Abstract
Targeting hyperactive MAPK signaling has proven to be an effective treatment for a variety of different cancers. Responses to the BARF inhibitors vemurafenib or dabrafenib and MEK inhibitors trametinib or cobimentinib are however transient and complete remission is rarely observed; rather outgrowth of resistant clones within progressed tumors appears inevitable. These resistant tumors display great heterogeneity, which poses a major challenge to any salvage therapy. Recent focus has therefore been on the early dynamics of inhibitor response during tumor regression. During this time cells can persist in an adapted tolerant state, which results in a phase of non-mutational drug-tolerance. Here we discuss how inhibition of the MAPK-pathway leads to an adaptive rewiring that evolves from the relief of immediate negative feedback loops to short-term gene expression changes and adaptation of intracellular signaling. Tolerance can also be mediated by external signaling from the tumor microenvironment, which itself adapts upon treatment and the selection for cells with an innate drug-tolerant phenotype. In pre-clinical models, combination with RTK inhibitors (lapatinib, dasatinib), HDAC inhibitors (vorinostat, entinostat) or drugs targeting cancer specific mechanisms such as nelfinavir in melanoma can overcome this early tolerance. A better understanding of how non-mutational tolerance is created and supported may hold the key to better combinational strategies that maintain drug sensitivity.
Background
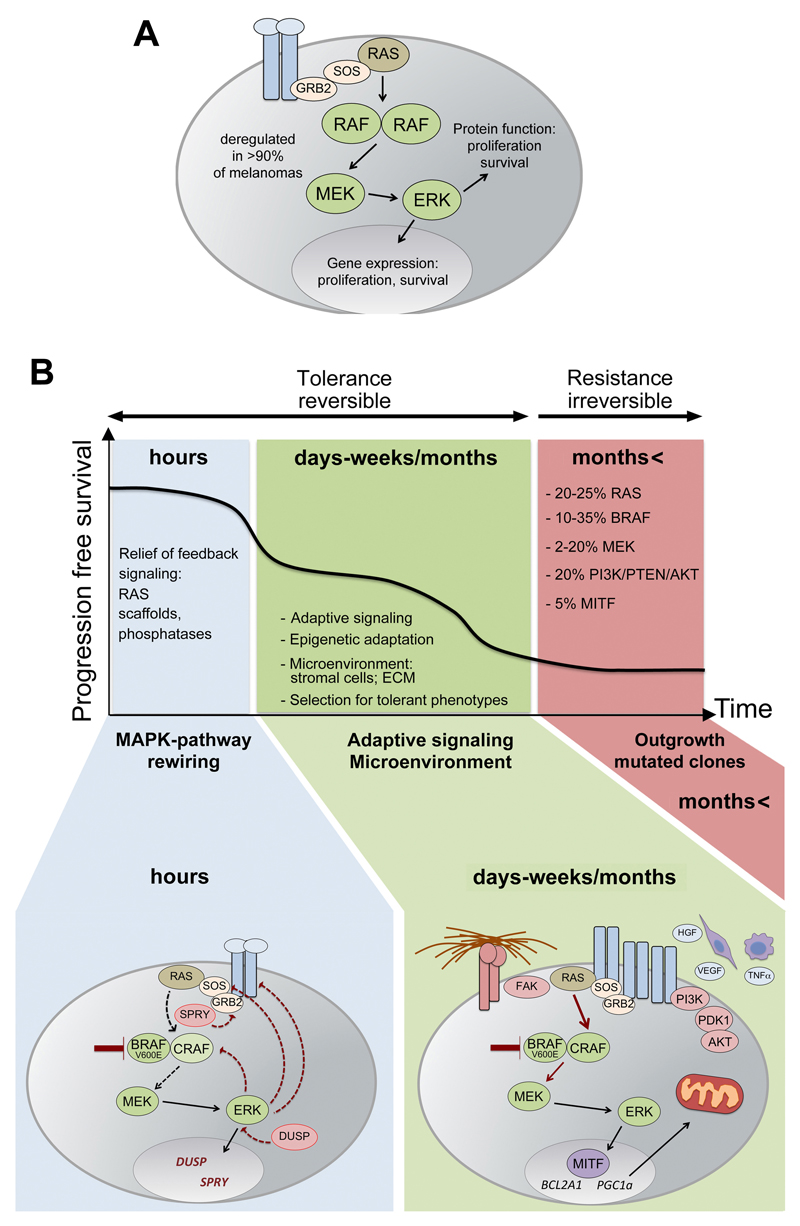
The ERK/MAPK pathway consisting of the small GTPases of the RAS family (e.g. HRAS, KRAS, NRAS), and the families of RAF, MEK and ERK kinases (ARAF, BRAF, CRAF, MEK1 and 2, and ERK1 and ERK2; Fig. 1A) is notoriously deregulated in a variety of cancers, which is why it is at the center of development of small molecule inhibitors for targeted cancer therapy (1). Under physiological conditions, the MAPK pathway regulates growth and survival downstream of many growth factor and cytokine receptors (1, 2). Receptor activation by growth factors causes a number of events including RAS activation through the guanine nucleotide exchange factor SOS. Active RAS can recruit RAF kinases to the membrane, thereby facilitating their dimerization, phosphorylation and activation (3). Active RAF then phosphorylates and activates the dual-specific kinase MEK, which phosphorylates ERK on serine and tyrosine. Phosphorylated, active ERK phosphorylates substrates in the cytoplasm, but after nuclear translocation it also phosphorylates transcription factors, often regulating genes required for survival and growth (Fig. 1A).
Figure 1.
