Abstract
Background
Delirium is a frequent complication after cardiac surgery and its occurrence is associated with poor outcomes. The purpose of this study was to investigate the impact of perioperative dexmedetomidine administration on the incidence of delirium in elderly patients after cardiac surgery.
Methods
This randomized, double-blinded, and placebo-controlled trial was conducted in two tertiary hospitals in Beijing between December 1, 2014 and July 19, 2015. Eligible patients were randomized into two groups. Dexmedetomidine (DEX) was administered during anesthesia and early postoperative period for patients in the DEX group, whereas normal saline was administered in the same rate for the same duration for patients in the control (CTRL) group. The primary endpoint was the incidence of delirium during the first five days after surgery. Secondary endpoints included the cognitive function assessed on postoperative days 6 and 30, the overall incidence of non-delirium complications within 30 days after surgery, and the all-cause 30-day mortality.
Results
Two hundred eighty-five patients were enrolled and randomized. Dexmedetomidine did not decrease the incidence of delirium (4.9% [7/142] in the DEX group vs 7.7% [11/143] in the CTRL group; OR 0.62, 95% CI 0.23 to 1.65, p = 0.341). Secondary endpoints were similar between the two groups; however, the incidence of pulmonary complications was slightly decreased (OR 0.51, 95% CI 0.26 to 1.00, p = 0.050) and the percentage of early extubation was significantly increased (OR 3.32, 95% CI 1.36 to 8.08, p = 0.008) in the DEX group. Dexmedetomidine decreased the required treatment for intraoperative tachycardia (21.1% [30/142] in the DEX group vs 33.6% [48/143] in the CTRL group, p = 0.019), but increased the required treatment for postoperative hypotension (84.5% [120/142] in the DEX group vs 69.9% [100/143] in the CTRL group, p = 0.003).
Conclusions
Dexmedetomidine administered during anesthesia and early postoperative period did not decrease the incidence of postoperative delirium in elderly patients undergoing elective cardiac surgery. However, considering the low delirium incidence, the trial might have been underpowered.
Trial Registration
ClinicalTrials.gov NCT02267538
Introduction
Delirium is a common complication after cardiac surgery, with reported incidences varied from 3% to 47% [1]. The occurrence of delirium after cardiac surgery is associated with worse outcomes; these include increased rate of complications, prolonged duration of mechanical ventilation, prolonged length of stay in ICU and hospital, and increased medical expenses during hospitalization, as well as increased readmission rate, compromised long-term cognitive function, decreased physical ability and life quality, and elevated long-term mortality after hospital discharge [2, 3]. The pathogenesis of postoperative delirium is not fully understood whilst previous studies demonstrated that deep anesthesia during surgery [4, 5] and use of high doses opiates and/or sedatives after surgery [6, 7] are important predisposing factors.
Dexmedetomidine is a highly selective alpha 2-adrenoceptor agonist with anxiolytic, sedative, and analgesic properties [8], and is widely used as an adjuvant during general anesthesia and for sedation during mechanical ventilation after surgery [9]. Studies showed that, for patients undergoing cardiac surgery, use of dexmedetomidine during general anesthesia decreased the consumption of opioid and other anesthetic drugs [10,11], and use of dexmedetomidine for sedation after surgery shortened the duration of mechanical ventilation and decreased the incidence of delirium [12,13]. We hypothesized that use of dexmedetomidine as an anesthetic adjuvant during cardiac surgery decreased the incidence of delirium, possibly by sparing the consumption of general anesthetics. Evidence in this aspect was still lacking. The purpose of this study was to investigate the effect of dexmedetomidine administered during and shortly after cardiac surgery on the incidence of delirium in elderly patients (age of 60 years or over).
Methods
Study design
This was a randomized, double-blind, and placebo-controlled two-center trial. The study protocol (S1 Protocol) was approved by the Ethics Committees of Peking University First Hospital (2014–805) and Beijing Fuwai Hospital (2015–646), and was registered with ClinicalTrials.gov number, NCT02267538. Written informed consent was obtained from each patient or, if the patient could not provide informed consent, from the surrogate of the patient.
Participants
Potential participants were screened the day before surgery. The inclusion criteria were elderly patients (age ≥ 60 years) who were scheduled to undergo elective coronary artery bypass graft and/or valve replacement surgery. Patients who met any of the following criteria were excluded: (1) previous history of schizophrenia, epilepsy, Parkinson disease, or severe dementia; (2) inability to communicate because of severe visual/auditory dysfunction or language barrier; (3) previous history of functional neurosurgery or brain injury; (4) preoperative sick sinus syndrome, severe bradycardia (heart rate < 50 beat per minute), second-degree or above atrioventricular block without pacemaker; (5) severe hepatic insufficiency (Child-Pugh grades C); or (6) severe renal insufficiency (requirement of renal replacement therapy); (7) patient refused to participate in the study.
Randomization, intervention and anesthesia management
Center-stratified randomization with a block size of 4 was done using the SAS statistical package version 9.3 (SAS Institute, Cary, NC, USA) by an independent biostatistician. Study drugs, either dexmedetomidine hydrochloride 200 μg /2 ml or 0.9% sodium chloride 2 ml, were provided as clear aqueous solutions in the same 3 ml bottles (manufactured by Jiangsu Hengrui Pharmaceutical Co., Ltd., China) and encoded according to the randomization order by an independent pharmacist who did not participated in the rest of the study. The randomization results were then sealed in sequentially numbered letters and stored at the site of investigation until the end of the study.
During the study period, a study coordinator distributed the study drugs according to the recruitment ranking number and recorded the study drug codes in the Case Report Form. Study drugs were diluted with normal saline to 50 ml before administration, for dexmedetomidine the final concentration was 4 μg/ml. In the operating room, study drug infusion was started once the intravenous access was established, firstly at a rate of [0.9 × kg] ml/h (i.e., 0.6 μg/kg for dexmedetomidine) for 10 minutes, then at a rate of [0.1 × kg] ml/h (i.e., 0.4 μg·kg-1·h-1 for dexmedetomidine) until the end of surgery. After surgery, study drug infusion was continued at a rate of [0.025 × kg] ml/h (i.e., 0.1 μg·kg-1·h-1 for dexmedetomidine) until the end of mechanical ventilation. All investigators, healthcare team members and patients were blinded to the treatment group assignment throughout the study period.
Premedication could be administered before anesthesia according to patients’ status. Anesthesia was induced with midazolam, etomidate, sufentanil, and propofol, and was maintained with sufentanil and propofol infusion and/or sevoflurane inhalation, with a target bispectral index (BIS) between 40 and 60. During surgery, hemodynamics was carefully maintained by adjusting fluid infusion and using inotropic and/or vasoactive drugs. All patients were transferred to the intensive care unit (ICU) after surgery. Patient-controlled analgesia pump was applied whenever possible. For patients who required additional analgesia, opiates were administered either intravenously or orally. For patients who required sedation (i.e., patients undergoing mechanical ventilation), propofol intravenous infusion was the first choice, with a target Richmond Agitation Sedation Scale (RASS) [14] maintained between -2 and +1. Midazolam was administered when necessary. For all enrolled patients, penehyclidine hydrochloride and scopolamine were prohibited, and open-labled dexmedetomidine was not allowed during the whole study period.
