Abstract
Because health care demand among IBS patients imposes a heavy economic burden, identifying high utilizers has potential for improving quality and efficiency of care. Previous research has not identified reliable predictors of utilization of IBS patients. We sought to identify factors predictive of health care utilization among severe IBS patients. 291 IBS patients completed testing whose content mapped onto the Andersen model of health care utilization. 2-stage hurdle models were used to determine predictors of health care use (probability and frequency). Separate analyses were conducted for mental health and medical services. Whether patients used any medical care was predicted by diet and insurance status. Tobacco use, education, and health insurance predicted the probability of using mental health care. The frequency of medical care was associated with alcohol use and physical health status, while frequency of mental health services was associated with marital status, tobacco use, education, distress, stress, and control beliefs over IBS symptoms. For IBS patients, the demand for health care involves a complex decision-making process influenced by many factors. Particularly strong determinants include predisposing characteristics (e.g., dietary pattern, tobacco use) and enabling factors (e.g., insurance coverage) that impede or facilitate demand. Which factors impact use depends on whether the focus is on the decision to use care or how much care is used. Decisions to use medical and mental health care are not simply influenced by symptom-specific factors but by a variety of lifestyle (e.g., dietary pattern, education, smoking) and economic (e.g., insurance coverage) factors.
Keywords: Diet, Utilization, Comorbidity, Disease management, Psychosocial factors, Cost
Irritable bowel syndrome (IBS) is a functional gastrointestinal (GI) disorder characterized by abdominal pain associated with diarrhea and/or constipation. As one of the most common diagnoses seen by gastroenterologists and primary care physicians (Mayer, 2008), IBS exacts substantial economic costs (Spiegel, 2013) estimated at $15 billion annually (Sandler et al., 2002). A significant source of these costs is the demand for health care services which is higher among IBS patients than those with other GI diseases or healthy individuals (Chang, 2004). Given its economic burden, a better understanding of the factors influencing health care use is needed to help identify patients at increased risk for poorer outcomes. Early identification of such patients may facilitate earlier implementation of targeted behaviorally-oriented disease management strategies that improve the quality of care (Longstreth et al., 2003) for symptoms that do not adequately respond to medical treatments.
Previous efforts to explain health care use of IBS patients have presumed that the factors that modify the IBS symptom experience (e.g. abdominal pain intensity, quality of life impairment, bowel type) also influence their decision to use health care resources (Kanazawa et al., 2004; Koloski, Talley, & Boyce, 2001; Talley, Boyce, & Jones, 1997; Talley, Gabriel, Harmsen, Zinsmeister, & Evans, 1995; Williams et al., 2006). A conceptual approach that emphasizes symptom factors has yielded few consistent predictors of health care use (Koloski et al., 2001). The notion that IBS patients seek health care because of the severity of GI symptoms is not well established (Koloski, Talley, Boyce, 2001). Neither the severity (Ringstrom, Abrahamsson, Strid, & Simren, 2007), duration (Lydeard & Jones, 1989), nor nature of GI symptoms (e.g., predominant bowel habit) reliably predicts treatment seeking behavior (Talley, Zinsmeister, & Melton, 1995). Psychological factors provide no more conclusive link to heath care use. Ringstrom et al. (2007) found that psychological factors such as fear of GI symptoms, anxiety, depression, quality of life impairment, and coping style predicted health care use, whereas Talley et al. (1997) found no relationship between health care and psychological factors. This pattern of data prompted Talley et al. to assert “other unknown factors are much more important” (Talley et al., 1997, p. 397) in understanding patterns of health care use among IBS patients.
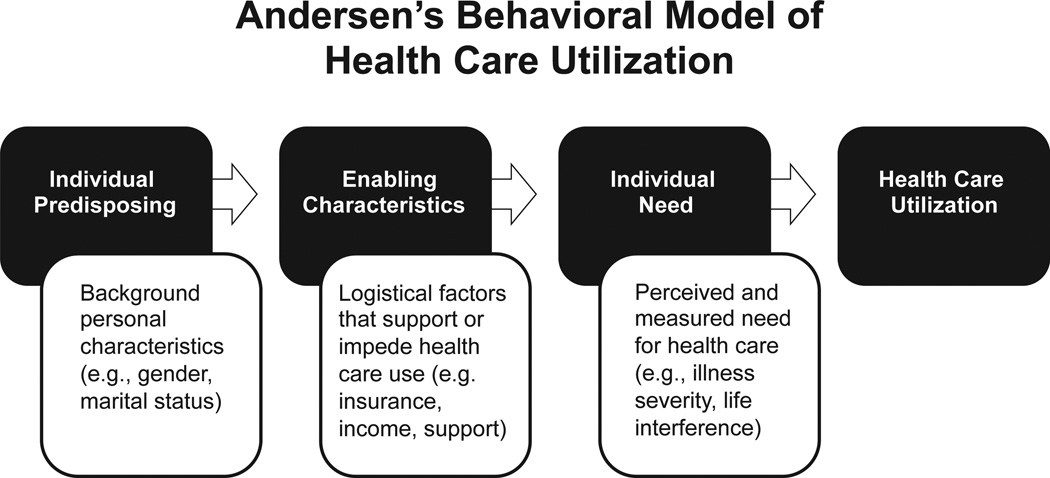
Potential clues come from the Andersen model (Andersen, 1995) of health care utilization which is a widely accepted conceptual framework for understanding why people access health care services. The model holds that the decision to use health care is influenced by three classes of factors: the predisposition to use services, the ability to use services, and the need for services. Predisposing factors are demographic and socioeconomic characteristics such as age, gender, race/ethnicity, marital status, health beliefs, and education level (Ringstrom et al., 2007). Even if individuals are predisposed to use health care services, certain characteristics must be in place for them to access them. These “enabling” factors represent the logistical aspects of obtaining care and include having health insurance, income, social support, and characteristics of the health care system. Without the ability to access health care, a predisposition to use these services does not necessarily lead to utilization. Last, for an individual to use health care, they must, of course, have a clinically meaningful health problem that registers a need for services. Need variables are often inferred from severity of an illness, its impact on activities of daily living or well-being, or duration. Fig. 1 provides a diagrammatic representation of the Andersen model.
Fig 1.
Andersen’s Behavioral Model of Health Care Utilization.
Further, the choice to use health care involves a two-stage decision making process. At the first stage, the individual makes the decision whether or not to contact a health care provider. At the next stage, the individual, working with their provider, determines the amount of treatment services to use. In other words, while the individual initiates the decision to contact a health care provider, the decision regarding intensity of treatment involves both the individual and the provider (Pohlmeier & Ulrich, 1995). Predisposing, enabling and need factors make up the context in which these decisions are made, each of which influences subsequent usage. The specific combination of factors that impact the decision of IBS patients to access health care is unknown.
This study sought to clarify the set of factors that impact health care utilization among patients with more severe IBS. Because of the two-stage nature of the decision-making process, it makes sense to examine these two aspects of health care use (probability of seeking help, frequency of use) which, to our knowledge, have not been simultaneously explored in patients with functional GI disorders. Because symptom factors have not emerged from previous research (Ringstrom et al., 2007; Talley et al., 1997; Williams et al., 2006) as a reliable predictor of health care use among IBS patients, we expected that enabling and predisposing factors may have a more robust impact on health care use as their influence is not disorder specific but cuts across the range of medical or mental health problems for which patients access care. Thus, we predicted that the magnitude of the relationship between health care use and both predisposing and enabling factors would be greater than that with need factors, such as symptoms and related distress.
1. Materials and methods
1.1. Participants
Participants were 291 consecutitvely enrolled IBS patients recruited at two tertiary academic medical centers in Buffalo, NY and Chicago, IL as part of an NIH-funded clinical trial, the details of which can be found elsewhere (Lackner et al., 2012). Patient characteristics are presented in Table 1. Participants were enrolled primarily through local media coverage, community advertising and physician referral. To be eligible for the study, all participants must have met the Rome III diagnostic criteria (Drossman, Corazziari, Talley, Thompson, & Whitehead, 2006) as determined by a board-certified gastroenterologist. Because this study was conducted as part of a clinical trial for moderately to severely affected patients with IBS (Lackner et al., 2012), participants must have also reported IBS symptoms of at least moderate intensity (i.e., symptom frequency of at least twice weekly for a minimum duration of 6 months and causing life interference). Participants with a comorbid organic GI illness that would adequately explain GI symptoms; mental retardation; current or past diagnosis of schizophrenia or other psychotic disorders; current diagnosis of depression with suicidal ideation; current diagnosis of psychoactive substance abuse were excluded. Institutional review board approval (UB, May 19, 2009; NU, December 19, 2008) Signed informed consent for each subject was obtained before s/he enrolled in the study. The study was completed in full compliance with the Declaration of Helsinki.
