Abstract
Background
Little is known about the association between the quality of trauma care and management of non-fatal injuries. We used emergency department (ED) wait times as a proxy for hospital structure, process, and availability of on-call surgeons with microsurgical skills. We evaluated the association between average hospital ED wait times and likelihood of undergoing digit replantation for patients with traumatic amputation digit injuries. We hypothesized that hospitals with shorter ED wait times were associated with higher odds of replantation.
Methods
Using the 2007-2012 National Trauma Data Bank, our final sample included 12,126 patients. We used regression modeling to first determine factors that were associated with longer ED wait times among patients with digit amputation injuries. Second, we examined the association between ED wait times for this population at a hospital-level and replantation after all types of digit amputation and after complicated thumb amputation injuries (CTAI) only.
Results
For patients with simple and CTAIs, and patients with CTAIs only longer ED wait times were associated with lower odds of replantation. Additionally, being minority and having no insurance were associated with longer ED wait times; teaching hospitals were associated with shorter ED wait times; and finally, for patients with CTAIs only there were no association between patients’ minority or insurance status and replantation.
Conclusions
Variation in ED wait times and its effects on treatment of traumatic digit amputation may reflect maldistribution of hand or plastic surgeons with the required microsurgical skills among trauma centers across the U.S.
Keywords: Hospital quality, Emergent care, Wait times, Amputation, Replantation, Equity in Access, Insurance
Introduction
Over-crowding is a major problem for emergent care centers across the U.S.1,2 Over the last decade, the number of patients seeking care at emergency departments (ED) has increased by 26%.3 With this rapid increase in patient-demand, health systems have had limited opportunities to expand structural capacity and optimize patient-flow processes, leading to substantially increased patient wait times.2 Long ED wait times have been associated with substantially lower patient satisfaction scores4 and significantly worse health outcomes.5-12 For example, patients with acute ST-segment elevation myocardial infarctions experience a 7.5% increase in 1-year mortality rate for every 30 minutes of treatment delay.8 Though the impact of wait times on health outcomes is concerning for the general population, it is particularly alarming for vulnerable populations, such as racial minorities, who utilize the ED more frequently than Whites13 and experience disproportionately longer wait times.14-16
To date, substantial effort has been dedicated to understanding the impact of ED wait times in the management of fatal traumatic injuries.14-16 However, little is known about their impact on the management of non-fatal injuries, such as traumatic digit amputations. Considered one of the most serious hand injuries, traumatic digit amputations afflict upwards of 45,000 people annually.17 Although not fatal, digit amputations can substantially impact patients’ function, aesthetics, quality of life, and occupation.18 Furthermore, children and individuals in their prime, income-earning years suffer a disproportionate number of these injuries.18 Consequently, choosing the most appropriate treatment can have significant and longstanding economic effects on the well-being of trauma patients. Little is known about inequality in ED wait times for digit amputation injuries and the associations between ED wait times and the type of treatment received because of their non-fatal nature.
Applying the conceptual framework of Donabedian quality of care19 and using the 2007 to 2012 National Trauma Data Bank (NTDB)20 developed and managed by the American College of Surgeons (ACS),21 we addressed the intersection of hospital quality, defined by ED wait times, and performance of digit (finger or thumb) replantation. ED wait times were merely used as a quality measure and not as an indicator to determine whether replantation was possible or not. Given the lack of nationalized data related to hospital quality metrics, hand/plastic surgeon staffing/availability, and treatment received for patients with traumatic digit amputation, we specifically chose ED wait times as a proxy for hospital-level efficiency and availability of hand/plastic surgeons with microsurgical skills. As such, our study aimed to examine any associations between hospital systems of care and the treatment received. We hypothesized that patients with traumatic digit amputation injuries treated at hospitals with overall lower ED wait times would have higher odds of undergoing replantation.
Methods
Data Source
We used the 2007-2012 NTDB, which is the largest collection of trauma data optionally reported by a growing number of trauma centers across the U.S.22 Participation is entirely voluntary with a yearly call for data and no outside incentive is given. Over the study period, out of roughly 1200 trauma centers in the U.S., the number of annually reported trauma centers in the NTDB grew from 43523 in 2007 to 80524 in 2012.22
In this study, we examined association between ED wait times, the time between acceptance to the ED and operation or discharge, and the treatment received. We used International Classification of Diseases, Ninth Revision Codes (ICD-9-CM). ICD-9 codes are used to define the injury diagnosis and undertaken procedure(s). We used diagnostic codes 885.0, 885.1, 886.0, 886.1 to classify traumatic digit amputations. Procedure codes 84.21 and 84.22 define replantation of the amputated finger and procedure codes 84.01 and 84.02 define revision amputations.
Cohort Selection
We included all trauma patients with valid ICD-9 codes who underwent a revision amputation or replantation after a digit amputation injury. Between 2007 and 2012, based on ICD-9 diagnosis and procedure codes, there were 13,337 reported cases of traumatic digit amputation. Because treatment of older patients may be related to many other confounding issues, our study cohort included patients 64 years or younger. Trauma level (I, II, or III) is designated by state officials and is verified by the ACS.25 The NTDB contains a separate record, labeled with a patient number, for each diagnosis a patient receives. In order to perform our analyses at a patient level, we grouped the injuries by patient number. Between 2007 and 2012 there were 12,577 patients younger than 65 years with traumatic digit (finger and thumb) amputations. Our final sample, after excluding patients with missing values, included 12,126 patients with traumatic digit amputations treated at 598 centers; among them, 409 patients experienced complicated thumb amputation injuries (CTAIs) (ICD-9 code 885.1). Because decision to attempt replantation is less debatable for CTAIs (ICD-9 code 885.1), we analyzed the association between decision to undergo replantation and ED wait times for (1) all traumatic digit amputation patients and (2) CTAI patients only. We verified the completeness of our cohort by matching the total number of digit amputation injuries (12,577) with sum of revision amputations (10,409) and replantation (2,168). See Figure, Supplemental Digital Content 1, which presents the schematic flow diagram of our study population, detailing the selection of patients in the National Trauma Data Bank. Source: The 2007-2012 National Trauma Data Bank, INSERT LINK. More than 5% of patients had missing values for race, insurance status, and ED wait times. Owing to its heterogonous assignment, ethnicity as defined by being Hispanic or not usually has extensive missing values in administrative and medical data. By creating a separate, “unspecified” category for each of these three variables, we included them in our regression models to avoid selection bias.26,27
Explanatory and Outcome Variables
The two main outcomes of interest in this study were ED wait times and incidence of replantation. At the patient level, our analysis included race, age, sex, injury severity score (ISS), presence of thumb or other finger amputation, presence of multiple- or single-digit amputations, presence and number of certain chronic conditions, being a smoker, having an alcohol problem, and insurance status. Age is represented by patient’s age at the time of injury and categorized into three mutually exclusive sets of under 18, between 18 and 44, and between 45 and 64. Based on patient-reported race, we generated three distinct categories of White, non-White, and race not specified (race missing). Insurance was measured using five distinct categories: private (commercial insurance, Blue Cross Blue Shield, and worker’s compensation), public (Medicaid or Medicare), other (no fault and other insurance), uninsured (self-pay), and unspecified.
