Abstract
Introduction
Endoscopic sinus surgery represents a cornerstone in the professional development of otorhinolaryngology trainees. Mastery of these surgical skills requires an understanding of paranasal sinus and skull base anatomy. The frontal sinus is associated with a wide range of variation and complex anatomical configuration, and thus represents an important challenge for all trainees performing endoscopic sinus surgery.
Methods
Forty-five otorhinolaryngology trainees and 20 medical school students from five academic institutions were enrolled and randomized into 1 of 2 groups. Each subject underwent learning of frontal recess anatomy with both traditional 2D learning methods using a standard DICOM viewing software (RadiAnt Dicom Viewer Version 1.9.16) and 3D learning utilizing a novel preoperative virtual planning software (Scopis Building Blocks), with half learning with the 2D method first and the other half learning with the 3D method first. Four questionnaires that included a total of twenty items were scored for subjects’ self-assessment on knowledge of frontal recess and frontal sinus drainage pathway anatomy following each learned modality. A two-sample Wilcoxon rank-sum test was used in the statistical analysis comparing the 2 groups.
Results
Most trainees (89%) believed that the virtual 3D planning software significantly improved their understanding of the spatial orientation of the frontal sinus drainage pathway.
Conclusion
Incorporation of virtual 3D planning surgical software may help augment trainees understanding and spatial orientation of the frontal recess and sinus anatomy. The potential increase in trainee proficiency and comprehension theoretically may translate to improved surgical skill and patient outcomes and in reduced surgical time.
Introduction
Endoscopic sinus surgery represents a key event in the professional development of otorhinolaryngology trainees. Mastery of these surgical skills requires a detailed understanding of paranasal sinus and skull base anatomy. The frontal sinus in particular is associated with a wide range of variation and complex anatomical configuration, and thus mastery of surgery for the frontal sinus is an important challenge for all trainees as they learn endoscopic sinus surgery.
Conventional learning and pre-surgical planning has traditionally involved review of two dimensional (2D) computed tomography images in a tri-planar format. For the novice trainee, this can create a challenge in thoroughly comprehending the three dimensional (3D) spatial orientation of the frontal recess and frontal sinus drainage pathway during endoscopic sinus surgery. In this study, we sought to evaluate the effectiveness of using a novel virtual three dimensional image viewing software to assist otolaryngology trainees in better understanding the anatomy and spatial orientation of the frontal recess and frontal sinus outflow tract.
Methods
A multi-institutional trial was conducted consisting of 45 otorhinolaryngology trainees and 20 medical school students from five academic institutions. Each subject underwent learning of frontal recess anatomy with both traditional 2D learning methods using a standard DICOM viewing software (RadiAnt Dicom Viewer Version 1.9.16 from Medixant, Pozan, Pland) and 3D learning utilizing a novel preoperative virtual planning software (Scopis Building Blocks Version 2.4.6 from Scopis GmbH, Berlin, Germany) The RadiAnt Dicom Viewer, which is available as a download directly from Medixant (http://www.radiantviewer.com/radiant-dicom-viewer-standard.php) presents the learner with conventional sagittal and coronal images that have been constructed from thin-cut axial data; the learner can scroll through images in each plane and adjust other parameters, including magnification and windows level/width settings (Figure 1). Scopis Building Blocks (SBB), which is available as a download from directly from Scopis (http://planning.scopis.com/#pricing) has a similar tool set, but also adds features that permit the learner to draw 3D boxes on relevant anatomic structures and to highlight the frontal sinus outflow pathway (Figure 2). Questionnaires that included a total of five items assessing the subjects’ knowledge of frontal recess and frontal sinus drainage pathway anatomy were completed by each subject preceding and following each learned modality (Figure 3). Statistical analysis comparing the 2 groups after the first learning methodology was performed with a two-sample Wilcoxon rank-sum test.
