Abstract
Background
The ideal vaginoplasty must be successful functionally as well as have a natural appearance, and also must retain its functionality and appearance over the long term. Conventional vaginoplasty techniques have functional limitations and are associated with recurrent complications, but rectosigmoid vaginoplasty is known to have a high satisfaction rate due to its functional similarity with the vagina. We conducted the present study to assess the usability of rectosigmoid vaginoplasty over the course of long-term follow-up.
Methods
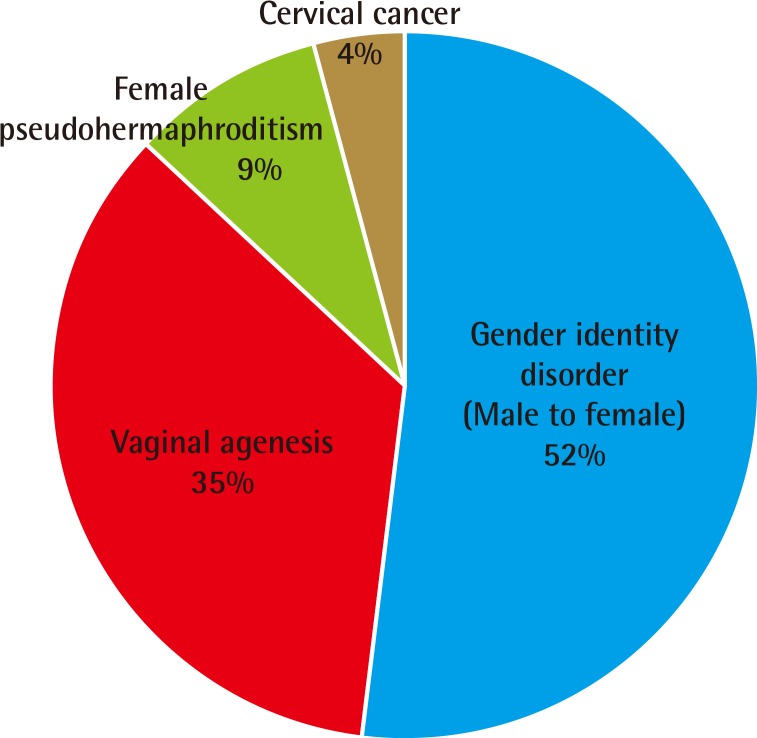
From March 1992 to February 2014, 84 patients were treated with rectosigmoid vaginoplasty; 44 had gender identity disorder, 29 had vaginal agenesis, 8 had female pseudohermaphroditism, and 3 had gynecologic malignancies after radical pelvic surgery. This retrospective study was based on a review of the patients' records, clinical examinations, complications, and questionnaires about appearance, function, and sexual intercourse.
Results
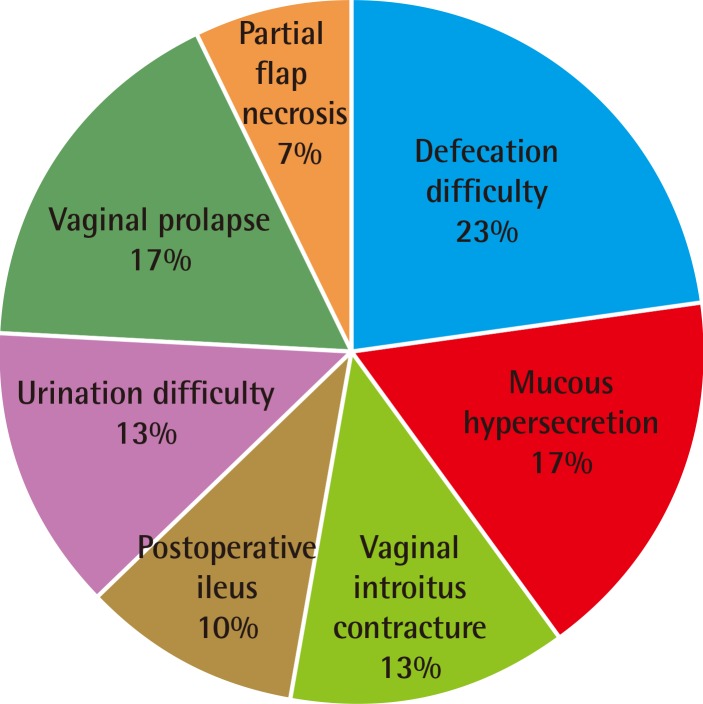
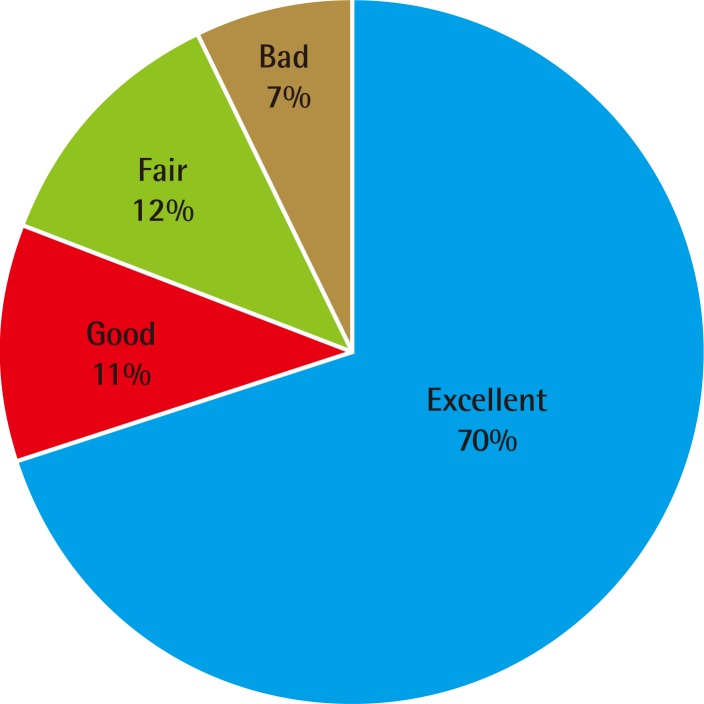
All patients who underwent rectosigmoid vaginoplasty were discharged within 2 weeks without surgical flap loss. The early complications were partial flap necrosis, difficulty in defecation, mucous hypersecretion, and postoperative ileus. The late complications were vaginal introitus contracture, vaginal prolapse, and difficulty in urination. The mean length and diameter of the neovagina 3.4 years after rectosigmoid vaginoplasty were 13.2 cm and 3.8 cm, respectively. On questionnaires about satisfaction, 70% of patients reported excellent satisfaction, 11% good, 12% fair, and 7% poor.
Conclusions
Rectosigmoid vaginoplasty is useful, safe, and well-accepted operative method with good functional and cosmetic results, such as natural lubrication and adequate vaginal length and width obtained without requiring the use of a dilator.
