Abstract
Electronic cigarettes are novel tobacco products that are frequently used these days. The cartridge contains liquid nicotine and accidental poisoning, even with a small oral dose, endangers children. We present here a mortality case of a 15-month-old child who ingested liquid nicotine mistaking it for cold medicine. When the emergency medical technicians arrived, she was found to have pulseless electrical activity. Spontaneous circulation was restored after approximately 40 minutes of cardiopulmonary resuscitation. The cotinine level in her urine was 1,716 ng/mL. Despite intensive supportive care, severe anoxic brain injury was found on computed tomography and the child ultimately died. This fatality highlights the need for public health efforts to minimize such accidents.
Keywords: Liquid nicotine, E-cigarettes, Intoxication
Introduction
Electronic-cigarettes (e-cigarettes) are devices designed to deliver nicotine without tobacco smoke by heating a solution of nicotine, flavoring, additives, propylene glycol, and/or vegetable glycerine. Invented by Lik Hon in Hong Kong in 2003, e-cigarettes became available in Europe and the United States in 20061). In Korea, they were introduced in 2007 and their increased usage was driven based on the notion that they are safer than conventional nicotine delivery systems, such as cigarettes, cigars, and tobacco pipes led to their increase use2). The liquid nicotine, which is contained in e-cigarette cartridge, can be easily refilled by the user. However, as more people use e-cigarettes, there has been an increase in the number of adverse events associated with toxic exposure to liquid nicotine. E-cigarettes are now accountable for 42% of nicotine exposure related calls made to Poison Control Centers in the United States3). According to the Korea Consumer Agency, 54 adverse event related to e-cigarettes were reported by the Consumer Injury Surveillance System from January 2012 to April 2015, and more than half of them (31 cases) were related to misunderstanding and misuse of the e-cigarette liquid. Especially, three of them were children (Table 1). As there are no regulations regarding childproof bottling and packaging or warning signs on liquid nicotine products, there is an increased risk of children unintentionally ingesting liquid nicotine. We present and discuss a mortality case of a 15-month-old child who ingested liquid nicotine mistaking it for cold medicine.
Table 1. Number of adverse cases related to E-cigarette use as reported in the Consumer Injury Surveillance System.
| Year | E-cigar liquid | E-cigar device | Total | |||
|---|---|---|---|---|---|---|
| Side effect | Misusing | Child case | Device-related | Liquid | ||
| 2012 | 4 | 1 | 1 | 4 | 0 | 10 |
| 2013 | 1 | 0 | 0 | 1 | 0 | 2 |
| 2014 | 6 | 2 | 2 | 7 | 0 | 17 |
| 2015 | 9 | 5 | 0 | 8 | 3 | 25 |
| Total | 20 | 8 | 3 | 20 | 3 | 54 |
Adapted from Korea Consumer Agency (http://www.kca.go.kr/).
Case report
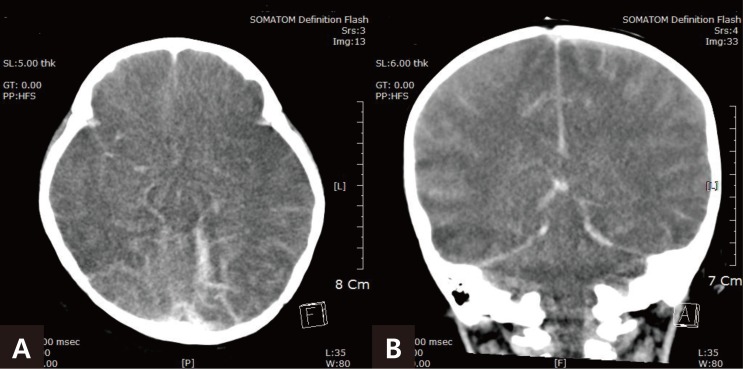
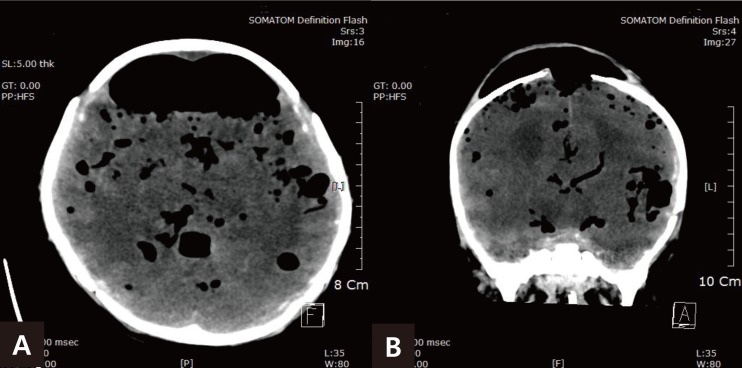