Injury Severity Score (ISS) was used to control for the severity of the injury.28 At the hospital level, we controlled for for-profit status, teaching status, number of hospital beds, trauma level, and geographic region of hospital. Hospitals were categorized as either for-profit or public and non-academic or academic. We used four categories for the number of beds: less than 200, between 200 and 400, between 401 and 600, and more than 600, with less than 200 beds serving as the reference category. We categorized the hospital trauma level into four mutually exclusive groups of level I, II, III or higher, and hospitals without a trauma level designation. Finally, the geographic location of each hospital was categorized by region into Midwest, Northeast, South, or West.
Analysis
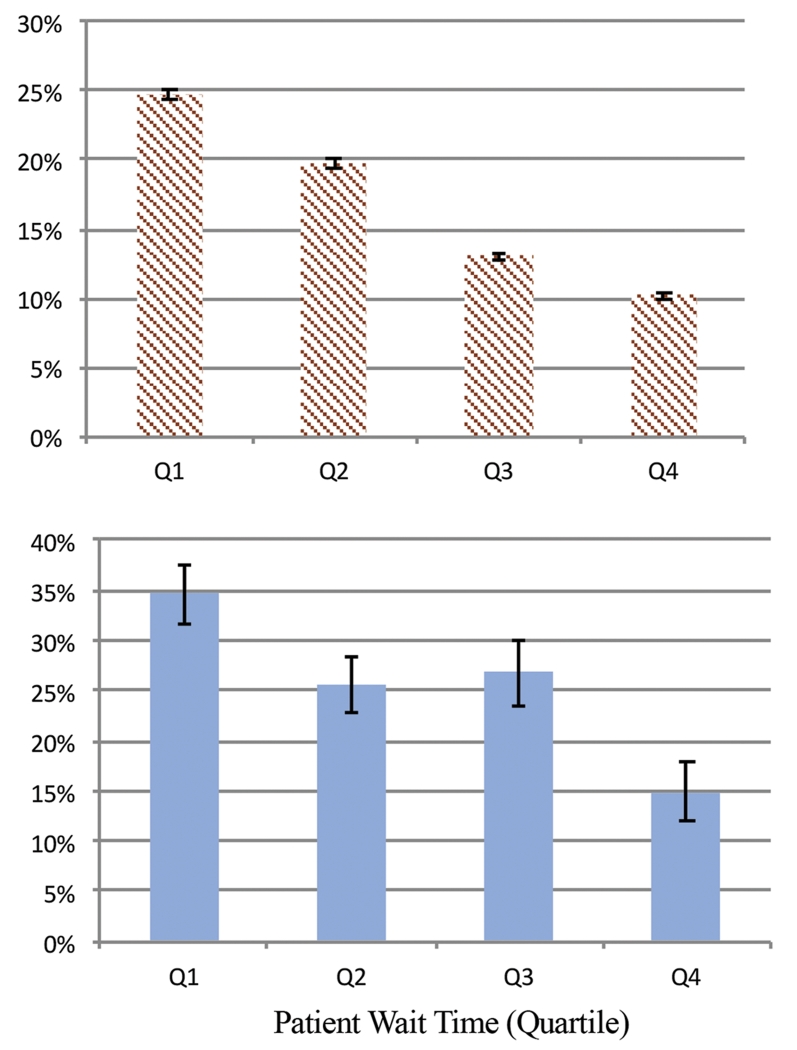
First, we looked at unadjusted characteristics of patients stratified by four quartiles based on the time (in minutes) that each patient spent in the ED. To determine the statistical significance between the lowest quartile and other quartiles, we used a Chi-squared test for categorical variables and a student t-test for continuous variables (Table 1). Additionally, we used Chi-squared test to show the statistical significance of the unadjusted time spent in ED, stratified by insurance status (Figure 1). We used a clustered variance estimation method, vce (cluster), to adjust for hospitals with repeated measures over time (Table 2). We then ran our second regression model to estimate the association between average ED wait times at the hospital-level, inclusive of patients with and without traumatic digit amputation, and the undertaken treatment option (replantation vs. revision amputation) for all traumatic digit amputations and for CTAIs (Table 3). Finally, based on the regression models described in Table 3, we estimated the adjusted predictive probability of undergoing replantation for each quartile of time spent at the ED (Figure 2).
Table 1. Characteristics of individuals under 65 with digit amputation injuries from 2007 to 2012, stratified by emergency department wait time.
