Abstract
Purpose
To demonstrate that the steep peripheral ring (red zone) on corneal topography after myopic laser in situ keratomileusis (LASIK) could possibly due to instrument error and not always to a real increase in corneal curvature.
Methods
A spherical model for the corneal surface and modifying topography software was used to analyze the cause of an error due to instrument design. This study involved modification of the software of a commercially available topographer.
Results
A small modification of the topography image results in a red zone on the corneal topography color map.
Conclusion
Corneal modeling indicates that the red zone could be an artifact due to an instrument-induced error. The steep curvature changes after LASIK, signified by the red zone, could be also an error due to the plotting algorithms of the corneal topographer, besides a steep curvature change.
Keywords: Irregular corneal astigmatism, Red zone, Topography, Spherical aberration
Introduction
Historically, the Placido disk was a device for the study of corneal curvature. Subsequently the corneascope was introduced that retained the image and quantified the corneal curvature albeit imperfectly.1 Computerized surveyors were the first instruments that allowed greater reliability for the measurement of corneal curvature and are still widely used today. Over time, various topographic indices have been developed to facilitate the clinical applications of corneal topography.2, 3
The corneal topographer exploits the principle that the anterior corneal surface is a convex mirror that reflects the image of a disk with alternate black-and-white circular bands. The reflected image is collected and stored in a computer in a number of common image formats. This image is then analyzed by software. First of all, the software measures the distance between the center of the image and each ring. This measurement is performed along the corneal meridians at angular intervals set by the manufacturer. The angle of each meridian and distance to the center of each ring in this meridian are the polar coordinates defining a point explored by the surveyor. The apparatus is designed in order to find the curvature at each point and not sagittal height, which would be more appropriate.4
Once all the measurements are completed, a table is stored on the hard disk in a text file. The next step, based on resulting measurements, is to apply the algorithm designed by the manufacturer to calculate the radius of curvature in each of the measured points. At the end of the process the data are known for each ring and each angular coordinate. Additionally the data are available for the distance from the center of the image (image center is plotted on the visual axis because it is assumed that the topography is centered and properly focused) and the corneal radius of curvature as the corneal meridian passing through that point. This set of corneal radii is plotted on the computer screen as a color map.
Eyes that have undergone myopic laser in situ keratomileusis (LASIK) often have a characteristic steep peripheral ring. This steep peripheral ring is commonly called a “red ring” or “red zone” that is present on postoperative instantaneous or tangential topography maps plotted with an adjustable or normalized scale using the Smolek–Klyce colors or international standard organization colors. The red ring occurs within the corneal region that has undergone surgery. The red ring was used by Vinciguerra to determine the cause of decentration and pseudodecentration after laser ablation.5 Dupps and Roberts used corneal biomechanics to explain the postoperative red zone. Their biomechanical model is a series of meridional arches or lamellae arranged from limbus to limbus.6 The destruction of these lamellae by excimer ablation elicits a shrinkage and corneal thickening around the ablated area.6 Roberts provided additional evidence for this theory by measuring the peripheral corneal thickness with the Orbscan II (Bausch and Lomb Inc., Rochester, NY, USA) in the corneal region with the red zone.7
The use of diverse physical instruments is crucial in Opthalmology. These instruments should be properly calibrated, so that their responses are in agreement with the corresponding theories. But only practitioners are able to criticize and correct the results given by these instruments, which may be ambiguous or uncertain even when they are well and carefully calibrated.
In this study we evaluate whether the creation of this red zone may be an artifact of corneal topographers, as a result of the method used to reflect the Placido disk rings at the edge of the surgical site. The potential clinical implication of this investigation is that the red zone on postoperative corneal topography could also be an artifact of corneal topography plotting algorithms.
Methods
The EyeSys Windows WorkStation V.2 software topographer (EyeSys Systems Technologies, Houston, TX, USA) was used in this study. This topographer has four calibration balls with radii of 6.13, 7.10, 7.94 and 9.00 mm. We randomly chose the 7.10 mm radius ball, and placed it in front of the topographer similar to the device calibration method. However we performed a topography of the calibration ball, as if it were an eye. Once the videokeratograph was captured, we used an option in the topographer software to edit and modify two adjacent rings in the image.
