Abstract
Caveolin-1 (Cav-1) is a trans-membrane protein that is a major component of the caveolae structure on the plasma membrane. Cav-1 is involved in the regulation of various cellular processes, including cell growth, differentiation, endocytosis, and in particular it has been implied in cellular senescence. Here we review current knowledge about Cav-1 in cellular signaling and discuss the role of Cav-1 in aging-related diseases.
Keywords: Caveolin 1, Caveolae, Cell Aging, Endocytosis
INTRODUCTION
Caveolae are structures with a diameter of 50-100 nm that have been identified by electron microscopy as flask-shaped invaginations in the membrane lipid rafts of various cell types and tissues, being especially abundant in endothelial cells and adipocytes.1,2,3 Although caveolae were discovered over 60 years ago, research on these structures has made slow progress until the discovery of caveolins, the structural proteins of caveolae.4,5,6 The identification of caveolins in caveolae structures has provided important insights into the differences between caveolae and lipid rafts.7,8,9 The caveolin family consists of 3 distinct proteins including caveolin-1 (Cav-1), caveolin-2 (Cav-2), and caveolin-3 (Cav-3).5,10,11 Of these, Cav-1 and Cav-2 are highly co-expressed in non-muscle cells, whereas Cav-3 is mainly found in skeletal and cardiac muscle cells.10,12,13 Among the caveolins, the structure and function of Cav-1 has been the most studied.14,15 Cav-1 is well established as the major structural protein of caveolae, because these structures disappear from the lipid rafts of Cav-1-depleted cells.16,17 Moreover, caveolae are composed of various molecules such as cholesterol, sphingolipids, cavins, and other trans-membrane proteins.10,11,18
Various signaling molecules and different types of membrane receptors are enriched in caveolae and regulate their specific functions by binding with caveolins.19,20,21,22 Therefore, caveolae and structural caveolins, particularly Cav-1, have been implicated in various cellular events such as endocytosis, cellular signaling, membrane transport, and immunity, as well as in related diseases.5,18,23,24,25 However, much remains to be discovered about caveolae structure, formation, regulation, and function in different cell types and in pathology.5,24,26 This review discusses caveolae and Cav-1 along with their functions, particularly in aging and aging-related diseases.
CAV-1/CAVEOLAE FUNCTIONS
1. Structure of Cav-1 and its function in caveolae formation
Cav-1 was the first protein identified in the caveolin family and is the most highly investigated among them.13,14,15 Experimental results have indicated that Cav-1 is a trans-membrane protein, but it is different from other trans-membrane proteins in that both terminals are located in the cytoplasm.2,27 Normally, Cav-1 predominantly localizes on the plasma membrane as an oligomer, but it is also found in the Golgi apparatus in its monomer form.7,28,29 The Cav-1 protein has two isoforms, Cav-1α and Cav-1β, which have different sizes due to differences in the translation initiation site of Cav-1 mRNA that results in Cav-1β lacking 32 amino acids at its N terminal. Therefore, Cav-1β, like Cav-1α, has one phosphorylation site at serine 80, which has been suggested as playing an important function in the regulation of the cholesterol tracking and secretory pathways. On the other hand, Cav-1α has an additional phosphorylation site at tyrosine 14, which has been proposed as having a vital role in the response to growth factors and other stimuli.18,23,30,31 In addition to these phosphorylation sites, the Cav-1 protein has three palmitoylation sites at cysteine 133, 143, and 156 that are required for oligomerization and cholesterol transport.7,32 The oligomerization domain is believed to be a central functional region of the Cav-1 protein because it is required for caveolae formation. Cav-1 is also known as a scaffolding protein that concentrates and functionally regulates various cellular signaling. Through the scaffolding domain, Cav-1 mainly interacts with different signaling molecules and regulates signaling cascade.18,33,34 Furthermore, Cav-1 binds to cholesterol with high affinity, a crucial property for the stabilization of Cav-1 in caveolae.4,35 Taken together, based on the characteristics and properties of Cav-1, it is believed that this protein is not only a structural protein but is also involved in broad cellular physiological processes such as vesicular transport and regulation of signal transduction and differentiation as well as associated diseases.
2. Cav-1 in cellular signaling
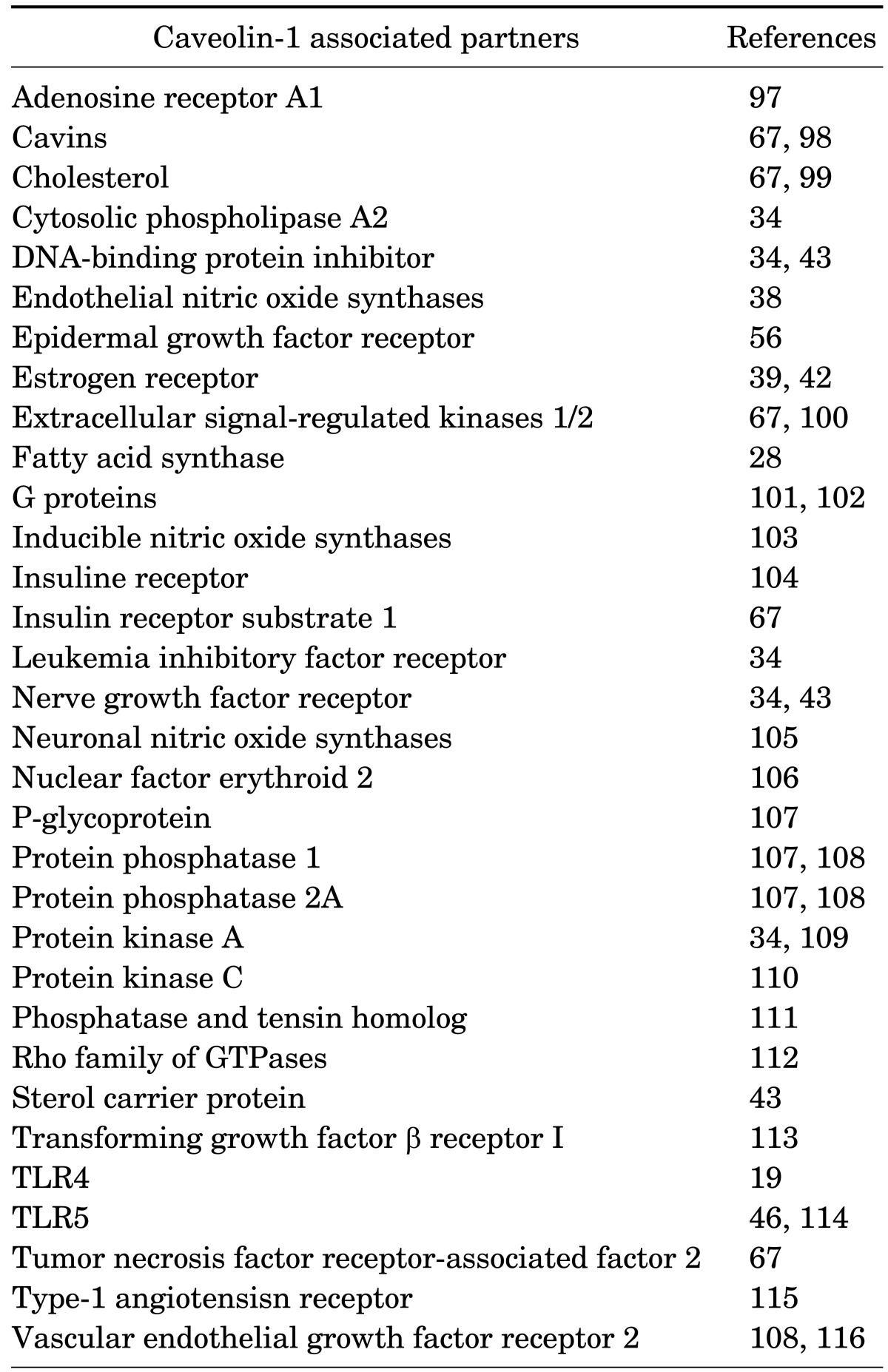
Cav-1 has been implicated as a specific regulator, which plays a role in signal transduction.13,36 Using methods that isolate caveolae structures, many proteins and lipids associated with caveolae have been detected.4,11,20,37 As a consequence, many of these molecules are believed to be associated with the regulation of signal transduction by Cav-1 (Table 1). eNOS, a nitric oxide synthase targeted to the caveolae, is the best characterized Cav-1 binding partner, and the presence of Cav-1 inhibited eNOS signaling in both in vitro and in vivo experiments.11,38 Moreover, Cav-1 has been proposed to attenuate the activity of other signal transduction proteins such as the epidermal growth factor (EGF) receptor (EGFR).4,39,40,41 In contrast, Cav-1 positively regulates several proteins such as the insulin and estrogen receptors.14,20,39,42 In most cases, signal proteins interact with the Cav-1 scaffolding domain via special binding motifs to activate signaling pathways.4,11,34 However, in some cases, companion proteins that lack binding motifs still interact with Cav-1, such as a nerve growth factor receptor, a sterol carrier protein or a DNA-binding protein inhibitor.34,43 Furthermore, Cav-1 is also involved in the regulation of cell fates such as cell proliferation, survival, and differentiation, leading to the development of associated diseases. For instance, down-regulation of Cav-1 leads to decreased E-cadherin expression but increased β-catenin transcription, subsequently enhancing the invasion of cancer cells.44 Along with this finding, the association of Cav-1 and metalloproteases also supports cancer invasion and metastasis.45 Moreover, Cav-1 also associates with different innate immune receptors such as Toll like receptors (TLRs), a class of proteins that play a key role in the innate immune systems.19,46 Hence, Cav-1, the major protein of caveolae, is important in the regulation of cellular signaling.