Table 1.
Means and percentages of the predisposing, enabling, and need variables for entire sample (N = 291).
| Variable | Mean ± SD | N(%) |
|---|---|---|
| Predisposing | ||
| Age | 40.85 ± 14.64 | |
| Number of Children | 0.96 ± 1.32 | |
| Body Mass Index | 26.43 ± 6.03 | |
| ETOH drinks/week | 2.81 ±4.88 | |
| Dietary Pattern | 34.02 ± 7.50 | |
| IBS Control Beliefs | 37.69 ± 8.05 | |
| Neuroticism | 20.57 + 6.11 | |
| Anxiety Sensitivity | 24.15 + 11.95 | |
| Stress | 6.92 + 3.29 | |
| Catastrophizing | 2.60 + 1.65 | |
| Gender (Female) | 231 (79.4) | |
| Race (White) | 260 (89.3) | |
| Married | 118(40.6) | |
| Disabled | 27 (9.3) | |
| Use Tobacco | 31 (10.7) | |
| Education | ||
| High school or less | 71 (24.4) | |
| College or associate degree | 136 (46.7) | |
| Graduate degree | 84 (28.9) | |
| Enabling | ||
| Social Support | 24.15 + 11.95 | |
| Income | 71.1 K + 49.3K | |
| Employment | ||
| Not working | 93 (32.0) | |
| Working <30 h/week | 52 (17.8) | |
| Working >30 h/week | 146 (50.2) | |
| Health Insurance | ||
| No insurance | 18 (6.2) | |
| Public insurance | 38 (13.1) | |
| Private Insurance | 235 (80.7) | |
| Need | ||
| IBS Symptom Severity | 285.72 + 74.72 | |
| Physical Health Status | 43.71 + 9.23 | |
| Medical Comorbidities, # | 5.66 + 5.30 | |
| Duration of IBS symptoms (years) | 16.15 + 13.74 | |
| Global Distress | 14.10 + 11.95 | |
| IBS Subtype | ||
| Mixed | 79 (27.2) | |
| Constipation | 83 (28.5) | |
| Diarrhea | 129 (44.3) |
1.2. Procedure
After a brief telephone interview to determine eligibility, participants underwent a medical examination administered by a board-certified gastroenterologist to confirm diagnosis of IBS based on Rome III criteria (Longstreth et al., 2006) and testing drawn from a battery of psychometrically validated measures detailed below. We categorized the measures into one of three domains of the Andersen model on the basis of prior research.
1.3. Measures
1.3.1. Predisposing factors
1.3.1.1. Dietary pattern
Participants completed a 10-item (7 questions about fruit and vegetable intake, 3 questions about foods high in fiber) measure called the Block Fruit/Vegetable/Fiber Screener (BFF-S: Block, Gillespie, Rosenbaum, & Jenson, 2000). The BFF-S asks respondents to characterize over the past 12 months their usual consumption of fruits and vegetables, fiber, and micro-nutrients found in fruits and vegetables using a 7-point frequency scale ranging from “never” to “twice a day or more”. Responses are summed, yielding a total score ranging from 10 to 70 with higher scores reflecting higher dietary intake. The screener has been validated against a “gold standard” 100-item, Block Food Frequency Questionnaire (Block et al., 1986).
1.3.1.2. IBS control beliefs
The IBS Locus of Control Scale (IBS-LOC: Lackner et al., 2007) is a 33-item, 5-point scale (1 = strongly disagree, 5 = strongly agree) that measures patients’ beliefs that their IBS symptoms are internally controlled (e.g., “my bowel symptoms are beyond all control”). Patients with higher internal locus of control beliefs see themselves as responsible for controlling their GI symptoms and take action to manage them. Internal consistency for the IBS-LOC in this sample was high (α = 0.82).
1.3.1.3. Neuroticism
The personality trait of neuroticism (chronic anxiety) was measured using the abbreviated Trait scale of the State Trait Anxiety Inventory (STAI: Spielberger, 1995). In responding to the 10 items of the STAI (e.g., “I worry too much over something that really doesn’t matter” and “I am content; I am a steady person”), participants indicate how they generally feel by rating the frequency of their feelings of anxiety on a 4-point scale ranging from 1 (almost never) to 4 (almost always). This scale is a well-validated measure whose items are calculated by averaging responses to this scale (after reverse scoring negatively-worded items). The trait anxiety scale exhibited good reliability in the current sample (α = 0.88).
1.3.1.4. Anxiety sensitivity
Anxiety sensitivity was measured using the 16-item Anxiety Sensitivity Inventory (ASI: Peterson & Reiss, 1993) which reflects fear of anxiety (e.g., “It scares me when I am anxious”), arousal-related bodily sensations (e.g., “It scares me when my heart beats rapidly”), and their consequences (e.g., “When I notice my heart is beating rapidly, I worry that I might have a heart attack”). Items are rated on a 6-point scale (0 = very little, 5 = very much) and yield a range of scores ranging from 0 to 64 with higher scores signifying greater fear of anxiety/arousal symptoms. The scale showed good internal consistency in the present sample (α = 0.89).
1.3.1.5. Stress
The four-item version of the Perceived Stress Scale (PSS: Cohen & Williamson, 1988) measures the degree to which individuals perceive situations in their life as uncontrollable, unpredictable, and overloading. These three factors are regarded as core aspects of the stress experience. Items are rated on a 5-point Likert scale ranging from 0 (never) to 4 (very often). Scores range from 0 to 16. Norms for the 4 item version of the PSS from a United States probability sample were 4.49 (Cohen & Williamson, 1988). The PSS exhibited good internal consistency in the current sample (α = 0.83).
1.3.2. Catastrophizing
Catastrophizing was measured using the two item version of Catastrophizing subscale of the Coping Strategies Questionnaire (Jensen, Keefe, Lefebvre, Romano, & Turner, 2003). Items ask patients to rate the frequency with which they, during an episode of pain, engage in various beliefs thought to index catastrophizing (e.g., “When I am in pain … I feel I can’t stand it anymore; It is terrible and I feel it is never going to get any better”). Respondents rate how characteristic each item is of them using a 6-point Likert scale ranging from 0 (never do) to 6 (always do). The two item measure correlates strongly (r = 0.91) with the full scale version of the Catastrophizing scale (Jensen et al., 2003) and showed good internal consistency in the present sample (α = 0.81).
Other predisposing factors assessed included age, number of children, body mass index, number of alcoholic drinks per week, gender, race/ethnicity, level of education, marital status, disability status, and current tobacco use (Yes/No).
1.3.3. Enabling factors
1.3.3.1. Social support
The short form of the Interpersonal Support Evaluation List (ISEL-12: House & Kahn, 1985) consists of a 12 statements concerning the perceived availability of social support. Items are rated on a 4-point scale with anchors ranging from “definitely true” to “definitely false”. A total score of all items (after reverse coding 6 items) yields an index of the patient’s general perception of social support. Psychometric studies support the ISEL-12 as a brief, internally consistent instrument with adequate convergent validity (Mosley et al., 1996) and exhibited good internal consistency in the current sample (α = 0.86).
Additional enabling factors assessed in the study include income, employment status, and health insurance coverage, if any, all of which were assessed during intake evaluation.
1.3.4. Need factors
1.3.4.1. IBS symptom severity
The Irritable Bowel Syndrome Symptom Severity Scale (IBS-SSS: Francis, Morris, & Whorwell, 1997) is a 5-item instrument used to measure severity of abdominal pain, frequency of abdominal pain, severity of abdominal distension, dissatisfaction with bowel habits, and interference with quality of life on a 100-point scale. Items are summed with total scores ranging 0 to 500 with higher scores signifying more severe symptoms. Rome III has recommended the IBSSS as a global measure of symptom severity (Irvine et al., 2006) Alpha for the IBS-SSS was .55.
1.3.4.2. Physical health
The 12-item Short Form (SF-12: Ware, Kosinski, & Keller, 1996) assesses self-reported physical health status across 6 domains: physical functioning, role functioning physical, bodily pain, general health, energy/fatigue (vitality), and role functioning. These domains yield a physical health status index called the Physical Component Summary (PCS). The Physical Component Summary of the SF- 12 has shown good reliability and validity (Ware et al., 1996) and had high internal consistency in the present sample (α = 0.84).
1.3.4.3. Mental health
Global psychological distress was assessed using the 18-item version of the Brief Symptom Inventory (BSI-18: Derogatis, 2000). The BSI-18 requires respondents to indicate on a 5-point scale (0 = not at all, 4 = extremely) their level of distress of 18 somatic and psychological symptoms for three types of problems (i.e., anxiety, somatization, depression). The average intensity of all items yields a composite index of psychological distress (Global Severity Index [GSI]). The GSI has been used extensively to measure global psychological distress in patients with IBS (Dorn et al., 2007). Internal consistency for the GSI in this sample was excellent (α = 0.92).
