Abstract
This follow up study aims to refine the roles of previously suggested candidate genes (CC chemokine ligands or CCLs) in multiple sclerosis (MS), and to test these markers in another autoimmune disorder, systemic lupus erythematosus (SLE). After stringent correction for multiple testing, we reject the importance of previously suggested borderline associations with CCLs in MS. A new finding is the differential distribution of CCL8 marker alleles and a haplotype in extreme severity subgroups of MS. In SLE, this study reveals strong associations with a marker and a haplotype encompassing the CCL14 gene, which suggests that a lupus relevant variant may lie within or in the proximity of this haplotype. Published by Elsevier B.V.
Keywords: Multiple sclerosis, Systemic lupus erythematosus, Candidate genes, CC chemokine ligands
1. Introduction
The development of autoimmunity is defined by complex interactions among genetic and environmental factors (Perl, 2004). A genetic predisposition is suggested by disease concordance rates of 25% or higher in monozygotic twins in both organ-specific and systemic autoimmmunity such as multiple sclerosis (MS) and systemic lupus erythematosus (SLE) (Perl, 2004). The Human Leukocyte Antigen (HLA) (6p21) locus has the largest impact on susceptibility for MS (IMSGC, 2007) and SLE (Nath et al., 2004). In MS, the HLA DRB1*1501 allele appears to have the main role in Caucasians (Oksenberg et al., 2004), but epistatic interactions among alleles aligning in the DR2 (DRB1–DRB5) haplotype have functional significance (Gregersen et al., 2006) and trans interactions among DRB1 susceptibility (e.g. DRB1*15, DRB1*17, DRB1*0301) and protective (e.g. DRB1*14, DRB1*11, DRB1*01, DRB1*10) allele combinations also play a role (Ramagopalan et al., 2007). In addition, HLA locus heterogeneity also exists in MS (de Jong et al., 2002; IMSGC, 2005; Brynedal et al., 2007). A recent whole genome association (WGA) in over 12,000 subjects shows very strong associations (p=8.94×10−81) for SNPs in the DRA locus, further confirming the importance of HLA in MS (IMSGC, 2007). In SLE, the HLA-DR2 and DR3 alleles as well as Class III mutations leading to deficiency in complements 2 and 4 are important determinants of disease susceptibility (Arnett and Reveille, 1992).
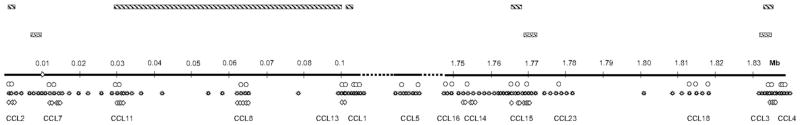
In contrast, non-HLA loci confer small risk to these disorders. Only studies in very large cohorts could conclusively identify disease variants in genes of IL2Rα (10p15) and IL7Rα (5p13) relevant for MS (Gregory et al., 2007; IMSGC, 2007; Lundmark et al., 2007). Likewise, SNPs in ITGAM (Harley et al., 2008) and STAT4 genes were recently associated with SLE (Remmers et al., 2007). CC chemokine ligand (CCL) genes control the differentiation, activation, and migration of immune cells, and their functional importance was repeatedly demonstrated in experimental autoimmune encephalomyelitis (EAE), MS (Mahad et al., 2004; Banisor et al., 2005; Savarin-Vuaillat and Ransohoff, 2007) and SLE (Wu et al., 2007; Rovin, 2008). Fourteen CCLs are encoded in 17q11.2–q12, where a meta-analysis revealed the highest non-parametric linkage in MS (The Transatlantic Multiple Sclerosis Genetics Cooperative, 2001). Quantitative trait loci of EAE were identified in regions of the mouse chromosome 11 and the rat chromosome 10, both synthenic to the human 17q11 (Teuscher et al., 1999; Jagodic et al., 2004). These observations prompted us some years ago to scan the 17q11.2–q12 region and the analyses repeatedly showed weak or moderate associations of rare SNP haplotypes encompassing CCL2, CCL11–CCL8–CCL13, CCL15 and CCL3 in MS families (Fig. 1) (Vyshkina et al., 2005; Vyshkina and Kalman, 2005, 2006).
Fig. 1.
The figure depicts the 17q11.2–q21 region (1.83 MB) with 1,508,243 bp gap between CCL1 and CCL5 and a 96,158 bp gap between CCL5 and CCL16. The lower part of the figure indicates the placing of markers in the phase I (open circles) (Vyshkina et al., 2005), phase II (open stars) (Vyshkina and Kalman, 2005) and present study (diamonds). Upper bars (striped) in the top part of the figure indicate MS-associated haplotypes in the phase I study and lower bars (dotted) indicate MS-associated haplotypes in the phase II study. Note the overlap in markers and haplotypes within the genes of CCL15 and CCL3. The main rational for the selection of the present markers was to include SNPs previously associated with MS, tagging SNPs and non-synonymous mutations in genes of interest.
In the present study, we asked if the associations of these CCL genes can be reproduced in a case–control MS cohort and if these markers also show association with SLE. In addition, we asked if the selected susceptibility markers show differential distribution in low and high severity subgroups of MS.