Dynamic responses to MAPK pathway inhibition. A, the MAPK pathway is controlled through membrane receptors, but in cancer mutations in RAS, BRAF or MEK lead to its deregulation. B, following on from immediate responses to MAPK inhibitor therapy is a phase of reversible non-mutational tolerance, before mutated resistant clones irreversibly reestablish tumor growth. Within hours of MAPK inhibition, pathway rewiring will lead to the disturbance of feedback signals allowing ERK activity to recover. Following on from this, intracellular signaling pathways rewire, partly due to extracellular signals leading to the adaption of cancer cells to the drug insult.
Due to its importance in driving growth and survival, it is not surprising that the MAPK pathway is often exploited by transformed cancer cells in order to proliferate without the need of external stimuli. RAS is mutated in ~30% of all cancers and more specifically the RAF kinase BRAF is mutated in ~50 of melanomas, but also ~10% of colorectal cancer and 11% in ovarian cancers. Inhibiting mutated RAS has proved difficult but effective drugs inhibiting BRAFV600E (the most prominent constitutively active BRAF mutant) or MEK in specific BRAF mutant melanoma have achieved FDA approval. Today, combination therapies using the BRAF inhibitor vemurafenib and the MEK inhibitor cobimetinib, or likewise dabrafenib with trametinib, are standard of care for the treatment of advanced melanoma (4, 5). The combination therapy is currently being trialed in a variety of different cancers including colorectal cancers (6).
Despite impressive initial responses, cures using these inhibitors are challenged by the development of resistance, which occurs in the majority of patients within a year after commencement of treatment (7, 8). Great effort has gone into characterizing the mechanisms that are involved in the development of resistance, and to date a catalogue of genetic alterations in resistant cells have been identified (8, 9). Initially it was thought that combination therapies tailored to the genetic alterations found in relapsed patients could be the answer to this challenge, but a major obstacle to this approach is the mutational intertumor and even intratumor heterogeneity of these mutations(8–10). Thus, understanding the response dynamics over the course of treatment with MAPK inhibitors could allow identifying new opportunities to improve the outcome of these therapies.
The transient nature of the activity of MAPK pathway inhibitors in vivo has been elegantly shown using a FRET reporter for ERK activity in melanoma allografts; ERK activity had recovered within one day (11). Unfortunately, this dynamic response is the result of many different mechanisms that ultimately can counteract the effect of BRAF or MEK inhibitors, and in patients these mechanisms are thought to come into action during different phases of the treatment period (Fig. 1B).
