Abstract
Bitter taste receptors (TAS2Rs or T2Rs) belong to the superfamily of seven-transmembrane G protein–coupled receptors, which are the targets of >50% of drugs currently on the market. Canonically, T2Rs are located in taste buds of the tongue, where they initiate bitter taste perception. However, accumulating evidence indicates that T2Rs are widely expressed throughout the body and mediate diverse nontasting roles through various specialized mechanisms. It has also become apparent that T2Rs and their polymorphisms are associated with human disorders. In this review, we summarize the physiological and pathophysiological roles that extraoral T2Rs play in processes as diverse as innate immunity and reproduction, and the major challenges in this emerging field.
Introduction
“Good medicine always tastes bitter.” This ancient Oriental wisdom may soon be verified with modern biology. Traditionally, bitter taste, one of five basic taste qualities, is thought to guide organisms to avoid harmful toxins and noxious substances and thus is critical to animal and human survival. The sensors for bitter compounds in vertebrates are bitter taste receptors (T2Rs or TAS2Rs), a class of G protein–coupled receptors (GPCRs) originally identified in type II taste receptor cells in the taste bud. Traditionally it has been assumed that, responding to the pressure of food selection, different species have evolved with different numbers of T2Rs: 25 in humans and 35 in mice (Shi et al., 2003; Chandrashekar et al., 2006). Over the past decade, however, the expression of T2Rs and their downstream signaling molecules have been found in several extraoral systems, including the digestive, respiratory, and genitourinary systems, as well as in brain and immune cells. Moreover, these receptors carry out different biological functions in their varied locations. These findings raise the intriguing possibilities that the evolution of T2Rs may also be influenced by the biological functions mediated by these receptors in the extraoral cells and tissues (Campbell et al., 2014), that these extraoral T2Rs may be attractive targets for new medicines, and that currently used bitter medicines may exert their pharmacological functions by acting on these extraoral receptors—which, until now, have been considered side effects or adverse effects.
In this review, we summarize our current understanding of bitter tasting in extraoral systems and the roles that extraoral T2Rs play in processes as diverse as innate immunity, secretion, contraction, reproduction, and urination. We also summarize the association of T2R polymorphisms with various disorders and the roles of T2Rs in abnormal conditions. As this is an emerging area and our understanding is still rudimentary, we discuss the obstacles that the field is encountering and offer our perspective on how to overcome them.
T2R signaling cascades
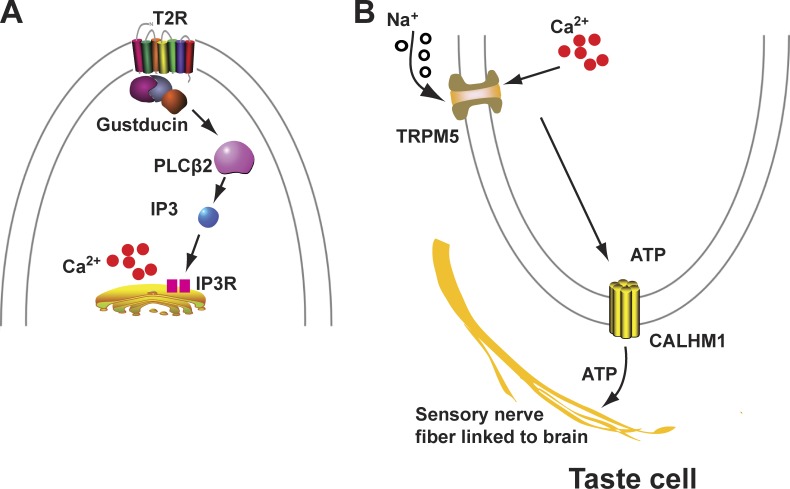
The canonical T2R signal transduction cascade shares common signaling molecules with sweet and umami receptors (i.e., T1Rs; Kautiainen, 1992; Wong et al., 1996; Huang et al., 1999; Chandrashekar et al., 2000; Mueller et al., 2005), which include heterotrimeric G protein subunits (i.e., α-gustducin [Gnat3], Gβ3, and Gγ13), a phospholipase C (PLCβ2), an inositol trisphosphate receptor (InsP3R), and a transient receptor potential cation channel (TRPM5; Fig. 1, A and B). Upon receptor activation, the G protein gustducin dissociates its α, Gnat3, and βγ subunits. The latter activates PLCβ2, leading to a release of Ca2+ from InsP3-sensitive Ca2+ stores and resulting in Na+ influx through TRPM5 channels. This Na+ influx depolarizes the cells and causes the release of neurotransmitter ATP through gap junction hemichannels or CALHM1 ion channels (Finger et al., 2005; Chaudhari and Roper, 2010; Taruno et al., 2013). Finally, released ATP activates purinergic receptors on nerves in the taste buds, and the resulting impulse is transmitted to the taste center in the central nervous system to initiate the perception of bitter taste (Taruno et al., 2013; Peng et al., 2015).
Figure 1.
The canonical T2R signaling pathway. (A) The invariant portion of T2R-mediated signaling in the tongue and extraoral cells/tissues includes bitter compounds binding (outside the cell; not depicted) with the receptors to increase intracellular calcium. (B) The remaining components of the T2R pathway in the taste bud.
In contrast, nonlingual T2Rs use at least three different mechanisms to execute biological roles tailored to their location. These three cascades have the same initial half (i.e., beginning from receptor activation to the increase in intracellular calcium concentration [[Ca2+]i]) as the canonical T2R signaling cascade (Fig. 1 A) and subsequently diverge to result in diverse functions in different cell types or tissues. These three mechanisms can be called cell-autonomous regulation, paracrine regulation, and endocrine regulation.
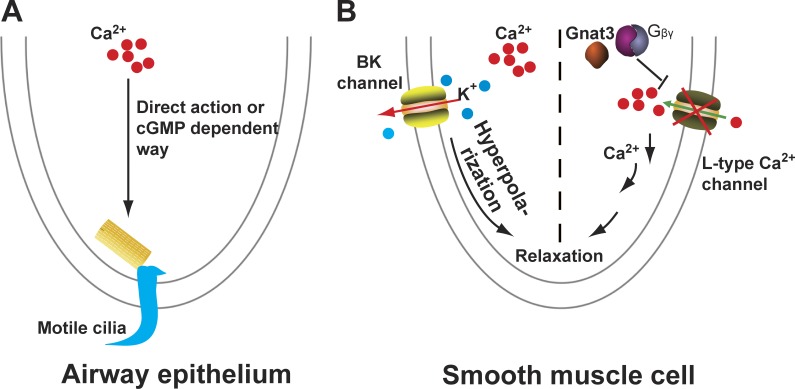
The cell autonomous regulation of T2Rs was originally found in the motile cilia of human airway epithelia (Shah et al., 2009). In this cellular location, bitter compounds elicit a dose-dependent increase in [Ca2+]i and consequently augment ciliary beat frequency (Fig. 2 A). The mechanism by which calcium influences ciliary beat frequency remains to be determined. Probably, calcium regulates the ciliary beat frequency directly or indirectly via a cyclic nucleotide-dependent manner (Salathe, 2007). Another cell-autonomous action occurs in airway smooth muscle, wherein bitter tastants dose dependently relax precontracted airways (Deshpande et al., 2010; Zhang et al., 2013). What remains debatable is how bitter tastants relax this smooth muscle. Deshpande et al. (2010) proposed that bitter tastants activate big conductance Ca2+-activated K+ (BK) channels and hyperpolarize the membrane, leading to relaxation (Fig. 2 B, left side). But by directly measuring BK channel currents, we and others found that bitter tastants do not activate these channels but instead inhibit them (Zhang et al., 2012; Wei et al., 2015). We recently discovered that the βγ subunits of gustducin are critical for bitter tastant–induced airway relaxation. These subunits can shut down L-type voltage-dependent Ca2+ channels and decrease [Ca2+]i (which is raised by bronchoconstrictors), leading to the relaxation (Fig. 2 B, right side; Zhang et al., 2013).
Figure 2.
The cell-autonomous model of the T2R signaling cascade. (A) Bitter tastants increase cilia beat frequency in airway epithelium. (B) Bitter tastants relax precontracted airway smooth muscle cells. cGMP, cyclic guanosine monophosphate.
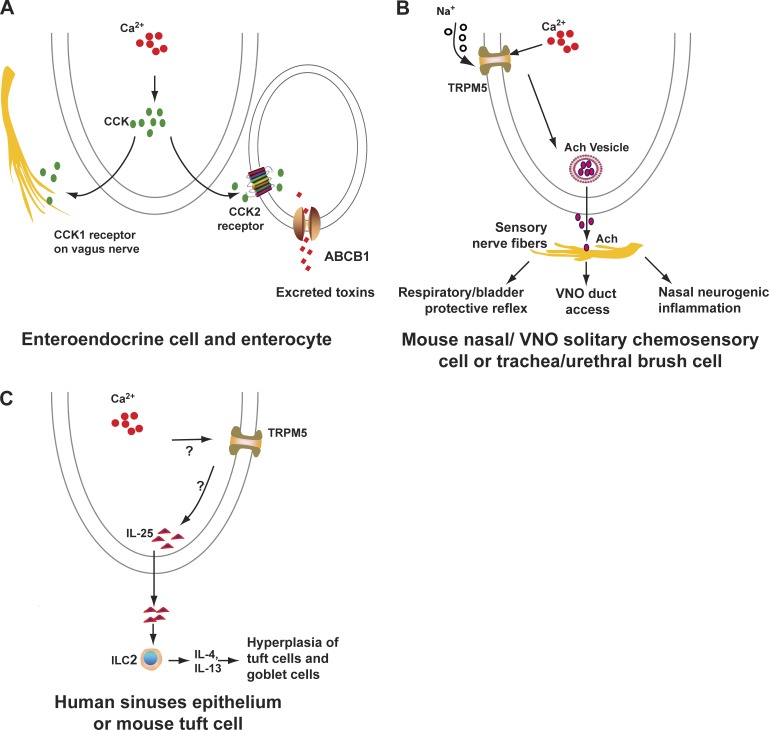
The paracrine role of T2Rs was first reported in a specialized small intestine enteroendocrine cell (EEC). Increased Ca2+ from the T2R activation leads to the release of a peptide hormone cholecystokinin (CCK), which acts either through CCK2 receptors in the neighboring enterocytes to promote multidrug resistance protein 1 (also known as ATP-binding cassette B1 [ABCB1]) to pump bitter tasting toxins out of the cells (Fig. 3 A, right side of the panel; Jeon et al., 2011) or through CCK1 receptors in sensory fibers of the vagal nerve that then transmit signals to the brain to control food intake (Fig. 3 A, left side; Cummings and Overduin, 2007). Solitary chemosensory cells (SCCs) from the nasal and vomeronasal cavity, or brush cells from the trachea in rodents, were found to release acetylcholine upon stimulation with bitter chemicals or bacterial signals. Acetylcholine then activates nicotinic acetylcholine receptors in the nearby sensory nerve fibers, which in turn decreases the breathing rate and closes the vomeronasal organ (VNO), or, alternatively, induces neurogenic inflammation in the nasal cavity (Fig. 3 B; Finger et al., 2003; Ogura et al., 2010; Tizzano et al., 2010; Krasteva et al., 2011; Saunders et al., 2014). A similar protective reflex in the bladder was also found in urethral brush cells (Fig. 3 B; Deckmann et al., 2014). Very recently, it was demonstrated that tuft cells in the gut orchestrate type 2 immunity to parasitic infection through the canonical GPCR taste receptor (T1R or T2R) cascade and also form a feedforward loop resulting in their own hyperplasia (Fig. 3 C; Gerbe et al., 2016; Howitt et al., 2016; von Moltke et al., 2016).
Figure 3.
The paracrine model of the T2R signaling cascade. (A) In the gut, dietary toxins or bitter compounds from bacteria activate T2Rs in EECs to release the peptide hormone CCK, which acts through CKK2 receptors in the neighboring enterocytes to promote ABCB1 to pump bitter-tasting toxins out of the enterocytes (right). Alternatively, CCK released by EECs can also activate CCK1 receptors on sensory fibers of the vagus nerve to send signals to the brain to limit food intake (left). (B) The paracrine model also operates in mouse SCCs from the nasal organ or VNO and in brush cells from the trachea and bladder, where bitter compounds or N-acyl homoserine lactones, bacterial quorum-sensing molecules, activate bitter-taste signaling to release Ach, which in turn activates sensory fibers to (a) initiate a protective reflex, leading to a decrease in respiratory rate or an increase in bladder contraction; (b) close the VNO duct; or (c) induce neurogenic inflammation in the nasal cavity. (C) In tuft cells from the gut, parasites activate the canonical taste cascade and release IL-25, which in turn increases the number of ILC2s and boosts the secretion of type 2 immune cytokines IL-13 and IL-4; these cytokines subsequently promote the hyperplasia of tuft cells and goblet cells.
