Abstract
Background and Objectives
Involvement in wartime combat often conveys a number of deleterious outcomes, including posttraumatic stress disorder (PTSD), depression, hostility aggression, and suicidal ideation. Less studied is the effect of engagement in wartime atrocities, including witnessing and perpetrating abusive violence.
Design and Methods
This study employed path analysis to examine the direct effects of involvement in wartime atrocities on hostility, aggression, depression, and suicidal ideation independent of combat exposure, as well as the indirect effects via guilt and PTSD symptom severity among 603 help-seeking male Vietnam War veterans.
Results
Involvement in wartime atrocities was predictive of increased guilt, PTSD severity, hostility, aggression, depressive symptoms, and suicidal ideation after controlling for overall combat exposure. Combat-related guilt played a minor role in mediating the effect of atrocity involvement on depression and suicidal ideation. PTSD severity had a larger mediational effect. However, it still accounted for less than half of the total effect of involvement in wartime atrocities on hostility, aggression, and suicidal ideation.
Conclusions
These findings highlight the heightened risk conveyed by involvement in wartime atrocities and suggest that the psychological sequelae experienced following atrocity involvement may extend well beyond guilt and PTSD.
Keywords: abusive violence, moral injury, guilt, posttraumatic stress disorder, depression, suicidal ideation
Introduction
The horrific toll of the Vietnam War is well-documented. At least 1 million (Lewy, 1978) and perhaps as many as 3 million Vietnamese civilians and combatants (Shenon, 1995) were killed during the 11-year conflict. Approximately 58,000 American servicemen were killed (Coffelt, Arnold, & Argabright, 2002), and another 300,000 were injured (Boyle, Decouflé, & O’Brien, 1989). Of those who returned, around 31% developed posttraumatic stress disorder (PTSD) (Kulka et al., 1990), a debilitating condition characterized by trauma re-experiencing, avoidance, negative cognitions and mood, and hyperarousal (American Psychiatric Association, 2013). Although the trauma precipitating PTSD is conventionally conceived of as unforeseeable and those it affects, as victims (Drescher et al., 2011), that is not always the case. For instance, researchers and clinicians have long documented cases of PTSD resulting from the perpetration of trauma, primarily stemming from involvement in wartime atrocities, such as those committed at My Lai (Breslau & Davis, 1987; Solomon, Zarcone, Yoerg, Scott, & Maurer, 1971; Yehuda, Southwick, & Giller, 1992). The inner conflict resulting from such wartime acts of commission or omission, termed “moral injury” (Drescher et al., 2011), has been the subject of renewed interest in recent years. Nevertheless, empirical work documenting the impact of involvement in wartime atrocities above and beyond PTSD is relatively scant and piecemeal. As such, the purpose of the present study was to devise and assess a comprehensive model linking involvement in wartime atrocities directly and indirectly to four broad domains of psychological and behavioral sequelae: guilt, PTSD, hostility and aggression, and depression and suicidal ideation.
The concept of moral injury stems from the premise that individuals have internalized standards of ethical behavior, or schemas (Drescher et al., 2011). When an individual engages in a morally reprehensible act, the discrepancy between behavior and personal schema creates a conflict, typically manifest as guilt (Lee, Scragg, & Turner, 2001). If one is unable to integrate the amoral act within existing self-schemas, the resulting conflict, or moral injury, may leave a lasting legacy (Horowitz, 1992). For instance, according to social-cognitive theories of PTSD (e.g., McCann & Pearlman, 1990), an individual who cannot assimilate amoral behaviors within extant cognitive structures is likely to experience intrusions (e.g., nightmares, unwelcome reminders of the trauma), hyperarousal, and distress, which in turn may stimulate the individual to actively avoid thoughts and situations that can trigger recall of the traumatic event. Although avoidance offers temporary relief of trauma-related distress, it can disrupt the recovery process by stymieing healthy integration of traumatic events via, for instance, the contextualization of amoral behaviors. As a result, perpetrators may accommodate, or alter, existing schemas, concluding that they themselves are inherently flawed and unworthy of forgiveness (Litz et al., 2009) and that social contracts of decency are untrustworthy (Drescher et al., 2011; Vargas, Hanson, Kraus, Drescher, & Foy, 2013).
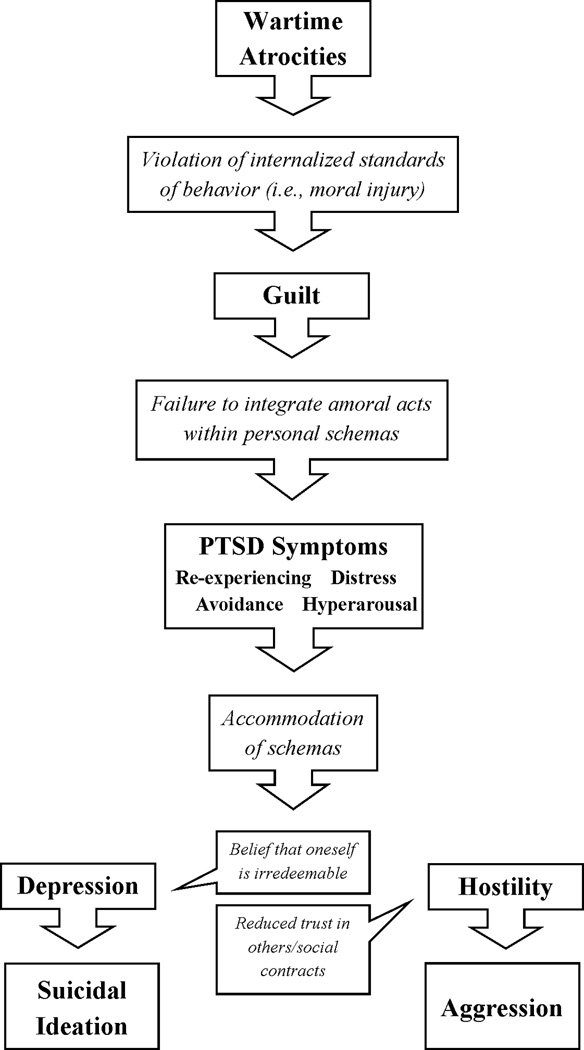
In an effort to assess the psychological and behavioral consequences of involvement in wartime atrocities, we have constructed a social-cognitive model of moral injury, integrating the above concepts with specific predictions concerning the development of guilt, PTSD, hostility, aggression, depression, and suicidal ideation (see Figure 1). According to our model, involvement in wartime atrocities, whether by acts of commission or omission, in most cases represents a violation of internalized standards of ethical behavior, thus qualifying as moral injury. This violation of personal standards, coupled with sense of responsibility for the event and perceived lack of justification for personal actions, results in guilt (Kubany & Manke, 1995). Indeed, empirical work indicates that degree of engagement in wartime atrocities experience is highly correlated with subsequent combat-related guilt (Beckham, Feldman, & Kirby, 1998; Marx et al., 2010).
