Abstract
Growing attention is being paid to obstetrical quality of care as patients are pressing the healthcare system to measure and improve quality. There is also an increasing recognition of persistent racial and ethnic disparities prevalent in obstetrical outcomes. Yet few studies have linked obstetrical quality of care with racial and ethnic disparities. This article reviews definitions of quality of care, health disparities, and health equity as they relate to obstetric care and outcomes, describes current efforts and challenges in obstetric quality measurement, and proposes three steps in an effort to develop, track, and improve quality and reduce disparities in obstetrics.
Keywords: Disparities, equity, quality of care, obstetrics, quality improvement
INTRODUCTION
Four million births occur annually in the United States and childbirth is a leading reason for hospitalization.1 Childbirth is the largest category for hospital admissions for commercial payers and Medicaid programs and the estimated annual hospital costs associated with childbirth and newborns are over $100 billion.2,3 The United States spends more on maternity care than any other country in the world, yet the US maternal mortality and infant mortality rates are among the highest of all industrialized countries.4,5 Hospital quality is associated with obstetric and neonatal outcomes and growing attention is being paid to obstetrical quality and safety as patients and payers are pressing the healthcare system to measure and improve quality of care.
At the same time there is a growing recognition of the intractable racial and ethnic disparities prevalent in obstetrical and perinatal outcomes.6 Persistent racial and ethnic disparities in maternal and infant outcomes exist between white and minority women.7,8 Infant mortality rates are twice and maternal mortality rates are three to four times higher in black versus white women.7,9 Infant and maternal mortality rates are also higher in some Hispanic and other minority groups as compared with white women. In fact, the obstetrics literature has documented racial and ethnic disparities across a range of obstetrical and perinatal outcomes.10 While there is a vast literature base documenting the association of social determinants of health (e.g., poverty, lack of education, poor nutritional status, smoking, and neighborhoods) with adverse maternal and perinatal outcomes,11 for the most part these factors are not modifiable solely by the healthcare system. Hospital quality is one of few modifiable factors that the healthcare system can address, yet few obstetrical studies have linked quality of care with racial and ethnic disparities.
Data suggest that obstetrical quality varies widely across US hospitals.12,13 Complications associated with childbirth occur in up to one quarter of deliveries and rates for these complications vary widely across hospitals.14,15 Studies by the Maternal Fetal Medicine Network investigators have documented variation among the 25 hospitals in their network in postpartum hemorrhage (from 1 to 5 %), peripartum infection (2 to 10%), and severe perineal laceration among forcep deliveries (8 to 48%).15 One in ten term infants experience a neonatal complication such as hypoxia, shock, or birth injury, and investigators have found that these rates vary sevenfold across hospitals.16,17 Obstetrical processes of care such as use of oxytocin, episiotomy and general anesthesia have also been shown to vary widely across hospitals.18 Studies have found tenfold variation in cesarean delivery rates across hospitals.19 In addition, variations in outcomes are related to structural measures of quality, such as personnel training and level of care. For instance, maternal complication rates are associated with obstetricians’ residency programs and provider volume. 12,20
The wide variation in obstetrical outcomes across hospitals, poor overall performance on perinatal indicators, and the persistent racial and ethnic disparities in obstetric and perinatal outcomes require innovative remedies that tackles these challenges together. Equity is one of the six essential domains of quality according to the Institute of Medicine yet little attention in obstetrics has focused on the intersection between quality of care and disparities.21 A growing portfolio of perinatal quality metrics have been endorsed by governmental agencies and professional bodies and the Centers for Medicaid and Medicare Services now requires hospitals to report on a few of these metrics.22 However, whether these metrics measure dimensions of care relevant to racial/ethnic disparities is unknown.
This article reviews the definitions of quality of care, health disparities, and health equity as they relate to obstetric care and outcomes. We describe current efforts and challenges in obstetric quality measurement and then discuss studies documenting racial and ethnic disparities in outcomes and quality authored by us and others. We end by suggesting three strategies that may help to reduce racial and ethnic disparities by focusing on quality of care.
QUALITY OF CARE
Definition
The Institute of Medicine defines healthcare quality as “the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and care consistent with current professional knowledge.”23 In its 2001 report, Crossing the Quality Chasm, the Institute of Medicine called for a redesign of the US health care system and provided a framework for improvement through six dimensions of care.21 The aims were built around the core need for health care to be: safe, effective, patient-centered, timely, efficient, and equitable. To achieve the goal of quality improvement and track progress requires a concerted effort to measure performance. Therefore over the past decade a great deal of effort has gone into developing and using quality measures in an effort to improve quality. Many government agencies and professional bodies have developed quality measures with the goal of improving care, by detecting suboptimal care based on the traditional Donabedian model,24 which assesses structure, process, and outcomes. Structural measures are generally applied to characteristics of the provider of care including hospitals (e.g. bed size), physicians (e.g. board certification), or systems of care (e.g. presence of electronic health records). Process measures focus on delivery of specific interventions and services to improve quality of care such as medications or procedures. Outcome measures provide information on health outcomes such as mortality, morbidity, and patient experience and satisfaction.