Keywords: Gender identity, Vagina, Surgical flap
INTRODUCTION
For many years, reconstruction of the female genitalia has been performed. Diverse methods are used for patients with vaginal agenesis, also known as Mayer-Rokitansky-Küster-Hauser syndrome; male pseudohermaphroditism; gender identity disorder; and for patients whose vagina has been removed due to a gynecologic neoplasm.
The methods of vaginal reconstruction include non-surgical treatment using vaginal expanders and surgical treatments, such as full-thickness skin grafts, split-thickness skin grafts, local flaps such as labial flaps, and penoscrotal vaginoplasty, which is used for gender identity disorder patients. Special materials are also used, such as peritoneum, bladder mucosa, amnion, and oxidized regenerated cellulose fabric. However, these surgical methods require the use of expanders or stents to prevent canal obstruction, and other complications, such as stenosis, contracture, and unpleasant odor may arise [1,2].
On the contrary, vaginal reconstruction using the rectosigmoid colon does not require expanders, since the use of the entire layer of the colon minimizes the chances of contracture. The reconstructed vaginal length and width are compatible with sexual intercourse. The texture is also similar to the normal vagina, and the natural lubrication gives satisfaction to patients with respect to the functional and aesthetic results [3].
Although reconstruction of the female genitalia using the rectosigmoid colon is effective because it has many advantages, No studies have reported the complications and viability of rectosigmoid vaginoplasty over the long term. Therefore, the authors of this paper analyzed the records of 84 patients who underwent rectosigmoid vaginoplasty over the course of 23 years to identify complications and characterize the long-term outcomes.
