Abstract
In light of the known associations between stress, negative affect, and relapse, mindfulness strategies hold promise as a means of reducing relapse susceptibility. In a pilot randomized clinical trial, we evaluated the effects of Mindfulness Based Relapse Prevention (MBRP), relative to a health education control condition (HE) among stimulant dependent adults receiving contingency management. All participants received a 12-week contingency management (CM) intervention. Following a 4-week CM-only lead in phase, participants were randomly assigned to concurrently receive MBRP (n=31) or HE (n=32). Stimulant dependent adults age 18 and over. A university based clinical research center. The primary outcomes were stimulant use, measured by urine drug screens weekly during the intervention and at 1-month post-treatment, negative affect, measured by the Beck Depression Inventory and Beck Anxiety Inventory, and psychiatric severity, measured by the Addiction Severity Index. Medium effect sizes favoring MBRP were observed for negative affect and overall psychiatric severity outcomes. Depression severity changed differentially over time as a function of group, with MBRP participants reporting greater reductions through follow-up (p=0.03; Effect Size=0.58). Likewise, the MBRP group evidenced greater declines in psychiatric severity, (p=0.01; Effect Size=0.61 at follow-up). Among those with depressive and anxiety disorders, MBRP was associated with lower odds of stimulant use relative to the control condition (Odds Ratio= 0.78, p=0.03 and OR=0.68, p=0.04). MBRP effectively reduces negative affect and psychiatric impairment, and is particularly effective in reducing stimulant use among stimulant dependent adults with mood and anxiety disorders.
Keywords: stimulants, mindfulness, treatment outcome, substance abuse, addiction
Introduction
In light of the associations between emotional stress, negative affect, and relapse (Breslin et al. 2002; Marlatt, 1996) coupled with evidence suggesting stress processing deficits in stimulant users (Li and Sinha, 2008), strategies to reduce stress reactivity and improve affect regulation have great potential benefit for stimulant dependent adults (Marcus & Zgierska, 2009). Mindfulness practice is one such approach (Marlatt and Chawla, 2007), which provides skills for coping with cravings and tolerating other forms of psychological discomfort that precipitate relapse (e.g., negative affect, stressful events). By promoting awareness and acceptance of one’s immediate experience, mindfulness may interrupt the automatic conditioned behavioral sequence that ensues from the time of craving to relapse. Mindfulness Based Relapse Prevention (MBRP) (Witkiewitz and Marlatt, 2005) offers a novel approach to processing situational cues that can trigger relapse, monitoring internal reactions to such cues or high risk situations, and using “mindful awareness” to promote positive behavioral choices.
A growing body of literature on meditation based interventions for substance use disorders provides preliminary evidence in support of this approach, with reductions in the use of substances including alcohol, stimulants, cannabis, nicotine, and opiates reported, relative to wait list and supportive or educational control conditions (see Chiessa & Serretti, 2014 for review). Moreover, process variables through which mindfulness interventions affect substance use outcomes have been recently proposed and investigated in preliminary studies, and include increased awareness with corresponding reductions in thought suppression, decreased automatic, non-mindful responding and judgment, and changes in affect regulation which, in turn, alters its relationship to craving (see Witkiewitz et al., 2014).
Initial studies of meditation-based approaches to substance use employed social drinkers or subgroups at risk for alcohol abuse and demonstrated positive effects of meditation interventions on post-treatment alcohol use in these populations (Murphy et al. 1986; Marlatt and George, 1984; Marlatt and Marques, 1977). Subsequently, preliminary data accumulated suggesting that mindfulness based therapies hold promise in reducing negative affect, substance use, and cravings (Brewer et al. 2009; Bowen et al. 2006; Bowen et al. 2009). More recently, Bowen et al. (2014) completed an RCT, in which an 8-week continuing care course of MBRP was compared to cognitive behavioral relapse prevention (RP) and usual treatment (TAU) among 286 adults who successfully completed addiction treatment. In that study, MBRP produced significant reductions in days using substances and heavy drinking at 12-month follow-up, relative to TAU or RP. Reductions in substance use and relapse risk through 6-month follow up were significant among those in MBRP, and comparable to those in RP, relative to TAU. Overall, therefore, MBRP performed comparably to RP as a continuing care approach in key outcome domains during and after treatment, and conferred additional longer-term benefit relative to RP and TAU 1 year after treatment.
To date, apart from the recent RCT conducted by Bowen et al., there are few well-designed efficacy studies of mindfulness interventions for substance users, with extant studies largely limited by the absence of adequate controls, small sample sizes, unmeasured compliance, and a lack of intervention fidelity measurement (Chiessa & Serretti, 2014). Moreover, the majority of studies have targeted alcohol users or combined cohorts of alcohol and drug users, leaving the efficacy of these approaches for stimulant users unknown. Additionally, the largest study of MBRP investigated its utility as a continuing care approach; as such, the impact of mindfulness techniques as part of a primary treatment approach for addictions has yet to be tested.
In light of these considerations, we conducted a pilot randomized clinical trial comparing the incremental efficacy and outcomes of MBRP to a Health Education (HE) control condition for stimulant dependent adults receiving contingency management (CM). Although the use of other platform behavioral interventions (i.e., other than CM) was considered (e.g., CBT, relapse prevention), the CBT and relapse prevention approaches share substantive overlap with the content of the MBRP intervention, which would make interpretation of incremental effects of mindfulness based training difficult to discern. As such, we selected CM as an empirically supported primary behavioral intervention strategy for stimulant users that is entirely distinct in its methodology from MBRP, a study design approach that has been used previously to evaluate the additive effects of CM and CBT or relapse prevention intervention strategies for stimulant users (Rawson et al., 2006). In this initial investigation we predicted that: (1) MBRP would produce greater improvement in negative affect (i.e., depression and anxiety) and overall psychiatric impairment, relative to HE; and (2) MBRP would produce incrementally greater reductions in stimulant use, relative to HE. In light of the selection of MBRP as an approach targeting negative affect among stimulant users, coupled with evidence suggesting that individuals with higher levels of negative affect prior to treatment is associated with better MBRP outcomes (Witkiewitz & Bowen, 2010; Brewer, Bowen, Smith, Marlatt, & Potenza, 2010; Witkiewitz & Black, 2014), a secondary aim was to test whether results differed between patients with and without affective and anxiety disorders. Finally, changes in process measures were examined to ascertain whether putative mechanisms of action of MBRP identified in prior work (Witkiewitz et al., 2014) extend to stimulant using populations.