A three-part classification of quality problems which has been widely used since its inception in the early 1990’s focuses on overuse, underuse, and misuse.25 Overuse is the provision of health services when their risks outweigh their benefits for the recipient of that care (e.g. doing surgery on a patient who is not going to benefit from the procedure). Underuse is failure to provide a health service when their benefits exceed their risks (e.g. immunizations). Misuse is the failure to effectively deliver a proven benefit so that its full potential benefit is not conveyed to the patient (e.g. antibiotics in the setting of a cold).
HEALTH DISPARITIES AND HEALTH EQUITY
Definition
There is a growing focus on reducing disparities and promoting health equity in health and healthcare, and the field of Obstetrics is no exception. The American Congress of Obstetricians and Gynecologists and other professional societies have prioritized reducing health disparities and published committee opinions and consensus statements.26 However, there has been ambiguity in exactly what a health disparity is.27,28 The National Institutes of Health defined health disparities as differences in the incidence, prevalence, mortality, and burden of disease and other adverse health conditions that exist among specific population groups in the United States.”29 However, disparities imply inequity or an injustice rather than a simple difference.30 The hallmark Institute of Medicine 2003 report on disparities, Unequal Treatment, defined disparities as “racial or ethnic differences in the quality of health-care that are not due to access-related factors or clinical needs, preferences, and appropriateness of intervention.”31
Experts in the field have emphasized the importance of clarity about the concepts of health disparities and health equity and stressed the underlying notion of social justice.28 Many rely on the originally conceived definition of a health disparity by The World Health Organization, “differences in health which are not only unnecessary and avoidable but, in addition, are considered unfair and unjust.”32 A recent government definition, Healthy People 2020 has included the concept of social justice in its definition of a health disparity: “… a particular type of health difference that is closely linked with economic, social, or environmental disadvantage. Health disparities adversely affect groups of people who have systematically experienced greater social or economic obstacles to health based on their racial or ethnic group, religion, socioeconomic-status, gender, age, or mental health; cognitive, sensory, or physical disability; sexual orientation of gender identify, geographic location; or other characteristics historically linked to discrimination or exclusion.”28 It is important to remember that a disparity is not simply a difference. Rather, it is a difference that systematically and negatively impact less advantaged groups.
A simple and helpful definition was given by Dr. Paula Braveman, “Health equity and health disparities are intertwined. Health equity means social justice in health (i.e. no one is denied the possibility to be healthy for belonging to a group that has historically been economically/socially disadvantaged). Health disparities are the metric we use to measure progress toward achieving health equity.”28
QUALITY MEASUREMENT IN OBSTETRICS
Measuring quality of care in obstetrics is complex: it involves assessing care for 2 separate individuals. Improving care requires reducing obstetric interventions that can harm infants and mothers (e.g. delivery) and avoiding suboptimal care such as underutilization of antenatal steroids, which can lead to neonatal complication.17 Imperfect quality measures coupled with wide variation in performance are current challenges in the field.
In recent years, numerous quality indicators have been proposed for measurement of obstetrical care in the United States.33 Patients, insurers, and providers all have a vested interest in the easy availability of obstetrical indicators. Many of the traditional obstetrical indicators are poor markers of obstetrical quality because they happen too infrequently, must be extensively risk-adjusted, and have not been linked to specific processes of care that can be improved upon. Use of risk-adjusted primary cesarean rates have been utilized as a marker of quality but studies have shown that primary cesarean rates that are either below or above predicted can be associated with poor neonatal outcomes, making the use of risk-adjusted primary cesarean rates problematic to assess quality.33 Perineal lacerations have been recommended as a quality indicator as they are easily tracked using coding data. However, their use is not endorsed by ACOG as quality indicators because they are not defined uniformly, are associated with non-modifiable risk factors, and reducing the use of operative vaginal delivery, in an effort to decrease severe perineal lacerations, likely would result in an increased rate of cesarean delivery.34
In addition, to shortcomings with specific quality indicators, another challenge in the field is feasibility. In order to monitor quality across hospitals, data must be available in routine sources to construct valid, reliable and case-mix adjusted indicators. According to the National Quality Forum and experts in the field, quality measures must be evidence-based, important, acceptable (precisely defined, reliable, valid, discriminatory, risk-adjusted if necessary, have consistent evidence linking process to outcomes), feasible, and usable.35
Currently there are a number of recommended obstetrical quality indicators. Table 1 lists some examples. The Agency for Healthcare Research and Quality (AHRQ) has proposed a set of obstetrics-related quality indicators for their inpatient, safety, and prevention indicators.36 The National Quality Forum has endorsed fourteen measures,37 and some of these measures are now being utilized by The Joint Commission as perinatal quality measures.38 Currently the Centers for Medicare and Medicaid Services mandates hospitals to report one of these measures, the elective delivery measure which includes non-medically indicated deliveries associated with medical induction.22 The focus on quality in maternity care extends internationally. Investigators in Europe have used a modified Delphi approach with use of an international multidisciplinary panel to select a list of indicators that reflect the quality of obstetrical care in maternity units.39 All of these efforts have enriched the debate about obstetrical quality considerably and have moved the field of quality measurement forward.
Table 1.
