Abstract
High tibial osteotomy (HTO) has been widely used for clinical treatment of osteoarthritis of the medial compartment of the knee, and both opening-wedge and closing-wedge HTO are the most commonly used methods. However, it remains unclear which technique has better clinical and radiological outcomes in practice. To systematically evaluate this issue, we conducted a comprehensive meta-analysis by pooling all available data for the opening-wedge HTO and closing-wedge HTO techniques from the electronic databases including PubMed, Embase, Wed of Science and Cochrane Library. A total of 22 studies encompassing 2582 cases were finally enrolled in the meta-analysis. There was no significant difference regarding surgery time, duration of hospitalization, knee pain VAS, Lysholm score and HSS knee score (clinical outcomes) between the opening-wedge and closing-wedge HTO groups (P > 0.05). However, the opening-wedge HTO group showed wider range of motion than the closing-wedge HTO group (P = 0.003). Moreover, as for Hip-Knee-Ankle angle and mean angle of correction, no significant difference was observed between the opening-wedge and closing-wedge HTO groups (P > 0.05), while the opening-wedge HTO group showed greater posterior tibial slope angle (P < 0.001) and lesser patellar height than the closing-wedge HTO group (P < 0.001). On light of the above analysis, we believe that individualized surgical approach should be introduced based on the clinical characteristics of each patient.
Introduction
Knee osteoarthritis (OA) is a common and multi-factorial arthritic disorder, which may lead to joint dysfunction, i.e. reduction of joint motion and physical disability, as a result of degeneration, destruction, and loss of articular cartilage of knee joint [1]. Most patients with knee OA would develop varus deformity, and varus malalignment further overloads the medial tibiofemoral compartment, causing degenerative changes in the articular cartilage at last. Both conservative methods and surgical treatment were used for treatment of pain and dysfunction in knee OA. Surgical treatment included various techniques, i.e. high tibial osteotomy (HTO), arthroscopic surgery and total knee arthroplasty. Among them, HTO is the most frequently used method in young and more active patients [2].
In previous studies, various techniques of HTO were documented and evaluated. Among them, closing-wedge HTO and opening-wedge HTO, which were stabilized by a locking plate [3, 4], were two of the most frequently used techniques. For the closing-wedge HTO, a wedge-shaped cut is made in the lateral; while for the opening-wedge HTO, the medial tibia is cut. Many previous studies have compared the advantages and disadvantages between the closing-wedge and the opening-wedge HTO [5–7]. For example, the closing-wedge HTO was more advantageous in patients with a medial compartment OA with varus deformity for decrease of the posterior tibial slope [8]. However, several disadvantages have been also reported for the closing-wedge HTO, such as the need for fibular osteotomy, bone stock loss and nervous system complications [4, 5]. Different from the closing-wedge HTO, the opening-wedge HTO which has been performed more recently and doesn’t need a fibula osteotomy, caused fewer co-morbidities related to the fibular ostetomy [4]. Compared to the closing-wedge HTO, the opening-wedge HTO has several advantages, i.e. easier adjustment of alignment correction, more rapid rehabilitation, as reported previously [9, 10].
In detail, the advantages, disadvantages and sometimes complications were compared between the opening-wedge and closing-wedge HTO [7, 8, 11]; however, the results remained inconsistent. In the present study, we performed a comprehensive meta-analysis of the clinical and radiological outcomes between the opening-wedge and closing-wedge HTO, to explore whether the opening-wedge HTO was superior to the closing-wedge HTO. Our study would provide reasons for clinical guidance of surgical choice.
Materials and methods
Eligibility criteria
Eligible studies must meet the following criteria: 1) articles published in English and peer-reviewed journals; 2) randomized controlled trials (RCTs) and non-RCTs design comparing clinical and/or radiographic outcomes between closing-wedge HTO and opening-wedge HTO; 3) patient samples were independent from each other (if samples from different studies overlapped, only the studies with the largest sample size were included).
Animal study, review, commentary and meeting abstracts without detailed and novel data were excluded from the meta-analysis.
Search strategy
We searched eligible studies for this meta-analysis from PubMed (http://www.ncbi.nlm.nih.gov), SCOPUS (http://www.scopus.com), EMBASE (http://www.elsevier.com/online-tools/embase), ISIWeb of Knowledge (http://apps.webofknowledge.com/) and Cochrane Library (http://www.cochranelibrary.com/). Search terms used in the title, abstract and MeSH term included (“Osteotomy” OR ‘‘Tibial”) and (“Closed” OR “Closing”) and (“Open”). After the initial electronic search, eligible studies were screen carefully for other eligible studies. Studies published in English before the 1st of April 2016 were considered.
Data extraction
For each eligible study, two independent investigators extracted the following data: 1) first author and publication year; 2) type of study design; 3) sample size, age and gender distribution; 4) follow-up periods; 5) clinical and radiographic outcomes; 6) other data if essential. Any disagreement of data was subject to the third author. Moreover, if essential data was not available directly from the manuscript, the corresponding author was contacted, or we calculated them, i.e. standard deviations and confidence intervals, from already provided data.
