Abstract
[Purpose] To estimate the effect of Klapp method on idiopathic scoliosis in school students. [Subjects and Methods] A single-blind randomized clinical trial with 22 students randomly divided into intervention group (n=12) and inactive control group (n=10). Exercise protocol consisted of Klapp method, 20 sessions, three times a week for intervention group, and inactivity for control group. Dorsal muscle strength was measured by dynamometer; body asymmetries and gibbosity angles were measured by biophotogrammetry. Data were obtained by Generalized Estimated Equation, with 5% significance level. Clinical impact for dependent variables was estimated by “d” Cohen. [Results] There was no change in intragroup analysis and intergroup for all postural symmetry variables. However, it was detected intergroup difference in extensor muscle strength and intergroup difference with marginal significance of gibbosity angles. Regarding extensor muscle strength, intervention group produced average improvement of 7.0 kgf compared to control group. Gibbosity angles progressed less in intervention group, with 5.71° average delay compared to control group. [Conclusion] Klapp method was effective for gibbosity stabilization and it improves spine extensor muscle strength.
Keywords: Scoliosis, Physical therapy, Posture
INTRODUCTION
Scoliosis is a progressive and deforming musculoskeletal dysfunction of the spine. It is characterized by a three-dimensional vertebra deviation, which has lateral inclination in frontal plane, along with contralateral rotation in transverse plane and alignment in sagittal plane1). Scoliosis has been associated with uneven growth of intervertebral disks2), pubertal growth3), as well as imbalance of stabilizing deep spinal muscles2). However, in most cases (80–85%) the cause is unknown, and it is called idiopathic scoliosis.
Scoliosis prevalence in adolescents is about 22%4). In this phase of growth and development, young people go through several changes and physical and psychosocial adaptation, resulting a wide range of postures, increasing susceptibility to posture changes4, 5).
Conservative therapies applied to correct scoliosis in adolescents or to prevent its progression are still scarce and inconclusive. In a systematic review, Negrini et al.6) reported lack of evidence that exercise decrease scoliosis deformities progression. More recently, other authors confirmed the same lack of quality studies and showed low effects of clinical impact7, 8).
Several kinesiotherapy techniques, manual therapy and mechanotherapy may be used in scoliosis treatment as follows: Iso-stretching9), Pilates10), Global Postural Reeducation (GPR)11), Schroth method7), spine rotation torque machines7), etc. These methods aim to perform active spinal realignment through stretching, trunk muscle strengthening and, to a lesser extent, motor control training.
Klapp method, focus of this study, consists of a set of stretching and strengthening postures usually applied, but that requires further investigation12). Rudolph Klapp, developer of the method, aimed to stretch and strengthen muscles by all fours positions, easily applied and that can be used in small groups12, 13). Klapp noted that bipedal animals have scoliosis, while quadrupeds not13). Therefore, such primitive positions would allow vertebrae repositioning, leading to spine realignment13).
This study aims to compare the effect of a Klapp Method exercise program on scoliosis progression, postural imbalances and spine extensor muscle strength in school students aged between 10 and 15 years. The tested hypothesis was that there would be no difference in body symmetry, spine extensor muscle strength and stabilization of scoliosis among school children aged between 10 and 15 years that underwent Klapp method compared to inactive control group.
SUBJECTS AND METHODS
It is a two arm randomized controlled trial, prospective, parallel, singleblinded, registred as RBR-53C3B8 (http://www.ensaiosclinicos.gov.br/rg/view/1952/) approved on document number 269/2012 of the Research Ethics Committee involving Human Beings (REC) of Federal University of Rio Grande do Norte (UFRN), under protocol 301/11-P.