Examples of Current Obstetric Quality Indicators by Quality Problem Addressed
| Measure Endorser | Indicator | Structure/Process /Outcome | Quality Problem Addressed |
|---|---|---|---|
| Joint Commission/NQF | Elective Delivery | Outcome | Overuse |
| Joint Commission/NQF | Cesarean rate for low-risk first births | Outcome | Overuse |
| NQF | Incidence of Episiotomy | Process | Overuse |
| AHRQ | Cesarean Delivery Rate | Outcome | Overuse |
| AHRQ | Primary Cesarean Delivery Rate |
Outcome | Overuse |
| AHRQ | Obstetric trauma – Vaginal with Instrument | Outcome | Overuse |
| AHRQ | Obstetric trauma – Vaginal without Instrument | Outcome | Overuse |
| AHRQ | Obstetric trauma – Cesarean delivery | Outcome | Overuse |
| NQF | Prophylactic Antibiotics at cesarean births | Process | Underuse |
| NQF | Appropriate DVT Prophylaxis in Women Undergoing Cesarean Delivery |
Process | Underuse |
| NQF | Intrapartum Antibiotic Prophylaxis for Group B Streptococcus |
Process | Underuse |
| NQF | Infants under 1500 g delivered at appropriate site | Process/Structure | Underuse |
| Joint Commission/NQF | Antenatal Steroids | Process | Underuse |
| Joint Commission/NQF | Exclusive Breast Milk Feeding | Outcome | Underuse |
While some strides have been made in maternity quality improvement, it is unclear whether the current portfolio of obstetric quality indicators is comprehensive enough to drive major improvement in the field. Our recent work has focused on assessing whether obstetric quality indicators are associated with maternal and neonatal morbidity.17 We examined whether hospital performance on two Joint Commission perinatal quality measures, elective (non-medically indicated) deliveries at greater or equal to 37 weeks and less than 39 weeks of gestation and cesarean delivery performed in low-risk mothers were associated with hospital performance on severe maternal and term neonatal morbidity. We found wide variation among hospital for elective deliveries performed before 39 weeks and for cesarean deliveries performed in low risk mothers. Severe maternal morbidity and neonatal morbidity at term rates varied four to five fold and seven-fold respectively. However there were no correlations between performance on the hospital quality indicators and hospital maternal and neonatal morbidity rates. We concluded that quality indicators may not be sufficiently comprehensive for guiding quality improvement in obstetric care.17 Others have also argued that the current repertoire of quality indicators are not comprehensive.16
DISPARITIES, OUTCOMES, AND QUALITY
Disparities in Obstetrical and Perinatal Outcomes
Half of all US births are to racial/ethnic minority women,40–42 and racial/ethnic minorities suffer a disproportionate number of maternal deaths as well as other adverse obstetric and perinatal outcomes. African American women are three to four times more likely to die from pregnancy-related causes than white women. This represents the largest disparity among all the conventional population perinatal health measures.7 Maternal mortality is also elevated among Native Americans/Native Alaskans, Asians/Pacific Islanders, and for certain subgroups of Latino women including Puerto Ricans.43–45 Maternal mortality ratios have increased over the last three decades,46,47 despite advances in diagnosis and acute critical care.48 In New York City, the most recent data demonstrates that black or African American women are twelve times more likely than whites to suffer a pregnancy-related death.49 The increase in the black-white maternal mortality disparity was attributed to a 45% decline in maternal mortality among white women in New York City.49
A number of pregnancy complications and comorbidities associated with maternal death are more common among minorities than whites. Potentially fatal complications of pregnancy include hemorrhage, hypertensive disorders of pregnancy, and cardiomyopathy and black women suffer greater mortality from all of them.50 A leading cause of death in Hispanic women following pregnancy in one study was hypertensive disease placing them at a threefold increased risk of death due to this complication.43 Minority women have been found to have both higher prevalence and higher case fatality rates for these disorders and for more common problems such as diabetes. Interestingly a national study published in 2007 that investigated pregnancy-related mortality among black versus white women found that black women did not have significantly higher prevalence of five specific pregnancy complications but for all five conditions black women had a case-fatality rate 2.4 to 3.3 times higher than that of white women.51
Reviews of racial/ethnic disparities in outcomes and care have documented disparities across a number of other maternal and perinatal outcomes.10 Black and Hispanic women have higher rates of severe maternal morbidity as well diabetes, and obesity. Asian and Hispanic women are at greater risk of developing gestational diabetes. Disparities also exist in the prevalence and severity of a number of other maternal complications including HIV and asthma.10
The disparities in adverse perinatal outcomes are well documented for minority versus white women. Part of the reason that the US does so poorly overall and compared with other countries with respect to perinatal outcomes is the persistent disparities in outcomes between white and minority women. In 2013, the infant mortality rate was much higher for blacks (11.11 deaths per 1000 live births), American Indians or Alaska Natives (7.61 deaths per 1000 live births), and Puerto Ricans (5.93 deaths per 1000 live births) versus whites (5.06 deaths per 1000 live births).9 Preterm birth is more common among black and Puerto Rican women than white women (16.3%, 13.0%, vs. 10.2% of births respectively).9 It has been estimated that disparities in preterm births are responsible for a major portion of the black-white and Puerto-Rican white disparities in infant mortality rates.9 Racial/ethnic disparities exist in the prevalence of preterm birth, fetal growth restriction, fetal demise, and congenital anomalies.10