Outcome assessment and follow-up schedule
Prior to the study, two investigators (XL and YZ) who performed interview and delirium assessments were trained to follow standard procedures and to use the Confusion Assessment Method (CAM) and the CAM for the Intensive Care Unit (CAM-ICU) by a psychiatrist. Both CAM and CAM-ICU make the diagnosis according to four features of delirium: (1) acute onset of mental status changes or a fluctuating course; (2) inattention; (3) disorganized thinking; and (4) altered level of consciousness. To have delirium diagnosed, a patient must display features 1 and 2, with either 3 or 4 [15,16].
Before surgery, detailed baseline data including demographics, comorbidities, medication, laboratory test results, diagnosis, and ASA classification were collected. Preoperative evaluations were performed with Mini-Mental State Examination (MMSE, scores range from 0 to 30, with higher scores indicating better cognitive function), Hospital Anxiety and Depression Scale (HADS, scores range from 0 to 42, with higher scores indicating more severe anxiety and depression), Barthel Index (BI, scores range from 0 to 100, with higher scores indicating better daily life activity), and CAM.
Intraoperative data including type of surgery, duration of anesthesia and surgery, names and doses of anesthetic drugs, use and duration of cardiopulmonary bypass and aortic cross-clamping, transfusion of blood products, and fluid balance were recorded. The average BIS values from 5 minutes after anesthesia induction to the end of surgery were acquired. After ICU admission, heart rate, blood pressure, respiratory rate, pulse oxygen saturation, urine output and fluid infusion were recorded hourly. Use of analgesics, sedatives, vasoactive drugs and occurrence of adverse events were documented. Acute Physiology and Chronic Health Evaluation II (APACHE II, scores range from 0 to 71, with higher scores indicating more severe illness) was scored according to the worst condition during the first 24 hours in the ICU.
Delirium was assessed daily (from 8 to 10 am) during postoperative days 1 to 5. Non-intubated patients were assessed with the CAM; intubated patients were assessed with the CAM-ICU. Before delirium assessment, the level of sedation/agitation was evaluated with the Richmond Agitation Sedation Scale (RASS) [14]. If the patient was deeply sedated or was unarousable (-4 or -5 on the RASS), delirium assessment was stopped and the patient was noted as comatose. If the RASS was above -4 (-3 through +5), delirium assessment was performed. For patients who were discharged or died before postoperative day 5, the results of last delirium assessment were used as the missing data. After the completion of daily delirium assessment, the intensity of pain both at rest and with coughing was evaluated using the numeric rating scale (NRS, an 11-point scale where 0 indicated no pain and 10 indicated the worst pain) and the subjective sleep quality was also evaluated using the NRS (an 11-point scale where 0 indicated the best sleep quality and 10 indicated the worst sleep experience).
On postoperative day 6, cognitive function was reevaluated using the MMSE; the duration of mechanical ventilation, the length of stay in the ICU and hospital after surgery, and the occurrence of non-delirium complications were recorded. Non-delirium complications were defined to be any medical conditions other than delirium that required therapeutic intervention and occurred within 30 days after surgery. On postoperative day 30, patients were followed-up by telephone interview; any conditions that led to re-hospitalization were documented; cognitive function was evaluated using Chinese version of Telephone Interview for Cognitive Status-modified scale (m-TICS, scores range from 0 to 48, with higher scores indicating better cognitive function).
The primary endpoint was the incidence of delirium within the first five days after surgery. Secondary endpoints included the cognitive function assessed on postoperative days 6 and 30, the overall incidence of non-delirium complications within 30 days after surgery, and the all-cause 30-day mortality. Other predefined endpoints included the severity of pain and subjective sleep quality during the first 5 days after surgery, the duration of mechanical ventilation, the length of stay in ICU and hospital after surgery, and the re-hospitalization rate within 30 days after surgery.
Statistical analysis
Sample size estimation
According to published data and our own results, we assumed that the incidence of delirium after cardiac surgery was 30% in the CTRL group patients [1,17]. A meta-analysis showed that the incidence of delirium was reduced by 63% (RR 0.36, 95% CI 0.21 to 0.64) when dexmedetomidine was used for sedation in patients after cardiac surgery [12]. We conservatively assumed that the incidence of delirium would be reduced by 50% in the dexmedetomidine group. With significance and power set at 0.05 (two-sided) and 80% respectively, the sample size required to detect differences was 236 patients. Taking into account a drop-out rate of about 17%, we planned to enroll 284 patients. Sample size calculation was performed with the PASS 11.0 software (StataCorp. LP, College Station, TX).
Outcome analyses
Continuous variables with normal distribution were analyzed using the unpaired t-test. Continuous variables with abnormal distribution or ordinal data were analyzed with Mann-Whitney U test. Median differences were calculated with the Hodges-Lehmann estimator. Categorical variables were analyzed using the Chi-squared test, continuity correction Chi-squared test or Fisher exact test, with odds ratio (OR) calculated by logistic analysis. Time-to-event results were analyzed using the Kaplan-Meier survival analysis, with the difference between groups tested by the log-rank test and hazard ratio (HR) calculated by Cox regression analysis.
Outcome and safety data were analyzed in the intent-to-treat population. We also did per-protocol analysis for the primary endpoint; patients who were randomized but did not complete study drug administration were excluded from per protocol analysis. Statistical analysis was performed with SAS statistical package (version 9.3, SAS Institute, Cary, NC, USA) by statisticians in Peking University First Hospital and Beijing Children’s Hospital, with two-sided P values of less than 0.05 as statistical significance. This manuscript adhered to the applicable CONSORT guideline.