Method
Participants
The study was conducted at a university based clinical research center. Participants were 63 stimulant dependent adults. The study was approved by the UCLA Institutional Review Board. Participants were recruited through newspaper advertisements, radio ads, and word of mouth. A trained research assistant screened all potential participants for eligibility by phone using a brief script. To be included in the study, participants were required to: (1) be ≥ 18 years old; (2) have a current DSM-IV diagnosis of stimulant dependence; (3) be able to read and understand English; and (4) be physically able to sit for a period of ≥ 30 minutes. Individuals were excluded if they: (1) exhibited medical impairment that compromised their safety as a participant; (2) required medical detoxification from any substances; (3) exhibited psychiatric impairment that warranted hospitalization or primary treatment; or (4) were homeless (unless arrangements were made for recovery home placement). Psychiatric diagnoses were assessed using the MINI International Neuropsychiatric Interview, and the study physician was consulted for a final determination concerning any conditions that compromised eligibility. After complete description of the study to participants, informed consent was obtained.
Participants agreed to: (1) twice weekly contingency management (CM) for 12 weeks; (2) randomization to 8 weekly MBRP or HE sessions; (3) in-person assessments weekly and at 1-month follow-up, with $20 compensation for weekly data collections visit and $30 for follow-up.
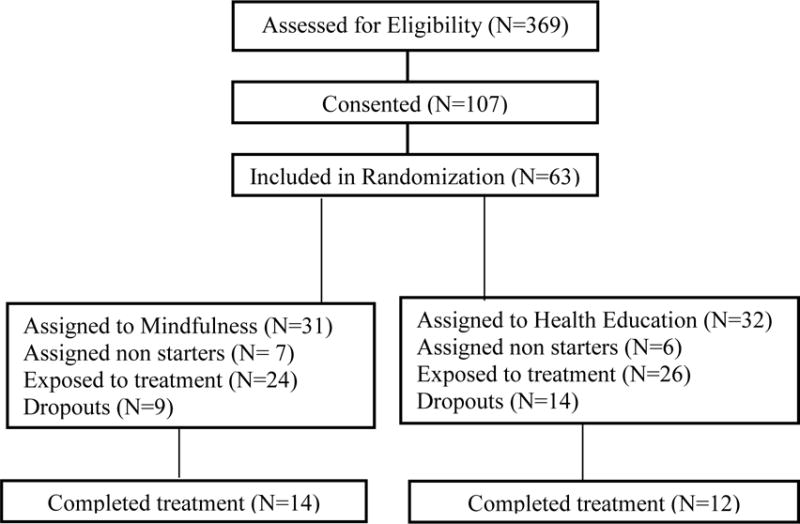
Over the 2-year study period, 369 individuals were screened, of whom 107 signed consent. Of those, 63 individuals completed the 4-week CM lead-In Phase and were assigned randomly into MBRP or HE using a random numbers table. This table was locked in the desk of the study director and after completion of baseline data collection and the CM lead-in, group assignment was given according to this table. Of the 63 individuals, 28 were admitted with methamphetamine dependence and 35 with cocaine dependence. Participants were assigned randomly into either CM + MBRP (n=31) or the CM + HE condition (n=32). Figure 1 depicts the study participant flow. There were no significant group differences in follow-up rates between the two study conditions.
Figure 1.
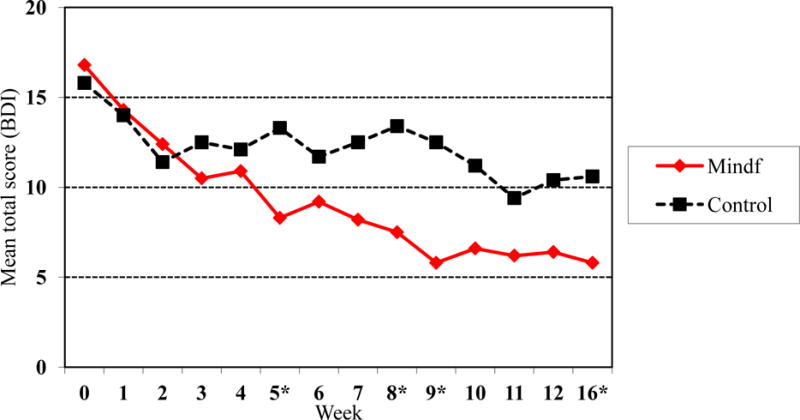
Mean total BDI scores over time by treatment group
Sample Characteristics
Of the 63 participants, 23 were terminated from the study. Eighteen of these 23 participants were terminated for a 2-week absence from protocol participation, four withdrew consent for reasons such as not enough compensation or no longer being interested in participating, and 1 participant was withdrawn by the investigator for tampering with the urine sample. For those who were terminated after randomization, following an intent-to-treat design, attempts were made to continue data collection. There were no statistically significant differences in baseline demographic characteristics, stimulant use frequency, and depression and anxiety symptoms between study completers (n=45) and dropouts (n=18).