In detail, clinical outcomes included, but not limited to, time course of surgical operation, duration of hospital stays, various sorts of knee scoring (Hospital for Special Surgery (HSS) knee score, knee pain visual analog score, Lysholm knee score and Wallgren-Tegner score), knee range of motion (ROM), as well as patient satisfaction (score). Radiographic outcomes included, but not limited to, mean angle of correction, hip–knee–ankle (HTA) angle, posterior tibial slope angle, and patellar height (PH).
Assessment of methodological quality
The revised Jadad scale by the Cochrane Non-randomized Studies Methods Working Group were used to assess methodological quality [12]. A total of 7 points were assigned to this scoring method, including the randomization process (2 points), allocation concealment (2 points), appropriateness of blinding (2 points), and a description of dropouts and withdrawals (1 point). A score of 4–7 points indicated high quality, and 0–3 indicating poor quality. Two investigators independently extracted the data using a standardized form. The final score was based on the consensus assessment from two investigators. If disagreements persisted, a third author was consulted.
Statistical analysis
The Stata 12.0 statistical software package (http://www.stata.com/) and the Review Manager 5.3 software (The Cochrane Collaboration) were applied to conduct publication bias analysis, meta-analysis and sensitivity analysis. Potential publication bias was determined by both the Egger regression test for a funnel plot [13] and the Begg–Mazumdar test, which is based on Kendall’s-τ [14]. For dichotomous variables, the odds ratio (OR) with 95% confidence interval (95% CI) was derived for each outcome; for continuous variables, we calculated the standardized mean difference and 95% CI. We performed the meta-analysis using a fixed-effect model if no significant heterogeneity was present; otherwise, a random-effect model was applied. To assess heterogeneity between studies, we performed a chi-square test and estimated the I2 statistic. For all analyses, P < 0.05 was considered statistically significant. The study was approved by the ethics committee of Lishui People’s Hospital of Wenzhou Medical University. All the protocols and experimental procedures were in accordance with the Declaration of Helsinki and other international rules (S1 Table).
Results
Literature search and eligible studies
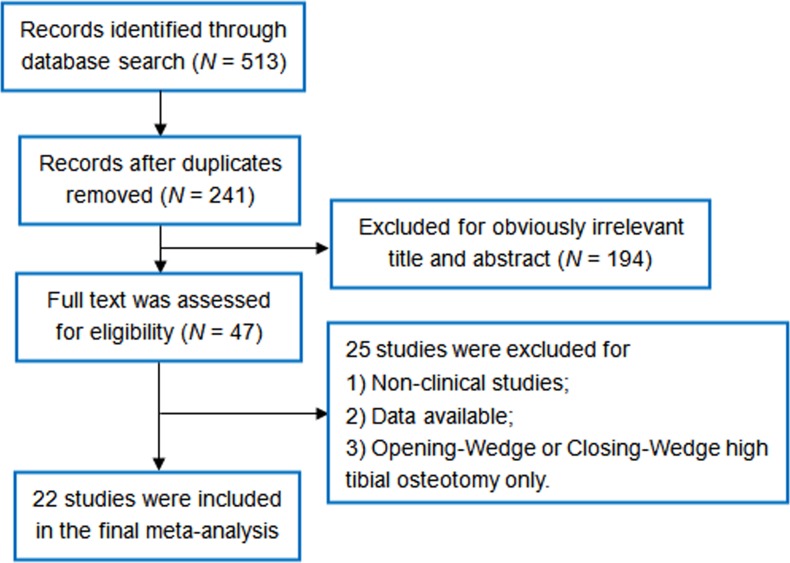
According to our literature search approaches, a total of 513 references were indexed. After excluding 487 studies for reasons specified in Fig 1 and S1 Fig, a total of 22 studies (7 RCTs and 15 non-RCTs) encompassing 2582 cases, including 1274 knees which were underwent opening-wedge HTO and 1308 ones with closing-wedge HTO operation, were finally enrolled in the final meta-analysis [5–8, 10, 15–31]. Table 1listed the detailed information of recruited studies for this meta-analysis, i.e. sample size, age and gender proportion, fixation approaches, etc. It is worth note that four studies [29, 32–34] were removed from the current meta-analysis due to sample duplication within other studies [17, 28, 31].
Fig 1. Flow diagram of the identification and selection of the studies included in this meta-analysis.
Table 1. Characteristics of the included studies.