1.3.4.4. Medical comorbidities
Medical comorbidity was assessed using a comorbidity checklist that covers 112 medical conditions common to IBS patients (Lackner et al., 2013). Respondents were asked whether a doctor had ever diagnosed them with a condition and, if so, whether the condition was present in the past 3 months. Persons were counted as current cases if the diagnosed condition was reported as present in the last 3 months. Number of medical comorbidities yields a total comorbidity score.
Additional need variables included the duration IBS symptoms and predominant bowel habit (diarrhea-, constipation-predominant, alternating) based on Rome classification.
1.3.5. Dependent measures
1.3.5.1. Health care use
Medical and mental health care use was assessed through a semi structured interview called the IBSOS Economic Form (IBSOS EF, Lackner & Dunlap, 2009). The IBSOS EF was modelled after the Form 90 Economic Data (Form 90 ED) which is an psychometrically validated (Bray et al., 2007; Miller and Del Boca, 1994; Scheurich et al., 2005; Tonigan, Miller, and Brown, 1997) instrument used to capture economic data including the quantity of health care utilization across different care settings (e.g., hospitalizations, emergency services, physician and mental health visits). In addition to these services, the IBSOS EF collected use data for services deemed relevant for IBS: rehabilitative care (e.g., physical therapy, chiropractic), alternative and complementary services (e.g., acupuncture, massage), laboratory services, surgical procedures, as well as devices (e.g. eye glasses). Using this form, subjects were first asked whether or not they had accessed specific medical or mental health care services in the past 3 months. For those individuals who used a given health care service, we then obtained information regarding the number of encounters (e.g., physician visits, diagnostic tests, admissions, emergency room visits) over the previous 3 months. Because the form collects data separately for medical care and mental health care services, we modeled medical care and mental health care separately for our study. Medical care was operationalized as any non-mental health encounter used for the management, assessment, and care of a disease or disorder. These medical care encounters were collapsed into one (medical) care category for ease of interpretation/analyses and because of the distribution of observations across categories. Additionally, a medical vs mental care categorization typifies the bifurcated way health care organizations organize health care use. For both medical and mental health care, the dependent variable representing any service use equals 1 if the individual used any services in the 3 month period and zero otherwise. The dependent variable representing frequency of use (among those who had any use) equals the individual’s reported number of encounters for the relevant category (medical care or mental health care) in the 3 month period.
1.3.6. Statistical strategy
Patient demographic and clinical characteristics were analyzed using measures of central tendency. Frequencies were calculated for categorical variables and means and standard deviations were calculated for continuous variables. Race was excluded from all further analyses due to lack of variance. Next, bivariate analyses were performed to test for associations between the independent variables and health care use probability. Student’s t-tests were performed for continuous independent variables and chi-square analyses for categorical independent variables. The alpha level for these analyses was set at 0.05.
Finally, because a sizable proportion of individuals typically do not to use health care services, utilization data often contain a significant number of zeroes. This calls for a two-stage model to identify predictors of both the probability (logistic regression) and, conditional on use, the frequency (negative binomial regression) of health care use. The hurdle model assumes that the statistical process governing individuals with zero counts and individuals with one or more counts may differ. That is, the decision on whether to use any care and the decision on the frequency of usage may be subject to different decision making processes. As noted above, the patient is responsible for making the initial decision to contact the health care professional (HCP), while the patient works with the HCP to determine the amount of treatment services to use. At both stages, predisposing, enabling and need factors may affect the subsequent usage decision, but how these factors or combination thereof affect the decision may differ across the two stages. An approach that recognizes the complexity of health care and its determinants across multiple domains has the potential to identify where and why differences in health services use occur. In addition, the hurdle model is methodologically attractive and appropriate because it accounts for prevalence of zeroes due to non-users (Jiménez-Martín, Labeaga, & Martínez-Granado, 2002; Pohlmeier & Ulrich, 1995). The alpha level for these two-stage models was set at 0.05.
With regard to the second stage (frequency), the regression coefficients obtained are not directly interpretable due to the negative binomial distribution being nonlinear. Therefore, the coefficients were transformed into incident rate ratios (IRRs) by computing their exponentials (i.e., eβ). The IRRs describe the change in an independent variable as a multiple of the health care utilization of the reference group. For example, if the IRR for gender was 1.5, females would utilize health care 50% more than males.
Because the participants were recruited as part of another larger study, a priori sample size/power calculations were not conducted. However, post-hoc power analyses indicate that for the logistic regression models, with the given medical care visit rate of 80% and the mental health care visit rate of 28%, to detect a significant odds ratio of 2 at an alpha level of 0.05, our sample size of 291 can reach the power of 70% for a binary predictor and the power of 98% for a continuous variable with 1 SD change. The sample size of 291 would also detect significant moderate effect sizes with relatively sufficient power for other scenarios considered in post-hoc power analysis.
2. Results
2.1. Characteristics of the sample
Table 1 presents the demographics and clinical characteristics of the sample, which was mostly female, white, educated, and chronically ill. Fifty-five percent of the patients were childless and half of the sample had BMIs ≥30. Patients drank an average of 3 alcoholic drinks per week and most (89%) did not use tobacco products. Levels of neuroticism and stress were above average for the sample based on normative data for the STAI-T and PSS. Sixty-eight percent of the sample worked at least 30 h per week; most (80.7%) reported having private health insurance; and more than half (58%) reported having a family income of greater than $50,000 per year. In general, patients reported having at least one person they counted on for social support.
2.1.1. Bivariate analysis
Table 2 compares the means and percentages of the predisposing, enabling, and need variables between health care users and non-users. Out of the 291 patients in the sample, 234 (80.4%) sought medical care within the past 3 months. The predisposing variables that distinguished users and non-users of medical care were gender and dietary intake of fruits, vegetables, and fiber. Female patients and patients who reported less daily intake of these foods were more likely to have used medical care. With regard to enabling variables, patients having health insurance (public or private) were more likely to have utilized health care services than those patients with no insurance. Finally, with regard to need variables, patients with more severe IBS symptoms and worse physical health were more likely to have utilized medical care.
Table 2.
Comparisons of means and percentages between users and non-users of health services in the past 3 months.