| ED Wait Time (Quartile) | Q1a | Q2a | Q3a | Q4a | Not Specified | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| N=12,577 | 3,045 | 2,963 | 2,914 | 2,872 | 783 | |||||
|
| ||||||||||
| Mean | SE | Mean | SE | Mean | SE | Mean | SE | Mean | SE | |
| Age | ||||||||||
| Less than 18 | 0.12 | 0.01 | 0.13 | 0.01 | *0.10 | 0.01 | *0.09 | 0.01 | 0.12 | 0.01 |
| 18 to 44 | 0.52 | 0.01 | *0.49 | 0.01 | *0.48 | 0.01 | 0.54 | 0.01 | *0.48 | 0.02 |
| 44 to 64 | 0.35 | 0.01 | *0.39 | 0.01 | *0.42 | 0.01 | *0.37 | 0.01 | *0.40 | 0.02 |
|
| ||||||||||
| Female | 0.12 | 0.01 | 0.13 | 0.01 | 0.13 | 0.01 | *0.14 | 0.01 | 0.13 | 0.01 |
|
| ||||||||||
| Race | ||||||||||
| White | 0.71 | 0.01 | 0.73 | 0.01 | 0.70 | 0.01 | *0.63 | 0.01 | *0.64 | 0.02 |
| Non-White | 0.29 | 0.01 | 0.27 | 0.01 | 0.30 | 0.01 | *0.38 | 0.01 | *0.36 | 0.02 |
| Race Not Specified | 0.07 | 0.00 | 0.06 | 0.00 | *0.06 | 0.00 | 0.07 | 0.00 | *0.12 | 0.01 |
|
| ||||||||||
| Habits/Co-morbidities | ||||||||||
| Smoking | 0.13 | 0.01 | 0.13 | 0.01 | *0.15 | 0.01 | 0.13 | 0.01 | *0.06 | 0.01 |
| Alcohol | 0.03 | 0.00 | 0.03 | 0.00 | 0.03 | 0.00 | *0.05 | 0.00 | 0.04 | 0.01 |
| Number of co-morbidities | 0.26 | 0.01 | 0.24 | 0.01 | 0.27 | 0.01 | 0.28 | 0.01 | *0.17 | 0.02 |
|
| ||||||||||
| Injury Characteristics | ||||||||||
| Injury Severity Score (ISS) | 5.22 | 0.10 | *4.60 | 0.08 | *4.21 | 0.07 | *4.66 | 0.09 | *4.00 | 0.15 |
| Multiple Digit | 0.29 | 0.01 | *0.24 | 0.01 | *0.17 | 0.01 | *0.14 | 0.01 | *0.23 | 0.02 |
| Thumb | 0.25 | 0.01 | *0.19 | 0.01 | *0.16 | 0.01 | *0.13 | 0.01 | *0.18 | 0.01 |
|
| ||||||||||
| Insurance | ||||||||||
| Private | 0.55 | 0.01 | *0.57 | 0.01 | 0.56 | 0.01 | *0.50 | 0.01 | *0.47 | 0.02 |
| Public | 0.10 | 0.01 | 0.11 | 0.01 | 0.11 | 0.01 | 0.11 | 0.01 | *0.07 | 0.01 |
| No Insurance | 0.18 | 0.01 | *0.16 | 0.01 | 0.17 | 0.01 | *0.21 | 0.01 | *0.13 | 0.01 |
| Other Insurance | 0.08 | 0.01 | 0.08 | 0.00 | 0.07 | 0.00 | 0.08 | 0.01 | *0.06 | 0.01 |
| Insurance Not Specified | 0.08 | 0.01 | 0.08 | 0.01 | 0.09 | 0.01 | *0.10 | 0.01 | *0.26 | 0.02 |
Source: The 2007-2012 National Trauma Data Bank.
Significant at the 95% confidence interval.
Q1: < 93 minutes; Q2: between 92 and 147 minutes; Q3: between 148 and 231 minutes; Q4: more than 231 minute
Figure 1.
Unadjusted average of wait times in emergency department, stratified by health insurance. Note: Differences in wait times in emergency department were significant at 95% confidence intervals for all types of insurance vs. private insurance. Source: NTDB, 2007 to 2012.
Table 2. GLM Regression Results Examining Emergency Department Wait Times.
| Beta | SE | 95% CI | P | |
|---|---|---|---|---|
| Patient Characteristics | ||||
|
| ||||
| Age | ||||
| Less than 18 | −0.20 | 0.05 | −0.30 - −0.10 | 0.000 |
| 18 to 44 | −0.06 | 0.04 | −0.14 - 0.01 | 0.091 |
| 44 to 64 (ref.) | 0.00 | |||
|
| ||||
| Female | −0.02 | 0.04 | −0.10 - 0.07 | 0.672 |
|
| ||||
| Race | ||||
| White (ref.) | 0.00 | |||
| Non-White | 0.06 | 0.03 | 0.00 - 0.11 | 0.050 |
| Race Not Specified | 0.15 | 0.10 | −0.04 - 0.35 | 0.124 |
|
| ||||
| Habits/Co-morbidities | ||||
| Smoking | −0.12 | 0.05 | −0.21 - −0.02 | 0.013 |
| Alcohol | 0.17 | 0.09 | −0.01 - 0.36 | 0.067 |
| Number of co-morbidities | 0.07 | 0.04 | −0.01 - 0.15 | 0.082 |
|
| ||||
| Injury Characteristics | ||||
| ISS Score | −0.01 | 0.00 | −0.02 - 0.00 | 0.032 |
| Multiple Digit | 0.16 | 0.10 | −0.05 - 0.36 | 0.130 |
| Thumb | −0.17 | 0.03 | −0.23 - −0.10 | 0.000 |
|
| ||||
| Insurance | ||||
| Private (ref.) | 0.00 | |||
| Public | 0.10 | 0.05 | 0.00 - 0.20 | 0.057 |
| No Insurance | 0.12 | 0.04 | 0.05 - 0.20 | 0.002 |
| Other Insurance | 0.38 | 0.26 | −0.12 - 0.88 | 0.140 |
| Insurance Not Specified | 0.88 | 0.40 | 0.10 - 1.66 | 0.026 |
|
| ||||
| Hospital Characteristics | ||||
|
| ||||
| Bed Size | ||||
| Less than 200 (ref.) | 0.00 | |||
| 200-400 | −0.14 | 0.11 | −0.35 - 0.07 | 0.178 |
| 401-600 | −0.04 | 0.12 | −0.27 - 0.19 | 0.744 |
| More than 600 | −0.17 | 0.12 | −0.40 - 0.07 | 0.163 |
|
| ||||
| Trauma Center Level | ||||
| Other Hospitals (ref.) | 0.00 | |||
| Level I | 0.28 | 0.09 | 0.11 - 0.45 | 0.001 |
| Level II | −0.08 | 0.09 | −0.25 - 0.08 | 0.327 |
| Level III | −0.18 | 0.11 | −0.39 - 0.04 | 0.104 |
|
| ||||
| Status | ||||
| For-Profit (vs. Public) | 0.07 | 0.13 | −0.17 - 0.32 | 0.558 |
| Non-Teaching (vs. Teaching) | 0.20 | 0.10 | 0.01 - 0.39 | 0.038 |
|
| ||||
| Geography | ||||
| Midwest (ref.) | 0.00 | |||
| Northeast | −0.20 | 0.11 | −0.42 - 0.02 | 0.074 |
| South | 0.05 | 0.08 | −0.11 - 0.21 | 0.532 |
| West | 0.01 | 0.15 | −0.27 - 0.30 | 0.933 |
|
| ||||
| Intercept | 5.20 | 0.12 | 4.96 - 5.43 | 0.000 |
N=12,126; AIC=12.75; Adjusted for 586 clusters in hospitals.
