Abstract
Spontaneous pneumomediastinum (SPM) is an uncommon finding in young adults presenting usually without any comorbidities or an underlying pathology. It is most commonly due to alveolar rupture in the setting of an inciting event such an underlying asthma, barotrauma, valsalva maneuver, or esophageal rupture. Individuals can have varying presentations, from chest pain, dyspnea and dysphagia, to anxiety, weakness, or facial and neck swelling. The majority of patients have subcutaneous emphysema on examination and can have abnormal laboratory findings such as an elevated C-reactive proteins and leukocytosis. Diagnostic modalities used include chest x-ray, CT scan, ultrasound and barium swallow or esophagram. Majority of individuals and treated conservatively with rest, analgesia and oxygen administration. The prognosis of SPM is usually good with resolution within several days in most cases and the recurrence rate is very low. We report the case of a 22-year-old female presented with SPM diagnosed by chest x-ray and chest CT scan who was treated conservatively with subsequent spontaneous resolution.
1. Introduction
Spontaneous pneumomediastinum (SPM) is a rare disease process with no clear etiology and is defined as non-traumatic presence of free air in the mediastinum in a patient with no known underlying disease. SPM usually occurs after coughing, vomiting, intense exertion, and Valsalva maneuvers, which result in a sudden increase in the intra-alveolar pressure. SPM is usually a self-limiting pathology with an age range of 15–41 years and a mean of 25 years in one study [1]. The most common symptoms of SPM are chest pain, neck pain, shortness of breath, difficulty in swallowing, weakness and swelling of the face and neck. The pathophysiology of SPM involves increased pressure gradient between the intra-alveolar and interstitial spaces, which enhances air leakage from small alveolar openings and ruptured alveoli into the perivascular adventitia yielding interstitial emphysema [6]. Diagnostic modalities includes chest radiograph, CT scan, ultrasound and contrast esophagography, with chest CT scan being the gold standard of diagnosis. Most individuals diagnosed with uncomplicated SPM should be treated conservatively with spontaneous resolution the most likely outcome.
2. Case presentation
A 22-year-old female with a past medical history of anxiety and migraine headache presented to the emergency department complaining of pain and tightness in her throat and chest, odynophagia, followed by progressive swelling of her upper chest, neck and face which began 2 hours prior to presentation. She denied any lip or tongue swelling, difficulties salivating, coughing or retching prior to presentation. She had no known history of asthma, bronchitis, or peptic ulcer disease. Her family history was non-contributory. She smokes half pack of cigarettes daily and denied alcohol or recreational drug use.
On examination, she was not in acute distress, vital signs revealed a blood pressure of 115/67 mmHg, pulse rate of 69/min, respiratory rate of 20/min and was saturating 100% on room air. She was 65 inches in height, with a BMI of 22. Head and neck examination revealed mild facial swelling with crepitus. There were no obvious oropharyngeal abnormalities and her trachea was midline. Examination of the chest also revealed diffuse crepitus consistent with subcutaneous emphysema. The remainder of her physical examination was unremarkable.
She had a white cell count of 18, 800/mm3, a hematocrit of 39% and a platelet count of 207,000/mm3. Her serum electrolytes, renal and liver function tests were all normal. Chest and neck radiograph revealed subcutaneous emphysema consistent with pneumomediastinum (Fig. 1).
Fig. 1.

Chest X-ray showing pneumomediastinum. The lungs are clear and there is no pneumothorax.