Inclusion criteria for the study were: age between 10 and 15 years, participation in the screening assessment for verification of suspected scoliosis by Adams sign2), to agree to participate in the study, to sign the informed consent (IC) term approved by REC of Federal University of Rio Grande do Norte. Participants excluded were those who had scheduled or undergone any corrective surgery of the spine before or during data collection process, those who were in physical therapy for scoliosis, those who had physical and/or mental disabilities, trauma, orthopedic, and/or rheumatologic injury that prevented maintenance of orthostatic position and participation in another experimental protocol.
Twenty-two students whose parents or guardians sought physical therapy services at the School Clinic of the Faculty of Health Sciences of Trairi (FACISA) UFRN, from April to July 2013, participated in this study.
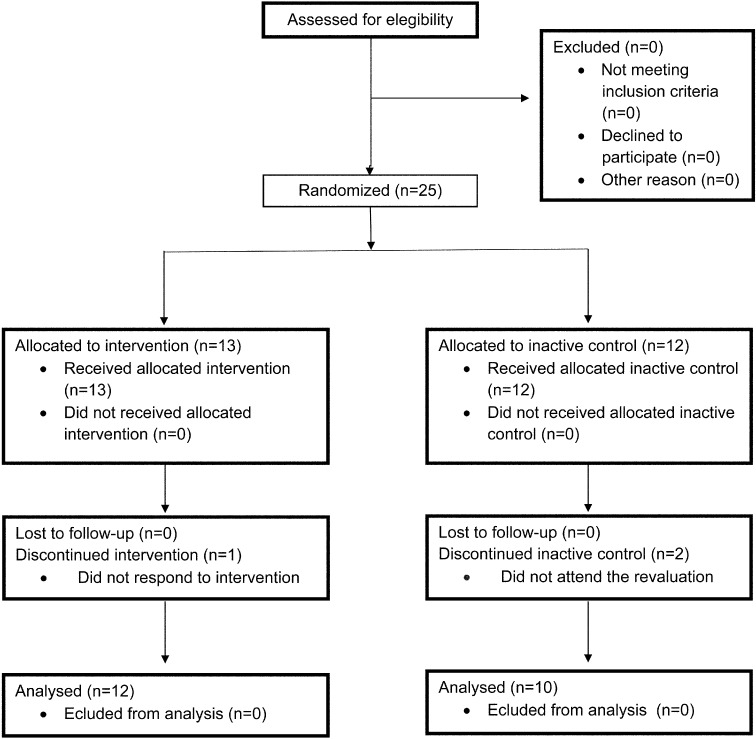
Sample was randomly allocated by the main researcher into two groups by Bioestat 5.0 software sampling function. Control group (CG) was composed of 10 students and 12 students in intervention group (IG). Both groups underwent postural assessment by computerized photogrammetry by a blinded examiner before and after intervention. CG did not perform any kind of intervention, and it was considered inactive control (Fig. 1).
Fig. 1.
Flow of participants throughout the study
Body posture alignment was analyzed by a blinded evaluator from computerized photogrammetry. This assessment consists in acquisition of standardized photographs regarding positioning of the volunteer and camera, and marking of anatomical landmarks.
A digital camera (Sony 6.0MP DSC-T9) was positioned on a level tripod (Vanguard VT-131) parallel to the floor, at a height of 0.90 cm from the ground, with auto-zoom and focal length of 1.80 m for anterior and posterior frontal plane, bilateral sagittal plane14). Distance between volunteer and the wall was 40 cm, marked on the floor to avoid change of position.
Photographs were analyzed with software AutoCAD12®15). Vertical reference has been set in the software by a graph marker with known value. Floor, tripod and camera horizontal alignment was measured with a wood level, and corrected in the software when needed. The back wall was covered with a white sheet.
Anatomical points were marked with Pimaco® 12 mm adhesives. These anatomical points were: glabella, tragus, acromion, anterior iliac spine (ASIS), tibial tuberosity, lateral malleolus, C7 spinous process, posterior superior iliac spine (PSIS), inferior angle of scapula and T3 spinous process. Angular and linear variables were analyzed, shown in Table 1.
