Abstract
Proper stratum corneum function plays a pivotal role in maintenance of skin health, and improper function leads to skin disease. The stratum corneum is comprised of corneocytes surrounded by intercelluar lipids including ceramides, free fatty acids, and cholesterol. Ceramide predominant moisturizers have become a mainstay of treatment of skin disease. New technologies for delivery of ceramides include multivesicular emulsions, which deposit ceramides in a timerelease manner for a continuous rather than burst effect. Here, the authors review the available data on the use of multivesicular emulsion ceramide moisturizers in various skin diseases.
The role of the stratum corneum (SC) in healthy and diseased skin has been receiving increased focus in the literature over the past decade. The SC serves as a predominant component of epidermal barrier function and is highly active in maintaining homeostasis by responding to many exogenous exposures. Besides serving as a permeability barrier and maintaining skin hydration, the SC provides other physiologic barrier functions, such as detecting microbial invasion, responding immunologically to avert various stimuli, preventing oxidative damage, and mitigating the effects of ultraviolet (UV) light exposure.1 While epidermal barrier impairment has long been a focus in the pathogenesis of atopic dermatitis (AD), recent data suggest its importance in other skin conditions including acne vulgaris (AV) and rosacea.2–5 In addition to prescription drugs, over-the-counter (OTC) therapeutic moisturizers and cleansers must be properly selected to maintain the functional and structural integrity of the skin. Ceramide-containing skin care formulations using multivesicular emulsion (MVE) technology represent one such set of skincare products that have been studied in the management of a variety of common skin diseases, including AD.
STRATUM CORNEUM FUNCTION IN HEALTH AND DISEASE
The structure of the SC has been traditionally referred to as a “brick and mortar” model. While corneocytes represent the bricks, intercellular lipids represent the mortar. Intracellular lipid precursors are sequestered into lamellar bodies within granular layer keratinocytes and processed into the lipids that are then incorporated into the lipid bilayer.6 This organized lamellar lipid membrane is composed of a physiologic ratio of ceramides (40–50%), cholesterol (25%), and free fatty acids (10–15%).7 Ceramides are natural skin lipids comprising a fatty acid and a sphingosine base. More than 10 different ceramide fractions exist, but among these, ceramide-1 (CER-1) has been shown to play an essential role in proper packing and ordering of the lamellar organization of SC lipids.8
A properly functioning SC is essential for healthy skin, as it maintains epidermal hydration and serves as a barrier that responds to environmental stressors, infections, irritants, and allergens.1 A defective epidermal barrier is a key contributing factor to many skin diseases, including eczematous disorders, psoriasis, acne, and rosacea.9 Barrier compromise may be the result of either genetically predisposed endogenous factors (i.e., underlying skin disease such as AD and ichthyosis) or exogenous factors, such as improper personal care products, climatic extremes, or contact with irritants and/or allergens.2,10
In AD, patients exhibit impaired SC lipid synthesis with decreased amounts of physiologic lipids and a predominance of ceramide deficiency. This is present in not only lesional skin, but also clinically nonaffected skin, resulting in innate epidermal barrier dysfunction in atopic skin. Abnormal “mortar” within the SC results in a “dilapidated epidermis” with increased transepidermal water loss (TEWL) and impaired epidermal barrier function. This SC dysfunction induces reactive inflammation as a self repair mechanism, with exposure to environmental irritants, allergens, and microbes resulting in further cutaneous inflammation.10
While AV is considered an inflammatory disease resulting from follicular hyperkeratosis, sebum production, and the follicular proliferation of Propionibacterium acnes, epidermal barrier abnormalities also play an important role.3,11 The skin of patients with AV has been shown to be associated with ceramide deficiency, which correlates directly to greater AV severity. Skin barrier permeability is theorized to contribute to follicular hyperkeratosis, promoting the formation of comedones.11 Moreover, many topical acne medications are known to cause skin irritation, further compromising SC barrier function during treatment.3
Rosacea is characterized by impairment and hyperactivity of the innate immune system of facial skin, neurovascular dysregulation, superficial vascular proliferation, and epidermal barrier dysfunction.12 SC barrier defects play a key role in the dryness and sensitivity rosacea patients experience. In fact, patients with erythrotelangiectatic rosacea (ETR) exhibit increased TEWL levels in both clinically affected and clinically normal facial skin.13 Moreover, epidermal barrier dysfunction in rosacea is accompanied by intolerance to many personal care products.14 In one study, 100 percent of ETR patients and 68 percent of papulopustular rosacea (PPR) patients reported a positive sting test to 5% lactic acid. By comparison only 19 percent of control patients experienced stinging. This objectively supports the greater skin sensitivity among rosacea patients compared to normals.15 As harsh skin care products can exacerbate rosacea, selection of gentle cleansers and moisturizers that repair and maintain the integrity of the epidermal barrier is extremely important.16
MOISTURIZER DESIGN AND FUNCTION
OTC skin care regimens must be properly selected to suit the personal preference of patients and provide support for the integrity of the SC. Proper selection of a moisturizer and skin cleanser can help improve and maintain skin barrier function and mitigate susceptibility to irritants, allergens, and microbes.17 The use of a moisturizer as an integral component of rosacea management is increasingly being evaluated in clinical trials. Corneometry and TEWL studies are commonly used outcomes in studies to evaluate the therapeutic impact of moisturizers because they can be objectively measured.1 These data can be used to better select OTC moisturizers in making specific recommendations to patients.