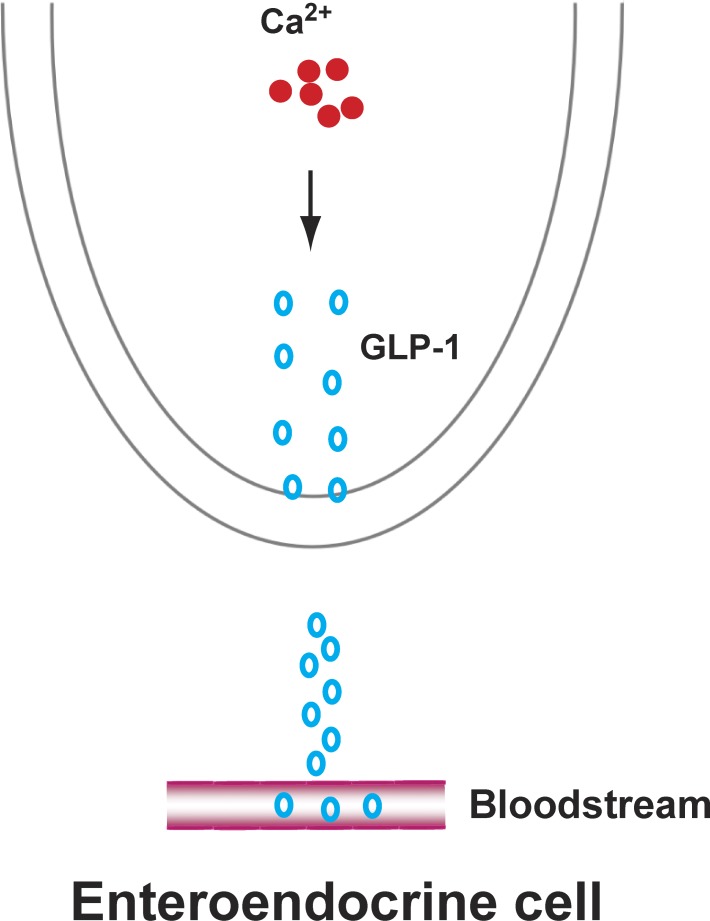
The endocrine mechanism of T2R signaling operates in tissues or cells in which T2R activation releases hormones that can be circulated via the bloodstream. Intestinal EECs release glucagonlike peptide 1 (GLP-1), which diffuses across the extracellular fluids to enter the circulation, and then stimulates the release of insulin from pancreatic β cells (Fig. 4; Dotson et al., 2008; Kim et al., 2014).
Figure 4.
The endocrine model of the T2R signaling pathway in EECs. These cells secrete GLP-1, which diffuses across the extracellular fluids to enter the circulation, and in turn stimulate the release of insulin from pancreatic β-cells.
Physiological roles of extraoral T2Rs
Shortly after the finding that gustducin is a G protein that couples with taste receptors in taste cells of the tongue (McLaughlin et al., 1992), this G protein was detected in gut cells by Höfer et al. (1996), raising the possibility that cells outside the oral cavity may use taste receptors as chemosensors. Indeed, several years later, Wu et al. (2002) and Finger et al. (2003) found T2Rs in the epithelia of the gut and nasal cavities, respectively. To date, T2Rs and their signaling components have been detected in a large number of cells and tissues located outside the mouth. Moreover, activation of these receptors produces a diverse range of biological responses under normal conditions. In this section, we summarize the physiological functions that are likely mediated by these receptors.
Innate immunity
Many mammalian organs directly contact the exterior, and such organs include, but are not limited to, those in the respiratory, gastrointestinal, reproduction, and urinary systems. Because of this external nature, these organs are readily and constantly exposed to a vast number of bacteria, fungi, and viruses, along with their derived substances. Therefore, a fundamental challenge to these organs is how to avoid infection. Intensive research has revealed that several immune mechanisms collaborate to achieve this. Of these mechanisms, innate immunity is a rapid response that is paramount for avoiding infection at the early stage. The epithelial barrier is a major component of innate immunity, which prevents microbe entry or pathogen colonization either by speeding up mucociliary clearance by increasing ciliary beat frequency or by directly producing antiorganismal compounds (Chaplin, 2010; Pastorelli et al., 2013; Shaykhiev and Crystal, 2013; Amjadi et al., 2014). Accumulating evidence suggests that T2R-mediated signaling contributes much to the innate immunity in the epithelia of the organs that are connected to the external environment.
Hitherto, most of the studies related to bitter tastants’ role in innate immunity have been focused on the respiratory system. Various T2Rs are expressed in the ciliated epithelial cells of human and rodent airways. Compared with primary cilia, which act as a sensory organelle, motile cilia function to move mucus or particles out of the airway. Human ciliated airway cells express T2R4, T2R43, and T2R46, and their activation with bitter chemicals increases [Ca2+]i and ciliary beat frequency, accelerating the clearance of microorganisms and their derived products (Shah et al., 2009). Interestingly, T2R38 is expressed in the apical membrane and cilia of human sinus epithelium, and its activation by its agonist or by microbe-derived quorum-sensing molecules (e.g., acyl-homoserine lactones [AHLs]) generates nitric oxide, a potent bactericide (Lee et al., 2012). Additionally, nitric oxide speeds up ciliary beat frequency in the human sinus epithelium through the guanylyl cyclase and protein kinase G pathway (Salathe, 2007). This phenomenon is conserved in mice, although mice do not have a T2R38 orthologue. Moreover, the response to quorum-sensing molecules depends on the canonical taste signaling components PLCβ2 and TRPM5, but not α-gustducin, based on genetic and pharmacological evidence (Lee et al., 2014a). Quorum-sensing molecules are a class of chemical signals regulating the expression of microbial genes involved in the formation of biofilm (Nealson et al., 1970; Nealson and Hastings, 1979; Eberhard et al., 1981; Davies et al., 1998; Marx, 2014). Once their concentration becomes sufficiently high, a biofilm is formed to protect the bacteria from the host immune defense system (Nealson et al., 1970; Nealson and Hastings, 1979; Eberhard et al., 1981; Davies et al., 1998; Marx, 2014). In this context, it makes sense that mammals use T2Rs as a sensory part of their rapid innate immune system to prevent bacteria from forming the biofilm.
The SCC is another type of airway epithelium cell harboring both T2Rs and most taste transduction components; it comprises 1% of cells in the surface of the respiratory system (Workman et al., 2015). Finger et al. (2003) first identified T2R-expressing SCCs in the rodent nasal cavity, which also houses many elements of the bitter taste signaling pathway, including Gα-gustducin, PLCβ2, and TRPM5 (Finger et al., 2003; Gulbransen et al., 2008; Lin et al., 2008). Bitter compounds or AHLs cause mouse nasal SCCs to release the neurotransmitter acetylcholine, which in turn stimulates neighboring peptidergic nociceptive trigeminal fibers to secrete calcitonin gene-related peptide and substance P, resulting in the initiation of a neurogenic inflammation response to block bacterial invasion (Saunders et al., 2014). Alternatively, the activated trigeminal fibers can mediate a protective reflex to depress the respiratory rate, thus avoiding further inhalation of irritating substances or microbes (Fig. 3 B; Finger et al., 2003; Tizzano et al., 2010; Krasteva et al., 2011). Recently, choline acetyltransferase enhanced green fluorescent protein (eGFP)–positive (ChAT-eGFP+) SCCs in the mouse VNO were shown to regulate VNO duct accessibility (Ogura et al., 2010). In the mouse trachea, ChAT-eGFP+ chemosensory cells (called brush cells) can regulate the breathing rate by sensing the local chemical composition; this uses a mechanism similar to that used by nasal SCCs, mentioned above (Fig. 3 B; Finger et al., 2003; Tizzano et al., 2010; Krasteva et al., 2011, 2012a). More recently, a similar brush cell response (i.e., acetylcholine release) has also been demonstrated in the mouse urethral system (Deckmann et al., 2014). In this system, hazardous bitter compounds bind with T2Rs in the brush cells, releasing acetylcholine, which then activates nearby urethral sensory nerve fibers and stimulates detrusor muscle contraction (Fig. 3 B; Deckmann et al., 2014). Further investigation of microorganism-derived materials is necessary to determine whether such a reflex also occurs when microbes access the urethra.
In human sinonasal epithelia, SCCs express a set of denatonium-responsive T2Rs that are absent in T2R38-expressing sinonasal ciliated cells and underlie a role distinct from the T2R38-mediated nitric oxide response observed in the ciliated epithelial cells (see above; Lee et al., 2012, 2014a). Activation of these T2Rs in SCCs propagates a calcium wave to the surrounding cells through gap junctions, causing a robust secretion of broad-spectrum antimicrobial peptides and β-defensin. However, they exert no effect on ciliary beat frequency. Interestingly, these SCCs also express T1R2/3 sweet taste receptors, which negatively regulate the T2R response. In healthy individuals, sweet taste receptors activated by airway surface liquid glucose (∼0.5 mM) suppress T2R-mediated antimicrobial peptide secretion. However, during microbial infection, T1R2/3 is deactivated as the interior bacteria reduce the glucose concentration by consuming it, consequently increasing T2R-mediated antimicrobial peptide release (Lee and Cohen, 2014; Lee et al., 2014b). Therefore, the two different defense systems mediated by ciliated epithelial T2Rs and SCC T2Rs work in concert to maintain human lower airway health.
The mammalian gut is colonized by microbiota, which comprises a collection of bacteria, archaea, viruses, fungi, and parasites (Sommer and Bäckhed, 2013). The single layer of gut epithelial cells orchestrates many ways to surveil the microbes (Peterson and Artis, 2014). Although the first extraoral cells found to express α-gustducin were tuft cells (also called brush cells) within the rat gastrointestinal tract (Höfer et al., 1996), the finding of T2Rs in gut epithelium took place several years later (Wu et al., 2002), and it was not until earlier this year that three different groups (Gerbe et al., 2016; Howitt et al., 2016; von Moltke et al., 2016) demonstrated that tuft cells harness taste transduction signaling to initiate type 2 immunity against pathogens often copresent with symbiotic microbes. In detail, tuft cells sense the parasite infection via canonical taste signaling and secrete IL-25, which increases the number of innate lymphoid cells (ILC2s) and their production of type 2 immune cytokines IL-4 and IL-13. Subsequently, these cytokines promote hyperplasia of tuft cells and goblet cells by facilitating intestinal stem cell differentiation (Fig. 3 C). However, which T2Rs or whether other taste receptors are involved in this process remains to be determined. It is reasonable to speculate that a mechanism similar to that which has been revealed in the SCCs or brush cells in the airway may be used to monitor microbiota in the gut.
Secretion
Endocrine, paracrine, and autocrine secretions are essential for maintaining body homeostasis. The gut is the largest endocrine organ and the source of gut hormones (Ahlman and Nilsson, 2001). Besides working as an innate defense barrier, intestinal epithelial cells house different subsets of cells that release hormones.
EECs, scattered along the epithelial layer of the GI tract from the stomach to the rectum, respond to an ingested meal by secreting a variety of gut hormones, including CCK, GLP-1, glucose-dependent insulinotropic peptide, peptide YY, somatostatin, ghrelin, and serotonin. These hormones perform functions ranging from modulating food intake to regulating insulin release (Psichas et al., 2015; Gribble and Reimann, 2016). The secretion from EECs is mainly triggered by the sensing of luminal contents via GPCRs, including the T2R family (Psichas et al., 2015). It is known that denatonium stimulates the mouse EEC cell line STC-1 to release CCK dose dependently, as does phenylthiocarbamide for GLP-1 (Wu et al., 2002; Chen et al., 2006). The extract of Hoodia gordonii activates T2R14 to secrete CCK in the human EEC line HuTu-80 (Le Nevé et al., 2010). Bitter tastants or extracts from bitter herbs cause GLP-1 secretion in the human EEC line NCI-H716 (Jang et al., 2007; Dotson et al., 2008; Suh et al., 2015).
In vivo studies also indicate that EECs have the capability to secrete hormones to regulate plasma glucose or the ingestion of toxic substances. Intragastric administration of bitter chemicals leads to a rise in the plasma ghrelin level, resulting in a short-term increase in food intake. This effect is subsequently followed by a long-term decrease in food intake caused by a delay in gastric emptying (Janssen et al., 2011). A gavage of denatonium followed by glucose or oral administration of herb extracts to db/db mice induces GLP-1 and subsequent insulin secretion, ultimately leading to a decrease in the blood glucose level (Kim et al., 2014; Suh et al., 2015). Nevertheless, in vivo direct evidence is needed to demonstrate that the glucose drop is exclusively caused by EECs because no immunostaining evidence exists depicting a colocalization between EEC markers and T2Rs, although α-gustducin and TRPM5 have both been detected in serotonin and GLP-1–producing ECCs.
In addition to EECs, SCCs in the gut also contain taste signaling elements. In the mouse stomach, α-gustducin–harboring SCCs locate in close proximity to the ghrelin and serotonin-releasing EECs. This has led to a hypothesis that SCCs perform a chemosensory role by forwarding messages from the lumen onto the EECs, which then secrete hormones (Hass et al., 2007). This seems possible, as denatonium causes an increase in Ca2+ in TRPM5-expressing SCCs, followed by a delayed Ca2+ response in the adjacent epithelium (Bezençon et al., 2008). However, T2R proteins have yet to be detected in gastrointestinal SCCs, although various T2R transcripts have been found in the epithelia of humans and rodents.
