools, no assessment of health informatics is reported. Few schools assess health informatics at multiple stages of training. Assessment is integral to effective training and should take place frequently to ensure understanding, inform teaching evaluation and drive learning.18 Update of the health informatics curriculum is infrequent compared to the pace of health informatics development. Only 41% of respondents said that their health informatics curriculum had been reviewed in the last two years, and in two schools there had been no review for over 10 years.
Strengths/limitations
Strengths of this study are the good response rate and senior roles of respondents. A wide range (72%) of UK medical schools are represented. The majority of respondents have senior roles such as Dean or Deputy Dean and can be expected to have a good knowledge of their medical school curriculum.
Limitations include data collection from only one educator in most schools and the depth of data that could be collected using online survey. Respondents may not have been aware of all health informatics education at their school; especially where health informatics education takes place informally during clinical teaching, where health informatics education is integrated with other topics or where respondents work exclusively on one phase of their curriculum. This risks under-reporting of health informatics teaching and assessment. Collection of data from students was beyond this study’s scope, therefore investigation of students’ confidence and competence in health informatics is limited. Because of the online survey approach, many data are categorical. This limits exploration of educators’ understanding and details of health informatics teaching and assessment.
Implications
There are four important considerations in the light of our findings. Firstly, as the use of technology rapidly increases in healthcare settings, doctors of tomorrow must be able to deploy their clinical skills in a highly computerised environment.
Secondly, students should be trained to employ decision-making strategies that reflect the accessibility of information and availability of data. Greenhalgh et al.,8 discussing challenges for evidence based medicine, argue that ‘students must be taught how to share both evidence and uncertainty with patients using appropriate decision aids and adapt their approach to individual needs, circumstances, and preferences’. Teaching undergraduates about the use of information to support front line decision making with patients requires insights not just from informatics but also cognitive psychology, implementation science and clinical practice. This is scarcely feasible within the time constraints of current informatics teaching.
Thirdly, as the capacity to store, analyse and utilise data collected during healthcare provision expands, it is increasingly important that doctors understand and can follow guidelines on collection, storage and access of data.
Finally, the rapid pace at which healthcare technology changes provides further challenges. While the research focus of the field shifts continually in line with technical progress, our findings suggest that the content of undergraduate health informatics teaching changes more slowly. For example, the ‘big data’ agenda has arisen in the last decade based on analysis that is older. Few medical curricula have kept pace. Development of postgraduate health informatics curricula will be necessary to keep professionals up to date throughout their careers.
Recommendations
Based on our findings, we recommend that national guidelines for health informatics teaching and assessment are reaffirmed and disseminated by national medical and educational bodies. Standards should define health informatics, outline which topics should be taught and state the level of competence required at graduation.
Given variation in educational practice, research should explore which pedagogies and assessment strategies are most effective for health informatics education.
To keep pace with the rapidly evolving field of health informatics, medical schools must ensure health informatics teaching meets General Medical Council guidelines with regular review and updates, and a named informatics lead would be beneficial.
Acknowledgements
None
Appendix 1: Survey questions
Informatics in Medical Education: A survey of current practice
Thank you for completing this survey about informatics in medical education
This survey is part of a small research project, led by Amitava Banerjee and Paul Taylor at the Farr Institute, UCL and Sarah Walpole, Hull York Medical School. By carrying out this survey, we aim to understand the current situation with regard to informatics training at medical schools in the UK.
We will summarise, write up, distribute to participants and leaders in medical education (such as the GMC) and submit for publication the results of this survey. We hope that the findings will help to inform the future development of medical education.
The project has ethical approval from UCL Research Ethics Committee, Project ID: 7979/002. All answers will be collated only by the research team (the three people) and will remain anonymous. By completing the survey you give your consent to participation in this research project. You may withdraw from the study (either by discontinuing answering the survey or by emailing sarah.walpole@hyms.ac.uk to ask for your responses to be withdrawn) at any time and there will be no penalty.
There are two pages to the survey. Please answer as many of the questions as you can. Please leave any questions or comments that you may have along with your contact details at the end of the survey.
Declarations
Competing Interests
None declared.