Source: The 2007 – 2012 National Trauma Data Bank.
Table 3. Regression Results Examining Odds of Replantation.
| All Digit Amputation Injuriesb | Comp. Thumb Amputation Injuriesc | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| OR | SE | P | 95% CI | OR | SE | P | 95% CI | |
| Patient Characteristics | ||||||||
|
| ||||||||
| Age | ||||||||
|
| ||||||||
| Less than 18 | 1.97 | 0.17 | 0.000 | 1.66-2.34 | 0.60 | 0.34 | 0.366 | 0.20-1.80 |
| 18 to 44 | 1.13 | 0.07 | 0.031 | 1.01-1.27 | 0.68 | 0.20 | 0.198 | 0.38-1.22 |
| 44 to 64 (ref.) | 1.00 | 1.00 | ||||||
|
| ||||||||
| Female | 1.01 | 0.08 | 0.850 | 0.87-1.18 | 0.90 | 0.39 | 0.804 | 0.38-2.10 |
|
| ||||||||
| Race | ||||||||
|
| ||||||||
| White (ref.) | 1.00 | 1.00 | ||||||
| Non-White | 0.90 | 0.06 | 0.107 | 0.80-1.02 | 1.16 | 0.42 | 0.671 | 0.58-2.34 |
| Race/Ethnicity Not Specified | 1.35 | 0.15 | 0.005 | 1.09-1.67 | 0.91 | 0.57 | 0.877 | 0.26-3.13 |
|
| ||||||||
| Habits/Co-morbidities | ||||||||
|
| ||||||||
| Smoking | 0.81 | 0.07 | 0.009 | 0.69-0.95 | 1.28 | 0.47 | 0.494 | 0.63-2.62 |
| Alcohol | 1.23 | 0.18 | 0.140 | 0.93-1.63 | 0.49 | 0.35 | 0.318 | 0.12-1.97 |
| Number of co-morbidities | 0.90 | 0.04 | 0.034 | 0.82-0.99 | 0.62 | 0.18 | 0.096 | 0.35-1.09 |
|
| ||||||||
| Injury Characteristics | ||||||||
|
| ||||||||
| ISS Score | 0.94 | 0.01 | 0.000 | 0.93-0.95 | 0.82 | 0.05 | 0.001 | 0.73-0.93 |
|
| ||||||||
| Insurance | ||||||||
|
| ||||||||
| Private (ref.) | 1.00 | 1.00 | ||||||
| Public | 0.82 | 0.08 | 0.043 | 0.68-0.99 | 0.95 | 0.47 | 0.923 | 0.36-2.49 |
| No Insurance | 0.75 | 0.06 | 0.000 | 0.65-0.87 | 0.56 | 0.21 | 0.130 | 0.27-1.18 |
| Other Insurance | 0.83 | 0.06 | 0.011 | 0.72-0.96 | 1.18 | 0.43 | 0.642 | 0.58-2.40 |
| Insurance Not Specified | 0.96 | 0.09 | 0.626 | 0.80-1.14 | 0.56 | 0.31 | 0.302 | 0.19-1.68 |
|
| ||||||||
| Hospital Characteristics | ||||||||
|
| ||||||||
| ED Wait Timea | ||||||||
|
| ||||||||
| Q1 (ref.) | 1.00 | 1.00 | ||||||
| Q2 | 0.77 | 0.05 | 0.000 | 0.67-0.87 | 0.67 | 0.22 | 0.214 | 0.36-1.26 |
| Q3 | 0.47 | 0.03 | 0.000 | 0.41-0.55 | 0.44 | 0.18 | 0.040 | 0.20-0.96 |
| Q4 | 0.36 | 0.03 | 0.000 | 0.30-0.42 | 0.26 | 0.13 | 0.006 | 0.10-0.69 |
| Time Not Specified | 0.66 | 0.07 | 0.000 | 0.53-0.83 | 1.52 | 0.75 | 0.401 | 0.57-4.00 |
|
| ||||||||
| Bed Size | ||||||||
|
| ||||||||
| Less than 200 (ref.) | 1.00 | 1.00 | ||||||
| 200-400 | 0.74 | 0.12 | 0.071 | 0.54-1.03 | 1.28 | 1.59 | 0.845 | 0.11-14.62 |
| 401-600 | 0.99 | 0.16 | 0.965 | 0.72-1.36 | 1.10 | 1.39 | 0.938 | 0.09-13.09 |
| More than 600 | 1.10 | 0.18 | 0.538 | 0.80-1.52 | 1.62 | 1.96 | 0.691 | 0.15-17.32 |
|
| ||||||||
| Status | ||||||||
|
| ||||||||
| For-Profit (vs. Public) | 1.01 | 0.13 | 0.917 | 0.79-1.30 | 0.97 | 0.67 | 0.970 | 0.25-3.75 |
| Teaching (vs. non-teaching) | 1.48 | 0.10 | 0.000 | 1.29-1.69 | 1.63 | 0.64 | 0.214 | 0.76-3.51 |
|
| ||||||||
| Trauma Center Level | ||||||||
|
| ||||||||
| Level I (ref.) | 1.00 | 1.00 | ||||||
| Other Hospitals | 1.08 | 0.08 | 0.317 | 0.93-1.25 | 0.68 | 0.25 | 0.285 | 0.34-1.38 |
| Level II | 0.48 | 0.05 | 0.000 | 0.40-0.58 | 0.49 | 0.27 | 0.199 | 0.16-1.46 |
| Level III or higher | 0.39 | 0.08 | 0.000 | 0.26-0.57 | - | - | - | - |
|
| ||||||||
| Geography | ||||||||
|
| ||||||||
| Midwest (ref.) | 1.00 | 1.00 | ||||||
| Northeast | 1.24 | 0.10 | 0.007 | 1.06-1.45 | 1.10 | 0.59 | 0.852 | 0.39-3.14 |
| South | 0.84 | 0.06 | 0.010 | 0.73-0.96 | 1.56 | 0.55 | 0.207 | 0.78-3.09 |
| West | 1.23 | 0.09 | 0.008 | 1.05-1.43 | 2.13 | 0.82 | 0.050 | 1.00-4.51 |
|
| ||||||||
| Intercept | 0.36 | 0.07 | 0.000 | 0.25-0.52 | 1.13 | 1.45 | 0.921 | 0.09-13.83 |
Source: the 2007-2012 National Trauma Data Bank.