T2Rs also play secretion roles in the lower gastrointestinal tract. T2R108 ligand 6-n-propyl-2-thiouracil (6-PTU) induces anion secretion in the human and rat large intestine, and this action is considered to be a protective response meant to flush out noxious irritants (Kaji et al., 2009). Hence, one function of T2Rs in the gastrointestinal epithelial cells is to limit the influence of toxic compounds by preventing their further intake or accelerating their excretion.
Several T2Rs are expressed in human and mouse thyrocytes and in human thyrocyte line Nthy-Ori3-1. These T2Rs negatively regulate thyroid-stimulating hormone-dependent iodide efflux in thyrocytes and thereby decrease the secretion of thyroid hormone. This might mediate a protective response to the ingestion of toxic compounds (Clark et al., 2015). Beyond these secretion roles in the gastrointestinal tract and thyroid, T2Rs in respiratory epithelium cells mediate the secretion of nitric oxide, neurotransmitters, and antimicrobial peptides (Krasteva et al., 2011; Lee et al., 2012, 2014b).
Contraction and relaxation
T2Rs in smooth muscles have attracted a lot of attention ever since Deshpande et al. (2010) reported that T2R agonists cause the relaxation of precontracted airway smooth muscle ex vivo and decrease airway resistance in vivo in mice. This relaxation is paradoxical, as bitter tastants can increase [Ca2+]i (to the level induced by bronchoconstrictors) in human cultured airway smooth muscle cells (Deshpande et al., 2010) or to a more modest level in freshly isolated relaxed mouse airway smooth muscle cells (Zhang et al., 2013). This paradox has stimulated a wave of research into the underlying relaxation mechanisms. Results have been controversial. In addition to the two mechanisms described in the T2R signaling transductions section (Fig. 2 B), several other possibilities have been proposed for bitter tastants–induced relaxation of airway smooth muscle. Grassin-Delyle et al. (2013) suggested the involvement of the phosphatidylinositol-3 kinase (PI3K) pathway based on studies using intact human bronchi. Tan and Sanderson (2014) determined that bitter tastants directly inhibit InsP3R-mediated Ca2+ oscillations to relax airways. Tazzeo et al. (2012) proposed that bitter tastants (such as caffeine) may act downstream of myosin light chain kinase to interfere with the contractile apparatus, causing airway smooth muscle relaxation.
Although the cellular mechanisms are still debatable, a consensus is that bitter tastants are potentially potent bronchodilators, as they produce airway relaxation and protect against airway constriction in vivo better than some of the currently used asthma medicines. To date, a variety of bitter compounds have been found to relax precontracted airway smooth muscle from humans, mice, and guinea pigs (Deshpande et al., 2010; Pulkkinen et al., 2012; Zhang et al., 2013; Tan and Sanderson, 2014; Camoretti-Mercado et al., 2015). An attractive feature of using bitter tastants as bronchodilators is that these compounds can produce relaxation in airways precontracted by a broad spectrum of agonists (although there are some efficacy differences; Pulkkinen et al., 2012; Camoretti-Mercado et al., 2015). For example, in guinea pig trachea, denatonium selectively inhibits contractions induced by carbachol, whereas chloroquine uniformly inhibits contractions evoked by prostaglandin E(2), thromboxane receptor agonist U-46619, leukotriene D(4), histamine, and antigen (Pulkkinen et al., 2012); in human airways, chloroquine inhibits [Ca2+]i elevation and contractile responses normally induced by histamine, but not those induced by endothelin-1. Conversely, aristolochic acid prevents contractile responses induced by endothelin-1, but not those induced by histamine (Camoretti-Mercado et al., 2015). This necessitates studying how each bitter compound performs against different bronchoconstrictors to appropriately assess its effectiveness as a bronchodilator.
Several studies have demonstrated the roles of bitter compounds in regulating vascular smooth muscle contractility. Manson et al. (2014) reported that bitter ligands for human T2R3, 4, 10, and 14 induce relaxation of precontracted human pulmonary arteries, guinea pig aorta, and mouse aorta. This relaxation is independent of the inhibition of L-type Ca2+ channels or activation of BK channels but is dependent on the formation of caveolae (Manson et al., 2014). Lund et al. (2013) revealed that hT2R46 is expressed in human aorta vascular smooth muscle cells, and intravenous injection of denatonium via catheter in rats leads to a transient drop in blood pressure. Interestingly, Upadhyaya et al. (2014) reported that dextromethorphan induces a vasoconstriction via a T2R1-mediated Ca2+ response in human pulmonary artery smooth muscle. The authors proposed that the calcium increase from the canonical T2R signaling pathway directly activates myosin light chain kinase and subsequently increases the phosphorylated myosin light chain, leading to constriction (Upadhyaya et al., 2014).
T2Rs and taste signaling elements are also present in mouse and human gastrointestinal smooth muscle cells. Bitter tastants induce a contraction when applied at lower concentrations (e.g., <100 µM for denatonium) and a relaxation at higher concentrations (e.g., >500 µM for denatonium). Intragastric administration of denatonium leads to a T2R-dependent delay in gastric emptying. Moreover, after intragastric denatonium administration, healthy volunteers showed an impaired fundic relaxation in response to nutrient infusion and a decreased nutrient volume tolerance and increased satiation during an oral nutrient challenge test (Avau et al., 2015). As the role of T2Rs in the gastrointestinal epithelia cannot be ruled out in these in vivo experiments, these results might be influenced by both epithelia and smooth muscle in the gastrointestinal tract. Undoubtedly, the protective role of T2Rs makes them valuable targets for drug development to treat gastrointestinal motility diseases.
Foster et al. (2013) reported that cardiac myocytes express five T2Rs and their downstream signaling elements. Using a heterologous expression system, Foster et al. (2014a) de-orphaned three of the five T2Rs expressed in these cells. In their function study, the authors found that sodium thiocyanate, a T2R108 agonist, elicited a 30–40% decrease in left ventricular pressure and systolic pressure, as well as a steady increase in aortic pressure, whereas sodium benzoate, a T2R137 agonist, and sodium arbutin, a T2R143 agonist, displayed a minor or modest effect, respectively, on these cardiac functions (Orsmark-Pietras et al., 2013; Foster et al., 2014a). Moreover, these effects are abrogated by Gi and Gβγ inhibitors (e.g., pertussis toxin and gallein). Therefore, T2R signaling may play an important role in regulating cardiac functions.
Reproduction and urination
T2Rs in the genitourinary system has been another area of attention. T2Rs and taste transduction cascade components (α-gustducin, Gγ13, and PLCCβ2) have been detected in different stages of spermatogenesis (with TRPM5 being observed only in the later spermatid phase; Li and Zhou, 2012). Bitter chemicals induce a rise in [Ca2+]i in spermatids, and individual spermatids exhibit different ligand activation profiles, indicating a unique T2R profile in each spermatid (Xu et al., 2013). Moreover, depletion of T2R105 results in smaller testes and is sufficient to lead to male infertility (Li and Zhou, 2012). These results suggest a crucial role for T2R receptors in spermatogenesis and a possible function in sensing and avoiding noxious chemicals that are present during fertilization.
In the female reproductive system, human T2R38 is expressed in the amniotic epithelium, syncytiotrophoblast, and decidua cells in human placenta, and in a placental cell line (JEG-3; Wölfle et al., 2016). Although the T2R38 agonist diphenidol evokes calcium influx in the placental cell line, there is no further functional characterization of T2R38 in placenta (Wölfle et al., 2016).
Seven T2Rs and α-gustducin are expressed in mouse whole kidney (Rajkumar et al., 2014; Liu et al., 2015). Conditional ablation of T2R105-positive cells causes an increase in the size of the glomerulus and renal tubule, accompanied by a lower cell density in the glomerulus (Liu et al., 2015). These results suggest an essential role of T2R105 in maintaining the structure and consequent homeostasis in bodily fluids and electrolytes (Liu et al., 2015).
As mentioned previously, activation of T2Rs in urethral chemosensory cells initiates a reflex loop, leading to bladder contraction (Deckmann et al., 2014). In this context, it is interesting that Zhai et al. (2016) showed that human and mouse detrusor smooth muscle express T2Rs, and T2R agonists can directly relax precontracted detrusor muscle strips. In vivo study showed that oral gavage of the bitter compound chloroquine suppresses overactive bladder symptoms in mice that possess partial bladder outlet obstruction. Thus, T2Rs are potential targets for treating this disorder.
Therefore, T2Rs appear to have a versatile modulatory role in reproduction and urination; however, unlike in other systems, their roles remain largely to be determined.
Other roles
Many T2R transcripts have been detected in polymorphonuclear neutrophils. Knockdown of highly abundant T2R43 or T2R31 in these cells remarkably blocks the chemotactic trans-migration induced by saccharin (Malki et al., 2015). Another study showed that human neutrophils express T2R38, and its binding with quorum-sensing molecules (N-(3-oxododecanoyl)-l-homoserinelactone or AHL-12) induces migration of neutrophils (Maurer et al., 2015). Additionally, a recent investigation showed that phagocytes also express T2R38, which can be activated by AHL-12 (Gaida et al., 2016a). These results suggest that bitter tastants function within the immune system by binding to food-borne substances that enter the bloodstream after ingestion, molecules produced by bacterial infections, or harmful endogenous metabolites.
Several investigations have demonstrated the existence of T2Rs in the different compartments of the central nervous system, such as the brain stem, brain cells, parabrachial nucleus, and horoid plexus (Singh et al., 2011; Dehkordi et al., 2012; Tomás et al., 2016). Although some bitter chemicals have the capability to cross the brain–blood barrier, it remains to be determined whether their concentrations could reach the high micromolar level that is needed to activate many T2Rs. It would be interesting to find out whether, within the central nervous system, there are endogenous bitter-tasting compounds that can be highly effectively at activating T2Rs. If so, T2Rs in the central nervous system could serve as sensors for these ligands.
T2Rs have also been detected in several other tissues or organs. Several T2Rs have been detected in human skin biopsies and in the immortal keratinocyte cell line; bitter compounds (diphenidol and amarogentin) induce the expression of differentiation markers in human skin primary cells (Wölfle et al., 2015). T2Rs and taste transduction pathway components are expressed in the ChAT-eGFP+ brush cells in the murine auditory tube, submucosal glands of the larynx and trachea, and the thymic medulla, and they may function as sensors for the composition of the local microenvironment, as has been demonstrated for SCCs and brush cells in the airway (Krasteva et al., 2012b; Panneck et al., 2014; Krasteva-Christ et al., 2015). However, direct experiments are needed to confirm this.
Potential roles of extraoral T2Rs in disease
Several studies have begun to reveal that T2R mutants can cause or contribute to diseases in the extraoral tissues, highlighting the important roles that these receptors play under pathophysiological conditions. T2R genes do not contain introns in their protein-coding regions, and their expression levels are usually low under normal conditions. These characteristics may lead to changes in their expression level under different pathological conditions. In this section, we summarize both T2R mutations and/or changes in T2R expression level that occur in various diseases and disorders. The major T2Rs and their associated disorders and diseases are listed in Table 1.