| Author | Year | Study design | Opening-wedge HTO | Closing-wedge HTO | Quality score | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Age | Gender (M/F) | Fixation method | N | Age | Gender (M/F) | Fixation method | ||||
| van Egmond et al. | 2016 | RCT | 25 | 47.1 (8.5) | 15/10 | Locked plate | 25 | 50.3 (7.4) | 16/9 | Locked plate | 4 |
| Duivenvoorden et al. | 2015 | RCS | 112 | 48.7 (10.1) | 73/39 | Puddu and Tomofix plate | 354 | 49.4 (9.0) | 203/151 | Three different staples | 6 |
| Nerhus et al. | 2015 | RCT | 35 | NA | NA | Staples | 35 | NA | NA | Puddu titanium plate | 4 |
| Deie et al. | 2014 | RCS | 9 | 57.5 (6.0) | 3/6 | Plate and screws | 12 | 57.8 (6.0) | 3/9 | Plate and screws | 6 |
| Portner et al. | 2014 | RCS | 26 | 43.9 (8.48) | 20/6 | Plate and screws | 18 | 46.5 (5.17) | 15/3 | Staples | 6 |
| Duivenvoorden et al. | 2014 | RCT | 36 | 49.9 (7.9) | 24/12 | Puddu plate | 45 | 49.5 (9.2) | 27/18 | Staples | 6 |
| Amzallag et al. | 2013 | PCS | 224 | 53.6 (8.6) | NA | NA | 97 | 49.7 (10.3) | NA | NA | 8 |
| Tabrizi et al. | 2013 | PCS | 21 | 36.5 (8.1) | 13/3 | Plates | 21 | 35.1 (9.7) | 12/4 | L or T plates | 7 |
| Bae et al. | 2013 | RCS | 30 | 56.3 (7.5) | 2/25 | Puddu plate | 78 | 58.8 (7.5) | 4/70 | Miniplate staple | 6 |
| Song et al. | 2012 | RCS | 50 | 57.9 | 10/40 | Wedge plates | 50 | 60.1 | 12/38 | Stepped staples | 7 |
| Ducat et al. | 2012 | PCS | 210 | 52 (9) | NA | NA | 92 | 49.7 (10.3) | NA | NA | 6 |
| Magnussen et al. | 2011 | RCS | 32 | 54 | 22/10 | Tomofix plate | 32 | 59 | 21/9 | Blade and screws | 8 |
| Song et al. | 2010 | RCS | 90 | 51 | 21/69 | Aescula plates | 104 | 57 | 16/88 | Staples | 6 |
| Gaasbeek et al. | 2010 | RCT | 25 | 47.0 (8.5) | 14/11 | Locked plate | 25 | 49.8 (8.4) | 16/9 | Locked plate | 4 |
| Hankemeier et al. | 2010 | RCS | 35 | 44 | NA | Fixed-angle plates | 26 | 53 | NA | Screw-plate | 5 |
| Luites et al. | 2009 | RCT | 23 | 53 | NA | TF plates and screws | 19 | 53 | NA | TF plates and screws | 5 |
| van den Bekerom et al. | 2008 | PCS | 20 | 52 | 10/10 | Puddu Plate | 20 | 52 | 9/11 | AO/ASIF L-plate | 7 |
| Schaefer et al. | 2008 | RCS | 90 | 46 | NA | T-Clamp | 66 | 47 | NA | Wedge Blount’s staples | 7 |
| El-Azab et al. | 2008 | RCS | 60 | NA | NA | NA | 60 | NA | NA | NA | 6 |
| Brouwer et al. | 2005 | RCT | 45 | 49.6 | 32/13 | Plates | 47 | 50.8 | 27/20 | L-plates | 4 |
| Hoell et al. | 2005 | RCS | 51 | 52.1 (8.4) | 32/19 | Puddu plates | 57 | 46.4 (8) | 40/17 | Coventry | |
| Magyar et al. | 1999 | RCT | 25 | 55 | NA | External fixation | 25 | 55 | NA | Staples | 5 |
HTO, high tibial osteotomy; RCT, ndomized controled trial; RCS, retrospective cohort study; PCS, prospective cohort study; NA, not available
Clinical outcomes
As for clinical outcomes, the following several aspects were compared between opening-wedge and closing-wedge HTO, i.e. surgery time, duration of hospital stays, HSS knee score (> 1 year follow-up), knee pain VAS, range of motion (flexion angle) and Lysholm knee score. Other parameters, including patient satisfaction (score), Wallgren-Tegner score, Insall-Salvati index and complete weight bearing (day), were not pooled in our meta-analyses due to limited studies (N < 2) or sample size. Notably, since no significant difference was observed for pre-operative characteristics between the opening-wedge and closing-wedge HTO groups, only the post-operative values of clinical outcomes were compared.
As shown in Table 2, there was no significant difference for surgery time (SMD = -0.18, 95% CI = -1.24–0.88, P = 0.741) [5, 19, 24, 30] and duration of hospitalization (SMD = -0.87, 95% CI = -2.09–0.36, P = 0.166) [5, 24, 31] as indicated by the random-effect model.