METHODS
We analyzed and retrospectively collected the medical records of patients who underwent rectosigmoid vaginoplasty in our medical center between March 1992 and February 2014. A total of 84 patients were included in this study, and the sample was composed of 44 gender identity disorder patients, 29 patients with vaginal agenesis, 8 female pseudohermaphroditism patients, and 3 patients with cervical cancer who had undergone radical hysterectomy (Fig. 1). The patients ranged in age from 23 to 47 years, with a mean age of 28 years. The observation period ranged from 0.5 years to 20 years, with a mean observation period of 3.4 years. The surgeon resected the part of the rectosigmoid colon where blood is supplied from the branch of the inferior mesenteric artery. The resected colon was descended to the vaginal canal, and the upper part was sutured and the lower part was anastomosed to the perineal or penile flap. Physical examinations, including measurements of the length and width of the newly reconstructed vagina, were performed during follow-up visits 1, 6, and 12 months after the procedure. Subsequently, annual physical examinations were conducted. The definition of vaginal width was the greatest distance between the two endpoints of the vaginal orifice. The vaginal length was defined as the distance from the vaginal orifice to the reconstructed vaginal vault.
Fig. 1. Characteristics of the study group.
The study group consisted of patients with gender identity disorder (male to female), vaginal agenesis, female pseudohermaphroditism, and cervical cancer.
We surveyed the operative method and complications using patient records, and interviewed the patients directly to inquire about any recent medical conditions. The patients were surveyed about their functional or aesthetic satisfaction with the newly reconstructed vagina, the presence of any complications, and orgasm or pain associated with sexual intercourse.
RESULTS
All patients were discharged from the hospital within 2 weeks without severe complications. During the follow-up period, no flaps showed total necrosis. A variety of complications occurred in 30 cases. Eleven cases only required a simple surgical intervention. The others required additional treatment.
Seven patients (23%) experienced difficulty in defecation, 5 (17%) experienced excessive mucous secretion, 3 (10%) experienced transient ileus, and 2 (7%) experienced partial necrosis of the rectosigmoid flap. The late complications included 5 cases of vaginal prolapse (17%), 4 cases of introitus contracture (13%), and 4 cases of micturition difficulty (13%) related to ureteral contracture (Fig. 2). According to the survey, constipation, frequent defecation, and urgent defecation occurred within 3 months of the surgery, and these symptoms all improved with time. Excessive mucous secretion, which is a common complication of rectosigmoid vaginoplasty, improved within 3 months. This symptom lasted longer in a few patients, but showed a clear decrease by approximately a year after surgery. Postoperative ileus was a common complication, but conservative care brought spontaneous relief. Four patients showed contracture of the vaginal introitus, and correction was performed with a multiple Z-plasty and local flap. In 4 of the 5 vaginal prolapse patients, the problem was resolved by excising the prolapsed mucosa and fixating it to the vaginal wall. One patient with severe vaginal prolapse had to undergo a second abdominal operation to ascend the rectosigmoid flap. Four patients suffered from voiding difficulty due to partial stenosis of the urethral orifice. Symptoms did not subside in 2 of these 4 patients, and they underwent excision and suture of the stricture site.
Fig. 2. Complications after rectosigmoid vaginoplasty.
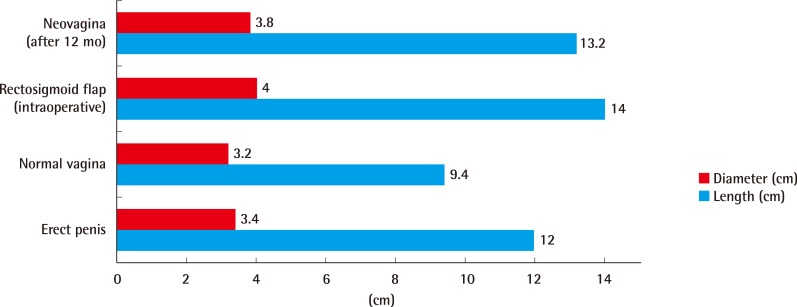
At a long-term (12-month) follow-up, the length of the vagina ranged from 11.3 to 15 cm, with a mean of 13.2 cm, which was not significantly different from the original length (14 cm). The width of the vagina ranged from 3.5 to 4.2 cm, with a mean of 3.8 cm, which was also similar to the original width (4 cm) (Fig. 3).
Fig. 3. Size of the rectosigmoid flap and neovagina.
A total of 79 patients had sexual intercourse after surgery, of whom 72 experienced orgasm. Two of these patients had mild intermittent abdominal pain, 6 had long-lasting abdominal pain, and 6 experienced a small amount of vaginal bleeding after intercourse. These symptoms appeared within 6 months of surgery and improved without further surgical treatment.