Disparities and Quality
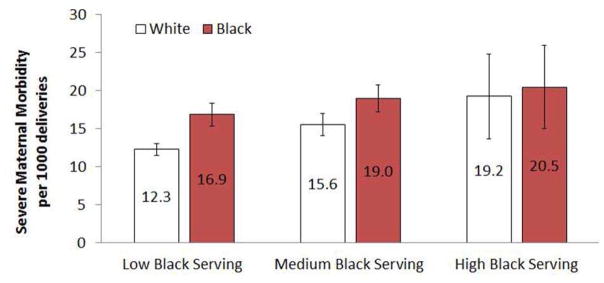
Significant racial/ethnic disparities in obstetric and perinatal outcomes have been evident for decades. Yet, little research has investigated the association between obstetrical quality and racial/ethnic disparities in these outcomes. Studies from other areas in medicine and more recently in obstetrics suggest that minorities receive care in different and lower quality hospitals than whites.52–54 Using data from the Nationwide Inpatient Sample, we found that blacks deliver in a concentrated set of hospitals and these hospitals have higher risk-adjusted severe maternal morbidity rates for both white and black deliveries.54 We ranked hospitals by their proportion of black deliveries into high black-serving (top 5%), medium black-serving (5% to 25% range), and low black-serving hospitals and analyzed the risks of severe maternal morbidity for black and white women by hospital black-serving status after adjusting adjusted for patient characteristics, comorbidities, hospital characteristics, and within-hospital clustering. Severe maternal morbidity occurred more frequently among black than white women (25.8 vs 11.8 per 1000 deliveries, respectively; p < .001) and after adjustment this differential declined but remained elevated (18.8 vs 13.3 per 1000 deliveries, respectively; p < .001). Women who delivered in high and medium black-serving hospitals had elevated rates of severe maternal morbidity rates compared with those in low black-serving hospitals in adjusted analyses (Figure 1).54
Figure 1.
Risk –adjusted severe maternal morbidity rates for black and white deliveries by site of care.
From Howell EA, Egorova N, Balbierz A, et al. Black-white differences in severe maternal morbidity and site of care. Am J Obstet Gynecol. 2016 Jan;214(1):122.e5; with permission.
In another study focused on New York City, after adjustment for patient case mix, we found seven-fold variation in severe maternal morbidity rates and white deliveries were more likely to be delivered in the low-morbidity hospitals: 65% of white versus 23% of black deliveries occurred in hospitals in the lowest tertile for morbidity.55 We estimated that black-white differences in delivery location may contribute as much as 47.7% of the racial disparity in severe maternal morbidity rates in New York City.55 In pediatrics, research by our team and others have also found that black very low-birthweight babies are more likely to be delivered in higher risk-adjusted very low birthweight neonatal mortality hospitals,56,57 and studies in other areas of medicine have demonstrated similar findings.53 Studies of acute myocardial infarction treatment have shown that black patients tend to receive care in hospitals with higher mortality rates and lower rates of effective evidence-based medical treatments compared with white patients.52 Studies have demonstrated that blacks and whites receive care from different providers and the physicians treating black patients are less likely to be board certified and may have less access to important clinical resources than physicians treating white patients.58
Others have also found differences in delivery-related indicators by hospital type and patients’ race and ethnicity.59 Investigators, using seven state inpatient databases, investigated 15 delivery-related indicators, (e.g. obstetric trauma, would complications, complicated vaginal delivery, hemorrhage) among white-serving, Hispanic-serving, and black-serving hospitals.59 They found differences in delivery-related indicators by hospital type and overall lower performance of black-serving hospitals compared to white- and Hispanic-serving hospitals. The authors concluded that obstetrical quality measures are needed to track racial/ethnic disparities at the facility and populations levels.59
Disparities and Quality Indicators
Few obstetrical quality measures have been utilized to track and reduce racial/ethnic disparities in obstetrics. We examined national trends and black-white differences in AHRQ obstetrics-related patient safety, inpatient quality indicators and inpatient neonatal and maternal mortality using national data.60 We included three Patient Safety Indicators: obstetrical trauma (3rd or 4th degree laceration) with instrument, obstetrical trauma without instrument, and birth trauma to neonate and four Inpatient Quality Indicators: c-section rate, primary c-section rate, uncomplicated vaginal birth after c-section (VBAC), and all VBACs. We found that all three patient safety indicators decreased over the 10-year study period and improvements occurred for both blacks and whites. For both blacks and whites, c-section rates increased by 60 to 65% and VBAC’s decreased by 70 to 75% over the study period. However, despite improvements for blacks and whites in some of these quality measures during the study period, the black-white maternal mortality gap widened and the neonatal mortality gap persisted. We concluded that AHRQ quality measures related to procedures do not contribute to our understanding of persistent racial/ethnic disparities in maternal or neonatal inpatient mortality.60
Although the Center for Disease Control tracks a number of important population health measures by race and ethnicity (e.g. maternal mortality, severe maternal morbidity, preterm birth, infant mortality, etc), few in the field of obstetrics track quality measures by race and ethnicity and establish targeted quality improvement efforts to reduce disparities.