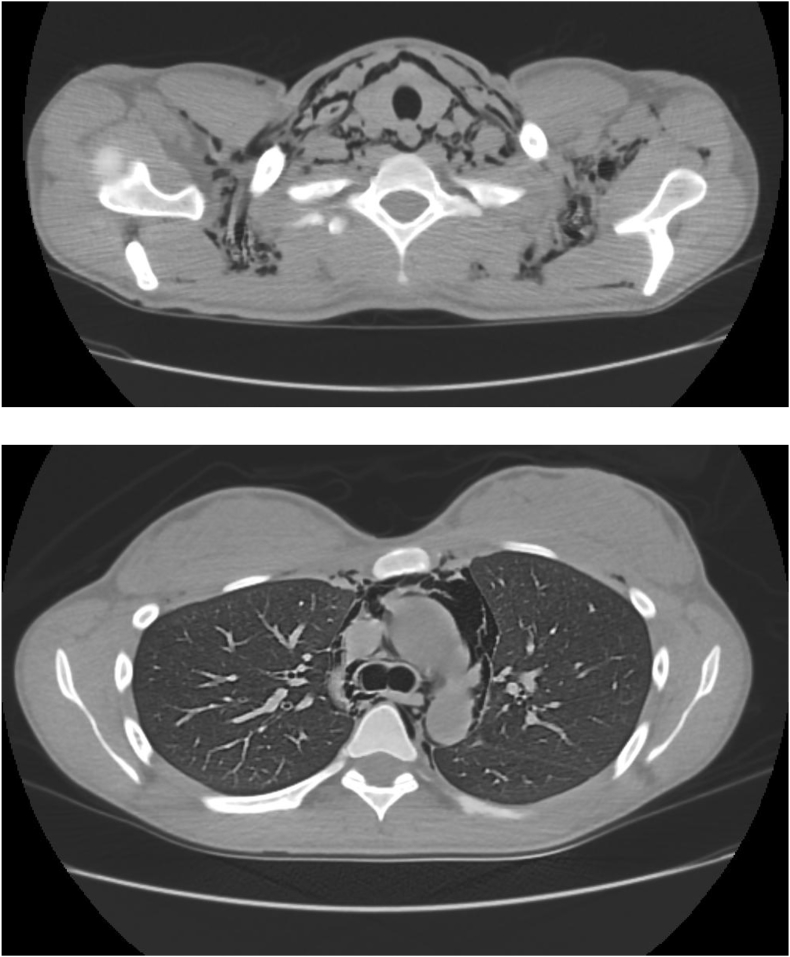
Computerized tomography (CT) scan of the neck and chest revealed extensive pneumomediastinum and soft tissue emphysema in the neck and upper chest with some extension into the retroperitoneum (Fig. 2A and B).
Fig. 2.
A, B: CT scan of Neck and Chest showing soft tissue emphysema in the neck and extensive pneumomediastinum.
The patient was admitted initially to the intensive care unit and was evaluated by cardiothoracic surgery and ENT services. She had a gastrograffin swallow followed by a barium esophagram done and both were normal. She was managed conservatively with resolution of her pneumomediastinum and was subsequently discharged in good health.
3. Discussion
Spontaneous pneumomediastinum (SPM) is a rare entity, which is frequently observed in young adult males with a tall thin body habits and usually occurs without any underlying etiology or pathology. The disease is usually a self-limiting process with an age range of 15–41 years and a mean of 25 years in one study [1]. SPM is defined as the non-traumatic presence of free air in the mediastinum in a patient with no known underlying disease [2]. The exact incidence of SPM is unknown and difficult to evaluate; however it has been reported to be approximately 1 in 30,000 emergency department visits [3]. The exact etiology of this process is unknown however there are several triggers which can induce SPM. Most common etiology for SPM is alveolar rupture, which occurs in the setting of an inciting event or trigger. The most common inciting event leading to alveolar rupture is an asthma exacerbation, which accounts for 20 to 30% of cases [4]. Triggers include asthma exacerbation, barotrauma, intrathoracic pressure increase, the valsalva maneuver, and withdrawal symptoms of illicit drugs [5]. Other causes of pneumomediastinum include coughing, mechanical ventilation, pneumonitis, emphysema, lung fibrosis, acute respiratory distress syndrome, heroin, marijuana, cocaine use, gas producing infections in the head and neck, tracheobronchial or esophageal rupture and facial fractures that lead to disruption of maxillary sinus walls [6], [7].
