Abstract
Importance
Obesity before and during pregnancy increases risk among mothers for poor health outcomes, such as diabetes, high blood pressure, and cardiovascular disease.
Objective
To describe trends in pre-pregnancy obesity rates among women in Wisconsin.
Methods
Cross-sectional data from Wisconsin birth certificates were analyzed. Prevalence of pre-pregnancy obesity (defined as body mass index = 30) among Wisconsin women who gave birth from 2011 through 2014 was compared across demographic and geographic dimensions.
Results
Overall, 27.8% of Wisconsin women who gave birth during 2011–2014 were obese. Obesity rates were highest among 40- to 44-year-old women (31.8%), women with a high school/GED diploma (32.8 %), American Indian/Alaska Native women (43.9%), and women with 5 or more pregnancies (35.4%). Obesity rates varied by county of residence (highest in Forest County, 45.2%) and city of residence (highest in the city of Racine, 34.8%).
Conclusions
There are significant socioeconomic, racial, and geographic disparities in pre-pregnancy obesity among women who give birth in Wisconsin.
INTRODUCTION
Obesity rates of 31.8% have been reported recently among women ages 20 to 39.1 This creates a public health concern because obese women are more likely to enter pregnancy with hypertension or diabetes—both which increase pregnancy risks. During pregnancy, gestational diabetes, preeclampsia, and cesarean section are more common among obese women, as well as spontaneous abortion and unexplained stillbirth.2 Furthermore, gestational weight gain, gestational diabetes, and smoking during pregnancy increase risk for childhood obesity.3 Although childhood obesity is well researched, there remains a dearth of research describing pre-pregnancy obesity trends. Our objective is to describe these trends among Wisconsin women, which should inform further research and community initiatives to improve the health of women and children across the life course.
METHODS
We used cross-sectional data from 2011 through 2014, published in the Wisconsin Interactive Statistics on Health (WISH) database by the Wisconsin Department of Health Services.4 The sample was limited to women who gave birth during 2011–2014, as these were the only years that included information on pre-pregnancy body mass index (BMI). Data from the WISH system came from resident birth certificates, vital records/electronic health records, the Office of Health Informatics, Division of Public Health, and the Wisconsin Department of Health Services. Pre-pregnancy BMI was calculated by the database curators using the mother’s height and weight, which are often reported retrospectively within the first trimester.4
For all births during or after 2011, the data system grouped races and ethnicities into 7 categories: white (non-Hispanic), Black/African American (non-Hispanic), American Indian/Alaska Native (non-Hispanic), Hispanic, Laotian/Hmong (non-Hispanic), other (non-Hispanic), and 2 or more races (non-Hispanic). The highest education level of mothers also was collected on the birth certificate and grouped into 6 categories: 8th grade or less, some high school, high school graduate/GED certificate, some college, college graduate, and post-graduate. Number of previous pregnancies includes live births, miscarriages, and other outcomes.5
The relationships between pre-pregnancy obesity (defined as a BMI ≥ 30) and 7 demographic variables were examined. These variables were race/ethnicity, maternal education, age, number of previous pregnancies, county, city, and ZIP code. The tables provided by the query system were then used to calculate the crude obesity prevalence as a function of each demographic variable. Rates for obesity by race/ethnicity were adjusted by age to control for confounding effects that may result from differences in rates of teen pregnancies across the demographic strata, as prevalence of obesity increased with age.5
RESULTS
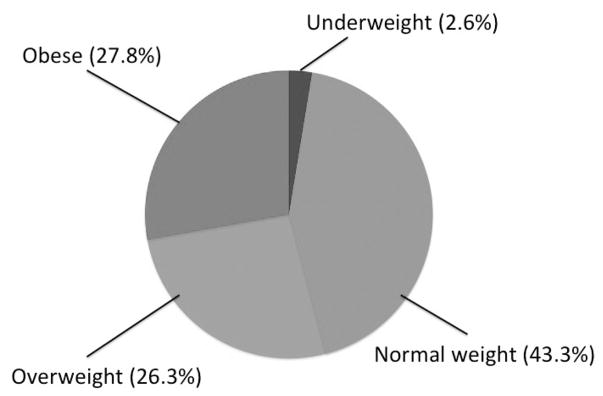
There were 268,655 live births documented between 2011 and 2014. Of these, 4,301 were missing data for BMI and were excluded from the analysis, leaving 264,354 births in the analytic sample. As shown in Figure 1, among the women who gave birth in Wisconsin during 2011–2014, 27.8% were obese. Table 1 shows the prevalence of pre-pregnancy obesity by race/ethnicity, education, age, and number of previous pregnancies. Tables 2 and 3 show the prevalence of pre-pregnancy obesity by geographic location, including all Wisconsin counties and the 38 most populous Wisconsin cities. Finally, Figure 2 illustrates the variation in average pre-pregnancy BMI across Wisconsin by county, as well as by ZIP codes within the city of Milwaukee.