Figure 1.
Social-cognitive model of moral injury.
Guilt may in turn precipitate the development of PTSD symptoms. When restitution is blocked or otherwise not possible, guilt-laden memories of the trauma may increasingly intrude upon daily life to the point that emotional processing of fear-based artifacts of the trauma are impeded (Ehlers & Steil, 1995; Joseph, Williams, & Yule, 1997; Riggs, Dancu, Gershuny, Greenberg, & Foa, 1992). This often leads to avoidance behaviors (e.g., social isolation, substance abuse) to escape feelings of guilt. Not only does chronic guilt tend to increase intrusions, distress, and avoidant coping—three hallmarks of PTSD—it also appears to hamper help-seeking and treatment response (Kubany & Manke, 1995; Owens, Chard, & Cox, 2008). In fact, empirical work indicates that involvement in wartime atrocities often conveys heightened PTSD symptom severity (Beckham et al., 1998; King, King, Gudanowski, & Vreven, 1995; Yehuda et al., 1992). Researchers have also found that participation in wartime atrocities is associated with increased odds of developing PTSD, independent of combat exposure (Breslau & Davis, 1987; Ferrajão & Oliveira, 2014).
If re-experiencing and intrusive symptoms of PTSD arise from the failure to integrate morally transgressive behavior into one’s internal schemas, resolution of this cognitive dissonance can be achieved in one of two ways (Litz et al., 2009): When an individual assimilates the traumatic event into her schema by attributing it to contextual, external factors, she may achieve moral repair without compromising sense of self and others. By contrast, when one accommodates his personal schemas by drawing global, stable attributions concerning the cause of the transgression, he perpetuates inner turmoil through the beliefs that he is unforgiveable (Litz et al., 2009) and that others may judge him and thus are untrustworthy (Vagas et al., 2013). Formation of these beliefs may in turn underlie depression (Drescher et al., 2011), self-harm (Litz et al., 2009), and hostility toward others (Owens et al., 2008).
Indeed, moral injury (Ferrajão & Oliveira, 2014) and combat-related guilt (Beckham et al., 1991; Fontana, Rosenheck, & Brett, 1992) have both been positively associated with depression symptoms. In turn, participation in wartime atrocities has been linked with increased suicidal ideation (Braš et al., 2007; Hiley-Young et al., 1995; Maguen et al., 2011; Maguen et al., 2012; Sher, 2009), with depression and PTSD symptoms partially mediating that link (Maguen et al., 2011). In one study of Vietnam veterans, guilt was the most prominent predictor of suicide attempts, over and above PTSD symptom severity and depression (Hendin & Haas, 1991). Similarly, a strong relationship between atrocity involvement and hostility (Strayer & Ellenhorn, 1975) has been found, as have associations between involvement in wartime atrocities and postmilitary acts of interpersonal violence (Beckham et al., 1997; Hiley-Young et al., 1995).
In the present study, we used path analysis to examine our social-cognitive model of moral injury. We specifically modeled the direct and indirect connections between involvement in wartime atrocities and guilt, PTSD, hostility, physical aggression, depression, and suicidal ideation to determine the extent and pathways by which atrocity involvement is associated with subsequent psychiatric and behavioral pathology.
Method
Participants and Procedures
The sample included 603 male combat veterans who sought services at a Veterans Affairs outpatient PTSD clinic between 1995 and 2000. Of these, 151 had been included in an earlier study on PTSD, involvement in wartime atrocities, guilt, and aggression (Beckham et al., 1998). Mean age was 51.00 years (SD = 5.71). Three hundred thirty-seven (56%) were African-American, 240 (40%), European-American. Mean education in years was 13.28 (SD = 2.14). Participants completed the following measures as part of their clinic evaluation.
Measures
Atrocities Exposure Subscale
Six items from the self-report Vietnam Era Stress Inventory (Wilson & Krauss, 1983) were used to capture participant involvement in the perpetration of war-time atrocities. Participants indicated on a scale of 1 (“never”) to 5 (“three or more times each week”) whether they were “directly involved as a participant” or were “indirectly involved as an observer” in “hurting”, “killing”, or “mutilating bodies of Vietnamese [civilians and soldiers (both Vietcong and NVA soldiers)] (e.g., cutting off ears, putting heads on sticks, placing bodies in grotesque positions)”. Although we considered constructing separate “witnessing” and “participating” scores, examination of the dimensionality of the data via Kabacoff’s (2003) SAS macro for parallel analysis (Horn, 1965; Humphreys & Montanelli, 1975) indicated a single latent factor underlying the six items in the scale. Thus, summary scores were generated by summing across all six items. Scale alpha was .87 in the present sample.
Combat Exposure Scale (CES)
Combat exposure was measured using the 7-item self-report CES (Keane et al., 1989). Respondents record the frequency with which they engaged in or were exposed to specific aspects of traditional combat on a range from 0 (“No/None/Never”) to 4 (“51+ times/76% or more/7 months or more”). Examples include “Were you ever under enemy fire?”, “How often did you fire rounds at the enemy?”, and “How often were you in danger of being injured or killed (i.e., pinned down, overrun, ambushed, near miss, etc.)?” The resulting items are then weighted and summed to produce a total score (ranging from 0 to 41). Scale alpha was .89 in the present sample.
Davidson Trauma Scale (DTS)
The self-report DTS (Davidson et al., 1997) was used to capture PTSD symptoms via 17 items. Each item measures the frequency (0, “not at all” to 4, “everyday”) and intensity (0, “not at all distressing” to 4, “extremely distressing”) of corresponding symptoms. Total symptom severity scores were calculated by summing frequency and intensity scores. Scale alpha was .95 in the present sample.
Beck Depression Inventory (BDI)
The BDI (Beck, Steer, & Brown, 1996) is a 21-item self-report questionnaire that measures attitudes and symptoms of depression. Respondents indicate the degree to which they experience or exhibit characteristics of depression along a four-point Likert scale, ranging from 0 to 3. A single item with responses ranging from “I don’t have any thoughts of killing myself” (0) to “I would kill myself if I had the chance” (3) was used to measure suicidal ideation. Amongst a subset of the sample who completed the Personality Assessment Inventory (Morey, 1991), this item was highly correlated with T-scores for the corresponding suicide clinical scale, r(50) = .62. The remaining 20 items were summed to construct a total depression score. Scale alpha was .90 in the present sample.
Trauma-Related Guilt Inventory (TRGI)
The 32-item self-report TRGI (Kubany et al., 1996) measures cognitive and emotional aspects of guilt associated with particular traumatic events. Respondents rate statements such as “I experience intense guilt that relates to what happened” on a scale of 0 (“extremely true/always true/always/extreme/extremely guilt”) to 4 (“not true at all/never true/never/none/not guilty at all”). Guilt was operationalized by summing four items corresponding to the global guilt subscale. In the present sample, scale alpha was .88.