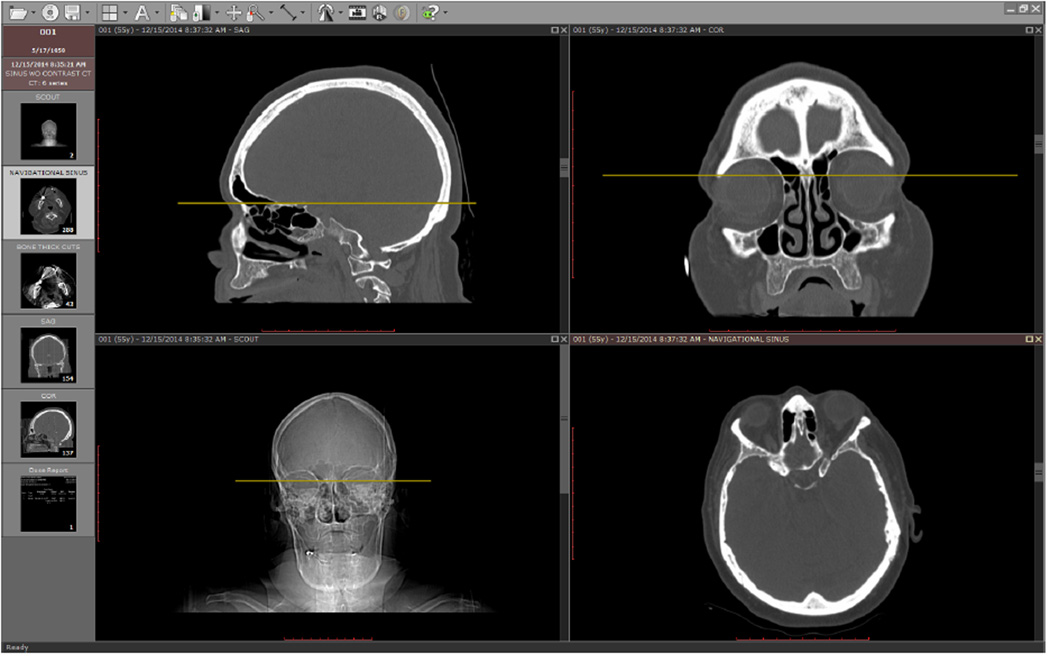
Figure 1.
The RadiAnt Dicom Viewer presents the user with conventional sagittal and coronal images that have been constructed from thin-cut axial imaging data. The learner can scroll through images in each plane and adjust other parameters, including magnification and window width/level settings.
Figure 2.
Scopis Building Blocks virtual planning 3 D software offers the user a conventional triplanar format as a platform for viewing the axial images as well as reconstructed coronal and sagittal images (left panel). In addition, software tools permit the addition of annotations of relevant structures at the discretion of the user (right panel). These tools permit the user to outline specific cells in the frontal recess by drawing boxes over them. Each annotation can be labeled and color-coded. Then, when scrolling though the scans, the user sees each annotation on each structure. Similarly, the user can draw the frontal sinus drainage pathway as a curvilinear line on the orthogonal CT scan images; this pathway is then projected with the other annotations.
Figure 3.
The self-assessment questionnaire developed for this study asked each learner to describe his or her ability to identify relevant frontal sinus and frontal recess anatomy.
Each trainee completed a pre-education self-assessment survey evaluating his or her understanding and knowledge of the frontal recess anatomy (Figure 3). All study participants then watched an educational video that reviewed frontal recess anatomy.(1) This video presentation (developed for the purposes of this project) summarized concepts of frontal sinus/recess anatomy as presented by Lee et al.(2) Subjects from each post-graduate year were then randomized to undergo either traditional 2D or 3D as their first learned modality. The 2D traditional learning consisted of review of a printed copy of the Lee et al. article on frontal recess and frontal sinus anatomy.(2) This was then followed by a 15 minute session reviewing sinus CT imaging using a standard DICOM viewer on up to 3 anonymized patients. The 3D learning consisted of an 8 minute video tutorial for Scopis Building Blocks software followed by a 15 minute session reviewing sinus CT imaging on up to 3 anonymized patients using the SBB software.(3) The same set of imaging studies was used for all participants in both groups. Following their respective learned modality, each trainee then completed a post-education self-assessment survey. Participants who performed traditional 2D learning first then completed the 3D learning task, and participants who completed the 3D learning task first, then performed traditional 2D learning. After completion of both learning modalities, trainees completed a comparison survey assessing the two techniques (Figure 4). Subjects also rated the 3D software at the conclusion of their participation (Figure 5).
Figure 4.
Each subject was asked to rate traditional 2D learning and 3D learning.
Figure 5.