Figure 1.
Pre-pregnancy Body Mass Index (BMI) Distribution Among Women Giving Birth in Wisconsin, 2011–2014
Table 1.
Body Mass Index (BMI) Distribution by Race/Ethnicity, Education, Age, and Number of Previous Pregnancies Among Women Giving Birth in Wisconsin, 2011–2014
| No. of Births | Obesity % (Crude) | Obesity % (Age-Adjusted) | |
|---|---|---|---|
| Age | |||
| <15 years | 166 | 10.8 | — |
| 15–19 years | 3,989 | 15.1 | — |
| 18–19 years | 11,387 | 21.0 | — |
| 20–24 years | 54,561 | 27.9 | — |
| 25–29 years | 83,639 | 28.3 | — |
| 30–34 years | 75,369 | 27.6 | — |
| 35–39 years | 29,215 | 30.8 | — |
| 40–44 years | 5,678 | 31.8 | — |
| 45+ years | 350 | 27.7 | — |
| Educationa | |||
| 8th grade or less | 9,376 | 23.1 | 22.6 |
| Some high school | 22,261 | 30.0 | 36.3 |
| High school graduate/GED diploma | 65,265 | 32.8 | 35.1 |
| Some college | 80,309 | 32.4 | 32.3 |
| College graduate | 58,997 | 21.4 | 20.6 |
| Post-graduate | 27,364 | 16.3 | 17.2 |
| Race/Ethnicityb | |||
| White | 194,089 | 26.6 | 26.4 |
| Black (non-Hispanic) | 24,710 | 38.2 | 43.0 |
| American Indian/Alaska Native | 2,839 | 43.9 | 46.4 |
| Hispanic | 25,007 | 30.7 | 32.8 |
| Laotian/Hmong | 6,215 | 21.0 | 29.5 |
| Other | 6,438 | 11.3 | 11.3 |
| 2 or more races (non-Hispanic) | 4,866 | 31.2 | 32.8 |
| Parity (number of previous pregnancies)c | |||
| 0 | 79,597 | 23.9 | 24.8 |
| 1 | 74,891 | 27.1 | 27.0 |
| 2 | 48,980 | 29.0 | 28.7 |
| 3 | 27,982 | 31.5 | 30.8 |
| 4 | 14,894 | 33.1 | 32.3 |
| 5 | 17,670 | 35.4 | 35.4 |
Excludes 782 women with missing education data.
Excludes 190 women with missing race/ethnicity data.
Excludes 340 women with missing parity data.
Table 2.
Body Mass Index (BMI) Distribution by County Among Women Giving Birth in Wisconsin, 2011–2014
| County | No. of Births | % Obese | Rank |
|---|---|---|---|
| Ozaukee | 3,223 | 20.3 | 1 |
| Dane | 24,325 | 21.6 | 2 |
| Waukesha | 14,942 | 21.9 | 3 |
| La Crosse | 4,991 | 23.0 | 4 |
| Florence | 112 | 25.2 | 5 |
| Vernon | 1,631 | 25.3 | 6 |
| Washington | 5,272 | 25.3 | 7 |
| St. Croix | 4,106 | 25.6 | 8 |
| Eau Claire | 4,685 | 25.9 | 9 |
| Walworth | 4,107 | 26.1 | 10 |
| Sauk | 2,921 | 26.3 | 11 |
| Marinette | 1,518 | 26.9 | 12 |
| Grant | 2,119 | 26.9 | 13 |
| Sheboygan | 4,972 | 27.7 | 14 |
| Brown | 13,539 | 27.8 | 15 |
| Sawyer | 649 | 28.1 | 16 |
| Clark | 2,256 | 28.3 | 17 |
| Green Lake | 798 | 28.4 | 18 |
| Polk | 1,684 | 28.4 | 19 |
| Milwaukee | 54,862 | 28.4 | 20 |
| Kenosha | 7,756 | 28.6 | 21 |
| Burnett | 505 | 28.6 | 22 |
| Portage | 2,756 | 28.6 | 23 |
| Manitowoc | 3,315 | 28.7 | 24 |
| Dunn | 1,797 | 28.8 | 25 |
| Green | 1,551 | 28.8 | 26 |
| Iron | 154 | 28.9 | 27 |
| Waushara | 906 | 29.0 | 28 |
| Wood | 3,251 | 29.1 | 29 |
| Outagamie | 8,978 | 29.2 | 30 |
| Rock | 7,517 | 29.3 | 31 |