Cook-Medley Hostility Scale
Hostility was measured using the short-form Cook-Medley Hostility Scale (Cook & Medley, 1954). Respondents complete 27 true/false self-report items reflecting their endorsement of items such as “I think most people would lie to get ahead” and “I have at times had to be rough with people who were rude or annoying”. A total hostility score was calculated by summing “true” responses. Scale alpha was .76 in the present sample.
Physical Aggression
Self-reported physical aggression was captured by the Violence subscale of the Conflict Tactics Scale (CTS; Straus, 1979). The CTS measures instances of verbal and physical aggression that occurred within the past year. Participants rate the frequency of 20 distinct events (e.g., insulting, slapping, beating up someone else) based on the following scale: 0 (“never”), 1 (“once”), 2 (“twice”), 3 (“3 to 5 times”), 4 (“6 to 10 times”), 5 (“11 to 20 times”), and 6 (“more than 20 times”). Consistent with prior applications of the CTS (e.g., Hasselmann & Reichenheim, 2006; Straus & Douglas, 2004), a 4-point ordinal scale of physical aggression was created, with a score of 0 reflecting no reported acts of physical aggression; 1, at least one occasion of minor physical aggression (i.e., throwing something at someone, or pushing, grabbing, shoving, or slapping someone); 2, one or more occasions of moderate physical aggression (i.e., biting, kicking, or punching someone); and 3, at least one act of violent physical aggression (i.e., beating up someone, threatening someone with a knife or gun, or using a knife or gun). Scale alpha across all 20 items was .91 in the present sample.
Data Analysis
Path analysis was used to test the hypothesized relationships. Path analysis is a multivariate method for examining direct and indirect effects within a causal model (Pedhazur, 1982). It is only prescribed when the proposed model is theoretically and empirically supported by previous research (Cook, Campbell, & Day, 1979). As such, the primary goal of path analysis is to estimate coefficients of modeled paths and determine goodness of fit, with good fit providing support for the proposed causal pathways. Given an ordinal dependent variable (aggression), modeling was performed using robust (mean- and variance-adjusted) weighted least squares method (WLSMV), available through Mplus 7. Model fit was evaluated using standard fit criteria (Hooper, Coughlan, & Mullen, 2008; Yu, 2002): root mean square error of approximation (RMSEA) ≤ .05, comparative fit index (CFI) ≥ 0.90, Tucker-Lewis Index (TLI) ≥ 0.95, and weighted root mean square residual (WRMR) ≤ 1.00. The chi-square test of model fit was also consulted, with non-significance indicative of minimal discrepancy between predicted and obtained covariance structures. Although others have distinguished between witnessing and participating in wartime atrocities in their analyses (Breslau & Davis, 1987; Ford, 1999; Huang & Kashubeck-West, 2015; Marx et al., 2010), there is an equal precedent for combining the two in a single measure of atrocity involvement (Beckham et al., 1998; King et al., 1995; McFall, Smith, Mackay, & Tarver, 1990; Yehuda et al., 1992). We opted for the latter given the strong correlation between witnessing and participating in wartime atrocities, r(601) = .77, p < .01.
The model was constructed as follows, proceeding from the first predictor in the model, combat exposure, to the final dependent variables, aggression and suicidal ideation: Direct paths were specified from combat exposure to involvement in wartime atrocities, from involvement to wartime atrocities to guilt, and from guilt to PTSD severity. Two diverging paths were then specified, one leading from PTSD severity to hostility and from hostility to aggression, the other leading from PTSD severity to depression and from depression to suicidal ideation. Variables were carried forward as predictors with each direct path such that aggression, for instance, was modeled as a function of combat exposure, atrocity involvement, guilt, PTSD severity, and hostility. In addition to these, indirect effects from each of the predictor variables to each of the outcome variables were modeled, with the exception of those proceeding directly from guilt to hostility and aggression. Those paths were not specified given little conceptual support for the direct linkage of guilt with hostility and aggression.
Where mediation of main effects was suggested, the significance of the indirect effects was tested via bootstrapped confidence intervals, which were generated using resampling with replacement (5,000 resamples). This method of mediation testing offers an advantage over conventional tests, such as Sobel’s z, because it does not penalize the estimate of the indirect effect for its inherent positive skew (Preacher & Hayes, 2008). Mediation is deemed significant when the resulting 95% confidence interval does not span 0.
Results
Scores on the CES indicated that the sample as a whole experienced moderate to heavy combat (see Table 1). Ninety-one percent of participants (n = 546) reported witnessing or participating in wartime atrocities. Seventy-six percent (n = 458) participated directly in killing, with 31% of veterans (n = 188) reporting that they participated in the mutilation of bodies. In turn, the mean DTS and BDI scores reflected high levels of PTSD and depression symptoms in the sample: The cutoff for PTSD is 40 (Davidson et al., 1997), and a total BDI score over 28—the sample BDI mean with the suicidal ideation item included was 28.50—is indicative of severe depression (Beck et al., 1996). According to the CTS, 41% of participants (n = 249) reported engaging in at least one act of violent aggression in the previous 12 months; 6% (n = 38), moderate aggression; 20% (n = 119), minor aggression; and 33% (n = 197), no aggression. Aside from the non-significant association of combat exposure with suicidal ideation, all of the study variables were positively intercorrelated (see Table 1).
Table 1.
Scale Means, Standard Deviations, and Intercorrelations
| Mean (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|---|
| Combat Exp (1) | 25.94 (10.76) | - | ||||||
| Atrocities (2) | 9.75 (6.56) | .70** | - | |||||
| DTS Total (3) | 92.79 (28.11) | .26** | .33** | - | ||||
| BDI Total (4) | 27.77 (11.21) | .23** | .27** | .66** | - | |||
| Guilt (5) | 2.46 (1.10) | .30** | .35** | .43** | .40** | - | ||
| Hostility (6) | 18.87 (4.64) | .15** | .18** | .28** | .35** | .10* | - | |
| Suic Ideation (7) | 0.73 (0.66) | .05 | .13** | .36** | .53** | .22** | .21** | - |
| Phys Aggression | 1.55 (1.32) | .11** | .17** | .29** | .26** | .11** | .29** | .17** |
Note. Spearman’s rank correlations reported for correlations involving Phys Aggression. Combat Exp = Combat exposure, DTS Total = Davidson Trauma Scale total, BDI Total = Beck Depression Inventory total, Suic Ideation = suicidal ideation, Phys Aggression = physical aggression.