2. Subjects and methods
2.1. Subjects
2.1.1. Patients with MS
Genomic DNA, blood or frozen brain tissue specimens of 523 Caucasian MS patients were obtained from the Multiple Sclerosis DNA Bank (MSDB), University of California San Francisco, San Francisco, CA, Accelerated Cure Project for Multiple Sclerosis (ACPMS), Boston, MA, Multiple Sclerosis Research Center of New York (MSRCNY), New York, NY, and the Human Brain and Spinal Fluid Resource Center (HBSFRC), Los Angeles, CA. All patients had definite MS (McDonald et al., 2001) with 61% relapsing–remitting (RR)–MS, 10% primary-progressive (PP)-MS, 23% secondary progressive (SP)-MS, and 1% progressive-relapsing (PR)-MS course (SP or PP-MS was not differentiated for 5%, all postmortem cases). Information concerning course of MS, age of onset (as defined by the treating physician), age at diagnosis of MS, EDSS at the time of specimen collection, time to reach maximum EDSS, (time to death from disease onset in case of the postmortem specimens), and medications during the disease course was collected for each MS patient.
2.1.2. Patients with SLE
Genomic DNA samples from 97 Caucasian patients with SLE that satisfied the established diagnostic criteria (Tan et al., 1982) were investigated.
2.1.3. Normal controls
Buccal swab specimens of 466 Caucasian normal controls were collected from staff members, spouses of MS patients and visitors at the MSRCNY, New York.
Patients and controls had similar average age (MS patients: 46.5; SLE: 44.5; controls: 43.2). The mean age of disease onset was 35.2 years in MS and 33.8 years in SLE. The female to male ratio was 2.35 (367/156) in the MS group; 12.9 (90/7) in the SLE group and 2.61 (313/120) in the control group. Human subjects were studied in accordance with IRB and HIPAA regulations.
2.2. DNA extraction
DNA was extracted by using the Qiagen Blood DNA Mini Kit (Qiagen, Valencia, CA).
2.3. SNPs
A total of 35 SNP markers (17q11.2–q12) were included in the study after removing 4 monomorphic markers and 3 markers with Hardy–Weinberg deviation in controls (NCBI dbSNP Build 127, http://www.ncbi.nlm.nih.gov/SNP). Thirty-one of these assays were previously developed and tested by Genaissance Pharmaceuticals (now part of Cogenics, New Haven, CT) (Vyshkina et al., 2005; Vyshkina and Kalman, 2005, 2006). An additional 4 new assays were successfully validated by Cogenics for the present study. From the previously validated CCL markers we selected those for the present study which repeatedly showed association with MS in families (Vyshkina et al., 2005; Vyshkina and Kalman, 2005). Of the total 35 SNPs, 10 markers were tagging SNPs that define haplotypes (http://www.hapmap.org) and 4 were non-synonymous SNPs. The mean heterozygosity of markers was 27.1% (range 7.4%–50.5%). Fig. 1 indicates the distribution of markers in the two previous studies (Vyshkina et al., 2005; Vyshkina and Kalman, 2005) and the present analyses, and the location of haplotypes associated with the disease.
2.4. Genotyping
Cogenics, a division of Clinical Data, Inc. was contracted to perform the SNP genotyping by using the Sequenom MassAR-RAY™ System.
2.5. Analyses
Allele and genotype frequencies and heterozygosity were determined by using the Pedigree Statistics in MERLIN (Multipoint Engine for Rapid Likelihood Inference, http://www.sph.umich.edu/csg/abecasis/Merlin/) (Abecasis et al., 2002). Deviations from the Hardy–Weinberg Equilibrium (HWE) were tested by using the χ2-statistics.
For associations of marker alleles, genotypes and haplotypes, the χ2-test was used. Distribution of LD within 17q11 was evaluated by using the Haploview v.4 program (http://www.broad.mit.edu/mpg/haploview/) (Barrett et al., 2005) and LDmax (Gold) (http://www.sph.umich.edu/csg/abecasis/GOLD/docs/stats.html) (Slatkin and Excoffier, 1996). Bonferroni correction was used for multiple testing. Only a few of the selected CCL markers are in LD with each other. Taking LD among some of the CCL markers into consideration when correction is made, would not affect the outcome.
2.6. Stratification of the MS cohort
Stratification was performed by separating patients with milder (EDSS≦4 at 10 years after onset) and more severe forms of the disease (EDSS≧6 at 10 years after onset). The two subgroups are designated as “mild” and “severe” MS hereafter. Mild MS was defined here by EDSS≦4 at 10 years (instead of EDSS≦3 at 10 years conventionally used to define “benign MS”) in order to retain power. The mild subgroup included 105 and the severe subgroup included 75 patients.
3. Results
3.1. Association of SNP alleles, genotypes and haplotypes with MS and SLE
Table 1A and B shows the associations of CCL gene SNP alleles with MS and SLE. All uncorrected p<0.05 are indicated. A total of 35 CCL markers were tested, requiring an overall α-value of 0.0014 to observe significance at 0.05 level. After correction for multiple testing, only PG28 (rs854680) remains significant in the SLE group.
Table 1.