| Trempealeau | 1,545 | 29.4 | 32 |
| Jefferson | 3,563 | 29.4 | 33 |
| Columbia | 2,377 | 29.4 | 34 |
| Barron | 2,055 | 29.4 | 35 |
| Calumet | 2,197 | 29.6 | 36 |
| Pierce | 1,492 | 29.8 | 37 |
| Kewaunee | 776 | 30.0 | 38 |
| Douglas | 1,637 | 30.1 | 39 |
| Rusk | 560 | 30.1 | 40 |
| Iowa | 1,060 | 30.2 | 41 |
| Door | 777 | 30.3 | 42 |
| Fond du Lac | 4,390 | 30.4 | 43 |
| Marathon | 6,409 | 30.5 | 44 |
| Bayfield | 497 | 30.7 | 45 |
| Jackson | 970 | 30.8 | 46 |
| Monroe | 2,358 | 30.8 | 47 |
| Washburn | 599 | 31.0 | 48 |
| Racine | 9,458 | 31.2 | 49 |
| Marquette | 606 | 31.4 | 50 |
| Winnebago | 7,405 | 31.6 | 51 |
| Waupaca | 2,067 | 31.6 | 52 |
| Dodge | 3,320 | 31.8 | 53 |
| Ashland | 697 | 31.9 | 54 |
| Richland | 696 | 32.0 | 55 |
| Chippewa | 2,815 | 32.2 | 56 |
| Pepin | 306 | 32.6 | 57 |
| Oneida | 1,199 | 33.1 | 58 |
| Oconto | 1,402 | 33.1 | 59 |
| Lafayette | 834 | 33.4 | 60 |
| Adams | 524 | 33.5 | 61 |
| Taylor | 884 | 34.0 | 62 |
| Price | 429 | 34.2 | 63 |
| Langlade | 775 | 34.4 | 64 |
| Crawford | 646 | 34.6 | 65 |
| Juneau | 1,082 | 35.8 | 66 |
| Shawano | 1,686 | 35.9 | 67 |
| Lincoln | 1,042 | 36.7 | 68 |
| Buffalo | 542 | 36.9 | 69 |
| Vilas | 711 | 37.8 | 70 |
| Menominee | 324 | 41.1 | 71 |
| Forest | 439 | 45.2 | 72 |
Excludes 5 women with missing county identifier.
Table 3.
Body Mass Index (BMI) Distribution by City Among Women Giving Birth in Wisconsin, 2011–2014
| City | No of Births | % Obese | Rank |
|---|---|---|---|
| Mequon/Thiensville | 772 | 13.7 | 1 |
| Wauwatosa | 2,443 | 14.2 | 2 |
| Brookfield | 1,261 | 15.3 | 3 |
| New Berlin | 1,405 | 18.8 | 4 |
| Franklin | 1,341 | 19.2 | 5 |
| Oak Creek | 1,703 | 20.0 | 6 |
| Fitchburg | 1,525 | 20.2 | 7 |
| Menomonee Falls | 1,419 | 20.8 | 8 |
| Madison | 12,251 | 21.3 | 9 |
| Muskego | 822 | 22.1 | 10 |
| De Pere | 1,620 | 22.8 | 11 |
| Caledonia | 596 | 23.0 | 12 |
| Mount Pleasant | 731 | 23.8 | 13 |
| Greenfield | 1,504 | 24.0 | 14 |
| La Crosse | 2,355 | 24.2 | 15 |
| Sun Prairie | 1,988 | 25.5 | 16 |
| South Milwaukee | 877 | 26.0 | 17 |
| Eau Claire | 3,456 | 26.1 | 18 |
| Steven’s Point | 1,289 | 26.2 | 19 |
| West Bend | 1,721 | 26.7 | 20 |
| Grand Chute | 269 | 27.1 | 21 |
| Waukesha | 3,962 | 28.1 | 22 |
| Manitowoc | 1,813 | 28.5 | 23 |
| Janesville | 3,308 | 29.2 | 24 |
| West Allis | 2,961 | 29.3 | 25 |
| Sheboygan | 2,823 | 29.8 | 26 |
| Green Bay | 8,473 | 29.8 | 27 |
| Appleton | 5,343 | 29.8 | 28 |
| Kenosha | 5,792 | 30.0 | 29 |
| Wausau | 2,528 | 30.0 | 30 |
| Oshkosh | 3,207 | 30.5 | 31 |
| Beloit | 2,195 | 31.0 | 32 |
| Milwaukee | 39,222 | 31.3 | 33 |
| Superior | 1,193 | 31.3 | 34 |
| Fond du Lac | 2,526 | 31.6 | 35 |
| Watertown | 1,168 | 33.2 | 36 |
| Neenah/Menasha | 2,765 | 34.0 | 37 |
| Racine | 5,781 | 34.8 | 38 |
Figure 2.
