Abstract
Calcinosis cutis is a rare disorder characterized by the deposition of calcium in the skin and subcutaneous tissue. Unilateral idiopathic calcinosis cutis has only rarely been reported in the literature. Here, we report the case of a 7-year-old healthy girl who presented with multiple asymptomatic hard nodules on the right side of her body. Histopathological, radiological, and extensive blood investigations confirmed the diagnosis of unilateral idiopathic calcinosis cutis.
Keywords: Iatrogenic calcinosis, Calcinosis cutis
Introduction
Calcinosis cutis is an aberrant calcium deposition in the skin and subcutaneous tissue. Clinical manifestations vary from localized nodules to debilitating lesions that can involve large areas of the body. There are 4 types of calcinosis cutis: idiopathic, dystrophic, metastatic, and iatrogenic. Determining the type of calcinosis is very important for accurate management. Here, we report the case of a 7-year-old girl with idiopathic calcinosis, few cases of which have been described in early childhood. The unilateral distribution of calcinosis cutis has been previously reported in rare cases in the literature [1, 2]. Furthermore, this is the first report that describes a unique unilateral presentation on the upper and lower limbs.
Case Presentation
A 7-year-old healthy girl was referred to our dermatology clinic for an evaluation of asymptomatic skin lesions involving multiple sites exclusively on the right side of her body. There was no history of an inciting traumatic event. Medical history, family history, and social history were all negative. According to the parents of the patient, the lesions had enlarged minimally since they were first noted 2 years prior to the visit. There had been no increase in the number of lesions since their first appearance. The patient did not experience any restrictions in the movement of her joints, and she did not have any systemic symptoms.
Clinical examination revealed multiple skin-colored, nontender, firm-to-hard mobile nodules of various sizes (0.5–1.0 cm) located over the right side of the patient's body, mainly around her joints (Fig. 1). No other abnormalities or deformities were noted during the examination.
Fig. 1.
a–d Multiple nodules of various sizes located mainly around the joints over the right side of the patient's body.
A laboratory evaluation revealed a normal blood count and normal liver and renal function tests. Serum calcium, phosphorus, uric acid, erythrocyte sedimentation rate, C-reactive protein, alkaline phosphatase, and creatine kinase were all normal. Low vitamin D levels were noted (26.42 ng/mL). A hormonal workup, including calcitonin, parathyroid hormone, and thyroid hormone levels, was also within normal limits. To exclude connective tissue disorders, extensive immunological investigations were performed, including complement C3 and C4, ANA, anti-Ds DNA, RNP Ab, SS-A Ab, SS-B Ab, and anti-Sm Ab. All values were normal.
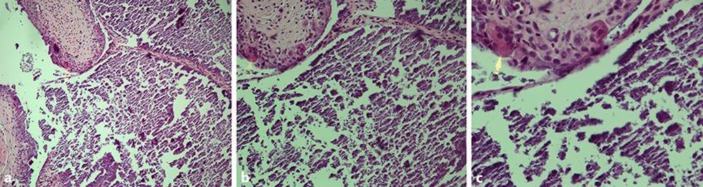
Plain radiographs revealed well-defined calcifications of various sizes in the involved areas. Histological examination of one of the nodules revealed thick, cheesy material at the time of the procedure and microscopic massive calcium deposits (Fig. 2).
Fig. 2.
a–c Tumoral calcinosis. a Lesion consisting of an area of basophilic calcified material with surrounding reactive giant cells. Hematoxylin and eosin. ×100. b, c Giant cells in high-power magnification. Hematoxylin and eosin. ×200 (b) and ×400 (c).
The patient had been seen by a pediatric rheumatologist for the calcifications, which had been managed conservatively with regular follow-up visits for the last year and no increase in the number of lesions or change in the patient's general health status.
Discussion
Based on the etiology, calcinosis cutis can be classified into 4 variants: idiopathic, dystrophic, metastatic, and iatrogenic [3]. Idiopathic calcinosis cutis is a skin calcification with no known etiology and an unclear pathogenesis, and serum calcium and phosphorus levels are normal [4]. The dystrophic type of calcinosis cutis is associated with infection, inflammatory processes, cutaneous neoplasm, or connective tissue diseases in which preexisting damage to the skin results in calcium deposits [5, 6]. Metastatic calcification results from systemic metabolic disorders and leads to elevated serum levels of calcium or phosphorus as well as calcium deposits in the skin and often other tissues. Iatrogenic and traumatic calcinosis are associated with medical procedures [7]. A few rare types have been variably classified as dystrophic or idiopathic. These types include calcinosis cutis circumscripta, calcinosis cutis universalis, tumoral calcinosis, subepidermal calcified nodule, and transplant-associated calcinosis cutis [8]. Idiopathic calcinosis is the rarest subtype. Only a small number of cases of idiopathic calcinosis have been reported in early childhood or adolescence. Neither local tissue injury nor systemic metabolic disorder can be demonstrated [4]. Idiopathic calcinosis with unique unilateral presentation has been previously reported in the literature in only 2 cases: 1 in association with ipsilateral porokeratotic eccrine ostial and dermal duct nevus and 1 on the right elbow of a child [1, 2].