The parents of a 15-month-old female infant called 119 after their child lost consciousness. The infant had ingested 5 mL of liquid nicotine (concentration: 10 mg/mL) used to refill an e-cigarette, mistaking it for cold medicine. She involuntary vomited immediately after ingestion but lost consciousness and was unresponsive. When the emergency medical technicians arrived, she was pulseless, and cardiopulmonary resuscitation (CPR) was performed before she was transferred to the hospital. After 40 minutes of CPR, she had a spontaneous return of circulation. Intubation and mechanical ventilation was applied and vasopressor drugs were administered to maintain blood pressure. Her vital signs at the time of admission to the intensive care unit (ICU) were as follows: blood pressure, 80/50 mmHg; pulse rate, 122 beats/min; and body temperature, 36℃. She weighed 12 kg (50th–75th percentile), and her height was 85 cm (20th–50th percentile). On physical examination, both pupils were fixed and dilated at 8 mm, and fecal incontinence was noticed. There was no response to sound or painful stimuli, and her hands and feet were pale and clammy. Initial laboratory studies revealed metabolic acidosis with pH 7.131 and base excess −10.8 mEq/L; a hepatic failure with aspartate transaminase and alanine transaminase levels of 801 IU/L and 452 IU/L, respectively. The cotinine level in urine measured 12 hours after admission to ICU using enzyme immunoassay was significantly elevated to 1,716 ng/mL. Electroencephalography (EEG) showed diffuse cerebral dysfunction with an alpha coma pattern. A diffusely decreased density of the cerebral cortex with severe brain edema was noted on the computed tomography (CT) scan, which was performed on the 5th hospital day (HD) (Fig. 1). After admission to the ICU, supportive treatments, such as mannitol, dexamethasone, inotropic agents, antidiuretic hormone, and antibiotics, were administered to maintain vital signs and to control infections. Despite these treatment, brain edema progressed and brain herniation with leakage of cerebrospinal fluid through the posterior fontanelle was noted the 23rd HD. A follow-up CT scan showed pneumocephalus with diffuse cerebral edema (Fig. 2). She continued to be unresponsive without self-respiration and was declared brain-dead after a follow-up EEG examination 43rd HD. Given her poor prognosis, she was transitioned to comfort care and died 44th HD.
Fig. 1. Severe cerebral edema was observed on computed tomography, which was performed on the 5th hospital day (A, axial plane; B, coronal plane).
Fig. 2. Diffuse pneumocephalus with brain herniation through the posterior fontanelle was observed on computed tomography, which was performed on the 38th hospital day (A, axial plane; B, coronal plane).
Discussion
Nicotine is isolated from the tobacco plant Nicotiana tabacum and sustains tobacco addition4). Nicotine can be rapidly absorbed through the skin, alveoli, or oropharyngeal mucosa, as well as through the gastrointestinal mucosa after inhalation, ingestion, or dermal contact5). Upon entering the arterial circulation, nicotine quickly moves to the brain6) and is subsequently transformed into inactive metabolites, such as cotinine, which is used as a liver biomarker4).
Nicotine acts on both parasympathetic and sympathetic nervous systems by binding to acetylcholine receptors. Signs and symptoms after ingestion of nicotine appear to be dose related. In general, low nicotine doses stimulate the neural and cardiovascular systems, while high doses suppress the vital systems4). Therefore, awakening effect with increased heart rate and blood pressure can be experienced at low doses7). Other early features of nicotine ingestion at mild to moderate toxic doses are a burning sensation in the mouth and throat, nausea, vomiting, abdominal pain, headache, confusion, dizziness, weakness, miosis, urination and defecation. Ingestion of higher doses leads to arrhythmias, bradycardia, convulsions, coma, respiratory failure, rapid progression to hypotension, and death8).