The participants ranged in age from 22 to 67 years (M=45.3, SD=8.9), with an average of 12.5 years of education (SD=1.8) (See Table 1). Forty-nine percent of participants identified their drug of choice as cocaine, with the remaining 51% reporting primary methamphetamine use. The MBRP (n=31) and control (n=32) groups were similar in age, ethnicity, educational attainment, gender distribution, employment status, and marital status (see Table 1). Forty-three percent had an Axis I mood or anxiety disorder. The most frequently observed diagnosis was Major Depressive Disorder (MDD), diagnosed in 43% of the sample (MBRP=53% versus HE=33%, p=0.10), followed by Generalized Anxiety Disorder (GAD), observed in 24% of the sample (MBRP=30% versus HE=19%, p=0.33). As such, these two diagnoses were selected as representative affective and anxiety disorders for analysis. All other diagnoses in these categories contained cell sizes with fewer than 5 participants (or less than 10% of those assigned to one or both of the study groups), which was not considered sufficient to warrant subgroup analysis. There were no differences between the study conditions in the prevalence of psychiatric disorders.
Table 1.
Sample characteristics.
| Sample (N=63) |
Mindfulness (n=31) |
Control (n=32) |
|
|---|---|---|---|
| Gender, N (%) | |||
| Male | 45 (71.4) | 21 (70) | 24 (75) |
| Female | 18 (28.6) | 10 (30) | 8 (25) |
| Age, M(sd) | 45.3 (8.9) | 44.6 (9.1) | 46.1 (8.8) |
| Yrs education, M(sd) | 12.6 (1.8) | 12.6 (1.3) | 12.5 (1.9) |
| Ethnicity, N (%) | |||
| Hispanic | 13 (20.6) | 7 (22.6) | 6 (18.8) |
| African-American | 28 (44.4) | 12 (38.7) | 16 (50.0) |
| White (non-Hisp) | 19 (30.2) | 9 (29.0) | 10 (31.2) |
| Other | 3 (4.7) | 3 (9.7) | 0 |
| Current employment, N (%) | |||
| Full time | 2 (3.2) | 1 (3.3) | 1 (3.1) |
| Part time | 12 (19.0) | 8 (26.6) | 4 (12.5) |
| Student | 2 (3.2) | 0 (0) | 2 (6.3) |
| Retired/disability/Homemaker | 18 (28.6) | 8 (26.6) | 10 (31.2) |
| Unemployed | 28 (44.4) | 13 (43.3) | 15 (46.9) |
| Marital status, N (%) | |||
| Legally married/Living with partner | 8 (12.7) | 4 (12.9) | 4 (12.5) |
| Separated/Divorced/Widowed | 15 (23.8) | 8 (25.8) | 7 (21.9) |
| Never married | 40 (63.5) | 19 (61.3) | 21 (65.6) |
| Primary drug, N (%) | |||
| Methamphetamine* | 28 (44.4) | 14 (45.2) | 14 (43.8) |
| Cocaine* | 35 (55.6) | 17 (54.8) | 14 (43.8) |
| Number of days using stimulants in past 30, M(SD) * | 5.3 (7.3) | 5.8 (7.2) | 4.8 (7.5) |
| BDI Score, M (SD) *+ | 15.1 (11.5) | 14.5 (9.6) | 15.6 (12.9) |
| BAI Score, M (SD) *+ | 9.8 (9.1) | 9.1 (8.7) | 10.4 (9.6) |
Score at baseline;
Beck Depression Inventory, Beck Anxiety Inventory
Procedure
Design
Participants were assigned to either CM+ MBRP or CM+ HE, with repeated assessments at baseline, weekly during the 12 week intervention phase, and at 1-month follow-up. Following the CM 4-week lead-in, participants were sequentially randomized by cohorts into either the 8-week MBRP or HE condition. CM was delivered concurrently with the experimental and control conditions over the remaining 8-week trial period.
Termination from the study could be a result of: (1) study completion; (2) missing two consecutive data collection visits; or (3) missing either 2 consecutive group interventions (MBRP or HE) or four consecutive urine samples. Therefore, a consistent 2-week absence from protocol participation was the criterion for study termination.
Interventions
Contingency Management
Twice-weekly CM was delivered utilizing the fishbowl method (Petry, 2006); during each visit participants provided a urine sample and meet briefly with the CM technician. Using the fishbowl technique, participants can earn increasing numbers of draws from a bowl containing 100 plastic chips that indicate different values: (1) 50 chips were marked with a motivational saying (i.e., “good job”); (2) 30 chips indicated the opportunity to select a voucher of relatively low value ($5); (3) 15 chips indicated the opportunity to select a voucher of medium value ($20); and (4) 5 chips indicating the opportunity to select a voucher of high value ($50). When samples were missed or positive for stimulants, the number of draws was ‘reset’ to a lower level.
Mindfulness Based Relapse Prevention
MBRP was delivered weekly in group format over 8 weeks. All sessions began with a guided meditation, followed by homework review and relapse prevention exercises, guided by the MBRP manual (Bowen et al. 2011). Goals of MBRP include increasing awareness of relapse triggers, interrupting “automatic” behavior sequences to promote mindful responses (versus “reactions”) to triggers and cravings, and practicing nonjudgmental awareness of one’s moment-to-moment experience. Participants were given meditation exercise CDs for between-session practice and a log to record time spent practicing. With consultation from research experts in MBRP (Marlatt, personal communication; Brewer, personal communication), sessions were modified from the 120 minute duration indicated in the MBRP manual to 75 minutes. To achieve this, meditation exercises were shortened; thus, none of the manual’s therapeutic content, topics, or themes were omitted. This modification was critical to achieving engagement, as pilot testing of the intervention prior to initiating the trial indicated that the 120 minute sessions adversely affected engagement. Shortening the sessions improved engagement substantially.