Clinical-Translational Advances
Minutes to Hours- relief of negative feedback mechanisms
Like all signaling pathways under physiological conditions, the MAPK pathway is usually kept in balance by negative feedback mechanisms driven by its own activity (Fig. 1B). After receptor stimulation and activation of the pathway, ERK directly phosphorylates and regulates the activity of many proteins in the MAPK signaling cascade (12). ERK phosphorylates RAF, which results in its reduced interaction with RAS, and as a consequence prevents its activation (13). In addition, ERK can inhibit SOS, the guanine nucleotide exchange factor for RAS, thereby impeding RAS activation. ERK also phosphorylates growth factor receptors such as EGFR, which in turn can interfere with recruitment of GRB2-SOS-RAS as well as regulate the endocytosis of active receptors (12). Moreover, Active MAPK signaling stimulates the expression of additional genes that negatively regulate the pathway. The best characterized of these are the Dual-Specific phosphatases (DUSPs) and the receptor activity regulating Sprouty (SPRY) genes that antagonize the ERK kinases activity and receptor signaling, respectively (14, 15).
Because these direct negative feedback mechanisms are dependent on ERK activity, any inhibition of ERK results in a new unrepressed steady state of the MAPK pathway, where any external stimulation would lead to hyper-activation due to a lack of feedback mechanisms (16). Indeed, an array of RTK ligands including HGF and EGF are able to elicit activation of the MAPK pathway in the presence of BRAF inhibition (16). This adaptive response can be effectively suppressed by combining pan RTK inhibitors with BRAF inhibition to stop ligand dependent RAS activation.
Days-Weeks – Adaptation by intracellular signaling and selection for drug-tolerant cells
The immediate changes in gene expression that are induced downstream of ERK (e.g. DUSP6 or cell cycle genes), are followed by a second wave of gene expression changes, and this can lead to major rewiring of signaling pathways in response to long-term MAPK inhibition (Fig. 1B). Importantly, this readjustment can result in adaptation of the tumor cells to the drug treatment, thereby creating a state of tolerance (Fig. 1B). This phase of tolerance is non-mutational and therefore reversible, and it is preceding the state of acquired resistance, when mutated fully resistant cells have re-established tumor growth.
A situation of non-mutational drug tolerance is found with MITF, a ‘melanoma transcription factor’ that had been shown previously to confer increased tolerance to BRAF and MEK inhibitors (17–19), and whose expression is tightly regulated downstream of oncogenic BRAF (20, 21). However this regulation is rewired after long-term pathway inhibition, and in ~80% of melanomas treatment with BRAF and MEK inhibitors for 2 weeks results in up-regulation of MITF (22). MITF up-regulation was also seen in pre-clinical models, where importantly, removal of the drug caused a reversion of MITF expression, demonstrating the non-mutational nature of the MITF mediated drug tolerance (22). A screen designed to target MITF expression during the phase of up-regulation identified the HIV-protease inhibitor nelfinavir as potent agent to be used in combination with BRAF or MEK inhibitors. Most strikingly, as MITF is a melanoma survival protein, this approach might also be suitable for NRAS mutant melanoma, and indeed MEK inhibitor/nelfinavir combination therapy completely blocked tumor growth in an NRASQ61K/BRAFV600E pre-clinical model (22).
Long-term MAPK inhibition can also induce metabolic rewiring. It is well documented that melanoma cells treated with BRAF inhibitors become dependent on oxidative phosphorylation (23–25), which leaves the cells resistant to ROS-based therapies, but vulnerable to mitochondrial uncouplers such as 2,4-dintirophenol (24, 25). This metabolic rewiring is governed by the transcriptional co-activator PGC1α, which intriguingly is a bona fide MITF target gene (24, 25). This indicates that MAPK inhibitor induced MITF up-regulation can directly contribute to metabolic rewiring. Overall, MITF expression levels in patients on treatment with BRAF and MEK inhibitors appear to be a good surrogate marker for response, and changes in MITF expression could be easily monitored by analyzing circulating DNA during treatment.
Another common adaptive response observed in response to MAPK signaling inhibition not only in melanoma but also in colorectal cancer involves enhanced RTK signaling. For instance, in colorectal cancer BRAF inhibition causes activation of EGFR due to inhibition of CDC25C (26). In melanoma, overexpression of ERBB3 is driven by up-regulation of transcription factor FOXD3 as a direct consequence of MEK or BRAF inhibition (27). ERBB3, in the presence of its ligand NRGB1, overcomes BRAF or MEK inhibition by enhanced AKT survival signaling which can be counteracted with combination therapy with the ERBB2 inhibitor lapatinib (27).