Determining the exact type of calcinosis cutis is very important for selecting accurate management. It is recommended that patients be evaluated for abnormalities of calcium and phosphorus metabolism and that they be assessed for associated systemic conditions, such as collagen vascular diseases, renal insufficiency, and vitamin D poisoning. In our patient, there was no history of trauma or constitutional symptoms; all of her blood samples fell within normal ranges. We accordingly diagnosed the patient with idiopathic calcinosis cutis.
Idiopathic calcinosis cutis is difficult to treat, particularly in children. Most medical measures, although beneficial in some cases, are not recommended for children because the risks outweigh the benefits. This situation poses a challenge to the medical treatment of idiopathic calcinosis cutis. Excision of the mass is an option, but its recurrence is not uncommon. Certain medical treatments after excision might be used in some cases. Intralesional corticosteroid is a safe example that can be used in children and may be beneficial. Probenecid, colchicine, and warfarin have been useful in some adult patients. Aluminum hydroxide antacids may be effective phosphate binders in patients with hyperphosphatemia, but their use in renal insufficiency may result in toxicity [3]. Bisphosphonates may be helpful in some individuals by inhibiting bone resorption followed by reducing calcium turnover, which may be a source of further calcium deposition. However, treatment is prolonged, and paradoxical hyperphosphatemia may result [9]. Various beneficial effects reported with the use of the calcium channel blocker diltiazem have been reported. The therapeutic effect of this drug is believed to be antagonism of a calcium-sodium ion pump [10]. Unless the exact pathogenesis or dystrophic variant of calcinosis cutis is determined, the medical line of prevention after surgical excision has more potential complications in children. In our case, there was no evident defect in calcium metabolism, so no treatment was planned.
In conclusion, after a clinical diagnosis of calcinosis cutis, a careful evaluation by history and laboratory workup should be performed to exclude possible associated abnormalities and correctly classify calcifying disorders. Our patient was subject to regular follow-up for any new local or systemic symptoms. We did not encounter any new lesions, growth in the present lesions, or laboratory abnormalities at the 1-year follow-up. The laboratory workup will be repeated after 1 year to detect any possible changes. Excision of the lesion has been offered to the patient and could provide a successful resolution; however, recurrence is possible.
Statement of Ethics
We confirm that the patient has provided written informed consent to use his photos for publications.
Disclosure Statement
The authors have nothing to disclose.
References
- 1.Vasudevan B, Sondhi V, Verma R, Neema S. A unique association of unilateral idiopathic calcinosis cutis with ipsilateral porokeratotic eccrine ostial and dermal duct nevus. Pediatr Dermatol. 2015;32:e8–e12. doi: 10.1111/pde.12458. [DOI] [PubMed] [Google Scholar]
- 2.Gupta SK, Balaga R, Banik S. Idiopathic calcinosis cutis over elbow in a 12-year old child. Case Rep Orthop. 2013;2013:241891. doi: 10.1155/2013/241891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boulman N, Slobodin G, Rozenbaum M, et al. Calcinosis in rheumatic diseases. Semin Arthritis Rheum. 2005;34:805–812. doi: 10.1016/j.semarthrit.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 4.Cohen PR, Tschen JA. Idiopathic calcinosis cutis of the penis. J Clin Aesthet Dermatol. 2012;5:23–30. [PMC free article] [PubMed] [Google Scholar]
- 5.James WD, Berger TG, Elston DM. Andrews’ Diseases of the Skin: Clinical Dermatology. ed 11. Philadelphia: Elsevier Saunders; 2011. [Google Scholar]
- 6.Dubey S, Sharma R, Maheshwari V. Scrotal calcinosis: idiopathic or dystrophic? Dermatol Online J. 2010;16:5. [PubMed] [Google Scholar]
- 7.Marzano AV, Kolesnikova LV, Gasparini G, Alessi E. Dystrophic calcinosis cutis in subacute lupus. Dermatology. 1999;198:90–92. doi: 10.1159/000018074. [DOI] [PubMed] [Google Scholar]
- 8.Bécuwe C, Roth B, Villedieu MH, Chouvet B, Kanitakis J, Claudy A. Milia-like idiopathic calcinosis cutis. Pediatr Dermatol. 2004;21:483–485. doi: 10.1111/j.0736-8046.2004.21415.x. [DOI] [PubMed] [Google Scholar]
- 9.Mukamel M, Horev G, Mimouni M. New insight into calcinosis of juvenile dermatomyositis: a study of composition and treatment. J Pediatr. 2001;138:763–766. doi: 10.1067/mpd.2001.112473. [DOI] [PubMed] [Google Scholar]
- 10.Palmieri GM, Sebes JI, Aelion JA, Moinuddin M, Ray MW, Wood GC, Leventhal MR. Treatment of calcinosis with diltiazem. Arthritis Rheum. 1995;38:1646–1654. doi: 10.1002/art.1780381117. [DOI] [PubMed] [Google Scholar]