Table 2. Overview of meta-analysis results.
| Index | Studies | Sample size | Heterogeneity (I2/P-value) | Effect | Model | ||
|---|---|---|---|---|---|---|---|
| Z-score | P-value | OR or SMD (95% CI) | |||||
| Clinical outcomes | |||||||
| Surgical time | 4 | 209/457 | 95.9% (<0.001) | 0.33 | 0.741 | -0.18 (-1.24, 0.88) | Random |
| Duration of hospitalization | 3 | 162/404 | 94.8% (<0.001) | 1.38 | 0.166 | -0.87 (-2.09, 0.36) | Random |
| HSS knee score | 4 | 201/224 | 0.0% (0.607) | 1.81 | 0.07 | 0.18 (-0.01, 0.37) | Fixed |
| Knee pain VAS | 5 | 154/161 | 0.0% (0.436) | 0.00 | 0.999 | 0.00 (-0.22, 0.22) | Fixed |
| Lysholm score | 4 | 120/122 | 0.0% (0.773) | 1.43 | 0.152 | 0.19 (-0.07, 0.44) | Fixed |
| Range of motion (flexion angle) | 3 | 152/164 | 0.0% (0.777) | 2.94 | 0.003 | 0.33 (0.11, 0.56) | Fixed |
| Radiological outcomes | |||||||
| Hip-Knee-Ankle angle | 7 | 459/397 | 82.8% (<0.001) | 0.81 | 0.415 | -0.15 (-0.52, 0.22) | Random |
| Mean angle of correction | 8 | 310/327 | 79.1% (<0.001) | 0.00 | 0.998 | 0.00 (-0.36, 0.36) | Random |
| Posterior tibial slope angle | 11 | 663/581 | 95.0% (<0.001) | 4.27 | <0.001 | 1.31 (0.71, 1.91) | Random |
| PH: Caton index | 2 | 249/122 | 0.0% (0.408) | 7.88 | <0.001 | -0.92 (-1.15, -0.56) | Fixed |
| PH: Insall-Salvati index | 3 | 82/64 | 17.9% (0.296) | 2.18 | 0.029 | -0.36 (-0.67, -0.04) | Fixed |
| PH: Blackburne-Peel ratio | 2 | 95/97 | 35.0% (0.215) | 0.88 | 0.377 | -0.13 (-0.41, 0.16) | Fixed |
VAS, Visual Analogue Scale; PH, patellar height; OR, odds ratios; SMD, standardized mean differences
As the main characteristics of clinical outcome, HSS knee score [6, 17, 21, 31], knee pain VAS [7, 17, 24, 25, 29] and Lysholm score [19, 25, 30, 31] were assessed in four, five and four studies, respectively. Our meta-analysis indicated that there was no significant difference regarding knee pain VAS (SMD = 0.00, 95% CI = -0.22–0.22, P = 0.999) and Lysholm score (SMD = 0.19, 95% CI = -0.07–0.44, P = 0.152), between the opening-wedge and closing-wedge HTO groups using the fixed-effect model (P > 0.05); while slightly but not significantly higher HSS knee score was observed in the opening-wedge HTO group, when compared with the closing-wedge HTO group (SMD = 0.18, 95% CI = -0.01–0.37, P = 0.07) using the fixed-effect model (I2 = 0.7%, P = 0.388) (Table 2).
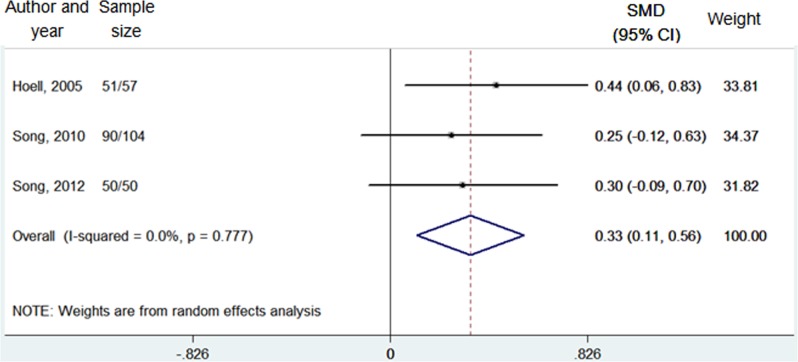
Interestingly, significant difference was observed regarding the range of motion (flexion angle) (P = 0.003) between the opening-wedge and closing-wedge HTO groups by the fixed-effect model (I2 = 0.0%, P = 777) (Table 2, Fig 2), and the opening-wedge HTO group showed wider range of motion than the closing-wedge HTO group (SMD = 0.33, 95% CI = 0.11–0.56) [6, 21, 30].
Fig 2. Forest plot of range of motion (flexion angle) between the opening-wedge and closing-wedge HTO group.
Note: sample size represented N opening-wedge HTO/N closing-wedge HTO; SMD, standardized mean difference.
Radiological outcomes
Hip-Knee-Ankle angle
A total of 7 studies encompassing 459 cases with opening-wedge HTO and 397 knees with closing -wedge HTO were included for HKA angle analysis [6, 8, 10, 15, 17, 18, 20]. As shown in Table 2, there was no significant difference regarding the HKA angle after surgical operation between the opening- and closing-wedge HTO groups (SMD = -0.15, 95% CI = -0.52–0.22, P = 0.415) using the random-effect model (I2 = 82.8%, P < 0.001) (S2 Fig).
Mean angle of correction
There were 8 studies including 637 knees with analysis of mean HKA angle of correction [7, 8, 10, 20, 24, 27, 29, 31]. After pooling all the data, we observed no significant difference between knees undergoing opening-wedge HTO and those undergoing opening-wedge HTO (SMD = 0.00, 95% CI = -0.36–0.36, P = 0.998) by the random-effect model (I2 = 79.1%, P < 0.001) (Table 2, S3 Fig).