p < .05,
p < .01
Path Analysis
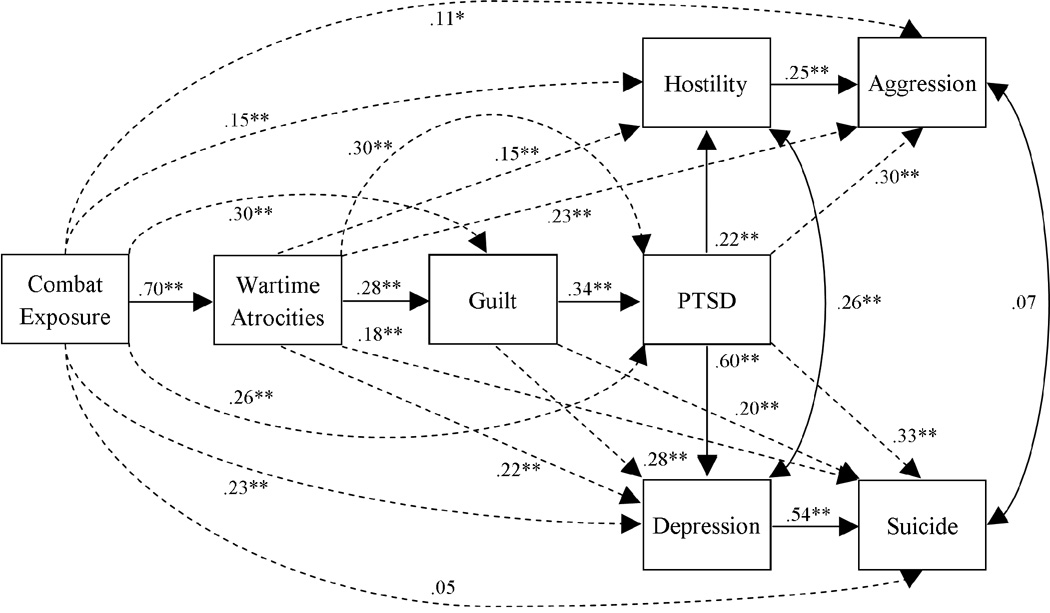
The results of the path analysis are presented in Figure 2. Model fit was good according to all five indices: RMSEA = .021 (90% CI: .000 to .068), CFI = 0.999, TLI = 0.992, WRMR = 0.248, and X2(4) = 5.074, p = .28. Combat exposure was directly associated with involvement in wartime atrocities, guilt, PTSD severity, hostility, aggression, and depression severity. Only the unadjusted relationship between combat exposure and suicidal ideation failed to reach significance. As predicted, involvement in wartime atrocities was positively associated with guilt, PTSD severity, hostility, aggression, depression severity, and suicidal ideation, suggesting potential mediation of the effect of combat exposure on all variables except suicidal ideation. Similarly, guilt was independently associated with PTSD severity, depression severity, and suicidal ideation. PTSD severity was directly associated with hostility and aggression as well as depression severity and suicidal ideation. Finally, hostility and depression severity were independently associated with aggression and suicidal ideation, respectively, after controlling for all other variables. Overall, the model explained 49% of the variance in involvement in wartime atrocities, 13% of the variance in guilt, 21% of the variance in PTSD symptom severity, 8% of the variance in hostility, 18% of the variance in self-reported aggression, 46% of the variance in depression severity, and 29% of the variance in suicidal ideation.
Figure 2.
Path analysis model of influence of involvement in wartime atrocities on PTSD, aggression, and suicide. Solid lines represent direct effects after controlling for predictors entered earlier in the model. Dashed lines represent unadjusted direct effects (i.e., direct effects not statistically adjusting for potential mediators/subsequently entered predictors). Numerical values are standardized effects.
*p < .05, **p < .01. N = 599.
Mediation Analyses
The results of the bootstrapped mediation analyses are reported in Tables 2–6. As predicted, the link between combat exposure and PTSD symptom severity was significantly—and nearly entirely—mediated by involvement in wartime atrocities. Guilt was a significant, albeit modest, mediator of the relationship between involvement in wartime atrocities and PTSD severity. The association between combat exposure and hostility was significantly mediated, primarily via atrocity involvement and PTSD symptom severity. Likewise, the association between involvement in wartime atrocities and hostility was significantly mediated, although only moderately so, by PTSD severity.
Table 2.
Standardized Direct and Indirect Effects on Guilt and PTSD (Results from Bootstrapping Analysis)
| Effect Pathway | Direct β (95% CI) | Indirect β (95% CI) |
|---|---|---|
| Combat Exp → Atrocities → Guilt | .11 (−.01 to .22) | .19 (.12 to .27) |
| Atrocities → Guilt → PTSD | .20 (.11 to .30) | .09 (.05 to .14) |
| Combat Exp → PTSD | .02 (−.09 to .12) | .24 (.17 to .31) |
| Combat Exp → Atrocities → PTSD | .14 (.07 to .21) | |
| Combat Exp → Guilt → PTSD | .04 (−.00 to .08) | |
| Combat Exp → Atrocities → Guilt → PTSD | .07 (.03 to .10) |
Note. Significant effects (as determined by 95% bootstrapped confidence intervals) are bolded. Combat Exp = combat exposure, PTSD = posttraumatic stress disorder.
Table 6.
Standardized Direct and Indirect Effects on Suicidal Ideation (Results from Bootstrapping Analysis)
| Effect Pathway | Direct β (95% CI) | Indirect β (95% CI) |
|---|---|---|
| PTSD → Depression → Suicide | .01 (−.08 to .10) | .32 (.25 to .40) |
| Guilt → Suicide | .02 (−.07 to .10) | .18 (.13 to .24) |
| Guilt → PTSD → Suicide | .00 (−.03 to .03) | |
| Guilt → Depression → Suicide | .07 (.03 to .11) | |
| Guilt → PTSD → Depression → Suicide | .11 (.07 to .15) | |
| Atrocities → Suicide | .05 (−.06 to .16) | .13 (.06 to .19) |
| Atrocities → Guilt → Suicide | .00 (−.02 to .03) | |
| Atrocities → PTSD → Suicide | .00 (−.02 to .02) | |
| Atrocities → Depression → Suicide | .00 (−.05 to .05) | |
| Atrocities → Guilt → PTSD → Suicide | .00 (−.01 to .01) | |
| Atrocities → Guilt → Depression → Suicide | .02 (.01 to .04) | |
| Atrocities → PTSD → Depression → Suicide | .07 (.03 to .10) | |
| Atrocities → Guilt → PTSD → Depression → Suicide | .03 (.01 to .05) |
Note. Significant effects (as determined by 95% bootstrapped confidence intervals) are bolded. PTSD = posttraumatic stress disorder, Suicide = suicidal ideation.
The association between combat exposure and physical aggression was completely mediated, primarily via involvement in wartime atrocities. The association between wartime atrocities and physical aggression was significantly mediated, albeit modestly so, with each of the significant paths involving PTSD severity. Hostility in turn significantly mediated the association between PTSD and physical aggression, although it accounted for just 20% of their covariance.
Turning to depression, the association between combat exposure and depression was almost entirely mediated by each of the paths including atrocity involvement. In turn, the association between atrocity involvement and depression was almost entirely mediated, primarily by PTSD severity. Although combat exposure was not directly associated with suicidal ideation, involvement in wartime atrocities was. This path was explained in large part by PTSD severity and depression and, to a lesser degree, guilt. In turn, the path from guilt to suicidal ideation was almost entirely mediated, again primarily via a single pathway through PTSD severity and depression. Finally, the direct association between PTSD severity and suicidal ideation was all but completely mediated by depression symptoms, which accounted for 98% of the shared variance between PTSD severity and suicidal ideation.