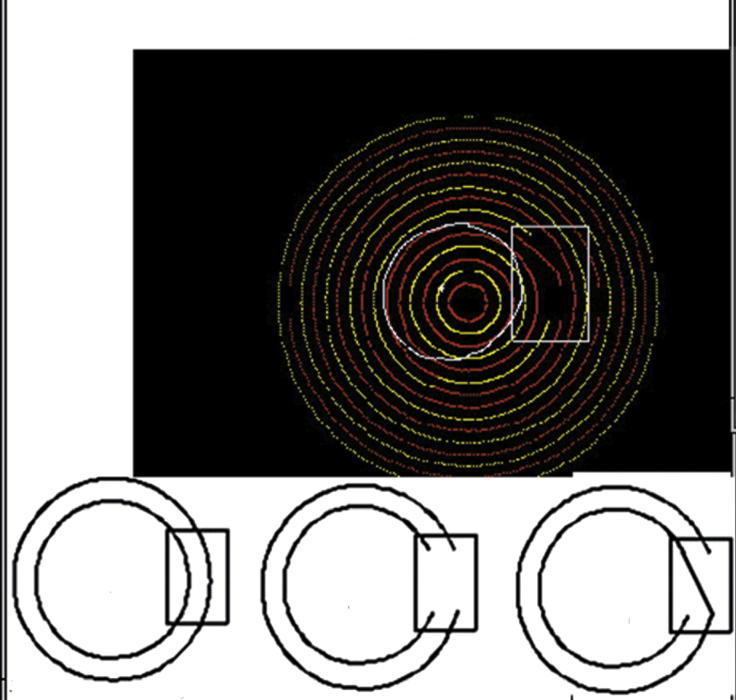
Fig. 1 presents the reflection image of the placido rings on the ball, and an schematic draws indicate the region and process for the modification.
Figure 1.
Up: image captures by EyeSys topographer for a spherical surface of 7.1 mm radius after software modification. It presents the reflection image of the placido rings on the ball. Once the videokeratograph was captured, we used an option in the topographer software to edit and modify two adjacent rings in the image. Down: explanation of the manipulation process of the computer algorithm in the EyeSys topographer. The schematic box shows the modified image due to software manipulation simulating ring tracing errors. A section of each of the two rings was deleted and a line was drawn connecting a free end of one of the rings with the other opposite free adjacent ring.
The details of the modification are explained in Fig. 1 down. A section of each of the two rings was deleted and a line was drawn connecting a free end of one of the rings with the other opposite free adjacent ring. The resulting topography is presented in Fig. 2 with the red zone.
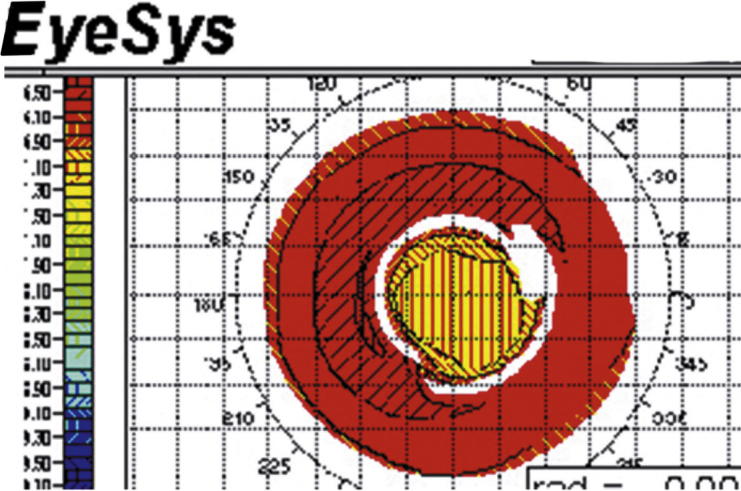
Figure 2.
Topography color map in the spherical surface of 7.1 mm radius after software modification, captured by the EyeSys topographer. It shows the red zone as a steep peripheral ring.
Results
A corneal topography was performed on a perfectly spherical model simulating an artificial cornea and the image was modified through software to simulate a discontinuity in the corneal curvature. The software then processed the modified image to plot the topography map.
By processing the modified image, the result was an abnormal topography map in which the central corneal map appears normal, but the region that was modified shows a red zone indicating an apparently smaller radius (Fig. 2).
Discussion
Corneal topography based on Placido disk imaging is inaccurate, particularly for irregular corneas which show considerable variability in measurements.8 Hence, topographies in irregular corneas should be interpreted with caution.9 The data from the topographers plot the distance to the center of each ring to the anterio-posterior axis that passes through the center of the cornea but the numbers are only real in flat or 2D representation of the cornea because the curvature of the cornea results in oblique imaging of the peripheral rings and they seem closer together the further they are from the central cornea. Many topographers change the spacing between the rings to account for the increased slope of the cornea in the periphery.
The radius of curvature for each point that the software reads is attached to an error even for a normal cornea. Therefore, the accuracy of the measurements in corneal topography decreases as the distance from the center of the cornea increases.3 This difference in accuracy between central and peripheral measures depends, among other factors, in the difference between corneal radii of both areas, so that, if a corneal topography is performed on a test sphere, we find the correct radius of curvature at any distance from the center.