Table 1. T2R-associated disorders and diseases.
| T2R type | Affected system | Effects | Reference |
|---|---|---|---|
| T2R38 | Human upper respiratory system | T2R38 genotype is correlated with susceptibility, severity, and prognosis of chronic rhinosinusitis, as well as biofilm formation in chronic rhinosinusitis patients | Lee et al., 2012; Lee and Cohen, 2013; Adappa et al., 2014, 2016a,b,c |
| Human colorectal cancer | T2R38 nonfunctional group has an increased risk of colorectal cancer in a population of Caucasian origin | Carrai et al., 2011 | |
| Human gingiva | T2R38 genotype is associated with gingival innate immunity and the risk of dental caries | Wendell et al., 2010; Gil et al., 2015 | |
| Human colonic mucosa | Increased number of T2R38 immunoreactive cells in overweight and obese subjects | Latorre et al., 2016 | |
| T2R19 | Blood glucose | T2R19 haplotype is associated with altered glucose and insulin homeostasis | Dotson et al., 2008 |
| T2R50 | Human heart | T2R50 SNPs (ID rs1376251) have a strong association with cardiovascular disease | Shiffman et al., 2008 |
| T2R42 | Thyroid | Thyroid-expressed T2R42 SNP (SNP type L196F) is associated with differences in circulating levels of thyroid hormones | Clark et al., 2015 |
| T2R16 | Longevity | An upstream position polymorphism of T2R16 is significantly associated with longevity | Campa et al., 2012 |
| T2Rs | Human leukocytes | 10 T2Rs are up-regulated in leukocytes in severe asthma patients | Orsmark-Pietras et al., 2013 |
| T2Rs | Human Parkinson’s disease patients’ brains | T2R5 and T2R50 are decreased, whereas T2R10 and T2R13 are augmented at both premotor and parkinsonian stages in the frontal cortex area | Garcia-Esparcia et al., 2013 |
| Human schizophrenia patients’ brains | T2R4, T2R5, T2R14, and T2R50 are down-regulated in the dorsolateral prefrontal cortex | Ansoleaga et al., 2015 | |
| T2R4 | Human breast cancer | T2R4 is down-regulated in breast cancer cells | Singh et al., 2014 |
| T2R105 | Mouse testes | Depletion of T2R105 results in smaller testes and leads to male infertility | Li and Zhou, 2012 |
| Mouse glomerulus and renal tubule | Ablation of T2R105-positive cells causes an increase in the size of the glomerulus and renal tubule and a lower cell density in the glomerulus | Liu et al., 2015 | |
| T2R126, T2R135, and T2R143 | Mouse heart | Starvation increases the expression of these T2Rs by two- to threefold | Foster et al., 2013 |
T2R polymorphisms
T2R polymorphisms dictate taste preference and extraoral T2R-mediated pathophysiology. Several excellent studies and reviews have summarized changes in bitter taste caused by T2R genetic variants and polymorphisms (Kim et al., 2003; Bufe et al., 2005; Li et al., 2011; Campa et al., 2012; Keller et al., 2013; Risso et al., 2014). In this section, we focus on the alteration in extraoral function attributed to T2R polymorphisms. Of all T2R family members, T2R38 polymorphism is the most extensively investigated one. The T2R38 protein has two common variants that differ in the amino acid residues at positions 49, 262, and 296. The functional variant contains proline, alanine, and valine, respectively, in these positions, so the genotype is designated as PAV, whereas the nonfunctional form contains alanine, valine, and isoleucine to give rise to the AVI genotype. Therefore, the combination of these two variants generates three common genotypes, i.e., two homozygotes, PAV/PAV and AVI/AVI, and one heterozygote, PAV/AVI. Most of the work on the relationship between T2R38 polymorphisms and respiratory disease has been published by Cohen and his colleagues. These authors showed that the functional T2R38 PAV/PAV phenotype has a much lower infection rate from gram-negative bacteria than the other two genotypes (Lee and Cohen, 2013). The same group further showed that nonfunctional T2R38 genotypes (AVI/AVI and AVI/PAV) are present in >90% of the chronic rhinosinusitis population undergoing functional endoscopic sinus surgery (Adappa et al., 2014). They also found that homozygous ΔF508 cystic fibrosis patients with nonfunctional alleles exhibit more severe sinonasal symptoms (Adappa et al., 2016b). Finally, they determined that individuals with T2R38 functional homozygotes have more than a threefold improvement in surgical outcomes when compared with chronic rhinosinusitis patients possessing nonfunctional homozygotes or heterozygotes (Adappa et al., 2016a). Most recently, they found that among 59 chronic rhinosinusitis patients, an inverse linear association exists between in vitro biofilm formation and phenylthiocarbamide taste intensity ratings (P = 0.019; Adappa et al., 2016c). All of these results indicate that the T2R38 genotype is correlated with susceptibility, severity, and prognosis in upper respiratory disorders. However, a recent study on an Italian population showed that there is no association between T2R38 alleles and chronic rhinosinusitis (Gallo et al., 2016). To firmly establish the role of T2R38 in chronic rhinosinusitis pathogenesis, studies with larger cohorts may be needed.
T2R38 polymorphism also relates to other diseases, such as cancer and cavities. Carrai et al. (2011) demonstrated that the nonfunctional group has an increased risk of colorectal cancer in comparison to the functional group in a population of Caucasian origin. In their study of the effect of T2R38 polymorphism on oral innate immunity, Gil et al. (2015) found a complicated set of responses when teeth were exposed to different pathogenic bacteria. In response to the cariogenic bacteria Streptococcus mutans, the transcription level of T2R38 in gingival epithelial cells was increased 4.3-fold in individuals with the PAV/PAV genotype, in contrast to a 1.2-fold increase in AVI/AVI individuals. IL-1α secretion in the PAV/PAV genotype was highest among all three genotypes, whereas the secretion of hBD-2 (antimicrobial peptide) and IL-1α in this genotype was decreased by 77% and 50%, respectively, after application of T2R38-specific small interfering RNA. When stimulated with the periodonatal pathogen Porphyromonas gingivalis, only the AVI/AVI T2R38 transcription levels increased by 4.4-fold. In addition, the levels of IL-1α and IL-8 were remarkably decreased when T2R38 was silenced (Gil et al., 2015). All these data suggest a genotype-dependent role of T2R38 in gingival innate immunity and a T2R38-associated risk of dental caries (Wendell et al., 2010) that may be more important than dietary habits.
Several other T2R polymorphisms are also correlated with various disorders as revealed by association studies. Dotson et al. (2008) found that the T2R19 haplotype is associated with altered glucose and insulin homeostasis. In a study involving 4,522 individuals aged 65 or above, Shiffman et al. (2008) reported that several human T2R50 single-nucleotide polymorphisms (SNPs; ID rs1376251) have strong associations with cardiovascular disease. Given that T2R50 is expressed in the heart (Foster et al., 2013), these SNPs may play a direct role in causing cardiovascular disease, rather than being involved in this disease indirectly via changes in food preference and diet, as proposed by Shiffman et al. (2008). Interestingly, another study indicated that the same SNPs of T2R50 could be useful in predicting statin-induced cardiovascular risk reduction in elderly women, but not in men (Akao et al., 2012); however, this sex difference disappeared when corrected for multiple comparisons (Akao et al., 2012). Thyroid-expressed T2R42 SNP (SNP type L196F) is associated with differences in circulating levels of thyroid hormones (Clark et al., 2015). Polymorphism of the position 212 bp upstream of human T2R16 is significantly associated with longevity—the frequency of A/A homozygotes is increased in older people. This site is most likely located in the promoter region for T2R16, suggesting a critical regulation role (Campa et al., 2012). Along with the important extraoral T2R functions, more T2R polymorphisms and their association with human health are expected to be discovered.
T2Rs in disorders and diseases
As airway smooth muscles express T2Rs and bitter compounds can profoundly relax constriction and decrease airway resistance in animal models of asthma, two questions immediately emerge: are T2R expression levels changed in asthmatic patients and are T2Rs desensitized in asthmatics, as are other GPCRs? Robinett et al. (2014) demonstrated that the mRNA expression levels of T2R10, 14, and 31 are not different between asthmatics and nonasthma controls, and T2R agonists relax airways from healthy and asthmatic specimens equally. As to the T2R desensitization, the same group found that pretreatment of human airway smooth muscle cells with a prototypical T2R agonist, quinine, results in ∼30% desensitization in both [Ca2+]i response and airway relaxation (Robinett et al., 2011). However, there is no cross-desensitization between T2R and β2 adrenergic receptor–mediated relaxation (An et al., 2012), indicating that both therapies could be combined to treat asthma. In addition, several T2Rs are up-regulated in leukocytes in severe asthma patients, and T2R agonists can inhibit the release of proinflammatory cytokines and eicosanoid release from blood leukocytes (Orsmark-Pietras et al., 2013). These findings suggest that T2R agonists may directly act on immune cells to perform their antiinflammatory role. All these findings underscore the potential of T2Rs as attractive targets for asthma management.
Although the pathophysiological roles of T2Rs have traditionally focused on the respiratory tract, their roles in other systems have begun to emerge. Low-fat diet or sterol depletion culture leads to an increase in the expression of most T2Rs in the mouse proximal intestine or the STC-1 cell line (a type of gut ECC), which may in turn stimulate the secretion of GLP-1 and CCK (Jeon et al., 2008). In human colonic mucosa, the number of T2R38 immunoreactive cells is significantly increased in overweight and obese subjects versus lean subjects and is also significantly correlated with body mass index values (Latorre et al., 2016). In the heart, the expression of T2R126, T2R135, and T2R143 is increased two- to threefold under starvation conditions both in vitro and in vivo (Foster et al., 2013). Subcutaneous administration of nitroglycerin (a myocardial antiischemic chemical) dramatically increases the T2R119 expression in heart and aorta (Csont et al., 2015). In the brains of Parkinson’s disease patients, T2R5 and T2R50 are decreased, whereas T2R10 and T2R13 are augmented at both premotor and parkinsonian stages in the frontal cortex area (Garcia-Esparcia et al., 2013). Interestingly, T2R4, T2R5, T2R14, and T2R50 are down-regulated in the dorsolateral prefrontal cortex of schizophrenia patients (Ansoleaga et al., 2015). As the heart is not directly exposed to the external environment and the brain is further isolated by the blood–brain barrier, the changes in T2Rs in these systems raise the possibility that endogenous ligands for T2Rs exist throughout the human body.
T2R expression has also been detected in tumor or cancer cells. Singh et al. (2014) found that the expression of T2R4 is down-regulated in breast cancer cells compared with noncancerous mammary epithelial cells, suggesting a mechanism by which the breast cancer cells may escape from apoptosis, which would otherwise be induced by bitter compounds. In a study of pancreatic cancer, Gaida et al. (2016a) found that T2R38 is expressed in both tumor cells from pancreatic cancer patients and tumor-derived cell lines. Moreover, the T2R38-specific ligand phenylthiourea or natural ligand AHL-12 activate mitogen-activated protein kinases p38 and ERK1/2 and up-regulate NFATc1 in a G protein–dependent manner. Intriguingly, although there is no correlation between the frequency of T2R38-positive tumor cells and clinical and pathological parameters, the T2R38 ligands increase the expression of efflux transporter ABCB1, suggesting the possible engagement of T2R38 in the chemoresistance of pancreatic cancer (Gaida et al., 2016b).
Future perspectives
Recent advances have discovered the widespread extent of extraoral T2Rs unearthed the important roles these receptors play in a variety of cellular functions, and have shown that their pathologies may potentially contribute to several disease conditions. At the same time, studies have raised many important questions about these receptors and have uncovered several challenges that need to be overcome to further deepen our understanding of extraoral T2R biology.
Profiling T2R expression
Owing to the lack of well-documented antibodies for T2Rs (in particular for mouse T2Rs), the expression profiling of T2Rs in the extraoral tissues has been largely generated using in situ hybridization with antisense probes to T2Rs (Foster et al., 2013; Prandi et al., 2013) or quantitative real-time PCR or reverse transcript PCR with a template (but without transcriptase as a control to confirm no genome DNA contamination; Shah et al., 2009; Deshpande et al., 2010; Foster et al., 2013; Xu et al., 2013; Zhang et al., 2013; Deckmann et al., 2014). As to the first method, not every laboratory can satisfy its technical requirements. With regard to the latter two, the ways to eliminate genome DNA involve purification of mRNA with poly(T)-tag (Raz et al., 2011), digestion by DNase (Raz et al., 2011), or filtering by a genome-specific binding column. Most studies use DNA digestion or a DNA-binding column, even though the current commonly used DNases or filters cannot completely remove genome contamination. This shortcoming could result in trace contamination with genome DNA in the samples; additionally, it casts doubts on the T2R expression profile because T2R genes are intronless (Cui et al., 2007) and the expression level of T2Rs in extraoral tissues is very low, therefore requiring a large number of PCR cycles for quantification (Clark et al., 2012). Interestingly, the DNase for eliminating genome DNA in RNA sequencing can yield higher-quality RNA preparations. Utilization of this DNase for T2R expression could generate more reliable results. However, generating specific antibodies against T2Rs to visualize these receptors in cells and tissues could provide a more accurate estimate of T2R expression levels and their cellular location. This in turn could provide insight into the potential roles of T2Rs in different cells and tissues.
De-orphaning nonhuman T2Rs
Although most human T2Rs are de-orphaned, the majority of T2Rs in other species are orphan receptors (Meyerhof et al., 2010; Ji et al., 2014). Identification of agonists and antagonists for T2Rs would facilitate the study of the physiological roles of T2Rs. One method to determine ligands of T2Rs is to isolate cells that express known T2R(s) and their signaling components and stimulate them with different bitter compounds. Gulbransen et al. (2008) was the first to use this approach to demonstrate that the bitter compound denatonium could activate T2R108 in the SCCs; this was determined by examining the Ca2+ response in either Trmp5-GFP+ or gustducin-GFP+ isolated nasal SCCs (Chandrashekar et al., 2000; Finger et al., 2003). This approach is applicable to cells that express only one or a few T2Rs, and it would be less useful for cell types that express multiple T2Rs. A more general approach to de-orphaning T2Rs is to engineer a T2R signaling system in heterologous expression cells, often HEK293 cells. For human T2R expression, T2Rs fused with cell membrane–targeting peptides coexpress with a chimeric Gα16–gust44 and, in some cases, transport protein 3 (RTP3) or RTP4 to enhance the transport of T2Rs to the cell membrane (Ueda et al., 2003; Behrens et al., 2006; Deshpande et al., 2010; Ji et al., 2014). Ilegems et al. (2010) also demonstrated that receptor expression enhanced protein 2 boosts the responsiveness of human T2R16 and T2R44 to their ligands. It would be interesting to determine whether a similar expression strategy would work for T2Rs from other species.