| Medical care visit |
Mental health care visit |
|||||
|---|---|---|---|---|---|---|
| Yes (n = 234) | No (n = 57) | p-value | Yes (n = 81) | No (n = 210) | p-value | |
| Predisposing | ||||||
| Age | 40.71 ± 14.43 | 41.42 ± 15.57 | 0.742 | 41.77 ± 14.24 | 40.50 ± 14.8 | 0.508 |
| Number of Children | 1.04 ± 1.38 | 0.64 ± 1.00 | 0.017 | 1.03 ± 1.27 | 0.93 ± 1.34 | 0.591 |
| Body Mass Index | 26.48 ± 6.10 | 26.23 ± 5.76 | 0.779 | 26.89 ± 6.80 | 26.25 ± 5.71 | 0.420 |
| ETOH drinks/week | 2.49 ± 3.93 | 4.14 ± 7.54 | 0.115 | 1.95 ± 3.58 | 3.15 ± 5.27 | 0.027 |
| Dietary Pattern | 33.54 ± 7.67 | 35.96 ± 6.44 | 0.025 | 33.96 ± 7.62 | 34.04 ± 7.47 | 0.939 |
| IBS Control Beliefs | 37.39 ± 8.03 | 38.91 ± 8.07 | 0.202 | 39.90 ± 7.16 | 36.84 ± 8.22 | 0.004 |
| Neuroticism | 20.71 ± 6.23 | 20.02 ± 5.60 | 0.454 | 23.51 ± 6.75 | 19.41 ± 5.43 | 0.001 |
| Anxiety Sensitivity | 24.10 + 11.95 | 24.38 ± 12.02 | 0.876 | 27.35 ± 12.52 | 22.90 ±11.50 | 0.005 |
| Stress | 7.00 ± 3.35 | 6.68 ± 2.97 | 0.522 | 8.59 ± 3.39 | 6.29 ± 3.01 | 0.001 |
| Catastrophizing | 2.65 ± 1.64 | 2.39 ± 1.70 | 0.276 | 2.74 ± 1.70 | 2.55 ± 1.63 | 0.367 |
| Gender(%) | 0.008 | 0.129 | ||||
| Male | 41 (68.3) | 19 (31.7) | 12 (20.0) | 48 (80.0) | ||
| Female | 193 (83.55) | 38 (16.45) | 69 (29.9) | 162 (70.1) | ||
| Married (%) | 0.125 | 0.307 | ||||
| Married | 100 (84.8) | 18 (15.2) | 29 (24.6) | 89 (75.4) | ||
| Not married | 134 (77.5) | 39 (22.5) | 52(30.1) | 121 (69.9) | ||
| Disabled (%) | 0.513 | 0.264 | ||||
| Disabled | 23 (85.2) | 4(14.8) | 10 (37.0) | 17 (63.0) | ||
| Not disabled | 211 (79.9) | 53 (20.1) | 71 (26.9) | 193 (73.1) | ||
| Use Tobacco (%) | 0.973 | 0.001 | ||||
| Yes | 25 (80.7) | 6 (19.3) | 15 (48.4) | 16 (51.6) | ||
| No | 209 (80.4) | 51 (19.6) | 66 (25.4) | 194 (74.6) | ||
| Education (%) | 0.191 | 0.287 | ||||
| High school or less | 58 (81.7) | 13 (18.3) | 18 (28.1) | 46 (71.9) | ||
| College/associate degree | 114(83.8) | 22 (16.2) | 31 (22.8) | 105 (77.2) | ||
| Graduate degree | 62 (73.8) | 22 (26.2) | 30 (35.7) | 54 (64.3) | ||
| Enabling | ||||||
| Social Support | 39.66 ± 6.55 | 39.33 ± 6.43 | 0.734 | 38.65 ± 6.90 | 39.97 ± 6.34 | 0.126 |
| Income | 71.8 K± 49.2 K | 67.8 K ± 49.7 K | 0.587 | 70.5 K± 51.2 K | 71.32 K± 48.6 K | 0.914 |
| Employment (%) | 0.574 | 0.114 | ||||
| Not working | 74 (79.6) | 19 (20.4) | 31 (33.3) | 62 (66.7) | ||
| Working <30 h/week | 40 (76.9) | 12 (23.1) | 15 (28.9) | 37(71.1) | ||
| Working >30 h/week | 120 (82.2) | 26 (17.8) | 35 (24.0) | 111 (76.0) | ||
| Health Insurance (%) | 0.001 | 0.011 | ||||
| No insurance | 7 (38.9) | 11 (61.1) | 2 (11.1) | 16 (88.9) | ||
| Public insurance | 33 (86.8) | 5 (13.2) | 16 (42.1) | 22 (57.9) | ||
| Private Insurance | 194 (82.6) | 41 (17.4) | 63 (26.8) | 172 (73.2) | ||
| Need | ||||||
| IBS Symptom Severity | 290 ± 75.85 | 267.56 ± 67.41 | 0.035 | 297.05 ± 63.44 | 281.29 ± 78.40 | 0.079 |
| Physical Health Status | 43.16 ± 9.33 | 46.02 ± 8.50 | 0.036 | 41.99 ± 9.53 | 4439 ± 9.05 | 0.041 |
| Medical Comorbidities, # | 5.81 ± 5.36 | 5.05 ± 5.09 | 0.346 | 7.55 ± 6.00 | 4.93 ± 4.83 | 0.005 |
| Duration of IBS symptoms | 16.43 ± 13.73 | 15.04 ± 13.83 | 0.496 | 18.83 ± 15.30 | 15.12 ± 12.98 | 0.078 |
| Global Distress | 14.27 ± 12.15 | 13.38 ± 11.14 | 0.621 | 20.16 ± 14.33 | 11.72 ± 9.94 | 0.001 |
| IBS Subtype (%) | 0.502 | 0.837 | ||||
| Mixed | 67 (84.8) | 12 (15.2) | 22 (27.8) | 57 (72.2) | ||
| Constipation | 66 (79.5) | 17 (20.5) | 25 (30.1) | 58 (69.9) | ||
| Diarrhea | 101 (78.3) | 28 (21.7) | 34 (26.4) | 95 (73.6) | ||
Note. Bolded numbers are statistically significant at 0.05 (unadjusted).
Eighty-one (27.8%) patients in the sample utilized mental health care within the past 3 months of their initial evaluation. For predisposing variables, patients higher in neuroticism and stress, and with stronger fears of arousal symptoms were more likely to access mental health services. Also, patients with stronger beliefs in their ability to control IBS symptoms (IBS-LOC) and those who used any tobacco products had a greater probability of using mental health services. Among enabling factors, patients who had public health insurance were more likely to have been treated for mental health issues than those with private or no insurance. With respect to need variables, patients with more physical comorbidities and psychological distress were more likely to have utilized mental health care.
2.2. Two-stage model
2.2.1. First stage: probability of health care utilization
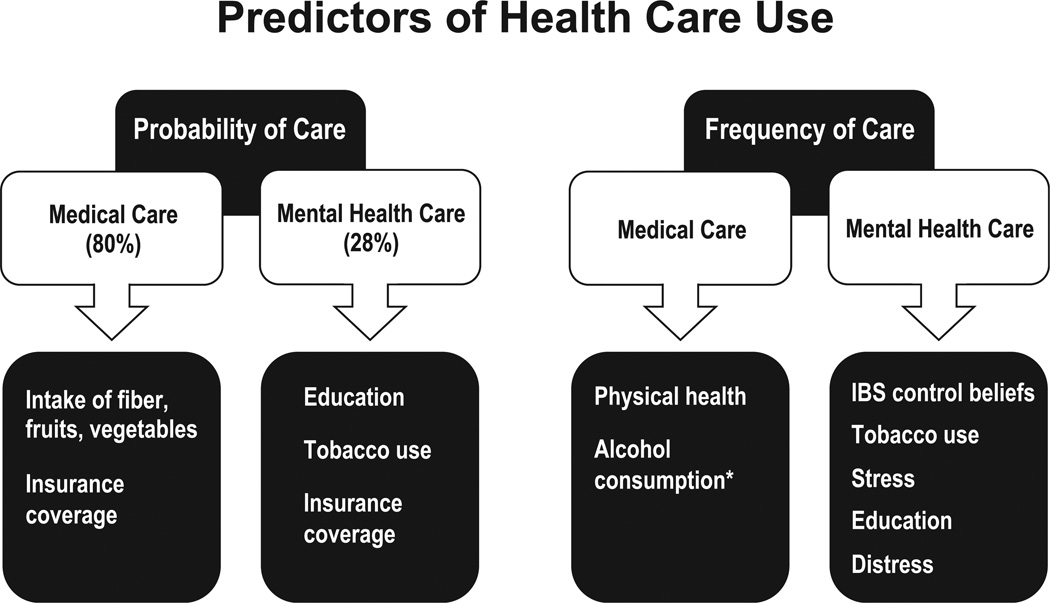
Separate binary logistic regressions were run for medical care and mental health care utilization. Results are shown in Table 3. For medical care utilization, significant independent predictors were dietary intake and type of health insurance. As mentioned in the bivariate analyses, patients who reported a relatively lower intake of fruits, fiber, and vegetables were more likely to have utilized medical care. Furthermore, patients with public health insurance were over 10 times more likely to have used medical care than those with no insurance, whereas patients with private health insurance were almost eight times more likely to have used medical care than those with no insurance.
Table 3.
Factors predicting the probability of utilizing medical and mental health care.