Marker allele association with MS and SLE
| A. Association with MS | |||||
|---|---|---|---|---|---|
|
| |||||
| Gene | 5′ to CCL11 | 3′ to CCL14 | Nonsyn CCL14 | ||
|
|
|
|
|
||
| Marker | PG13 | PG28 | PG29 | ||
| MS–control | χ2 | 4.34 | 4.89 | 4.23 | |
| P | 0.037 | 0.027 | 0.04 | ||
| ↑Allele | T(T/C) | A(C/A) | T(T/C) | ||
| Freq. in controls/MS | 0.850/0.882 | 0.221/0.267 | 0.936/0.958 | ||
| B. Association with SLE | |||||
|
| |||||
| Gene | Nonsyn CCL11 | 3′ to CCL14 | Nonsyn CCL15 | 5′ to CCL3 | |
|
|
|
|
|
|
|
| Marker | PG14 | PG28 | PG38 | PG46 | |
|
| |||||
| SLE–control | χ2 | 3.96 | 33.65 | 5.26 | 4.01 |
| P | 0.047 | 6.59−9 | 0.022 | 0.045 | |
| ↑Allele | G(G/A) | A(C/A) | T(C/T) | G(G/T) | |
| Freq. in controls/SLE | 0.818/0.881 | 0.221/0.460 | 0.039/0.079 | 0.633/0.713 | |
All marker alleles with a p<0.05 are indicated for CCL markers in MS (A) and SLE (B). In the row of alleles, the allele that is increased in the disease is indicated and the major and minor alleles of each SNP, respectively, are shown in parenthesis. After Bonferroni correction, only the A (minor) allele of PG28 shows significant association with SLE.
Table 2A and B indicates all uncorrected p-values <0.05 for the distribution of CCL marker genotypes in MS and SLE. After Bonferroni correction for multiple testing, only the shift towards the AA, AC genotypes of PG28 (rs854680) remains significant in the SLE cohort.
Table 2.
Marker genotype association with MS and SLE
| A. Association with MS | |||||
|---|---|---|---|---|---|
|
| |||||
| Gene | Nonsyn CCL14 | ||||
|
|
|
||||
| Marker | PG29 | ||||
| MS–control | χ2 | 6.18 | |||
| p | 0.046 | ||||
| Genotype | CC/CT/TT | ||||
| Freq. in controls | 0/0.127/0.873 | ||||
| Freq. in MS | 0.002/0.081/0.917 | ||||
| B. Association with SLE | |||||
|
| |||||
| Gene | 3′ to CCL14 | Nonsyn CCL15 | 5′ to CCL15 | 5′ to CCL15 | |
|
|
|
|
|
|
|
| Marker | PG28 | PG38 | PG39 | PG40 | |
|
| |||||
| SLE–control | χ2 | 36.6 | 6.61 | 6.97 | 6.45 |
| p | <0.0001 | 0.037 | 0.031 | 0.040 | |
| Genotype | AA/AC/CC | CC/CT/TT | AA/AT/TT | CC/CG/GG | |
| Freq. in controls | 0.037/0.368/0.595 | 0.924/0.074/0.002 | 0/0.102/0.898 | 0/0.097/0.903 | |
| Freq. in SLE | 0.127/0.667/0.206 | 0.843/0.157/0 | 0.012/0.151/0.837 | 0.11/0.135/0.854 | |
All SNP genotype associations (p<0.05) with MS (A) and SLE (B) are indicated. After correction for multiple testing, significant deviation only in the PG28 genotype distribution is noted in SLE patients as compared to controls.
We also analyzed association of SNP haplotypes with MS and SLE. Only observations significant after correction for multiple testing are shown in Table 3. A total of 13 two-marker haplotypes were tested within regions of allelic associations. Each marker pair may generate 3 independent haplotypes, bringing the total number of independent testing to 39 in two groups (39 tests). This number of comparisons would require an α-value of 0.0013 to observe significance at 0.05 level. While several haplotypes within CCL11, CCL8, CCL14, CCL15 and CCL3 show borderline associations with MS (where we previously detected associations in families), none of the associations could survive Bonferroni correction (data not shown). There is only a two-marker haplotype of PG28–PG29 encompassing CCL14 that remains significant after correction for multiple testing in the SLE group (Table 3). PG28 (rs854680) is located 1641bp from the 3′ UTR of the CCL14 gene. PG29 (rs16971802) is a non-synonymous SNP (C → T) in exon II of the CCL14 gene, which changes glutamine → lysine at protein level. Further extension of this haplotype into the CCL4 gene (PG28–PG29–PG30–PG31–PG32) also reveals a significant association (Table 3).
Table 3.
Association of SNP haplotypes with SLE
| Association with SLE | |||||
|---|---|---|---|---|---|
|
| |||||
| Gene | Haplotype markers | Haplotype | Haplotype frequency in controls/SLE | SLE–control | |
|
| |||||
| χ2 | P | ||||
| 3′ to CCL14-nonsyn CCL14 | PG28–PG29 | CT | 0.764/0.600 | 20.68 | 5.44−6 |
| AT | 0.173/0.315 | 19.26 | 1.14−5 | ||
| 3′ to CCL14-5′ to CCL14 | PG28–PG29–PG30–PG31–PG32 | CTAAG | 0.687/0.544 | 13.18 | 3.00−4 |
| ATAAG | 0.092/0.188 | 13.88 | 2.00−4 | ||
Haplotypes of PG28–29 and PG28–29–30–31–32 show significant associations with SLE, while none of the haplotypes are associated with MS (data not shown) after correction for multiple testing. The PG28–29 haplotype defined by the A–T alleles, and the PG28–PG29–PG30–PG31–PG32 haplotype defined by the A–T–A–A–G alleles are increased in SLE.