Funding
Funding for the online survey platform was provided by UCL. No further funding of sponsorship was required.
Ethical approval
The project had ethical approval from University College London Research Ethics Committee, Project ID: 7979/002.
Guarantor
AB
Contributorship
SW, PT and AB all contributed to design of the study and the online questionnaire survey. SW conducted the survey, collected the data, performed preliminary analysis and formulated the first draft. All co-authors contributed to the final manuscript.
Provenance
Not commissioned; peer-reviewed by Michael Pearson
References
- 1.Devitt N, Murphy J. A survey of the information management and technology training needs of doctors in an acute NHS trust in the United Kingdom. Health Info Libr J 2004; 21: 164–172. [DOI] [PubMed] [Google Scholar]
- 2.Murphy J, Stramer K, Clamp S, Grubb P, Gosland J, Davis S. Health informatics education for clinicians and managers – what’s holding up progress? Int J Med Inform 2004; 73: 205–213. [DOI] [PubMed] [Google Scholar]
- 3.Shortell SM, Weist EM, Sow M-SK, Foster A, Tahir R. Implementing the Institute of Medicine’s recommended curriculum content in schools of public health: a baseline assessment. Am J Public Health 2004; 94: 1671–1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krause ND, Roulette GD, Papp KK, Kaelber D. Assessing medical informatics confidence among 1st and 2nd year medical students. AMIA Annu Symp Proc 2006; 989. [PMC free article] [PubMed] [Google Scholar]
- 5.NHS Commissioning Board. Everyone counts: planning for patients 2013/14, London: NHS, 2013. [Google Scholar]
- 6.UK Department of Health. Review of information technology in NHS: announcement of government review, https://www.gov.uk/government/news/review-of-information-technology-in-nhs (2016, accessed 10 May 2016).
- 7.UK Council for Health Informatics Professions (UKCHIP) What is Health Informatics? http://www.ukchip.org/?page_id=1512 (accessed 13 October 2015).
- 8.Greenhalgh T, Howick J, Maskrey N. Evidence based medicine: a movement in crisis? BMJ 2014; 13: g3725–g3725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Foley T, Franchi E, Gassert CA, et al. Health Information Management and Informatics Core Competencies for Individuals Working. Chicago, 2008, www.ahima.org (accessed 10 May 2016).
- 10.Mantas J, Ammenwerth E, Demiris G, et al. Recommendations of the International Medical Informatics Association (IMIA) on education in biomedical and health informatics. Methods Inf Med 2010; 49: 105–120. [DOI] [PubMed] [Google Scholar]
- 11.GMC. Outcomes for graduates; outcomes 2 – the doctor as a practitioner. London, 2015, http://www.gmc-uk.org/education/undergraduate/undergrad_outcomes_2.asp (accessed 10 May 2016).
- 12.Embedding Informatics in Clinical Education Team. Learning to Manage Health Information: a theme for clinical education 2012, London: NHS, 2012. [Google Scholar]
- 13.Royal College of Physicians, Department of Health. Embedding informatics in clinical education, http://www.eiceresources.org/ (2009, accessed 10 May 2016).
- 14.Medical Schools Council. UK Medical Schools A-Z, http://www.medschools.ac.uk/Students/UKMedicalSchools/Pages/UK-Medical-Schools-A-Z.aspx (2016, accessed 3 March 2016).
- 15.HSCIC. Learning to manage health information: education and training standards version 5, http://www.eiceresources.org/learning-to-manage (2015, accessed 13 October 2015).
- 16.Röhrig R, Stausberg J, Dugas M. Development of national competency-based learning objectives ‘medical informatics’ for undergraduate medical education. Methods Inf Med 2013; 52: 184–188. [DOI] [PubMed] [Google Scholar]
- 17.Liu X, Wang Z. Information literacy education for medical students in China. Med Educ 2009; 43: 818–818. [DOI] [PubMed] [Google Scholar]
- 18.Holmboe ES, Sherbino J, Long DM, Swing SR, Frank JR. The role of assessment in competency-based medical education. Med Teach 2010; 32: 676–682. [DOI] [PubMed] [Google Scholar]