Discussion
As early as 1974, Haley observed that witnessing or directly participating in wartime atrocities conferred a significant risk well beyond conventional “traumatic war neurosis” among Vietnam War veterans. Nevertheless, little empirical work documenting the impact of involvement in wartime atrocities above and beyond the effects of PTSD has been conducted in the intervening years. As such, the purpose of the present study was to undertake a comprehensive examination of the pathways by which involvement in wartime atrocities may affect combat-related guilt, PTSD severity, hostility, aggression, depression severity, and suicidal ideation, independent of combat exposure. In support of our social-cognitive model of moral injury (Figure 1), our statistical model provided a good fit to the data. Consistent with previous work (Beckham et al., 1998; King et al., 1995; Marx et al., 2010), involvement in wartime atrocities was associated with PTSD and depression symptom severity independent of combat exposure. In fact, atrocity involvement almost entirely mediated the association between combat exposure and PTSD and depression severity. In support of previous findings (Huang & Kashubeck-West, 2015; Marx et al., 2010), guilt accounted for a portion of the effect of involvement in wartime atrocities on PTSD and depression severity as well as on suicidal ideation. However, heightened PTSD symptom severity played a larger explanatory role than guilt, particularly in explaining the effect of atrocity involvement on depression severity. Finally, involvement in atrocities entirely mediated the association between combat exposure and physical aggression.
These findings highlight the extent to which involvement in wartime atrocities may convey greater psychological and behavioral risks above and beyond combat exposure. Even after controlling for combat exposure, involvement in wartime atrocities was significantly associated with greater PTSD severity, hostility, aggression, depression severity, and suicidal ideation. Although guilt was included in many of the significant paths linking combat exposure and involvement in atrocities with the aforementioned outcomes, it was not integral. For instance, as the sole mediator of the relationship between involvement in atrocities and PTSD, guilt only accounted for approximately one third of the covariance between the two. Guilt also accounted for just 17% of the association between atrocity involvement and depression. For no other associations was guilt a unique mediator. Instead, PTSD severity accounted for much of the influence of involvement in atrocities on hostility, aggression, depression severity, and suicidal ideation. This suggests that PTSD symptoms—whether re-experiencing, avoidance, numbing, or hyperarousal—rather than guilt, may drive much of the heightened risk associated with involvement in wartime atrocities.
That said, involvement in wartime atrocities was still significantly associated with hostility, aggression, and suicidal ideation even after controlling for PTSD severity. This would suggest that there is something uniquely injurious about participating in or witnessing wartime atrocities that is not entirely captured by either the conventional definition of PTSD or the construct of guilt. Our findings suggest that moral injury as a theoretical construct may help explain an important element of the trauma associated with exposure to atrocities. As researchers and clinicians have become more aware of the concept of moral injury, there has been a greater effort to develop corresponding treatments. For instance, a number of clinicians have recently proposed treatments that emphasize self-forgiveness and connection with a moral authority towards facilitating moral repair (Drescher et al., 2011; Litz et al., 2009; Maguen & Litz, 2012). However, research in the area of moral injury is scant, and, absent a universally accepted conceptualization of moral injury, treatment components will be difficult to develop and evaluate.
There are several limitations to the present study that bear mention. First and foremost is the cross-sectional nature of the data. Namely, it prohibits any definitive conclusions about the mechanisms linking involvement in atrocities to heightened aggression and suicidal ideation as well as their directionality. Moreover, any kind of transactional process amongst the observed variables—for instance, feedback between guilt and depressive symptoms—is impossible to capture with the present dataset. Such investigations are best addressed with longitudinal data. However, absent that, the current dataset provided strong empirical support for the investigated model.
The present analyses are similarly limited by the retrospective self-report nature of the data. In light of evidence that combat veterans with PTSD are prone to over-report their symptoms (Frueh, Hamner, Cahill, Gold, & Hamlin, 2000), it is possible that data from the present sample are biased such that current symptoms and past experiences may be exaggerated. That said, the means and frequencies reported here may not be entirely reliable. However, we do not anticipate that the covariances between the variables are subject to a systematic bias. That is, unless a subset of individuals exaggerated all of their experiences and symptoms, the relationships between variables theoretically should not be affected by an over-reporting bias.
That said, the composition of the present sample of exclusively male Vietnam veterans, plus the circumstances of their moral injury, involvement in wartime atrocities, places a decided limitation on the generalizability of the results. Moreover, the present sample was one characterized by severe PTSD, with a mean DTS score (92.79) nearly two standard deviations above the conventional cutoff score of 40 for PTSD. To the degree that the present results may extend to a younger sample of veterans of the wars in Iraq and Afghanistan remains an empirical question, yet one that merits further research.
There were also a number of limitations regarding the variables available for analysis. Although the present dataset was useful for examining the outcomes predicted by the social-cognitive model of moral injury, we were unable to test the proposed mechanisms driving these outcomes (e.g., violation of internalized standards of behavior, failure to integrate amoral acts within personal schemas). Thus, an important future direction would be to examine these mechanisms empirically, preferably using prospective longitudinal data.
Another limitation was the use of a single item to capture suicidal ideation. Ideally, a multiple-item scale would have been available for that purpose in order to convey greater reliability. Nevertheless, the item that was used (with responses ranging from “I don’t have any thoughts of killing myself” to “I would kill myself if I had the chance”) was unambiguously worded and demonstrated strong construct validity in the present sample. In any case, future investigations should incorporate a multi-item validated measurement of suicidal ideation.
One set of outcomes not explored in the present analyses due to lack of data is substance abuse. Although little research has been conducted on the association between involvement in wartime atrocities and subsequent drug and alcohol abuse, there is some evidence to suggest a link. For instance, Yager and colleagues (1984) found that Vietnam veterans who participated in wartime atrocities reported greater cannabis use than other veterans. Similarly, Wilk and colleagues (2010) found that involvement in wartime atrocities amongst Iraq War veterans increased the odds of screening positive for alcohol abuse and demonstrating alcohol-related behavioral problems by a factor of 1.61, even after controlling for psychiatric problems, exposure to injury and/or death, and killing/injuring others. Thus, potential substance misuse should be an additional consideration for researchers of combat-related PTSD and clinicians alike.
A final limitation is the implied measurement of moral injury. Although moral injury was introduced in the literature as early as 1974 (Haley, 1974), formal research on it is still in its infancy. Not until very recently have any instruments been developed to measure it. For instance, the Moral Injury Event Scale (MIES; Nash et al., 2013) and the Moral Injury Questionnaire – Military Version (MIQ-M; Currier et al., 2015) were not published until 2013 and 2015, respectively, well after the present dataset was collected. Until that time, researchers identified moral injury based on the nature of the trauma (namely that the traumatized violated moral or ethical standards) and associated guilt (for example, see Stein et al., 2012). In light of this and that the MIES and MIQ-M are predominantly composed of items reflecting violation of ethical standards via acts of omission or commission, we would argue that, by measuring involvement in wartime atrocities and combat-related guilt, we have in essence captured moral injury in a manner consistent with prior researchers. Nevertheless, the concept of moral injury is one that could benefit from further refinement, both within the present research and the field at large.