Traditional moisturizers, classified as either creams, lotions, or ointments, offer occlusive and/or humectant qualities, with each offering different aesthetic properties. The use of a personal care product is largely influenced by aesthetic characteristics, as a patient who does not like the product will likely not adhere to the prescribed regimen. Ointments are greasy mixtures of fats, waxes, oils, and hydrocarbons. Since they are anhydrous, they may contain little or no preservatives as there are minimal concerns for bacterial contamination in the absence of water. Creams and lotions, on the other hand, are emulsions, or mixtures of two nonsoluble ingredients, where the internal phase is dispersed in droplets in the external phase, held together by emulsifiers. Creams and lotions can be formulated as either oil-in-water or water-in-oil emulsions.18
Moisturizers improve skin hydration using a combination of occlusive, humectant, and emollient ingredients. Common occlusives include petrolatum, dimethicone, and mineral oil, which essentially form a seal over the skin and prevent evaporative water loss. Humectants act from the inside-out, attracting water from the dermis into the SC, and sustain water content within the SC. In humid environments, they also may act from the outside-in, attracting moisture from the ambient atmosphere. Glycerin and hyaluronic acid are examples of commonly used humectants. Finally, emollients, which may sometimes exhibit some occlusive properties, provide a sleek quality to the formulation. They also add smoothness to the skin by acting as a sealant within fine fissures and microfissures present in xerotic skin. These include lanolin and light mineral oil. Most moisturizers contain a combination of all three ingredient types, with some ingredients providing overlap of characteristics.19
The newest generation of moisturizers contains barrier repair ingredients in addition to traditional moisturizer components. The most common of such ingredients are ceramides, which help replace the deficient lipids in some skin diseases characterized by SC barrier impairment. It is unclear whether exogenously applied ceramides are actually incorporated in the extracellular lipid matrix, or whether they provide some humectancy and occlusivity. Advancements in cosmetic chemistry have resulted in the development of bio-identical synthetic ceramides that are commonly incorporated into skin care products (notably CER-1, CER-3, and CER-6), which have been shown to function similar to natural ceramides.20
Both proper ingredients and optimized formulations must be considered when selecting OTC skin care products. MVE technology has been developed to enhance effectiveness of individual ingredients used on the skin, with time-released or sequential delivery after initial application. MVE is a novel formulation unlike traditional moisturizer emulsions.21 The MVE comprises concentric layers of oil-in-water emulsions. Similar to nesting dolls, one vesicle is contained within another inside the MVE.22 Once the product is applied to the skin, there is a sequential opening of each vesicle, with a gradual release of the ceramides and other ingredient contents, rather than the burst of immediate release with some other products.
While many OTC moisturizers contain skin barrier repair ingredients, others may be available by prescription only. The differences in formulations and therapeutic effectiveness of the OTCs and the prescription counterparts are blurred in many cases. Prescription barrier creams are not considered drugs by the United States Food and Drug Administration (FDA), but rather 510K medical devices, and as such do not require the rigorous testing needed for approval of a new drug application. Many of the 510K devices have been shown to be effective in treating skin diseases with stratum corneum dysfunction (e.g., AD). However, it is unclear whether they are truly more efficacious than some OTC formulations or just more expensive? In one head-to-head study, an OTC moisturizer was as effective in treating eczema as were two difference prescription 510K devices.23 Further research is needed to fully understand the differences between specific products.
