Abstract
The subcutaneous implantable cardioverter-defibrillator (S-ICD) is a novel technology with proven efficacy in sudden cardiac death prevention; however, there is a lack of long-term safety data. We describe the case of a 55-year-old female patient implanted with an S-ICD due to idiopathic ventricular fibrillation, who subsequently presented with inappropriate shocks leading to ventricular fibrillation that was successfully terminated by another shock. Inappropriate shocks were due to intermittent T wave oversensing during periods of rate-dependent right bundle branch block. Assessment of the S-ICD electrograms during an exercise test allowed successful reprogramming of the device׳s sensing vector with no further events.
Keywords: Implantable defibrillator, Ventricular fibrillation, Inappropriate shock, Bundle branch block, Oversensing
1. Case report
A 55-year-old female patient was referred to us for insertion of an implantable cardioverter-defibrillator (ICD) after cardiac arrest due to idiopathic ventricular fibrillation. As she was young and had no indications for cardiac resynchronization therapy or bradycardia support, she was screened for a subcutaneous ICD (S-ICD). We recorded the surface eletrocardiogram from the anticipated location of the device׳s three sensing electrodes in the supine and standing positions and during a limited treadmill exercise test (using the Modified Bruce protocol as she was still recovering from cardiac arrest and had limited mobility). When compared with the manufacturer׳s template, the patient passed the screening in all three vectors and an S-ICD (SQ-RX® pulse generator model 1010 and Q-TRAK® lead; Boston Scientific, Marlborough, MA, USA) was implanted with a successful defibrillation test. The device automatically selected the primary sensing vector and was programmed with a conditional zone over 200 beats per minute and a shock zone over 240 beats per minute.
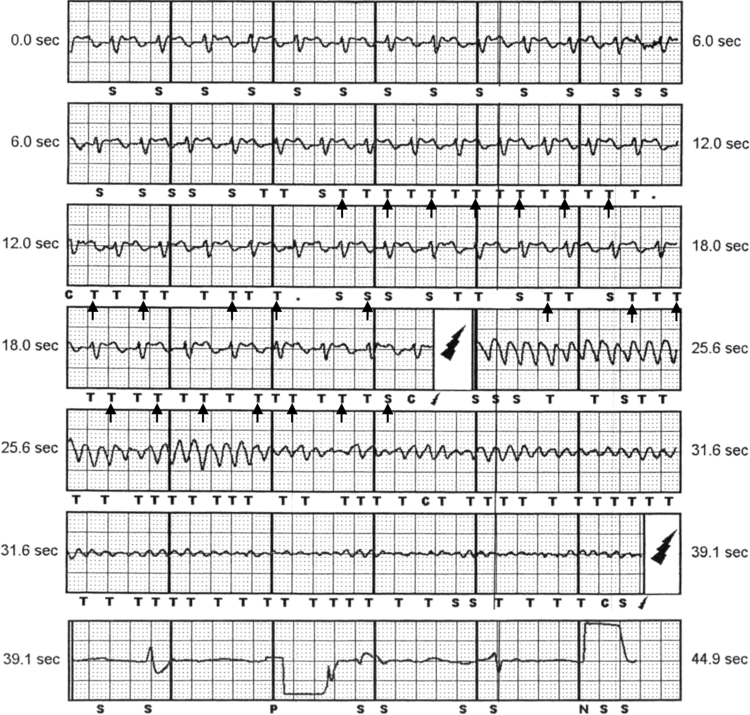
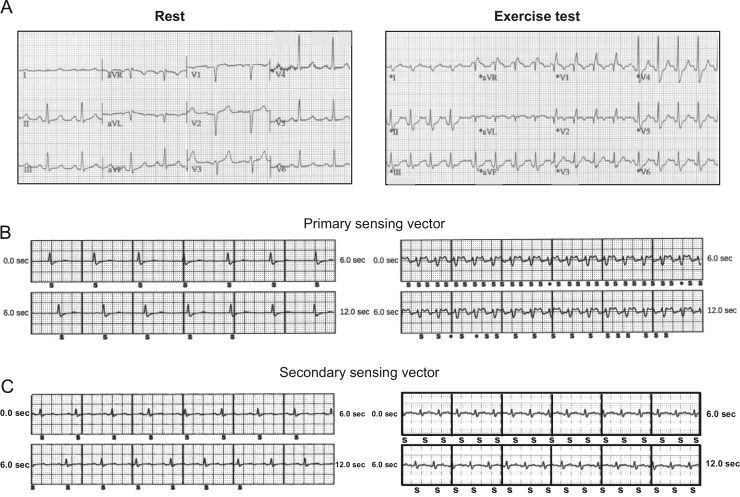
One month later, while the patient was swimming, the device delivered two shocks and the patient collapsed, followed by a third shock and recovery of consciousness. The device was interrogated and revealed inappropriate detection of ventricular tachycardia and ICD discharge due to T wave oversensing (TWOS). The second shock induced ventricular fibrillation, which was successfully terminated by a third, appropriate shock (Fig. 1). When reviewing the stored electrograms immediately prior to the first shock, we observed that the QRS and T waves morphology changed, with decreased R wave amplitude and increased T wave amplitude (resulting in decreased R/T wave ratio), leading to TWOS and double counting. The patient underwent repeat treadmill exercise testing, this time through stage 3 of the full Bruce protocol. On this occasion, we observed a rate-dependent right bundle branch block (RBBB), which reproduced the altered R/T wave ratio observed in the primary sensing vector prior to the inappropriate shock (Fig. 2). The other sensing vectors were also screened during the exercise test for altered QRS-T wave morphology with rate-dependent RBBB; the secondary sensing vector was unaffected (Fig. 2), allowing for successful sensing reprogramming. The patient was able to continue her usual exercise activities and has had no further shocks during 12 months of follow-up.