Results
Patient population
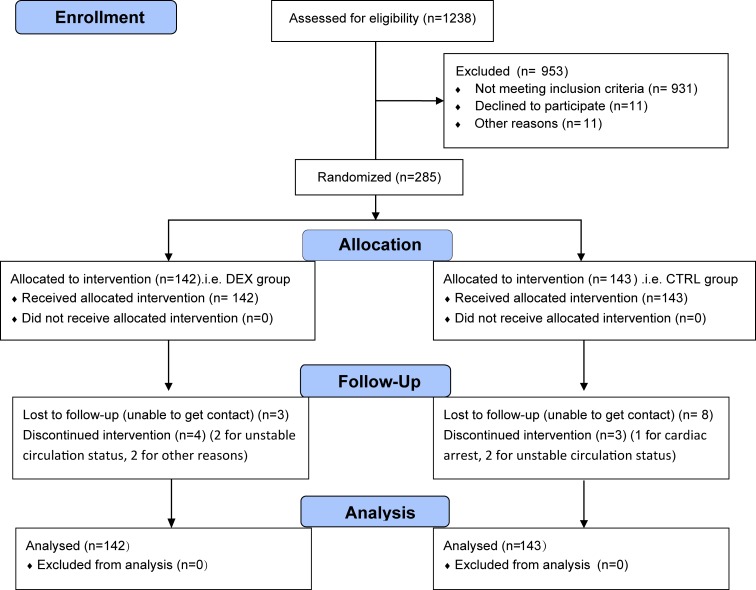
From December 1, 2014 to July 19, 2015, 1238 patients were screened for eligibility; 307 patients met the inclusion/exclusion criteria; 285 patients gave consents and were randomized into the study, among them 142 in the DEX group and 143 in the CTRL group. During the study period, postoperative study drug infusion was not completed in 7 patients (4 cases in the DEX group and 3 cases in the CTRL group) because of cardiac arrest, unstable circulation status or other reasons in the ICU; 6 patients died within 30 days after surgery (2 cases in the DEX group and 4 cases in the CTRL group). At postoperative day 30, 11 patients (3 cases in the DEX group and 8 cases in the CTRL group) were lost to follow-up. Each of these patients was included in the final Intention-to-Treat analysis (Fig 1).
Fig 1. Flow Diagram of the study.
DEX, dexmedetomidine; CTRL, control; ITT, Intention-to-Treat.
The percentage of patients with baseline hyperlipidemia was lower in the DEX group than in the CTRL Group (p = 0.005). During intraoperative period, the median average BIS value was lower in the DEX group than in the CTRL group (median 42 [interquartile range 38 to 46] with DEX vs 44 [41 to 49] with CTRL, p < 0.001). There were no significant differences between the two groups regarding other baseline parameters and perioperative variables (Tables 1 and 2).
Table 1. Baseline data.
| CTRL group (n = 143) | DEX group (n = 142) | |
|---|---|---|
| Age, year | 67.5 ± 5.3 | 66.4 ± 5.4 |
| Male gender | 102 (71.3%) | 95 (66.9%) |
| BMI, kg/m2 | 24.9 ± 2.8 | 25.3 ± 3.4 |
| Education, year | 9 (5 to 10) | 9 (5 to 12) |
| Comorbidities | ||
| Hypertension | 91 (63.6%) | 89 (62.7%) |
| Arrhythmia | 29 (20.3%) | 32 (22.5%) |
| Stroke | 33 (23.1%) | 26 (18.3%) |
| COPD | 4 (2.8%) | 7 (4.9%) |
| Diabetes Mellitus | 49 (34.3%) | 43 (30.3%) |
| Hyperlipidemiaa | 61 (42.7%) | 38 (26.8%) |
| Chronic kidney diseaseb | 7 (4.9%) | 1 (0.7%) |
| Tumorc | 3 (2.1%) | 7 (4.9%) |
| Thyroid diseased | 3 (2.1%) | 4 (2.8%) |
| Smokinge | 66 (46.2%) | 51 (35.9%) |
| Acute myocardial infarction | 11 (7.7%) | 17 (12.0%) |
| Preoperative medications | ||
| CCB | 45 (31.5%) | 33 (23.2%) |
| ACEI/ARB | 46 (32.2%) | 50 (35.2%) |
| β-blocker | 66 (46.2%) | 63 (44.4%) |
| Statins | 75 (52.4%) | 63 (44.4%) |
| Antiplatelet drugsf | 82 (57.3%) | 85 (59.9%) |
| EuroSCORE | 3 (2 to 5) | 3 (2 to 5) |
| History of surgery | 52 (36.4%) | 55 (38.7%) |
| History of general anesthesia | 24 (16.8%) | 24 (16.9%) |
| NYHA function classg | (n = 132) | (n = 125) |
| I | 2 (1.5%) | 2 (1.6%) |
| II | 92 (69.7%) | 87 (69.6%) |
| III | 36 (27.3%) | 33 (26.4%) |
| IV | 2 (1.5%) | 3 (2.4%) |
| LVEF% | 64.8 (58.2 to 70.6) | 64.4 (56.2 to 70.4) |
| ASA Classification | ||
| II | 2 (1.4%) | 1 (0.7%) |
| III | 129 (90.2%) | 128 (90.1%) |
| IV | 12 (8.4%) | 13 (9.2%) |
| MMSE score | 29 (28 to 30) | 29 (28 to 30) |
| HAD score | 8 (4 to 12) | 8 (4 to 12) |
| BI score | 100 (95 to 100) | 100 (95 to 100) |
| Delirium | 0 (0.0%) | 0 (0.0%) |
Results are presented as mean ± standard deviation, number (%) or median (interquartile range).
BMI, body mass index; COPD, chronic obstructive pulmonary disease; CCB, calcium channel blocker; ACEI/ARB, angiotensin converting enzyme inhibitor/angiotensin receptor blocker; NYHA, New York Heart Association; EuroSCORE, European System for Cardiac Operative Risk Evaluation; MMSE, Mini-Mental State Examination; HAD, Hospital Anxiety and Depression Scale; BI, Barthel Index.
a Serum total cholesterol > 5.18 mmol/L, triglyceride > 1.7mmol/L, or low density lipoprotein > 3.37 mmol/L
b Diagnosed according to KDIGO criteria
c Including breast cancer, lung cancer, gastric cancer, rectal cancer, and atrial myxoma
d Including thyroid nodule/adenoma/cancer, hyperthyroidism/hypothyroidism, and history of thyroid surgery
eSmoking regularly for more than 1 year
f Including aspirin, clopidogrel, and ticagrelor
g exclude patients with acute myocardial infarction.
Table 2. Intra- and postoperative data.