TABLE 1. Summary of caveolin-1 binding partners.
3. Cav-1 gene regulation mechanisms
Cav-1 has various functions in the regulation of cells and tissues, and the mechanisms of Cav-1 gene regulation have been investigated. Initial data shows that both the levels of Cav-1 mRNA and protein are up-regulated during adipogenesis, and glucose transporter 4 (GLUT4) may play a role in this process, but the detailed mechanism is still unknown.47 Subsequently, Yamamoto investigated the function of the adenylyl cyclase pathway on Cav-1 gene expression and observed that Cav-1 mRNA levels decreased by activating this pathway.48 In addition to this finding, other data suggests that Myc, a transcription factor, and prolactin are involved in the negative regulation of Cav-1 mRNA.49,50 Details about the underlying mechanisms have recently emerged, providing evidence that certain element and transcription factors are involved in Cav-1 gene regulation. For instance, sterol regulatory element-binding protein 1 inhibits Cav-1 gene transcription, resulting in the control of intracellular, free cholesterol transport.51 In addition to this finding, the transcription factor GATA-6, a GATA-binding factor 6, was shown to bind to the Cav-1 promoter and suppress gene expression.52 On the other hand, FOXO, the O subclass of the forkhead family of transcription factors, has been identified as a binding partner of the Cav-1 promoter and promotes Cav-1 gene expression.53 Moreover, epigenetic marks that control gene expression without modifying the DNA sequence have also been investigated as important factors that regulate Cav-1 expression.10 Epigenetic processes induce DNA promoter hypermethylation by adding methyl groups to cytosine residues by DNA methyltransferase on CpG dinucleotides that have a high density at promoter regions of the genome, named CpG islands, and this CpG island methylation inhibits the activation of transcriptional elements.54 To date, many studies have shown that epigenetics plays a crucial role in the methylation and histone modifications of Cav-1, and the majority of these reports have focused on the effects of epigenetics in various cancer types such as breast, prostate, lung, liver, ovarian, and colon cancer.10,55
CAV-1 IN AGING-RELATED DISEASES
1. Aging
Cav-1 is well known as a gatekeeper of cellular senescence and is widely used to detect the aging phenotype.51,52,53 Senescent human diploid fibroblasts (HDFs) show an increased level of Cav-1, and studies show that it colocalizes with EGFR.56 Cav-1 is also involved in senescence-associated morphological changes by modulation of focal adhesion kinase and actin stress fiber formation.57,58 Moreover, overexpression of Cav-1 induces premature cellular senescence in primary cultures of murine fibroblasts.59 Another experiment with Cav-1 knockout (KO) mice showed that the presence of Cav-1 was important for maintaining good health.60 Cav-1 is also believed to be an important regulator of premature senescence of the lung fibroblasts of cigarette smokers.61 Interestingly, a reduction of the Cav-1 level in senescent HDF cells induced the restoration of the extracellular signal-regulated kinases (Erks) signaling pathway upon EGF stimulation, not only in terms of its phosphorylation but also its translocation into the nucleus and activation of transcriptional factors similar to young HDF cells.58 Reduction of Cav-1 in senescent cells can lead to morphological changes similar to young cells, causing them to become small and spindle-shaped.57 These results clearly point towards a central role of Cav-1 in suppressing mitogenic signaling and regulating morphological changes, leading to the promotion of cellular senescence.
Increased Cav-1 expression affects tissue aging by inducing tissue-specific dysfunctions and age-related diseases. Moreover, in the skin of the elderly, Cav-1 upregulation contributes to skin aging by suppressing collagen synthesis via the transforming growth factor-β pathway in dermal fibroblasts.62 In vascular aging, it is well known that Cav-1 is essential for vascular function and is involved in senescence phenotypes and inflammatory responses.63 Cav-1 has also been associated with various age-related diseases, such as cancer, type II diabetes, atherosclerosis, and infectious diseases, as discussed in the following sections.
2. Cancer
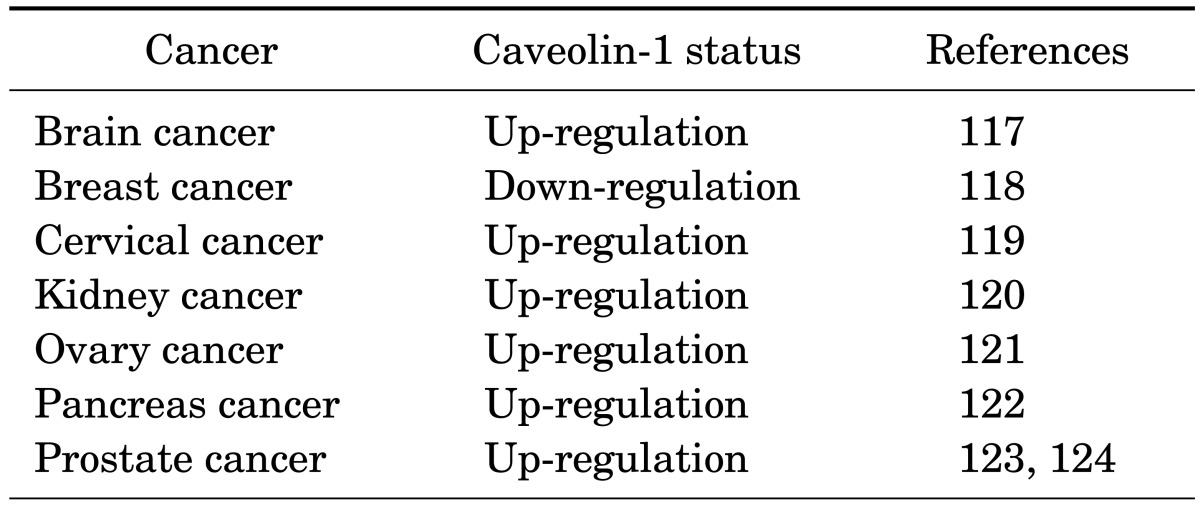
Older tissues are considered to be fertile ground for cancer development since a number of cells in those tissues accumulate mutations leading to an increased cancer rate in the elderly.64 Much evidence has emerged about the functions of Cav-1 in cancer.11 Cav-1 was initially hypothesized to be a tumor suppressor, since Cav-1 maps to a tumor suppressor region of the genome.11,65 Moreover, experimental results showed that Cav-1 was deleted or down-regulated in many oncogene-transformed cells and that oncogene-transformed phenotypes could be reversed by the re-introduction of Cav-1 expression.11 However, Cav-1 does not only function as a tumor suppressor in cancer, since different explanations of Cav-1 expression levels have been proposed, and Cav-1 mutations are diverse depending on the cancer type.66,67 For instance, Cav-1 expression levels are down-regulated in various cancers such as ovarian, lung, and mammary carcinomas, but are up-regulated in other cancers such as bladder, esophagus, and prostate carcinomas.65 Contradictory roles of Cav-1 in various cancers have been shown in animal models and human patients. Specifically, Cav-1 increases in metastatic breast and prostate cancers compared with that in primary tumors68 and promotes cell survival through Akt, a serine/threonine-specific protein kinsase, signaling and by regulating metastatic cancer microenvironments in patients with metastatic prostate cancers. Cav-1 is also secreted during prostate cancer development, indicating its potential as a diagnostic and therapeutic target.69
These results suggest the two faces of Cav-1, since it may be lost, promoting the growth of cancer cells in early stages, but enhances expression in late stages of cancer, provoking tumors to become aggressive and metastasize (Table 2).