Posterior tibial slope angle
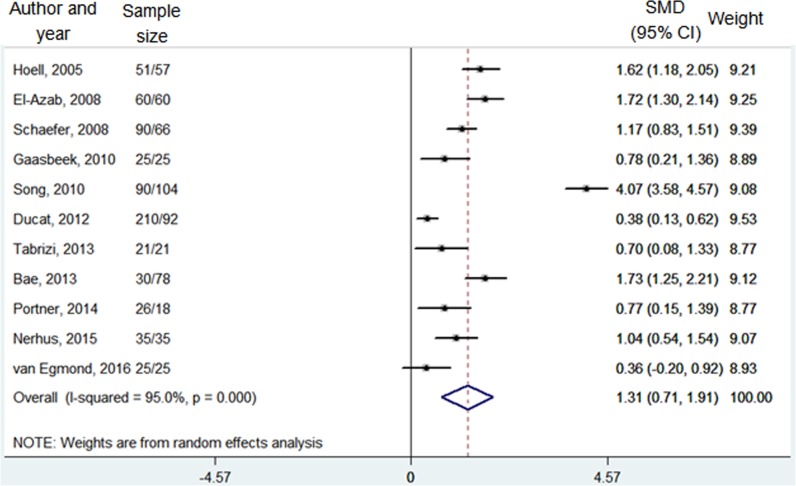
Data on 663 knees with opening-wedge HTO and 581 knees with closing-wedge HTO from a total of 11 studies were pooled together regarding the posterior tibial slope angle [6–8, 16, 19, 20, 22, 24, 27, 28, 30]. Meta-analysis with random-effect model (I2 = 95.0%, P < 0.001) showed that there was a significantly greater posterior tibial slope angle in the opening-wedge HTO cases compared to the closing-wedge HTO ones (SMD = 1.31, 95% CI = 0.71–1.91, P < 0.001) (Table 2 and Fig 3).
Fig 3. Forest plot of posterior tibial slope angle between the opening-wedge and closing-wedge HTO grou.
Note: sample size represented N opening-wedge HTO/N closing-wedge HTO; SMD, standardized mean difference.
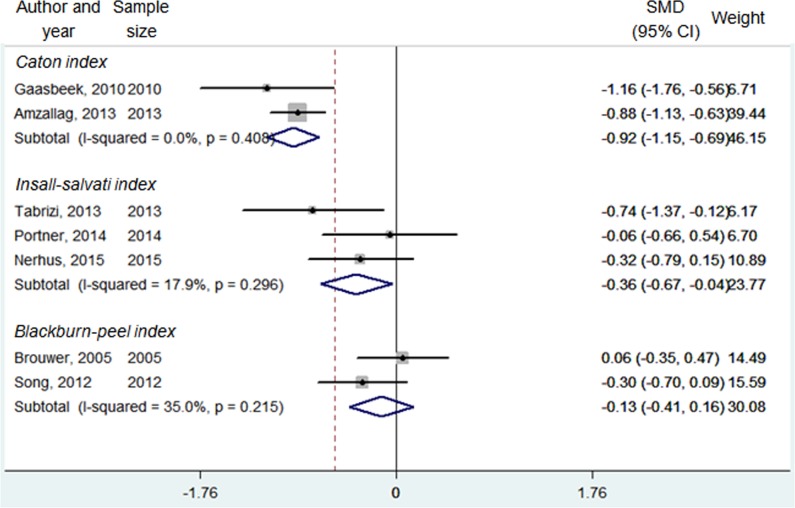
Patellar height
Besides, three indicators of patellar height were analyzed, including Caton index [18, 24], Insall-Salvati index [8, 16, 19] and Blackburne-Peel ratio [21, 29]. As shown in Table 2 and Fig 4, there was a significantly greater patellar height measured by the Caton index (SMD = -0.92, 95% CI = -1.15 –(-0.56), P < 0.001) and Insall-Salvati index (SMD = -0.36, 95% CI = -0.67 –(-0.04), P < 0.001) in the closing-wedge HTO group when compared with the opening-wedge HTO group. However, when measured by Blackburne-Peel ratio, no significant difference was observed between these two groups.
Fig 4. Forest plot of patellar height (Caton index, Insall-Salvati index and Blackburne-Peel index) between the opening-wedge and closing-wedge HTO group.
Note: sample size represented N opening-wedge HTO/N closing-wedge HTO; SMD, standardized mean difference.
Discussion
In the present study, we performed a comprehensive meta-analysis of clinical and radiographic outcomes between the opening-wedge and closing-wedge HTO groups. For most of the included indexes, no significant difference was observed between these two groups. However, for some outcomes, i.e., postoperative range of motion (flexion angle), posterior tibial slope angle and patellar height, there was indeed significant difference between the opening-wedge and closing-wedge HTO groups.