| CTRL group (n = 143) | DEX group (n = 142) | P value | |
|---|---|---|---|
| Premedication | |||
| Morphinea, mg | 10 (5 to 10) | 10 (5 to 10) | 0.500 |
| Estazolamb, mg | 2 (1 to 2) | 2 (1 to 2) | 0.569 |
| Duration of anesthesia, min | 256 (217 to 300) | 250 (220 to 294) | 0.889 |
| Dose of anesthetics | |||
| Midazolamc, mg | 3 (2 to 5) | 3 (2 to 5) | 0.171 |
| Propofol, mg | 600 (400 to 920) | 520 (300 to 825) | 0.098 |
| Etomidated, mg | 20 (20 to 20) | 20 (20 to 20) | 0.702 |
| Sufentanile, μg | 200 (150 to 300) | 225 (140 to 300) | 0.967 |
| Fentanyle, mg | 1.88 (1.70 to 2.03) | 1.55 (1.50 to 1.60) | 0.133 |
| Average BIS valuef | 44 (41 to 49) (n = 128) | 42 (38 to 46) (n = 130) | < 0.001 |
| Duration of surgery, min | 185 (157 to 235) | 180 (159 to 225) | 0.651 |
| Type of surgery | 0.731 | ||
| CABG | 103 (72.0%) | 101 (71.1%) | |
| Valve replacement | 19 (13.3%) | 23 (16.2%) | |
| CABG and valve replacement | 21 (14.7%) | 18 (12.7%) | |
| Use of CPB | 82 (57.3%) | 82 (57.7%) | 0.945 |
| Duration of CPBg, min | 101 (81 to 130) | 105 (84 to 129) | 0.979 |
| Duration of AOCg, min | 72 (49 to 92) | 71 (59 to 91) | 0.477 |
| Duration of hypothermiag, min | 60 (40 to 83) | 59 (48 to 77) | 0.395 |
| APACHE II score | 8 (7 to 11) | 8 (6 to 10) | 0.099 |
| Use of PCA | 15 (10.5%) | 20 (14.1%) | 0.355 |
| Additional sedatives/analgesics | |||
| Propofolh, mg | 700 (400 to 1200) | 600 (400 to 1000) | 0.299 |
| Benzodiazepinesi | 61 (42.7%) | 76 (53.5%) | 0.067 |
| Analgesics intravenouslyj | 10 (7.0%) | 9 (6.3%) | 0.825 |
| Analgesics orallyk | 74 (51.7%) | 87 (61.3%) | 0.105 |
| Total duration of study drug Infusion, h | 18.7 (13.3 to 23.5) | 18.7 (13.1 to 21.6) | 0.279 |
Results are presented as mean ± standard deviation, number (%) or median (interquartile range).
BIS, bispectral index; CABG, coronary artery bypass graft; CPB, cardiopulmonary bypass; AOC, aortic cross clamping; APACHE, acute physiology and chronic health evaluation; PCA, patient-controlled analgesia.
a Data of 130 patients (63 in CTRL group and 67 in DEX group) who received morphine as premedication
b data of 261 patients (128 in CTRL group and 133 in DEX group) who received estazolam as premedication
c data of 280 patients (141 in CTRL group and 139 in DEX group) who received midazolam during anesthesia
d data of 125 patients (61 in CTRL group and 64 in DEX group) who received etomidate during anesthesia
e data of 279 patients (139 in CTRL group and 140 in DEX group) who received sufentanil and 6 patients (4 in CTRL group and 2 in DEX group) who received fentanyl during anesthesia
f average BIS value from 5 minutes after anesthesia induction to the end of the surgery. Data were missed in 27 patients (15 in CTRL group and 12 in DEX group)
g data of patients who underwent surgery with CPB
h data of 173 patients (88 in CTRL group and 85 in DEX group) who received propofol during the postoperative period
I Including diazepam, lorazepam, midazolam, and estazolam
j Including morphine, fentanyl, and pethidine
k Including oxycodone-acetaminophen tablet and morphine sulfate sustained-release tablet.
Effectiveness analysis
There was no significant difference between the two groups regarding the incidence of delirium during the first 5 days after surgery (4.9% [7/142] in the DEX group vs 7.7% [11/143] in the CTRL group; odds ratio [OR] 0.62, 95% CI 0.23 to 1.65; p = 0.341) (Table 3). Per-protocol analysis also showed no significant difference in the incidence of delirium between groups (2.9% [4/138] in the DEX group vs 5.7% [8/140] in the CTRL group; OR 0.49, 95% CI 0.15 to 1.68; p = 0.257).
Table 3. Effectiveness outcomes.
| CTRL group (n = 143) | DEX group (n = 142) | Estimated effects | P value | |
|---|---|---|---|---|
| Primary outcome | ||||
| Incidence of delirium within the first 5 days after surgery | 11 (7.7%) | 7 (4.9%) | 0.62 (0.23 to 1.65) | 0.341 |
| Secondary outcomes | ||||
| MMSE score on postoperative day 6a | 29 (27 to 30) | 29 (27 to 30) | 0 (0 to 0) | 0.830 |
| m-TICS score on postoperative day 30b | 34 (32 to 36) | 34 (32 to 37) | 0 (-1 to 0) | 0.405 |
| Incidence of non-delirium complications within 30 days after surgery | 84 (58.7%) | 73 (51.4%) | 0.74 (0.47 to 1.19) | 0.214 |
| Stroke | 3 (2.1%) | 3 (2.1%) | 1.01 (0.20 to 5.08) | 0.993 |
| New onset arrythmiac | 51 (35.7%) | 42 (29.6%) | 0.76 (0.46to 1.25) | 0.274 |
| Pulmonary complicationsd | 27 (18.9%) | 15 (10.6%) | 0.51 (0.26 to 1.00) | 0.050 |
| Upper gastrointestinal bleedinge | 4 (2.8%) | 2 (1.4%) | 0.50 (0.09 to 2.75) | 0.423 |
| Surgical bleedingf | 3 (2.1%) | 3 (2.1%) | 1.01 (0.20 to 5.08) | 0.993 |
| Wound dehiscence or infectiong | 7 (4.9%) | 11 (7.7%) | 1.63 (0.61 to 4.34) | 0.326 |
| Acute kidney injuryh | 44 (30.8%) | 37 (26.1%) | 0.79 (0.47 to 1.33) | 0.378 |
| IABP assistance | 12 (8.4%) | 6 (4.2%) | 0.48 (0.18 to 1.32) | 0.156 |
| All cause 30-day mortalityi | 4 (3.0%) | 2 (1.4%) | 0.48 (0.09 to 2.66) | 0.399 |
| Other outcomes | ||||
| Pain score after surgery, at restj | ||||
| Day 1 | 3 (2 to 5) | 3 (1 to 5) | 0 (-1 to 0) | 0.596 |
| Day 2 | 3 (2 to 5) | 4 (2 to 5) | 0 (-1 to 0) | 0.743 |
| Day 3 | 2 (2 to 4) | 3 (2 to 4) | 0 (-1 to 0) | 0.282 |
| Day 4 | 2 (1 to 3) | 2 (1 to 3) | 0 (0 to 0) | 0.368 |
| Day 5 | 1(1 to 2) | 2 (1 to 2) | 0 (0 to 0) | 0.397 |
| Pain score after surgery, with coughingj | ||||
| Day 1 | 4 (3 to 6) | 4 (2 to 6) | 0 (-1 to 0) | 0.486 |
| Day 2 | 4 (3 to 6) | 5 (3 to 6) | 0 (-1 to 0) | 0.414 |
| Day 3 | 4 (2 to 5) | 4 (3 to 5) | 0 (-1 to 0) | 0.187 |
| Day 4 | 3 (2 to 4) | 3 (2 to 4) | 0 (-1 to 0) | 0.127 |
| Day 5 | 2 (2 to 3) | 2 (2 to 3) | 0 (0 to 0) | 0.378 |
| Subjective sleep quality after surgery, scorek | ||||
| Day 1 | 2 (0 to 6) | 2 (0 to 5) | 0 (0 to 0) | 0.777 |
| Day 2 | 3 (2 to 6) | 3 (2 to 6) | 0 (-1 to 1) | 0.919 |
| Day 3 | 2 (2 to 4) | 2 (2 to 5) | 0 (0 to 0) | 0.835 |
| Day 4 | 2 (0 to 4) | 2 (1 to 4) | 0 (0 to 0) | 0.321 |
| Day 5 | 2 (0 to 2) | 2 (0 to 3) | 0 (0 to 0) | 0.174 |