Table 1. Description of linear and angular measurements of postural variables.
| Measurement | Initials | Description |
|---|---|---|
| Horizontal alignment of the head | HHA | Angle formed by the line between the right and left tragus and the line drawn horizontally, parallel to the ground. |
| Horizontal alignment of the shoulder | SHA | Angle formed by the line between the right and left acromions and the line drawn horizontally, parallel to the ground. |
| Horizontal alignment of the anteriosuperior iliac spine | ASHA | Angle formed by the line between right and left anterosuperior iliac spine (ASIS) and the line drawn horizontally, parallel to the ground. |
| Horizontal alignment of the tibial tuberosity | TTHA | Angle formed by the line between the left and right tibial tuberosity and the line drawn horizontally, parallel to the ground. |
| Thales triangle | ΔT | Angle formed by the intersection line passing through the medial edge of the upper limb with the straight line adjacent the waist. |
| Head protusion angle | HPA | Angle formed by the intersection line connecting the ear tragus and the spinous process of C7 with the line parallel to the ground. |
| Body vertical alignment | BVA | Formed by the intersection line connecting the acromion and lateral malleolus with the line perpendicular to the ground. |
| Inferior horizontal angle of the scapula | ISHA | Line between the inferior angle of the right and left scapula and the line drawn horizontally, parallel to the ground. |
| Horizontal angle of the posterosuperior iliac spine | PSHA | Line between the right and left anterosuperior iliac spines and the line drawn horizontally, parallel to the ground. |
| Gibbosity angle | ΔG | Angle between the axis of coordinates x/ tangent line to the hump/y axis. |
A pilot study was previously conducted to verify intra-rater reliability for computerized photogrammetry use. The examiner performed analysis of images with a 7 day interval and results were analyzed using intraclass correlation coefficient (ICC), which showed excellent level of reliability (ICC>0.70) for angular and linear measurements used in this study.
Paraspinal muscle strength was measured by a manual back dynamometer (Crown, Industrial Oswaldo Filizola LTDA) with circular and analogue display, capacity from 1 to 200 kgf and 1kgf division. Students were told to stand up with slightly bent knees, anterior flexion of the trunk and outstretched arms holding the instrument bar. All participants were informed about equipment operation, measurement protocol procedure and performance of maximum force to familiarize them with the dynamometer. Subsequently, according to evaluator signal, the volunteer was instructed to perform a maximum contraction, seeking to exert force from lumbar muscles, and this procedure was performed twice, with one-minute interval between measurements, and obtained mean measures16).
IG intervention was developed by applying Klapp method and consisted of 20 sessions, 50 minutes each session, three times a week. Two IG were formed, with a maximum of 9 students in each IG, with one therapist for every three students, but only one therapist provided verbal command during intervention.
Participants were asked to use proper clothes for the practice of therapeutic exercises (short for boys and shorts and shirt for girls) in order to facilitate control over the participants’ spine. CG did not receive any intervention, thus constituting an inactive CG.
In each session, a sequence of 8 postures of Klapp method was carried out, each one was maintained for 5 minutes. Positions held were “crawling”, “slide”, “lide as snake movement”, “bunny hopping”, “turn the arm”, “big arch”, “crawling near the ground” and “big curve”12, 13) (Fig. 2).
Fig. 2.
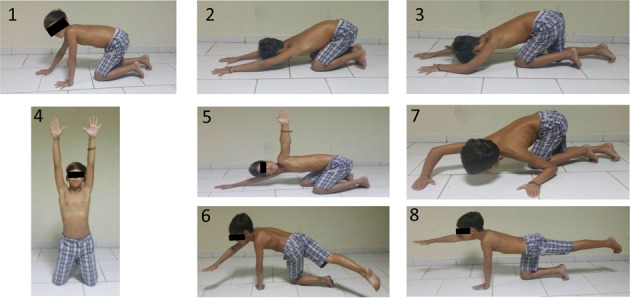
Exercises accomplished by the participants underwent the Klapp method intervention1) Lateral crawl; 2) Horizontal sliding; 3) Crawl posture near the ground; 4) Bunny hopping; 5) Arm turn; 6) Big arch; 7) Lateral crawl near the ground; 8) Big curve.