Conclusion
In sum, these findings highlight the extent to which involvement in wartime atrocities poses an increased risk for hostility, aggression, depression, and suicidal ideation. Although guilt and PTSD accounted for some of the heightened risk, the unique impact of atrocity involvement remained substantial. The implication is that treatments aimed at ameliorating PTSD symptoms may be insufficient for reducing risk of harm to others and self in cases of moral injury. It would be helpful to evaluate whether and how evidence-based psychotherapies for PTSD may address this dimension, and potentially develop treatment components or approaches that may specifically target moral injury.
Table 3.
Standardized Direct and Indirect Effects on Hostility (Results from Bootstrapping Analysis)
| Effect Pathway | Direct β (95% CI) | Indirect β (95% CI) |
|---|---|---|
| Atrocities → Hostility | .08 (−.03 to .19) | .07 (.03 to .10) |
| Atrocities → PTSD → Hostility | .05 (.02 to .07) | |
| Atrocities → Guilt → PTSD → Hostility | .02 (.01 to .03) | |
| Combat Exp → Hostility | .04 (−.07 to .14) | .12 (.04 to .19) |
| Combat Exp → Atrocities → Hostility | .06 (−.02 to .13) | |
| Combat Exp → PTSD → Hostility | .00 (−.02 to .03) | |
| Combat Exp → Atrocities → PTSD → Hostility | .03 (.01 to .05) | |
| Combat Exp → Guilt → PTSD → Hostility | .01 (−.00 to .02) | |
| Combat Exp → Atrocities → Guilt → PTSD → Hostility | .02 (.01 to .02) |
Note. Significant effects (as determined by 95% bootstrapped confidence intervals) are bolded. Combat Exp = combat exposure, PTSD = posttraumatic stress disorder.
Table 4.
Standardized Direct and Indirect Effects on Aggression (Results from Bootstrapping Analysis)
| Effect Pathway | Direct β (95% CI) | Indirect β (95% CI) |
|---|---|---|
| PTSD → Hostility → Aggression | .24 (.15 to .34) | .06 (.03 to .08) |
| Atrocities → Aggression | .12 (.01 to .24) | .11 (.06 to .16) |
| Atrocities → PTSD → Aggression | .05 (.02 to .08) | |
| Atrocities → Hostility → Aggression | .02 (−.01 to .05) | |
| Atrocities → Guilt → PTSD → Aggression | .02 (.01 to .04) | |
| Atrocities → PTSD → Hostility → Aggression | .01 (.00 to .02) | |
| Atrocities → Guilt → PTSD → Hostility → Aggression | .01 (.00 to .01) | |
| Combat Exp → Aggression | −.07 (−.19 to .04) | .19 (.10 to .27) |
| Combat Exp → Atrocities → Aggression | .09 (.01 to .17) | |
| Combat Exp → PTSD → Aggression | .00 (−.02 to .03) | |
| Combat Exp → Hostility → Aggression | .01 (−.02 to .04) | |
| Combat Exp → Atrocities → PTSD → Aggression | .03 (.01 to .06) | |
| Combat Exp → Guilt → PTSD → Aggression | .01 (−.00 to .02) | |
| Combat Exp → Atrocities → Hostility → Aggression | .01 (−.01 to .04) | |
| Combat Exp → PTSD → Hostility → Aggression | .00 (−.01 to .01) | |
| Combat Exp → Atrocities → Guilt → PTSD → Aggression | .02 (.01 to .03) | |
| Combat Exp → Atrocities → PTSD → Hostility → Aggression | .01 (.00 to .01) | |
| Combat Exp → Guilt → PTSD → Hostility → Aggression | .00 (−.00 to .01) | |
| Combat Exp → Atrocities → Guilt → PTSD → Hostility → Aggression | .00 (.00 to .01) |
Note. Significant effects (as determined by 95% bootstrapped confidence intervals) are bolded. Combat Exp = combat exposure, PTSD = posttraumatic stress disorder.
Table 5.
Standardized Direct and Indirect Effects on Depression (Results from Bootstrapping Analysis)
| Effect Pathway | Direct β (95% CI) | Indirect β (95% CI) |
|---|---|---|
| Atrocities → Depression | .01 (−.08 to .10) | .22 (.15 to .28) |
| Atrocities → Guilt → Depression | .04 (.01 to .06) | |
| Atrocities → PTSD → Depression | .12 (.06 to .18) | |
| Atrocities → Guilt → PTSD → Depression | .06 (.03 to .08) | |
| Combat Exp → Depression | .03 (−.06 to .11) | .20 (.12 to .28) |
| Combat Exp → Atrocities → Depression | .00 (−.06 to .07) | |
| Combat Exp → Guilt → Depression | .01 (−.00 to .03) | |
| Combat Exp → PTSD → Depression | .01 (−.05 to .07) | |
| Combat Exp → Atrocities → Guilt → Depression | .03 (.01 to .04) | |
| Combat Exp → Atrocities → PTSD → Depression | .09 (.04 to .13) | |
| Combat Exp → Guilt → PTSD → Depression | .02 (−.00 to .05) | |
| Combat Exp → Atrocities → Guilt → PTSD → Depression | .04 (.02 to .06) |
Note. Significant effects (as determined by 95% bootstrapped confidence intervals) are bolded. Combat Exp = combat exposure, PTSD = posttraumatic stress disorder.
Footnotes
Disclosure Statement
The authors have no competing interests, financial or otherwise, to report.