TABLE 2. Caveolin-1 status in various cancer.
3. Type II diabetes
The rate of type II diabetes is increased in the elderly, but the underlying mechanisms remain partly unknown.70 Recent evidence shows that Cav-1 may play a role as a mediator in insulin signaling and a defect of Cav-1 is involved in non-obese type II diabetes development. The first clues about the function of Cav-1 in type II diabetes came from experimental results in Cav-1 KO mice that showed these mice to be insulin resistant with attenuated insulin signaling.71,72 Additionally, other studies have determined that the level of Cav-1 in skeletal muscle was associated with age-dependent type II diabetes.73 During aging, Cav-1 directly binds to insulin receptors and mediates the ensuing signaling pathways, leading to increased glucose absorption in the muscle. Cav-1 downregulation in old mice caused severe impairments of glucose and insulin tolerance, whereas Cav-1 upregulation in aged diabetic JYD mice, non-diabetic C57BL/6 , DBA/2 mice, develop insulin resistance and type 2 diabetes when they grow old, significantly improved insulin sensitivity, with a concomitant increase in glucose uptake by the skeletal muscle. In addition, sex hormones are implicated in the regulation of Cav-1 expression, which subsequently affects insulin resistance and type II diabetes in aged, male, diabetic JYD mice.74 Moreover, the mechanistic links between Cav-1 and type II diabetes have become better understood, and Cav-1 expression is associated with the RhoA/Rho kinase, a small GTPases protein of Ras family, pathway that controls diabetes.75 This research suggests various roles of Cav-1 in type II diabetes. In addition, increased Cav-1 expression in the smooth muscle upregulates the RhoA/Rho kinase pathway, leading to an increase in sustained muscle contractions in diabetic mice and patients with hyperglycemia. However, most studies on Cav-1 were limited to muscle tissues, and the roles Cav-1 in type II diabetes need to be further studied in liver, adipose tissues, and other related tissues.
4. Atherosclerosis
Atherosclerosis is a disease that is classified as a universal form of vascular aging in which lipids and cellular debris build up inside blood vessels, and Cav-1 has been shown to have an important function in the development of this disease.76 Cav-1 is abundantly expressed in endothelial cells as the main transporter of cholesterol and low-density lipoprotein (LDL) and is therefore involved in key events leading to atherosclerosis development.77 Some lipoproteins involved in lipid metabolism are also enriched and regulated in caveolae structures,78 and Cav-1 expression was sufficient to induce atherosclerosis in a mouse model.79 Furthermore, Cav-1 KO mice displayed selective loss of endothelial functions, leading to pulmonary and cardiac defects, atherosclerosis, and tissue ischemia. Analysis of lipoproteins in the plasma from Cav-1 KO mice displays a shift in their distribution towards an atherogenic profile characteristic of hypertriglyceridemia (elevated VLDL/chylomicrons), with intolerance in the clearance of oral fat load independent of lipoprotein and hepatic lipase activities.80 Moreover, it has been proposed that Cav-1 has two different functions in accelerating atherosclerosis. In endothelial cells, Cav-1 regulates low-density protein transcytosis in the intima as well as, it also involves in development of atherosclerosis by amplifying inflammation in macrophages, subsequently enhancing plaque formation.28,81 Therefore, this data suggests that caveolae and caveolin-1 must plays an important role in the regulation of endothelial function and in the development of atherosclerosis.
5. Infectious diseases
The elderly population is more susceptible to infection by age-associated changes in physiology and anatomy as well as the weakening of the immune system.82,83 Along with aging, epithelial cells experience changes in their signaling pathways and functions, subsequently affecting the ability of physical barriers such as the skin, bladder, and bronchial and digestive systems to prevent infection.83 Interestingly, caveolae-dependent endocytosis is elevated in senescent host cells, and this pathway may serve as a gateway toward increased infection in the elderly.84 Caveolae-dependent infection is divided into 2 different categories, infection by caveolae-dependent endocytosis and Cav-1-dependent actin rearrangement. The ability of caveolae, with their flask-shaped invagination structures, to exit the plasma membrane as enclosed vesicles first gave rise to the idea of an endocytotic function of these structures in 1975.85 Additionally, it has been established that caveolae have an advantage over other endocytotic pathways, since they ferry most cargo directly to the Golgi apparatus or endoplasmic reticulum without lysosome fusion.84,86,87 Hence, the caveolae-mediated endocytosis pathway protects cargo from degradation by lysosome enzymes and maintains them in the cytoplasm. Therefore, many viruses and bacteria use this as a smart pathway to escape the lysosomal degradation in host cells and cause disease.84,88,89,90 On the other hand, Cav-1 is highly expressed and is important for enhancing Salmonella typhimurium (S. typhimurium) infection in M-like cells and senescent fibroblasts. More importantly, the mechanism of Cav-1-mediated invasion of S. typhimurium has been identified. Unlike other pathogens, Cav-1 is involved in the early phagocytotic processing of S. typhimurium into host cells through binding with SopE, a bacterial effector protein delivered into host cells via the type III secretion system. After injecting into host cells, SopE binds and activates cellular Rac1 protein, leading to cellular responses such as the rearrangement of actin fibers for facilitating infection. The expression of Cav-1 recruits and induces association of Rac1 and SopE in caveolae for invasion of S. typhimurium into host cells.82,84 M cells are found in peyer's patch which is known as a main gate of S. typhimurium infection. Interestingly, during differentiation of M cells from epithelial precursor cells, Cav-1 remarkably increased and finally mediated the transcytosis of S. typhimurium. These results indicate that up-regulated Cav-1 in senescent host cells or M cells may explain the high susceptibility to microbial infections that occurs with age.