3.2. Association of marker alleles and haplotypes with severity of MS
Distributions of all 35 markers were tested in the mild and severe subgroups of MS and then haplotypes of markers within CCL8 with p<0.006 were analyzed. Significant differences in the distribution of two-marker haplotypes in the CCL8 gene were observed after correction for multiple testing (6 two-marker haplotypes tested within CCL genes; 3 independent haplotypes for each marker combination; required α-value≤0.003) (Table 4). The CGC allele combination of the three-marker PG19–PG22–PG23 haplotype was also increased in the severe and decreased in the mild subgroup of MS. None of the other investigated markers or haplotypes segregated differentially with severity subgroups of MS. Comparisons of marker alleles and haplotypes in the PP-MS/PR-MS vs. RR-MS/SP-MS subgroups were unrevealing.
Table 4.
Association of CCL haplotypes with severity of MS
| Gene | Haplotype markers | Haplotype | Haplotype frequency in: controls/severe MS/mild MS | χ2 | P |
|---|---|---|---|---|---|
| 5′ to CCL8-intron CCL8 | PG19–PG22 | CG | 0.170/0.230/0.112 | 8.95 | 0.003 |
| Intron CCL8 | PG22–PG23 | AT | 0.822/0.767/0.890 | 9.75 | 0.002 |
| GC | 0.178/0.233/0.110 | 8.47 | 0.002 | ||
| Intron CCL8-synon CCL8 | PG23–PG24 | TA | 0.823/0.777/0.890 | 8.47 | 0.004 |
| CC | 0.177/0.223/0.110 | 8.47 | 0.004 | ||
| 5′ to CCL8-intron CCL8 | PG19–PG22–PG23 | CGC | 0.175/0.230/0.110 | 9.37 | 0.002 |
| Intron CCL8-synon CCL8 | PG22–PG23–PG24 | ATA | 0.825/0.770/0.890 | 9.38 | 0.002 |
| GCC | 0.175/0.223/0.110 | 8.47 | 0.004 |
The CGC allele combination of PG19–PG22–PG23 is increased in the severe and decreased in the mild subgroup of MS.
4. Discussion
4.1. Candidate genes of inflammation
A phenotypic characteristic of MS is heterogeneity defined by various balances of inflammation and neurodegeneration (Lucchinetti et al., 2000; Bielekova et al., 2005). Neurodegeneration is the major pathological correlate of disability (Zivadinov and Bakshi, 2004), and inflammation can both directly and indirectly contribute to it (Bielekova et al., 2005). These observations influenced our inflammatory candidate gene selection in two earlier studies that revealed modest but reproducible observations for variants of CCL genes (Vyskina et al., 2005a; Vyshkina and Kalman, 2005, 2006). These previous SNP association studies were performed in independent cohorts of 257 and 361 MS families with various structures, and in consensus suggested haplotypes (but not individual markers) associated with the disease (Fig. 1). Associations with two rare haplotypes in CCL15 were significant in the TRANSMIT analyses even after correction for multiple testing, and MS-associated haplotypes within both CCL15 and CCL3 overlapped in the phase I and phase II studies (Vyshkina et al., 2005; Vyshkina and Kalman, 2005). Here we aimed to conclude our analyses concerning these candidate markers in MS, and to generate comparative data in another autoimmune disease, SLE.
4.2. Present findings in MS
4.2.1. SNP markers in CCL genes tested in MS
In the present cohort of 523 MS patients and 466 controls, we only detected weak p-values for associations with previously highlighted markers and haplotypes, which all became non-significant after Bonferroni correction. Assuming a genotypic relative risk of 1.3 for heterozygous and 1.8 for homozygous state of the high risk allele with 0.20 frequency, we had 73% power to detect a p= 0.05, while we had 80% power for risk alleles with 0.25 frequency and only 30% power for risk alleles with 0.05 or lower frequency (Purcell et al., 2003). Therefore, this study unambiguously excluded the association of the tested gene markers with MS since most markers had an allele frequency of 0.2 or higher. However, it is important noting that no direct marker only haplotype associations were detected in the previous CCL studies, and the frequency of all CCL haplotypes which showed association with the disease was very low (0.02) (Vyshkina et al., 2005; Vyshkina and Kalman, 2005). Therefore, the present study is in agreement with the data of the recent WGA study that revealed no significant p-values in the proximity of our CCL gene markers (IMSGC, 2007). The biological significance of previously detected associations of MS with low frequency haplotypes in CCL15 and CCL3 genes remains uncertain (Vyshkina et al., 2005; Vyshkina and Kalman, 2005).