DISCUSSION – NEXT STEPS
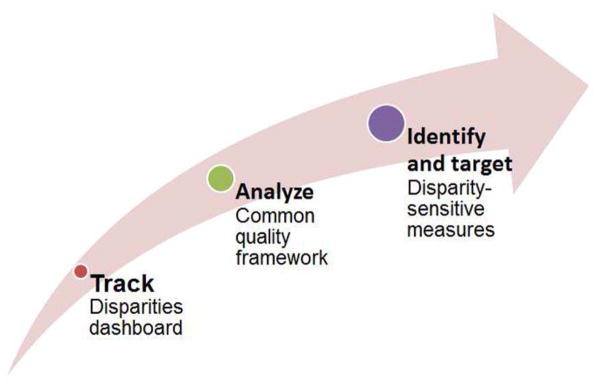
There is a need to develop, track, and improve upon quality measures that are sensitive to disparities in obstetrics and there are three major steps we suggest to move forward (Figure 2). First, The Joint Commission and others have recommended stratifying quality information by race and ethnicity, as well as other sociodemographics, in an effort to track and improve quality for all segments of the population.61 Disparities dashboards have been utilized in some hospitals across the nation to stratify quality metrics by race and ethnicity. The first step in this process is to ensure that hospitals and clinicians collect self-identified race and ethnicity data from their patients.61 Proper training of staff is required and patient education is needed to explain why this information is important. Next, obstetric quality measures should be stratified by race and ethnicity and reviewed by leadership and staff. Quality gaps should be identified and targeted interventions should be introduced to reduce disparities.61 Progress should be monitored.
Figure 2.
Three strategies to reduce disparities by focusing on quality of care.
Second, a great deal of research and progress can be made by using the common quality of care framework of overuse, underuse, and misuse in the setting of racial and ethnic disparities in obstetrics to better understand where we go from here.25 Two of the current Joint Commission perinatal indicators, elective delivery before 39 weeks, and low-risk cesarean, are both primarily overuse measures.17,38 Overutilization of both of these measures may be associated with poor outcomes for babies and moms but our recent data indicated that neither is correlated with severe maternal morbidity or neonatal morbidity at term.17 Data demonstrate that racial and ethnic disparities in severe maternal morbidity and neonatal morbidity at term exist.17 Clearly, additional quality measures are needed that are patient-centered and correlated with important obstetric outcomes, such as severe maternal morbidity and neonatal morbidity. Further, data from other areas of medicine, suggest that overuse of procedures may be more likely to occur in whites than non-whites.62 The extent to which overuse is a quality problem in obstetrics has been studied in one area, cesarean delivery. Several studies have documented higher risks of cesarean delivery among nonwhite women as compared with white women even after adjusting for patient factors.63 However, the extent to which overuse contributes to disparities in obstetric outcomes has not been fully investigated. In contrast, the field of disparities is full of examples of underuse, underutilization of procedures and treatments, for minorities.31 This has also been shown in the setting of obstetrics.10
Third, an expanded set of quality measures are needed in the field. The National Quality Forum in 2008 developed criteria for “disparities sensitive” measures.64 The guiding principles were:
How prevalent was the condition in the disparity population?
What is the impact of the condition for the health of the disparity population?
How strong is the evidence linking improvement in the measure to improved outcomes for any group, but particularly for members of disparity populations?
How large is the disparity gap in quality?
Is the measure actionable? 64
These guiding principles should be used to develop a robust set of quality measures that can help us track and reduce disparities. Examples may be the use of antibiotics in the setting of preterm labor or the use of progesterone in specific high risk groups for the prevention of preterm birth.
Nearly half of all births are to minority mothers and persistent racial and ethnic disparities in obstetric and perinatal outcomes exist. Efforts to reduce racial and ethnic disparities in maternal health are needed. While much of the focus on reducing racial and ethnic disparities in obstetrics examines social determinants of health, there is ample evidence that differences in quality of care contribute to racial and ethnic disparities in obstetric and perinatal outcomes. Quality of care is one of few modifiable factors that the healthcare system can address. We propose three steps in an effort to develop, track, and improve quality and reduce disparities in obstetrics. The use of disparities dashboards to monitor and intervene on racial/ethnic disparities in commonly utilized quality metrics, the assessment of quality problems related to disparities using a common quality framework, and the development of disparities-sensitive metrics in the field of obstetrics can help us to better understand current quality gaps in the care we provide for our patients.
KEY POINTS.
Quality of care in obstetrics varies widely and racial and ethnic disparities in obstetric and perinatal outcomes persist.
Growing evidence suggests that quality of care contributes to racial and ethnic disparities in obstetrical and perinatal outcomes.
Quality measures should be utilized to track and reduce racial/ethnic disparities in obstetrics.