Strength and postural asymmetry variables were described by mean and standard deviation. To estimate Klapp protocol effects, it was used the Generalized Equation Estimated (GEE) based on the linear model and taken into account Wald x2 estimates for the difference between groups and moments, and post hoc Bonferroni test for observing interaction group-time. Significance level α≤0.05 was adopted. Effect size of clinical impact for the study variables was calculated by ratio “d” Cohen, with values above 0.8 considered a strong effect size; moderate between 0.5 and 0.8 and low below 0.517).
RESULTS
Twenty-five adolescents were eligible for the study, and they were allocated to IG (n=13) and CG (n=12). Three were lost during follow-up, resulting 22 participants, 12 in IG and 10 in CG. Fifteen (65.22%) were girls and 8 (34.78%) boys, mean age of 11.90 (± 1.41) years.
In Table 2, results show no significant difference in paraspinal muscle strength post-intervention in IG and CG. Intergroup analysis indicates significant difference (p<0.01) between IG and CG, best shown in Table 3, in which we highlight that IG muscle strength after intervention (GIa) becomes greater than CG before (CGb), (p<0.001) and after (CGa) (p<0.01), with moderate clinical implications (d>0.5), and IG before (GIb) and CGb are alike.
Table 2. Pre and Post-intervention with Klapp method for the treatment of scoliosis in adolescents.
| Measurements | Intervention group | Control group | ||||
|---|---|---|---|---|---|---|
| Pre Mean ± SD | Post Mean ± SD | Cohen’d | Pre Mean ± SD | Post Mean ± SD | Cohen’d | |
| Muscle strength | 31.12 ± 12.53 | 36.66 ± 13.01** | 0.43 | 31.25 ± 8.94 | 36.50 ± 9.74** | 0.56 |
| HHA | 0.59 ± 0.84 | 1.28 ± 0.74 | 0.24 | 0.34 ± 0.65 | 0.23 ± 0.72 | 0.05 |
| SHA | 0.24 ± 0.84 | 0.35 ± 0.41 | 0.07 | 0.16 ± 0.41 | 0.58 ± 0.51 | 0.31 |
| ASHA | 0.30 ± 0.55 | 0.30 ± 0.58 | 0.001 | 0.18 ± 0.59 | 0.24 ± 0.42 | 0.04 |
| TTHA | 0.25 ± 0.60 | 0.42 ± 0.58 | 0.08 | 0.32 ± 0.83 | 0.86 ± 0.64 | 0.23 |
| ΔT | 1.53 ± 1.61 | 1.44 ± 1.49 | 0.02 | 2.4 ± 1.34 | 1.71 ± 2.06 | 0.12 |
| HPAd | 82.35 ± 1.81 | 81.98 ± 1.49 | 0.06 | 82.11 ± 2.94 | 82.44 ± 3.05 | 0.03 |
| BVAd | 87.35 ± 0.31 | 87.43 ± 0.36 | 0.07 | 87.17 ± 0.47 | 87.74 ± 0.48 | 0.36 |
| HPAe | 83.64 ± 1.93 | 81.77 ± 2.25 | 0.25 | 82.54 ± 2.75 | 79.78 ± 3.50 | 0.29 |
| BVAe | 87.12 ± 0.32 | 87.28 ± 0.32 | 0.14 | 87.04 ± 0.22 | 86.92 ± 0.53 | 0.10 |
| ISHA | 2.35 ± 0.81 | 1.08 ± 0.93 | 0.40 | 0.76 ± 1.08 | 1.22 ± 1.10 | 0.16 |
| PSHA | 0.28 ± 0.76 | 1.10 ± 0.74 | 0.32 | 1.33 ± 0.83 | 0.54 ± 0.79 | 0.30 |
| ΔG | 4.04 ± 7.20 | 0.47 ± 7.90 | 0.47 | 3.47 ± 8.26 | 5.71 ± 5.15 | 0.33 |
**p<0.05 between groups
Table 3. Interaction between experimental protocol and time of evaluation on measures of muscle strength and gibbosity angle.