| Predictors | Medical care |
Mental health care |
||
|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Predisposing | ||||
| Age | 0.99 (0.95–1.03) | 0.505 | 0.99 (0.97–1.04) | 0.930 |
| Number of Children | 1.17 (0.79–1.73) | 0.436 | 1.24 (0.90–1.70) | 0.189 |
| Body Mass Index | 1.01 (0.94–1.09) | 0.783 | 0.99 (0.93–1.05) | 0.636 |
| ETOH drinks/week | 0.95 (0.88–1.03) | 0.197 | 0.91 (0.82–1.01) | 0.086 |
| Dietary Pattern | 0.94 (0.89–0.99) | 0.022 | 1.01 (0.96–1.06) | 0.728 |
| IBS Control Beliefs | 1.01 (0.96–1.07) | 0.633 | 1.05 (0.99–1.10) | 0.071 |
| Neuroticism | 1.10 (0.99–1.23) | 0.093 | 1.06(0.97–1.16) | 0.196 |
| Anxiety Sensitivity | 0.97 (0.93–1.02) | 0.190 | 0.99 (0.95–1.04) | 0.788 |
| Stress | 0.94(0.80–1.11) | 0.487 | 1.14(0.99–1.31) | 0.079 |
| Catastrophizing | 0.98 (0.73–1.30) | 0.866 | 0.83 (0.64–1.07) | 0.154 |
| Gender | 1.30 (0.50–3.43) | 0.590 | 1.33 (0.50–3.54) | 0.575 |
| Married | 1.73 (0.64–4.68) | 0.284 | 0.51 (0.21–1.23) | 0.133 |
| Disabled | 0.72 (0.14–3.59) | 0.684 | 0.79 (0.18–3.43) | 0.750 |
| Use Tobacco | 1.82 (0.48–6.89) | 0.380 | 3.94 (1.34–11.61) | 0.013 |
| Education | ||||
| College vs. High School | 0.72 (0.26–2.00) | 0.521 | 0.62 (0.24–1.60) | 0.319 |
| College vs. Grad degree | 0.50 (0.16–1.08) | 0.071 | 2.63 (1.20–5.76) | 0.016 |
| Enabling | ||||
| Social Support | 1.01 (0.94–1.07) | 0.987 | 1.01 (0.94–1.07) | 0.963 |
| Income | 1.02 (0.98–1.05) | 0.687 | 0.99(0.96–1.01) | 0.345 |
| Employment | ||||
| Full-time vs. Part-time | 1.14 (0.38–3.47) | 0.814 | 1.53 (0.49–4.77) | 0.464 |
| Full-time vs. None | 1.99 (0.71–5.53) | 0.190 | 0.83 (0.33–2.10) | 0.699 |
| Health Insurance | ||||
| None vs. Private | 8.32 (1.94–35.66) | 0.004 | 10.03 (1.03–23.99) | 0.033 |
| None vs. Public | 10.33 (1.79–59.75) | 0.009 | 17.71 (1.09–38.70) | 0.015 |
| Need | ||||
| IBS Symptom Severity | 1.01 (0.99–1.04) | 0.303 | 1.01 (0.99–1.03) | 0.620 |
| Physical Health Status | 0.94 (0.89–1.08) | 0.076 | 1.03 (0.98–1.08) | 0.306 |
| Medical Comorbidities, # | 1.05 (0.94–1.17) | 0.408 | 1.05 (0.96–1.14) | 0.316 |
| Duration of IBS symptoms | 0.99 (0.97–1.03) | 0.914 | 1.01 (0.98–1.04) | 0.442 |
| Global Distress | 0.97 (0.92–1.03) | 0.367 | 1.04 (0.99–1.09) | 0.105 |
| IBS Subtype | ||||
| Mixed vs. Constipation | 0.58 (0.20–1.74) | 0.337 | 1.65 (0.63–4.33) | 0.313 |
| Mixed vs. Diarrhea | 0.57 (0.21–1.58) | 0.285 | 1.35(0.54–3.41) | 0.523 |
Note. Bolded numbers are statistically significant.
OR = Odds Ratio.
With regard to mental health care utilization, education level, type of health insurance, and current tobacco use emerged as significant predictors. Patients with a graduate degree were 2.6 times more likely to have used mental health care than those who have an undergraduate degree or less education. As with medical care, patients with any type of health insurance were more likely to have utilized treatment for mental health issues than those with no insurance. Finally, patients who used any type of tobacco products were almost four times more likely to have utilized mental health services than those who did not use tobacco.
2.2.2. Second stage: frequency of health care utilization
Results for the negative binomial regressions analyzing the frequency of health care utilization are shown in Table 4. For frequency of medical care utilization, the number of alcoholic drinks per week and physical health status were significant predictors. The number of medical encounters significantly declined as patients’ alcohol intake increased. Each additional drink per week was associated with an estimated 5% decrease in medical care visits. For example, an additional 10 drinks per week (0.95 ^ 10 = 0.599) was associated with a 40% decline in frequency of utilizing medical care. As for physical health, a one-unit decrease on the SF12-PCS was associated with about a 3% increase in medical care visits. The average number of medical visits for those patients who utilized medical care was 3.4 (SD = 3.2).
Table 4.
Factors predicting the frequency of utilizing medical and mental health care services.
| Predictors | Medical care |
Mental health care |
||
|---|---|---|---|---|
| IRR (95% CI) | p-value | IRR (95% CI) | p-value | |
| Predisposing | ||||
| Age | 0.99 (0.98–1.02) | 0.905 | 0.98 (0.94–1.02) | 0.186 |
| Number of Children | 1.02 (0.88–1.18) | 0.817 | 1.99 (0.93–1.45) | 0.132 |
| Body Mass Index | 0.99 (0.96–1.02) | 0.393 | 0.97(0.93–1.01) | 0.128 |
| ETOH drinks/week | 0.95 (0.92–0.98) | 0.033 | 0.96 (0.91–1.07) | 0.234 |
| Dietary Pattern | 0.99 (0.98–1.02) | 0.678 | 0.97 (0.92–1.04) | 0.527 |
| IBS Control Beliefs | 0.99 (0.98–1.02) | 0.864 | 1.03 (1.01–1.08) | 0.021 |
| Neuroticism | 1.01 (0.96–1.05) | 0.949 | 1.03 (0.98–1.08) | 0.174 |
| Anxiety Sensitivity | 1.01 (0.98–1.03) | 0.611 | 1.02 (0.98–1.10) | 0.199 |
| Stress | 1.01 (0.94–1.07) | 0.977 | 1.12 (1.02–1.21) | 0.015 |
| Catastrophizing | 1.05 (0.94–1.16) | 0.384 | 1.09 (0.95–1.25) | 0.126 |
| Gender | 1.12(0.71–1.75) | 0.645 | 1.21 (0.89–1.93) | 0.502 |
| Married | 0.91 (0.61–1.37) | 0.663 | 0.62 (0.37–0.92) | 0.031 |
| Disabled | 1.03 (0.55–1.93) | 0.924 | 1.20 (0.54–2.64) | 0.663 |
| Use Tobacco | 1.20 (0.69–2.08) | 0.511 | 1.99 (1.15–3.49) | 0.014 |
| Education | ||||
| College vs. High School | 1.20 (0.85–2.21) | 0.397 | 1.16(0.76–1.85) | 0.284 |
| College vs. Grad degree | 1.06 (0.86–1.24) | 0.742 | 2.88 (1.80–4.62) | 0.001 |
| Enabling | ||||
| Social Support | 0.99 (0.97–1.02) | 0.616 | 0.99 (0.96–1.02) | 0.958 |
| Income | 0.98 (0.96–1.03) | 0.778 | 0.98 (0.95–1.03) | 0.769 |
| Employment | ||||
| Full-time vs. Part-time | 1.32 (0.84–2.12) | 0.231 | 1.43(0.79–2.61) | 0.232 |
| Full-time vs. None | 1.30 (0.83–2.03) | 0.253 | 1.66(0.95–2.91) | 0.113 |
| Health Insurance | ||||
| None vs. Private | 1.86 (0.80–4.29) | 0.148 | 1.27 (0.52–3.14) | 0.602 |
| None vs. Public | 1.90 (0.77–4.67) | 0.162 | 1.51 (0.49–4.62) | 0.475 |
| Need | ||||
| IBS Symptom Severity | 1.01 (0.98–1.03) | 0.976 | 1.01 (0.99–1.06) | 0.539 |
| Physical Health Status | 0.97 (0.95–0.99) | 0.026 | 1.02 (0.99–1.05) | 0.098 |
| Medical Comorbidities, # | 1.03 (0.99–1.08) | 0.105 | 1.03 (0.98–1.09) | 0.210 |
| Duration of IBS symptoms | 0.99 (0.97–1.01) | 0.223 | 0.99 (0.98–1.02) | 0.414 |
| Global Distress | 1.01 (0.98–1.03) | 0.603 | 1.04 (1.01–1.09) | 0.005 |
| IBS Subtype | ||||
| Mixed vs. Constipation | 0.96 (0.63–1.47) | 0.849 | 0.78 (0.45–1.33) | 0.369 |
| Mixed vs. Diarrhea | 0.89 (0.59–1.33) | 0.560 | 0.79 (0.49–1.37) | 0.409 |
Note. Bolded numbers are statistically significant.
IRR = Incident Rate Ratio.
A number of factors emerged as significant independent predictors of the frequency of mental health care visits. Patients with graduate degrees had approximately a 180% higher rate of mental health care visits than patients with a college degree. There was no significant difference between college graduates and patients who had a high school diploma or less education. Unmarried patients had about 38% more mental health care visits than married patients, and patients using tobacco products had an estimated 99% more visits than nonusers of tobacco. Finally, mental health care visits were greater in patients who reported more stress, distress, and had stronger beliefs in their ability to control IBS symptoms. A one-unit increase on each measure was associated with increased relative rate of frequency in visits of 12%, 4%, and 3%, respectively. Of patients who utilized mental health services, the average number of mental care visits was 6.1 (SD = 5.6). Data for two-stage model are diagrammatically represented in Fig. 2.
Fig 2.
Predictors of Health Care Use. Note. * Denotes inverse relationship.