The most common symptoms of pneumomediastinum are chest pain, neck pain, dyspnea, dysphagia, weakness and swelling of the face and neck. One retrospective study which reviewed the clinical literature, revealed the most common symptoms to be retrosternal chest pain (68%), dyspnea (44%) and throat symptoms, such as pain or discomfort [8]. Our patients' main symptoms were chest pain, throat discomfort and swelling of her face and neck. Physical examination findings includes subcutaneous emphysema which occurs when intrathoracic air leaks into the soft tissues, hamman's sign, which is the crepitation detected at the time of the apex beat during cardiac auscultation and pneumothorax [7]. In one retrospective case series, 65% of patients had subcutaneous emphysema, 52% had a hamman's crunch and 11% had a small pneumothorax [1]. Our patient did not have any hamman's sign or pneumothorax but she did have mediastinal, neck and facial crepitus consistent with subcutaneous emphysema. Non-specific laboratory findings such as leukocytosis and elevations in C-reactive protein (CRP) have been reported. In one retrospective study either leukocytosis or increased CRP was seen in 80% of patients [8]. Leukocytosis of 18,800 per mm3 was present in our patient without any evidence of localized or systemic infection.
The pathophysiology of SPM involves increased pressure gradient between the intra-alveolar and interstitial spaces, which enhances air leakage from small alveolar openings and ruptured alveoli into the perivascular adventitia yielding interstitial emphysema [6]. This pressure gradient leads to air dissection along the vascular sheaths toward the hilum [6]. An abrupt increase in mediastinal pressure may result in a pneumothorax, however, because the visceral layers of the deep cervical fascia are contiguous with the mediastinum, air usually decompresses into the neck, preventing physiologic tamponade and pneumothorax [6]. Elevated pressure in the deep cervical fascia then favors dissection along blood vessels to other planes in the neck [6].
Diagnostic evaluation of SPM includes chest radiograph, CT scan, ultrasound and contrast esophagography especially when evaluating for esophageal perforation. Initial evaluation should involve anteroposterior and lateral chest x-ray views. Chest radiograph typically reveals free air tracking along the mediastinum or subcutaneous air in the shoulders or neck [9]. Other radiological signs include the spinnaker sail sign or “angel wing sign,” which is more commonly seen in the pediatric population, due to the dissecting air elevating the thymus; the ring sign, which is due to air surrounding the pulmonary artery or its main branches; and the Naclieros V sign, which is due to a hyperlucent V shape between the descending aorta and the left hemidiaphragm [9], [10], [11]. Chest radiographs have been shown to underestimate the severity of SPM in 10–30% of cases [12].
Posteroanterior chest radiographs typically reveal a radiolucency between the left heart border and the mediastinal pleura, however, approximately 50% of cases will be missed by the posteroanterior chest view [6]. Lateral chest radiographs are more sensitive for identifying pneumomediastinum [6]. CT scan is the next diagnostic tool used which is more sensitive and can detect small pockets of air in the mediastinum or subcutaneous tissues, which may not be visible on chest radiograph. CT scan is considered the gold standard for diagnosis of SPM. In one retrospective study, CXR alone poorly detected approximately 30% of SPM and that chest CT scan was needed to make the diagnosis in these cases [13]. Electrocardiography can also be obtained especially when chest pain is the presenting complaint, to evaluate for cardiac etiologies of chest pain for example pericarditis. There have also been reports using ultrasound as an initial screening tool for the evaluation of SPM. Ultrasound findings include hyperechoic artifacts extending along the aortic arch contour and “comet tails” or vertical gas artifacts in the anterolateral cervical region and have even identified a thin anechoic band identified as air, separating the pericardium from the pleural line [9].
Most individuals diagnosed with uncomplicated SPM should be treated conservatively with rest, oxygen administration and analgesia, with particular avoidance of any maneuvers, which can result in an increase in intrathoracic pressure. Underlying triggers and coexisting pathology such as asthma or pneumothorax should be treated. Once the diagnosis of SPM has been established, patients should be hospitalized for a minimum of 24 hours to avoid any potential complications [2]. The prognosis of SPM is good with resolution within several days and the recurrence rate is very low. Although recurrent cases have been reported, it is very rare, with one retrospective study revealing no recurrence rate in their 2-year follow up [8].