Q1: < 93 minutes; Q2: between 92 and 147 minutes; Q3: between 148 and 231 minutes; Q4: more than 231 minute
Number of Patients=12,126; Number of Hospitals=598; Wald Chi2=763.02, P < 0.001, R2=0.08.
Number of Patients= 409; Number of Hospitals=100; Wald Chi2=43.96, P < 0.021, R2=0.12.
Figure 2.
Risk adjusted predicted probability of undergoing replantation among: (A) Patients with all types of digit amputation injuries; (B) Patients with complicated thumb amputation injuries. Note: Differences in all patient wait times vs. the top quartile (< 92 minutes) wait times were significant at the 95% confidence interval. Q1: < 93 minutes; Q2: between 92 and 147 minutes; Q3: between 148 and 231 minutes; Q4: more than 231 minute. Source: NTDB, 2007 to 2012.
Results
Table 1 presents the characteristics of patients younger than 65 years of age with traumatic digit amputation. We stratified patients based on their ED wait times. Older patients spent more time in ED with four (p=0.010), seven (p < 0.001), and two percentage points (p=0.091) more adults between ages 44 and 64 with wait times in the 2nd (93-147 minutes), 3rd (148-231 minutes), and 4th quartiles (> 231 minutes), than the first quartile (<93 minutes), respectively. There were nine and seven percentage points more non-Whites among patients in the 3rd and 4th quartiles (p < 0.050). Five percentage points fewer people with private insurance were in the 4th quartile compared with first quartile. The average ISS score in the 1st quartile was 5.22 and was significantly higher than ISS in other quartiles (p < 0.001 for all). Additionally, substantially more patients with multiple-digit and thumb amputations were in the 1st quartile (p < 0.001 for all).
Figure 1 shows the unadjusted average of wait times in ED based on health insurance. Compared with individuals with private insurance, those with public, no insurance, or other insurance, on average, spent 15, 31, and 83 minutes longer in ED, respectively.
Table 2 represents the results of our GLM regression analysis. Being less than 18 years of age was associated with shorter wait times in the ED by a factor of 0.82 (beta=−0.20, CI: −0.30 - −0.10). Being non-White was associated with longer wait times by a factor of 1.13 (beta=0.06, CI:0.00 – 0.11). Higher ISS and having a thumb amputation were associated with shorter wait times by factors of 0.99 (beta=-0.01, CI:-0.02 – 0.00), and 0.84 (beta=−0.17, CI=−0.23 −0.10), respectively. Compared with private insurance, having public or no insurance was associated with longer wait times by factors of 1.11 (beta=0.10, CI:0.00 – 0.20) and 1.13 (beta=0.12, CI:0.05 – 0.20). At the hospital level, being a level I trauma center was associated with longer wait times by a factor of 1.32 (beta=0.28, CI=0.11 – 0.45) compared with hospitals with full capacity but without trauma level designation. Additionally, compared with academic hospitals, being a non-academic center was associated with longer wait times by a factor of 1.22 (beta=0.20, CI=0.01 – 0.39).
Table 3 shows that for all digit amputation injuries (A) and for CTAIs only (B), hospital level ED wait times were associated with replantation. For example, odds of replantation for all digit amputation injuries that were treated in hospitals with more than 231 minutes ED wait times (4st Q) compared with those being treated in hospitals with less than 93 minutes ED wait times (1st Q) was OR=0.36 (CI: 0.30 −0.42). For CTAIs only, odds of replantation if treated in hospitals with ED wait times at the 4th quartile compared with being treated at hospitals within the first quartile was OR= 0.26 (CI: 0.10 - 0.69).
Figure 2 shows the adjusted predicted probability of replantation stratified by wait times in the ED. For all digit amputation injuries, compared with fewer than 93 minutes (1st Q) probability of replantation decreased by 5, 12, and 15 percentage points in 2nd, 3rd, and 4th ED wait times quartiles, respectively (p < 0.001 for all). For CTAIs, compared with fewer than 93 minutes (1st Q) probability of replantation decreased by 10, 8, and 20 percentage points in 2nd, 3rd, and 4th ED wait time quartiles, respectively (p < 0.001 for all).
Discussion
We used ED wait times as a proxy for hospital structure and availability of on-call hand or plastic surgeons with microsurgical skills. For both patient groups (patients consisting of simple and complicated finger and thumb amputation injuries and patients with CTAIs only), longer ED wait times were associated with lower odds of undergoing a replantation. Our evaluation yielded three additional findings. First, being minority and having no insurance were associated with longer ED wait times. Second, academic hospitals were associated with shorter ED wait times. Finally, for patients with CTAIs only, compared with those with all types of digit amputation injuries, there were no association between patients’ minority or insurance status and replantation.