| Incidence of coma within the first 5 days after surgery | 2 (1.4%) | 2 (1.4%) | 1.00 (0.14 to 7.25) | 0.994 |
| Duration of delirium among patients who developed delirium, d | 2 (1 to 4) | 2 (1 to 3) | 1 (-1 to 2) | 0.328 |
| Duration of mechanical ventilation, h (median [95% CI]) | 15.0 (13.9 to 16.1) | 15.0 (13.7 to 16.3) | 1.28 (1.01 to 1.63) | 0.044 |
| Extubation within 24 hours after surgery | 122 (85.3%) | 135 (95.1%) | 3.32 (1.36 to 8.08) | 0.008 |
| Length of stay in ICU after surgery, h (median [95% CI]) | 46.0 (44.8 to 47.2) | 45.0 (43.5 to 46.5) | 1.03 (0.82 to 1.31) | 0.788 |
| Length of stay in hospital after surgery, d (median [95% CI]) | 9 (8 to 10) | 9 (8 to 10) | 0.97 (0.77 to 1.23) | 0.826 |
| Re-hospitalization within 30 days after surgeryi | 15 (11.1%) | 16 (11.5%) | 1.04 (0.49 to 2.20) | 0.917 |
Results are presented as number (%) or median (interquartile range), unless otherwise indicated. Estimated effects were calculated in the direction of DEX vs. or minus CTRL; results are presented as odds ratio (95% CI), median difference (95% CI) or hazard ratio (95% CI).
MMSE, Mini-Mental State Examination; m-TICS, modified Telephone Interview for Cognitive Status; IABP, intra-aortic balloon pump; ICU, intensive care unit; CI, confidence interval.
a 5 patients (3 in CTRL group and 2 in DEX group) did not complete the MMSE test on postoperative day 6
b 17 patients (12 in CTRL group and 5 in DEX group) did not complete the m-TICS test on postoperative day 30
c including new onset atrial fibrillation, II/III degree atrioventricular block, frequently premature ventricular contractions, premature ventricular contractions (bigeminy/trigeminy), ventricular tachycardia, and ventricular fibrillation
d including pulmonary infection, pneumothorax and pleural effusion needed intervention (closed drainage of pleural cavity, needle/catheter insertion for drainage, lung recruitment maneuvers)
e positive occult blood test results in gastric contents or stool with decreased hemoglobin, and requirement of blood transfusion
f bleeding after surgery that required secondary surgical hemostasis
g need further debridement and /or suturing
h diagnosed according to KDIGO criteria
I 11 patients (8 in CTRL group and 3 in DEX group) were lost to follow up
j assessed with numeric rating scale where 0 = no pain and 10 = the most severe pain
k assessed with numeric rating scale where 0 = the best possible sleep and 10 = the worst possible sleep.
The MMSE Score assessed on postoperative day 6 (median difference 0, 95% CI 0 to 0; p = 0.830) and m-TICS score assessed on postoperative day 30 (median difference 0, 95% CI -1 to 0; p = 0.405) were similar between the two groups; there were no significant differences between the two groups regarding the overall incidence of non-delirium complications within 30 days after surgery (OR 0.74, 95% CI 0.47 to 1.19; p = 0.214) and all-cause 30-day mortality (OR 0.48, 95% CI 0.09 to 2.66, p = 0.399), despite of the fact that the incidence of pulmonary complications tended to be lower in the DEX group than in the CTRL group (OR 0.51, 95% CI 0.26 to 1.00; p = 0.050) (Table 3).
The intensity of pain both at rest and with coughing as well as the subjective sleep quality at postoperative days 1 to 5 were similar between the two groups. The duration of mechanical ventilation was shorter in the DEX group than in the CTRL group (hazard ratio [HR] 1.28, 95% CI 1.01 to 1.63, p = 0.044); the percentage of patients extubated within 24 hours after surgery was higher in the DEX group than in the CTRL group (OR 3.32, 95% CI 1.36 to 8.08; p = 0.008). There were no significant differences between the two groups regarding the incidence of coma within 5 days after surgery, the duration of delirium, the lengths of stay in ICU and hospital after surgery, and the rate of re-hospitalization within 30 days after surgery (Table 3, S1 Dataset).
Safety analysis
The percentage of patients requiring intraoperative treatment for tachycardia was lower in the DEX group than in the CTRL group (21.1% [30/142] in the DEX Group vs 33.6% [48/143] in the CTRL Group; p = 0.019); on the other hand, the percentage of patients requiring postoperative treatment for hypotension was higher in DEX group than in the CTRL group (84.5% [120/142] in the DEX Group vs 69.9% [100/143] in the CTRL Group; p = 0.003) (Table 4).
Table 4. Adverse events.
| CTRL group (n = 143) | DEX group (n = 142) | P value | |
|---|---|---|---|
| Intraoperative period | |||
| Bradycardiaa | 14 (9.8%) | 21 (14.8%) | 0.199 |
| Treatment for bradycardiab | 11 (7.7%) | 19 (13.4%) | 0.118 |
| Hypotensionc | 10 (7.0%) | 10 (7.0%) | 0.987 |
| Treatment for hypotensiond | 101 (70.6%) | 112 (78.9%) | 0.109 |
| Treatment for tachycardiae | 48 (33.6%) | 30 (21.1%) | 0.019 |
| Treatment for hypertensionf | 45 (31.5%) | 35 (24.6%) | 0.200 |
| Postoperative period | |||
| Bradycardiaa | 6 (4.2%) | 2 (1.4%) | 0.287 |
| Treatment for bradycardiab | 5 (3.5%) | 3 (2.1%) | 0.727 |
| Hypotensionc | 10 (7.0%) | 5 (3.5%) | 0.189 |
| Treatment for hypotensiond | 100 (69.9%) | 120 (84.5%) | 0.003 |
| Treatment for tachycardiae | 11 (7.7%) | 14 (9.9%) | 0.518 |
| Treatment for hypertensionf | 63 (44.1%) | 48 (33.8%) | 0.076 |
Results are presented as number (%).
a Heart rate < 45 beat per minute or a decrease of more than 30% from baseline (average value in the ward), and lasting for at least 5 minutes
b intrasvenous injection of atropine, and/or intravenous infusion of isoprenaline
c a decrease of systolic blood pressure of more than 30% from baseline (average value in the ward) and lasting for at least 15 minutes
d intravenous administration of vasoactive and/or inotropic drugs, including ephedrine, phenylephrine, aramine, dopamine, norepinephrine, epinephrine, dobutamine, milrinone, and/or levosimendan
e intravenous administration of esmolol
f intravenous administration of sodium nitroprusside, urapidil, nicardipine, and/or ditiazem.