4. Conclusion
Although the incidence of SPM is quite low, one must keep this diagnosis as part of the differentials especially when evaluating a young adult who presents with symptoms such as chest pain and dyspnea. High index of suspicion is key to early diagnosis in order to avoid potential complications.
Source(s) of financial support in the form of grants
None.
Conflicts of interest
None.
References
- 1.Panacek E.A., Singer A.J., Sherman B.W., Prescott A., Rutherford W.F. Spontaneous pneumomediastinum: clinical and natural history. Ann. Emerg. Med. 1992;21:1222–1227. doi: 10.1016/s0196-0644(05)81750-0. [DOI] [PubMed] [Google Scholar]
- 2.Weissberg D., Weissberg D. Spontaneous mediastinal emphysema. Eur. J. Cardiothorac. Surg. 2004;26:885–888. doi: 10.1016/j.ejcts.2004.05.050. [DOI] [PubMed] [Google Scholar]
- 3.Newcomb A.E., Clarke C.P. Spontaneous pneumomediastinum: a benign curiosity or a significant problem? Chest. 2005;128:3298–3302. doi: 10.1378/chest.128.5.3298. [DOI] [PubMed] [Google Scholar]
- 4.Wong K.S., Wu H.M., Lai S.H., Chiu C.Y. Spontaneous pneumomediastinum: analysis of 87 pediatric patients. Pediatr. Emerg. Care. 2013;29:988. doi: 10.1097/PEC.0b013e3182a26a08. [DOI] [PubMed] [Google Scholar]
- 5.Bolvardi E., Pishbin E., Ebrahimi M., Mahmoudi Gharaee A., Bagherian F. Spontaneous pneumomediastinum with a rare presentation. Case Rep. Emerg. Med. 2014;2014:451407. doi: 10.1155/2014/451407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee Y.J., Jin S.W., Jang S.H. A case of spontaneous pneumomediastinum and pneumopericardium in a young adult. Korean J. Intern Med. 2001;16:205–209. doi: 10.3904/kjim.2001.16.3.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tezel C., Varer P., Baysungur V., Okur E., Halezeroglu S. Spontaneous pneumomediastinum: report of two cases. Ulus. Travma Acil Cerrahi Derg. 2011;17(4):368–370. doi: 10.5505/tjtes.2011.22755. [DOI] [PubMed] [Google Scholar]
- 8.Takada K., Matsumoto S., Hiramatsu T., Kojima E., Watanabe H., Sizu M., Okachi S., Ninomiya K. Management of spontaneous pneumomediastinum based on clinical experience of 25 cases. Respir. Med. 2008 Sep;102(9):1329–1334. doi: 10.1016/j.rmed.2008.03.023. [DOI] [PubMed] [Google Scholar]
- 9.Zachariah S., Gharahbaghian L., Perera P., Joshi N. Spontaneous pneumomediastinum on bedside ultrasound: case report and review of the literature. West J. Emerg. Med. 2015;16:321. doi: 10.5811/westjem.2015.1.24514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sahni S., Verma S., Grullon J. Spontaneous pneumomediastinum: time for consensus. N. Am. J. Med. Sci. 2013;5:460–464. doi: 10.4103/1947-2714.117296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Russo A., Del Vecchio C., Zaottini A. Role of emergency thoracic ultrasonography in spontaneous pneumomediastinum. Two case report. G. Chir. 2012;33:285–296. [PubMed] [Google Scholar]
- 12.Okada M., Adachi H., Shibuya Y. Diagnosis and treatment of patients with spontaneous pneumomediastinum. Respir. Investig. 2014;57:36–40. doi: 10.1016/j.resinv.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 13.Kaneki T., Kubo K., Kawashima A. Spontaneous pneumomediastinum in 33 patients: yield of chest computed tomography for the diagnosis of the mild type. Respiration. 2000;67:408–411. doi: 10.1159/000029539. [DOI] [PubMed] [Google Scholar]