REFERENCES
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Beckham JC, Feldman ME, Kirby AC. Atrocities exposure in Vietnam combat veterans with chronic posttraumatic stress disorder: Relationship to combat exposure, symptom severity, guilt, and interpersonal violence. Journal of Traumatic Stress. 1998;11:777–785. doi: 10.1023/A:1024453618638. [DOI] [PubMed] [Google Scholar]
- Boyle CA, Decouflé P, O’Brien TR. Long-term health consequences of military service in Vietnam. Epidemiologic Reviews. 1989;11:1–27. doi: 10.1093/oxfordjournals.epirev.a036031. [DOI] [PubMed] [Google Scholar]
- Braš M, Lončar Z, Boban M, Gregurek R, Brajković L, Tomičić H, Kalenić B. Self-inflicted burns in patients with chronic combat-related post-traumatic stress disorder. Collegium Antropologicum. 2007;31:1173–1177. [PubMed] [Google Scholar]
- Breslau N, Davis GC. Posttraumatic stress disorder: The etiologic specificity of wartime stressors. American Journal of Psychiatry. 1987;144:578–583. doi: 10.1176/ajp.144.5.578. [DOI] [PubMed] [Google Scholar]
- Coffelt RD, Arnold RJ, Argabright D. An electronic database of combat area causalities. Washington, DC: National Archives and Records Administration; 2002. [Google Scholar]
- Cook TD, Campbell DT, Day A. Quasi-experimentation: Design and analysis issues for field settings. Boston: Houghton Mifflin; 1979. pp. 19–21. [Google Scholar]
- Cook WW, Medley DM. Proposed hostility and pharisaic-virtue scales for the MMPI. Journal of Applied Psychology. 1954;38:414–418. [Google Scholar]
- Currier JM, Holland JM, Drescher K, Foy D. Initial psychometric evaluation of the Moral Injury Questionnaire—Military version. Clinical Psychology and Psychotherapy. 2015;22:54–63. doi: 10.1002/cpp.1866. [DOI] [PubMed] [Google Scholar]
- Davidson JR, Book SW, Colket JT, Tupler LA, Roth S, David D, Feldman ME. Assessment of a new self-rating scale for post-traumatic stress disorder. Psychological Medicine. 1997;27:153–160. doi: 10.1017/s0033291796004229. [DOI] [PubMed] [Google Scholar]
- Drescher KD, Foy DW, Kelly C, Leshner A, Schutz K, Litz B. An exploration of the viability and usefulness of the construct of moral injury in war veterans. Traumatology. 2011;17:8–13. [Google Scholar]
- Ehlers A, Steil R. Maintenance of intrusive memories in posttraumatic stress disorder: A cognitive approach. Behavioural and Cognitive Psychotherapy. 1995;23:217–249. doi: 10.1017/S135246580001585X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrajão PC, Oliveira RA. Self-awareness of mental states, self-integration of personal schemas, perceived social support, posttraumatic and depression levels, and moral injury: A mixed-method study among Portuguese war veterans. Traumatology. 2014;20:277–285. [Google Scholar]
- Fontana A, Rosenheck R, Brett E. War zone traumas and posttraumatic stress disorder symptomatology. Journal of Nervous and Mental Disease. 1992;180:748–755. doi: 10.1097/00005053-199212000-00002. [DOI] [PubMed] [Google Scholar]
- Ford JD. Disorders of extreme stress following war-zone military trauma: Associated features of posttraumatic stress disorder or comorbid but distinct syndromes? Journal of Consulting and Clinical Psychology. 1999;67:3–12. doi: 10.1037//0022-006x.67.1.3. [DOI] [PubMed] [Google Scholar]
- Frueh BC, Hamner MB, Cahill SP, Gold PB, Hamlin KL. Apparent symptom overreporting in combat veterans evaluated for PTSD. Clinical Psychology Review. 2000;20:853–885. doi: 10.1016/s0272-7358(99)00015-x. [DOI] [PubMed] [Google Scholar]
- Hasselmann MH, Reichenheim ME. Parental violence and the occurrence of severe and acute malnutrition in childhood. Paediatric and Perinatal Epidemiology. 2006;20:299–311. doi: 10.1111/j.1365-3016.2006.00735.x. [DOI] [PubMed] [Google Scholar]
- Haley SA. When the patient reports atrocities: Specific treatment considerations of the Vietnam veteran. Archives of General Psychiatry. 1974;30:191–196. doi: 10.1001/archpsyc.1974.01760080051008. doi:0.1001/archpsyc.1974.01760080051008. [DOI] [PubMed] [Google Scholar]
- Hendin H, Haas AP. Suicide and guilt as manifestations of PTSD in Vietnam combat veterans. American Journal of Psychiatry. 1991;148:586–591. doi: 10.1176/ajp.148.5.586. [DOI] [PubMed] [Google Scholar]
- Hiley-Young B, Blake DD, Abueg FR, Rozynko V, Gusman FD. Warzone violence in Vietnam: An examination of premilitary, military, and postmilitary factors in PTSD in-patients. Journal of Traumatic Stress. 1995;8:125–141. doi: 10.1007/BF02105411. [DOI] [PubMed] [Google Scholar]
- Hooper D, Coughlan J, Mullen MR. Structural equation modelling: Guidelines for determining model fit. Journal of Business Research Methods. 2008;6:53–60. [Google Scholar]
- Horn JL. A rationale and technique for estimating the number of factors in factor analysis. Psychometrika. 1965;30:179–185. doi: 10.1007/BF02289447. [DOI] [PubMed] [Google Scholar]
- Horowitz MJ. The effects of psychic trauma on mind: Structure and processing of meaning. In: Barron IjW, Eagle MN, Wolitzky D., editors. Interface of psychoanalysis and psychology. Washington, DC: American Psychological Association; 1992. pp. 489–500. [Google Scholar]
- Huang H, Kashubeck-West S. Exposure, agency, perceived threat, and guilt as predictors of posttraumatic stress disorder in veterans. Journal of Counseling and Development. 2015;93:3–13. [Google Scholar]
- Humphreys LG, Montanelli RG., Jr An investigation of the parallel analysis criterion for determination of the number of common factors. Multivariate Behavioral Research. 1975;10:193–205. [Google Scholar]
- Joseph S, Williams R, Yule W. Understanding post-traumatic stress: A psychosocial perspective on PTSD and treatment. Chichester, UK: Wiley; 1997. [Google Scholar]
- Kabacoff RI. Determining the dimensionality of data: A SAS macro for parallel analysis; Proceedings of the 28th Annual Meeting of SAS Users Group International; Seattle, WA. 2003. [Retrieved 12 July 2016]. from http://www2.sas.com/proceedings/sugi28/090-28.pdf. [Google Scholar]
- Keane TM, Fairbank JA, Caddell JM, Zimering RT, Taylor KL, Mora CA. Clinical evaluation of a measure to assess combat exposure. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1989;1:53–55. [Google Scholar]
- King DW, King LA, Gudanowski DM, Vreven DL. Alternative representations of war zone stressors: Relationships to posttraumatic stress disorder in male and female Vietnam veterans. Journal of Abnormal Psychology. 1995;104:184–196. doi: 10.1037//0021-843x.104.1.184. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Gino A, Denny NR, Torigoe RY. Relationship of cynical hostility and PTSD among Vietnam veterans. Journal of Traumatic Stress. 1994;7:21–31. doi: 10.1007/BF02111909. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Haynes SN, Abueg FR, Manke FP, Brennan JM, Stahura C. Development and validation of the Trauma-Related Guilt Inventory (TRGI) Psychological Assessment. 1996;8:428–444. [Google Scholar]
- Kubany ES, Manke FP. Cognitive therapy for trauma-related guilt: Conceptual bases and treatment outlines. Cognitive and Behavioral Practice. 1995;2:27–61. [Google Scholar]
- Kulka RA, Schlenger WF, Fairbank JA, Hough RI, Jordan BK, Marmar CR, Weiss DS. Trauma and the Vietnam War generation: Report of findings from the National Vietnam Veterans Readjustment Study. New York: Brunner Mazel; 1990. [Google Scholar]
- Lee DA, Scragg P, Turner S. The role of shame and guilt in traumatic events: A clinical model of shame-based and guilt-based PTSD. British Journal of Medical Psychology. 2001;74:451–466. doi: 10.1348/000711201161109. [DOI] [PubMed] [Google Scholar]
- Lewy G. America in Vietnam. New York: Oxford University Press; 1978. [Google Scholar]
- Litz BT, Stein N, Delaney E, Lebowitz L, Nash WP, Silva C, Maguen S. Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clinical Psychology Review. 2009;29:695–706. doi: 10.1016/j.cpr.2009.07.003. [DOI] [PubMed] [Google Scholar]
- Maguen S, Litz B. Moral injury in the context of war. 2012 Retrieved from Department of Veterans Affairs website: http://www.ptsd.va.gov/professional/co-occurring/moral_injury_at_war.asp.