Discussion
Our results showed that for elderly patients undergoing elective cardiac surgery, dexmedetomidine administered during anesthesia and early postoperative period did not decrease the incidence of delirium within the first 5 days after surgery. The results of cognitive function assessed on postoperative days 6 and 30, the overall incidence of non-delirium complications within 30 days after surgery as well as the all-cause 30-day mortality were similar between the two groups. Dexmedetomidine infusion decreased the required treatment for intraoperative tachycardia but increased the required treatment for postoperative hypotension.
In the present study, the incidence of delirium in the CTRL group was 7.7%, much lower than our and others’ previous studies [17–21]. The reasons that led to the low delirium incidence in the current patient population may include the followings. Firstly, anticholinergic drugs were less used in the current study. For example, in our previous studies, 39.9% to 46.7% of patients received anticholinergics (especially penehyclidine hydrochloride, an anticholinergic with high blood-brain barrier penetrating property) [17, 18, 21], which might have led to higher incidence of delirium [22, 23]. In the present study, only 10.2% of patients received anticholinergics (only atropine for treatment of bradycardia). Secondly, benzodiazepines were much less used than previously. Benzodiazepines were often used as the main sedatives for patients in the ICU [13, 17, 24], which may increase the incidence of delirium [25, 26]. In the present study, propofol was used as the first choice sedative, which may be responsible for decreasing the incidence of delirium per se [27]. Thirdly, delirium-preventing measures were used more commonly in daily nursing practice, including reorientation, cognitive stimulating, sleep promotion, and hearing/vision aids [28]. Interestingly, some previous studies also reported low incidence of postoperative delirium [29, 30].
Dexmedetomidine has been used for sedation in mechanically ventilated patients after cardiac surgery. In two randomized trials, postoperative sedation with dexmedetomidine reduced the incidence of delirium (1/30 [3%] with dexmedetomidine vs 15/30 [50%] with propofol vs 15/30 [50%] with midazolam; P < 0.001 [13] and 16/91 [17.5%] with dexmedetomidine vs 29/92 [31.5%] with propofol; P = 0.028 [31], respectively). In two other randomized trials, however, use of dexmedetomidine sedation did not reduce the incidences of postoperative delirium despite trends of decrease (13/152 [8.6%] with dexmedetomidine vs 22/147 [15.0%] with morphine; P = 0.088 [32] and 1/32 [3.1%] with dexmedetomidine vs 5/32 [15.6%] with normal saline; P = 0.086 [33], respectively). It should be mentioned that, in the two later studies, droperidol or gabapentin was administered as or as part of the premedication [32,33], which might partially explain the reasons of low delirium incidence [34,35] and non-significant results (i.e., underpowered studies). In the present study, we administered a sedative dose dexmedetomidine during anesthesia but a sub-sedative dose dexmedetomidine during mechanical ventilation after surgery. Our results found that dexmedetomidine did not decrease the incident of delirium. Our neutral results were attributable to several reasons. Firstly, the protocol requested that the BIS value be maintained between 40 and 60 during surgery but the median average BIS value was lower in the DEX group than in the CTRL group, indicating a deeper level of anesthesia in the DEX group. Indeed, deep anesthesia and low BIS was reported to increase the incidence of delirium [4, 5]. Secondly, the dose and timing of postoperative DEX administration was not enough. In previous studies, sedative dose dexmedetomidine decreased the incidence of delirium after cardiac surgery [13, 31]. In a recent study of our group, the effect of low-dose dexmedetomidine (0.1 μg·kg-1·h-1) in decreasing delirium in postoperative ICU patients was dose-dependent [36]. Thirdly, although not statistically significant, slightly more benzodiazepines were administered in patients of the DEX group (P = 0.067 compared with CTRL group). This might have increased the occurrence of delirium and counteracted the effect of dexmedetomidine. Fourthly, the incidence of delirium in the CTRL group of our study was far lower than we expected (7.7% instead of 30%). Therefore, our pre-calculated sample size was insufficient to detect the difference between the two groups. It is true that if the sample size calculation is based on the current incidences of delirium in our present study, 1181 cases in each group are needed to verify the effect of dexmedetomidine.
Dexmedetomidine produces a mild analgesic effect by activating the α2 adrenoceptors in the spine cord [37,38]. Our study did not find significant differences in the NRS pain scores and the use of analgesics after surgery. This was very likely due to a large dose of opiates usually used during cardiac anesthesia which might have masked the analgesic effect of dexmedetomidine. Dexmedetomidine produces a hypnotic effect by activating the endogenous sleep-promoting pathway [39, 40] and improves the sleep quality in mechanically ventilated patients [41]. Our study did not find significant difference in the subjective sleep quality after surgery. As discussed above, this was possibly due to the short duration of dexmedetomidine infusion.
In the present study, use of dexmedetomidine did not decrease the overall incidence of non-delirium complications, but it tended to decrease the incidence of pulmonary complications after surgery. In accordance with this, the duration of mechanical ventilation was shortened and the percentage of extubation within 24 hours after surgery was increased in the DEX group. Preclinical studies demonstrated that dexmedetomidine suppressed oxidative stress and inflammatory response [42], and attenuated the degree of acute lung injury produced by remote organ ischemia/reperfusion [43]. It warrants future study to verify its pulmonary protection. Regarding safety, the use of dexmedetomidine decreased the required treatment for intraoperative tachycardia; however, it increased the required treatment for postoperative hypotension and therefore, its safety, other benefits and long-term outcome are subjected to study further.
There were several limitations in our study. Firstly, our study excluded patients who were unable to communicate due to visual/auditory dysfunction, language barrier or psychiatric disease, and those with severe hepatic or kidney disease. These patients were at a great increased risk of delirium. Therefore, the extrapolation of our study was limited. Secondly, delirium was assessed once daily in the present study. Considering the transient and fluctuating characteristics of delirium, we might have missed some positive cases. Lastly, because of the low incidence of delirium in the CTRL group, this trial was underpowered to detect difference between the two groups. A large sample size randomized trial is needed to further clarify the effects of perioperative dexmedetomidine (S1 CONSORT checklist).
Conclusions
Our study showed that dexmedetomidine administered during anesthesia and early postoperative period did not decrease the incidence of postoperative delirium in elderly patients undergoing elective cardiac surgery. However, considering the low delirium incidence, the trial might have been underpowered. Dexmedetomidine decreased the required treatment for intraoperative tachycardia, but increased the required treatment for postoperative hypotension.