A major cause of topographic distortion is the lack of correspondence between data on the corneal angles and data on the topographic image. Kronemyer reported that a point of reflection on the cornea and the corresponding point on the topography image require the same angular coordinate to ensure reliable data.10 According to Kronemyer, this is only possible if a reflected point always passes perpendicularly through the optical axis, or stated differently, a point on a placido ring, the reflected point from the cornea and the image point are on a plane containing the optical axis.10 However, in cases with astigmatism, correct alignment with the optical axis is only possible in the meridians with maximum and minimum curvature.
Based on Kronemyer’s conclusions this would be even more important for an irregular cornea.10 Merlin states that “the radius is reliable … when curvature variations are variations of radius always centered on the keratoscope axis”.11
Additionally, it is imperative that the points on a meridian on the image have the same order as the Placido rings. For example, at each angular coordinate of the image and from the center to the periphery, the first image point should be produced by the reflection of a point-object of the first ring, and the second ring would correspond to the second and so on. An abrupt change on the corneal surface (e.g. a scar) can crosslink two adjacent rings or produce an erroneous reflection akin to an image reflecting from the corrugated surface of a pond.
Using a biomechanical model, Dupps and Roberts,6 present a possible explanation for the occurrence of the red zone after LASIK in myopic eyes. They propose that postoperatively, the corneal lamellae would shrink increasing corneal thickness at the edge of the nascent corneal region resulting in a significant increase in corneal curvature. This increase in corneal curvature would be plotted as a red zone on the corneal topography maps.
Roberts confirms this theory by measuring the thickness of the ring with an Orbscan II corneal topographer.7 Roberts makes the interesting observation that photoablation is not necessary to create a red ring as it occurs by creation of the corneal flap with a microkeratome.7
The Orbscan II uses a Placido disk to map the front corneal surface. The back surface is scanned by only two projectors, located at 45° left and right of a video camera.12, 13, 14 Each of these projectors focuses a narrow vertical strip of light onto the cornea. Both bands of lights move horizontally, sweeping across the cornea while a video camera records each successive shots. The typesetting of all images produced a moiré effect, which is analyzed with internal software.
Therefore, the Orbscan II algorithms contain the same sources of error for plotting the anterior corneal surface as than any other Placido based topographer. Hence, corneal pachymetry may not be reliable in irregular corneas with this instrument.
Our study shows that a local change in the reflection of the rings causes a red zone from altered point with a Placido-based topographer. It would be interesting to determine whether this phenomenon occurs when the disturbance is provoked directly in the ball test. The intentional introduction of a Placido ring tracing error can produce an apparent steep peripheral corneal feature on a color curvature map using a spherical test object.
Although corneal topographers have continuously evolved and their accuracy has vastly improved since the 1990 s, they will give incorrect answers if they incorrectly label the ring reflections. This is indeed what the authors, of this work, have demonstrated by editing the ring image. Practitioners should take care when interpreting topography maps to ensure that the rings have been correctly processed.
We believe our study using a single experiment with no quantitative analysis or replication of the effect is enough strong because the modification of a computer algorithm will always have the same result. Based on this observation, we concluded that this problem is due to software error and repeated tests of the same error are not required.
This comment is also addressed by Velarde’s thesis.15 Velarde developed an experimental model with PMMA and silicone hydrogel contact lenses on a fluorosilicone acrylate ball and performed an excimer ablation on the contact lenses. Subsequently the topography of the contact lenses was measured with the Orbscan II (Baush & Lomb) and the Oculus Easygraph corneal topographers (Oculus).15 Velarde observed that all models had steepened corneal curvature at the periphery of the abation on tangential topographic maps in all cases. If topographers are reliable, then Velarde’s15 observations indicate that removing material centrally resulted in an addition of material around the treated area, which is obviously impossible. Hence, another explanation for the topographic red zone is warranted.
In Velarde’s models, similar to post-LASIK corneas, there is a circular area surrounding the surgical corneal region similar to a scar.15 We believe it is physically impossible that the rings reflected in the topography are perfectly concentric to the scar without interference from the scar. It is likely that some rings will be reflected partially within and partially outside the scar. These rays will scatter unpredictably due to interference from the scar and in some cases creating an irregularity similar to that induced by our software manipulation. This phenomenon will create the red zone.
The red ring can occur for any corneal irregularity, such as the edge of a keratoplasty, an ulcer or the edge of a flap incision. The red ring does not appear if the cornea adjacent to the scar is opaque because a reflection of the Placido mires is not produced in that region. In this case the topography map would show a lack of information that does not affect the corneal periphery.