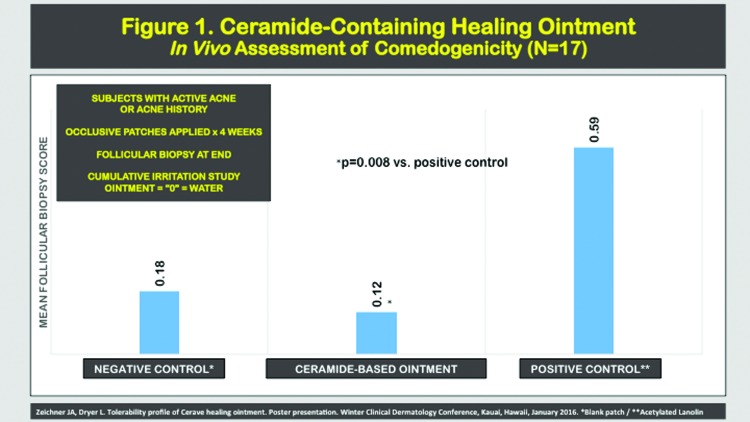
A newer ceramide-containing ointment base formulation is available which may be preferable in patients where greater initial occlusivity is desired. Figure 1 shows data supporting lack of comedogenicity with this ointment formulation.
Figure 1.
Ceramide-containing healing ointment; in vivo assessment of comedogenicity (N=17)
MULTIVESICULAR EMULSION CERAMIDE-BASED SKIN CARE PRODUCTS IN TREATING ECZEMA
AD is characterized by a defective skin barrier in both clinically affected and nonaffected skin.1,2,7,10 As a result, patients with AD suffer from an innate compromise of their skin barrier, which is worsened in areas where eczematous dermatitis is present.1,2,10 Proper selection of skin care cleansers and moisturizers have been shown to enhance clearance of eczema and improve related symptoms. In one study, MVE ceramide-containing moisturizing cream and liquid cleanser were used concurrently with fluocinonide (FLU) cream 0.05% in treating mild-to-moderate eczematous dermatitis.20 Two non-moisturizer comparator groups were also enrolled—one using a bar cleanser with the FLU cream, and the other using an MVE ceramide liquid cleanser with FLU cream. Sixty subjects, ages 5 to 80, participated and were followed for four weeks. Clearance rates were statistically better in patients who used the MVE ceramide liquid cleanser and moisturizer compared to those who used the bar cleanser (76% vs. 15%, p=0.0001). Subjects who used the MVE ceramide liquid cleanser had numerically high clearance rates compared to those who used the bar cleanser (37% vs. 15%, p=0.155). Moreover, patients who used the combination of the MVE ceramide liquid cleanser and moisturizing cream with the FLU cream cleared faster than subjects in both of the other groups. Finally, individual signs and symptoms including redness, scaling, lichenification, excoriation, and pruritus all showed the fastest onset and greatest degree of improvement at all timepoints in the study in patients using the MVE ceramide cleanser and moisturizing cream.20
While topical corticosteroids (TCS) are a mainstay of treatment for AD, steroid-sparing agents, such as topical calcineurin inhibitors, prescription barrier creams, and OTC moisturizers, are used to minimize TCS exposure. Ceramide-containing moisturizers and cleansers have been demonstrated to act as steroid-sparing agents, decreasing the duration of TCS use during flares and reducing the need to start TCS therapy altogether by reducing AD flares.24,25 In a recent cohort study, 151 patients with mild-to-moderate AD used a twice-daily regimen of only a MVE ceramide liquid cleanser and moisturizing cream for six weeks. Patients were separated into adult and pediatric groups, and both cohorts achieved statistically significant improvements in SCORAD scores (p=0.0001 in both groups) and itching (p=0.0001 in both groups) compared to baseline.24
MULTIVESICULAR EMULSION CERAMIDE-BASED SKIN CARE PRODUCTS IN TREATING ACNE
Proper skin care recommendations are a necessary component of treating AV. While ceramide reduction may occur in AV, at least during flares, skin irritation from topical acne medications often leads to nonadherence and poor clinical outcomes. A recent consensus paper summarized a systematic literature review on the topic of AV, related ceramide deficiency, and the role of moisturizers in acne treatment. The group of 11 Canadian expert dermatologists agreed that moisturizers improve AV medication-related dryness. In addition, ceramide-containing moisturizers complement prescription drugs for AV, can enhance clinical outcomes, and should be considered when making treatment recommendations for AV patients.24