- Maguen S, Luxton DD, Skopp NA, Gahm GA, Reger MA, Metzler TJ, Marmar CR. Killing in combat, mental health symptoms, and suicidal ideation in Iraq war veterans. Journal of Anxiety Disorders. 2011;25:563–567. doi: 10.1016/j.janxdis.2011.01.003. [DOI] [PubMed] [Google Scholar]
- Maguen S, Metzler TJ, Bosch J, Marmar CR, Knight SJ, Neylan TC. Killing in combat may be independently associated with suicidal ideation. Depression and Anxiety. 2012;29:918–923. doi: 10.1002/da.21954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marx BP, Foley KM, Feinstein BA, Wolf EJ, Kaloupek DG, Keane TM. Combat-related guilt mediates the relations between exposure to combat-related abusive violence and psychiatric diagnoses. Depression and Anxiety. 2010;27:287–293. doi: 10.1002/da.20659. [DOI] [PubMed] [Google Scholar]
- McCann L, Pearlman LA. Psychological trauma and the adult survivor: Theory, therapy, and transformation. Philadelphia: Brunner/Mazel; 1990. [Google Scholar]
- McFall ME, Smith DE, Mackay PW, Tarver DJ. Reliability and validity of Mississippi Scale for Combat-Related Posttraumatic Stress Disorder. Psychological Assessment. 1990;2:114–121. [Google Scholar]
- McFall M, Fontana A, Raskind M, Rosenheck R. Analysis of violent behavior in Vietnam combat veteran psychiatric inpatients with posttraumatic stress disorder. Journal of Traumatic Stress. 1999;12:501–517. doi: 10.1023/A:1024771121189. [DOI] [PubMed] [Google Scholar]
- Morey LC. Personality Assessment Inventory: Professional manual. Tampa, FL: Psychological Assessment Resources; 1991. [Google Scholar]
- Nash WP, Marino Carper TL, Mills MA, Au T, Goldsmith A, Litz BT. Psychometric evaluation of the moral injury events scale. Military Medicine. 2013;178:646–652. doi: 10.7205/MILMED-D-13-00017. [DOI] [PubMed] [Google Scholar]
- Owens GP, Chard KM, Ann Cox T. The relationship between maladaptive cognitions, anger expression, and posttraumatic stress disorder among veterans in residential treatment. Journal of Aggression, Maltreatment & Trauma. 2008;17:439–452. [Google Scholar]
- Pedhazur EJ. Multiple regression in behavioral research: Explanation and prediction. 2nd. Fort Worth, TX: Holt, Rinehart, & Winston; 1982. [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Riggs DS, Dancu CV, Gershuny BS, Greenberg D, Foa EB. Anger and post-traumatic stress disorder in female crime victims. Journal of Traumatic Stress. 1992;5:613–625. [Google Scholar]
- Shenon P. 20 years after victory, Vietnamese communists ponder how to celebrate. 1993 Apr 23; Retrieved from http://www.nytimes.com. [Google Scholar]
- Sher L. A model of suicidal behavior in war veterans with posttraumatic mood disorder. Medical Hypotheses. 2009;73:215–219. doi: 10.1016/j.mehy.2008.12.052. [DOI] [PubMed] [Google Scholar]
- Solomon GF, Zarcone VP, Yoerg R, Scott NR, Maurer RG. Three psychiatric causalities from Vietnam. Archives of General Psychiatry. 1971;25:522–524. doi: 10.1001/archpsyc.1971.01750180042007. [DOI] [PubMed] [Google Scholar]
- Stein NR, Mills MA, Arditte K, Mendoza C, Borah AM, Resick PA, Litz BT. A scheme for categorizing traumatic military events. Behavior Modification. 2012;36:787–807. doi: 10.1177/0145445512446945. [DOI] [PubMed] [Google Scholar]
- Straus MA. Measuring intrafamily conflict and violence: The conflict tactics (CT) scales. Journal of Marriage and the Family. 1979;41:75–88. [Google Scholar]
- Straus MA, Douglas EM. A short form of the Revised Conflict Tactics Scales, and typologies for severity and mutuality. Violence and Victims. 2004;19:507–520. doi: 10.1891/vivi.19.5.507.63686. [DOI] [PubMed] [Google Scholar]
- Strayer R, Ellenhorn L. Vietnam veterans: A study exploring adjustment patterns and attitudes. Journal of Social Issues. 1975;31:81–93. [Google Scholar]
- Vargas AF, Hanson T, Kraus D, Drescher K, Foy D. Moral injury themes in combat veterans’ narrative responses from the National Vietnam Veterans’ Readjustment Study. Traumatology. 2013;19:243–250. [Google Scholar]
- Wilk JE, Bliese PD, Kim PY, Thomas JL, McGurk D, Hoge CW. Relationship of combat experiences to alcohol misuse among US soldiers returning from the Iraq war. Drug and Alcohol Dependence. 2010;108:115–121. doi: 10.1016/j.drugalcdep.2009.12.003. [DOI] [PubMed] [Google Scholar]
- Wilson JP, Krauss GE. Posttraumatic stress disorders (PTSD): Collected papers. Cleveland, OH: Cleveland State University; 1983. Vietnam era stress inventory. [Google Scholar]
- Yager T, Laufer R, Gallops M. Some problems associated with war experience in men of the Vietnam generation. Archives of General Psychiatry. 1984;41:327–333. doi: 10.1001/archpsyc.1984.01790150017003. [DOI] [PubMed] [Google Scholar]
- Yehuda R, Southwick SM, Giller EL. Exposure to atrocities and severity of chronic posttraumatic stress disorder in Vietnam combat veterans. American Journal of Psychiatry. 1992;149:333–336. doi: 10.1176/ajp.149.3.333. [DOI] [PubMed] [Google Scholar]
- Yu C-Y. Doctoral dissertation. Los Angeles: University of California; 2002. Evaluating cutoff criteria of model fit indices for latent variable models with binary and continuous outcomes. Retrieved from http://statmodel2.com/download/Yudissertation.pdf. [Google Scholar]