Another route in which MAPK pathway inhibition drives increased RTK activity is through RTK stabilization. Whereby, MAPK pathway inhibition blocks the ADAM7/10 mediated shedding of RTKs from the cell membrane (28). An example for this stabilization is AXL, which has been linked to an aggressive and resistant phenotype in melanoma (19, 28, 29). To combat this RTK stabilization the use of selective RTK inhibitors or a neutralizing antibody to TIMP1 in combination with MAPKi is suggested.
In some cases it is also argued that drug-treatment leads to the selection of cancer cell sub-populations differing in their transcriptional state, which are slow-cycling in the absence of drug, but thrive in the presence of drug. For instance overexpression of EGFR/PDGFR is an indirect consequence of MAPK pathway inhibition due to enrichment of EGFR high cells from a heterogeneous population determined by variable levels of its transcriptional repressor SOX10 (30). Under conditions of intermittent drug-dosing this is a reversible response, but continuous drug administration might lead to the permanent establishment of RTK high clones, which initiate acquired resistance. This is in fact seen in relapsed BRAF mutant melanoma and colorectal cancer patients, whose tumours have been found to overexpress a range of RTKs including MET, PDGFR and IGF1R (31–34).
Exposure to MAPK inhibitor (MAPKi) for 9-12 days induces drug-tolerant melanoma cells that display chromatin modifications paralleled by up-regulation of histone demethylases (35). Short-term exposure to MEK inhibitors in BRAF mutant colorectal cells results in increased STAT3 activity that results in epigenetic remodeling via HDAC activity, and inhibition of both the epigenetic modifiers such as HDACs (using vorinostat or entinostat) and MEK can lead to greater treatment potency (36). Again, also here selection for distinct sub-populations can occur, which was seen for melanoma cells differing in the expression of the histone demethylase JARID1B; JARID1Bhigh cells are slow cycling and are characterised by an increase in oxidative phosphorylation (37).
Days-Weeks – Adaptation through the tumor microenvironment
Because of its central role in all cells, it is not surprising to find that inhibition of the MAPK pathway eventually leads to a rewiring of intracellular signaling not only in the tumor cells, but also in the non-tumor cells in the microenvironment. The tumor microenvironment is dynamic and adapts to antagonize treatment in the context of both targeted therapy and chemo/radio-therapies (38–40). Specifically, several stromal cell types can confer tolerance to MAPK pathway inhibition treated cancer cells (41).
Stromal fibroblasts can universally antagonize different targeted treatments in several cancer types including colorectal cancer and ERBB2 positive breast cancer. Fibroblasts drive internal changes in neighboring cancer cells through a secretome rich in growth factors and cytokines. Specifically, tolerance to BRAF inhibitors in melanoma can be induced by fibroblasts through secretion of HGF; a strong inducer of the MAPK cascade that can counteract the pathway inhibition through partial re-activation (16, 42). Indeed it was observed that in patients high intratumor HGF expression levels were correlated with response. In addition, HGF can also antagonize MEK inhibition by increasing AKT induced survival signaling, thus providing a rationale for the combination of MAPK and AKT inhibitors in order to overcome the adaptive fibroblast secretome (42). Fibroblasts also influence treatment response through their ability to remodel the extracellular matrix (ECM). Remodeling the ECM can drive adaptation of melanomas treated with BRAF inhibitors by creating a fibronectin and collagen rich matrix environment that can facilitate reactivation of the MAPK pathway through integrin/FAK signaling (11, 43).
Tumor Associated Macrophages (TAMs) represent another stromal cell type that can contribute to tolerance to MAPK inhibition and accumulation of TAMs within tumors during treatment strongly correlates with faster relapse (38, 39). As with fibroblasts, the secretome of TAMs contains growth factors, cytokines and other signaling molecules (44). VEGF secretion by TAMs leads to partial re-activation of the MAPK pathway in the presence of BRAF inhibitor (39), whereas TNFα enhances survival signaling through MITF (38). The adaptive inflammatory reaction induced by accumulated macrophages can be overcome by either inhibiting macrophage differentiation with Colony Stimulating Factor Receptor inhibitors or targeting the inflammatory signaling induced by NFκB with IKappaB Kinase inhibitors (38, 39). Both of these proposed strategies decrease the abundance of TAMs and thus remove the antagonistic secretome.