3. Discussion
We sought to identify predictors of health care use in a sample of IBS patients. To this end, we adopted the Andersen model which holds that the decision to use health care is a function of three main elements: the demographic and socioeconomic qualities that predispose patients to use services, enabling factors that impede or facilitate access to services, and patient needs (e.g. illness severity). In our subset of IBS patients, the decision to use any medical care was associated with the predisposing factor of dietary intake (frequency of fruit, fiber, and vegetable intake). Patients who consumed more of these foods were less likely to utilize medical care. While the IBS symptom relieving benefits of dietary changes is unclear (Brandt et al., 2009), they may have an independent impact on health care use that, to our knowledge, has been unexplored. Consuming higher levels of fruit, fiber and vegetables may be part of a healthier lifestyle that is manifested behaviorally in less health care use than patients who eat less fruits, fiber and vegetables. Only a handful of studies have investigated the impact of dietary intake on health care utilization (Collins, Patterson, & Fitzgerald, 2011; Lo, Wahlqvist, Chang, Kao, & Lee, 2013). Our data extends the general pattern of these data to the problem of functional GI disorders and warrant replication with a more fine grained dietary intake measure than the screener we used.
Of predisposing factors, both tobacco use and educational attainment were significant independent predictors of the probability of using mental health care. Our data echo the broader literature showing that smokers consume more mental health services (Heiligenstein & Smith, 2006; Pahl, Brook, Zhang, & Brook, 2014). Similarly, education has been found to predict health care use, even after controlling for confounding factors such as income and health insurance (Burgard & Hawkins, 2014; Fleury, Grenier, Bamvita, & Caron, 2014; Kanazawa et al., 2004; Sialubanje, Massar, Hamer, & Ruiter, 2014; Williams et al., 2006). More educated persons may be more aware of health problems and available resources and therefore more likely to use health care services to maintain their health.
For both medical care and mental health care, IBS patients with health insurance had a higher probability of using medical or mental health care than those patients without insurance. This finding echoes broader research showing that having health insurance is one of strongest determinants of utilization. Kasper, Giovannini, and Hoffman (2000) found that adults who had insurance after a lapse in coverage accessed more health care services while those who lost their health insurance reported a reduction in access to medical services. While intuitive, the relationship between financial resources like insurance and health care use to our knowledge has not been empirically validated in IBS patients and has implications for practitioners and health care organizations who are seeking to identify those at high risk for utilization and link them to resources and interventions that help them manage more effectively symptoms unresolved through conventional medical options.
Our results support the notion that the decision to use any health care and the further decision of how much health care to use are different decision making processes subject to different explanatory influences. Whereas dietary intake was associated with the decision to use any medical care, it was unrelated to how much medical care was used. Significant predictors of the level (frequency) of medical care use were alcohol consumption and physical health, neither of which predicted the initial decision of whether to seek any medical care. Patients who either consumed more alcohol or reported better physical health consumed fewer health care resources. We expected that alcohol consumption would show a similar relationship to health care use as tobacco use. We found the opposite. While somewhat counterintuitive, an inverse relationship between alcohol consumption and medical health care use echoes findings of several epidemiological studies showing that non-problem drinking was associated with less health care use (hospital visits, hospitalizations and medical emergencies) (Klatsky, Armstrong, & Friedman, 1989; Longnecker & MacMahon, 1988; Rice & Duncan, 1995). Further study is necessary to clarify this relationship and its underlying mechanism(s). It is possible that non-problem alcohol drinkers use less health care because they make healthier lifestyle choices in general and not simply because they consume alcohol.
Different variables predicted the frequency of mental vs medical health services use. Frequency of mental health care increased with marital status (unmarried), education level, and tobacco use. Additional predictors of mental health care use included emotional distress, patients’ beliefs they had greater control over their IBS symptoms (internal locus of control beliefs), and stress. The association between mental health care use and internalized control beliefs is notable. We expected that patients with stronger control beliefs would be more likely to manage symptoms on their own and as a result use (Talley et al., 1997) fewer health care resources. While “internals” may be empowered to control their health on their own, they also may be more likely to seek out health care resources when their own symptom self-management efforts fall short. Having stronger illness control beliefs, like being better educated, may not necessarily be a prescription for reducing health care use.
In our study, predisposing factors predictive of medical care use were limited to consumption of fruits, fiber and vegetables and alcohol. The relatively homogenous composition of our sample may have reduced variability of other predisposing factors such as race, age, and income level. If so, a larger more diverse sample may yield different results. Like others (Ringstrom et al., 2007; Talley et al., 1997), we found that the severity of GI symptoms – what the Andersen model classifies as a “need” factor – was not a significant predictor of overall health care use. These data do not diminish the clinical importance of GI symptoms. They are, after all, the most direct influences of care for GI disorders. In understanding patterns of health care use in general, their influence should be put in context of a larger set of enabling and predisposing factors that cuts across different health problems.
With relatively few exceptions, the behavioral literature has given short shrift to health care utilization as an outcome measure. To our knowledge, health care use is not a standard part of assessment battery of empirically supported treatments (e.g., Agras, Walsh, Fairburn, Wilson, & Kraemer, 2000; DeRubeis et al., 2005) This is disappointing given Kazdin and Wilson (1978)’s prescient exhortation 38 years ago that breadth of change is an important dimension for gauging the therapeutic value of psychological treatments that emphasize symptom self-management. They did not simply see breadth of change as simply an useful secondary outcome measure (Kazdin & Wilson, 1978) but fundamental to evaluating how well a treatment worked. Breadth of change was inextricably linked to efficacy and was no less important than durability of improvement, magnitude of treatment effect, or clinical significance of therapeutic gain. In an increasingly competitive value-based health care environment, health care use is primed to become an increasingly important measure for gauging the clinical value of interventions of any denomination. Understanding patterns of health care use and their determinants is fundamental to laying a foundation for establishing the efficacy profile of novel treatments like CBT and, for that matter, other dietary, exercise and pharmacological treatments for IBS and other disorders that are a public health threat. This paper outlines an innovative, potentially impactful conceptual and methodological framework for studying health care use that behavioral and non-behavioral clinical trialists alike can apply to their work.
While the study improves upon aspects of prior research in a number of ways, it is not without limitations. Because data were collected via self-report, they are subjective and vulnerable to varying degrees of error, distortion, and bias. While the breadth of our testing battery is a strength of this study, it was not designed as an exhaustive investigation of the universe of factors that may impact utilization. Our data are cross sectional and therefore cannot establish causal relationships between predictor variables and health care use. At best, our data outline a working model of health care use of more severely affected IBS patients. Additionally, our findings are based on a subset of treatment-seeking individuals who voluntarily enrolled in a randomized controlled trial of a behavioral treatment for a physical health problem. For this reason, our subjects may be more psychologically minded patients and therefore more likely to access mental health services. Because the sample was predominantly White, middle class, and female, results may not necessarily generalize to more heterogeneous samples. Nor do our data necessarily extend to community populations (i.e., non-users) who represent the majority of individuals with symptoms of IBS (Spiller et al., 2007). It is possible that a more diverse sample yields alternative predictive models highlighting different influences on health care utilization. Because this study was based on a clinical trial for IBS, we did not have a control group that would have allowed us to determine the specificity of findings. We did not collect actual claims data. While this was not the intended objective of the study, cost data would have enriched our understanding of utilization as an outcome and the impact these costs have on our health care system. Our application of the Andersen model focused on individual level factors, and not on community and system level delivery factors which are particularly important in managed care environments (de Boer, Wijker, & de Haes, 1997). We acknowledge that a limitation with relying on the number of encounters is that it obscures the qualitative differences between health services accessed (e.g., preventive services, annual checkups vs. emergency room visits, reassurance seeking physician visits). We only collected data for use of outpatient mental health care visits. We are unable to discern whether the demand for medical care was due to mental health problems (e.g., anxiety of noncardiac chest pain triggering ER visit, primary care visits for depression). Because our study lacked a control group, we do not know whether the pattern of data is specific to IBS. In some cases, marginal group differences were statistically significant. Where these differences are clinically significant is unclear. It is possible that a small, seemingly trivial unit change in behavior amounts to larger impact on health care (Marteau, Ogilvie, Roland, Suhrcke, & Kelly, 2011). Finally, the number of comparisons renders us vulnerable to Type I error and therefore our results should be interpreted judiciously. That said, this study was not designed as a definitive exploration of the predictors of health care use but an explorative test of two different types of health care use from the perspective of the Andersen model. Further research with a larger sample size can make more definitive conclusions.