6. Immunosenescence
Recent evidence has been used to outline the function of Cav-1 in both adaptive and innate immunity. Cav-1 is believed to have an important function in the activation of lymphocytes since it induces T lymphocyte proliferation and cytokine production91,92 and stimulates B lymphocytes to develop an immune response against thymus-independent antigens.93 Moreover, Cav-1 KO mice show defects in innate immunity, resulting in insignificant decrease in survival by infection or increased production of inflammatory cytokines.94 Along with this finding, several papers have reported an association between Cav-1 and Toll-like receptors (TLRs), receptors that recognize the conserved structures of microbes early in infection. The initial evidence was provided by Lei and Morrison,95 who showed that Cav-1 expression was altered in lipopolysaccharide (LPS)-activated murine macrophages, and they suggested that Cav-1 levels might be correlated with LPS signaling. More interestingly, a new function of Cav-1 in age-associated immunity (immunosenescence) has recently emerged, since there is evidence of a direct interaction between Cav-1 and TLR5.46 This interaction is important to maintain TLR5 expression and signaling during the aging process.46 Experimental results also support Cav-1 dependent TLR5 preservation in aging. Overexpressed Cav-1 in vitro enhances TLR5 mRNA through the mitogen-activated protein kinases (MAPKs) pathway and prolonged TLR5 protein half-life through direct interaction.96 KO mice research also demonstrate that TLR5/MyD88, an adaptor protein of TLRs, signaling is regulated by Cav-1 and induces the production of pro-inflammatory cytokines by stimulation of a TLR5 agonist flagellin.46 Moreover, it also proved that flagellin-conjugated antigens induce a significantly higher level of specific antibodies in response to the antigen and better protection against lethal challenges.46 It means that Cav-1/TLR5 signaling plays a key role in age-associated innate immune responses and that stimulation of Cav-1/TLR5 may be a good model of a mucosal vaccine adjuvant against infection via overcoming immunosenescence in the elderly.
CONCLUSIONS
Cav-1/caveolae have emerged as having vital functions in aging and aging-related diseases. The different density of Cav-1/caveolae in different cell types or tissues may associate with particular functions (Table 1). In aging, Cav-1 is up-regulated, causing cellular senescence with changing in cellular morphology, weakening the proliferation rate as well as cellular signaling. However, Cav-1 up-regulation also has a vital role in maintaining and stabilizing TLR5 against immunosenescence. These results significantly contribute to our understanding of innate immunity in aging and support the need to extend Cav-1 research in immunity. Moreover, Cav-1 expression level changes in various types of cancer, subsequently affecting cancer growth rates, are considered to be a valuable prognostic marker for cancer. Furthermore, the function of Cav-1/caveolae in other aging related-diseases such as type II diabetes and atherosclerosis is also well established and suggests that Cav-1/caveolae may serve as a therapeutic target for these diseases. Taken together, Cav-1/caveolae research in the aging field is important to more deeply understand the underlying mechanisms of Cav-1-dependent aging processes as well as efficiently develop therapies against aging-related diseases.
Footnotes
CONFLICT OF INTEREST STATEMENT: None declared.
References
- 1.Thomas CM, Smart EJ. Caveolae structure and function. J Cell Mol Med. 2008;12:796–809. doi: 10.1111/j.1582-4934.2008.00295.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu P, Rudick M, Anderson RG. Multiple functions of caveolin-1. J Biol Chem. 2002;277:41295–41298. doi: 10.1074/jbc.R200020200. [DOI] [PubMed] [Google Scholar]
- 3.Anderson RG. The caveolae membrane system. Annu Rev Biochem. 1998;67:199–225. doi: 10.1146/annurev.biochem.67.1.199. [DOI] [PubMed] [Google Scholar]
- 4.Boscher C, Nabi IR. Caveolin-1: role in cell signaling. In: Jasmin JF, Frank PG, Lisanti MP, editors. Caveolins and Caveolae. New York: Springer; 2012. pp. 29–50. [Google Scholar]
- 5.Parton RG, Simons K. The multiple faces of caveolae. Nat Rev Mol Cell Biol. 2007;8:185–194. doi: 10.1038/nrm2122. [DOI] [PubMed] [Google Scholar]
- 6.Schlegel A, Lisanti MP. A molecular dissection of caveolin-1 membrane attachment and oligomerization Two separate regions of the caveolin-1 C-terminal domain mediate membrane binding and oligomer/oligomer interactions in vivo. J Biol Chem. 2000;275:21605–21617. doi: 10.1074/jbc.M002558200. [DOI] [PubMed] [Google Scholar]
- 7.Razani B, Woodman SE, Lisanti MP. Caveolae: from cell biology to animal physiology. Pharmacol Rev. 2002;54:431–467. doi: 10.1124/pr.54.3.431. [DOI] [PubMed] [Google Scholar]
- 8.Sowa G, Pypaert M, Sessa WC. Distinction between signaling mechanisms in lipid rafts vs. caveolae. Proc Natl Acad Sci U S A. 2001;98:14072–14077. doi: 10.1073/pnas.241409998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patel HH, Murray F, Insel PA. Caveolae as organizers of pharmacologically relevant signal transduction molecules. Annu Rev Pharmacol Toxicol. 2008;48:359–391. doi: 10.1146/annurev.pharmtox.48.121506.124841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Low JY, Nicholson HD. Epigenetic modifications of caveolae associated proteins in health and disease. BMC Genet. 2015;16:71. doi: 10.1186/s12863-015-0231-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Quest AF, Gutierrez-Pajares JL, Torres VA. Caveolin-1: an ambiguous partner in cell signalling and cancer. J Cell Mol Med. 2008;12:1130–1150. doi: 10.1111/j.1582-4934.2008.00331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Helmond ZK, Miners JS, Bednall E, Chalmers KA, Zhang Y, Wilcock GK, et al. Caveolin-1 and -2 and their relationship to cerebral amyloid angiopathy in Alzheimer's disease. Neuropathol Appl Neurobiol. 2007;33:317–327. doi: 10.1111/j.1365-2990.2006.00815.x. [DOI] [PubMed] [Google Scholar]
- 13.Williams TM, Lisanti MP. The caveolin proteins. Genome Biol. 2004;5:214. doi: 10.1186/gb-2004-5-3-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yun JH, Park SJ, Jo A, Kang JL, Jou I, Park JS, et al. Caveolin-1 is involved in reactive oxygen species-induced SHP-2 activation in astrocytes. Exp Mol Med. 2011;43:660–668. doi: 10.3858/emm.2011.43.12.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stahlhut M, van Deurs B. Identification of filamin as a novel ligand for caveolin-1: evidence for the organization of caveolin-1-associated membrane domains by the actin cytoskeleton. Mol Biol Cell. 2000;11:325–337. doi: 10.1091/mbc.11.1.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.González-Muñoz E, López-Iglesias C, Calvo M, Palacín M, Zorzano A, Camps M. Caveolin-1 loss of function accelerates glucose transporter 4 and insulin receptor degradation in 3T3-L1 adipocytes. Endocrinology. 2009;150:3493–3502. doi: 10.1210/en.2008-1520. [DOI] [PubMed] [Google Scholar]