The master’s level study therapist, who was formally trained prior to this study in Mindfulness Based Stress Reduction and had over 10 years of experience as a mindfulness practitioner, participated in a 2-day, manualized MBRP training seminar (Witkiewitz et al. 2005). The seminar included didactic material, role plays, and supervised practice delivering the manualized meditation exercises. The MBRP seminar trainer provided weekly supervision to the study therapist during initial phases of the trial; subsequently, the P.I. conducted ongoing fidelity monitoring on a random 50% of sessions using the MBRP Adherence Scale (Chawla et al. 2010) and provided feedback as needed to the study therapist.
Health Education
HE participants received 8 weekly manualized, group health psychoeducation sessions of equivalent duration to MBRP. The intervention comprised a multimedia educational program addressing various health and wellness topics including the 6 dimensions of health (e.g., intellectual, social, emotional, physical, environmental, and spiritual) and specific topics within these areas, including nutrition, dental care, acupuncture, skin care, cancer screening, sleep hygiene, physical activity, and traffic safety. Content was adapted from a wellness manual (Kinnunen et al. 2008) used in a study of exercise for smoking cessation. The HE facilitator held a master’s degree in public health, and was a certified health educator.
Fidelity Assessments
Standardized fidelity ratings were made on 50.8% of the 59 MBRP sessions. These showed acceptable to excellent fidelity on all 4 domains of the MBRP Adherence and Competence Scale, e.g., mean % MBRP components delivery (85%), Discussion of Key Concepts (100%), Therapist Style/Approach (4.5 on a scale from 1 to 5), and Overall Therapist Performance (4.2 on a scale from 1 to 5).
Measures
Within one week of obtaining informed consent, a trained research assistant administered the Mini-International Neuropsychiatric Interview (MINI) (Sheehan et al. 1998), a brief structured diagnostic interview for assessing DSM-IV psychiatric disorders. Diagnoses of stimulant dependence and depressive and anxiety disorders were made based upon the MINI. Eligible participants with stimulant dependence initiated the 4-week CM lead-in phase, and within one week, completed additional assessments described below.
Stimulant use was assessed weekly using urine toxicology assays. All samples were immediately analyzed for the presence of amphetamine, methamphetamine, and cocaine metabolites (benzoylecognine; BE) using enzyme immunoassay test (EMIT) procedures. A 300 ng/ml BE cutoff was used to define a positive sample. If urine samples were missed, refused, or determined invalid (via quality control procedures within the urine assay), the sample was considered positive, a commonly used procedure in clinical trials targeting substance use disorders (see Ling et al., 2009). The Addiction Severity Index (ASI), administered at baseline, treatment-end, and follow-up, provided data concerning days of stimulant use in the past 30, as well as psychiatric and drug severity composite scores (McLellan et al. 1992).
The Beck Depression Inventory-II (Beck, 1967) was administered at baseline, weekly during treatment, and at follow-up. Anxiety severity was assessed using the Beck Anxiety Inventory (Beck and Steer, 1990) was used to quantify anxiety severity over the past week.
As part of their weekly therapy homework, participants in the MBRP condition were given a mindfulness practice log to complete, in which they recorded the number of minutes spent practicing mindfulness meditations, which were provided to them on a CD for take-home practice. At the end of the trial, weekly minutes logged by participants were summed for descriptive purposes, as an indicator of feasibility and acceptability of the intervention in the target population.
Several measures of putative psychological mechanisms of action of MBRP were employed (see Witkiewitz, Bowen, Harrop, Douglas, Enkema, & Sedgwick, 2014). Emotion regulation was assessed using the Difficulty in Emotion Regulation Scale (DERS) (Gratz and Roemer, 2004), a 36-item self-report measure. The DERS assesses multiple aspects of affective dysregulation, including awareness, understanding, and acceptance of emotions on a Likert scale; global scores range from 36 to 180. Higher scores on the DERS indicate greater difficulties with emotion regulation. The White Bear Suppression Inventory (WBSI) (Wegner and Zanakos, 1994) was used to measure thought suppression, or deliberate attempts to avoid unwanted thoughts. Through its emphasis on acceptance, MBRP promotes reductions in thought suppression. Acquisition of mindfulness skills was assessed at baseline and treatment-end using the Five Factor Mindfulness Questionnaire (FFMQ) (Baer et al. 2004), a 39-item self-report measure. Items are rated on a 5-point Likert-type scale. Higher scores indicate greater acquisition of mindfulness skills.
Data Analyses
The primary outcome was the likelihood of producing stimulant-free urines over the course of the 8-week intervention. Secondary outcomes included depression severity, measured by BDI score, anxiety severity, as indicated by BAI score, and psychiatric and addiction severity as measured by ASI composite scores in the psychiatric and drug domains. A generalized linear model (with generalized estimating equations: GEE) was used to assess differential changes over time in these secondary outcomes.
To examine the impact of MBRP on putative mechanisms of action of the intervention, process measures were administered at baseline and weekly throughout the intervention phase. Changes in emotional regulation (measured by the DERS), thought suppression (measured by the WBSI), and mindfulness skills (measured by the FFMQ) were evaluated as a function of intervention condition.
To test the hypothesis that MBRP would produce reductions in stimulant use among those with MDD and GAD, multivariate logistic regression analyses were conducted, controlling for demographic variables, baseline stimulant use, and alcohol dependence, each of which have been shown to be associated with treatment outcomes among stimulant users (see Glasner-Edwards et al., 2009; Reiber et al., 2000) with the odds of producing a stimulant free urine sample during the intervention phase as the primary outcome. The model tested the interaction of diagnosis status (coded dichotomously for the presence or absence of a diagnosis of MDD or GAD, respectively, for each of the analyses) × treatment week × treatment group. Alpha was set at .05 for all statistical analyses.