Finally, cellular rewiring can promote the establishment of resistant cells in heterogeneous tumors. Thereby cells from either melanoma of lung adenocarcinomas responding to MAPK inhibition can act in a paracrine manner to nurture resistant cells (45). A therapy induced secretome was identified downstream of transcriptional activator FRA1 (FOSL1) that among other growth factors contained IGF1. IGF1 resulted in PI3K survival signaling that if inhibited was able to prolong the response phase when combined with BRAF inhibitor (45).
Conclusions
It has become apparent that the mutational heterogeneity detected in tumors from patients relapsed on MAPK inhibitors presents a major challenge and strategies to improve responses to these inhibitors must consider the dynamics of the response.
When thinking about strategies to target the adaptive phase it is important to understand the underlying mechanisms. Indeed the re-wiring that occurs after MAPK inhibition can be thought of as a temporal process where universal immediate changes eventually evolve into more divergent changes. While the initial stage of pathway rewiring is primarily dependent on the loss of kinase activity of ERK, the following adaptive events appear to be mediated by changes in gene expression primarily induced by transcription factors, which in turn increase survival signaling and metabolic adaptation.
This adaptive phase is further cemented with the additional stromal and cellular heterogeneity also adding to this increased survival signaling. It remains to be seen whether targeting common processes like increased PI3K signaling or transcriptional changes is a possible route to a successful drug combination, but it seems more promising than tackling the complexity of intra- and intertumor mutation heterogeneity at the stage of progression. In addition to this, the idea of drug holidays is also a plausible solution as this tolerance stage is transient and reversible allowing one to conceive that removing the MAPK inhibitors for a period of time can allow rewiring reversal and regained sensitivity. Indeed there is pre-clinical evidence pointing in this direction (46). With the recent insight we have gained into the relevance of non-mutational tolerance, it is clear that the complexity during this early response stage needs to be better understood in order to capitalize on this universal phase therapeutically.
Acknowledgments
Work in the laboratory of CW is funded by Cancer Research UK (C11591/A16416).
Footnotes
The authors declare no conflict of interest
References
- 1.Holderfield M, Deuker MM, McCormick F, McMahon M. Targeting RAF kinases for cancer therapy: BRAF-mutated melanoma and beyond. Nat Rev Cancer. 2014;14:455–67. doi: 10.1038/nrc3760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wellbrock C, Karasarides M, Marais R. The RAF proteins take centre stage. Nat Rev Mol Cell Biol. 2004;5:875–85. doi: 10.1038/nrm1498. [DOI] [PubMed] [Google Scholar]
- 3.Chang F, Steelman LS, Lee JT, Shelton JG, Navolanic PM, Blalock WL, et al. Signal transduction mediated by the Ras//Raf//MEK//ERK pathway from cytokine receptors to transcription factors: potential targeting for therapeutic intervention. J Leuk. 2003;17:1263–93. doi: 10.1038/sj.leu.2402945. [DOI] [PubMed] [Google Scholar]
- 4.Boespflug Al, Thomas L. Cobimetinib and vemurafenib for the treatment of melanoma. Expert Opin Pharmacother. 2016;17:1005–11. doi: 10.1517/14656566.2016.1168806. [DOI] [PubMed] [Google Scholar]
- 5.Grob JJ, Amonkar MM, Karaszewska B, Schachter J, Dummer R, Mackiewicz A, et al. Comparison of dabrafenib and trametinib combination therapy with vemurafenib monotherapy on health-related quality of life in patients with unresectable or metastatic cutaneous BRAF Val600-mutation-positive melanoma (COMBI-v): results of a phase 3, open-label, randomised trial. Lancet Oncol. 2015;16:1389–98. doi: 10.1016/S1470-2045(15)00087-X. [DOI] [PubMed] [Google Scholar]