- 17.Miyawaki-Shimizu K, Predescu D, Shimizu J, Broman M, Predescu S, Malik AB. siRNA-induced caveolin-1 knockdown in mice increases lung vascular permeability via the junctional pathway. Am J Physiol Lung Cell Mol Physiol. 2006;290:L405–L413. doi: 10.1152/ajplung.00292.2005. [DOI] [PubMed] [Google Scholar]
- 18.Parton RG, del Pozo MA. Caveolae as plasma membrane sensors, protectors and organizers. Nat Rev Mol Cell Biol. 2013;14:98–112. doi: 10.1038/nrm3512. [DOI] [PubMed] [Google Scholar]
- 19.Wang XM, Kim HP, Nakahira K, Ryter SW, Choi AM. The heme oxygenase-1/carbon monoxide pathway suppresses TLR4 signaling by regulating the interaction of TLR4 with caveolin-1. J Immunol. 2009;182:3809–3818. doi: 10.4049/jimmunol.0712437. [DOI] [PubMed] [Google Scholar]
- 20.Pike LJ. Growth factor receptors, lipid rafts and caveolae: an evolving story. Biochim Biophys Acta. 2005;1746:260–273. doi: 10.1016/j.bbamcr.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 21.Gratton JP, Bernatchez P, Sessa WC. Caveolae and caveolins in the cardiovascular system. Circ Res. 2004;94:1408–1417. doi: 10.1161/01.RES.0000129178.56294.17. [DOI] [PubMed] [Google Scholar]
- 22.Smith RM, Harada S, Smith JA, Zhang S, Jarett L. Insulin-induced protein tyrosine phosphorylation cascade and signalling molecules are localized in a caveolin-enriched cell membrane domain. Cell Signal. 1998;10:355–362. doi: 10.1016/s0898-6568(97)00170-8. [DOI] [PubMed] [Google Scholar]
- 23.Lajoie P, Nabi IR. Lipid rafts, caveolae, and their endocytosis. In: Kwang WJ, editor. International Review of Cell and Molecular Biology. AmsterdamL: Academic Press; 2010. pp. 135–163. [DOI] [PubMed] [Google Scholar]
- 24.Bastiani M, Parton RG. Caveolae at a glance. J Cell Sci. 2010;123:3831–3836. doi: 10.1242/jcs.070102. [DOI] [PubMed] [Google Scholar]
- 25.Quest AF, Leyton L, Párraga M. Caveolins, caveolae, and lipid rafts in cellular transport, signaling, and disease. Biochem Cell Biol. 2004;82:129–144. doi: 10.1139/o03-071. [DOI] [PubMed] [Google Scholar]
- 26.Cheng JPX, Nichols BJ. Caveolae: one function or many? Trends Cell Biol. 2016;26:177–189. doi: 10.1016/j.tcb.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 27.Levine TB, Levine AB. Metabolic Syndrome and Cardiovascular Disease. New York: John Wiley & Sons; 2012. [Google Scholar]
- 28.Jasmin JF, Frank PG, Lisanti MP. Caveolins and caveolae: roles in signaling and disease mechanisms. New York: Springer; 2012. [Google Scholar]
- 29.Lin YC, Lin CH, Kuo CY, Yang VC. ABCA1 modulates the oligomerization and Golgi exit of caveolin-1 during HDL-mediated cholesterol efflux in aortic endothelial cells. Biochem Biophys Res Commun. 2009;382:189–195. doi: 10.1016/j.bbrc.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 30.Boettcher JP, Kirchner M, Churin Y, Kaushansky A, Pompaiah M, Thorn H, et al. Tyrosine-phosphorylated caveolin-1 blocks bacterial uptake by inducing Vav2-RhoA-mediated cytoskeletal rearrangements. PLoS Biol. 2010;8 doi: 10.1371/journal.pbio.1000457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schlegel A, Arvan P, Lisanti MP. Caveolin-1 binding to endoplasmic reticulum membranes and entry into the regulated secretory pathway are regulated by serine phosphorylation. Protein sorting at the level of the endoplasmic reticulum. J Biol Chem. 2001;276:4398–4408. doi: 10.1074/jbc.M005448200. [DOI] [PubMed] [Google Scholar]
- 32.Qin H, Bollag WB. The caveolin-1 scaffolding domain peptide decreases phosphatidylglycerol levels and inhibits calcium-induced differentiation in mouse keratinocytes. PLoS One. 2013;8:e80946. doi: 10.1371/journal.pone.0080946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Collins BM, Davis MJ, Hancock JF, Parton RG. Structure-based reassessment of the caveolin signaling model: do caveolae regulate signaling through caveolin-protein interactions? Dev Cell. 2012;23:11–20. doi: 10.1016/j.devcel.2012.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Byrne DP, Dart C, Rigden DJ. Evaluating caveolin interactions: do proteins interact with the caveolin scaffolding domain through a widespread aromatic residue-rich motif? PLoS One. 2012;7:e44879. doi: 10.1371/journal.pone.0044879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Le Lay S, Rodriguez M, Jessup W, Rentero C, Li Q, Cartland S, et al. Caveolin-1-mediated apolipoprotein A-I membrane binding sites are not required for cholesterol efflux. PLoS One. 2011;6:e23353. doi: 10.1371/journal.pone.0023353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Joshi B, Bastiani M, Strugnell SS, Boscher C, Parton RG, Nabi IR. Phosphocaveolin-1 is a mechanotransducer that induces caveola biogenesis via Egr1 transcriptional regulation. J Cell Biol. 2012;199:425–435. doi: 10.1083/jcb.201207089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cameron PL, Ruffin JW, Bollag R, Rasmussen H, Cameron RS. Identification of caveolin and caveolin-related proteins in the brain. J Neurosci. 1997;17:9520–9535. doi: 10.1523/JNEUROSCI.17-24-09520.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen Z, Bakhshi FR, Shajahan AN, Sharma T, Mao M, Trane A, et al. Nitric oxide-dependent Src activation and resultant caveolin-1 phosphorylation promote eNOS/caveolin-1 binding and eNOS inhibition. Mol Biol Cell. 2012;23:1388–1398. doi: 10.1091/mbc.E11-09-0811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen X, Whiting C, Borza C, Hu W, Mont S, Bulus N, et al. Integrin alpha1beta1 regulates epidermal growth factor receptor activation by controlling peroxisome proliferator-activated receptor gamma-dependent caveolin-1 expression. Mol Cell Biol. 2010;30:3048–3058. doi: 10.1128/MCB.00892-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lajoie P, Partridge EA, Guay G, Goetz JG, Pawling J, Lagana A, et al. Plasma membrane domain organization regulates EGFR signaling in tumor cells. J Cell Biol. 2007;179:341–356. doi: 10.1083/jcb.200611106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Labrecque L, Nyalendo C, Langlois S, Durocher Y, Roghi C, Murphy G, et al. Src-mediated tyrosine phosphorylation of caveolin-1 induces its association with membrane type 1 matrix metalloproteinase. J Biol Chem. 2004;279:52132–52140. doi: 10.1074/jbc.M409617200. [DOI] [PubMed] [Google Scholar]
- 42.Schlegel A, Wang C, Katzenellenbogen BS, Pestell RG, Lisanti MP. Caveolin-1 potentiates estrogen receptor alpha (ERalpha) signaling. caveolin-1 drives ligand-independent nuclear translocation and activation of ERalpha. J Biol Chem. 1999;274:33551–33556. doi: 10.1074/jbc.274.47.33551. [DOI] [PubMed] [Google Scholar]
- 43.Zhang X, Ling MT, Wang Q, Lau CK, Leung SC, Lee TK, et al. Identification of a novel inhibitor of differentiation-1 (ID-1) binding partner, caveolin-1, and its role in epithelial-mesenchymal transition and resistance to apoptosis in prostate cancer cells. J Biol Chem. 2007;282:33284–33294. doi: 10.1074/jbc.M705089200. [DOI] [PubMed] [Google Scholar]