4.2.2. Candidate markers in subgroups of MS
Testing the distribution of all CCL markers in the PP-MS/PR-MS vs. RR-MS/SP-MS subgroups resulted in no significant observation. However, stratification of MS patients into mild and severe subgroups revealed a differential distribution of a PG19–PG22–PG23 haplotype within the CCL8 gene. The severe subgroup had an increased frequency of the C–G–C haplotype, suggesting that these variants may increase the probability of developing a more rapidly progressing form of MS. CCL8 is highly expressed by astrocytes and microglia in active plaques and attracts CCR2, CCR3 and CCR5 positive monocytes and macrophages to lesions of MS and EAE (McManus et al., 1998; Banisor et al., 2005). The CCL8–CCR2 interaction was suggested to be involved in the fine tuning of immune response (O’Boyle et al., 2007). Therefore, the differential distribution of the CCL8 haplotype may result in a differential immune modulatory effect in extreme severity subgroups of MS. We could not evaluate the marker distribution in more polarized severity subgroups because of the loss of power (e.g. using EDSS≦3 at 10 years for defining mild MS would have included only 20 patients).
Identifying disease modifying genes in MS has been impeded by several methodological difficulties (e.g. definition of outcome measures and selection of markers, cohort size and composition, methods of analyses) (Kantarci et al., 2002). Numerous disease modifier candidates have been proposed, but only the HLA Class II variants have thus far survived scrutiny (Kantarci et al., 2002). HLA DR alleles have a differential distribution in mild and severe subgroups of MS (Barcellos and Thomson al., 2003; DeLuca et al., 2007; Ramagopalan et al., 2007), and epistatic interactions between HLA DR2 alleles in LD with each other determine clinical disease severity by differentially controlling T cell activation (Gregersen et al., 2006). The disease modifying role of ApoE4 is still being debated (Ramagopalan et al., 2007). This study suggests a new potential disease modifying candidate.
4.3. Findings in SLE
4.3.1. CCL gene SNP markers in SLE
None but one of the tested markers showed association with SLE. The associations of PG28 (1641 bp from 3′ UTR of CCL14) and the PG28–PG32 haplotype with SLE are novel findings, and the p-values are impressive considering the small size of the patient cohort. Among the markers defining this haplotype only PG29 (rs16971802) is a non-synonymous mutation. The current marker selection only allows a partial evaluation of LD in this region, but our preceding analyses with evenly distributed 232 markers in 17q11.2–q12 showed a large LD block encompassing CCL14–CCL15–CCL23–CCL18–CCL3–CCL4 (Vyshkina et al., 2005). PG28–PG32 are located in this extensive LD block suggesting that a lupus relevant mutation may lie within or in the proximity of this haplotype, possibly within the CCL14 gene itself. CCL14 (HCC-2) was characterized at DNA, mRNA and protein levels only recently (Pardigol et al., 1998), and its involvement in human diseases is still being explored. CCL14 binds to multiple CC chemokine receptors (CCR) including CCR1, CCR3 and CCR5 (this latter is a HIV-1 co-receptor). It may have functional significance in inhibiting HIV entry into CCR5 expressing cells (Blain et al., 2007) and controlling allergic airway inflammation and growth of cancer (Gupta et al., 2008). CCL14 has never been implicated in MS, and this is the first time when an association was detected in this region with SLE. However, a polymorphism in CCR5 was associated with SLE (Mamtani et al., 2007), which further supports a potential role for the CCL14–CCR5 axis in lupus. CCL14 may represent one of the susceptibility genes in the 17p12–q11 region that has been considered a susceptibility locus in SLE (Johansson et al., 2004).
In summary, identification of non-HLA susceptibility markers in MS is hampered by their small effects and a genetic heterogeneity of the disease underscored by recent studies in very large cohorts (Gregory et al., 2007; IMSGC, 2007; Lundmark et al., 2007). In the present follow up study, we excluded a major importance of CCL variants in MS. However, the increased frequency of the PG19–PG22–PG23 C–G–C haplotype (CCL8) in the severe and its decreased frequency in the mild subgroup of MS is a new finding which may have functional relevance and merit further evaluation. The associations of SLE with a SNP marker and haplotype in the CCL14 gene likely indicate a disease relevant mutation in the nearby region and warrant further LD mapping in larger cohorts.
Acknowledgments
This study was supported in part by the National Multiple Sclerosis Society, Veterans Administration, the Alliance for Lupus Research and grants AI 061066, AI 048079, and AI 072648 from the National Institutes of Health.