Notwithstanding these limitations, our findings bring into sharper focus the factors that may govern the decisions among IBS patients to access health care. Health care use is not simply an outcome. It is the product of a complex cognitive process about which we do not fully understand. Conventional wisdom that health care is necessarily driven solely by symptoms that define the disorder for which patients seek one type of treatment is not wholly accurate. The decision to use health care and the frequency of use are qualitatively different decision-making processes subject to different influences. Their relative impact depends on whether the focus is on medical or mental health care. If there is a unifying theme of our data, it is the importance of behavioral factors in explaining patterns of health care use. What patients eat, the activities they think they can and cannot do, their beliefs about symptoms and their expected impact on their lives, and their lifestyle choices (e.g. use of tobacco) have a particularly strong impact on the demand for health care. Understanding their specific impact on health care use has the potential to support the development of disease management strategies tailored to specific utilization drivers to optimize health care practices and outcomes. In the end, this approach can help identify vulnerable patients and triage them to more patient-centered interventions such as CBT (Lackner et al., 2008) earlier in the course of their illness with the goal of improving the quality and efficiency of care, quality of life, and satisfaction for patients and providers.
4. Coda
Thirty-one years has passed since I (JML) received my doctorate from Rutgers. I had the fortune of working with Terry both at the Alcohol Research Lab on research parsing out the pharmacological vs expectancy effects of alcohol and the Eating Disorders Clinic running clinical trials on CBT for bulimia. While bulimia and alcoholism are outside my clinical or research focus, the lessons I learned under the supervision of Terry Wilson have left a strong and enduring imprint on me, one that shapes my work research on brain-gut interactions underlying functional GI disorders. The conceptual and practical value of theory, methodological rigor, statistical sophistication, and clarity of communication were lessons that I took from my years under Terry. As editor of BRAT, supervisor, and an independent researcher, Terry sees the value of a good study on the basis of its ability to raise as many questions as it answers. If the study “shook these up” in the process, it had even more value and impact potential. It is in this spirit that this study was conducted.
Acknowledgments
We would like to thank members of the IBSOS Research Group (Rebecca Firth, Darren Brenner, Leonard Katz, Susan Krasner, Christopher Radziwon, Michael Sitrin, Jim Jaccard, Chang-Xing Ma, Ann Marie Carosella) for their assistance on various aspects of the research reported in this manuscript.
This work was supported by a grant from the National Institutes of Health, USA (DK77738) to the senior author.
Abbreviations
- IBS
Irritable Bowel Syndrome
- GI
Gastrointestinal
- BFF-S
Block Fruit Fiber Screener
- IBS-LOC
IBS-Specific Locus of Control
- STAI
State-Trait Anxiety Inventory
- ASI
Anxiety Sensitivity Inventory
- PSS
Perceived Stress Scale
- ISEL
Interpersonal Support Evaluation List
- IBS-SSS
Irritable Bowel Syndrome Symptom Severity Scale
- PCS
Physical Component Summary
- SF-12
Short Form-12
- BSI
Brief Symptom Inventory
- GSI
Global Severity Index
- IBSOS EF
IBS Outcome Study Economic Form
- STAI-T
State-Trait Anxiety Inventory Trait anxiety
- IRRs
Incident rate ratios
- M
Mean
- SD
Standard Deviation
- ANOVA
Analysis of variance
Footnotes
Declaration of funding interests
The authors report no competing interests.
References
- Agras WS, Walsh T, Fairburn CG, Wilson GT, Kraemer HC. A multicenter comparison of cognitive-behavioral therapy and interpersonal psychotherapy for bulimia nervosa. Arch. Gen. Psychiatry. 2000;57:459–466. doi: 10.1001/archpsyc.57.5.459. [DOI] [PubMed] [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- Block G, Gillespie C, Rosenbaum EH, Jenson C. A rapid food screener to assess fat and fruit and vegetable intake. American Journal of Preventive Medicine. 2000;18:284–288. doi: 10.1016/s0749-3797(00)00119-7. [DOI] [PubMed] [Google Scholar]
- Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L. A data-based approach to diet questionnaire design and testing. American Journal of Epidemiology. 1986;124:453–469. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- de Boer AG, Wijker W, de Haes HC. Predictors of health care utilization in the chronically ill: A review of the literature. Health Policy. 1997;42:101–115. doi: 10.1016/s0168-8510(97)00062-6. [DOI] [PubMed] [Google Scholar]
- Brandt LJ, Chey WD, Foxx-Orenstein AE, Schiller LR, Schoenfeld PS, Spiegel BM, et al. An evidence-based position statement on the management of irritable bowel syndrome. American Journal of Gastroenterology. 2009;104(Suppl 1):S1–S35. doi: 10.1038/ajg.2008.122. [DOI] [PubMed] [Google Scholar]
- Bray JW, Zarkin GA, Miller WR, Mitra D, Kivlahan DR, Martin DJ, et al. Measuring economic outcomes of alcohol treatment using the Economic Form 90. Journal of Studies on Alcohol and Drugs. 2007;68(2):248–255. doi: 10.15288/jsad.2007.68.248. [DOI] [PubMed] [Google Scholar]
- Burgard SA, Hawkins JM. Race/Ethnicity, educational attainment, and foregone health care in the United States in the 2007–2009 recession. American Journal of Public Health. 2014;104:12. doi: 10.2105/AJPH.2013.301512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang L. Review article: Epidemiology and quality of life in functional gastrointestinal disorders. Alimentary Pharmacology & Therapeutics. 2004;20(Suppl 7):31–39. doi: 10.1111/j.1365-2036.2004.02183.x. [DOI] [PubMed] [Google Scholar]
- Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapam S, Oskamp S, editors. The social psychology of health: Claremont Symposium on applied social psychology. Newbury Park, CA: Sage; 1988. [Google Scholar]
- Collins CE, Patterson A, Fitzgerald D. Higher diet quality does not predict lower medicare costs but does predict number of claims in mid-aged australian women. Nutrients. 2011;3(1) doi: 10.3390/nu3010040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR. Brief symptom inventory (BSI) 18. Minneapolis: National Computer System; 2000. [Google Scholar]
- DeRubeis RJ, Hollon SD, Amsterdam JD, Shelton RC, Young PR, Salomon RM, et al. Cognitive therapy vs medications in the treatment of moderate to severe depression. Archives of General Psychiatry. 2005;62:409–416. doi: 10.1001/archpsyc.62.4.409. [DOI] [PubMed] [Google Scholar]
- Dorn SD, Palsson OS, Thiwan SI, Kanazawa M, Clark WC, van Tilburg, et al. Increased colonic pain sensitivity in irritable bowel syndrome is the result of an increased tendency to report pain rather than increased neurosensory sensitivity. Gut. 2007;56:1202–1209. doi: 10.1136/gut.2006.117390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drossman DA, Corazziari E, Talley NJ, Thompson WG, Whitehead W. Rome III. The functional gastrointestinal disorders: Diagnosis, pathophysiology and treatment: A multinational consensus. 2. McLean, VA: Degnon Associates; 2006. [Google Scholar]
- Fleury M-J, Grenier G, Bamvita J-M, Caron J. Determinants and patterns of service utilization and recourse to professionals for mental health reasons. BMC Health Services Research. 2014;14:161. doi: 10.1186/1472-6963-14-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: A simple method of monitoring irritable bowel syndrome and its progress. Alimentary Pharmacology & Therapeutics. 1997;11:395–402. doi: 10.1046/j.1365-2036.1997.142318000.x. [DOI] [PubMed] [Google Scholar]
- Heiligenstein E, Smith SS. Smoking and mental health problems in treatment-seeking university students. Nicotine & Tobacco Research. 2006;8:519–523. doi: 10.1080/14622200600789718. [DOI] [PubMed] [Google Scholar]
- House JS, Kahn RL. Measures and concepts of social support. In: Cohen S, Syme SL, editors. Social support and health. New York: Academic Press; 1985. pp. 83–108. [Google Scholar]
- Irvine EJ, Whitehead WE, Chey WD, Matsueda K, Shaw M, Talley NJ, et al. Design of treatment trials for functional gastrointestinal disorders. Gastroenterology. 2006;130:1538–1551. doi: 10.1053/j.gastro.2005.11.058. [DOI] [PubMed] [Google Scholar]
- Jensen MP, Keefe FJ, Lefebvre JC, Romano JM, Turner JA. One- and two-item measures of pain beliefs and coping strategies. Pain. 2003;104:453–469. doi: 10.1016/S0304-3959(03)00076-9. [DOI] [PubMed] [Google Scholar]