| Groups | Difference of means (95% CI) | Cohen’d |
|---|---|---|
| Muscle strength | ||
| IGb-CGb | −4.04 (−9.86: 1.78) | 0.37 |
| IGb-IGa | 3.92 (−4.08: 11.94) | 0.30 |
| CGb-CGa | 2.15 (−2.70: 7.02) | 0.23 |
| IGa-CGb | 7.96 (3.22: 12.71)* | 0.72 |
| IGa-CGa | 6.19 (1.64: 10.75)* | 0.54 |
| ∆G | ||
| IGb-CGb | 0.95 (−7.78: 7.97) | 0.12 |
| IGb-IGa | 3.56 (−2.03: 9.17) | 0.47 |
| CGb-CGa | −2.23 (−7.97: 3.49) | 0.31 |
| IGa-CGb | −3.47 (−11.28: 4.33) | 0.42 |
| IGa-CGa | −5.71 (−11.97: 0.55) | 0.87 |
IGb: intervention group before; IGa: intervention group after. CGb: control group before; CGa: control group after. *p<0.05
ΔG showed no intra-group change post-intervention both in IG (p=0.35) and CG (p=0.35), Table 2. However, there was a marginally significant intergroup difference (p=0.08) that was deeply analyzed in Table 3. It is possible to see that IG avoided a 5.71° progression in ΔG, representing strong clinical impact (d=0.87). Other angular and linear measurements evaluated did not change after this experimental protocol.
DISCUSSION
This study showed that Klapp method improved spinal extensor muscle strength moderately in a 20 sessions protocol and prevented progression of gibbosity angle with strong clinical impact, even showing marginal statistical significance. Other body symmetry measures showed no change after application of the method.
Ineffectiveness in changing body symmetry in study participants, after intervention, may have occurred because of minimal body asymmetries, in some measures were less than a degree of deviation. Postural changes are frequent in children and adolescents, because in this development stage, posture undergoes many adjustments and adaptations to body changes demanded by biopsychosocial factors18). Some of these changes are inherent to the child’s postural development and tend to disappear during growth, as lumbar hyperlordosis, knee valgus and internal hip rotation19). On the other hand, some asymmetries might be caused by daily demands on the body and result in negative impacts on posture during childhood and adult age18, 19).
Similar to our experimental protocol, Iunes and colleagues12) applied Klapp method in 16 adolescents aged 15 ± 2.61 years old. It was observed improvement in post intervention body asymmetries. However, it was not analyzed any effect on scoliosis curvature, therefore, this study showed to be effective in restraining its progression. On the other hand, these authors demonstrated that Klapp method significantly interferes with postural asymmetries, but do not report clinical impact. Distinction between intervention parameters stand on the weekly frequency of visits, where this study there were three visits against two from Iunes and colleagues’ study12).
Savian et al.18) used stretching as scoliosis treatment method in 17 women, five sessions per week for eight weeks. Gibbosity was analyzed by two rulers, that informed values in centimeters of gibbosity. It was observed significant decrease in gibbosity, median of 1.05 cm before treatment and 0.70 after protocol. However, the absence of an inactive control group, which would avoid a possible effect of regression to the mean, caused by the use of a possible homogeneous intervention regarding scoliosis severity, or change by natural history of pubertal growth, make findings limited. Moreover, it is difficult to compare these results with ours, because the measurement was not through angular measures and it was unrelated to the gold standard, which is Cobb angle. Protocol used in this study also demonstrated greater efficiency results with half number of visits.