Conclusion
The fact that the red zone appears during experimental modeling with an excimer and that it can be induced in a normal topography with software, seems sufficient to assert that the red zone after myopic LASIK could be an unreliable instrument artifact.
The red ring on post-myopic-LASIK topographies is well documented. Therefore we demonstrate that such a tracing error could be also an instrument false reading. Practitioners should take care when interpreting topography maps to ensure that the rings have been correctly processed. Also practitioners are able to criticize and correct the results given by these instruments, which may be ambiguous or uncertain even when they are well and carefully calibrated.
Financial support
The authors received no financial support for this study and have no financial or proprietary interest in the materials present in this study.
Conflict of interest
None of the authors have a commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangements) that might be perceived as a conflict of interest in connection with the submitted manuscript.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
Contributor Information
Alicia Galindo-Ferreiro, Email: ali_galindo@yahoo.es.
Alberto Galvez-Ruiz, Email: algarui@yahoo.com.
Silvana A. Schellini, Email: sschellini@gmail.com.
Julio Galindo-Alonso, Email: julgalin@gmail.com.
References
- 1.Rowsey J.J., Reynolds A.E., Brown R. Corneal topography: Corneascope. Arch Ophthalmol. 1981;99:1093–1100. doi: 10.1001/archopht.1981.03930011093022. [DOI] [PubMed] [Google Scholar]
- 2.Maloney R.K., Bogan S.J., Waring G.O., 3rd. Determination of corneal image-forming properties from corneal topography. Am J Ophthalmol. 1993;115:31–41. doi: 10.1016/s0002-9394(14)73521-4. [DOI] [PubMed] [Google Scholar]
- 3.Cohen K.L., Tripoli N.K., Pellom A.C., Kupper L.L., Fryczkowski A.W. A new photogrammetric method for quantifying corneal topography. Investigat Ophthalmol Visual Sci. 1984;25:323–330. [PubMed] [Google Scholar]
- 4.Carroll J.P. A method to describe corneal topography. Optom Vis Sci: off Publ Am Acad Optom. 1994;71:259–264. doi: 10.1097/00006324-199404000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Vinciguerra P., Randazzo A., Albe E., Epstein D. Tangential topography corneal map to diagnose laser treatment decentration. J Refract Surg. 2007;23(Suppl. 9):S1057–S1064. doi: 10.3928/1081-597X-20071102-15. [DOI] [PubMed] [Google Scholar]
- 6.Dupps W.J., Jr, Roberts C. Effect of acute biomechanical changes on corneal curvature after photokeratectomy. J Refract Surg. 2001;17:658–669. doi: 10.3928/1081-597X-20011101-05. [DOI] [PubMed] [Google Scholar]
- 7.Roberts C. The cornea is not a piece of plastic. J Refract Surg. 2000;16:407–413. doi: 10.3928/1081-597X-20000701-03. [DOI] [PubMed] [Google Scholar]
- 8.Kounis G.A., Tsilimbaris M.K., Kymionis G.D., Ginis H.S., Pallikaris I.G. Estimating variability in placido-based topographic systems. Optom Vision Sci: Off Publ Am Acad Optom. 2007;84:962–968. doi: 10.1097/OPX.0b013e318157a68c. [DOI] [PubMed] [Google Scholar]
- 9.Rabinowitz Y.S. Corneal topography. Curr Opin Ophthalmol. 1995;6:57–62. doi: 10.1097/00055735-199508000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Kronemyer B. New filter improves topography system. Ocular Surg News. 1995:7–15. [Google Scholar]
- 11.Merlin U., Cantera E. Corneal topography. In: Burrato L., editor. The Clinical Atlas thoroughfare. Slack; New Jersey: 1996. pp. 9–93. [Google Scholar]
- 12.Kawara T. Corneal topography using moire contour fringes. Appl Opt. 1979;18:3675–3678. doi: 10.1364/AO.18.003675. [DOI] [PubMed] [Google Scholar]
- 13.Corbett M., O’Bratt D., Stultiens B., Jongsma F., Marshall J. Corneal topography using a new moiré image-based system. Eur J Implant Ref Surg. 1995;7:354–371. [Google Scholar]
- 14.Patel S., Marshall J., Fitzke F.W. Shape and radius of posterior corneal surface. Refract Corneal Surg. 1993;9:173–181. [PubMed] [Google Scholar]
- 15.Velarde J. Sobre el encurvamiento periférico en la topografía corneal tras cirugía refractiva (LASIK) para corrección de miopía y la relación con parámetros oculares biomecánicos y quirúrgicos: Available at: <http://bucserver01.unican.es/xmlui/bitstream/handle/10902/4852/Tesis%20JIVR.pdf>. [Accessed May 10, 2013].