Results
The mean proportion of stimulant-free urine samples provided during the 8-week intervention phase did not differ between those who received MBRP relative to HE (.73 versus .70, respectively, p>0.05) (see Table 3). Likewise, no group effect was observed in the odds of stimulant-free urines over time (OR<1). However, in mixed model analyses examining stimulant use outcomes as a function of group, time, and psychiatric diagnosis, two three-way interactions between group × time × psychiatric diagnostic status were observed. For those with MDD, after controlling for GAD, alcohol dependence, and demographics, MBRP conferred a significantly greater benefit, reducing the likelihood of stimulant use (OR = 0.78, p = 0.03, η2=0.20), relative to HE. Similarly, among the subgroup with GAD, after controlling for MDD, alcohol dependence, and demographics, MBRP participation effectively reduced the odds of stimulant use significantly over time (OR = 0.68, p = 0.04; η2=0.13), relative to HE.
Table 3.
Stimulant use and negative affect outcomes as a function of treatment condition.
| Baseline (n=63) |
Week 12 (n=43) |
Week 16 (n=44) |
||
|---|---|---|---|---|
| N (%) stimulant free UDS | ||||
| Overall sample | 41 (65.0%) | 28 (64.1%) | 26 (59.1%) | |
| MBRP | ||||
| Individuals with Major Depressive Disorder | 62.1% | 87.5% | 100% | |
| Individuals with Generalized Anxiety Disorder | 40.0% | 66.6% | 96.0% | |
| Health ED | ||||
| Individuals with Major Depressive Disorder | 60.0% | 62.5% | 50.0% | |
| Individuals with Generalized Anxiety Disorder | 33.3% | 33.3% | 60.0% | |
| Secondary outcomes M(SD) | ||||
| Depression (BDI) | ||||
| Overall sample | 15.1 (11.5) | 8.7 (11.2) | 6.8 (7.9) | |
| MBRP (49.2%) | 14.5 (9.6) | 5.3 (7.2) | 4.7 (6.9) | |
| Health Ed (50.8%) | 15.6 (12.9) | 12.0 (13.4) | 9.0 (8.5) | |
| Anxiety (BAI) | ||||
| Overall sample | 9.8 (9.1) | 6.8 (11.8) | 5.9 (9.2) | |
| MBRP(49.2%) | 9.1 (8.7) | 5.2 (9.2) | 3.2 (7.4) | |
| Health Ed (50.8%) | 10.4 (9.6) | 8.3 (13.9) | 9.0 (10.2) | |
ASI-drug severity scores over time did not differ significantly as a function of group (p>0.05).
Depression severity, measured by the BDI-II, decreased significantly during and after treatment for those in the MBRP, relative to HE, evidenced by a significant group × time interaction (χ2=2.88, df=1, p=0.04, d = 0.58; see Figure 1). Pairwise comparisons at mid-treatment (t=−2.09, df=32, p=0.02), end-of-treatment (t=−1.92, df=33, p=0.03), and 1 month post-treatment (t=−2.17, df=42, p=0.01) revealed significantly lower BDI-II scores among MBRP participants. Although inspection of Figure 2 suggests that anxiety decreased to a greater extent over time for the MBRP group, the group × time interaction failed to achieve significance, despite a larger effect size (χ2=1.53, df=1, p =0.10, d = 0.72). Again, however, pairwise contrasts, while not significant at mid- and end-of-treatment, showed an advantage of MBRP on anxiety severity at 1-month follow-up (t=−2.34, df=28, p=0.01). Additionally, the ASI psychiatric severity composite improved significantly over time for those in MBRP, relative to HE (χ2=3.07, df=1, p =0.04, d = 0.61; see Figure 3). Pairwise contrasts were significant only at 1-month follow-up (t=−2.33, df=41, p=0.01), but not at mid- or end-of-treatment.
Figure 2.
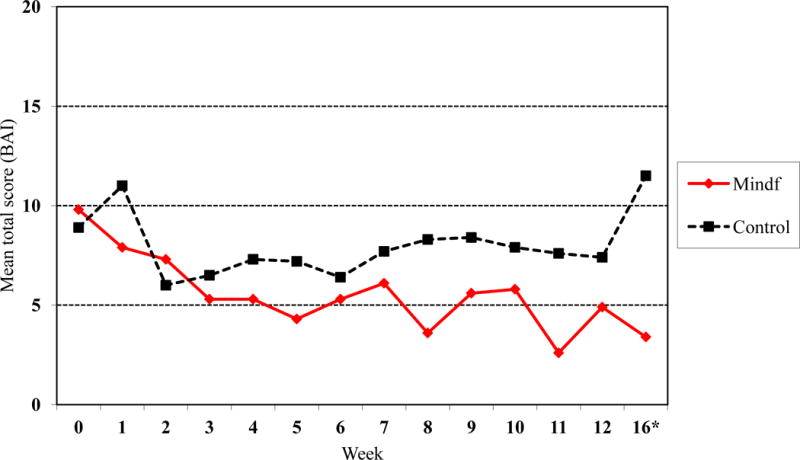
Mean total BAI scores across time by treatment group
Figure 3.