- Jiménez-Martín S, Labeaga JM, Martínez-Granado M. Latent class versus two-part models in the demand for physician services across the European Union. Health Economics. 2002;11:301–321. doi: 10.1002/hec.672. [DOI] [PubMed] [Google Scholar]
- Kanazawa M, Endo Y, Whitehead WE, Kano M, Hongo M, Fukudo S. Patients and nonconsulters with irritable bowel syndrome reporting a parental history of bowel problems have more impaired psychological distress. Digestive Diseases and Sciences. 2004;49:1046–1053. doi: 10.1023/b:ddas.0000034570.52305.10. [DOI] [PubMed] [Google Scholar]
- Kasper JD, Giovannini TA, Hoffman C. Gaining and losing health insurance: Strengthening the evidence for effects on access to care and health outcomes. Medical Care Research and Review. 2000;57:298–318. doi: 10.1177/107755870005700302. discussion 319-225. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Wilson GT. Criteria for evaluating psychotherapy. Archives of General Psychiatry. 1978;35:407–416. doi: 10.1001/archpsyc.1978.01770280017001. [DOI] [PubMed] [Google Scholar]
- Klatsky AL, Armstrong MA, Friedman GD. Alcohol use and subsequent cerebrovascular disease hospitalizations. Stroke. 1989;20:741–746. doi: 10.1161/01.str.20.6.741. [DOI] [PubMed] [Google Scholar]
- Koloski NA, Talley NJ, Boyce PM. Predictors of health care seeking for irritable bowel syndrome and nonulcer dyspepsia: A critical review of the literature on symptom and psychosocial factors. American Journal of Gastroenterology. 2001;96:1340–1349. doi: 10.1111/j.1572-0241.2001.03789.x. [DOI] [PubMed] [Google Scholar]
- Lackner JM, Jaccard J, Krasner SS, Katz LA, Gudleski GD, Holroyd K. Self-administered cognitive behavior therapy for moderate to severe irritable bowel syndrome: Clinical efficacy, tolerability, feasibility. Clinical Gastroenterology and Hepatology. 2008;6:899–906. doi: 10.1016/j.cgh.2008.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lackner JM, Dunlap L. Economic assessment schedule for health care use of IBS. Buffalo: University at Buffalo School of Medicine; 2009. [Google Scholar]
- Lackner JM, Keefer L, Jaccard J, Firth R, Brenner D, Bratten J, et al. The irritable bowel syndrome outcome study (IBSOS): Rationale and design of a randomized, placebo-controlled trial with 12 month follow up of self- versus clinician-administered CBT for moderate to severe irritable bowel syndrome. Contemporary Clinical Trials. 2012;33:1293–1310. doi: 10.1016/j.cct.2012.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lackner JM, Krasner SS, Quigley B, Gudleski GD, Powell C, Katz L, et al. Cognitive behavior therapy improves severity of IBS Symptoms by modifying patients’ illness beliefs: Results of a randomized clinical trial. Gastroenterology. 2007;132(Suppl 2):A-520. [Google Scholar]
- Lackner JM, Ma CX, Keefer L, Brenner DM, Gudleski GD, Satchidanand N, et al. Type, rather than number, of mental and physical comorbidities increases the severity of symptoms in patients with irritable bowel syndrome. Clinical Gastroenterology and Hepatology. 2013 doi: 10.1016/j.cgh.2013.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longnecker MP, MacMahon B. Associations between alcoholic beverage consumption and hospitalization, 1983 national health interview survey. American Journal of Public Health. 1988;78:153–156. doi: 10.2105/ajph.78.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480–1491. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- Longstreth GF, Wilson A, Knight K, Wong J, Chiou CF, Barghout V, et al. Irritable bowel syndrome, health care use, and costs: A U.S. Managed care perspective. American Journal of Gastroenterology. 2003;98:600–607. doi: 10.1111/j.1572-0241.2003.07296.x. [DOI] [PubMed] [Google Scholar]
- Lo YT, Wahlqvist ML, Chang YH, Kao S, Lee MS. Dietary diversity predicts type of medical expenditure in elders. American Journal of Managed Care. 2013;19:e415–e423. [PubMed] [Google Scholar]
- Lydeard S, Jones R. Factors affecting the decision to consult with dyspepsia: Comparison of consulters and non-consulters. The Journal of the Royal College of General Practitioners. 1989;39:495–498. [PMC free article] [PubMed] [Google Scholar]
- Marteau TM, Ogilvie D, Roland M, Suhrcke M, Kelly MP. Judging nudging: Can nudging improve population health? 2011;342 doi: 10.1136/bmj.d228. [DOI] [PubMed] [Google Scholar]
- Mayer EA. Clinical practice. Irritable bowel syndrome. The New England Journal of Medicine. 2008;358:1692–1699. doi: 10.1056/NEJMcp0801447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Del Boca FK. Measurement of drinking behavior using the Form 90 family of instruments. Journal of Studies on Alcohol Supplement. 1994;12:112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Mosley TH, Jr, Payne TJ, Plaud JJ, Johnson CA, Wittrock DA, Seville JL, et al. Psychometric properties of the weekly stress inventory (WSI): Extension to a patient sample with coronary heart disease. Journal of Behavioral Medicine. 1996;19:273–287. doi: 10.1007/BF01857769. [DOI] [PubMed] [Google Scholar]
- Pahl K, Brook JS, Zhang C, Brook DW. Psychosocial predictors of mental health service utilization among women during their mid-sixties. The Journal of Behavioral Health Services and Research. 2014;31:31. doi: 10.1007/s11414-014-9414-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson RA, Reiss S. Anxiety sensitivity index: Revised test manual. Worthington, OH: IDS Publishing Corporation; 1993. [Google Scholar]
- Pohlmeier W, Ulrich V. An econometric-model of the 2-part decisionmaking process in the demand for health-care. Journal of Human Resources. 1995;30:339–361. [Google Scholar]
- Rice C, Duncan DF. Alcohol use and reported physician visits in older adults. Preventive Medicine. 1995;24:229–234. doi: 10.1006/pmed.1995.1038. [DOI] [PubMed] [Google Scholar]
- Ringstrom G, Abrahamsson H, Strid H, Simren M. Why do subjects with irritable bowel syndrome seek health care for their symptoms? Scandinavian Journal of Gastroenterology. 2007;42:1194–1203. doi: 10.1080/00365520701320455. [DOI] [PubMed] [Google Scholar]
- Sandler RS, Everhart JE, Donowitz M, Adams E, Cronin K, Goodman C, et al. The burden of selected digestive diseases in the United States. Gastroenterology. 2002;122:1500–1511. doi: 10.1053/gast.2002.32978. [DOI] [PubMed] [Google Scholar]
- Scheurich A, Müller MJ, Anghelescu I, Lörch B, Dreher M, Hautzinger M, et al. Reliability and validity of the Form 90 interview. European Addiction Research. 2005;11(1):50–56. doi: 10.1159/000081417. [DOI] [PubMed] [Google Scholar]
- Sialubanje C, Massar K, Hamer DH, Ruiter RA. Personal and environmental predictors of the intention to use maternal healthcare services in Kalomo, Zambia. Health Education Research. 2014;29:1028–1040. doi: 10.1093/her/cyu057. [DOI] [PubMed] [Google Scholar]
- Spiegel BM. Burden of illness in irritable bowel syndrome: Looking beyond the patient. Clinical Gastroenterology and Hepatology. 2013;11:156–157. doi: 10.1016/j.cgh.2012.10.023. [DOI] [PubMed] [Google Scholar]
- Spielberger CD. State-trait personality inventory (STPI) Redwood City: Mind Garden; 1995. [Google Scholar]
- Spiller R, Aziz Q, Creed F, Emmanuel A, Houghton L, Hungin P, et al. Clinical Services Committee of The British Society of G. Guidelines on the irritable bowel syndrome: Mechanisms and practical management. Gut. 2007;56:1770–1798. doi: 10.1136/gut.2007.119446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talley NJ, Boyce PM, Jones M. Predictors of health care seeking for irritable bowel syndrome: A population based study. Gut. 1997;41:394–398. doi: 10.1136/gut.41.3.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talley NJ, Gabriel SE, Harmsen WS, Zinsmeister AR, Evans RW. Medical costs in community subjects with irritable bowel syndrome. Gastroenterology. 1995;109:1736–1741. doi: 10.1016/0016-5085(95)90738-6. [DOI] [PubMed] [Google Scholar]
- Talley NJ, Zinsmeister AR, Melton LJ. Irritable bowel syndrome in a community: Symptom subgroups, risk factors, and health care utilization. American Journal of Epidemiology. 1995;142:76–83. doi: 10.1093/oxfordjournals.aje.a117548. [DOI] [PubMed] [Google Scholar]
- Tonigan JS, Miller WR, Brown JM. The reliability of Form 90: An instrument for assessing alcohol treatment outcome. Journal of Studies on Alcohol. 1997;58:358–364. doi: 10.15288/jsa.1997.58.358. [DOI] [PubMed] [Google Scholar]
- Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Williams RE, Black CL, Kim HY, Andrews EB, Mangel AW, Buda JJ, et al. Determinants of healthcare-seeking behaviour among subjects with irritable bowel syndrome. Alimentary Pharmacology & Therapeutics. 2006;23:1667–1675. doi: 10.1111/j.1365-2036.2006.02928.x. [DOI] [PubMed] [Google Scholar]