References
- Abecasis GR, Cherny SS, Cookson WO, Cardon LR. Merlin-rapid analysis of dense genetic maps using sparse gene flow trees. Nat Genet. 2002;30:97–101. doi: 10.1038/ng786. [DOI] [PubMed] [Google Scholar]
- Arnett FC, Reveille JD. Genetics of systemic lupus erythematosus. Rheum Dis Clin North Am. 1992;18:865–892. [PubMed] [Google Scholar]
- Banisor I, Leist TP, Kalman B. Involvement of β-chemokines in the development of inflammatory demyelination. J Neuroinflammation. 2005;2:7. doi: 10.1186/1742-2094-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barcellos LF, Thomson G. Genetic analysis of multiple sclerosis in Europeans. J Neuroimmunol. 2003;143:1–6. doi: 10.1016/j.jneuroim.2003.08.004. [DOI] [PubMed] [Google Scholar]
- Barret JC, Fry B, Maller J, Daly MJ. Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics. 2005;21:263–265. doi: 10.1093/bioinformatics/bth457. [DOI] [PubMed] [Google Scholar]
- Bielekova B, Kadom N, Fisher E, Jeffries N, Ohayon J, Richert N, Howard T, Bash CN, Frank JA, Stone L, Martin R, Cutter G, McFarland HF. MRI as a marker for disease heterogeneity in multiple sclerosis. Neurology. 2005;65:1071–1076. doi: 10.1212/01.wnl.0000178984.30534.f9. [DOI] [PubMed] [Google Scholar]
- Blain KY, Kwiatkowski W, Zhao Q, La Fleur D, Naik C, Chun TW, Tsareva T, Kanakaraj P, Laird MW, Shah R, George L, Sanyal I, Moore PA, Demeler B, Choe S. Structural and functional characterization of CC chemokine CCL14. Biochemistry. 2007;46:10008–10015. doi: 10.1021/bi700936w. [DOI] [PubMed] [Google Scholar]
- Brynedal B, Duvefelt K, Jonasdottir G, Roos IM, Akesson E, Palmgren J, Hillert J. HLA-A confers an HLA-DRB1 independent influence on the risk of multiple sclerosis. PLoS ONE. 2007;2:e664. doi: 10.1371/journal.pone.0000664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jong BA, Huizinga TW, Zanelli E, Giphart MJ, Bollen EL, Uitdehaag BM, Polman CH, Westendorp RG. Evidence for additional genetic risk indicators of relapse-onset MS within the HLA region. Neurology. 2002;59:549–555. doi: 10.1212/wnl.59.4.549. [DOI] [PubMed] [Google Scholar]
- DeLuca GC, Ramagopalan SV, Herrera BM, Dyment DA, Lincoln MR, Montpetit A, Pugliatti M, Barnardo MC, Risch NJ, Sadovnick AD, Chao M, Sotgiu S, Hudson TJ, Ebers GC. An extremes of outcome strategy provides evidence that multiple sclerosis severity is determined by alleles at the HLA-DRB1 locus. Proc Natl Acad Sci U S A. 2007;104:20896–20901. doi: 10.1073/pnas.0707731105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregersen JW, Kranc KR, Ke X, Svendsen P, Madsen LS, Thomsen AR, Cardon LR, Bell JI, Gugger L. Functional epistasis on a common MHC haplotype associated with multiple sclerosis. Nature. 2006;443:574–577. doi: 10.1038/nature05133. [DOI] [PubMed] [Google Scholar]
- Gregory SG, Schmidt S, Seth P, Oksenberg JR, Hart J, Prokop A, Caillier SJ, Ban M, Goris A, Barcellos LF, Lincoln R, McCauley JL, Sawcer SJ, Compston DA, Dubois B, Hauser SL, Garcia-Blanco MA, Pericak-Vance MA, Haines JL for the Multiple Sclerosis Genetics Group. Interleukin 7 receptor alpha chain, (IL7R) shows allelic and functional association with multiple sclerosis. Nat Genet. 2007;39:1083–1091. doi: 10.1038/ng2103. [DOI] [PubMed] [Google Scholar]
- Gupta S, Fuchs B, Schulz-Maronde S, Heitland A, Escher SE, Mack M, Tillmann HC, Braun A, Forssmann WG, Elsner J, Forssmann U. Intravascular inactivation of CCR5 by n-nonanoyl-CC chemokine ligand 14 and inhibition of allergic airway inflammation. J Leukoc Biol. 2008;83:765–773. doi: 10.1189/jlb.0607429. [DOI] [PubMed] [Google Scholar]
- Harley JB, Alarcon-Riquelme ME, Criswell LA, Jacob CO, Kimberly RP, Moser KL, Tsao BP, Vyse TJ, Langefeld CD. Genome-wide association scan in women with systemic lupus erythematosus identifies susceptibility variants in ITGAM, PXK, KIAA1542 and other loci. Nat Genet. 2008;40:204–210. doi: 10.1038/ng.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Multiple Sclerosis Genetics Consortium. Sawcer S, Ban M, Maranian M, Yeo TW, Compston A, Kirby A, Daly MJ, De Jager PL, Walsh E, Lander ES, Rioux JD, Hafler DA, Ivinson A, Rimmler J, Gregory SG, Schmidt S, Pericak-Vance MA, Akesson E, Hillert J, Datta P, Oturai A, Ryder LP, Harbo HF, Spurkland A, Myhr KM, Laaksonen M, Booth D, Heard R, Stewart G, Lincoln R, Barcellos LF, Hauser SL, Oksenberg JR, Kenealy SJ, Haines JL. A high-density screen for linkage in multiple sclerosis. Am J Hum Genet. 2005;77:454–467. doi: 10.1086/444547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Multiple Sclerosis Genetics Consortium. Hafler DA, Compston A, Sawcer S, Lander ES, Daly MJ, De Jager PL, de Bakker PI, Gabriel SB, Mirel DB, Ivinson AJ, Pericak-Vance MA, Gregory SG, Rioux JD, McCauley JL, Haines JL, Barcellos LF, Cree B, Oksenberg JR, Hauser SL. Risk alleles for multiple sclerosis identified by a genomewide study. N Engl J Med. 2007;357:851–862. doi: 10.1056/NEJMoa073493. [DOI] [PubMed] [Google Scholar]