Supporting information
(DOC)
(XLS)
(DOC)
Acknowledgments
The authors gratefully acknowledge Dr. Xin-Yu Sun (MD, Professor, Department of Psychiatrics, Peking University Sixth Hospital, Beijing, China) for her help in psychiatric consultation and training for delirium assessment.
Data availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The study was supported by a Scientific Research Fund (2015) from Peking University First Hospital. Study drugs were manufactured and supplied by Jiangsu Hengrui Medicine Co., Ltd, Jiangsu, China. The study sponsors had no role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication study.
References
- 1.Groen JA, Banayan D, Gupta S, Xu S, Bhalerao S. Treatment of delirium following cardiac surgery. J Card Surg 2012, 27(5):589–593. 10.1111/j.1540-8191.2012.01508.x [DOI] [PubMed] [Google Scholar]
- 2.Witlox J, Eurelings LS, de Jonghe JF, Kalisvaart KJ, Eikelenboom P, van Gool WA. Delirium in elderly patients and the risk of post discharge mortality, institutionalization, and dementia: a meta-analysis. JAMA 2010, 304(4):443–451. 10.1001/jama.2010.1013 [DOI] [PubMed] [Google Scholar]
- 3.Koster S, Hensens AG, van der Palen J. The long-term cognitive and functional outcomes of postoperative delirium after cardiac surgery. Ann Thoric Surg 2009, 87(5):1469–1474. [DOI] [PubMed] [Google Scholar]
- 4.Chan MT, Cheng BC, Lee TM, Gin T. BIS-guided anesthesia decreases postoperative delirium and cognitive decline. J Neurosurg Anesthesiol 2013, 25(1):33–42. 10.1097/ANA.0b013e3182712fba [DOI] [PubMed] [Google Scholar]
- 5.Radtke FM, Franck M, Lendner J, Kruger S, Wernecke KD, Spies CD. Monitoring depth of anaesthesia in a randomized trial decreases the rate of postoperative delirium but not postoperative cognitive dysfunction. Br J Anaesth 2013, 110 Suppl 1:i98–i105. [DOI] [PubMed] [Google Scholar]
- 6.Guenther U, Riedel L, Radtke FM. Patients prone for postoperative delirium: preoperative assessment, perioperative prophylaxis, postoperative treatment. Curr Opin Anaesthesiol 2016. [DOI] [PubMed] [Google Scholar]
- 7.Leung JM, Sands LP, Lim E, Tsai TL, Kinjo S. Does preoperative risk for delirium moderate the effects of postoperative pain and opiate use on postoperative delirium? Am J Geriatr Psychiatry 2013, 21(10):946–956. PMCID: PMC3742555 10.1016/j.jagp.2013.01.069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mo Y, Zimmermann AE. Role of dexmedetomidine for the prevention and treatment of delirium in intensive care unit patients. Ann Pharmacother 2013, 47(6):869–876. 10.1345/aph.1AR708 [DOI] [PubMed] [Google Scholar]
- 9.Gerresheim G, Schwemmer U. Dexmedetomidine. Anesthesist 2013, 62(8):661–674. [DOI] [PubMed] [Google Scholar]
- 10.Abdel-Meguid ME. Dexmedetomidine as anesthetic adjunct for fast tracking and pain control in off-pump coronary artery bypass. Saudi J Anaesth 2013, 7(1):6–8. PMCID: PMC3657928 10.4103/1658-354X.109557 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 11.Khalil MA, Abdel AM. The impact of dexmedetomidine infusion in sparing morphine consumption in off-pump coronary artery bypass grafting. Semin Cardiothorac Vasc Anesth 2013, 17(1):66–71. 10.1177/1089253212463969 [DOI] [PubMed] [Google Scholar]
- 12.Lin YY, He B, Chen J, Wang ZN. Can dexmedetomidine be a safe and efficacious sedative agent in post-cardiac surgery patients? a meta-analysis. Crit Care 2012, 16(5):R169 PMCID: PMC3682268 10.1186/cc11646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maldonado JR, Wysong A, van der Starre PJ, Block T, Miller C, Reitz BA. Dexmedetomidine and the reduction of postoperative delirium after cardiac surgery. Psychosomatics 2009, 50(3):206–217. 10.1176/appi.psy.50.3.206 [DOI] [PubMed] [Google Scholar]
- 14.Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O'Neal PV, Keane KA, et al. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med 2002, 166(10):1338–1344. 10.1164/rccm.2107138 [DOI] [PubMed] [Google Scholar]
- 15.Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA 2001, 286(21):2703–2710. [DOI] [PubMed] [Google Scholar]
- 16.Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI: Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 1990; 113: 941–8. [DOI] [PubMed] [Google Scholar]
- 17.Mu DL, Wang DX, Li LH, Shan GJ, Li J, Yu QJ, et al. High serum cortisol level is associated with increased risk of delirium after coronary artery bypass graft surgery: a prospective cohort study. Crit Care 2010, 14(6):R238 PMCID: PMC3219980 10.1186/cc9393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mu DL, Wang DX, Li LH, Shan GJ, Li J, Yu QJ, et al. Postoperative delirium is associated with cognitive dysfunction one week after coronary artery bypass grafting surgery. Beijing Da Xue Xue Bao 2011, 43(2):242–249. [PubMed] [Google Scholar]
- 19.Rudolph JL, Babikian VL, Birjiniuk V, Crittenden MD, Treanor PR, Pochay VE, et al. Atherosclerosis is associated with delirium after coronary artery bypass graft surgery. J Am Geriatr Soc 2005, 53(3):462–466. 10.1111/j.1532-5415.2005.53165.x [DOI] [PubMed] [Google Scholar]
- 20.Santos FS, Velasco IT, Fraguas RJ. Risk factors for delirium in the elderly after coronary artery bypass graft surgery. Int Psychogeriater 2004, 16(2):175–193. [PubMed] [Google Scholar]
- 21.Mu DL, Li LH, Wang DX, Li N, Shan GJ, Li J, et al. High postoperative serum cortisol level is associated with increased risk of cognitive dysfunction early after coronary artery bypass graft surgery: a prospective cohort study. Plos One 2013, 8(10):e77637PMCID: PMC3797042 10.1371/journal.pone.0077637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Han L, McCusker J, Cole M, Abrahamowicz M, Primeau F, Elie M. Use of medications with anticholinergic effect predicts clinical severity of delirium symptoms in older medical inpatients. Arch Intern Med 2001, 161(8):1099–1105. [DOI] [PubMed] [Google Scholar]