Segura et al.19) used Pilates method and GPR in sixteen girls aged 10–16 years, 8 in each group. The authors observed a 1.87° decrease in Cobb angle in Pilates group and 3.5° in GPR group, measured after 20 sessions. Both methods were performed individually, and that may have best results compared to our study, which was conducted collectively in a ratio of 3 participants for each therapist. However, there are misconceptions in data analysis from this study, which only intragroup comparison is made through t test and not intergroup. Also there was absence of inactive control group, it would avoid effect of regression to the mean or changes by the natural history of the disease.
In this study, it was observed significant improvement in spine extensor muscle strength in IG compared to post-intervention CG. Otman, Kose and Yakut20) detected improvement in Cobb angle and spine rotator muscle strength in adolescents with idiopathic scoliosis after applying Schroth method. His experimental protocol was based on five sessions per week, four hours a day, for six weeks of intervention, and it was continued at home for the same time. Mcintire et al.21) also identified improved isometric strength of trunk rotators after 16 weeks of intervention with rotational strengthening exercises in MedX devices, both in the group that performed 32 supervised visits using elastic band, as well as in the group that performed unsupervised exercises.
Both methods above have shown effectiveness in reducing scoliosis degree, whereas our study only found refrained progression. One must consider that results obtained with Schroth20) method protocol had unfeasible intervention logistics from a clinical point of view and the strengthening equipment from Mcintire et al.21) study have a high cost because of its individual application. Besides, long-term effects of these methods on motor learning and on the action of spine postural muscles are questionable.
GPR, Schroth and Iso-stretching are methods aimed to increase extensibility, strengthen muscles globally and realign vertebrae through postures maintained by isometric and/or eccentric contractions in extreme ranges, causing discomfort and poor relation with postures in activities of daily life. Mechanotherapeutic methods, such as MedX Machine, are based on dynamic strengthening of extensor and rotation muscles of the spine. However, these devices use uniplanar movements, little functional in its appliance and affect mainly phasic muscles, which are not first choice in spine segmental stabilization, especially in common daily demands.
Pilates method also aims to achieve these physical properties of extensibility, strength and mainly motor control through slow and repetitive movements22). Engine control property aims to make muscles more coordinated to perform anticipatory action of postural control and, thus, to stabilize body segments that underpin the movement of body levers23), which seems more suitable in postural dysfunction situations. This method has its characteristic because it uses functional movements in intermediate ranges, of slow and repeated execution, essential to generate motor learning24).
Klapp method is similar to GPR and Iso-stretching in developing flexibility and strength in muscle tissue by eccentric action, as well as the ability to stimulate motor learning in postural muscles, like Pilates, for functional and coordinated movements. This last characteristic is due to the adoption of positions that follow the sequence of human development and, therefore, has functional basis to promote motor learning and suitable motor spine control25). However, this potential has a limit on Klapp method at developing only all four positions, while most functional human activities are in standing position, enabling occurrence of scoliosis.
Studies focusing on the use of isolated kinesiotherapy to stretch and strengthen muscles show evidence that this might not to be the most appropriate way of care in scoliosis, where there is dysfunction of anticipatory postural activation26), besides imbalance of length-tension relationship of stabilizer muscles27) and central processing dysfunctions28). In this case, evidence supports the need to gather therapeutic methods that enable modification of rheological properties with exercises for motor control and have central effect on learning and human movement29).
Klapp method seems to be able to stretch and strengthen muscles and thus interfere with scoliosis curve magnitude, especially in the critical period of growth spurt where scoliosis tends to worsen, between 10 and 14 years old for girls and 12 and 16 years old for boys, same age from our sample2).