- Jagodic M, Becanovic K, Sheng JR, Wu X, Bäckdahl L, Lorentzen JC, Wallström E, Olsson T. An advanced intercross line resolves Eae18 into two narrow quantitative trait loci syntenic to multiple sclerosis candidate loci. J Immunol. 2004;173:1366–1373. doi: 10.4049/jimmunol.173.2.1366. [DOI] [PubMed] [Google Scholar]
- Johansson CM, Zunec R, Garcia MA, Scherbarth HR, Tate GA, Paira S, Navarro SM, Perandones CE, Gamron S, Alvarellos A, Graf CE, Manni J, Berbotto GA, Palatnik SA, Catoggio LJ, Battagliotti CG, Sebastiani GD, Migliaresi S, Galeazzi M, Pons-Estel BA, Alarcon-Riquelme ME Collaborative Group on the Genetics of SLE, and Argentine Collaborative Group. Chromosome 17p12–q11 harbors susceptibility loci for systemic lupus erythematosus. Hum Genet. 2004;115:230–238. doi: 10.1007/s00439-004-1145-3. [DOI] [PubMed] [Google Scholar]
- Kantarci OH, de Andrade M, Weinshenker BG. Identifying disease modifying genes in multiple sclerosis. J Neuroimmunol. 2002;123:144–159. doi: 10.1016/s0165-5728(01)00481-7. [DOI] [PubMed] [Google Scholar]
- Lucchinetti C, Brück W, Parisi J, Scheithauer B, Rodriguez M, Lassmann H. Heterogeneity of multiple sclerosis lesions: Implications for the pathogenesis of demyelination. Annals of Neurology. 2000;47:707–717. doi: 10.1002/1531-8249(200006)47:6<707::aid-ana3>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- Lundmark F, Duvefelt K, Iacobaeus E, Kockum I, Wallström E, Khademi M, Oturai A, Ryder LP, Saarela J, Harbo HF, Celius EG, Salter H, Olsson T, Hillert J. Variation in interleukin 7 receptor alpha chain, (IL7R) influences risk of multiple sclerosis. Nat Genet. 2007;39:1108–1113. doi: 10.1038/ng2106. [DOI] [PubMed] [Google Scholar]
- Mahad DJ, Trebst C, Kivisakk P, Staugaitis SM, Tucky B, Wei T, Lucchinetti CF, Lassmann H, Ransohoff RM. Expression of chemokine receptors CCR1 and CCR5 reflects differential activation of mononuclear phagocytes in pattern II and pattern III multiple sclerosis lesions. J Neuropathol Exp Neurol. 2004;63:262–273. doi: 10.1093/jnen/63.3.262. [DOI] [PubMed] [Google Scholar]
- Mamtani M, Rovin B, Brey R, Camargo JF, Kulkarni H, Herrera M, Correa P, Holliday S, Anaya JM, Ahuja SK. CCL3L1 gene-containing segmental duplications and polymorphisms in CCR5 affect risk of systemic lupus erythematosus. Ann Rheum. 2007 doi: 10.1136/ard.2007.078048. [Electronic publication ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald WI, Compston A, Edan G, Goodkin D, Hartung HP, Lublin FD, McFarland HF, Paty DW, Polman CH, Reingold SC, Sandberg-Wollheim M, Sibley W, Thompson A, van den Noort S, Weinshenker BY, Wolinsky JS. Recommended diagnostic criteria for multiple sclerosis: guidelines from the international panel on the diagnosis of multiple sclerosis. Ann Neurol. 2001;50:121–127. doi: 10.1002/ana.1032. [DOI] [PubMed] [Google Scholar]
- McManus C, Berman JW, Brett FM, Staunton H, Farrell M, Brosnan CF. MCP-1, MCP-2 and MCP-3 expression in multiple sclerosis lesions: an immunohistochemical and in situ hybridization study. J Neuroimmunol. 1998;86:20–29. doi: 10.1016/s0165-5728(98)00002-2. [DOI] [PubMed] [Google Scholar]
- Nath SK, Kelly JA, Harley JB, Scofield RH. Mapping the systematic lupus erythematosus susceptibility genes. In: Perl A, editor. Autoimmunity. Methods and Protocols. Humana; Totowa, NJ: 2004. [DOI] [PubMed] [Google Scholar]
- O’Boyle G, Brain JG, Kirby JA, Ali S. Chemokine-mediated inflammation: Identification of a possible regulatory role for CCR2. Mol Immunol. 2007;44:1944–1953. doi: 10.1016/j.molimm.2006.09.033. [DOI] [PubMed] [Google Scholar]