- 44.Lu Z, Ghosh S, Wang Z, Hunter T. Downregulation of caveolin-1 function by EGF leads to the loss of E-cadherin, increased transcriptional activity of beta-catenin, and enhanced tumor cell invasion. Cancer Cell. 2003;4:499–515. doi: 10.1016/s1535-6108(03)00304-0. [DOI] [PubMed] [Google Scholar]
- 45.Williams TM, Lisanti MP. Caveolin-1 in oncogenic transformation, cancer, and metastasis. Am J Physiol Cell Physiol. 2005;288:C494–C506. doi: 10.1152/ajpcell.00458.2004. [DOI] [PubMed] [Google Scholar]
- 46.Lim JS, Nguyen KC, Nguyen CT, Jang IS, Han JM, Fabian C, et al. Flagellin-dependent TLR5/caveolin-1 as a promising immune activator in immunosenescence. Aging Cell. 2015;14:907–915. doi: 10.1111/acel.12383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Scherer PE, Lisanti MP, Baldini G, Sargiacomo M, Mastick CC, Lodish HF. Induction of caveolin during adipogenesis and association of GLUT4 with caveolin-rich vesicles. J Cell Biol. 1994;127:1233–1243. doi: 10.1083/jcb.127.5.1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yamamoto M, Okumura S, Oka N, Schwencke C, Ishikawa Y. Downregulation of caveolin expression by cAMP signal. Life Sci. 1999;64:1349–1357. doi: 10.1016/s0024-3205(99)00070-3. [DOI] [PubMed] [Google Scholar]
- 49.Park WY, Cho KA, Park JS, Kim DI, Park SC. Attenuation of EGF signaling in senescent cells by caveolin. Ann N Y Acad Sci. 2001;928:79–84. doi: 10.1111/j.1749-6632.2001.tb05638.x. [DOI] [PubMed] [Google Scholar]
- 50.Park DS, Razani B, Lasorella A, Schreiber-Agus N, Pestell RG, Iavarone A, et al. Evidence that Myc isoforms transcriptionally repress caveolin-1 gene expression via an INR-dependent mechanism. Biochemistry. 2001;40:3354–3362. doi: 10.1021/bi002787b. [DOI] [PubMed] [Google Scholar]
- 51.Bist A, Fielding PE, Fielding CJ. Two sterol regulatory element-like sequences mediate up-regulation of caveolin gene transcription in response to low density lipoprotein free cholesterol. Proc Natl Acad Sci U S A. 1997;94:10693–10698. doi: 10.1073/pnas.94.20.10693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Boopathi E, Gomes CM, Goldfarb R, John M, Srinivasan VG, Alanzi J, et al. Transcriptional repression of Caveolin-1 (CAV1) gene expression by GATA-6 in bladder smooth muscle hypertrophy in mice and human beings. Am J Pathol. 2011;178:2236–2251. doi: 10.1016/j.ajpath.2011.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.van den Heuvel AP, Schulze A, Burgering BM. Direct control of caveolin-1 expression by FOXO transcription factors. Biochem J. 2005;385:795–802. doi: 10.1042/BJ20041449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Verma M, Srivastava S. Epigenetics in cancer: implications for early detection and prevention. Lancet Oncol. 2002;3:755–763. doi: 10.1016/s1470-2045(02)00932-4. [DOI] [PubMed] [Google Scholar]
- 55.Deb M, Sengupta D, Kar S, Rath SK, Roy S, Das G, et al. Epigenetic drift towards histone modifications regulates CAV1 gene expression in colon cancer. Gene. 2016;581:75–84. doi: 10.1016/j.gene.2016.01.029. [DOI] [PubMed] [Google Scholar]
- 56.Park WY, Park JS, Cho KA, Kim DI, Ko YG, Seo JS, et al. Up-regulation of caveolin attenuates epidermal growth factor signaling in senescent cells. J Biol Chem. 2000;275:20847–20852. doi: 10.1074/jbc.M908162199. [DOI] [PubMed] [Google Scholar]
- 57.Cho KA, Ryu SJ, Oh YS, Park JH, Lee JW, Kim HP, et al. Morphological adjustment of senescent cells by modulating caveolin-1 status. J Biol Chem. 2004;279:42270–42278. doi: 10.1074/jbc.M402352200. [DOI] [PubMed] [Google Scholar]
- 58.Cho KA, Ryu SJ, Park JS, Jang IS, Ahn JS, Kim KT, et al. Senescent phenotype can be reversed by reduction of caveolin status. J Biol Chem. 2003;278:27789–27795. doi: 10.1074/jbc.M208105200. [DOI] [PubMed] [Google Scholar]
- 59.Volonte D, Zhang K, Lisanti MP, Galbiati F. Expression of caveolin-1 induces premature cellular senescence in primary cultures of murine fibroblasts. Mol Biol Cell. 2002;13:2502–2517. doi: 10.1091/mbc.01-11-0529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Head BP, Peart JN, Panneerselvam M, Yokoyama T, Pearn ML, Niesman IR, et al. Loss of caveolin-1 accelerates neurodegeneration and aging. PLoS One. 2010;5:e15697. doi: 10.1371/journal.pone.0015697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Volonte D, Kahkonen B, Shapiro S, Di Y, Galbiati F. Caveolin-1 expression is required for the development of pulmonary emphysema through activation of the ATM-p53-p21 pathway. J Biol Chem. 2009;284:5462–5466. doi: 10.1074/jbc.C800225200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lee JA, Choi DI, Choi JY, Kim SO, Cho KA, Lee JB, et al. Methyl-β-cyclodextrin up-regulates collagen I expression in chronologically-aged skin via its anti-caveolin-1 activity. Oncotarget. 2015;6:1942–1953. doi: 10.18632/oncotarget.3039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Powter EE, Coleman PR, Tran MH, Lay AJ, Bertolino P, Parton RG, et al. Caveolae control the anti-inflammatory phenotype of senescent endothelial cells. Aging Cell. 2015;14:102–111. doi: 10.1111/acel.12270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.de Magalhães JP. How ageing processes influence cancer. Nat Rev Cancer. 2013;13:357–365. doi: 10.1038/nrc3497. [DOI] [PubMed] [Google Scholar]
- 65.Williams TM, Lisanti MP. Caveolin-1 in oncogenic transformation, cancer, and metastasis. Am J Physiol Cell Physiol. 2005;288:C494–C506. doi: 10.1152/ajpcell.00458.2004. [DOI] [PubMed] [Google Scholar]
- 66.Martinez-Outschoorn UE, Sotgia F, Lisanti MP. Caveolae and signalling in cancer. Nat Rev Cancer. 2015;15:225–237. doi: 10.1038/nrc3915. [DOI] [PubMed] [Google Scholar]
- 67.Boscher C, Nabi IR. Caveolin-1: role in cell signaling. In: Jasmin JF, Frank PG, Lisanti MP, editors. Caveolins and Caveolae: Roles in Signaling and Disease Mechanisms. New York, NY: Springer; 2012. pp. 29–50. [Google Scholar]
- 68.Yang G, Truong LD, Timme TL, Ren C, Wheeler TM, Park SH, et al. Elevated expression of caveolin is associated with prostate and breast cancer. Clin Cancer Res. 1998;4:1873–1880. [PubMed] [Google Scholar]
- 69.Li L, Ittmann MM, Ayala G, Tsai MJ, Amato RJ, Wheeler TM, et al. The emerging role of the PI3-K-Akt pathway in prostate cancer progression. Prostate Cancer Prostatic Dis. 2005;8:108–118. doi: 10.1038/sj.pcan.4500776. [DOI] [PubMed] [Google Scholar]
- 70.Gunasekaran U, Gannon M. Type 2 diabetes and the aging pancreatic beta cell. Aging (Albany NY) 2011;3:565–575. doi: 10.18632/aging.100350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cohen AW, Razani B, Wang XB, Combs TP, Williams TM, Scherer PE, et al. Caveolin-1-deficient mice show insulin resistance and defective insulin receptor protein expression in adipose tissue. Am J Physiol Cell Physiol. 2003;285:C222–C235. doi: 10.1152/ajpcell.00006.2003. [DOI] [PubMed] [Google Scholar]