A lethal dose of nicotine has been estimated to be as less as 40 mg in adults and 1 mg/kg in children. However, it is recommended that children who have ingested 0.2 mg/kg or more of nicotine and who are symptomatic be referred for medical assessment9,10). In our case, the patient ingested 5 mL (50 mg) of liquid nicotine, which corresponded to a dose of 3 mg/kg higher than the lethal dose which directly caused cardiopulmonary arrest and hypoxic brain damage.
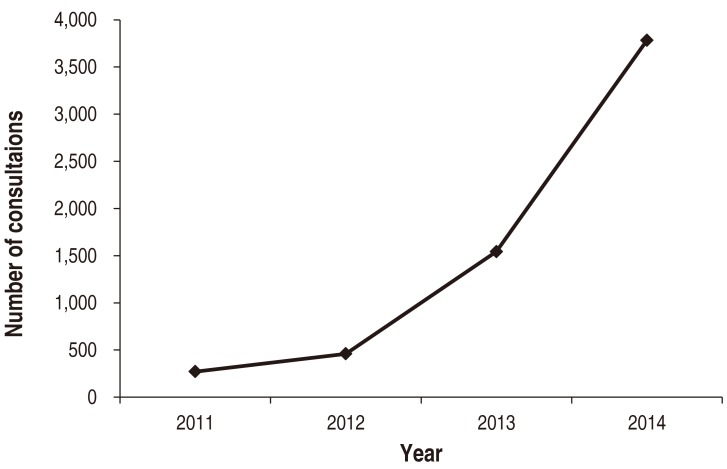
Important history taking that emergency physician should ask of the child's caregiver are the time of ingestion, the amount swallowed, whether the ingestion was witnessed or unwitnessed, whether the child has vomited since the time of ingestion, and whether any signs of seizure activity have been observed. Treatment of liquid nicotine poisoning is usually supportive. At Emergency Department arrival, immediate treatment should be initiated focusing on stabilizing the patient and correcting any life-threatening symptoms, possibly including respiratory support with mechanical ventilation. Anticholinergic drugs can be administered to counteract effects such as bradycardia, bronchorrhea, excessive salivation, and wheezing. Use of activated charcoal is an option for patients who present within 1 hour of ingestion, but it is infrequently used because of concerns about spiration. Gastric lavage may be initiated if recommended by poison control experts. Antiemetic medications could be administered who presents with nausea and vomiting. Benzodiazepines and barbiturates can be used to control seizures. Although hypertension and tachycardia in the initial phase are usually treated with adrenergic antagonists, this treatment is not recommended. Hemodialysis does not remove nicotine from the bloodstream and it is not recommended11). According to the American Association of Poison Control Centers, the number of consultations related to e-cigarette nicotine exposure has been increasing each year (Fig. 3). In particular, it has doubled from 2013 to 2014. Although the incidence of serious outcome is less than 0.1% of all cases, a majority of serious cases occur in children under 5 years (Table 2)12).
Fig. 3. The number of consultations related to E-cigarette nicotine exposure has been increasing year by year. This data was provided by the American Association of Poison Control Center.
Table 2. Number of consultations related to E-cigarette nicotine exposure according to age group.
| Age (yr) | E-cigar device | E-cigar liquid |
|---|---|---|
| ≤5 | 701 (52.7) | 111 (67.3) |
| 6–12 | 27 (2.0) | 5 (3.0) |
| 13–18 | 74 (5.6) | 5 (3.0) |
| ≥19 | 440 (33.1) | 35 (21.2) |
| Unknown | 88 (6.6) | 9 (5.5) |
| Total | 1,330 (100) | 165 (100) |
Values are presented as number (%).
Adapted from National Poison Data System 2013 Annual Report (http://www.aapcc.org/annual-reports/).