MVE ceramide moisturizers and cleansers have been shown to improve therapeutic outcomes in treating patients with AV. In one open-label clinical trial, 20 patients with mild-to-moderate AV combined twice-daily MVE ceramide hydrating cleanser and ceramide-containing MVE moisturizing cream with prescription topical therapy.25 During the 12-week treatment period, all patients washed their faces with the designated cleanser and applied the moisturizer prior to application of the study topical AV medication in the morning and at night. In the morning, patients applied fixed-dose combination clindamycin phosphate 1.2%/benzoyl peroxide 2.5% gel and in the evening applied micronized tretinoin 0.05% gel. At Week 12, 60 percent of patients were considered a treatment success. The combination therapy was extremely well-tolerated, with the overwhelming majority of patients experiencing no cutaneous adverse events throughout the study. It was concluded that the MVE ceramide cleanser and moisturizing cream contributed substantially to the highly favorable tolerability with cutaneous minimal side effects, did not interfere with efficacy when applied prior to the topical medications used, and improved adherence to the regimen, which collectively account for the favorable overall treatment outcome.25
MULTIVESICULAR EMULSION CERAMIDE-BASED SKIN CARE PRODUCTS IN TREATING ROSACEA
Given the impaired SC barrier in both ETR and PPR, gentle skin cleansers and moisturizers are recommended for all rosacea patients. Permeability barrier defects exist in both clinically affected and normal-appearing facial skin, so proper skin care is important not only during a flare, but also between flares. Barrier repairing moisturizers and proper cleansers may assist in decreasing rosacea flares and reduce dryness and sensitivity.16 Moreover, moisturizers, including MVE ceramide moisturizing cream, have been shown to mitigate stinging associated with application of azelaic acid (AzA) 15% gel in some PPR patients.26 In a split-face, open label study, 102 patients with mild-to-moderate PPR applied AzA 15% gel after facial washing and then applied a moisturizer only to the right side. Two different moisturizers were evaluated, one of which was a MVE ceramide moisturizing cream. At the end of the seven-day study, there were statistically significant decreases in burning and stinging on the side using the moisturizer compared to baseline (p=0.008).26 Additionally, in vitro data showed that application of moisturizers (including MVE ceramide-containing lotion) prior to AzA 15% gel did not adversely impact penetration of AzA into human skin, which correlates with clinical data observed in MVE ceramide-containing cream applied before application of tazarotene 0.1% cream in AV.27,28 A percutaneous penetration study on human skin showed that moisturizers may be applied before or after azelaic acid gel 15%, without affecting the skin absorption profile of AzA. In fact, a MVE ceramide moisturizing lotion actually enhanced penetration of AzA when applied prior to the drug to human skin.27 This is clinically relevant as MVE ceramide-containing mosturizers have been shown to reduce skin stinging in rosacea and are commonly used alongside topical prescription drugs such as AzA.
CONCLUSION
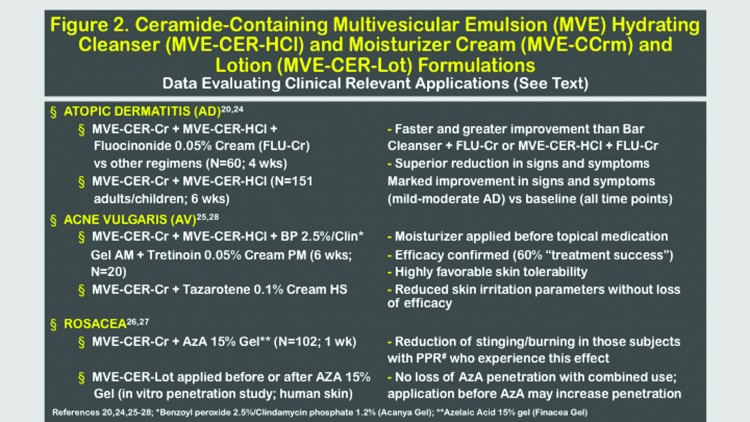
Skin barrier dysfunction plays an important role in the pathophysiology of many skin diseases. Proper selection of skin care products that address SC dysfunction can enhance therapeutic outcomes, while improper selection may exacerbate disease or augment skin irritation from topically applied agents. In choosing topical skin care products, both the ingredients and formulation must be considered. Two products may contain almost identical ingredient lists, but can be formulated very differently, affecting their cosmetic acceptability, efficacy, and tolerability. Data exists on the use of MVE ceramide-containing skin care products in eczema, acne, and rosacea, and can be considered when designing therapeutic regimens for these and other skin diseases associated with SC permeability barrier impairment. Figure 2 depicts a summary of clinically relevant applications of MVE ceramide-containing formulations.