We recognize some limitations in our study. The first is the absence of X-ray examinations to measure Cobb angle, which prevents more precise statements about the degree of scoliosis and stratification of severity, despite photogrammetry has proven validation. Another limitation is the difficulty of little playful physical therapy methods, including Klapp, to promote adhesion of children and adolescents. Finally, we highlight the failure to carry out follow-up for at least six months or a year, in order to identify the medium and long term impact of the method and verify if Klapp method only modifies rheological properties of soft tissue or also generates motor learning.
Possible questions regarding sample size concerning improvement found on spine extensor muscle strength and gibbosity angle become unfounded due to the magnitude of the evidenced clinical effect22) and the existing dependency relationship between sample size and power of hypothesis testing in determining statistical significance.
Klapp method is a scoliosis management method that has clinical utility in outpatient services and primary care, by allowing the physical therapist to provide individual and collective care, added to its self-management capacity for those participating in the program. This last feature needs to be studied through clinical teaching in community settings, such as schools, and to be measured their ability to empower children for self-care.
Klapp method was effective for gibbosity stabilization and strengthening of extensor muscles. However, it was not able to modify body asymmetries.
REFERENCES
- 1.Kadoury S, Labelle H: Classification of three-dimensional thoracic deformities in adolescent idiopathic scoliosis from a multivariate analysis. Eur Spine J, 2012, 21: 40–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Busscher I, Wapstra FH, Veldhuizen AG: Predicting growth and curve progression in the individual patient with adolescent idiopathic scoliosis: design of a prospective longitudinal cohort study. BMC Musculoskelet Disord, 2010, 11: 93–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baroni MP, Sanchis GJ, de Assis SJ, et al. : Factors associated with scoliosis in schoolchildren: a cross-sectional population-based study. J Epidemiol, 2015, 25: 212–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Santos CI, Cunha AB, Braga VP, et al. : Ocorrência de desvios posturais em escolares do ensino público fundamental de Jaguariúna, São Paulo. Rev Paul Pediatr, 2009, 27: 74–80. [Google Scholar]
- 5.Sedrez JA, da Rosa MI, Noll M, et al. : Risk factors associated with structural postural changes in the spinal column of children and adolescents Rev Paul Pediatr, 2015, 33: 72–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Negrini S, Antonini G, Carabalona R, et al. : Physical exercises as a treatment for adolescent idiopathic scoliosis. A systematic review. Pediatr Rehabil, 2003, 6: 227–235. [DOI] [PubMed] [Google Scholar]
- 7.Mordecai SC, Dabke HV: Efficacy of exercise therapy for the treatment of adolescent idiopathic scoliosis: a review of the literature. Eur Spine J, 2012, 21: 382–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Romano M, Minozzi S, Bettany-Saltikov J, et al. : Exercises for adolescent idiopathic scoliosis. Cochrane Database Syst Rev, 2012, (8): CD007837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Monte-Raso VV, Ferreira PA, Carvalho MS, et al. : Efeito da técnica isostretching no equilíbrio postural. Fisioter pesqui, 2009, 16: 137–42. [Google Scholar]
- 10.Silva AC, Mannrich G: Pilates na reabilitação: uma revisão sistemática. Fisioter Mov, 2009, 3: 449–455. [Google Scholar]