- 23.Hshieh TT, Fong TG, Marcantonio ER, Inouye SK. Cholinergic deficiency hypothesis in delirium: a synthesis of current evidence. J Gerontol A Biol Sci Med Sci 2008, 63(7):764–772. PMCID: PMC2917793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Riker RR, Shehabi Y, Bokesch PM, Ceraso D, Wisemandle W, Koura F, et al. Dexmedetomidine vs midazolam for sedation of critically ill patients: a randomized trial. JAMA 2009, 301(5):489–499. 10.1001/jama.2009.56 [DOI] [PubMed] [Google Scholar]
- 25.Pandharipande P, Cotton BA, Shintani A, Thompson J, Pun BT, Morris JJ, et al. Prevalence and risk factors for development of delirium in surgical and trauma intensive care unit patients. J Trauma 2008, 65(1):34–41. PMCID: PMC3773485 10.1097/TA.0b013e31814b2c4d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pandharipande P, Shintani A, Peterson J, Pun BT, Wilkinson GR, Dittus RS, et al. Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. Anesthesiology 2006, 104(1):21–26. [DOI] [PubMed] [Google Scholar]
- 27.Fraser GL, Devlin JW, Worby CP, Alhazzani W, Barr J, Dasta JF, et al. Benzodiazepine versus nonbenzodiazepine-based sedation for mechanically ventilated, critically ill adults: a systematic review and meta-analysis of randomized trials. Crit Care Med 2013, 41(9 Suppl 1):S30–S38. [DOI] [PubMed] [Google Scholar]
- 28.Inouye SK, Bogardus SJ, Williams CS, Leo-Summers L, Agostini JV. The role of adherence on the effectiveness of nonpharmacologic interventions: evidence from the delirium prevention trial. Arch Intern Med 2003, 163(8):958–964. 10.1001/archinte.163.8.958 [DOI] [PubMed] [Google Scholar]
- 29.Mariscalco G, Cottini M, Zanobini M, Salis S, Dominici C, Banach M,et al. Preoperative statin therapy is not associated with a decrease in the incidence of delirium after cardiac operations. Ann Thorac Surg 2012, 93(5):1439–1447. 10.1016/j.athoracsur.2012.02.012 [DOI] [PubMed] [Google Scholar]
- 30.Bucerius J, Gummert JF, Borger MA, Walther T, Doll N, Falk V, et al. Predictors of delirium after cardiac surgery delirium: effect of beating-heart (off-pump) surgery. J Thorac Cardiovasc Surg 2004, 127(1):57–64. [DOI] [PubMed] [Google Scholar]
- 31.Djaiani G, Silverton N, Fedorko L, Carroll J, Styra R, Rao V, et al. Dexmedetomidine versus Propofol Sedation Reduces Delirium after Cardiac Surgery: A Randomized Controlled Trial. Anesthesiology. 2016, 124(2):362–8. 10.1097/ALN.0000000000000951 [DOI] [PubMed] [Google Scholar]
- 32.Shehabi Y, Grant P, Wolfenden H, Hammond N, Bass F, Campbell M, et al. Prevalence of delirium with dexmedetomidine compared with morphine based therapy after cardiac surgery: a randomized controlled trial (DEXmedetomidine COmpared to Morphine-DEXCOM Study). Anesthesiology 2009, 111(5):1075–1084. 10.1097/ALN.0b013e3181b6a783 [DOI] [PubMed] [Google Scholar]
- 33.Priye S, Jagannath S, Singh D, Shivaprakash S, Reddy DP. Dexmedetomidine as an adjunct in postoperative analgesia following cardiac surgery: A randomized, double-blind study. Saudi J Anaesth 2015, 9(4):353–358. 10.4103/1658-354X.154715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lacasse H, Perreault MM, Williamson DR. Systematic review of antipsychotics for the treatment of hospital-associated delirium in medically or surgically ill patients. Ann Pharmacother 2006; 40(11): 1966–1973. 10.1345/aph.1H241 [DOI] [PubMed] [Google Scholar]
- 35.Leung JM, Sands LP, Rico M, Petersen KL, Rowbotham MC, Dahl JB, et al. Pilot clinical trial of gabapentin to decrease postoperative delirium in older patients. Neurology 2006; 67(7): 1251–1253. 10.1212/01.wnl.0000233831.87781.a9 [DOI] [PubMed] [Google Scholar]
- 36.Su X, Meng ZT, Wu XH, Cui F, Li HL, Wang DX, et al. Dexmedetomidine decreases the incidence of delirium in elderly patients after non-cardiac surgery: a randomized, double-blind, placebo-controlled trial. Lancet 2016, 388(10054):1893–1902. 10.1016/S0140-6736(16)30580-3 [DOI] [PubMed] [Google Scholar]
- 37.Lin TF, Yeh YC, Lin FS, Wang YP, Lin CJ, Sun WZ, et al. Effect of combining dexmedetomidine and morphine for intravenous patient-controlled analgesia. Br J Anaesth 2009, 102(1):117–122. 10.1093/bja/aen320 [DOI] [PubMed] [Google Scholar]
- 38.Chrysostomou C, Schmitt CG. Dexmedetomidine: sedation, analgesia and beyond. Expert Opin Drug Metab Toxicol 2008, 4(5):619–627. 10.1517/17425255.4.5.619 [DOI] [PubMed] [Google Scholar]
- 39.Huupponen E, Maksimow A, Lapinlampi P, Sarkela M, Saastamoinen A, Snapir A, et al. Electroencephalogram spindle activity during dexmedetomidine sedation and physiological sleep. Acta Anaesthesiol Scand 2008, 52(2):289–294. 10.1111/j.1399-6576.2007.01537.x [DOI] [PubMed] [Google Scholar]
- 40.Nelson LE, Lu J, Guo T, Saper CB, Franks NP, Maze M. The alpha2-adrenoceptor agonist dexmedetomidine converges on an endogenous sleep-promoting pathway to exert its sedative effects. Anesthesiology 2003, 98(2):428–436. [DOI] [PubMed] [Google Scholar]
- 41.Alexopoulou C, Kondili E, Diamantaki E, Psarologakis C, Kokkini S, Bolaki M,. Effects of dexmedetomidine on sleep quality in critically ill patients: a pilot study. Anesthesiology 2014, 121(4):801–807. 10.1097/ALN.0000000000000361 [DOI] [PubMed] [Google Scholar]
- 42.Gao S, Wang Y, Zhao J, Su A. Effects of dexmedetomidine pretreatment on heme oxygenase-1 expression and oxidative stress during one-lung ventilation. Int J Clin Exp Pathol 2015, 8(3):3144–3149. PMCID: PMC4440140 [PMC free article] [PubMed] [Google Scholar]
- 43.Chi X, Wei X, Gao W, Guan J, Yu X, Wang Y, et al. Dexmedetomidine ameliorates acute lung injury following orthotopic autologous liver transplantation in rats probably by inhibiting Toll-like receptor 4-nuclear factor kappa B signaling. J Transl Med 2015,13:190 PMCID: PMC4467671. 10.1186/s12967-015-0554-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(XLS)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.