- 72.Razani B, Combs TP, Wang XB, Frank PG, Park DS, Russell RG, et al. Caveolin-1-deficient mice are lean, resistant to diet-induced obesity, and show hypertriglyceridemia with adipocyte abnormalities. J Biol Chem. 2002;277:8635–8647. doi: 10.1074/jbc.M110970200. [DOI] [PubMed] [Google Scholar]
- 73.Oh YS, Khil LY, Cho KA, Ryu SJ, Ha MK, Cheon GJ, et al. A potential role for skeletal muscle caveolin-1 as an insulin sensitivity modulator in ageing-dependent non-obese type 2 diabetes: studies in a new mouse model. Diabetologia. 2008;51:1025–1034. doi: 10.1007/s00125-008-0993-0. [DOI] [PubMed] [Google Scholar]
- 74.Oh YS, Lee TS, Cheon GJ, Jang IS, Jun HS, Park SC. Modulation of insulin sensitivity and caveolin-1 expression by orchidectomy in a nonobese type 2 diabetes animal model. Mol Med. 2011;17:4–11. doi: 10.2119/molmed.2009.00105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mahavadi S, Nalli A, Kumar D, Bhattacharya S, Zhou R, Grider J, et al. Increased expression of caveolin-1 is associated with up-regulation of the RhoA/Rho kinase pathway and smooth muscle contraction in diabetes (1110.11) FASEB J. 2014;28 [Google Scholar]
- 76.Drab M, Verkade P, Elger M, Kasper M, Lohn M, Lauterbach B, et al. Loss of caveolae, vascular dysfunction, and pulmonary defects in caveolin-1 gene-disrupted mice. Science. 2001;293:2449–2452. doi: 10.1126/science.1062688. [DOI] [PubMed] [Google Scholar]
- 77.Ross R. Atherosclerosis--an inflammatory disease. N Engl J Med. 1999;340:115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 78.Frank PG, Woodman SE, Park DS, Lisanti MP. Caveolin, caveolae, and endothelial cell function. Arterioscler Thromb Vasc Biol. 2003;23:1161–1168. doi: 10.1161/01.ATV.0000070546.16946.3A. [DOI] [PubMed] [Google Scholar]
- 79.Fernández-Hernando C, Yu J, Dávalos A, Prendergast J, Sessa WC. Endothelial-specific overexpression of caveolin-1 accelerates atherosclerosis in apolipoprotein E-deficient mice. Am J Pathol. 2010;177:998–1003. doi: 10.2353/ajpath.2010.091287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Razani B, Combs TP, Wang XB, Frank PG, Park DS, Russell RG, et al. Caveolin-1-deficient mice are lean, resistant to diet-induced obesity, and show hypertriglyceridemia with adipocyte abnormalities. J Biol Chem. 2002;277:8635–8647. doi: 10.1074/jbc.M110970200. [DOI] [PubMed] [Google Scholar]
- 81.Frank PG. Endothelial caveolae and caveolin-1 as key regulators of atherosclerosis. Am J Pathol. 2010;177:544–546. doi: 10.2353/ajpath.2010.100247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lim JS, Shin M, Kim HJ, Kim KS, Choy HE, Cho KA. Caveolin-1 mediates Salmonella invasion via the regulation of SopE-dependent Rac1 activation and actin reorganization. J Infect Dis. 2014;210:793–802. doi: 10.1093/infdis/jiu152. [DOI] [PubMed] [Google Scholar]
- 83.Gavazzi G, Krause KH. Ageing and infection. Lancet Infect Dis. 2002;2:659–666. doi: 10.1016/s1473-3099(02)00437-1. [DOI] [PubMed] [Google Scholar]
- 84.Lim JS, Choy HE, Park SC, Han JM, Jang IS, Cho KA. Caveolae-mediated entry of Salmonella typhimurium into senescent nonphagocytotic host cells. Aging Cell. 2010;9:243–251. doi: 10.1111/j.1474-9726.2010.00554.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Simionescu N, Siminoescu M, Palade GE. Permeability of muscle capillaries to small heme-peptides. Evidence for the existence of patent transendothelial channels. J Cell Biol. 1975;64:586–607. doi: 10.1083/jcb.64.3.586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kiss AL, Botos E. Endocytosis via caveolae: alternative pathway with distinct cellular compartments to avoid lysosomal degradation? J Cell Mol Med. 2009;13:1228–1237. doi: 10.1111/j.1582-4934.2009.00754.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gruenberg J, van der Goot FG. Mechanisms of pathogen entry through the endosomal compartments. Nat Rev Mol Cell Biol. 2006;7:495–504. doi: 10.1038/nrm1959. [DOI] [PubMed] [Google Scholar]
- 88.Pang H, Le PU, Nabi IR. Ganglioside GM1 levels are a determinant of the extent of caveolae/raft-dependent endocytosis of cholera toxin to the Golgi apparatus. J Cell Sci. 2004;117:1421–1430. doi: 10.1242/jcs.01009. [DOI] [PubMed] [Google Scholar]
- 89.Ferrari A, Pellegrini V, Arcangeli C, Fittipaldi A, Giacca M, Beltram F. Caveolae-mediated internalization of extracellular HIV-1 tat fusion proteins visualized in real time. Mol Ther. 2003;8:284–294. doi: 10.1016/s1525-0016(03)00122-9. [DOI] [PubMed] [Google Scholar]
- 90.Schubert W, Frank PG, Razani B, Park DS, Chow CW, Lisanti MP. Caveolae-deficient endothelial cells show defects in the uptake and transport of albumin in vivo. J Biol Chem. 2001;276:48619–48622. doi: 10.1074/jbc.C100613200. [DOI] [PubMed] [Google Scholar]
- 91.Tomassian T, Humphries LA, Liu SD, Silva O, Brooks DG, Miceli MC. Caveolin-1 orchestrates TCR synaptic polarity, signal specificity, and function in CD8 T cells. J Immunol. 2011;187:2993–3002. doi: 10.4049/jimmunol.1101447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ohnuma K, Uchiyama M, Yamochi T, Nishibashi K, Hosono O, Takahashi N, et al. Caveolin-1 triggers T-cell activation via CD26 in association with CARMA1. J Biol Chem. 2007;282:10117–10131. doi: 10.1074/jbc.M609157200. [DOI] [PubMed] [Google Scholar]
- 93.Medina FA, Williams TM, Sotgia F, Tanowitz HB, Lisanti MP. A novel role for caveolin-1 in B lymphocyte function and the development of thymus-independent immune responses. Cell Cycle. 2006;5:1865–1871. doi: 10.4161/cc.5.16.3132. [DOI] [PubMed] [Google Scholar]
- 94.Medina FA, de Almeida CJ, Dew E, Li J, Bonuccelli G, Williams TM, et al. Caveolin-1-deficient mice show defects in innate immunity and inflammatory immune response during Salmonella enterica serovar Typhimurium infection. Infect Immun. 2006;74:6665–6674. doi: 10.1128/IAI.00949-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lei MG, Morrison DC. Differential expression of caveolin-1 in lipopolysaccharide-activated murine macrophages. Infect Immun. 2000;68:5084–5089. doi: 10.1128/iai.68.9.5084-5089.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lim JS, Nguyen KC, Han JM, Jang IS, Fabian C, Cho KA. Direct Regulation of TLR5 Expression by Caveolin-1. Mol Cells. 2015;38:1111–1117. doi: 10.14348/molcells.2015.0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Escriche M, Burgueño J, Ciruela F, Canela EI, Mallol J, Enrich C, et al. Ligand-induced caveolae-mediated internalization of A1 adenosine receptors: morphological evidence of endosomal sorting and receptor recycling. Exp Cell Res. 2003;285:72–90. doi: 10.1016/s0014-4827(02)00090-3. [DOI] [PubMed] [Google Scholar]
- 98.Liu L, Xu HX, Wang WQ, Wu CT, Chen T, Qin Y, et al. Cavin-1 is essential for the tumor-promoting effect of caveolin-1 and enhances its prognostic potency in pancreatic cancer. Oncogene. 2014;33:2728–2736. doi: 10.1038/onc.2013.223. [DOI] [PubMed] [Google Scholar]