Fig. 1.
Subcutaneous implantable cardioverter-defibrillator electrograms. Electrograms from the subcutaneous implantable cardioverter-defibrillator indicating double counting due to T wave oversensing (arrows) followed by an inappropriate shock inducing ventricular fibrillation and successful termination by a subsequent appropriate shock.
Fig. 2.
Resting and exercise test electrocardiograms. 12-lead surface electrocardiogram and subcutaneous implantable cardioverter-defibrillator (S-ICD) electrograms at rest (left) and during a treadmill exercise test (right). A – 12-lead surface electrocardiogram indicating new right bundle branch block during exercise (not present at rest). B – S-ICD electrogram from the primary sensing vector indicating a change in QRS-T wave morphology with exercise (similar to QRS-T wave morphology prior to the inappropriate shock, Fig. 1). C – S-ICD electrogram from the secondary sensing vector indicating that QRS-T wave morphology does not change significantly with exercise.
2. Discussion
The S-ICD is a recently introduced technology for the prevention of sudden cardiac death with clinical trial-supported efficacy [1]. The advantage of the S-ICD is that it is entirely subcutaneous, avoiding the need for transvenous leads and their associated complications. As the leads are extracardiac, sensing and programming differ compared to those of the transvenous ICD (T-ICD), posing new challenges. Currently, this device should be considered for patients with an indication for ICD when pacing therapy for bradycardia support, cardiac resynchronization, or antitachycardia pacing is not necessary. The S-ICD could be especially considered for young patients, those at high risk for bacteremia (due to indwelling catheters/hardware or immunocompromised states), and those with difficult venous access [2].
The 360-day rate of inappropriate shocks observed in the EFFORTLESS S-ICD Registry was 7% [1]. With T-ICDs, supraventricular tachycardias account for the majority of inappropriate shocks [3], whereas with the S-ICD, oversensing (especially TWOS) is the primary cause of inappropriate shocks [1]. These findings align with those of a simulation study comparing single- and dual-chamber ICD algorithms to the S-ICD conditional zone discriminator algorithms based on morphology and R/T ratio, which were more specific for supraventricular arrhythmia discrimination than the manufacturers’ T-ICD algorithms [4]. However, because the S-ICD relies on “far-field” electrograms (resembling a surface electrocardiogram), it may be more sensitive to QRS-T wave morphology changes compared to the local “near-field” ventricular electrograms from the T-ICD, rendering the S-ICD more prone to TWOS. Further, the S-ICD has a fixed sensing algorithm that can only be adjusted by changing the therapy zone frequency or by changing the sensing vector and stored template. TWOS incidence in T-ICDs has decreased over time due to the development of several algorithms for filtering and rectification, minimum sensing threshold, automatic sensitivity adjustment, and T wave rejection [5]. Even so, TWOS still induces inappropriate shocks in 1–3.8% of T-ICD recipients, depending on underlying etiology [6], [7].
Rate-dependent RBBB is not commonly observed during routine clinical exercise testing [8]. In the S-ICD, when new RBBB arises, the QRS-T wave morphology recorded by the device may also change. In this case, the R/T wave ratio may decrease to a threshold where the T wave is above the sensing decay curve following R wave detection and is therefore counted by the device׳s detection algorithm. In our case, analysis of the stored event indicated a change in QRS-T wave morphology and TWOS prior to the inappropriate shock, a phenomenon that was reproduced in the subsequent exercise test but not in the first exercise test, as the patient was unable to achieve maximal exercise capacity. This case highlights the difficulties in preventing oversensing due to dynamic changes in the QRS-T wave morphology and the importance of performing a full exercise test as part of the screening, ensuring that the patient reaches the maximal exercise level they may achieve in daily life.