Acknowledgments
Supported by the National Institute on Minority Health and Health Disparities (R01MD007651) and by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health (R01HD078565). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
disclosure statement
The Authors have nothing to disclose
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.DeFrances CJ, Cullen KA, Kozak LJ. National Hospital Discharge Survey: 2005 annual summary with detailed diagnosis and procedure data. Vital Health Stat. 2007 Dec;13(165):1–209. [PubMed] [Google Scholar]
- 2.Andrews RM. The national hospital bill: the most expensive conditions by payer. 2008 Paper presented at: (HCUP Statistical Brief 59); 2008; Rockville, MD. [Google Scholar]
- 3. [Accessed July 16, 2016];Transforming Maternity Care – United States Maternity Care Facts and Figures. 2012 http://transform.childbirthconnection.org/resources/datacenter/factsandfigures/
- 4.MacDorman MF, Mathews TJ. Behind international rankings of infant mortality: how the United States compares with Europe. Int J Health Serv. 2010;40(4):577–588. doi: 10.2190/HS.40.4.a. [DOI] [PubMed] [Google Scholar]
- 5.Amnesty International. Deadly Delivery: The Maternal Health Care Crisis in the US. London, UK: Amnesty International; 2010. [Google Scholar]
- 6.Willis E, McManus P, Magallanes N, Johnson S, Majnik A. Conquering racial disparities in perinatal outcomes. Clin Perinatol. 2014 Dec;41(4):847–875. doi: 10.1016/j.clp.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 7.Callaghan WM. Overview of maternal mortality in the United States. Semin Perinatol. 2012 Feb;36(1):2–6. doi: 10.1053/j.semperi.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 8.Mathews TJ, MacDorman MF. Infant Mortality Statistics From the 2006 Period Linked Birth/Infant Death Data Set. Natl Vital Stat Rep. 2010;57(17):1–32. [PubMed] [Google Scholar]
- 9.Matthews TJ, MacDorman MF, Thoma ME. Infant Mortality Statistics From the 2013 Period Linked Birth/Infant Death Data Set. Natl Vital Stat Rep. 2015 Aug 6;64(9):1–30. [PubMed] [Google Scholar]
- 10.Bryant AS, Worjoloh A, Caughey AB, Washington AE. Racial/ethnic disparities in obstetric outcomes and care: prevalence and determinants. Am J Obstet Gynecol. 2010 Apr;202(4):335–343. doi: 10.1016/j.ajog.2009.10.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Institute of Medicine. Preterm births: Causes, consequences and prevention. Washington, D.C: The National Academy of Science; Jul 13, 2006. [Google Scholar]
- 12.Asch DA, Nicholson S, Srinivas S, Herrin J, Epstein AJ. Evaluating obstetrical residency programs using patient outcomes. JAMA. 2009 Sep 23;302(12):1277–1283. doi: 10.1001/jama.2009.1356. [DOI] [PubMed] [Google Scholar]
- 13.Glance LG, Dick AW, Glantz JC, et al. Rates of major obstetrical complications vary almost fivefold among US hospitals. Health Aff (Millwood) 2014 Aug;33(8):1330–1336. doi: 10.1377/hlthaff.2013.1359. [DOI] [PubMed] [Google Scholar]
- 14.Gregory KD, Fridman M, Shah S, Korst LM. Global measures of quality- and patient safety-related childbirth outcomes: should we monitor adverse or ideal rates? Am J Obstet Gynecol. 2009 Jun;200(6):681, e681–687. doi: 10.1016/j.ajog.2009.02.033. [DOI] [PubMed] [Google Scholar]
- 15.Bailit JL, Grobman WA, Rice MM, et al. Risk-adjusted models for adverse obstetric outcomes and variation in risk-adjusted outcomes across hospitals. Am J Obstet Gynecol. 2013 Nov;209(5):446e441–446e430. doi: 10.1016/j.ajog.2013.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Korst LM, Fridman M, Michael CL, et al. Monitoring Childbirth Morbidity Using Hospital Discharge Data: Further Development And Application Of A Composite Measure. Am J Obstet Gynecol. 2014 Mar 10; doi: 10.1016/j.ajog.2014.03.011. [DOI] [PubMed] [Google Scholar]
- 17.Howell EA, Zeitlin J, Hebert PL, Balbierz A, Egorova N. Association between hospital-level obstetric quality indicators and maternal and neonatal morbidity. JAMA. 2014 Oct 15;312(15):1531–1541. doi: 10.1001/jama.2014.13381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grobman WA, Bailit JL, Rice MM, et al. Can differences in obstetric outcomes be explained by differences in the care provided? The MFMU Network APEX Study. Am J Obstet Gynecol. 2014 Mar 11; doi: 10.1016/j.ajog.2014.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kozhimannil KB, Law MR, Virnig BA. Cesarean delivery rates vary tenfold among US hospitals; reducing variation may address quality and cost issues. Health Aff (Millwood) 2013 Mar;32(3):527–535. doi: 10.1377/hlthaff.2012.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Janakiraman V, Lazar J, Joynt KE, Jha AK. Hospital volume, provider volume, and complications after childbirth in U.S. hospitals. Obstet Gynecol. 2011 Sep;118(3):521–527. doi: 10.1097/AOG.0b013e31822a65e4. [DOI] [PubMed] [Google Scholar]
- 21.Institute of Medicine (IOM) Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C: National Academy Press; 2001. Crossing the Quality Chasm. [Google Scholar]
- 22.Center for Medicare and Medicaid Services. [Accessed July 16, 2016];Hospital Compare. http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalCompare.html.