- 6.Corcoran RB. New therapeutic strategies for BRAF mutant colorectal cancers. J Gastrointest Oncol. 2015;6:650–9. doi: 10.3978/j.issn.2078-6891.2015.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson DB, Menzies AM, Zimmer L, Eroglu Z, Ye F, Zhao S, et al. Acquired BRAF inhibitor resistance: A multicenter meta-analysis of the spectrum and frequencies, clinical behaviour, and phenotypic associations of resistance mechanisms. Eur J Cancer. 2015;51:2792–9. doi: 10.1016/j.ejca.2015.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shi H, Hugo W, Kong X, Hong A, Koya RC, Moriceau G, et al. Acquired Resistance and Clonal Evolution in Melanoma during BRAF Inhibitor Therapy. Cancer Discov. 2014;4:80–93. doi: 10.1158/2159-8290.CD-13-0642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van Allen EM, Wagle N, Sucker A, Treacy DJ, Johannessen CM, Goetz EM, et al. The Genetic Landscape of Clinical Resistance to RAF Inhibition in Metastatic Melanoma. Cancer Discov. 2014;4:94–109. doi: 10.1158/2159-8290.CD-13-0617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kemper K, Krijgsman O, Cornelissen, Steijger P, Shahrabi A, Weeber F, Song JY, et al. Intra, and inter, tumor heterogeneity in a vemurafenib, resistant melanoma patient and derived xenografts. EMBO Mol Med. 2015;7:1104–18. doi: 10.15252/emmm.201404914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hirata E, Girotti MR, Viros A, Hooper S, Spencer-Dene B, Matsuda M, et al. Intravital Imaging Reveals How BRAF Inhibition Generates Drug-Tolerant Microenvironments with High Integrin Œ≤1/FAK Signaling. Cancer Cell. 2015;27:574–88. doi: 10.1016/j.ccell.2015.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Avraham R, Yarden Y. Feedback regulation of EGFR signalling: decision making by early and delayed loops. Nat Rev Mol Cell Biol. 2011;12:104–17. doi: 10.1038/nrm3048. [DOI] [PubMed] [Google Scholar]
- 13.Dougherty MK, Müller Jr, Ritt DA, Zhou M, Zhou XZ, Copeland TD, et al. Regulation of Raf-1 by Direct Feedback Phosphorylation. Mol Cell. 2005;17:215–24. doi: 10.1016/j.molcel.2004.11.055. [DOI] [PubMed] [Google Scholar]
- 14.Eblaghie MC, Lunn JS, Dickinson RJ, Münsterberg AE, Sanz-Ezquerro J-J, Farrell ER, et al. Negative Feedback Regulation of FGF Signaling Levels by Pyst1/MKP3 in Chick Embryos. Curr Bio. 2003;13:1009–18. doi: 10.1016/s0960-9822(03)00381-6. [DOI] [PubMed] [Google Scholar]
- 15.Hanafusa H, Torii S, Yasunaga T, Nishida E. Sprouty1 and Sprouty2 provide a control mechanism for the Ras/MAPK signalling pathway. Nat Cell Biol. 2002;4:850–8. doi: 10.1038/ncb867. [DOI] [PubMed] [Google Scholar]
- 16.Lito P, Pratilas CA, Joseph EW, Tadi M, Halilovic E, Zubrowski M, et al. Relief of Profound Feedback Inhibition of Mitogenic Signaling by RAF Inhibitors Attenuates Their Activity in BRAFV600E Melanomas. Cancer Cell. 2012;22:668–82. doi: 10.1016/j.ccr.2012.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haq R, Yokoyama S, Hawryluk EB, Jönsson GrB, Frederick DT, McHenry K, et al. BCL2A1 is a lineage-specific antiapoptotic melanoma oncogene that confers resistance to BRAF inhibition. PNAS. 2013a;110:4321–6. doi: 10.1073/pnas.1205575110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith MP, Ferguson J, Arozarena I, Hayward R, Marais R, Chapman A, et al. Effect of SMURF2 Targeting on Susceptibility to MEK Inhibitors in Melanoma. JNCI. 2013;105:33–46. doi: 10.1093/jnci/djs471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muller J, Krijgsman O, Tsoi J, Robert L, Hugo W, Song C, et al. Low MITF/AXL ratio predicts early resistance to multiple targeted drugs in melanoma. Nat Commun. 