Receptor antagonists can help dissect receptor function. To date, a handful of T2R antagonists from different sources (primarily from plants) have been found. Similar to T2R agonists (Meyerhof et al., 2010; Levit et al., 2014), T2R antagonists may interact with one T2R or multiple T2Rs. Likewise, a single T2R might be inactivated by more than one antagonist. Probenecid, an Food and Drug Administration–approved inhibitor of the multidrug resistance protein 1 transporter and used to treat gout in clinics, inhibits human T2R16, T2R38, and T2R43, but not T2R31 (Greene et al., 2011) and has been successfully applied to probe T2R’s physiological roles (Pydi et al., 2015). GIV3727, an inhibitor of the human sweet taste receptor, inhibits T2R31 and T2R43 (Slack et al., 2010). Sakuranetin, 6-methoxysakuranetin, and jaceosidin, isolated from the leaves of the native North American plant Eriodictyon californicum, are T2R31 antagonists. Derived from edible plants, 3β-hydroxypelenolide or 3β-hydroxydihydrocostunolide can inhibit several T2Rs with different sensitivity (Brockhoff et al., 2011). Pydi et al. (2014, 2015) identified two amino acid derivatives, γ-aminobutryic acid and Nα, Nα-Bis(carboxymethyl)-l-lysine, and a plant hormone abscisic acid as competitive inhibitors of quinine-activated T2R4. Recently, three flavones (i.e., 4′-fluoro-6-methoxyflavanone, 6,3′-dimethoxyflavanone, and 6-methoxyflavanone) have been demonstrated to inhibit T2R39, and 6-methoxyflavanone also inhibits T2R14 (Roland et al., 2014). These antagonists should be useful to probe the physiological roles of human T2Rs expressed in different extraoral cells and tissues. But the number of known antagonists and the number of T2Rs they act on are very limited; further exploration is needed.
Analyzing extraoral T2R functions genetically
Besides the expression profiling of T2Rs, the roles of T2Rs in extraoral tissues in humans have been studied by using T2R agonists and antagonists and the inhibitors of T2R signaling components. These approaches have been applied to mice, although occasionally genetic deletion of T2R signaling components such as α-gustducin (Janssen et al., 2011; Lee et al., 2014a; Avau et al., 2015) and TRMP5 (Lee et al., 2014a; Saunders et al., 2014) have been used. To dissect the roles of T2Rs, a desirable approach is to genetically ablate these receptors. So far, only T2R105 (Li and Zhou, 2012; Rajkumar et al., 2014) and T2R131 (Voigt et al., 2012, 2015; Prandi et al., 2013; Soultanova et al., 2015) have been studied genetically to some extent. A potential challenge when probing T2R function with genetic approaches is that T2Rs may be redundant (as many T2R agonists activate multiple T2R receptors); therefore, deletion of a single T2R may have little effect. However, the fact that a cell type or tissue may express only a small subset of T2Rs, e.g., five in rodent heart (Foster et al., 2013), offers opportunities to knock out the entire subset of T2Rs using newly developed, highly efficient genomic editing methods such as CRISPR/Cas9 technology. Most T2Rs locate in genomes in just a few clusters, making it easier to knock out all the T2Rs in mice or other species with this technology after a few cycles of cross-breeding (Wang et al., 2013; Foster et al., 2014b). It is expected that these T2R transgenic knockout mice will greatly facilitate our understanding of the physiological roles of T2Rs in the extraoral systems.
Identifying physiological ligands for T2Rs
Canonically, T2Rs are known to detect bitter tastants in the diet. With recent advances in understanding the role of oral microbiota (Avila et al., 2009; Dewhirst et al., 2010), it is reasonable to speculate that T2Rs may also sense symbiotic microorganisms and their derivatives in the oral cavity. The same idea could be also applied to the T2Rs in the organs, which directly contact external environments. In other words, T2Rs in gastroenterological and respiratory systems could function as sensors of bitter tastants that are injected or inhaled, and also of microorganisms and their derivatives. However, because the threshold for T2R activation is high, generally in the micromolar range, it is not clear what would be the primary or physiological ligands for T2Rs in the systems that do not directly interact with the external environment. One possibility is that certain bitter-tasting endogenous bioactive compounds that circulate in the bloodstream may serve as physiological ligands for T2Rs in the extraoral cells and tissues. Interestingly, using a heterologous expression system, Lossow et al. (2016) recently reported that progesterone can activate mouse T2R110 and T2R114, raising the possibility that this reproductively important hormone may be one of the endogenous ligands for T2Rs. The method by which Yoshikawa et al. (2013) identified a physiological ligand for olfactory receptor 288 using fractionation of crude tissue extracts may be instructive for searching for T2Rs’ endogenous ligands.
Studying T2R transcription regulation
So far, only one regulator, sterol regulatory element–binding protein (SREBP-2), has been demonstrated to target the transcription machinery of T2Rs. SREBP-2 activates the transcription of T2R138 by directly binding to the promoter region in STC-1 cells (Jeon et al., 2008). Studying T2R regulators would facilitate identifying T2R physiological functions, especially when T2R knockout mice are lacking. T2Rs locate in chromosomes as clusters, suggesting that common gene regulatory mechanisms may exist to control the T2R loci. For example, after analyzing regions near T2R loci in silico, Foster et al. (2013, 2014a, 2015) detected cis-regulatory domains, which are overlaps of histone marks and DNase-I hypersensitivity regions and indicative of active enhancer and promoter regions, in the mouse T2R143/135/126 cluster as well as in the regions proximal to human T2R5 and T2R14 loci. Besides such local control regions, long-range cis-regulatory elements in chromatin may also exist to regulate T2R transcription; these elements, despite a large separation along the DNA, can interact with each other to work in a regulatory capacity because of their proximity in 3-D (Harmston and Lenhard, 2013; Heinz et al., 2015). A detailed analysis of the transcript regulatory elements of T2Rs would be informative to enhance our understanding of T2Rs’ roles.
Conclusion
Cumulative evidence indicates that T2Rs mediate a variety of functions in nonlingual tissues and may underlie several human diseases or disorders. Targeting of T2Rs in extraoral tissues is showing promise for the development of new therapeutics. The wide expression of extraoral T2Rs underscores the possibility that they might be accountable for the many side effects of current medicines because most drugs have a bitter taste (Clark et al., 2012). However, all this reinforces the necessity to fully characterize T2R physiology and pathophysiology at different extraoral locations. With this knowledge, we may one day understand the true biological basis through which bitter drugs can act as “good medicine.”
ACKNOWLEDGMENTS
Research in the laboratory of R. ZhuGe is supported by the National Institutes of Health grant HL117104.
The authors declare no competing financial interests.
Lesley C. Anson served as editor.
Footnotes
Abbreviations used:
- AHL
- acyl-homoserine lactone
- CCK
- cholecystokinin
- EEC
- enteroendocrine cell
- GPCR
- G protein–coupled receptor
- SCC
- solitary chemosensory cell
- SNP
- single-nucleotide polymorphism
- VNO
- vomerolnasal organ
References
- Adappa N.D., Zhang Z., Palmer J.N., Kennedy D.W., Doghramji L., Lysenko A., Reed D.R., Scott T., Zhao N.W., Owens D., et al. 2014. The bitter taste receptor T2R38 is an independent risk factor for chronic rhinosinusitis requiring sinus surgery. Int. Forum Allergy Rhinol. 4:3–7. 10.1002/alr.21253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adappa N.D., Farquhar D., Palmer J.N., Kennedy D.W., Doghramji L., Morris S.A., Owens D., Mansfield C., Lysenko A., Lee R.J., et al. 2016a TAS2R38 genotype predicts surgical outcome in nonpolypoid chronic rhinosinusitis. Int. Forum Allergy Rhinol. 6:25–33. 10.1002/alr.21666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adappa N.D., Truesdale C.M., Workman A.D., Doghramji L., Mansfield C., Kennedy D.W., Palmer J.N., Cowart B.J., and Cohen N.A.. 2016c Correlation of T2R38 taste phenotype and in vitro biofilm formation from nonpolypoid chronic rhinosinusitis patients. Int. Forum Allergy Rhinol. 6:783–791. 10.1002/alr.21803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adappa N.D., Workman A.D., Hadjiliadis D., Dorgan D.J., Frame D., Brooks S., Doghramji L., Palmer J.N., Mansfield C., Reed D.R., and Cohen N.A.. 2016b T2R38 genotype is correlated with sinonasal quality of life in homozygous ΔF508 cystic fibrosis patients. Int. Forum Allergy Rhinol. 6:356–361. 10.1002/alr.21675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahlman H., and Nilsson O.. 2001. The gut as the largest endocrine organ in the body. Ann. Oncol. 12(Suppl 2):S63–S68. 10.1093/annonc/12.suppl_2.S63 [DOI] [PubMed] [Google Scholar]
- Akao H., Polisecki E., Kajinami K., Trompet S., Robertson M., Ford I., Jukema J.W., de Craen A.J., Westendorp R.G., Shepherd J., et al. 2012. KIF6, LPA, TAS2R50, and VAMP8 genetic variation, low density lipoprotein cholesterol lowering response to pravastatin, and heart disease risk reduction in the elderly. Atherosclerosis. 220:456–462. 10.1016/j.atherosclerosis.2011.11.037 [DOI] [PubMed] [Google Scholar]
- Amjadi F., Salehi E., Mehdizadeh M., and Aflatoonian R.. 2014. Role of the innate immunity in female reproductive tract. Adv. Biomed. Res. 3 10.4103/2277-9175.124626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- An S.S., Wang W.C., Koziol-White C.J., Ahn K., Lee D.Y., Kurten R.C., Panettieri R.A. Jr., and Liggett S.B.. 2012. TAS2R activation promotes airway smooth muscle relaxation despite β2-adrenergic receptor tachyphylaxis. Am. J. Physiol. Lung Cell. Mol. Physiol. 303:L304–L311. 10.1152/ajplung.00126.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ansoleaga B., Garcia-Esparcia P., Pinacho R., Haro J.M., Ramos B., and Ferrer I.. 2015. Decrease in olfactory and taste receptor expression in the dorsolateral prefrontal cortex in chronic schizophrenia. J. Psychiatr. Res. 60:109–116. 10.1016/j.jpsychires.2014.09.012 [DOI] [PubMed] [Google Scholar]
- Avau B., Rotondo A., Thijs T., Andrews C.N., Janssen P., Tack J., and Depoortere I.. 2015. Targeting extra-oral bitter taste receptors modulates gastrointestinal motility with effects on satiation. Sci. Rep. 5 10.1038/srep15985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avila M., Ojcius D.M., and Yilmaz O.. 2009. The oral microbiota: living with a permanent guest. DNA Cell Biol. 28:405–411. 10.1089/dna.2009.0874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behrens M., Bartelt J., Reichling C., Winnig M., Kuhn C., and Meyerhof W.. 2006. Members of RTP and REEP gene families influence functional bitter taste receptor expression. J. Biol. Chem. 281:20650–20659. 10.1074/jbc.M513637200 [DOI] [PubMed] [Google Scholar]
- Bezençon C., Fürholz A., Raymond F., Mansourian R., Métairon S., Le Coutre J., and Damak S.. 2008. Murine intestinal cells expressing Trpm5 are mostly brush cells and express markers of neuronal and inflammatory cells. J. Comp. Neurol. 509:514–525. 10.1002/cne.21768 [DOI] [PubMed] [Google Scholar]