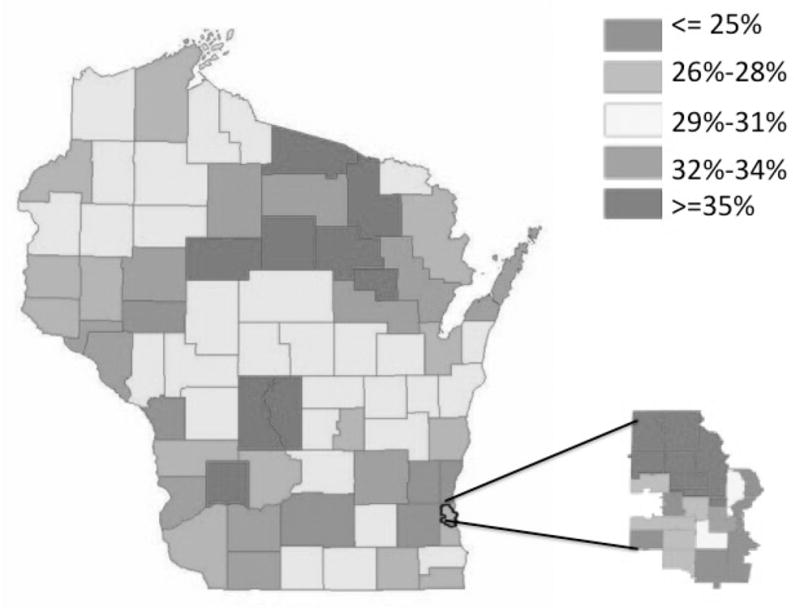
Pre-pregnancy Body Mass Index (BMI) Distribution by County and Milwaukee ZIP Code Among Women Giving Birth in Wisconsin, 2011–2014
Disparities in pre-pregnancy obesity by maternal age, education, race/ethnicity, and number of previous pregnancies
As shown in Table 1, rates of pre-pregnancy obesity increased with age, from a rate of 10.8% among teenagers less than 15 years old to a rate of 31.8% among 40- to 44-year-old women. Obesity rates were highest among women giving birth with a high school/GED diploma (32.8%). Overall, the rate of pre-pregnancy obesity decreased with increasing levels of maternal education, with the lowest rates of pre-pregnancy obesity among women with a post-graduate degree (16.3%). Obesity rates were highest among American Indian/Alaska Native (non-Hispanic) women giving birth (43.4%), followed by non-Hispanic black/African American women (38.2%), compared to Laotian/Hmong women with the lowest rate of pre-pregnancy obesity (21.0%). When adjusted for age, the magnitude of these racial disparities was even greater. Finally, women who had 5 or more previous pregnancies had the highest obesity rates when comparing by parity (35.4%). Overall, the pre-pregnancy obesity rate was higher among women with more children.
Disparities in pre-pregnancy obesity by geographic location
As highlighted in Tables 2 and 3, as well as Figure 2, our data indicated a stark contrast in pre-pregnancy obesity prevalence by Wisconsin county, city, and Milwaukee ZIP code of residence. As depicted in the map of Wisconsin counties (Figure 2), high prevalence of pre-pregnancy obesity among women giving birth is found in north-central and northeastern Wisconsin. Forest County had the highest pre-pregnancy obesity prevalence at 45.2%, whereas Ozaukee County had the lowest prevalence at 20.3%. Among Wisconsin’s 38 largest cities, Racine had the highest rate of pre-pregnancy obesity (34.8%) and Mequon/Thiensville had the lowest rate (13.7%).