As for clinical outcomes, only the range of motion (flexion angle) showed significant difference between the opening-wedge HTO and closing-wedge HTO groups (P = 0.003), and the former exhibited wider range of motion than the latter (SMD = 0.33, 95% CI = 0.11–0.56). As we know, a portion of patients undergoing the opening-wedge HTO were required to receive range-of-motion exercise during the early postoperative period, and in Song et al. study [6, 21], all the opening-wedge HTO patients received the range-of-motion exercise, which was not the case for the closing-wedge group. In our meta-analysis, two studies from Song et al. constitute the largest portion of the overall sample size, which might lead to biased result regarding the range of motion (flexion angle).
As for the patellar height, we pooled data from three distinct measuring methods, including Caton index, Insall-Salvati index and Blackburne-Peel index. Our analyses showed that the patellar height, as measured by Caton index and Insall-Salvati index, was significantly decreased after the opening-wedge HTO than that after the closing-wedge HTO. Careful examination of the raw data from previous studies, we observed that the patellar height was decreased after the opening-wedge HTO, while increased after the closing-wedge HTO. The possible explanation of this controversial result was that the opening-wedge HTO may lower the tibial tuberosity leading to decreased patella height, while the closing-wedge HTO could elevate the tibial tuberosity as a result of a proximalisation of the proximal tibia [35]. Different from our meta-analysis, Takeuchi et al. found that patellar height was maintained after opening-wedge HTO and speculated that this result was due to range-of-motion exercises during the early postoperative period [36]. However, in Song et al. study, in which range-of-motion exercise was recommended after opening-wedge HTO, most patients showed a significant decrease in patellar height after surgery as well, suggesting that range-of-motion exercise was not the main cause of decrease in patellar height [21]. Intriguingly, slight but not significant reduction of patella height as measured by Blackburne-Peel index was observed in the opening-wedge HTO group when compared with that of the closing-wedge group (P = 0.377). This inconsistency may be resulted from the limited sample size, which could cause publication bias and insufficient statistical power.
Moreover, the result of the meta-analysis showed that posterior tibial slope angle after opening-wedge HTO was significantly increased than that after closing-wedge HTO (SMD = 1.31, 95% CI = 0.71–1.91). Similar with the patellar height, the posterior slope was increased following the opening-wedge HTO, while decreased after the closing-wedge HTO. It is one frequently reported problem associated with the opening-wedge HTO that posterior tibial slope might be increased. Several theories have been put forward to explain the etiology of changes of posterior tibial slope following HTO. The most widely accepted theory is that the unique anatomic geometry of the proximal tibia is responsible for the change of posterior tibial slope angle following HTO [37]. This geometric shape requires a smaller opening gap at the anterior part of the osteotomy site than the posteromedial part, as the former is closer to the hinge point of osteotomy if the posterior tibial slope angle remains unchanged [38].
Several limitations should be presented to interpret the present results. Firstly, different surgical approaches were included and mixed in the current meta-analysis, which may confound the meta-analysis result. Secondly, though most of the included studies were of high-quality, a small portion of the included studies were of low-quality as indicated by the revised Jaded scale (Table 1). Insufficient method description, low reliability of radiographic results, and study design in these studies might lead to between-group heterogeneity. Thirdly, although all the eligible studies were included in this meta-analysis, the sample size was relatively small, which may induce type-II statistic error. Updated meta-analysis of this issue is essential for a more solid conclusion in future.
Conclusions
Except for the range of motion (flexion angle), posterior tibial slope angle and patellar height, both the opening-wedge and closing-wedge HTO had satisfactory and comparable clinical and radiographic outcomes. On light of the above analysis, we believe that individualized surgical approach should be introduced based on the clinical characteristics of each patient.
Supporting information
(DOC)
(DOC)
Note: sample size represented N opening-wedge HTO/N closing-wedge HTO; SMD, standardized mean difference.
(DOC)
Note: sample size represented N opening-wedge HTO/N closing-wedge HTO; SMD, standardized mean difference.
(DOC)
Acknowledgments
We thank Xiaoyong Sheng for helpful discussion of the architecture of this manuscript.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported by the Science and Technology Bureau of Lishui (No. 2014JYZB24). The funder has no role in study design, data collection, manuscript preparation and submission.