According to the Korean Toxic Chemicals Control Act, e-cigarette nicotine content of more than 1% is classified as a hazardous chemical substance, toxic agent, and the container must indicate the name of the substance, pictorial symbols, signals, risks, safety phases, preventive measures, and provider information. However, according to a report published by the Korean Consumer Agency in 2015, 6 of 9 mixed products (66%) and 3 of 16 undiluted liquid nicotine products (18%) did not even specify the name of the substance on the container. Furthermore, 91% and 87% of all liquid nicotine products had no pictorial symbols and warning, respectively13). In most cases, warning signs were difficult to recognize due to fine prints, being written in a foreign language, or positioning on the container. Moreover, 75% of undiluted liquid nicotine products had containers that resembled those of eye drops, causing possible confusion for the user (Fig. 4). The National Health Promotion Act prohibits using phrases, images, or photos indicative of food or flavor on nicotine products except for cigarettes. However, some liquid nicotine products had images of fruit on the container to emphasize their flavor13). Therefore, there are at high risks for unintentional ingestion of nicotine products, as in our case where liquid nicotine was mistaken for cold medicine because there was no labeling on the container.
Fig. 4. Without proper labeling, containers of liquid nicotine (A) and eye drops (B) are similar.
In conclusion, the use of e-cigarettes is increasing with little awareness of liquid nicotine's toxicity. Even though we attempted all means to maintain the child's vital signs, hypoxic brain damage was fatal and irreversible. Although serious events or fatal overdoses of this agent have rarely been reported, even a small dose which is fatal to children can lead to death, as in our case. Therefore, efforts should be made to increase public awareness nicotine toxicity to prevent such accidents.
Footnotes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Hajek P, Etter JF, Benowitz N, Eissenberg T, McRobbie H. Electronic cigarettes: review of use, content, safety, effects on smokers and potential for harm and benefit. Addiction. 2014;109:1801–1810. doi: 10.1111/add.12659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Farsalinos KE, Polosa R. Safety evaluation and risk assessment of electronic cigarettes as tobacco cigarette substitutes: a systematic review. Ther Adv Drug Saf. 2014;5:67–86. doi: 10.1177/2042098614524430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gill N, Sangha G, Poonai N, Lim R. E-cigarette liquid nicotine ingestion in a child: case report and discussion. CJEM. 2015;17:699–703. doi: 10.1017/cem.2015.10. [DOI] [PubMed] [Google Scholar]
- 4.Jun YJ, Kim H, Park S. Suicidal death by nicotine poisoning. Korean J Leg Med. 2014;38:167–170. [Google Scholar]
- 5.Solarino B, Rosenbaum F, Riesselmann B, Buschmann CT, Tsokos M. Death due to ingestion of nicotine-containing solution: case report and review of the literature. Forensic Sci Int. 2010;195:e19–e22. doi: 10.1016/j.forsciint.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 6.Benowitz NL. Pharmacology of nicotine: addiction, smoking-induced disease, and therapeutics. Annu Rev Pharmacol Toxicol. 2009;49:57–71. doi: 10.1146/annurev.pharmtox.48.113006.094742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benowitz NL. Clinical pharmacology of nicotine: implications for understanding, preventing, and treating tobacco addiction. Clin Pharmacol Ther. 2008;83:531–541. doi: 10.1038/clpt.2008.3. [DOI] [PubMed] [Google Scholar]
- 8.Lavoie FW, Harris TM. Fatal nicotine ingestion. J Emerg Med. 1991;9:133–136. doi: 10.1016/0736-4679(91)90318-a. [DOI] [PubMed] [Google Scholar]
- 9.Gupta S, Gandhi A, Manikonda R. Accidental nicotine liquid ingestion: emerging paediatric problem. Arch Dis Child. 2014;99:1149. doi: 10.1136/archdischild-2014-306750. [DOI] [PubMed] [Google Scholar]
- 10.Mayer B. How much nicotine kills a human? Tracing back the generally accepted lethal dose to dubious self-experiments in the nineteenth century. Arch Toxicol. 2014;88:5–7. doi: 10.1007/s00204-013-1127-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Normandin PA, Benotti SA. Pediatric emergency update: lethality of liquid nicotine in e-cigarettes. J Emerg Nurs. 2015;41:357–359. doi: 10.1016/j.jen.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 12.Appleton S. Frequency and outcomes of accidental ingestion of tobacco products in young children. Regul Toxicol Pharmacol. 2011;61:210–214. doi: 10.1016/j.yrtph.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 13.Korea Consumer Agency. Study on the electronic cigarette safety and awareness [Internet] Eumseong: Korea Consumer Agency; c2013. [cited 2015 May 5]. Available from: http://www.kca.go.kr. [Google Scholar]