Recently, a case of S-ICD TWOS resulting from the development of RBBB after alcohol septal ablation in a patient with hypertrophic cardiomyopathy was reported. In this case, as RBBB was persistent and R wave amplitude was low in all three sensing vectors, the authors chose to implant a new T-ICD [9]. In our case, TWOS was resolved by reprogramming the sensing vector to one unaffected by the rate-dependent RBBB.
In conclusion, despite the detection/discrimination algorithms used to avoid tachycardia misclassification, inappropriate shocks remain a complication of S-ICDs and can induce life-threatening arrhythmias. Exercise-related bundle branch block should be sought out during screening for S-ICD and patients with this abnormality should be evaluated with an exercise test after S-ICD implantation; during this test, each sensing vector should be assessed to identify the vector with the highest discrimination between R and T waves.
Conflict of interest
Dr. Maria João Sousa is awaiting approval to receive educational grants from Boston Scientific. Dr. Betts has received honoraria from Boston Scientific for teaching and speaker fees.
Funding sources
Dr Betts׳ salary is part funded by the Oxford Biomedical Research Centre.
Contributor Information
Maria João Sousa, Email: maria.sousa.101@sapo.pt, ep.doctors@ouh.nhs.uk.
Tim Betts, Email: tim.betts@ouh.nhs.uk.
References
- 1.Lambiase P.D., Barr C., Theuns D.A. Worldwide experience with a totally subcutaneous implantable defibrillator: early results from the EFFORTLESS S-ICD Registry. Eur Heart J. 2014;35(25):1657–1665. doi: 10.1093/eurheartj/ehu112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Authors/Task Force Members, Priori SG, Blomström-Lundqvist C, Mazzanti A, et al. ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J. Aug 29; 2015. pii: ehv316. [Epub ahead of print]. [DOI] [PubMed]
- 3.Daubert J.P., Zareba W., Cannom D.S. Inappropriate implantable cardioverter-defibrillator shocks in MADIT II: frequency, mechanisms, predictors, and survival impact. J Am Coll Cardiol. 2008;51(14):1357–1365. doi: 10.1016/j.jacc.2007.09.073. [DOI] [PubMed] [Google Scholar]
- 4.Gold M.R., Theuns D.A., Knight B.P. Head-to-head comparison of arrhythmia discrimination performance of subcutaneous and transvenous ICD arrhythmia detection algorithms: the START Study. J Cardiovasc Electrophysiol. 2012;23:359–366. doi: 10.1111/j.1540-8167.2011.02199.x. [DOI] [PubMed] [Google Scholar]
- 5.Swerdlow C., Asirvatham S., Ellenbogen K., Friedman P. Troubleshooting implanted cardioverter defibrillator sensing problems I. Circ Arrhythm Electrophysiol. 2014;7:1237–1261. doi: 10.1161/CIRCEP.114.002344. [DOI] [PubMed] [Google Scholar]
- 6.Guédon-Moreau L., Kouakam C., Klug D. Decreased delivery of inappropriate shocks achieved by remote monitoring of ICD: a substudy of the ECOST Trial. J Cardiovasc Electrophysiol. 2014;25(7):763–770. doi: 10.1111/jce.12405. [DOI] [PubMed] [Google Scholar]
- 7.Rodríguez-Mañero M., Asmundis C., Sacher F. T-Wave oversensing in patients with Brugada Syndrome: true bipolar versus integrated bipolar implantable cardioverter defibrillator leads – multicenter retrospective study. Circ Arrhythm Electrophysiol. 2015;8:792–798. doi: 10.1161/CIRCEP.115.002871. [DOI] [PubMed] [Google Scholar]
- 8.Stein R., Nguyen P., Abella J. Prevalence and prognostic significance of exercise-induced right bundle branch block. Am J Cardiol. 2010;105(5):677–680. doi: 10.1016/j.amjcard.2009.10.050. [DOI] [PubMed] [Google Scholar]
- 9.Van Dijk V.F., Liebregts M., Luermans J.G. Inappropriate shock due to T wave oversensing by a subcutaneous ICD after alcohol septal ablation for hypertrophic cardiomyopathy. Pacing Clin Electrophysiol. 2015 doi: 10.1111/pace.12784. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]