- Oksenberg JR, Barcellos LF, Cree BA, Baranzini SE, Bugawan TL, Khan O, Lincoln RR, Swerdlin A, Mignot E, Lin L, Goodin D, Erlich HA, Schmidt S, Thomson G, Reich DE, Pericak-Vance MA, Haines JL, Hauser SL. Mapping multiple sclerosis susceptibility to the HLA-DR locus in African Americans. Am J Hum Genet. 2004;74:160–167. doi: 10.1086/380997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pardigol A, Forssmann U, Zucht HD, Loetscher P, Schulz-Knappe P, Baggiolini M, Forssmann WG, Mägert HJ. HCC-2, a human chemokine: gene structure, expression pattern, and biological activity. Proc Natl Acad Sci U S A. 1998;95:6308–6313. doi: 10.1073/pnas.95.11.6308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perl A. Pathogenesis and spectrum of autoimmunity. In: Perl A, editor. Autoimmunity. Methods and Protocols. Humana Press; Totowa, NJ: 2004. pp. 1–8. [Google Scholar]
- Purcell S, Cherny SS, Sham PC. Genetic power calculator: design of linkage and association genetic mapping studies of complex traits. Bioinformatics. 2003;19:149–150. doi: 10.1093/bioinformatics/19.1.149. [DOI] [PubMed] [Google Scholar]
- Ramagopalan SV, Morris AP, Dyment DA, Herrera BM, DeLuca GC, Lincoln MR, Orton SM, Chao MJ, Sadovnick AD, Ebers GC. The inheritance of resistance alleles in multiple sclerosis. PLoS Genet. 2007;3:1607–1613. doi: 10.1371/journal.pgen.0030150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remmers EF, Plenge RM, Lee AT, Graham RR, Hom G, Behrens TW, de Bakker PIW, Le JM, Lee HS, Batliwalla F, Li W, Masters SL, Booty MG, Carulli JP, Padyukov L, Alfredsson L, Klareskog L, Chen WV, Amos CI, Criswell LA, Seldin MF, Kastner DL, Gregersen PK. STAT4 and the risk of rheumatoid arthritis and systemic lupus erythematosus. N Engl J Med. 2007;357:977–986. doi: 10.1056/NEJMoa073003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rovin BH. The chemokine network in systemic lupus erythematous nephritis. Front Biosci. 2008;13:904–922. doi: 10.2741/2731. [DOI] [PubMed] [Google Scholar]
- Savarin-Vuaillat C, Ransohoff RM. Chemokines and chemokine receptors in neurological disease: raise, retain, or reduce. Neurotherapeutics. 2007;4:590–601. doi: 10.1016/j.nurt.2007.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slatkin M, Excoffier L. Testing for linkage disequilibrium in genotypic data using the expectation–maximization algorithm. Heredity. 1996;76:377–383. doi: 10.1038/hdy.1996.55. [DOI] [PubMed] [Google Scholar]
- Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, Schaller JG, Talal N, Winchester RJ. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arth Rheum. 1982;25:1271–1277. doi: 10.1002/art.1780251101. [DOI] [PubMed] [Google Scholar]
- Teuscher C, Butterfield RJ, Ma RZ, Zachary JF, Doerge RW, Blankenhorn EP. Sequence polymorphisms in the chemokines Scya1, (TCA-3), Scya2, (monocyte chemoattractant protein, (MCP)-1), and Scya12, (MCP-5) are candidates for eae7, a locus controlling susceptibility to monophasic remitting/nonrelapsing experimental allergic encephalomyelitis. J Immunol. 1999;163:2262–2266. [PubMed] [Google Scholar]
- The Transatlantic Multiple Sclerosis Genetics Cooperative. A meta-analysis of genomic screens in multiple sclerosis. Mult Scler. 2001;7:3–11. doi: 10.1177/135245850100700102. [DOI] [PubMed] [Google Scholar]
- Vyshkina T, Yao Shugart Y, Birnbaum G, Leist TP, Kalman B. Association of haplotypes in the β-chemokine locus with multiple sclerosis. Eur J Hum Genet. 2005;13:240–247. doi: 10.1038/sj.ejhg.5201295. [DOI] [PubMed] [Google Scholar]
- Vyshkina T, Kalman B. Haplotypes within genes of β-chemokines are associated with multiple sclerosis: a second phase study. Human Genetics. 2005;118:67–75. doi: 10.1007/s00439-005-0003-2. [DOI] [PubMed] [Google Scholar]
- Vyshkina T, Kalman B. Analyses of a MS-associated haplotype encompassing the CCL3 gene. J Neuroimmunol. 2006;176:216–218. doi: 10.1016/j.jneuroim.2006.03.018. [DOI] [PubMed] [Google Scholar]
- Wu T, Xie C, Wang HW, Zhou XJ, Schwartz N, Calixto S, Mackay M, Aranow C, Putterman C, Mohan C. Elevated urinary VCAM-1, P-selectin, soluble TNF receptor-1, and CXC chemokine ligand 16 in multiple murine lupus strains and human lupus nephritis. J Immunol. 2007;179:7166–7175. doi: 10.4049/jimmunol.179.10.7166. [DOI] [PubMed] [Google Scholar]
- Zivadinov R, Bakshi R. Central nervous system atrophy and clinical status in multiple sclerosis. J Neuroimaging. 2004;14(3 Suppl):27S–35S. doi: 10.1177/1051228404266266. [DOI] [PubMed] [Google Scholar]