Our study supports earlier research showing that vulnerable populations, such as minority groups and uninsured individuals, experience disproportionately delayed access to care in the ED. A 2008 evaluation of ED quality and efficiency found that White patients with acute myocardial infarction (AMI) waited a median time of 24 minutes to see an emergency medicine physician while African-Americans and Hispanics waited median times of 31 and 33 minutes, respectively.11 Similarly, studies have shown that wait times for uninsured patients can be as high as 33% longer than wait times for patients with insurance.29 There are several possible explanations for the race- and insurance-related disparities in ED wait times. First, efficient and effective EDs (higher-quality EDs) may be less accessible to vulnerable populations since minority patients tend to reside closer to low-quality hospitals, as defined by mortality rate, relative to their White counterparts.30 Given that many patients seek care through nearby facilities,31 minority or uninsured patients may disproportionately seek treatment at low-quality hospitals close to their place of residence.32
Second, an unfavorable payer-mix at hospitals serving predominantly minority patients may severely impact patient wait times. Haider et al showed that hospitals serving predominantly minority populations can have nearly double the percentage of uninsured patients compared to hospitals serving predominantly majority or mixed populations.33 The increased proportion of uninsured patients may drive higher patient volumes and longer wait times. Moreover, lower quality hospitals may not have the resources to (1) staff hand/plastic surgeons with microsurgical skills at all times;34 (2) maintain a strong plastic and hand surgery residency/fellowship training program;35 or (3) invest in process improvement tools that could reduce patient wait times.36
Regarding the impact of hospital-level characteristics on timely access to care in the ED, our analysis revealed that being an academic hospital was associated with decreased wait times for patients seeking treatment for traumatic digit amputations. These findings substantiate earlier studies, which found that teaching status impacts quality-of-care processes and patient outcomes. For example, patients with acute myocardial infarction (AMI) who are treated at teaching hospitals are more likely to receive guideline-recommended treatment modalities, such as aspirin, angiotensin-converting enzyme inhibitors, and beta-blockers compared to those treated at non-teaching hospitals.37 With respect to complex surgical procedures, research shows that teaching hospitals have lower operative mortality rates for hepatic, pancreatic, and esophageal resections compared to non-teaching hospitals.38 The superior surgical treatment at academic hospitals may be attributed to a higher volume of complex surgeries and the lower risk of adverse events associated with high-volume hospitals.39
Our results agree with previous findings that process components of hospital quality, such as ED wait times, affect quality of patient care and outcomes.12,40 Over-crowding is one of the primary drivers of increased patient wait times and has been shown to directly impact the process of patient care. Studies show that over-crowding is associated with delayed access to antibiotics for treatment of pneumonia,12,41 delayed use of thrombolysis for treatment of AMI,42 and increased time to analgesic administration for patients with severe pain from hip fractures.43 ED process inefficiencies are largely derived from resource and capacity constraints; when the ED is operating at or above capacity, delivery of multi-step patient care is less efficient.43,44 Over-crowding has also been associated with worse clinical guideline adherence rates. 40 Importantly, the problem of delayed access to care has significant consequences for patient outcomes. For example, patients admitted to the ED during periods of over-crowding experience 5% greater odds of death compared to those admitted during periods with manageable volume and lower patient wait times.45 In cases of CTAIs, longer ED wait times could be attributed to the unavailability of an on-call hand or plastic surgeon with the necessary microsurgical skills.46 Replantation of the thumb is mostly performed in level I or II trauma centers, and it is the optimal treatment option; thus, race and insurance type were not associated with complicated thumb replantation. Many stakeholders have argued that expansion of insurance coverage under the Affordable Care Act (ACA) may lead to increase in ED crowding. When there is a shortage of physicians, this argument seems logical. However, in a study, published in the New England Journal of Medicine,47 examining the Massachusetts’s healthcare reform, the authors did not find any change in utilization of ED due to expansion of health coverage.
Our study had a few limitations. First, the NTDB is not a nationally representative sample of all trauma centers in the U.S. and, among those centers that report their trauma cases, only about 67% had associated ICD-9 codes. Thus, our findings may not be generalizable. However, our results were in agreement with the related literature from other sources. Second, the NTDB lacks certain information, such as the location of these centers, the number and expertise surgeons, and the distance of the center to the patients’ residences, making it impossible to further investigate the reasons behind longer wait times. Additionally, excepting insurance status, there is no socioeconomic information to include in our analytic models. Because the NTDB is not a longitudinal dataset, we were unable to follow patients over time to evaluate the rate of replantation success as the ultimate outcome measure. Finally, these discrepancies may be due to surgeon characteristics. The wait times may point to a maldistribution of microsurgical expertise in various trauma centers rather than just differences in ED process of care. Despite these shortcomings, we were able to evaluate the association between quality of a trauma center, measured by ED wait times, and probability of undergoing replantation, an optimal but complex surgical treatment.
Owing to lack of a recommended treatment guideline for digit amputation injuries, over- (attempt to replant when it is not recommended) or under-treatment (revision amputation when replant is recommended) may occur more often than it should. In 2006, the Institute of Medicine’s Committee on the Future of Emergency Care in the U.S. created a vision which included a reduction in ED overcrowding, fragmentation, and on-call specialist shortages.48 Policy-makers and hospital systems have explored a number of solutions to resolve problems in the timeliness of ED care. One strategy involved improving hospital efficiency and patient flow by implementing process management tools. These tools, employed extensively in the business world, aim to increase patient throughput by reducing delays and improving quality. Queuing theory analytics are mathematical methods for understanding patient volume trends which allow EDs to pre-allocate resources and capacity to meet changing patient demand.49 A study by Alavi-Moghaddam found that adding a senior emergency resident to the floor staff decreased patient wait times by 10%.49 Moreover, adding 50% more staff to specialist consultations reduced patients’ length of stay by 90-minutes.49
The reallocation of capacity and resources via regionalization of trauma care services is a much-needed approach to improving ED efficiency and effectiveness. Regionalization was initially recommended by the IOM as a way for under-equipped hospitals to selectively refer complex or high-risk cases to better-resourced trauma centers.50 It is important to note that under the leadership of Dr. Scott Levin, MD, the American Society for Surgery of the Hand (ASSH) initiated a joint task force with the American College of Surgeons (ACS) to address issues related to regionalization of hand trauma care in the U.S.51 A few other possibilities include paying academic centers premiums to care for uninsured or patients of lower socioeconomic classes or requiring plastic surgery board eligible candidates to perform community service for a period following residency graduation.
Supplementary Material
Acknowledgments
Funding: This work was supported by the American Foundation for Surgery of the Hand Clinical Grant (to Dr. Elham Mahmoudi), and a Midcareer Investigator Award in Patient-Oriented Research (2 K24-AR053120-06) (to Dr. Kevin C. Chung)
Footnotes
Author Contributions:
Access to data: Dr. Mahmoudi had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Swiatek, Peter, Mahmoudi, Elham, Chung, Kevin
Acquisition, analysis, or interpretation of data: Mahmoudi, Elham
Drafting the manuscript: Mahmoudi, Elham; Swiatek, Peter.
Critical revision of the manuscript for important intellectual content: Chung, Kevin; Mahmoudi, Elham.