- Brockhoff A., Behrens M., Roudnitzky N., Appendino G., Avonto C., and Meyerhof W.. 2011. Receptor agonism and antagonism of dietary bitter compounds. J. Neurosci. 31:14775–14782. 10.1523/JNEUROSCI.2923-11.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bufe B., Breslin P.A., Kuhn C., Reed D.R., Tharp C.D., Slack J.P., Kim U.K., Drayna D., and Meyerhof W.. 2005. The molecular basis of individual differences in phenylthiocarbamide and propylthiouracil bitterness perception. Curr. Biol. 15:322–327. 10.1016/j.cub.2005.01.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camoretti-Mercado B., Pauer S.H., Yong H.M., Smith D.C., Deshpande D.A., An S.S., and Liggett S.B.. 2015. Pleiotropic effects of bitter taste receptors on [Ca2+]i mobilization, hyperpolarization, and relaxation of human airway smooth muscle cells. PLoS One. 10 10.1371/journal.pone.0131582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campa D., De Rango F., Carrai M., Crocco P., Montesanto A., Canzian F., Rose G., Rizzato C., Passarino G., and Barale R.. 2012. Bitter taste receptor polymorphisms and human aging. PLoS One. 7 10.1371/journal.pone.0045232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell M.C., Ranciaro A., Zinshteyn D., Rawlings-Goss R., Hirbo J., Thompson S., Woldemeskel D., Froment A., Rucker J.B., Omar S.A., et al. 2014. Origin and differential selection of allelic variation at TAS2R16 associated with salicin bitter taste sensitivity in Africa. Mol. Biol. Evol. 31:288–302. 10.1093/molbev/mst211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrai M., Steinke V., Vodicka P., Pardini B., Rahner N., Holinski-Feder E., Morak M., Schackert H.K., Görgens H., Stemmler S., et al. 2011. Association between TAS2R38 gene polymorphisms and colorectal cancer risk: a case-control study in two independent populations of Caucasian origin. PLoS One. 6 10.1371/journal.pone.0020464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandrashekar J., Mueller K.L., Hoon M.A., Adler E., Feng L., Guo W., Zuker C.S., and Ryba N.J.. 2000. T2Rs function as bitter taste receptors. Cell. 100:703–711. 10.1016/S0092-8674(00)80706-0 [DOI] [PubMed] [Google Scholar]
- Chandrashekar J., Hoon M.A., Ryba N.J., and Zuker C.S.. 2006. The receptors and cells for mammalian taste. Nature. 444:288–294. 10.1038/nature05401 [DOI] [PubMed] [Google Scholar]
- Chaplin D.D. 2010. Overview of the immune response. J. Allergy Clin. Immunol. 125(2, Suppl 2):S3–S23. 10.1016/j.jaci.2009.12.980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhari N., and Roper S.D.. 2010. The cell biology of taste. J. Cell Biol. 190:285–296. (published erratum appears in J. Cell Biol. 2010. 191:429) 10.1083/jcb.201003144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen M.C., Wu S.V., Reeve J.R. Jr., and Rozengurt E.. 2006. Bitter stimuli induce Ca2+ signaling and CCK release in enteroendocrine STC-1 cells: role of l-type voltage-sensitive Ca2+ channels. Am. J. Physiol. Cell Physiol. 291:C726–C739. 10.1152/ajpcell.00003.2006 [DOI] [PubMed] [Google Scholar]
- Clark A.A., Liggett S.B., and Munger S.D.. 2012. Extraoral bitter taste receptors as mediators of off-target drug effects. FASEB J. 26:4827–4831. 10.1096/fj.12-215087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark A.A., Dotson C.D., Elson A.E., Voigt A., Boehm U., Meyerhof W., Steinle N.I., and Munger S.D.. 2015. TAS2R bitter taste receptors regulate thyroid function. FASEB J. 29:164–172. 10.1096/fj.14-262246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csont T., Murlasits Z., Ménesi D., Kelemen J.Z., Bencsik P., Pipicz M., Fekete V., Zvara Á., Puskás L.G., and Ferdinandy P.. 2015. Tissue-specific gene expression in rat hearts and aortas in a model of vascular nitrate tolerance. J. Cardiovasc. Pharmacol. 65:485–493. 10.1097/FJC.0000000000000218 [DOI] [PubMed] [Google Scholar]
- Cui W., Taub D.D., and Gardner K.. 2007. qPrimerDepot: a primer database for quantitative real time PCR. Nucleic Acids Res. 35(Database):D805–D809. 10.1093/nar/gkl767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings D.E., and Overduin J.. 2007. Gastrointestinal regulation of food intake. J. Clin. Invest. 117:13–23. 10.1172/JCI30227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies D.G., Parsek M.R., Pearson J.P., Iglewski B.H., Costerton J.W., and Greenberg E.P.. 1998. The involvement of cell-to-cell signals in the development of a bacterial biofilm. Science. 280:295–298. 10.1126/science.280.5361.295 [DOI] [PubMed] [Google Scholar]
- Deckmann K., Filipski K., Krasteva-Christ G., Fronius M., Althaus M., Rafiq A., Papadakis T., Renno L., Jurastow I., Wessels L., et al. 2014. Bitter triggers acetylcholine release from polymodal urethral chemosensory cells and bladder reflexes. Proc. Natl. Acad. Sci. USA. 111:8287–8292. 10.1073/pnas.1402436111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dehkordi O., Rose J.E., Fatemi M., Allard J.S., Balan K.V., Young J.K., Fatima S., Millis R.M., and Jayam-Trouth A.. 2012. Neuronal expression of bitter taste receptors and downstream signaling molecules in the rat brainstem. Brain Res. 1475:1–10. 10.1016/j.brainres.2012.07.038 [DOI] [PubMed] [Google Scholar]
- Deshpande D.A., Wang W.C., McIlmoyle E.L., Robinett K.S., Schillinger R.M., An S.S., Sham J.S., and Liggett S.B.. 2010. Bitter taste receptors on airway smooth muscle bronchodilate by localized calcium signaling and reverse obstruction. Nat. Med. 16:1299–1304. 10.1038/nm.2237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewhirst F.E., Chen T., Izard J., Paster B.J., Tanner A.C., Yu W.H., Lakshmanan A., and Wade W.G.. 2010. The human oral microbiome. J. Bacteriol. 192:5002–5017. 10.1128/JB.00542-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dotson C.D., Zhang L., Xu H., Shin Y.K., Vigues S., Ott S.H., Elson A.E., Choi H.J., Shaw H., Egan J.M., et al. 2008. Bitter taste receptors influence glucose homeostasis. PLoS One. 3 10.1371/journal.pone.0003974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eberhard A., Burlingame A.L., Eberhard C., Kenyon G.L., Nealson K.H., and Oppenheimer N.J.. 1981. Structural identification of autoinducer of Photobacterium fischeri luciferase. Biochemistry. 20:2444–2449. 10.1021/bi00512a013 [DOI] [PubMed] [Google Scholar]
- Finger T.E., Böttger B., Hansen A., Anderson K.T., Alimohammadi H., and Silver W.L.. 2003. Solitary chemoreceptor cells in the nasal cavity serve as sentinels of respiration. Proc. Natl. Acad. Sci. USA. 100:8981–8986. 10.1073/pnas.1531172100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finger T.E., Danilova V., Barrows J., Bartel D.L., Vigers A.J., Stone L., Hellekant G., and Kinnamon S.C.. 2005. ATP signaling is crucial for communication from taste buds to gustatory nerves. Science. 310:1495–1499. 10.1126/science.1118435 [DOI] [PubMed] [Google Scholar]
- Foster S.R., Porrello E.R., Purdue B., Chan H.W., Voigt A., Frenzel S., Hannan R.D., Moritz K.M., Simmons D.G., Molenaar P., et al. 2013. Expression, regulation and putative nutrient-sensing function of taste GPCRs in the heart. PLoS One. 8 10.1371/journal.pone.0064579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster S.R., Blank K., See Hoe L.E., Behrens M., Meyerhof W., Peart J.N., and Thomas W.G.. 2014a Bitter taste receptor agonists elicit G-protein-dependent negative inotropy in the murine heart. FASEB J. 28:4497–4508. 10.1096/fj.14-256305 [DOI] [PubMed] [Google Scholar]
- Foster S.R., Roura E., and Thomas W.G.. 2014b Extrasensory perception: odorant and taste receptors beyond the nose and mouth. Pharmacol. Ther. 142:41–61. 10.1016/j.pharmthera.2013.11.004 [DOI] [PubMed] [Google Scholar]
- Foster S.R., Porrello E.R., Stefani M., Smith N.J., Molenaar P., dos Remedios C.G., Thomas W.G., and Ramialison M.. 2015. Cardiac gene expression data and in silico analysis provide novel insights into human and mouse taste receptor gene regulation. Naunyn Schmiedebergs Arch. Pharmacol. 388:1009–1027. 10.1007/s00210-015-1118-1 [DOI] [PubMed] [Google Scholar]
- Gaida M.M., Dapunt U., and Hänsch G.M.. 2016a Sensing developing biofilms: the bitter receptor T2R38 on myeloid cells. Pathog. Dis. 74 10.1093/femspd/ftw004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaida M.M., Mayer C., Dapunt U., Stegmaier S., Schirmacher P., Wabnitz G.H., and Hänsch G.M.. 2016b Expression of the bitter receptor T2R38 in pancreatic cancer: localization in lipid droplets and activation by a bacteria-derived quorum-sensing molecule. Oncotarget. 7:12623–12632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo S., Grossi S., Montrasio G., Binelli G., Cinquetti R., Simmen D., Castelnuovo P., and Campomenosi P.. 2016. TAS2R38 taste receptor gene and chronic rhinosinusitis: new data from an Italian population. BMC Med. Genet. 17 10.1186/s12881-016-0321-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Esparcia P., Schlüter A., Carmona M., Moreno J., Ansoleaga B., Torrejón-Escribano B., Gustincich S., Pujol A., and Ferrer I.. 2013. Functional genomics reveals dysregulation of cortical olfactory receptors in Parkinson disease: novel putative chemoreceptors in the human brain. J. Neuropathol. Exp. Neurol. 72:524–539. 10.1097/NEN.0b013e318294fd76 [DOI] [PubMed] [Google Scholar]
- Gerbe F., Sidot E., Smyth D.J., Ohmoto M., Matsumoto I., Dardalhon V., Cesses P., Garnier L., Pouzolles M., Brulin B., et al. 2016. Intestinal epithelial tuft cells initiate type 2 mucosal immunity to helminth parasites. Nature. 529:226–230. 10.1038/nature16527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gil S., Coldwell S., Drury J.L., Arroyo F., Phi T., Saadat S., Kwong D., and Chung W.O.. 2015. Genotype-specific regulation of oral innate immunity by T2R38 taste receptor. Mol. Immunol. 68(2, 2 Pt C):663–670. 10.1016/j.molimm.2015.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grassin-Delyle S., Abrial C., Fayad-Kobeissi S., Brollo M., Faisy C., Alvarez J.C., Naline E., and Devillier P.. 2013. The expression and relaxant effect of bitter taste receptors in human bronchi. Respir. Res. 14 10.1186/1465-9921-14-134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene T.A., Alarcon S., Thomas A., Berdougo E., Doranz B.J., Breslin P.A., and Rucker J.B.. 2011. Probenecid inhibits the human bitter taste receptor TAS2R16 and suppresses bitter perception of salicin. PLoS One. 6 10.1371/journal.pone.0020123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gribble F.M., and Reimann F.. 2016. Enteroendocrine cells: chemosensors in the intestinal epithelium. Annu. Rev. Physiol. 78:277–299. 10.1146/annurev-physiol-021115-105439 [DOI] [PubMed] [Google Scholar]
- Gulbransen B.D., Clapp T.R., Finger T.E., and Kinnamon S.C.. 2008. Nasal solitary chemoreceptor cell responses to bitter and trigeminal stimulants in vitro. J. Neurophysiol. 99:2929–2937. 10.1152/jn.00066.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmston N., and Lenhard B.. 2013. Chromatin and epigenetic features of long-range gene regulation. Nucleic Acids Res. 41:7185–7199. 10.1093/nar/gkt499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hass N., Schwarzenbacher K., and Breer H.. 2007. A cluster of gustducin-expressing cells in the mouse stomach associated with two distinct populations of enteroendocrine cells. Histochem. Cell Biol. 128:457–471. 10.1007/s00418-007-0325-3 [DOI] [PubMed] [Google Scholar]
- Heinz S., Romanoski C.E., Benner C., and Glass C.K.. 2015. The selection and function of cell type-specific enhancers. Nat. Rev. Mol. Cell Biol. 16:144–154. 10.1038/nrm3949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Höfer D., Püschel B., and Drenckhahn D.. 1996. Taste receptor-like cells in the rat gut identified by expression of α-gustducin. Proc. Natl. Acad. Sci. USA. 93:6631–6634. 10.1073/pnas.93.13.6631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howitt M.R., Lavoie S., Michaud M., Blum A.M., Tran S.V., Weinstock J.V., Gallini C.A., Redding K., Margolskee R.F., Osborne L.C., et al. 2016. Tuft cells, taste-chemosensory cells, orchestrate parasite type 2 immunity in the gut. Science. 351:1329–1333. 10.1126/science.aaf1648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang L., Shanker Y.G., Dubauskaite J., Zheng J.Z., Yan W., Rosenzweig S., Spielman A.I., Max M., and Margolskee R.F.. 1999. Gγ13 colocalizes with gustducin in taste receptor cells and mediates IP3 responses to bitter denatonium. Nat. Neurosci. 2:1055–1062. 10.1038/15981 [DOI] [PubMed] [Google Scholar]