Each subject also rated the 3D software though this questionnaire.
Approval to conduct this study was obtained from institutional review boards in accordance with local policies.
Results
A total of 45 otorhinolaryngology trainees and 20 medical school students were enrolled in this study from five separate institutions. All trainees successfully completed all educational and learning tasks. With the exception of one resident, all completed each questionnaire in its entirety.
When compared to traditional 2D learning, 3D learning was perceived by the trainees to be a more effective learning technique in understanding the spatial orientation of the frontal sinus and frontal sinus outflow tract. When asked which learning modality helped most in understanding the spatial orientation of the frontal sinus pathway, 89.23% (58/65) of respondents choose the 3D learning as their preferred technique.
When asked which learning modality helped most in understanding the spatial orientation of the frontal sinus, 56 learners (86%) chose 3D learning, 3 learners (5%) chose traditional 2D learning, and the remaining 6 learners (9%) reported no difference between the two modalities.
Thirty-nine study participants were asked to complete a post study questionnaire independently assessing SBB software. All participants with the exception of two either agreed (N = 20) or strongly agreed (N=17) that they would recommend this software as an educational tool to others. Seventeen (89.74%) trainees either strongly agreed (N=15) or agreed (N=20) that they would go on to utilize the software in their clinical practice if the 3D software were available.
A two-sample Wilcoxon rank-sum test was performed to assess the subjects’ perceived increase in knowledge and understanding of frontal recess and frontal sinus anatomy following their first learned modality (either 2D of 3D learning techniques). When asked to rate their ability to identify the natural drainage pathway of the frontal sinus the change noted between the pre and post questionnaire self-assessments were found to be statistically different for both the 2D and 3D learning techniques, with more improvement noted with the 3D learning modality (P = 0.0266). When assessing the subjects understanding of the spatial orientation of the frontal sinus the delta change between pre and post learning modalities did not reach statistical significance difference between the two groups, however the trend of improved understanding was in favor of the 3D learning technique.
Discussion
Endoscopic frontal sinus surgery in particular is associated with a wide range of complex anatomic variations, thus making a comprehensive understanding of the various cell types and their relationships to the natural frontal sinus drainage pathway a prerequisite for safe, efficient and effective endoscopic frontal sinus surgery. The introduction and popularization of image guidance systems have also played a significant role in the evolution of endoscopic surgery, by acting as useful adjuncts in intra-operative site localization and helping to improve surgical confidence.(4) The use of such technology, however, does not supersede nor replace having a thorough understanding of paranasal sinus and skull base anatomy. Failure to have a detailed understanding for frontal recess anatomy and perform appropriate preoperative surgical planning can potentially lead to devastating complications such as iatrogenic CSF leaks, neurovascular injury, and incomplete removal of frontal recess cells leading to stenosis and scarring of the frontal sinus outflow tract.(5, 11, 12)
The primary objective of this study was to assess a novel three dimensional training modality in improving otolaryngology trainees understanding and spatial orientation of frontal recess anatomy. This study demonstrates that otorhinolaryngology trainees consider reconstructed 3D modeling of CT sinus imaging to be more effective in understanding the configuration of the frontal recess and frontal sinus outflow tract anatomy than traditional two dimensional triplanar viewing. All trainees, with the exception of one, perceived 3D planning to be more effective in improving their understanding and spatial orientation of the frontal sinus drainage pathway. Ninety percent reported that 3D SBB was more effective in understanding the spatial orientation of the formal sinus (18/20).
Due to its complicated anatomical configuration, addressing the frontal sinus surgically can often times be disorienting and frustrating, even for the experienced endoscopic sinus surgeon. P.J. Wormald first introduced the concept of transforming cells of the frontal recess into three dimensional blocks to help simplify the complex surgical dissection of the frontal sinus; in this approach, the surgeon develops a pre-operative step-by-step surgical plan to address the various cell types of the frontal recess thereby defining the natural drainage pathway.(10) The SBB software represents the implementation of Wormald’s “building blocks” concept for both surgical planning and education. SBB software allows the user to construct three-dimensional building blocks in the context of a traditional triplanar format (Figure 2). Specifically, the software allows the user to draw rectangular boxes over frontal recess cells; from these “drawn” 2D boxes, the software builds a 3D box. Each cell can be separately highlighted and the reconstructed 3D boxes can then be displayed all at once or selectively. Similarly, the user can outline the frontal sinus drainage pathway on the orthogonal CT images, and then the software will display its relationship to the 3D boxes that represent the underlying anatomy. One can then freely rotate and view the constructed 3D building blocks in multiple planes and accurately outline the natural drainage pathway of the frontal sinus from different observation perspectives. This added dynamic dimension allows the user to visualize the anatomy in a more understandable 3D anatomical perspective. The introduction of this novel technique into residency training has the potential to augment trainee proficiency and comprehension of frontal sinus anatomy. This theoretically could aid in enhancement of surgical skill leading to improved patient outcomes and reduced operative time.