2014;5 doi: 10.1038/ncomms6712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wellbrock C, Rana S, Paterson H, Pickersgill H, Brummelkamp T, Marais R. Oncogenic BRAF Regulates Melanoma Proliferation through the Lineage Specific Factor MITF. PLoS ONE. 2008;3:e2734. doi: 10.1371/journal.pone.0002734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wellbrock C, Arozarena I. Microphthalmia-associated transcription factor in melanoma development and MAP-kinase pathway targeted therapy. Pigment Cell Melanoma Res. 2015;28:390–406. doi: 10.1111/pcmr.12370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith MP, Brunton H, Rowling EJ, Ferguson J, Arozarena I, Miskolczi Z, et al. Inhibiting Drivers of Non-mutational Drug Tolerance Is a Salvage Strategy for Targeted Melanoma Therapy. Cancer Cell. 2016;29:270–84. doi: 10.1016/j.ccell.2016.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Corazao-Rozas P, Guerreschi P, Jendoubi M, André F, Jonneaux Al, Scalbert C, et al. Mitochondrial oxidative stress is the achille’s heel of melanoma cells resistant to Braf-mutant inhibitor. Oncotarget. 2013 Nov;4(11) doi: 10.18632/oncotarget.1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haq R, Shoag J, Andreu-Perez P, Yokoyama S, Edelman H, Rowe GC, et al. Oncogenic BRAF Regulates Oxidative Metabolism via PGC1a and MITF. Cancer Cell. 2013b;23:302–15. doi: 10.1016/j.ccr.2013.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vazquez F, Lim J-H, Chim H, Bhalla K, Girnun G, Pierce K, et al. PGC1a Expression Defines a Subset of Human Melanoma Tumors with Increased Mitochondrial Capacity and Resistance to Oxidative Stress. Cancer Cell. 2013;23:287–301. doi: 10.1016/j.ccr.2012.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prahallad A, Sun C, Huang S, Di Nicolantonio F, Salazar R, Zecchin D, et al. Unresponsiveness of colon cancer to BRAF(V600E) inhibition through feedback activation of EGFR. Nature. 2012;483:100–3. doi: 10.1038/nature10868. [DOI] [PubMed] [Google Scholar]
- 27.Abel EV, Basile KJ, Kugel CH, Witkiewicz AK, Le K, Amaravadi RK, et al. Melanoma adapts to RAF/MEK inhibitors through FOXD3-mediated upregulation of ERBB3. J Clin Invest. 2013;123:2155–68. doi: 10.1172/JCI65780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miller MA, Oudin MJ, Sullivan RJ, Wang SJ, Meyer AS, Im H, et al. Reduced Proteolytic Shedding of Receptor Tyrosine Kinases Is a Post-Translational Mechanism of Kinase Inhibitor Resistance. Cancer Discov. 2016 doi: 10.1158/2159-8290.CD-15-0933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Konieczkowski DJ, Johannessen CM, Abudayyeh O, Kim JW, Cooper ZA, Piris A, et al. A Melanoma Cell State Distinction Influences Sensitivity to MAPK Pathway Inhibitors. Cancer Discov. 2014;4:816–27. doi: 10.1158/2159-8290.CD-13-0424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sun C, Wang L, Huang S, Heynen GJJE, Prahallad A, Robert C, et al. Reversible and adaptive resistance to BRAF(V600E) inhibition in melanoma. Nature. 2014;508:118–22. doi: 10.1038/nature13121. [DOI] [PubMed] [Google Scholar]
- 31.Pietrantonio F, Oddo D, Gloghini A, Valtorta E, Berenato R, Barault L, et al. MET-driven resistance to dual EGFR and BRAF blockade may be overcome by switching from EGFR to MET inhibition in BRAF mutated colorectal cancer. Cancer Discov. 2016 doi: 10.1158/2159-8290.CD-16-0297. [DOI] [PubMed] [Google Scholar]