DISCUSSION
The overall rate of pre-pregnancy obesity among women giving birth during 2011–2014 was 27.8%, which is lower than averages previously reported.1 However, our results show that pre-pregnancy obesity rates in Wisconsin vary significantly by demographic and geographic factors. The highest prevalence of pre-pregnancy obesity in Wisconsin is among American Indian/Alaska Native women and African American women. These results are consistent with previous research in Wisconsin6 and elsewhere in the United States.7,8 Furthermore, these trends highlight persistent disparities and inequality faced by American Indian and African American women in Wisconsin that are at least partially explained by the disproportionate economic hardship experienced by these racial/ethnic groups.
Parity and maternal age at the time of birth are closely related variables, and it is difficult to isolate the two influences in these data. Our results indicate that pre-pregnancy obesity rates were highest among mothers who already had 5 or more children. These results are consistent with previous research showing that parity is a strong, positive predictor of maternal obesity.9 The difficulty is that women who are older will likely have had more prior pregnancies than younger women giving birth. Because women tend not to lose all weight gained during each pregnancy, prior pregnancy likely results in a higher BMI, but it also is associated with greater age. Given that parity and maternal age are positively related, we also see a corresponding linear trend with increasing rates of obesity as maternal age increases.
Consistent with previous research, rates of pre-pregnancy obesity were generally greatest among women with less education in Wisconsin.10 Additionally, the stark socioeconomic disparities pertaining to pre-pregnancy obesity were best highlighted by our data enumerating pre-pregnancy obesity rates by geographic location. These data indicate that pre-pregnancy obesity affects both rural and urban impoverished populations. The finding that rates are highest among women in north-central and northeastern Wisconsin is not surprising, given the social, demographic, and racial composition of these counties.
The map of Milwaukee ZIP codes also provides elucidating information, as the ZIP codes with the highest rates of pre-pregnancy obesity are largely low-income, Black/African American non-Hispanic and Hispanic neighborhoods. These data highlight geographic areas that are most underserved in terms of pre-pregnancy obesity. Although it is outside the scope of this paper, these results may direct further research into food security, economic hardship, and the built environment to investigate related causes to the wide disparities in pre-pregnancy obesity in these counties, cities, and Milwaukee ZIP codes.
Strengths of this descriptive study include a large, diverse, and robust sample size. In addition, as these data are compiled from birth certificate data, future research may be able to access individual-level data in order to provide a more complete picture of pre-pregnancy obesity in Wisconsin, as well as examine the relationship between pre-pregnancy obesity of women and their children.
The results of this study should be considered in light of their limitations. First, mothers’ height and weight measurements may be obtained inconsistently by hospitals. Additionally, weight measurements are often obtained retrospectively in the first trimester and may not truly reflect the mother’s weight immediately prior to conception. Recent validation studies suggest that most hospitals record self-reported measurements from mothers, and these estimates can result in substantial misclassification of pre-pregnancy BMI.10 Finally, this cross-sectional data cannot establish a causal relationship between pre-pregnancy obesity and race/ethnicity, maternal education, age, number of previous pregnancies, county, city, and ZIP code. A multivariable analysis would control for confounding factors and may be useful in teasing apart the complexity of the variables used in this analysis; this presents a further direction of study.
These results have important implications with regards to the life course approach to epidemiology, which is an interdisciplinary framework that examines the long-term outcomes of exposures during gestation, childhood, adolescence, and adulthood.11 In 2013, Ehrenthal et al conducted a historical cohort study of mothers who gave birth between 2004 and 2007 and followed up with their children when they were 4 years old. Their results indicated that preconception risk factors of mothers—such as pre-pregnancy obesity—were more predictive of childhood obesity than prenatal factors.12 Therefore, promoting healthy BMI in women before pregnancy has the potential not only to increase the health of mothers, but also the health of their children.
Although these results can only highlight associations, they do point to populations within Wisconsin that are most in need of targeted intervention. Pre-pregnancy obesity is linked with complications that lead to extra procedures and extended hospital stays that incur higher medical costs than low-risk births. Additionally, there is a well-established relationship between increased BMI and incident chronic diseases such as hypertension, diabetes, and cardiovascular disease that incur higher health care costs. Recent studies have found these costs to be substantial. In a recent study published in 2015, the short-term economic burden of maternal overweight, gestational diabetes, and related conditions was estimated to be more than $1.8 billion. Although this estimate did not account for long-term consequences, it is reasonable to conjecture that the long-term economic costs present a burden to our country’s health care system as well.13 The relationship between pre-pregnancy obesity and direct/indirect health care costs presents another future research direction.