Figure 2.
Ceramide-containing multivesicular emulsion (MVE) hydrating cleanser (MVE-CER-HCl) and moisturizer cream (MVE-CCrm) and lotion (MVE-CER-Lot) formulations (data evaluating clinical relevant applications [see text])
Footnotes
Disclosure:Dr. Del Rosso is a consultant, researcher, and/or speaker for Aqua/Amirall, Bayer Dermatology, BioPharmX, Celgene, Cutanea, Dermira, Ferndale, Foamix, Galderma, Genentech, Johnson & Johnson, Leo Pharma, Inc., Novan, Novartis, Pharmaderm, Promius, Sebacia, SunPharma, Taro Pharmaceuticals, Unilever, and Valeant.
REFERENCES
- 1.Del Rosso JQ, Levin J. The clinical relevance of maintaining the functional integrity of the statum corneum in both healthy and disease-affected skin. J Clin Aesthet Dermatol. 2011;4(9):22–42. [PMC free article] [PubMed] [Google Scholar]
- 2.Del Rosso JQ, Zeichner J, Alexis A, et al. Understanding the epidermal barrier in healthy and compromised skin: clinically relevant information for the dermatology practitioner. J Clin Aesthet Dermatol. 2016;9(4):S1–S8. [PMC free article] [PubMed] [Google Scholar]
- 3.Thiboutot D, Del Rosso JQ. Acne vulgaris and the epidermal barrier: is acne vulgaris associated with inherent epidermal abnormalities that cause impairment of barrier functions? Do any topical acne therapies alter the structural and/or functional integrity of the epidermal barrier? J Clin Aesthet Dermatol. 2013;6(2):18–24. [PMC free article] [PubMed] [Google Scholar]
- 4.Dirschka T, Tronnier H, Folster-Holst R. Epithelial barrier function and atopic diathesis in rosacea and perioral dermatitis. Br J Dermatol. 2004;150:1136–1141. doi: 10.1111/j.1365-2133.2004.05985.x. [DOI] [PubMed] [Google Scholar]
- 5.Dasgupta BR, Bajor J, Mazzati DJ, Manoj M. Cosmeceuticals: function and the skin barrier. In: Draelos ZD, editor. Cosmeceuticals. 3rd ed. Elsevier; Philadelphia: 2016. pp. 3–10. [Google Scholar]
- 6.Sajic D, Asiniwasis R, Skotnicki-Grant S. A look at epidermal barrier function in atopic dermatitis: physiologic lipid replacement and the role of ceramides. Skin Therapy Lett. 2012;17(7):6–9. [PubMed] [Google Scholar]
- 7.Harding CR. The stratum corneum: structure and function in health and disease. Dermatol Ther. 2004;17:6–15. doi: 10.1111/j.1396-0296.2004.04s1001.x. [DOI] [PubMed] [Google Scholar]
- 8.Bouwstra JA, Gooris GS, Dubbelaar FER, et al. Role of ceramide 1 in the molecular organization of the stratum corneum lipids. J Lipid Res. 1998;39:186–196. [PubMed] [Google Scholar]
- 9.Sator PG, Schmidt JB, Hönigsmann H. Comparison of epidermal hydration and skin surface lipids in healthy individuals and in patients with atopic dermatitis. J Am Acad Dermatol. 2003;48(3):352–358. doi: 10.1067/mjd.2003.105. [DOI] [PubMed] [Google Scholar]
- 10.Sajic D, Asiniwasis R, Skotnicki-Grant S. A look at epidermal barrier function in atopic dermatitis: physiologic lipid replacement and the role of ceramides. Skin Therapy Lett. 2012;17:6–9. [PubMed] [Google Scholar]
- 11.Yamamoto A, Takenouchi K, Ito M. Impaired water barrier function in acne vulgaris. Arch Dermatol Res. 1995;287(2):214–218. doi: 10.1007/BF01262335. [DOI] [PubMed] [Google Scholar]
- 12.Crawford GH, Pelle MT, James WD. Rosacea: I. Etiology, pathogenesis, and subtype classification. J Am Acad Dermatol. 2004;51(3):327–341. doi: 10.1016/j.jaad.2004.03.030. quiz 342–344. [DOI] [PubMed] [Google Scholar]