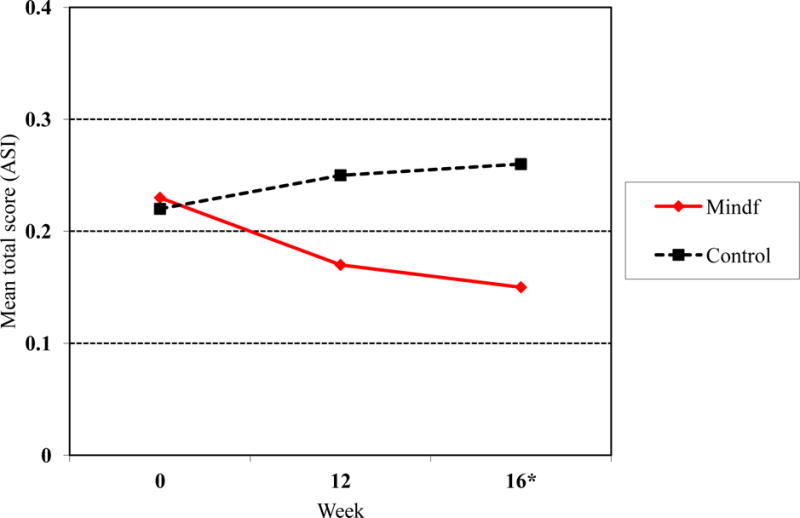
Mean ASI psychiatric composite scores at weeks 0, 12 and 16 by treatment group.
Changes in potential mechanisms of action of MBRP were examined using GEE models. Analysis of changes in the FFMQ failed to reveal a significant group × time interaction effect (χ2<1); however, pairwise comparisons revealed that MBRP participants had significantly higher scores at mid-treatment (t=2.32, df=41, p=0.01). Though a difference was also observed at treatment-end, the effect did not achieve significance (t=1.36, df=42, p=0.09). Likewise, despite a non-significant group × time interaction on the DERS, the MBRP group had significantly lower scores (indicating less difficulty in emotion regulation) at both treatment-end (t=−2.02, df=41, p=0.02) and follow-up (t=−1.93, df=42, p=0.03). On the WBSI, though MBRP participant scores changed in the predicted direction, relative to those in HE, neither the group × time interaction nor any of the pairwise comparisons were significant.
Participants in the MBRP group reported practicing mindfulness on an average of 18.5 days over the 8-week intervention (SD = 16.0; range 0–49). On average, over the 8-week period, participants practiced for a total of 145.3 minutes (SD = 287.0; range 0–1188).
Discussion
Although previous studies have supported the use of mindfulness interventions for individuals with depression (Ma and Teasdale, 2004; Segal et al. 2010) and anxiety (Kabat-Zinn et al. 1992; Hoffman et al. 2010) and to reduce relapse in individuals with addicted populations (Bowen et al. 2009; Bowen et al. 2014; Garland et al. 2010), this is the first RCT evaluating the efficacy of MBRP in conjunction with contingency management as a primary intervention approach for stimulant dependence. Findings from this study extend prior literature on the efficacy of mindfulness for depression, in demonstrating that therapeutic effects generalize to populations with addictions, as greater improvements in depression symptoms were demonstrated in individuals randomized to MBRP relative to HE. Likewise, greater improvements in overall psychiatric severity were observed among those who received MBRP. Though the group × time interaction for anxiety symptoms was not significant, a medium effect size was observed for changes in anxiety severity among those who received MBRP, indicating a clinically significant impact of the intervention. Findings are consistent with documented benefits of mindfulness meditation in facilitating affect regulation (Hoffman et al. 2010).
MDD and GAD were present in 43% and 24% of the study sample, respectively, and depression severity scores were clinically significant at baseline. Given the well established contribution of negative affective states to relapse risk, coupled with the documented efficacy of mindfulness strategies for improvement in depressive and anxiety syndromes in non-addicted populations (see Hollon & Ponniah, 2010; Marchand, 2012), it was hypothesized that MBRP would produce greater reductions in stimulant use among those with affective and anxiety disorders, relative to HE. Consistent with these predictions, despite the absence, overall, of significant between-group differences in stimulant use, those who were diagnosed with either MDD or GAD at baseline who received MBRP were less likely to use stimulants over the course of treatment, relative to those randomized to HE. These findings suggest that the utility of mindfulness-based interventions for individuals with addictions may be greatest for those with clinically significant negative affect. This effect may be explained, in part, by the acquisition of coping skills emphasizing acceptance of negative affect and discomfort in MBRP, which in turn, may replace maladaptive self-medication behaviors. An important aspect of mindfulness training is learning to tolerate negative affect rather than avoiding it; this may be particularly useful for individuals who are accustomed to responding to distress with substance use (Bowen et al. 2014).
In the present study, those who received mindfulness training showed evidence of skills acquisition; not only did they report practicing mindfulness exercises between sessions, but some evidence of mindfulness-specific process changes emerged. Group differences in measures of emotional regulation and acquisition of mindfulness skills emerged at mid- and end-of-treatment, suggesting that stimulant users have the capacity to learn and apply mindfulness skills, and to benefit from the emphasis on coping with negative affect through acceptance, self-observation, and mindful awareness. Though the overall effects of intervention group on mindfulness process variables were not significant over time, the between-group differences observed at mid- and end-of-treatment suggest that the MBRP intervention impacted mindfulness-specific psychological processes among stimulant dependent adults.
Several limitations of the present study warrant comment. As a pilot study, this investigation is limited by small sample size; as such, replication of the findings with a larger population of stimulant users is warranted to confirm the reliability of the observed effects. In addition, though subgroup analyses revealed that concurrent psychiatric diagnoses of MDD and GAD are important predictors of treatment response, no distinction was made between substance-induced depression or anxiety versus substance-independent symptoms due to limitations of the diagnostic instrument. Future studies should assess diagnoses more thoroughly to elucidate the diagnostic features of drug users who can benefit the most from mindfulness-based interventions. Moreover, because of limited cell sizes of individuals with mood and anxiety disorders other than MDD and GAD, analyses of other diagnostic groups could not be undertaken, leaving the generalizability of the subgroup effects of MBRP to other mood and anxiety disorders unknown. In addition, although attrition rates were comparable to those observed in other studies of CM and skills-based behavioral interventions such as CBT among stimulant users (Rawson et al., 2006), dropout may have confounded interpretation of stimulant use and other outcomes, as those who dropped out may have done so because they were doing poorly, leaving a more homogenous, motivated, treatment-compliant group for comparisons. These concerns, however, are mitigated by the observation that the dropouts versus completers did not differ on key outcome measures at baseline, coupled with the intent-to-treat design employed in this investigation. Finally, because it is well established that the platform intervention (CM) is robust and efficacious for stimulant users, the study may have been limited by a ceiling effect of CM on stimulant use outcomes. Future studies pairing MBRP with less potent behavioral interventions for addictions should advance our understanding of the potential for mindfulness-based interventions to impact drug use outcomes directly.