- 23.Lohr K Committee to Design a Strategy for Quality Review and Assurance in Medicare, editor. Medicare: a strategy for quality assurance. Vol. 1. Washington, DC: IOM, National Academy Press; 1990. [Google Scholar]
- 24.Boulkedid R, Alberti C, Sibony O. Quality indicator development and implementation in maternity units. Best Pract Res Clin Obstet Gynaecol. 2013 Aug;27(4):609–619. doi: 10.1016/j.bpobgyn.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 25.Chassin MR. Quality of care. Time to act. JAMA. 1991 Dec 25;266(24):3472–3473. [PubMed] [Google Scholar]
- 26.ACOG Committee Opinion No. 649: Racial and Ethnic Disparities in Obstetrics and Gynecology. Obstet Gynecol. 2015 Dec;126(6):e130–134. doi: 10.1097/AOG.0000000000001213. [DOI] [PubMed] [Google Scholar]
- 27.Dehlendorf C, Bryant AS, Huddleston HG, Jacoby VL, Fujimoto VY. Health disparities: definitions and measurements. Am J Obstet Gynecol. 2010 Mar;202(3):212–213. doi: 10.1016/j.ajog.2009.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Braveman P. What are health disparities and health equity? We need to be clear. Public Health Rep. 2014 Jan-Feb;129(Suppl 2):5–8. doi: 10.1177/00333549141291S203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Braveman PA, Kumanyika S, Fielding J, et al. Health disparities and health equity: the issue is justice. Am J Public Health. 2011 Dec;101(Suppl 1):S149–155. doi: 10.2105/AJPH.2010.300062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hebert PL, Sisk JE, Howell EA. When does a difference become a disparity? Conceptualizing racial and ethnic disparities in health. Health Aff (Millwood) 2008 Mar-Apr;27(2):374–382. doi: 10.1377/hlthaff.27.2.374. [DOI] [PubMed] [Google Scholar]
- 31.Smedley BD, Stith AY, Nelson AR, editors. Care IoM-CoUaERaEDiH, editor. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, D.C: National Academies Press; 2003. [PubMed] [Google Scholar]
- 32.Whitehead M. The concepts and principles of equity and health. Health Promot Int. 1991 Jan 1;6(3):217–228. [Google Scholar]
- 33.Bailit JL. Measuring the quality of inpatient obstetrical care. Obstet Gynecol Surv. 2007 Mar;62(3):207–213. doi: 10.1097/01.ogx.0000256800.21193.ce. [DOI] [PubMed] [Google Scholar]
- 34.ACOG Committee Opinion No. 647: Limitations of Perineal Lacerations as an Obstetric Quality Measure. Obstet Gynecol. 2015 Nov;126(5):e108–111. doi: 10.1097/AOG.0000000000001151. [DOI] [PubMed] [Google Scholar]
- 35.Main EK. New perinatal quality measures from the National Quality Forum, the Joint Commission and the Leapfrog Group. Curr Opin Obstet Gynecol. 2009 Dec;21(6):532–540. doi: 10.1097/GCO.0b013e328332d1b0. [DOI] [PubMed] [Google Scholar]
- 36.Agency for Healthcare Research and Quality. [Accessed July 16, 2016];AHRQ Quality Indicators. http://www.qualityindicators.ahrq.gov/
- 37.National Quality Forum. [Accessed July 16, 2016];NQF Endorses Perinatal Measures. 2012 http://www.qualityforum.org/News_And_Resources/Press_Releases/2012/NQF_Endorses_Perinatal_Measures.aspx.
- 38.The Joint Commission. [Accessed July 16, 2016];Specifications Manual for Joint Commission National Quality Measures (v2016A) 2016 https://manual.jointcommission.org/releases/TJC2016A/
- 39.Boulkedid R, Sibony O, Goffinet F, Fauconnier A, Branger B, Alberti C. Quality indicators for continuous monitoring to improve maternal and infant health in maternity departments: a modified Delphi survey of an international multidisciplinary panel. PLoS One. 2013;8(4):e60663. doi: 10.1371/journal.pone.0060663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2005. Natl Vital Stat Rep. 2007 Dec 5;56(6):1–103. [PubMed] [Google Scholar]
- 41.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Kirmeyer S. Births: final data for 2004. Natl Vital Stat Rep. 2006 Sep 29;55(1):1–101. [PubMed] [Google Scholar]
- 42.Tavernise S. Whites Account for Under Half of Births in U.S. - NYTimes.com. [Accessed May 17, 2012];The New Yorks Times. 2012 http://www.nytimes.com/2012/05/17/us/whites-account-for-under-half-of-births-in-us.html?pagewanted=2&_r=1&ref=race.