References
- 1.Fibel KH, Hillstrom HJ, Halpern BC. State-of-the-Art management of knee osteoarthritis. World J Clin Cases. 2015;3(2):89–101. 10.12998/wjcc.v3.i2.89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agneskirchner JD, Hurschler C, Wrann CD, Lobenhoffer P. The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy. 2007;23(8):852–61. 10.1016/j.arthro.2007.05.018 [DOI] [PubMed] [Google Scholar]
- 3.Esenkaya I, Unay K, Akan K. Proximal tibial osteotomies for the medial compartment arthrosis of the knee: a historical journey. Strategies Trauma Limb Reconstr. 2012;7(1):13–21. 10.1007/s11751-012-0131-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee DC, Byun SJ. High tibial osteotomy. Knee Surg Relat Res. 2012;24(2):61–9. 10.5792/ksrr.2012.24.2.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duivenvoorden T, van Diggele P, Reijman M, Bos PK, van Egmond J, Bierma-Zeinstra SM, et al. Adverse events and survival after closing- and opening-wedge high tibial osteotomy: a comparative study of 412 patients. Knee Surg Sports Traumatol Arthrosc. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Song EK, Seon JK, Park SJ, Jeong MS. The complications of high tibial osteotomy: closing- versus opening-wedge methods. J Bone Joint Surg Br. 2010;92(9):1245–52. 10.1302/0301-620X.92B9.23660 [DOI] [PubMed] [Google Scholar]
- 7.van Egmond N, van Grinsven S, van Loon CJ, Gaasbeek RD, van Kampen A. Better clinical results after closed- compared to open-wedge high tibial osteotomy in patients with medial knee osteoarthritis and varus leg alignment. Knee Surg Sports Traumatol Arthrosc. 2016;24(1):34–41. 10.1007/s00167-014-3303-z [DOI] [PubMed] [Google Scholar]
- 8.Nerhus TK, Ekeland A, Solberg G, Sivertsen EA, Madsen JE, Heir S. Radiological outcomes in a randomized trial comparing opening wedge and closing wedge techniques of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2015. [DOI] [PubMed] [Google Scholar]
- 9.Nakamura E, Mizuta H, Kudo S, Takagi K, Sakamoto K. Open-wedge osteotomy of the proximal tibia with hemicallotasis. J Bone Joint Surg Br. 2001;83(8):1111–5. [DOI] [PubMed] [Google Scholar]
- 10.Hankemeier S, Mommsen P, Krettek C, Jagodzinski M, Brand J, Meyer C, et al. Accuracy of high tibial osteotomy: comparison between open- and closed-wedge technique. Knee Surg Sports Traumatol Arthrosc. 2010;18(10):1328–33. 10.1007/s00167-009-1020-9 [DOI] [PubMed] [Google Scholar]
- 11.Brouwer RW, Huizinga MR, Duivenvoorden T, van Raaij TM, Verhagen AP, Bierma-Zeinstra SM, et al. Osteotomy for treating knee osteoarthritis. Cochrane Database Syst Rev. 2014;12:CD004019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clark HD, Wells GA, Huet C, McAlister FA, Salmi LR, Fergusson D, et al. Assessing the quality of randomized trials: reliability of the Jadad scale. Control Clin Trials. 1999;20(5):448–52. [DOI] [PubMed] [Google Scholar]
- 13.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101. [PubMed] [Google Scholar]
- 15.Deie M, Hoso T, Shimada N, Iwaki D, Nakamae A, Adachi N, et al. Differences between opening versus closing high tibial osteotomy on clinical outcomes and gait analysis. Knee. 2014;21(6):1046–51. 10.1016/j.knee.2014.04.007 [DOI] [PubMed] [Google Scholar]
- 16.Portner O. High tibial valgus osteotomy: closing, opening or combined? Patellar height as a determining factor. Clin Orthop Relat Res. 2014;472(11):3432–40. 10.1007/s11999-014-3821-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duivenvoorden T, Brouwer RW, Baan A, Bos PK, Reijman M, Bierma-Zeinstra SM, et al. Comparison of closing-wedge and opening-wedge high tibial osteotomy for medial compartment osteoarthritis of the knee: a randomized controlled trial with a six-year follow-up. J Bone Joint Surg Am. 2014;96(17):1425–32. 10.2106/JBJS.M.00786 [DOI] [PubMed] [Google Scholar]
- 18.Amzallag J, Pujol N, Maqdes A, Beaufils P, Judet T, Catonne Y. Patellar height modification after high tibial osteotomy by either medial opening-wedge or lateral closing-wedge osteotomies. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):255–9. 10.1007/s00167-012-2304-z [DOI] [PubMed] [Google Scholar]
- 19.Tabrizi A, Soleimanpour J, Sadighi A, Zare AJ. A short term follow up comparison of genu varum corrective surgery using open and closed wedge high tibial osteotomy. Malays Orthop J. 2013;7(1):7–12. 10.5704/MOJ.1303.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bae DK, Song SJ, Kim HJ, Seo JW. Change in limb length after high tibial osteotomy using computer-assisted surgery: a comparative study of closed- and open-wedge osteotomies. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):120–6. 10.1007/s00167-012-1898-5 [DOI] [PubMed] [Google Scholar]
- 21.Song IH, Song EK, Seo HY, Lee KB, Yim JH, Seon JK. Patellofemoral alignment and anterior knee pain after closing- and opening-wedge valgus high tibial osteotomy. Arthroscopy. 2012;28(8):1087–93. 10.1016/j.arthro.2012.02.002 [DOI] [PubMed] [Google Scholar]