- 13.Dirschka T, Tronnier H, Folster-Holst R. Epithelial barrier function and atopic diathesis in rosacea and perioral dermatitis. Br J Dermatol. 2004;150:1136–1141. doi: 10.1111/j.1365-2133.2004.05985.x. [DOI] [PubMed] [Google Scholar]
- 14.Torok HM. Rosacea skin care. Cutis. 2000;66(4) Suppl:14–16. [PubMed] [Google Scholar]
- 15.Lonne-Rahm SB, Fischer T, Berg M. Stinging and Rosacea. Acta Derm Venereol (Stockh). 1999;79(6):460–461. doi: 10.1080/000155599750009915. [DOI] [PubMed] [Google Scholar]
- 16.Levin J, Miller R. A guide to the ingredients and potential benefits of over-the-counter cleansers and moisturizers for rosacea patients. J Clin Aesthet Dermatol. 2011;4(8):31–49. [PMC free article] [PubMed] [Google Scholar]
- 17.Wolf R, Parish L. Barrier-repair prescription moisturizers: do we really need them? Facts and controversies. Clin Dermatol. 2013;31(6):787–791. doi: 10.1016/j.clindermatol.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 18.Palefsky I. Creams, lotions, and ointments. In: Draelos ZD, editor. Cosmetic Dermatology. 1st ed. Wiley-Blackwell; Hoboken, NJ: 2010. pp. 71–74. [Google Scholar]
- 19.Rawlings AV, Canestrari DA, Dobkowski B. Moisturizer technology versus clinical performance. Derm Ther. 2004;17:49–56. doi: 10.1111/j.1396-0296.2004.04s1006.x. [DOI] [PubMed] [Google Scholar]
- 20.Draelos ZD. The effect of ceramide-containing skin care products on eczema resolution duration. Cutis. 2008;81(1):87–91. [PubMed] [Google Scholar]
- 21.Espinoza R Inventor; HealthPoint, LTD, assignee. Multivesicular emulsion drug delivery systems. US Patent 6,709,663. March 23, 2004
- 22.Bikowski J, Shroot B. Multivesicular emulsion: a novel, controlled-release delivery system for topical dermatological agents. J Drugs Dermatol. 2006;5(10):942–946. [PubMed] [Google Scholar]
- 23.Miller DW, Koch SB, Yentzer BA, et al. An over-the-counter moisturizer is as clinically effective as, and more cost-effective than, prescription barrier creams in the treatment of children with mild-to-moderate atopic dermatitis: a randomized, controlled trial. J Drugs Dermatol. 2011;10(5):531–537. [PubMed] [Google Scholar]
- 24.Lynde CW, Andriessen A, Barankin B, et al. Moisturizers and ceramide-containing moisturizers may offer concomitant therapy with benefits. J Clin Aesthet Dermatol. 2014;7(3):18–26. [PMC free article] [PubMed] [Google Scholar]
- 25.Zeichner JA, Patel RV, Haddican M, Wong V. Efficacy and safety of a ceramide containing moisturizer followed by fixed-dose clindamycin phosphate 1.2%/benzoyl peroxide 2.5% gel in the morning in combination with a ceramide containing moisturizer followed by tretinoin 0.05% gel in the evening for the treatment of facial acne vulgaris. J Drugs Dermatol. 2012;11(6):748–752. [PubMed] [Google Scholar]
- 26.Del Rosso JQ. The use of moisturizers as an integral component of topical therapy for rosacea: clinical results based on the Assessment of Skin Characteristics Study. Cutis. 2009;84(2):72–76. [PubMed] [Google Scholar]
- 27.Del Rosso JQ, Lehman PA, Raney SG. Impact of order of application of moisturizers on percutaneous absorption kinetics: evaluation of sequential application of moisturizer lotions and azelaic acid gel 15% using a human skin model. Cutis. 2009;83(3):119–124. [PubMed] [Google Scholar]
- 28.Tanghetti E, et al. Moisturizer use enhances facial tolerability of tazarotene 0.1% cream without compromising efficacy in patients with acne vulgaris. Poster presented at 32nd Annual Hawaii Dermatology Seminar; 2008. [Google Scholar]