Results of this pilot RCT comparing MBRP to a control intervention indicate preliminary evidence for the benefit of MBRP as an intervention for stimulant users. Findings suggest that: (1) stimulant users can engage in mindfulness and practice mindfulness meditation in between sessions; (2) MBRP yields improvement in depressive and anxiety symptoms and reduces overall severity of psychiatric impairment among stimulant dependent adults; (3) MBRP is particularly helpful to stimulant users with MDD or GAD in reducing stimulant use; and (4) Stimulant users may learn to regulate negative affect and practice mindful living, suggesting that the putative mechanisms of action of mindfulness interventions may be the same in drug using populations as those observed in non-addicted clinical populations. Future larger-scale controlled trials employing MBRP for addicted populations can further our understanding of the efficacy and key ingredients of mindfulness-based interventions among substance users with and without psychiatric comorbidities.
Table 2.
Participant Flow through the Study.
|
Acknowledgments
The authors would like to thank Anne Bellows Lee, Hailey Winetrobe, Megan Holmes, Mary Olaer, and all of the research staff at the UCLA ISAP Clinical Research Center. We also thank Alan Marlatt, Katie Witkiewitz, Neharika Chawla, Sarah Bowen, and Judson Brewer for valuable input during the development and implementation phases of the project. We appreciate Elizabeth Suti’s contribution to the study as the mindfulness interventionist. The research presented in this paper was supported by grants R21 DA029255, K23 DA020085 and T32 DA07272-21 from the National Institute on Drug Abuse.
Footnotes
Conflict of Interest: No conflict exists. All authors of this paper declare that they have no conflict of interest.
References
- Baer RA, Smith GT, Allen KB. Assessment of mindfulness by self-report: the Kentucky Inventory of Mindfulness Skills. Assessment. 2004;11(3):191–206. doi: 10.1177/1073191104268029. [DOI] [PubMed] [Google Scholar]
- Beck AT. Depression: Clinical, experimental, and theoretical aspects. New York: Harper and Row; 1967. [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck Anxiety Inventory. Psychological Corporation; San Antonio, TX: 1990. [Google Scholar]
- Breslin FC, Zack M, McMain S. An information-processing analysis of mindfulness: implications for relapse prevention in the treatment of substance abuse. Clinical Psychology: Science and Practice. 2002;9(3):275–299. [Google Scholar]
- Bowen SK, Witkiewitz K, Dillworth TM, Chawla N, Simpson TL, Ostafin BD. Mindfulness meditation and substance use in an incarcerated population. Psychology of Addictive Behaviors. 2006;20(3):343–347. doi: 10.1037/0893-164X.20.3.343. [DOI] [PubMed] [Google Scholar]
- Bowen S, Chawla N, Collins S, Witkiewitz K, Hsu S, Grow J. Mindfulness-based relapse prevention for substance use disorders: a pilot efficacy trial. Substance Abuse. 2009;30(4):205–305. doi: 10.1080/08897070903250084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Chawla N, Marlatt GA. Mindfulness-Based Relapse Prevention for Addictive Behaviors: A Clinician’s Guide. Guilford Press; 2011. [Google Scholar]
- Bowen S, Witkiewitz K, Clifasefi SL, Grow J, Chawla N, Hsu SH. Relative Efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: a randomized clinical trial. JAMA Psychiatry. 2014;71(5):547–556. doi: 10.1001/jamapsychiatry.2013.4546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Sinha R, Chen JA, Michalsen RN, Babuscio TA, Nich C. Mindfulness training and stress reactivity in substance abuse: results from a randomized, controlled stage I pilot study. Substance Abuse. 2009;30(4):306–317. doi: 10.1080/08897070903250241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Bowen S, Smith JT, Marlatt GA, Potenza MN. Mindfulness-based treatments for co-occurring depression and substance use disorders: what can we learn from the brain? Addiction. 2010;105(10):1698–1706. doi: 10.1111/j.1360-0443.2009.02890.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chawla N, Collins SE, Bowen S, Hsu S, Grow J, Douglas SA, Marlatt GA. The Mindfulness-Based Relapse Prevention Adherence and Competence Scale: Development, Interrater Reliability and Validity. Psychotherapy Research. 2010;20(4):388–397. doi: 10.1080/10503300903544257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiessa A, Serretti A. Are mindfulness-based interventions effective for substance use disorders? A systematic review of the evidence. Substance Use and Misuse. 2014;49(5):492–512. doi: 10.3109/10826084.2013.770027. [DOI] [PubMed] [Google Scholar]
- Garland EL, Gaylord SA, Boettiger CA, Howard MO. Mindfulness training Modifies cognitive, affective, and physiological mechanisms implicated in alcohol dependence: results of a randomized, controlled pilot trial. Journal of Psychoactive Drugs. 2010;42(2):177–192. doi: 10.1080/02791072.2010.10400690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasner-Edwards S, Marinelli-Casey P, Hillhouse M, Ang A, Mooney LJ, Rawson R, Methamphetamine Treatment Project Corporate Authors Depression among methamphetamine users: Association with outcomes from the Methamphetamine Treatment Project at 3-year follow-up. Journal of Nervous and Mental Disease. 2009;197(4):225–231. doi: 10.1097/NMD.0b013e31819db6fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–54. [Google Scholar]