Obesity is complex and multifaceted. Biological, socioeconomic, and behavioral factors alone are unable to encompass the entire scope of obesity. However, our results indicate that pre-pregnancy obesity is associated with socioeconomic and geographic factors that are likely related. Given the direct health and economic burden to individual women, families, and communities, and that obesity in mothers increases the obesity risk in the next generation, further research and community interventions are needed.
Acknowledgments
We would like to extend our gratitude to Lisa Charron for her help preparing the map of Wisconsin.
Funding/Support: Funding for this project was provided by the University of Wisconsin School of Medicine and Public Health through the Wisconsin Partnership Program.
Footnotes
Financial Disclosures: None declared.
References
- 1.Declerq E, Macdorman M, Cabral H, Stotland N. Prepregnancy Body Mass Index and Infant Mortality in 38 U.S. States, 2012–2013. Obstet Gynecol. 2016;127(2):279–287. doi: 10.1097/AOG.0000000000001241. [DOI] [PubMed] [Google Scholar]
- 2.Leddy MA, Power ML, Schulkin J. The Impact of Maternal Obesity on Maternal and Fetal Health. Rev Obstet Gynecol. 2008;1(4):170–178. [PMC free article] [PubMed] [Google Scholar]
- 3.Portela DS, Vieira TO, Matos SM, Oliveira NFD, Vieira GO. Maternal obesity, environmental factors, cesarean delivery and breastfeeding as determinants of overweight and obesity in children: results from a cohort. BMC Pregnancy Childbirth. 2015;15:94. doi: 10.1186/s12884-015-0518-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WISH Query: Birth Counts Module. Wisconsin Department of Health Services; 2014. [Accessed Sept. 27, 2016]. https://www.dhs.wisconsin.gov/wish/birth/form.htm. [Google Scholar]
- 5.Definitions of Measures Used in Birth-Related Modules. Wisconsin Department of Health Services; [Accessed Sept. 27, 2016]. https://www.dhs.wisconsin.gov/wish/measures.htm. 20154. [Google Scholar]
- 6.Zeal C, Remington P, Ndiaye M, Stewart K, Stattelman-Scanlan D. The Epidemiology of Maternal Overweight in Dane County, Wisconsin. WMJ. 2014;113(1):24–27. [PubMed] [Google Scholar]
- 7.Ehrenberg HM, Dierker L, Milluzzi C, Mercer BM. Prevalence of maternal obesity in an urban center. Am J Obstet Gynecol. 2002;187(5):1189–1193. doi: 10.1067/mob.2002.127125. [DOI] [PubMed] [Google Scholar]
- 8.Broussard BA, Johnson A, Himes JH, et al. Prevalence of obesity in American Indians and Alaska Natives. Am J Clin Nutr. 1991;53(6 Suppl):1535S–1542S. doi: 10.1093/ajcn/53.6.1535S. [DOI] [PubMed] [Google Scholar]
- 9.Kim SY, Dietz PM, England L, Morrow B, Callaghan WM. Trends in Pre-pregnancy Obesity in Nine States, 1993–2003. Obesity. 2007;15(4):986–993. doi: 10.1038/oby.2007.621. [DOI] [PubMed] [Google Scholar]
- 10.Bodnar LM, Abrams B, Bertolet M, et al. Validity of Birth Certificate-Derived Maternal Weight Data. Paediatr Perinat Epidemiol. 2014;28(3):203–212. doi: 10.1111/ppe.12120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol. 2002;31(2):285–293. [PubMed] [Google Scholar]
- 12.Ehrenthal DB, Maiden K, Rao A, et al. Independent Relation of Maternal Prenatal Factors to Early Childhood Obesity in the Offspring. Obstet Gynecol. 2013;121(1):115–121. doi: 10.1097/aog.0b013e318278f56a. [DOI] [PubMed] [Google Scholar]
- 13.Lenoir-Wijnkoop I, Beek EMVD, Garssen J, Nuijten MJC, Uauy RD. Health economic modeling to assess short-term costs of maternal overweight, gestational diabetes, and related macrosomia—a pilot evaluation. Front Pharmacol. 2015;6:103. doi: 10.3389/fphar.2015.00103. [DOI] [PMC free article] [PubMed] [Google Scholar]