- 11.Toledo PC, Mello DB, Araújo ME, et al. : Efeitos da Reeducação Postural Global em escolares com escoliose. Fisioter Pesqui, 2011, 18: 329–334. [Google Scholar]
- 12.Iunes DH, Cecílio MB, Dozza MA, et al. : Análise quantitativa do tratamento da escoliose idiopática com o método klapp por meio da biofotogrametria computadorizada. Braz J Phys Ther, 2010, 14: 133–140. [Google Scholar]
- 13.Fischinger B: Sistema Prof. Klapp. In Escoliose em fisioterapia. São Paulo: Panamed Editorial, 1984. [Google Scholar]
- 14.Mota YL, Mochizuki L, Carvalho GA: Influência da resolução e da distância da câmera nas medidas feitas pelo software de avaliação postural (Sapo). Rev Bras Med Esporte, 2011, 17: 334–338. [Google Scholar]
- 15.Döhnert MB, Tomasi E: Validade da fotogrametria computadorizada na detecção de escoliose idiopática adolescente. Braz J Phys Ther, 2008, 12: 290–297. [Google Scholar]
- 16.Cavazzotto TG, Tratis L, Ferreira SA, et al. : Muscular static strength test performance: comparison between normotensive and hypertensive workers. Rev Assoc Med Bras, 2012, 58: 574–579. [DOI] [PubMed] [Google Scholar]
- 17.Cohen J: Statistical power analysis for the behavioural sciences. Hillsdale: Lawrence Erlbaum Associates, 1988. [Google Scholar]
- 18.Savian NU, Faria CR, Ferreira DM, et al. : Escoliose idiopática: influência de exercícios de alongamento na gibosidade, flexibilidade e qualidade de vida. Rev Terapia Man, 2011, 9: 749–755. [Google Scholar]
- 19.Segura DC, Nascimento FC, Chiossi CA, et al. : Estudo comparativo do tratamento da escoliose idiopática adolescente através dos métodos de RPG e Pilates. Rev Saude Pesquisa, 2011, 4: 200–206. [Google Scholar]
- 20.Otman S, Kose N, Yakut Y: The efficacy of Schroth s 3-dimensional exercise therapy in the treatment of adolescent idiopathic scoliosis in Turkey. Saudi Med J, 2005, 26: 1429–1435. [PubMed] [Google Scholar]
- 21.McIntire K, Asher M, Burton D, et al. : Trunk rotational strength training for the management of adolescent idiopathic scoliosis (AIS). Stud Health Technol Inform, 2006, 123: 273–280. [PubMed] [Google Scholar]
- 22.Queiroz BC, Cagliari MF, Amorim CF, et al. : Muscle activation during four Pilates core stability exercises in quadruped position. Arch Phys Med Rehabil, 2010, 91: 86–92. [DOI] [PubMed] [Google Scholar]
- 23.Endleman I, Critchley DJ, Critchley DJ: Transversus abdominis and obliquus internus activity during pilates exercises: measurement with ultrasound scanning. Arch Phys Med Rehabil, 2008, 89: 2205–2212. [DOI] [PubMed] [Google Scholar]
- 24.Segal NA, Hein J, Basford JR: The effects of Pilates training on flexibility and body composition: an observational study. Arch Phys Med Rehabil, 2004, 85: 1977–1981. [DOI] [PubMed] [Google Scholar]
- 25.Smania N, Picelli A, Romano M, et al. : Neurophysiological basis of rehabilitation of adolescent idiopathic scoliosis. Disabil Rehabil, 2008, 30: 763–771. [DOI] [PubMed] [Google Scholar]
- 26.Chan YL, Cheng JC, Guo X, et al. : MRI evaluation of multifidus muscles in adolescent idiopathic scoliosis. Pediatr Radiol, 1999, 29: 360–363. [DOI] [PubMed] [Google Scholar]
- 27.Koppenhaver SL, Fritz JM, Hebert JJ, et al. : Association between changes in abdominal and lumbar multifidus muscle thickness and clinical improvement after spinal manipulation. J Orthop Sports Phys Ther, 2011, 41: 389–399. [DOI] [PubMed] [Google Scholar]
- 28.Potoupnis M, Kapetanos G, Kimiskidis VK, et al. : Is the central nervous system a causative factor in idiopathic scoliosis? Stud Health Technol Inform, 2002, 91: 10–11. [PubMed] [Google Scholar]
- 29.Balagué F, Mannion AF, Pellisé F, et al. : Non-specific low back pain. Lancet, 2012, 379: 482–491. [DOI] [PubMed] [Google Scholar]