- 32.Villanueva J, Vultur A, Lee JT, Somasundaram R, Fukunaga-Kalabis M, Cipolla AK, et al. Acquired Resistance to BRAF Inhibitors Mediated by a RAF Kinase Switch in Melanoma Can Be Overcome by Cotargeting MEK and IGF-1R/PI3K. Cancer Cell. 2010;18:683–95. doi: 10.1016/j.ccr.2010.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lezcano C, Lee C-W, Larson AR, Menzies AM, Kefford RF, Thompson JF, et al. Evaluation of stromal HGF immunoreactivity as a biomarker for melanoma response to RAF inhibitors. Mod Pathol. 2014;27:1193–202. doi: 10.1038/modpathol.2013.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nazarian R, Shi H, Wang Q, Kong X, Koya RC, Lee H, et al. Melanomas acquire resistance to B-RAF(V600E) inhibition by RTK or N-RAS upregulation. Nature. 2010;468:973–7. doi: 10.1038/nature09626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Menon DR, Das S, Krepler C, Vultur A, Rinner B, Schauer S, et al. A stress-induced early innate response causes multidrug tolerance in melanoma. Oncogene. 2014 doi: 10.1038/onc.2014.432. [DOI] [PubMed] [Google Scholar]
- 36.Carson R, Celtikci B, Fenning C, Javadi A, Crawford N, Carbonell LP, et al. HDAC inhibition overcomes acute resistance to MEK inhibition in BRAF mutant colorectal cancer by down-regulation of c-FLIP(L) Clin Cancer Res. 2015;21:3230–40. doi: 10.1158/1078-0432.CCR-14-2701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roesch A, Vultur A, Bogeski I, Wang H, Zimmermann KM, Speicher D, et al. Overcoming Intrinsic Multidrug Resistance in Melanoma by Blocking the Mitochondrial Respiratory Chain of Slow-Cycling JARID1Bhigh Cells. Cancer Cell. 2013;23:811–25. doi: 10.1016/j.ccr.2013.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Smith MP, Sanchez-Laorden B, O'Brien K, Brunton H, Ferguson J, Young H, et al. The Immune Microenvironment Confers Resistance to MAPK Pathway Inhibitors through Macrophage-Derived TNFa. Cancer Discov. 2014;4:1214–29. doi: 10.1158/2159-8290.CD-13-1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang T, Xiao M, Ge Y, Krepler C, Belser E, Lopez-Coral A, et al. BRAF Inhibition Stimulates Melanoma-Associated Macrophages to Drive Tumor Growth. Clin Cancer Res. 2015;21:1652–64. doi: 10.1158/1078-0432.CCR-14-1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen F, Zhuang X, Lin L, Yu P, Wang Y, Shi Y, et al. New horizons in tumor microenvironment biology: challenges and opportunities. BMC Med. 2015;13:1–14. doi: 10.1186/s12916-015-0278-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wilson TR, Fridlyand J, Yan Y, Penuel E, Burton L, Chan E, et al. Widespread potential for growth-factor-driven resistance to anticancer kinase inhibitors. Nature. 2012;487:505–9. doi: 10.1038/nature11249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Straussman R, Morikawa T, Shee K, Barzily-Rokni M, Qian ZR, Du J, et al. Tumour micro-environment elicits innate resistance to RAF inhibitors through HGF secretion. Nature. 2012;487:500–4. doi: 10.1038/nature11183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fedorenko IV, Wargo JA, Flaherty KT, Messina JL, Smalley KSM. BRAF inhibition generates a host/tumor niche that mediates therapeutic escape. J Invest Dermatol. 2015;135:3115–24. doi: 10.1038/jid.2015.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cook J, Hagemann T. Tumour-associated macrophages and cancer. Curr Opin Pharmacol. 2013;13:595–601. doi: 10.1016/j.coph.2013.05.017. [DOI] [PubMed] [Google Scholar]
- 45.Obenauf AC, Zou Y, Ji AL, Vanharanta S, Shu W, Shi H, et al. Therapy-induced tumour secretomes promote resistance and tumour progression. Nature. 2015;520:368–72. doi: 10.1038/nature14336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Das Thakur M, Salangsang F, Landman AS, Sellers WR, Pryer NK, Levesque MP, et al. Modelling vemurafenib resistance in melanoma reveals a strategy to forestall drug resistance. Nature. 2013;494:251–5. doi: 10.1038/nature11814. [DOI] [PMC free article] [PubMed] [Google Scholar]