The survey showed that 59 patients (70%) reported excellent satisfaction after rectosigmoid vaginoplasty, 9 patients (11%) reported good satisfaction, 10 patients (12%) reported fair satisfaction, and 6 patients (7%) reported poor satisfaction. Overall, over 80% of patients reported being satisfied with the outcomes of rectosigmoid vaginoplasty (Fig. 4).
Fig. 4. Patient satisfaction after rectosigmoid vaginoplasty (%).
DISCUSSION
Vaginoplasty using a bowel segment has been continually researched and improved since it was developed by Baldwin [4] in 1904. The rectum, ileum, and sigmoid colon are compatible for vagina substitutes because once the vagina is made, they are covered with bowel mucosa, which lubricates the vaginal canal. Moreover, the vaginal length and width are well preserved in this technique. Vaginal stents are not needed for a long time in the prevention of contracture because introitus contracture in rectosigmoid vaginoplasty is uncommon [5]. Additionally, many studies have confirmed that rectosigmoid vaginoplasty leads to sufficient vaginal length, natural lubrication, and the possibility of early sexual intercourse [6].
However, this surgical approach has clear drawbacks. One of them is that it requires bowel surgery, which is associated with dangerous complications such as peritonitis and intestinal obstruction. In addition, patients can suffer from complications, such as a fistula at the anastomosed site, vaginal prolapse, and excessive lubrication that causes patients to frequently change pads [7]. Excessive mucosal secretion through the vagina is the most common complication, but this usually resolves within 6 months after surgery; in our patient cohort, this symptom persisted for a year in only 2 cases [7,8,9,10,11]. Ileus after bowel surgery is known to develop in 50% of cases, but in our hospital, only 10% of patients showed transient ileus, and all of them recovered with conservative care. Difficulty in defecation, which is caused by contracture around the anastomosed site of the bowel segment, resolved with time. Three months after surgery, no particular difficulty was experienced by our patients. Most of the complications were solved with only conservative care, but some complications needed surgical treatment. Two patients had partial flap loss, requiring re-anastomosis of the necrotized area. In cases of vaginal introitus contracture, although it is a very rare complication, it was necessary to correct the condition by excision, Z-plasty, and a local flap when expanders failed to alleviate the condition. In our hospital, 5 patients suffered from vaginal prolapse. This occurs due to the extensive flap length and incomplete fixation of the proximal end of the flap. It is corrected by resecting the prolapsed mucosa and fixating it firmly to the vaginal wall. Most of the cases were repaired by this procedure, but in 1 patient, an abdominal resection had to be performed to ascend and fix the prolapsed flap. Although difficulties in micturition resolved with time, resection of the obstructed area and simple suturing had to be performed when symptoms did not subside. During the follow-up period, patients complained of scars on their abdomen, although scar-reducing ointment and scar revisions were used. However, laparoscopy-assisted surgery dramatically reduced scars to a size of <1 cm. These patients also recovered faster and were discharged from the hospital 3 days sooner than the former group.
The average length of the rectosigmoid flap in this research was 14 cm. In long-term follow-up observations, the length of the vagina was found to have slightly decreased to 13.2 cm. The average width of the rectosigmoid flap was 4 cm, and we observed no contracture during the follow-up period; the width was only reduced to 3.8 cm [7]. In addition, the newly reconstructed vagina was longer than the normal female vagina (9.4 cm on average), and was strong enough to endure penile insertion [12,13,14]. Seventy-nine of the 84 patients we interviewed had sexual intercourse, and 72 of them were able to experience orgasm. This implies that rectosigmoid vaginoplasty is suitable for sexual intercourse and brings satisfying results with respect to sexual pleasure. Infrequent complications, such as postcoital pain and vaginal spotting, were reported, but most of these complications improved within 6 months. Sufficient vaginal length should be considered to avoid postcoital pain, which can persist due to vaginal introitus contracture or short vaginal length.
This research has limitations in terms of patient selection. The length and width of the vagina are objective evaluation tools, but since gender identity disorder patients and vaginal agenesis patients have different perineal anatomy, patients' expectations and satisfaction after surgery can differ depending on the patient group [15]. In light of the postoperative vaginal structure and function, rectosigmoid vaginoplasty is thought to be an efficient method of female vaginal reconstruction. Hence, this research did not take into account differences among patient groups.