- 99.Yang G, Xu H, Li Z, Li F. Interactions of caveolin-1 scaffolding and intramembrane regions containing a CRAC motif with cholesterol in lipid bilayers. Biochim Biophys Acta. 2014;1838:2588–2599. doi: 10.1016/j.bbamem.2014.06.018. [DOI] [PubMed] [Google Scholar]
- 100.Engelman JA, Chu C, Lin A, Jo H, Ikezu T, Okamoto T, et al. Caveolin-mediated regulation of signaling along the p42/44 MAP kinase cascade in vivo. A role for the caveolin-scaffolding domain. FEBS Lett. 1998;428:205–211. doi: 10.1016/s0014-5793(98)00470-0. [DOI] [PubMed] [Google Scholar]
- 101.Sato M, Hutchinson DS, Halls ML, Furness SG, Bengtsson T, Evans BA, et al. Interaction with caveolin-1 modulates G protein coupling of mouse β3-adrenoceptor. J Biol Chem. 2012;287:20674–20688. doi: 10.1074/jbc.M111.280651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Calizo RC, Scarlata S. A role for G-proteins in directing G-protein-coupled receptor-caveolae localization. Biochemistry. 2012;51:9513–9523. doi: 10.1021/bi301107p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Shen J, Lee W, Li Y, Lau CF, Ng KM, Fung ML, et al. Interaction of caveolin-1, nitric oxide, and nitric oxide synthases in hypoxic human SK-N-MC neuroblastoma cells. J Neurochem. 2008;107:478–487. doi: 10.1111/j.1471-4159.2008.05630.x. [DOI] [PubMed] [Google Scholar]
- 104.Kabayama K, Sato T, Saito K, Loberto N, Prinetti A, Sonnino S, et al. Dissociation of the insulin receptor and caveolin-1 complex by ganglioside GM3 in the state of insulin resistance. Proc Natl Acad Sci U S A. 2007;104:13678–13683. doi: 10.1073/pnas.0703650104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sato Y, Sagami I, Shimizu T. Identification of caveolin-1-interacting sites in neuronal nitric-oxide synthase. Molecular mechanism for inhibition of NO formation. J Biol Chem. 2004;279:8827–8836. doi: 10.1074/jbc.M310327200. [DOI] [PubMed] [Google Scholar]
- 106.Volonte D, Liu Z, Musille PM, Stoppani E, Wakabayashi N, Di YP, et al. Inhibition of nuclear factor-erythroid 2-related factor (Nrf2) by caveolin-1 promotes stress-induced premature senescence. Mol Biol Cell. 2013;24:1852–1862. doi: 10.1091/mbc.E12-09-0666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Li L, Ren C, Yang G, Goltsov AA, Tabata K, Thompson TC. Caveolin-1 promotes autoregulatory, Akt-mediated induction of cancer-promoting growth factors in prostate cancer cells. Mol Cancer Res. 2009;7:1781–1791. doi: 10.1158/1541-7786.MCR-09-0255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Mercier I, Jasmin JF, Lisanti MP. Caveolins in Cancer Pathogenesis, Prevention and Therapy. New York: Springer; 2011. [Google Scholar]
- 109.Razani B, Lisanti MP. Two distinct caveolin-1 domains mediate the functional interaction of caveolin-1 with protein kinase A. Am J Physiol Cell Physiol. 2001;281:C1241–C1250. doi: 10.1152/ajpcell.2001.281.4.C1241. [DOI] [PubMed] [Google Scholar]
- 110.Jiao J, Garg V, Yang B, Elton TS, Hu K. Protein kinase C-epsilon induces caveolin-dependent internalization of vascular adenosine 5'-triphosphate-sensitive K+ channels. Hypertension. 2008;52:499–506. doi: 10.1161/HYPERTENSIONAHA.108.110817. [DOI] [PubMed] [Google Scholar]
- 111.Conde-Perez A, Gros G, Longvert C, Pedersen M, Petit V, Aktary Z, et al. A caveolin-dependent and PI3K/AKT-independent role of PTEN in β-catenin transcriptional activity. Nat Commun. 2015;6:8093. doi: 10.1038/ncomms9093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Senetta R, Stella G, Pozzi E, Sturli N, Massi D, Cassoni P. Caveolin-1 as a promoter of tumour spreading: when, how, where and why. J Cell Mol Med. 2013;17:325–336. doi: 10.1111/jcmm.12030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Razani B, Zhang XL, Bitzer M, von Gersdorff G, Böttinger EP, Lisanti MP. Caveolin-1 regulates transforming growth factor (TGF)-beta/SMAD signaling through an interaction with the TGF-beta type I receptor. J Biol Chem. 2001;276:6727–6738. doi: 10.1074/jbc.M008340200. [DOI] [PubMed] [Google Scholar]
- 114.Lim JS, Nguyen KC, Han JM, Jang IS, Fabian C, Cho KA. Direct Regulation of TLR5 Expression by Caveolin-1. Mol Cells. 2015;38:1111–1117. doi: 10.14348/molcells.2015.0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Czikora I, Feher A, Lucas R, Fulton DJ, Bagi Z. Caveolin-1 prevents sustained angiotensin II-induced resistance artery constriction and obesity-induced high blood pressure. Am J Physiol Heart Circ Physiol. 2015;308:H376–H385. doi: 10.1152/ajpheart.00649.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Tahir SA, Park S, Thompson TC. Caveolin-1 regulates VEGF-stimulated angiogenic activities in prostate cancer and endothelial cells. Cancer Biol Ther. 2009;8:2286–2296. doi: 10.4161/cbt.8.23.10138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hehlgans S, Cordes N. Caveolin-1: an essential modulator of cancer cell radio-and chemoresistance. Am J Cancer Res. 2011;1:521–530. [PMC free article] [PubMed] [Google Scholar]
- 118.Chiu WT, Lee HT, Huang FJ, Aldape KD, Yao J, Steeg PS, et al. Caveolin-1 upregulation mediates suppression of primary breast tumor growth and brain metastases by stat3 inhibition. Cancer Res. 2011;71:4932–4943. doi: 10.1158/0008-5472.CAN-10-4249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Suprynowicz FA, Disbrow GL, Krawczyk E, Simic V, Lantzky K, Schlegel R. HPV-16 E5 oncoprotein upregulates lipid raft components caveolin-1 and ganglioside GM1 at the plasma membrane of cervical cells. Oncogene. 2008;27:1071–1078. doi: 10.1038/sj.onc.1210725. [DOI] [PubMed] [Google Scholar]
- 120.Park J, Bae E, Lee C, Yoon SS, Chae YS, Ahn KS, et al. RNA interference-directed caveolin-1 knockdown sensitizes SN12CPM6 cells to doxorubicin-induced apoptosis and reduces lung metastasis. Tumour Biol. 2010;31:643–650. doi: 10.1007/s13277-010-0081-1. [DOI] [PubMed] [Google Scholar]
- 121.Diaz-Valdivia N, Bravo D, Huerta H, Henriquez S, Gabler F, Vega M, et al. Enhanced caveolin-1 expression increases migration, anchorage-independent growth and invasion of endometrial adenocarcinoma cells. BMC Cancer. 2015;15:463. doi: 10.1186/s12885-015-1477-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Chatterjee M, Ben-Josef E, Thomas DG, Morgan MA, Zalupski MM, Khan G, et al. Caveolin-1 is associated with tumor progression and confers a multi-modality resistance phenotype in pancreatic cancer. Sci Rep. 2015;5:10867. doi: 10.1038/srep10867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Yang G, Goltsov AA, Ren C, Kurosaka S, Edamura K, Logothetis R, et al. Caveolin-1 upregulation contributes to c-Myc-induced high-grade prostatic intraepithelial neoplasia and prostate cancer. Mol Cancer Res. 2012;10:218–229. doi: 10.1158/1541-7786.MCR-11-0451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Thompson TC, Tahir SA, Li L, Watanabe M, Naruishi K, Yang G, et al. The role of caveolin-1 in prostate cancer: clinical implications. Prostate Cancer Prostatic Dis. 2010;13:6–11. doi: 10.1038/pcan.2009.29. [DOI] [PMC free article] [PubMed] [Google Scholar]