Statistical analysis: Mahmoudi, Elham
Study supervision: Mahmoudi, Elham
Supplemental Digital Content 1, See figure which shows the Schematic flow diagram of our study population, detailing the selection of patients in the National Trauma Data Bank. Source: The 2007-2012 National Trauma Data Bank, INSERT LINK.
References
- 1.Rutman LE, Migita R, Woodward GA, Klein EJ. Creating a leaner pediatric emergency department: how rapid design and testing of a front-end model led to decreased wait time. Pediatric emergency care. 2015;31(6):395–398. doi: 10.1097/PEC.0000000000000455. [DOI] [PubMed] [Google Scholar]
- 2.Horwitz LI, Green J, Bradley EH. US emergency department performance on wait time and length of visit. Annals of emergency medicine. 2010;55(2):133–141. doi: 10.1016/j.annemergmed.2009.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Advance Data: From Vital and Health Statistics. CDC: Centers for Disease Control; Apr 22, 2002. National Hospital Ambulatory Medical Care Survey: 2000 Emergency Department Summary [press release] 2002. [Google Scholar]
- 4.Rodi SW, Grau MV, Orsini CM. Evaluation of a fast track unit: alignment of resources and demand results in improved satisfaction and decreased length of stay for emergency department patients. Quality management in health care. 2006;15(3):163–170. doi: 10.1097/00019514-200607000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. The New England journal of medicine. 2001;345(19):1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 6.Houck PM, Bratzler DW, Nsa W, Ma A, Bartlett JG. Timing of antibiotic administration and outcomes for Medicare patients hospitalized with community-acquired pneumonia. Archives of internal medicine. 2004;164(6):637–644. doi: 10.1001/archinte.164.6.637. [DOI] [PubMed] [Google Scholar]
- 7.Wardlaw JM, Zoppo G, Yamaguchi T, Berge E. Thrombolysis for acute ischaemic stroke. The Cochrane database of systematic reviews. 2003;(3):CD000213. doi: 10.1002/14651858.CD000213. [DOI] [PubMed] [Google Scholar]
- 8.De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109(10):1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 9.McNamara RL, Wang Y, Herrin J, et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. Journal of the American College of Cardiology. 2006;47(11):2180–2186. doi: 10.1016/j.jacc.2005.12.072. [DOI] [PubMed] [Google Scholar]
- 10.Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. Jama. 2000;283(22):2941–2947. doi: 10.1001/jama.283.22.2941. [DOI] [PubMed] [Google Scholar]
- 11.Wilper AP, Woolhandler S, Lasser KE, et al. Waits to see an emergency department physician: U.S. trends and predictors, 1997-2004. Health Aff (Millwood) 2008;27(2):w84–95. doi: 10.1377/hlthaff.27.2.w84. [DOI] [PubMed] [Google Scholar]
- 12.Pines JM, Hollander JE, Localio AR, Metlay JP. The association between emergency department crowding and hospital performance on antibiotic timing for pneumonia and percutaneous intervention for myocardial infarction. Acad Emerg Med. 2006;13(8):873–878. doi: 10.1197/j.aem.2006.03.568. [DOI] [PubMed] [Google Scholar]
- 13.McCaig LF, Burt CW. National Hospital Ambulatory Medical Care Survey: 2001 emergency department summary. Advance data. 2003;(335):1–29. [PubMed] [Google Scholar]
- 14.James CA, Bourgeois FT, Shannon MW. Association of race/ethnicity with emergency department wait times. Pediatrics. 2005;115(3):e310–315. doi: 10.1542/peds.2004-1541. [DOI] [PubMed] [Google Scholar]
- 15.Schrader CD, Lewis LM. Racial disparity in emergency department triage. The Journal of emergency medicine. 2013;44(2):511–518. doi: 10.1016/j.jemermed.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 16.Sonnenfeld N, Pitts SR, Schappert SM, Decker SL. Emergency department volume and racial and ethnic differences in waiting times in the United States. Medical care. 2012;50(4):335–341. doi: 10.1097/MLR.0b013e318245a53c. [DOI] [PubMed] [Google Scholar]
- 17.Bureau of Labor Statistics [Accessed November 7, 2011];2011 http://data.bls.gov/data.
- 18.Giladi AM, McGlinn EP, Shauver MJ, Voice TP, Chung KC. Measuring outcomes and determining long-term disability after revision amputation for treatment of traumatic finger and thumb amputation injuries. Plastic and reconstructive surgery. 2014;134(5):746e–755e. doi: 10.1097/PRS.0000000000000591. [DOI] [PubMed] [Google Scholar]
- 19.Donabedian A. The quality of care: How can it be assessed? JAMA : the journal of the American Medical Association. 1988;260(12):1743–1748. doi: 10.1001/jama.260.12.1743. [DOI] [PubMed] [Google Scholar]
- 20.Haider AH, Weygandt PL, Bentley JM, et al. Disparities in trauma care and outcomes in the United States: a systematic review and meta-analysis. The journal of trauma and acute care surgery. 2013;74(5):1195. doi: 10.1097/TA.0b013e31828c331d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American College of Surgeons (ACS) [Accessed July 10, 2015];National Trauma Data Bank Report 2014. https://www.facs.org/~/media/files/qualityprograms/trauma/ntdb/ntdbannualreport2014.ashx.
- 22.Haider AH, Saleem T, Leow JJ, et al. Influence of the National Trauma Data Bank on the study of trauma outcomes: is it time to set research best practices to further enhance its impact? Journal of the American College of Surgeons. 2012;214(5):756–768. doi: 10.1016/j.jamcollsurg.2011.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Trauma Data Bank 2008: Annual Report. American College of Surgeons Committee on Trauma; 2008. [Google Scholar]
- 24.National Trauma Data Bank 2013: Annual Report. National Trauma Data Bank; 2013. [Google Scholar]
- 25.American Trauma Society (ATS) [Accessed March 15, 2015];Trauma Center Levels Explained. 2015 http://www.amtrauma.org/?page=TraumaLevels.