This study showed that rectosigmoid vaginoplasty resulted in adequate vaginal length and width for sexual intercourse, and had aesthetically and functionally satisfactory outcomes over the long term. Moreover, no stents or dilator was needed postoperatively, natural lubricant prevented discomfort, and most of the complications resolved with time. Finally, laparoscopy-assisted bowel surgery resulted in minimal scarring on patients' abdomens and minimized the risk of infection during surgery. This implies that rectosigmoid vaginoplasty is still a useful surgical option for female vaginal reconstruction [16].
Footnotes
This study was supported by research funds from Dong-A University.
No potential conflict of interest relevant to this article was reported.
References
- 1.Frank RT. The formation of an artificial vagina without operation. Am J Obstet Gynecol. 1938;35:1053–1055. [Google Scholar]
- 2.Kim SK, Jung YH. Reconstruction of the female genitalia. J Korean Soc Plast Reconstr Surg. 1996;23:804–817. [Google Scholar]
- 3.Fotopoulou C, Neumann U, Klapp C, et al. Long-term effects of neovaginal reconstruction with sigmoid loop technique on sexual function and self image in patients with gynecologic malignancies: results of a prospective study. Gynecol Oncol. 2008;111:400–406. doi: 10.1016/j.ygyno.2008.09.018. [DOI] [PubMed] [Google Scholar]
- 4.Baldwin JF. XIV. The formation of an artificial vagina by intestinal trransplantation. Ann Surg. 1904;40:398–403. [PMC free article] [PubMed] [Google Scholar]
- 5.Davies MC, Creighton SM. Vaginoplasty. Curr Opin Urol. 2007;17:415–418. doi: 10.1097/MOU.0b013e3282f0d5b3. [DOI] [PubMed] [Google Scholar]
- 6.Hensle TW, Shabsigh A, Shabsigh R, et al. Sexual function following bowel vaginoplasty. J Urol. 2006;175:2283–2286. doi: 10.1016/S0022-5347(06)00337-5. [DOI] [PubMed] [Google Scholar]
- 7.Kwun Kim S, Hoon Park J, Cheol Lee K, et al. Long-term results in patients after rectosigmoid vaginoplasty. Plast Reconstr Surg. 2003;112:143–151. doi: 10.1097/01.PRS.0000066169.78208.D4. [DOI] [PubMed] [Google Scholar]
- 8.Khen-Dunlop N, Lortat-Jacob S, Thibaud E, et al. Rokitansky syndrome: clinical experience and results of sigmoid vaginoplasty in 23 young girls. J Urol. 2007;177:1107–1111. doi: 10.1016/j.juro.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 9.Kapoor R, Sharma DK, Singh KJ, et al. Sigmoid vaginoplasty: long-term results. Urology. 2006;67:1212–1215. doi: 10.1016/j.urology.2005.12.037. [DOI] [PubMed] [Google Scholar]
- 10.O'Connor JL, DeMarco RT, Pope JCt, et al. Bowel vaginoplasty in children: a retrospective review. J Pediatr Surg. 2004;39:1205–1208. doi: 10.1016/j.jpedsurg.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 11.Karateke A, Haliloglu B, Parlak O, et al. Intestinal vaginoplasty: seven years' experience of a tertiary center. Fertil Steril. 2010;94:2312–2315. doi: 10.1016/j.fertnstert.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 12.Tan JS, Lukacz ES, Menefee SA, et al. Determinants of vaginal length. Am J Obstet Gynecol. 2006;195:1846–1850. doi: 10.1016/j.ajog.2006.06.063. [DOI] [PubMed] [Google Scholar]
- 13.Barnhart KT, Izquierdo A, Pretorius ES, et al. Baseline dimensions of the human vagina. Hum Reprod. 2006;21:1618–1622. doi: 10.1093/humrep/del022. [DOI] [PubMed] [Google Scholar]
- 14.Wylie KR, Eardley I. Penile size and the ‘small penis syndrome’. BJU Int. 2007;99:1449–1455. doi: 10.1111/j.1464-410X.2007.06806.x. [DOI] [PubMed] [Google Scholar]
- 15.Fang RH, Chen TJ, Chen TH. Anatomic study of vaginal width in male-to-female transsexual surgery. Plast Reconstr Surg. 2003;112:511–514. doi: 10.1097/01.PRS.0000070946.57378.BB. [DOI] [PubMed] [Google Scholar]
- 16.Kim C, Campbell B, Ferrer F. Robotic sigmoid vaginoplasty: a novel technique. Urology. 2008;72:847–849. doi: 10.1016/j.urology.2008.04.004. [DOI] [PubMed] [Google Scholar]