- Ilegems E., Iwatsuki K., Kokrashvili Z., Benard O., Ninomiya Y., and Margolskee R.F.. 2010. REEP2 enhances sweet receptor function by recruitment to lipid rafts. J. Neurosci. 30:13774–13783. 10.1523/JNEUROSCI.0091-10.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang H.J., Kokrashvili Z., Theodorakis M.J., Carlson O.D., Kim B.J., Zhou J., Kim H.H., Xu X., Chan S.L., Juhaszova M., et al. 2007. Gut-expressed gustducin and taste receptors regulate secretion of glucagon-like peptide-1. Proc. Natl. Acad. Sci. USA. 104:15069–15074. 10.1073/pnas.0706890104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen S., Laermans J., Verhulst P.J., Thijs T., Tack J., and Depoortere I.. 2011. Bitter taste receptors and α-gustducin regulate the secretion of ghrelin with functional effects on food intake and gastric emptying. Proc. Natl. Acad. Sci. USA. 108:2094–2099. 10.1073/pnas.1011508108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeon T.I., Zhu B., Larson J.L., and Osborne T.F.. 2008. SREBP-2 regulates gut peptide secretion through intestinal bitter taste receptor signaling in mice. J. Clin. Invest. 118:3693–3700. 10.1172/JCI36461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeon T.I., Seo Y.K., and Osborne T.F.. 2011. Gut bitter taste receptor signalling induces ABCB1 through a mechanism involving CCK. Biochem. J. 438:33–37. 10.1042/BJ20110009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji M., Su X., Su X., Chen Y., Huang W., Zhang J., Gao Z., Li C., and Lu X.. 2014. Identification of novel compounds for human bitter taste receptors. Chem. Biol. Drug Des. 84:63–74. 10.1111/cbdd.12293 [DOI] [PubMed] [Google Scholar]
- Kaji I., Karaki S., Fukami Y., Terasaki M., and Kuwahara A.. 2009. Secretory effects of a luminal bitter tastant and expressions of bitter taste receptors, T2Rs, in the human and rat large intestine. Am. J. Physiol. Gastrointest. Liver Physiol. 296:G971–G981. 10.1152/ajpgi.90514.2008 [DOI] [PubMed] [Google Scholar]
- Kautiainen A. 1992. Determination of hemoglobin adducts from aldehydes formed during lipid peroxidation in vitro. Chem. Biol. Interact. 83:55–63. 10.1016/0009-2797(92)90091-X [DOI] [PubMed] [Google Scholar]
- Keller M., Liu X., Wohland T., Rohde K., Gast M.T., Stumvoll M., Kovacs P., Tönjes A., and Böttcher Y.. 2013. TAS2R38 and its influence on smoking behavior and glucose homeostasis in the German Sorbs. PLoS One. 8 10.1371/journal.pone.0080512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim K.S., Egan J.M., and Jang H.J.. 2014. Denatonium induces secretion of glucagon-like peptide-1 through activation of bitter taste receptor pathways. Diabetologia. 57:2117–2125. (published erratum appears in Diabetologia 2014. 57:2428) 10.1007/s00125-014-3326-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim U.K., Jorgenson E., Coon H., Leppert M., Risch N., and Drayna D.. 2003. Positional cloning of the human quantitative trait locus underlying taste sensitivity to phenylthiocarbamide. Science. 299:1221–1225. 10.1126/science.1080190 [DOI] [PubMed] [Google Scholar]
- Krasteva G., Canning B.J., Hartmann P., Veres T.Z., Papadakis T., Mühlfeld C., Schliecker K., Tallini Y.N., Braun A., Hackstein H., et al. 2011. Cholinergic chemosensory cells in the trachea regulate breathing. Proc. Natl. Acad. Sci. USA. 108:9478–9483. 10.1073/pnas.1019418108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krasteva G., Canning B.J., Papadakis T., and Kummer W.. 2012a Cholinergic brush cells in the trachea mediate respiratory responses to quorum sensing molecules. Life Sci. 91:992–996. 10.1016/j.lfs.2012.06.014 [DOI] [PubMed] [Google Scholar]
- Krasteva G., Hartmann P., Papadakis T., Bodenbenner M., Wessels L., Weihe E., Schütz B., Langheinrich A.C., Chubanov V., Gudermann T., et al. 2012b Cholinergic chemosensory cells in the auditory tube. Histochem. Cell Biol. 137:483–497. 10.1007/s00418-012-0911-x [DOI] [PubMed] [Google Scholar]
- Krasteva-Christ G., Soultanova A., Schütz B., Papadakis T., Weiss C., Deckmann K., Chubanov V., Gudermann T., Voigt A., Meyerhof W., et al. 2015. Identification of cholinergic chemosensory cells in mouse tracheal and laryngeal glandular ducts. Int. Immunopharmacol. 29:158–165. 10.1016/j.intimp.2015.05.028 [DOI] [PubMed] [Google Scholar]
- Latorre R., Huynh J., Mazzoni M., Gupta A., Bonora E., Clavenzani P., Chang L., Mayer E.A., De Giorgio R., and Sternini C.. 2016. Expression of the bitter taste receptor, T2R38, in enteroendocrine cells of the colonic mucosa of overweight/obese vs. lean subjects. PLoS One. 11 10.1371/journal.pone.0147468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee R.J., and Cohen N.A.. 2013. The emerging role of the bitter taste receptor T2R38 in upper respiratory infection and chronic rhinosinusitis. Am. J. Rhinol. Allergy. 27:283–286. 10.2500/ajra.2013.27.3911 [DOI] [PubMed] [Google Scholar]
- Lee R.J., and Cohen N.A.. 2014. Bitter and sweet taste receptors in the respiratory epithelium in health and disease. J. Mol. Med. 92:1235–1244. 10.1007/s00109-014-1222-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee R.J., Xiong G., Kofonow J.M., Chen B., Lysenko A., Jiang P., Abraham V., Doghramji L., Adappa N.D., Palmer J.N., et al. 2012. T2R38 taste receptor polymorphisms underlie susceptibility to upper respiratory infection. J. Clin. Invest. 122:4145–4159. 10.1172/JCI64240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee R.J., Chen B., Redding K.M., Margolskee R.F., and Cohen N.A.. 2014a Mouse nasal epithelial innate immune responses to Pseudomonas aeruginosa quorum-sensing molecules require taste signaling components. Innate Immun. 20:606–617. 10.1177/1753425913503386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee R.J., Kofonow J.M., Rosen P.L., Siebert A.P., Chen B., Doghramji L., Xiong G., Adappa N.D., Palmer J.N., Kennedy D.W., et al. 2014b Bitter and sweet taste receptors regulate human upper respiratory innate immunity. J. Clin. Invest. 124:1393–1405. 10.1172/JCI72094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Nevé B., Foltz M., Daniel H., and Gouka R.. 2010. The steroid glycoside H.g.-12 from Hoodia gordonii activates the human bitter receptor TAS2R14 and induces CCK release from HuTu-80 cells. Am. J. Physiol. Gastrointest. Liver Physiol. 299:G1368–G1375. 10.1152/ajpgi.00135.2010 [DOI] [PubMed] [Google Scholar]
- Levit A., Nowak S., Peters M., Wiener A., Meyerhof W., Behrens M., and Niv M.Y.. 2014. The bitter pill: clinical drugs that activate the human bitter taste receptor TAS2R14. FASEB J. 28:1181–1197. 10.1096/fj.13-242594 [DOI] [PubMed] [Google Scholar]
- Li F., and Zhou M.. 2012. Depletion of bitter taste transduction leads to massive spermatid loss in transgenic mice. Mol. Hum. Reprod. 18:289–297. 10.1093/molehr/gas005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H., Pakstis A.J., Kidd J.R., and Kidd K.K.. 2011. Selection on the human bitter taste gene, TAS2R16, in Eurasian populations. Hum. Biol. 83:363–377. 10.3378/027.083.0303 [DOI] [PubMed] [Google Scholar]
- Lin W., Ogura T., Margolskee R.F., Finger T.E., and Restrepo D.. 2008. TRPM5-expressing solitary chemosensory cells respond to odorous irritants. J. Neurophysiol. 99:1451–1460. 10.1152/jn.01195.2007 [DOI] [PubMed] [Google Scholar]
- Liu X., Gu F., Jiang L., Chen F., and Li F.. 2015. Expression of bitter taste receptor Tas2r105 in mouse kidney. Biochem. Biophys. Res. Commun. 458:733–738. 10.1016/j.bbrc.2015.01.089 [DOI] [PubMed] [Google Scholar]
- Lossow K., Hübner S., Roudnitzky N., Slack J.P., Pollastro F., Behrens M., and Meyerhof W.. 2016. Comprehensive analysis of mouse bitter taste receptors reveals different molecular receptive ranges for orthologous receptors in mice and humans. J. Biol. Chem. 291:15358–15377. 10.1074/jbc.M116.718544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund T.C., Kobs A.J., Kramer A., Nyquist M., Kuroki M.T., Osborn J., Lidke D.S., Low-Nam S.T., Blazar B.R., and Tolar J.. 2013. Bone marrow stromal and vascular smooth muscle cells have chemosensory capacity via bitter taste receptor expression. PLoS One. 8 10.1371/journal.pone.0058945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malki A., Fiedler J., Fricke K., Ballweg I., Pfaffl M.W., and Krautwurst D.. 2015. Class I odorant receptors, TAS1R and TAS2R taste receptors, are markers for subpopulations of circulating leukocytes. J. Leukoc. Biol. 97:533–545. 10.1189/jlb.2A0714-331RR [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manson M.L., Säfholm J., Al-Ameri M., Bergman P., Orre A.C., Swärd K., James A., Dahlén S.E., and Adner M.. 2014. Bitter taste receptor agonists mediate relaxation of human and rodent vascular smooth muscle. Eur. J. Pharmacol. 740:302–311. 10.1016/j.ejphar.2014.07.005 [DOI] [PubMed] [Google Scholar]
- Marx V. 2014. Cell communication: stop the microbial chatter. Nature. 511:493–497. 10.1038/511493a [DOI] [PubMed] [Google Scholar]
- Maurer S., Wabnitz G.H., Kahle N.A., Stegmaier S., Prior B., Giese T., Gaida M.M., Samstag Y., and Hänsch G.M.. 2015. Tasting Pseudomonas aeruginosa biofilms: human neutrophils express the bitter receptor T2R38 as sensor for the quorum sensing molecule N-(3-oxododecanoyl)-L-homoserine lactone. Front. Immunol. 6 10.3389/fimmu.2015.00369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin S.K., McKinnon P.J., and Margolskee R.F.. 1992. Gustducin is a taste-cell-specific G protein closely related to the transducins. Nature. 357:563–569. 10.1038/357563a0 [DOI] [PubMed] [Google Scholar]
- Meyerhof W., Batram C., Kuhn C., Brockhoff A., Chudoba E., Bufe B., Appendino G., and Behrens M.. 2010. The molecular receptive ranges of human TAS2R bitter taste receptors. Chem. Senses. 35:157–170. 10.1093/chemse/bjp092 [DOI] [PubMed] [Google Scholar]
- Mueller K.L., Hoon M.A., Erlenbach I., Chandrashekar J., Zuker C.S., and Ryba N.J.. 2005. The receptors and coding logic for bitter taste. Nature. 434:225–229. 10.1038/nature03352 [DOI] [PubMed] [Google Scholar]
- Nealson K.H., and Hastings J.W.. 1979. Bacterial bioluminescence: its control and ecological significance. Microbiol. Rev. 43:496–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nealson K.H., Platt T., and Hastings J.W.. 1970. Cellular control of the synthesis and activity of the bacterial luminescent system. J. Bacteriol. 104:313–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogura T., Krosnowski K., Zhang L., Bekkerman M., and Lin W.. 2010. Chemoreception regulates chemical access to mouse vomeronasal organ: role of solitary chemosensory cells. PLoS One. 5 10.1371/journal.pone.0011924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orsmark-Pietras C., James A., Konradsen J.R., Nordlund B., Söderhäll C., Pulkkinen V., Pedroletti C., Daham K., Kupczyk M., Dahlén B., et al. 2013. Transcriptome analysis reveals upregulation of bitter taste receptors in severe asthmatics. Eur. Respir. J. 42:65–78. 10.1183/09031936.00077712 [DOI] [PubMed] [Google Scholar]
- Panneck A.R., Rafiq A., Schütz B., Soultanova A., Deckmann K., Chubanov V., Gudermann T., Weihe E., Krasteva-Christ G., Grau V., et al. 2014. Cholinergic epithelial cell with chemosensory traits in murine thymic medulla. Cell Tissue Res. 358:737–748. 10.1007/s00441-014-2002-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pastorelli L., De Salvo C., Mercado J.R., Vecchi M., and Pizarro T.T.. 2013. Central role of the gut epithelial barrier in the pathogenesis of chronic intestinal inflammation: lessons learned from animal models and human genetics. Front. Immunol. 4 10.3389/fimmu.2013.00280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng Y., Gillis-Smith S., Jin H., Tränkner D., Ryba N.J., and Zuker C.S.. 2015. Sweet and bitter taste in the brain of awake behaving animals. Nature. 527:512–515. 10.1038/nature15763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson L.W., and Artis D.. 2014. Intestinal epithelial cells: regulators of barrier function and immune homeostasis. Nat. Rev. Immunol. 14:141–153. 10.1038/nri3608 [DOI] [PubMed] [Google Scholar]