- 26.Heckman JJ. Sample selection bias as a specification error (with an application to the estimation of labor supply functions) National Bureau of Economic Research Cambridge, Mass.; USA: 1977. [Google Scholar]
- 27.Wood L, Egger M, Gluud LL, et al. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta-epidemiological study. Bmj. 2008;336(7644):601–605. doi: 10.1136/bmj.39465.451748.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Babu MA, Nahed BV, DeMoya MA, Curry WT. Is trauma transfer influenced by factors other than medical need? An examination of insurance status and transfer in patients with mild head injury. Neurosurgery. 2011;69(3):659–667. doi: 10.1227/NEU.0b013e31821bc667. [DOI] [PubMed] [Google Scholar]
- 29.de Araujo P, Khraiche M, Tukan A. Does overcrowding and health insurance type impact patient outcomes in emergency departments? Health economics review. 2013;3(1):25. doi: 10.1186/2191-1991-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baicker K, Chandra A, Skinner JS. Geographic variation in health care and the problem of measuring racial disparities. Perspectives in biology and medicine. 2005;48(1 Suppl):S42–53. [PubMed] [Google Scholar]
- 31.Finlayson SR, Birkmeyer JD, Tosteson AN, Nease RF., Jr. Patient preferences for location of care: implications for regionalization. Medical care. 1999;37(2):204–209. doi: 10.1097/00005650-199902000-00010. [DOI] [PubMed] [Google Scholar]
- 32.Haider AH, Hashmi ZG, Zafar SN, et al. Minority trauma patients tend to cluster at trauma centers with worse-than-expected mortality: can this phenomenon help explain racial disparities in trauma outcomes? Annals of surgery. 2013;258(4):572–579. doi: 10.1097/SLA.0b013e3182a50148. discussion 579-581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Haider AH, Ong’uti S, Efron DT, et al. Association between hospitals caring for a disproportionately high percentage of minority trauma patients and increased mortality: a nationwide analysis of 434 hospitals. Archives of surgery. 2012;147(1):63–70. doi: 10.1001/archsurg.2011.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sears ED, Chung KC. Future Education and Practice Initiatives in Hand Surgery: Improving Fulfillment of Patient Needs. Hand clinics. 2014;30(3):377–386. doi: 10.1016/j.hcl.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 35.Borman KR, Vick LR, Biester TW, Mitchell ME. Changing demographics of residents choosing fellowships: longterm data from the American Board of Surgery. Journal of the American College of Surgeons. 2008;206(5):782–788. doi: 10.1016/j.jamcollsurg.2007.12.012. [DOI] [PubMed] [Google Scholar]
- 36.Werner RM, Goldman LE, Dudley RA. Comparison of change in quality of care between safety-net and non-safety-net hospitals. Jama. 2008;299(18):2180–2187. doi: 10.1001/jama.299.18.2180. [DOI] [PubMed] [Google Scholar]
- 37.Allison JJ, Kiefe CI, Weissman NW, et al. Relationship of hospital teaching status with quality of care and mortality for Medicare patients with acute MI. Jama. 2000;284(10):1256–1262. doi: 10.1001/jama.284.10.1256. [DOI] [PubMed] [Google Scholar]
- 38.Dimick JB, Cowan JA, Jr., Colletti LM, Upchurch GR., Jr. Hospital teaching status and outcomes of complex surgical procedures in the United States. Archives of surgery. 2004;139(2):137–141. doi: 10.1001/archsurg.139.2.137. [DOI] [PubMed] [Google Scholar]
- 39.Dimick C. The project management plus: project management skills create opportunities for HIM professionals. Journal of AHIMA / American Health Information Management Association. 2011;82(8):28–31. [PubMed] [Google Scholar]
- 40.Diercks DB, Roe MT, Chen AY, et al. Prolonged emergency department stays of non-ST-segment-elevation myocardial infarction patients are associated with worse adherence to the American College of Cardiology/American Heart Association guidelines for management and increased adverse events. Annals of emergency medicine. 2007;50(5):489–496. doi: 10.1016/j.annemergmed.2007.03.033. [DOI] [PubMed] [Google Scholar]
- 41.Pines JM, Localio AR, Hollander JE, et al. The impact of emergency department crowding measures on time to antibiotics for patients with community-acquired pneumonia. Annals of emergency medicine. 2007;50(5):510–516. doi: 10.1016/j.annemergmed.2007.07.021. [DOI] [PubMed] [Google Scholar]
- 42.Schull MJ, Vermeulen M, Slaughter G, Morrison L, Daly P. Emergency department crowding and thrombolysis delays in acute myocardial infarction. Annals of emergency medicine. 2004;44(6):577–585. doi: 10.1016/j.annemergmed.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 43.Hwang U, Richardson LD, Sonuyi TO, Morrison RS. The effect of emergency department crowding on the management of pain in older adults with hip fracture. Journal of the American Geriatrics Society. 2006;54(2):270–275. doi: 10.1111/j.1532-5415.2005.00587.x. [DOI] [PubMed] [Google Scholar]
- 44.Pines JM, Morton MJ, Datner EM, Hollander JE. Systematic delays in antibiotic administration in the emergency department for adult patients admitted with pneumonia. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2006;13(9):939–945. doi: 10.1197/j.aem.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 45.Sun BC, Hsia RY, Weiss RE, et al. Effect of emergency department crowding on outcomes of admitted patients. Annals of emergency medicine. 2013;61(6):605–611. doi: 10.1016/j.annemergmed.2012.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Godina M. Early microsurgical reconstruction of complex trauma of the extremities. Orthopedic Trauma Directions. 2006;4(05):29–35. doi: 10.1097/00006534-198609000-00001. [DOI] [PubMed] [Google Scholar]
- 47.Chen C, Scheffler G, Chandra A. Massachusetts’ health care reform and emergency department utilization. New England Journal of Medicine. 2011;365(12):e25. doi: 10.1056/NEJMp1109273. [DOI] [PubMed] [Google Scholar]
- 48.Institute Of M IOM report: the future of emergency care in the United States health system. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2006;13(10):1081–1085. doi: 10.1197/j.aem.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 49.Alavi-Moghaddam M, Forouzanfar R, Alamdari S, et al. Application of Queuing Analytic Theory to Decrease Waiting Times in Emergency Department: Does it Make Sense? Archives of trauma research. 2012;1(3):101–107. doi: 10.5812/atr.7177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Emergency Medical Services at the Crossroads. Institute of Medicine of the National Academies; 2006. [Google Scholar]
- 51.American Society for Surgery of the Hand (ASSH) [Accessed July 6, 2016];Join a Committee. 2016 https://www.assh.org/Member-Resources/Get-Involved/Join-a-Committee.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.