Incorporating novel techniques such as virtual reality simulators and cadaver dissection have become a vital part in many otolaryngology training programs and have been shown to augment learning in multiple applications such as lower airway evaluation, temporal bone dissection, and endoscopic sinus surgery.(6, 7, 8) The use of 3D educational tools has also gained significant traction in the academic arena; recent literature demonstrates the potential to improve surgical training.(7, 9) Furthermore, SBB is the planning software for Scopis Navigation; thus, this navigation system can further bridge the gap between reviewing CT scans and actual surgery, by displaying trainees’ annotation on the CT scans during navigation in actual surgical cases. SBB should be viewed in this context when assessing its potential to impact training for sinus surgery.
Others have also assessed the utility of reconstructed 3D CT for clinical practice and surgical planning. Isaacs et al conducted a study that included two otolaryngologists who reviewed 25 CT imaging studies of patients referred for paranasal sinus diseases. The examiners then rated the usefulness of each study (both 2D & reconstructed & 3D CT imaging) to identify various anatomic subsites of the frontal recess using a modified 5-point Likert scale. The authors reported 3D CT to be more effective at defining intersinus septal cells, supraorbital ethmoid cells, and the anterior-posterior dimension of the frontal sinus outflow tract when compared conventional triplanar CT.(9) Based on the current literature, there appears to be a potential benefit of incorporating virtual three dimensional viewing software for both surgical training as well as daily clinical assessment of the frontal recess and frontal sinus. The extent of benefit and necessity of this modality, however, requires further investigation..
Limitations of this study include development and use of non-validated questionnaires. The survey questions were constructed to minimize bias in assessing the SBB and comparing it to traditional learning methods. Utilizing a level I assessment on Kirkpatrick’s framework for evaluating a new educational tool, the current study represents an evaluation of trainees ‘reactions’ and ‘experiences’ using a novel 3D training modality.(13) Admittedly, the absence a formal test of subject’s ability to identify structures and then apply that knowledge in the operating room prevents definitive conclusions about this impact of 3D learning on trainee performance. At a practical level, it was problematic to develop a standardized testing model for the assessment of trainee knowledge, due to insufficient resources for the creation of rigorous testing. Obviously, subsequent studies will be required to actually measure an objective increase in knowledge, the degree to which this technique can be applied to the operating room setting, and finally the effect on patient care and surgical outcomes.
It is important to mention that the 3D planning software should be used in conjunction with, traditional 2D learning methods. Incorporating this novel modality will likely serve to augment current curriculum and didactic training in learning the frontal recess and frontal sinus anatomy.
A key advantage of the 3D learning with SBB is that the software is available as a download from the company that produces it. The current price of the version used in this study is $300. Of note, the hardware requirements for running the software do not include a dedicated workstation; in fact, most business-class personal computers are adequately powered to run the software easily. The advent of cloud computing also may facilitate the development of anonymized patient data sets, with and without annotation and commentary in a low-cost library that learners across the globe can share and grow.
Conclusion
The ability to reconstruct CT imaging into a three dimensional dynamic perspective appears to have benefit for the trainee in understanding the complex anatomy and spatial orientation of the frontal recess and frontal sinus drainage pathway. The potential increase in trainee proficiency and comprehension theoretically may improve surgical skills and patient outcomes and reduce surgical time. Future randomized controlled studies are required to confirm these hypotheses.
Acknowledgments
MJC serves as a consultant for JNJ/Acclarent (Irvine, CA), Medical Metrics (Houston, TX) and Medtronic ENT (Jacksonville, FL).