- 43.Hopkins FW, MacKay AP, Koonin LM, Berg CJ, Irwin M, Atrash HK. Pregnancy-related mortality in Hispanic women in the United States. Obstet Gynecol. 1999 Nov;94(5 Pt 1):747–752. doi: 10.1016/s0029-7844(99)00393-2. [DOI] [PubMed] [Google Scholar]
- 44.CDC. Pregnancy-related deaths among Hispanic, Asian/Pacific Islander, and American Indian/Alaska Native women--United States, 1991–1997. MMWR Morb Mortal Wkly Rep. 2001 May 11;50(18):361–364. [PubMed] [Google Scholar]
- 45.Gray KE, Wallace ER, Nelson KR, Reed SD, Schiff MA. Population-based study of risk factors for severe maternal morbidity. Paediatr Perinat Epidemiol. 2012 Nov;26(6):506–514. doi: 10.1111/ppe.12011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Berg CJ, Atrash HK, Koonin LM, Tucker M. Pregnancy-related mortality in the United States, 1987–1990. Obstet Gynecol. 1996 Aug;88(2):161–167. doi: 10.1016/0029-7844(96)00135-4. [DOI] [PubMed] [Google Scholar]
- 47.Heron M, Hoyert DL, Murphy SL, Xu J, Kochanek KD, Tejada-Vera B. Deaths: final data for 2006. Natl Vital Stat Rep. 2009 Apr 17;57(14):1–134. [PubMed] [Google Scholar]
- 48.Pahlavan P, Nezhat C. Hemorrhage in obstetrics and gynecology. Curr Opin Obstet Gynecol. 2001 Aug;13(4):419–424. doi: 10.1097/00001703-200108000-00008. [DOI] [PubMed] [Google Scholar]
- 49.New York City Department of Health and Mental Hygiene Bureau of Maternal Health. Pregnancy-Associated Mortality New York City, 2006–2010. New York: 2015. [Google Scholar]
- 50.Harper MA, Espeland MA, Dugan E, Meyer R, Lane K, Williams S. Racial disparity in pregnancy-related mortality following a live birth outcome. Ann Epidemiol. 2004 Apr;14(4):274–279. doi: 10.1016/S1047-2797(03)00128-5. [DOI] [PubMed] [Google Scholar]
- 51.Tucker MJ, Berg CJ, Callaghan WM, Hsia J. The Black–White Disparity in Pregnancy-Related Mortality From 5 Conditions: Differences in Prevalence and Case-Fatality Rates. American Journal of Public Health. 2007 Feb 01;97(2):247–251. doi: 10.2105/AJPH.2005.072975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Barnato AE, Lucas FL, Staiger D, Wennberg DE, Chandra A. Hospital-level racial disparities in acute myocardial infarction treatment and outcomes. Med Care. 2005 Apr;43(4):308–319. doi: 10.1097/01.mlr.0000156848.62086.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cheng EM, Keyhani S, Ofner S, et al. Lower use of carotid artery imaging at minority-serving hospitals. Neurology. 2012 Jul 10;79(2):138–144. doi: 10.1212/WNL.0b013e31825f04c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Howell EA, Egorova N, Balbierz A, Zeitlin J, Hebert PL. Black-white differences in severe maternal morbidity and site of care. Am J Obstet Gynecol. 2016 Jan;214(1):122, e121–127. doi: 10.1016/j.ajog.2015.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Howell EA, Egorova NN, Balbierz A, Zeitlin J, Hebert PL. Site of delivery contribution to black-white severe maternal morbidity disparity. Am J Obstet Gynecol. 2016 May 12; doi: 10.1016/j.ajog.2016.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Howell EA, Hebert P, Chatterjee S, Kleinman LC, Chassin MR. Black/white differences in very low birth weight neonatal mortality rates among New York City hospitals. Pediatrics. 2008 Mar;121(3):e407–415. doi: 10.1542/peds.2007-0910. [DOI] [PubMed] [Google Scholar]
- 57.Morales LS, Staiger D, Horbar JD, et al. Mortality among very low-birthweight infants in hospitals serving minority populations. Am J Public Health. 2005 Dec;95(12):2206–2212. doi: 10.2105/AJPH.2004.046730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004 Aug 5;351(6):575–584. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- 59.Creanga AA, Bateman BT, Mhyre JM, Kuklina E, Shilkrut A, Callaghan WM. Performance of racial and ethnic minority-serving hospitals on delivery-related indicators. Am J Obstet Gynecol. 2014 Jun 5; doi: 10.1016/j.ajog.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 60.Howell EA, Zeitlin J, Hebert P, Balbierz A, Egorova N. Paradoxical trends and racial differences in obstetric quality and neonatal and maternal mortality. Obstet Gynecol. 2013 Jun;121(6):1201–1208. doi: 10.1097/AOG.0b013e3182932238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ramos R, Davis JL, Ross T, Grant CG, Green BL. Measuring health disparities and health inequities: do you have REGAL data? Qual Manag Health Care. 2012 Jul-Sep;21(3):176–187. doi: 10.1097/QMH.0b013e31825e8889. [DOI] [PubMed] [Google Scholar]
- 62.Kressin NR, Groeneveld PW. Race/Ethnicity and overuse of care: a systematic review. Milbank Q. 2015 Mar;93(1):112–138. doi: 10.1111/1468-0009.12107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bryant AS, Washington S, Kuppermann M, Cheng YW, Caughey AB. Quality and equality in obstetric care: racial and ethnic differences in caesarean section delivery rates. Paediatr Perinat Epidemiol. 2009 Sep;23(5):454–462. doi: 10.1111/j.1365-3016.2009.01059.x. [DOI] [PubMed] [Google Scholar]
- 64.National Quality Forum. [Accessed July 16, 2016];National Voluntary Consensus Standards for Ambulatory Care — Measuring Healthcare Disparities. 2008 http://www.qualityforum.org/Publications/2008/03/National_Voluntary_Consensus_Standards_for_Ambulatory_Care%e2%80%94Measuring_Healthcare_Disparities.aspx.