- Hoffman SG, Sawyer AT, Oh D. The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78(2):169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollon SD, Ponniah K. A review of empirically supported psychological therapies for mood disorders in adults. Depression and Anxiety. 2010;27(10):891–932. doi: 10.1002/da.20741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J, Massion AO, Kristeller J, Peterson LG, Fletcher KE, Pbert L. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. American Journal of Psychiatry. 1992;149(7):936–943. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- Kinnunen T, Leeman RF, Korhonen T, Quiles ZN, Terwal DM, Garvey AJ, Hartley HL. Exercise as an adjunct to nicotine gum in treating tobacco dependence among women. Nicotine Tobacco Research. 2008;10(4):689–703. doi: 10.1080/14622200801979043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C-SR, Sinha R. Inhibitory control and emotional stress regulation: Neuroimaging evidence for frontal–limbic dysfunction in psycho-stimulant addiction. Neuroscience and Biobehavioral Reviews. 2008;32(3):581–597. doi: 10.1016/j.neubiorev.2007.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ling W, Hillhouse M, Domier C, Doraimani G, Hunter J, Thomas C, Bilangi R. Buprenorphine tapering schedule and illicit opioid use. Addiction. 2009;104(2):256–265. doi: 10.1111/j.1360-0443.2008.02455.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma SH, Teasdale JD. Mindfulness-based cognitive therapy for depression: replication And exploration of differential relapse prevention effects. Journal of Consulting and Clinical Psychology. 2004;72(1):31–40. doi: 10.1037/0022-006X.72.1.31. [DOI] [PubMed] [Google Scholar]
- Marchand WR. Mindfulness-based stress reduction, mindfulness-based cognitive therapy, and Zen meditation for depression, anxiety, pain, and psychological distress. Journal of Psychiatric Practice. 2012;18(4):233–252. doi: 10.1097/01.pra.0000416014.53215.86. [DOI] [PubMed] [Google Scholar]
- Marcus MT, Zgierska A. Mindfulness-based therapies for substance use disorders: part 1. Substance Abuse. 2009;30(4):263–265. doi: 10.1080/08897070903250027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA, Marques JK. Meditation, self-control, and alcohol use. In: Stuart RB, editor. Behavioral self-management: Strategies, techniques, and outcomes. New York: Brunner/Mazel; 1977. pp. 117–153. [Google Scholar]
- Marlatt GA, George WH. Relapse prevention: introduction and overview of the model. British Journal of Addiction. 1984;79(3):261–273. doi: 10.1111/j.1360-0443.1984.tb00274.x. [DOI] [PubMed] [Google Scholar]
- Marlatt GA. Taxonomy of high-risk situations for alcohol relapse: evolution and development of a cognitive-behavioral model. Journal of Addiction. 1996;91(Suppl):S37–49. [PubMed] [Google Scholar]
- Marlatt GA, Chawla N. Meditation and alcohol use. Southern Medical Journal. 2007;100(4):451–453. doi: 10.1097/SMJ.0b013e3180381416. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati H, Argeriou M. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Murphy TJ, Pagano RR, Marlatt GA. Lifestyle modification with heavy alcohol drinkers: effects of aerobic exercise and meditation. Addictive Behaviors. 1986;11(2):175–86. doi: 10.1016/0306-4603(86)90043-2. [DOI] [PubMed] [Google Scholar]
- Petry NM. Contingency management treatments. British Journal of Psychiatry. 2006;189(2):97–98. doi: 10.1192/bjp.bp.106.022293. [DOI] [PubMed] [Google Scholar]
- Rawson RA, McCann MJ, Flammino F, Shoptaw S, Miotto K, Reiber C, Ling W. A comparison of contingency management and cognitive-behavioral approaches for stimulant-dependent individuals. Addiction. 2006;101(2):267–274. doi: 10.1111/j.1360-0443.2006.01312.x. [DOI] [PubMed] [Google Scholar]
- Reiber C, Galloway G, Cohen J, Hsu JC, Lord RH. A descriptive analysis of participant characteristics and patterns of substance use in the CSAT methamphetamine treatment project: the first six months. Journal of Psychoactive Drugs. 2000;32(2):183–191. doi: 10.1080/02791072.2000.10400227. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Bieling P, Young T, MacQueen G, Cooke R. Antidepressant monotherapy vs sequential pharmacotherapy and mindfulness-based cognitive therapy, or placebo for relapse prophylaxis in recurrent depression. Archives of General Psychiatry. 2010;67(12):1256–1264. doi: 10.1001/archgenpsychiatry.2010.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- Wegner DM, Zanakos S. Chronic thought suppression. Journal of Pers onality. 1994;62:615–640. doi: 10.1111/j.1467-6494.1994.tb00311.x. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA, Walker D. Mindfulness-based relapse prevention for alcohol and substance use disorders. Journal of Cognitive Psychotherapy. 2005;19(3):211–228. [Google Scholar]
- Witkiewitz K, Black DS. Unresolved issues in the application of mindfulness-based interventions for substance use disorders. Substance Use and Misuse. 2014;49(5):601–604. doi: 10.3109/10826084.2014.852797. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S, Harrop EN, Douglas H, Enkema M, Sedgwick C. Mindfulness- based treatment to prevent addictive behavior relapse: theoretical models and hypothesized mechanisms of change. Subst Use and Misuse. 2014;49(5):513–524. doi: 10.3109/10826084.2014.891845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S. Depression, Craving and Substance Use Following a Randomized Trial of Mindfulness-Based Relapse Prevention. Journal of Consulting and Clinical Psychology. 2010;78(3):362–374. doi: 10.1037/a0019172. [DOI] [PMC free article] [PubMed] [Google Scholar]