- Prandi S., Bromke M., Hübner S., Voigt A., Boehm U., Meyerhof W., and Behrens M.. 2013. A subset of mouse colonic goblet cells expresses the bitter taste receptor Tas2r131. PLoS One. 8 10.1371/journal.pone.0082820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Psichas A., Reimann F., and Gribble F.M.. 2015. Gut chemosensing mechanisms. J. Clin. Invest. 125:908–917. 10.1172/JCI76309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulkkinen V., Manson M.L., Säfholm J., Adner M., and Dahlén S.E.. 2012. The bitter taste receptor (TAS2R) agonists denatonium and chloroquine display distinct patterns of relaxation of the guinea pig trachea. Am. J. Physiol. Lung Cell. Mol. Physiol. 303:L956–L966. 10.1152/ajplung.00205.2012 [DOI] [PubMed] [Google Scholar]
- Pydi S.P., Sobotkiewicz T., Billakanti R., Bhullar R.P., Loewen M.C., and Chelikani P.. 2014. Amino acid derivatives as bitter taste receptor (T2R) blockers. J. Biol. Chem. 289:25054–25066. 10.1074/jbc.M114.576975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pydi S.P., Jaggupilli A., Nelson K.M., Abrams S.R., Bhullar R.P., Loewen M.C., and Chelikani P.. 2015. Abscisic acid acts as a blocker of the bitter taste G protein-coupled receptor T2R4. Biochemistry. 54:2622–2631. 10.1021/acs.biochem.5b00265 [DOI] [PubMed] [Google Scholar]
- Rajkumar P., Aisenberg W.H., Acres O.W., Protzko R.J., and Pluznick J.L.. 2014. Identification and characterization of novel renal sensory receptors. PLoS One. 9 10.1371/journal.pone.0111053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raz T., Kapranov P., Lipson D., Letovsky S., Milos P.M., and Thompson J.F.. 2011. Protocol dependence of sequencing-based gene expression measurements. PLoS One. 6 10.1371/journal.pone.0019287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Risso D., Tofanelli S., Morini G., Luiselli D., and Drayna D.. 2014. Genetic variation in taste receptor pseudogenes provides evidence for a dynamic role in human evolution. BMC Evol. Biol. 14 10.1186/s12862-014-0198-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinett K.S., Deshpande D.A., Malone M.M., and Liggett S.B.. 2011. Agonist-promoted homologous desensitization of human airway smooth muscle bitter taste receptors. Am. J. Respir. Cell Mol. Biol. 45:1069–1074. 10.1165/rcmb.2011-0061OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinett K.S., Koziol-White C.J., Akoluk A., An S.S., Panettieri R.A. Jr., and Liggett S.B.. 2014. Bitter taste receptor function in asthmatic and nonasthmatic human airway smooth muscle cells. Am. J. Respir. Cell Mol. Biol. 50:678–683. 10.1165/rcmb.2013-0439RC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roland W.S., Gouka R.J., Gruppen H., Driesse M., van Buren L., Smit G., and Vincken J.P.. 2014. 6-methoxyflavanones as bitter taste receptor blockers for hTAS2R39. PLoS One. 9 10.1371/journal.pone.0094451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salathe M. 2007. Regulation of mammalian ciliary beating. Annu. Rev. Physiol. 69:401–422. 10.1146/annurev.physiol.69.040705.141253 [DOI] [PubMed] [Google Scholar]
- Saunders C.J., Christensen M., Finger T.E., and Tizzano M.. 2014. Cholinergic neurotransmission links solitary chemosensory cells to nasal inflammation. Proc. Natl. Acad. Sci. USA. 111:6075–6080. 10.1073/pnas.1402251111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah A.S., Ben-Shahar Y., Moninger T.O., Kline J.N., and Welsh M.J.. 2009. Motile cilia of human airway epithelia are chemosensory. Science. 325:1131–1134. 10.1126/science.1173869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaykhiev R., and Crystal R.G.. 2013. Innate immunity and chronic obstructive pulmonary disease: a mini-review. Gerontology. 59:481–489. 10.1159/000354173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi P., Zhang J., Yang H., and Zhang Y.P.. 2003. Adaptive diversification of bitter taste receptor genes in mammalian evolution. Mol. Biol. Evol. 20:805–814. 10.1093/molbev/msg083 [DOI] [PubMed] [Google Scholar]
- Shiffman D., O’Meara E.S., Bare L.A., Rowland C.M., Louie J.Z., Arellano A.R., Lumley T., Rice K., Iakoubova O., Luke M.M., et al. 2008. Association of gene variants with incident myocardial infarction in the cardiovascular health study. Arterioscler. Thromb. Vasc. Biol. 28:173–179. 10.1161/ATVBAHA.107.153981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh N., Vrontakis M., Parkinson F., and Chelikani P.. 2011. Functional bitter taste receptors are expressed in brain cells. Biochem. Biophys. Res. Commun. 406:146–151. 10.1016/j.bbrc.2011.02.016 [DOI] [PubMed] [Google Scholar]
- Singh N., Chakraborty R., Bhullar R.P., and Chelikani P.. 2014. Differential expression of bitter taste receptors in non-cancerous breast epithelial and breast cancer cells. Biochem. Biophys. Res. Commun. 446:499–503. 10.1016/j.bbrc.2014.02.140 [DOI] [PubMed] [Google Scholar]
- Slack J.P., Brockhoff A., Batram C., Menzel S., Sonnabend C., Born S., Galindo M.M., Kohl S., Thalmann S., Ostopovici-Halip L., et al. 2010. Modulation of bitter taste perception by a small molecule hTAS2R antagonist. Curr. Biol. 20:1104–1109. 10.1016/j.cub.2010.04.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommer F., and Bäckhed F.. 2013. The gut microbiota--masters of host development and physiology. Nat. Rev. Microbiol. 11:227–238. 10.1038/nrmicro2974 [DOI] [PubMed] [Google Scholar]
- Soultanova A., Voigt A., Chubanov V., Gudermann T., Meyerhof W., Boehm U., and Kummer W.. 2015. Cholinergic chemosensory cells of the thymic medulla express the bitter receptor Tas2r131. Int. Immunopharmacol. 29:143–147. 10.1016/j.intimp.2015.06.005 [DOI] [PubMed] [Google Scholar]
- Suh H.W., Lee K.B., Kim K.S., Yang H.J., Choi E.K., Shin M.H., Park Y.S., Na Y.C., Ahn K.S., Jang Y.P., et al. 2015. A bitter herbal medicine Gentiana scabra root extract stimulates glucagon-like peptide-1 secretion and regulates blood glucose in db/db mouse. J. Ethnopharmacol. 172:219–226. 10.1016/j.jep.2015.06.042 [DOI] [PubMed] [Google Scholar]
- Tan X., and Sanderson M.J.. 2014. Bitter tasting compounds dilate airways by inhibiting airway smooth muscle calcium oscillations and calcium sensitivity. Br. J. Pharmacol. 171:646–662. 10.1111/bph.12460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taruno A., Vingtdeux V., Ohmoto M., Ma Z., Dvoryanchikov G., Li A., Adrien L., Zhao H., Leung S., Abernethy M., et al. 2013. CALHM1 ion channel mediates purinergic neurotransmission of sweet, bitter and umami tastes. Nature. 495:223–226. 10.1038/nature11906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tazzeo T., Bates G., Roman H.N., Lauzon A.M., Khasnis M.D., Eto M., and Janssen L.J.. 2012. Caffeine relaxes smooth muscle through actin depolymerization. Am. J. Physiol. Lung Cell. Mol. Physiol. 303:L334–L342. 10.1152/ajplung.00103.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tizzano M., Gulbransen B.D., Vandenbeuch A., Clapp T.R., Herman J.P., Sibhatu H.M., Churchill M.E., Silver W.L., Kinnamon S.C., and Finger T.E.. 2010. Nasal chemosensory cells use bitter taste signaling to detect irritants and bacterial signals. Proc. Natl. Acad. Sci. USA. 107:3210–3215. 10.1073/pnas.0911934107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomás J., Santos C.R., Quintela T., and Gonçalves I.. 2016. “Tasting” the cerebrospinal fluid: another function of the choroid plexus? Neuroscience. 320:160–171. 10.1016/j.neuroscience.2016.01.057 [DOI] [PubMed] [Google Scholar]
- Ueda T., Ugawa S., Yamamura H., Imaizumi Y., and Shimada S.. 2003. Functional interaction between T2R taste receptors and G-protein α subunits expressed in taste receptor cells. J. Neurosci. 23:7376–7380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Upadhyaya J.D., Singh N., Sikarwar A.S., Chakraborty R., Pydi S.P., Bhullar R.P., Dakshinamurti S., and Chelikani P.. 2014. Dextromethorphan mediated bitter taste receptor activation in the pulmonary circuit causes vasoconstriction. PLoS One. 9 10.1371/journal.pone.0110373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voigt A., Hübner S., Lossow K., Hermans-Borgmeyer I., Boehm U., and Meyerhof W.. 2012. Genetic labeling of Tas1r1 and Tas2r131 taste receptor cells in mice. Chem. Senses. 37:897–911. 10.1093/chemse/bjs082 [DOI] [PubMed] [Google Scholar]
- Voigt A., Hübner S., Döring L., Perlach N., Hermans-Borgmeyer I., Boehm U., and Meyerhof W.. 2015. Cre-mediated recombination in Tas2r131 cells—a unique way to explore bitter taste receptor function inside and outside of the taste system. Chem. Senses. 40:627–639. 10.1093/chemse/bjv049 [DOI] [PubMed] [Google Scholar]
- von Moltke J., Ji M., Liang H.E., and Locksley R.M.. 2016. Tuft-cell-derived IL-25 regulates an intestinal ILC2-epithelial response circuit. Nature. 529:221–225. 10.1038/nature16161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H., Yang H., Shivalila C.S., Dawlaty M.M., Cheng A.W., Zhang F., and Jaenisch R.. 2013. One-step generation of mice carrying mutations in multiple genes by CRISPR/Cas-mediated genome engineering. Cell. 153:910–918. 10.1016/j.cell.2013.04.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei M.Y., Xue L., Tan L., Sai W.B., Liu X.C., Jiang Q.J., Shen J., Peng Y.B., Zhao P., Yu M.F., et al. 2015. Involvement of large-conductance Ca2+-activated K+ channels in chloroquine-induced force alterations in pre-contracted airway smooth muscle. PLoS One. 10 10.1371/journal.pone.0121566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wendell S., Wang X., Brown M., Cooper M.E., DeSensi R.S., Weyant R.J., Crout R., McNeil D.W., and Marazita M.L.. 2010. Taste genes associated with dental caries. J. Dent. Res. 89:1198–1202. 10.1177/0022034510381502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wölfle U., Elsholz F.A., Kersten A., Haarhaus B., Müller W.E., and Schempp C.M.. 2015. Expression and functional activity of the bitter taste receptors TAS2R1 and TAS2R38 in human keratinocytes. Skin Pharmacol. Physiol. 28:137–146. 10.1159/000367631 [DOI] [PubMed] [Google Scholar]
- Wölfle U., Elsholz F.A., Kersten A., Haarhaus B., Schumacher U., and Schempp C.M.. 2016. Expression and functional activity of the human bitter taste receptor TAS2R38 in human placental tissues and JEG-3 cells. Molecules. 21 10.3390/molecules21030306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong G.T., Gannon K.S., and Margolskee R.F.. 1996. Transduction of bitter and sweet taste by gustducin. Nature. 381:796–800. 10.1038/381796a0 [DOI] [PubMed] [Google Scholar]
- Workman A.D., Palmer J.N., Adappa N.D., and Cohen N.A.. 2015. The role of bitter and sweet taste receptors in upper irway Immunity. Curr. Allergy Asthma Rep. 15 10.1007/s11882-015-0571-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu S.V., Rozengurt N., Yang M., Young S.H., Sinnett-Smith J., and Rozengurt E.. 2002. Expression of bitter taste receptors of the T2R family in the gastrointestinal tract and enteroendocrine STC-1 cells. Proc. Natl. Acad. Sci. USA. 99:2392–2397. 10.1073/pnas.042617699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu J., Cao J., Iguchi N., Riethmacher D., and Huang L.. 2013. Functional characterization of bitter-taste receptors expressed in mammalian testis. Mol. Hum. Reprod. 19:17–28. 10.1093/molehr/gas040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshikawa K., Nakagawa H., Mori N., Watanabe H., and Touhara K.. 2013. An unsaturated aliphatic alcohol as a natural ligand for a mouse odorant receptor. Nat. Chem. Biol. 9:160–162. 10.1038/nchembio.1164 [DOI] [PubMed] [Google Scholar]
- Zhai K., Yang Z., Zhu X., Nyirimigabo E., Mi Y., Wang Y., Liu Q., Man L., Wu S., Jin J., and Ji G.. 2016. Activation of bitter taste receptors (tas2rs) relaxes detrusor smooth muscle and suppresses overactive bladder symptoms. Oncotarget. 7:21156–21167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C.H., Chen C., Lifshitz L.M., Fogarty K.E., Zhu M.S., and ZhuGe R.. 2012. Activation of BK channels may not be required for bitter tastant-induced bronchodilation. Nat. Med. 18:648–650. [DOI] [PubMed] [Google Scholar]
- Zhang C.-H., Lifshitz L.M., Uy K.F., Ikebe M., Fogarty K.E., and ZhuGe R.. 2013. The cellular and molecular basis of bitter tastant-induced bronchodilation. PLoS Biol. 11 (published erratum appears in PLoS Biol. 2013. 11.) 10.1371/journal.pbio.1001501 [DOI] [PMC free article] [PubMed] [Google Scholar]