AL serves as a consultant for ENTvantage (Austin, TX), Medtronic ENT (Jacksonville, FL), 480 Biomedical (Boston, MA), Aerin Medical (Sunnyvale, CA) and Laurimed LLC (Redwood City, CA).
Scopis GmbH (Berlin, Germany) provided access to the Scopis Building Blocks software in-kind. Scopis GmbH was not involved in any aspect of the study design, data collection, data analysis or manuscript preparation.
The Department of Otorhinolaryngology at the University of Texas McGovern Medical School at Houston receives industry research funding from Intersect ENT (Menlo Park, CA), Allakos (San Carlos, CA) and Amgen (Thousand Oaks, CA).
Financial Support: AL is supported by the Center for Clinical and Translational Sciences, which is funded by National Institutes of Health Clinical and Translational Award UL1 TR000371 and KL2 TR000370 from the National Center for Advancing Translational Science. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Advancing Translational Science or the National Institutes of Health.
Footnotes
Conflict of Interest:
AA, KS and CC have no financial conflict of interests to declare.
References
- 1.Agbetoba AA, Amber UL, Citardi MJ. Radiographic Review of Frontal Recess Anatomy. 2015 Jan; Available at https://vimeo.com/153712415. [Google Scholar]
- 2.Lee WT, Kuhn FA, Citardi MJ. 3D Computed Tomographic Analysis of Frontal Recess Anatomy in Patients Without Frontal Sinusitis. Otolaryngology -- Head and Neck Surgery. 2004 Sep;131:164–173. doi: 10.1016/j.otohns.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 3.Wormald PJ. Tutorial 1: How to utilize Scopis Building Blocks to prepare for surgery. [Published on Sep 25, 2014]; Available at http://planning.scopis.com/ [Google Scholar]
- 4.Ramakrishnan VR, Orlandi RR, Citardi MJ, et al. The use of image-guided surgery in endoscopic sinus surgery: an evidence-based review with recommendations. Int Forum Allergy Rhinol. 2013;3:236–241. doi: 10.1002/alr.21094. [DOI] [PubMed] [Google Scholar]
- 5.Javer AR, Alandejani T. Prevention and management of complications in frontal sinus surgery. Otolaryngol Clin North Am. 2010 Aug;43(4):827–838. doi: 10.1016/j.otc.2010.04.021. [DOI] [PubMed] [Google Scholar]
- 6.Abou-Elhamd KE, Al-Sultan AI, Rashad UM. Simulation in ENT medical education. J Laryngol Otol. 2010 Mar;124(3):237–241. doi: 10.1017/S0022215109991885. [DOI] [PubMed] [Google Scholar]
- 7.Yao WC, Regone RM, Huyhn N, Butler EB, Takashima M. Three-dimensional sinus imaging as an adjunct to two-dimensional imaging to accelerate education and improve spatial orientation. Laryngoscope. 2014;124:596–601. doi: 10.1002/lary.24316. [DOI] [PubMed] [Google Scholar]
- 8.Arora A, Lau LY, Awad Z, Darzi A, Singh A, Tolley N. Virtual reality simulation training in Otolaryngology. Int J Surg. 2014;12(2):87–94. doi: 10.1016/j.ijsu.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 9.Isaacs SJ, Goyal P. Comparison between three-dimensional and triplanar computed tomography imaging of the frontal recess. Am J Rhinol Allergy. 2009 Sep-Oct;23(5):502–505. doi: 10.2500/ajra.2009.23.3350. [DOI] [PubMed] [Google Scholar]
- 10.Wormald PJ. Surgery of the frontal recess and frontal sinus. Rhinology. 2005 Jun;43(2):82–85. [PubMed] [Google Scholar]
- 11.Kennedy DW, Senior BA. Endoscopic Sinus Surgery - A Review. Otolaryngol Clin Nor Am. 1997;30:313–330. [PubMed] [Google Scholar]
- 12.Ramadan HH. Surgical causes of failure in endoscopic sinus surgery. Laryngoscope. 1999;109:27–29. doi: 10.1097/00005537-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Schumann PL, Anderson PH, Scott TW, Lawton L. A Framework For Evaluating Simulations As Educational Tool. Developments in Business Simulation and Experiential Learning. 2001;28:215–220. [Google Scholar]