- 22.Ducat A, Sariali E, Lebel B, Mertl P, Hernigou P, Flecher X, et al. Posterior tibial slope changes after opening- and closing-wedge high tibial osteotomy: a comparative prospective multicenter study. Orthop Traumatol Surg Res. 2012;98(1):68–74. 10.1016/j.otsr.2011.08.013 [DOI] [PubMed] [Google Scholar]
- 23.Magnussen RA, Lustig S, Demey G, Neyret P, Servien E. The effect of medial opening and lateral closing high tibial osteotomy on leg length. Am J Sports Med. 2011;39(9):1900–5. 10.1177/0363546511410025 [DOI] [PubMed] [Google Scholar]
- 24.Gaasbeek RD, Nicolaas L, Rijnberg WJ, van Loon CJ, van Kampen A. Correction accuracy and collateral laxity in open versus closed wedge high tibial osteotomy. A one-year randomised controlled study. Int Orthop. 2010;34(2):201–7. 10.1007/s00264-009-0861-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Luites JW, Brinkman JM, Wymenga AB, van Heerwaarden RJ. Fixation stability of opening- versus closing-wedge high tibial osteotomy: a randomised clinical trial using radiostereometry. J Bone Joint Surg Br. 2009;91(11):1459–65. 10.1302/0301-620X.91B11.22614 [DOI] [PubMed] [Google Scholar]
- 26.van den Bekerom MP, Patt TW, Kleinhout MY, van der Vis HM, Albers GH. Early complications after high tibial osteotomy: a comparison of two techniques. J Knee Surg. 2008;21(1):68–74. [DOI] [PubMed] [Google Scholar]
- 27.Schaefer TK, Majewski M, Hirschmann MT, Friederich NF. Comparison of sagittal and frontal plane alignment after open- and closed-wedge osteotomy: a matched-pair analysis. J Int Med Res. 2008;36(5):1085–93. [DOI] [PubMed] [Google Scholar]
- 28.El-Azab H, Halawa A, Anetzberger H, Imhoff AB, Hinterwimmer S. The effect of closed- and open-wedge high tibial osteotomy on tibial slope: a retrospective radiological review of 120 cases. J Bone Joint Surg Br. 2008;90(9):1193–7. 10.1302/0301-620X.90B9.20688 [DOI] [PubMed] [Google Scholar]
- 29.Brouwer RW, Bierma-Zeinstra SM, van Raaij TM, Verhaar JA. Osteotomy for medial compartment arthritis of the knee using a closing wedge or an opening wedge controlled by a Puddu plate. A one-year randomised, controlled study. J Bone Joint Surg Br. 2006;88(11):1454–9. 10.1302/0301-620X.88B11.17743 [DOI] [PubMed] [Google Scholar]
- 30.Hoell S, Suttmoeller J, Stoll V, Fuchs S, Gosheger G. The high tibial osteotomy, open versus closed wedge, a comparison of methods in 108 patients. Arch Orthop Trauma Surg. 2005;125(9):638–43. 10.1007/s00402-005-0004-6 [DOI] [PubMed] [Google Scholar]
- 31.Magyar G, Ahl TL, Vibe P, Toksvig-Larsen S, Lindstrand A. Open-wedge osteotomy by hemicallotasis or the closed-wedge technique for osteoarthritis of the knee. A randomised study of 50 operations. J Bone Joint Surg Br. 1999;81(3):444–8. [DOI] [PubMed] [Google Scholar]
- 32.van Raaij TM, Brouwer RW, de Vlieger R, Reijman M, Verhaar JA. Opposite cortical fracture in high tibial osteotomy: lateral closing compared to the medial opening-wedge technique. Acta Orthop. 2008;79(4):508–14. 10.1080/17453670710015508 [DOI] [PubMed] [Google Scholar]
- 33.El-Azab H, Glabgly P, Paul J, Imhoff AB, Hinterwimmer S. Patellar height and posterior tibial slope after open- and closed-wedge high tibial osteotomy: a radiological study on 100 patients. Am J Sports Med. 2010;38(2):323–9. 10.1177/0363546509348050 [DOI] [PubMed] [Google Scholar]
- 34.Magyar G, Toksvig-Larsen S, Lindstrand A. Changes in osseous correction after proximal tibial osteotomy: radiostereometry of closed- and open-wedge osteotomy in 33 patients. Acta Orthop Scand. 1999;70(5):473–7. [DOI] [PubMed] [Google Scholar]
- 35.Brouwer RW, Bierma-Zeinstra SM, van Koeveringe AJ, Verhaar JA. Patellar height and the inclination of the tibial plateau after high tibial osteotomy. The open versus the closed-wedge technique. J Bone Joint Surg Br. 2005;87(9):1227–32. 10.1302/0301-620X.87B9.15972 [DOI] [PubMed] [Google Scholar]
- 36.Takeuchi R, Ishikawa H, Aratake M, Bito H, Saito I, Kumagai K, et al. Medial opening wedge high tibial osteotomy with early full weight bearing. Arthroscopy. 2009;25(1):46–53. 10.1016/j.arthro.2008.08.015 [DOI] [PubMed] [Google Scholar]
- 37.Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32(2):376–82. [DOI] [PubMed] [Google Scholar]
- 38.Asada S, Akagi M, Mori S, Matsushita T, Hashimoto K, Hamanishi C. Increase in posterior tibial slope would result in correction loss in frontal plane after medial open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2012;20(3):571–8. 10.1007/s00167-011-1610-1 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOC)
Note: sample size represented N opening-wedge HTO/N closing-wedge HTO; SMD, standardized mean difference.
(DOC)
Note: sample size represented N opening-wedge HTO/N closing-wedge HTO; SMD, standardized mean difference.
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.