Abstract
A 23-year-old male presented with a 3-month history of left purulent rhinorrhea, progressive nasal obstruction, and intermittent epistaxis. A fiberoptic examination revealed a large vascular polypoid mass completely filling the left nasal cavity. CT and MRI scans showed a large hypervascular mass involving the left nasal airway, maxillary antrum, and the anterior ethmoid cells. There was no bony erosion or contiguous spread, and the remaining sinuses, orbit, and cranial fossa were uninvolved. The patient underwent complete removal of the mass via an external lateral rhinotomy approach. The soft mass was large and vascular. A microscopic analysis revealed an undifferentiated tumor consisting of a solid sheet of small, round blue cells. Mitotic figures were also present. Immunohistochemically, the tumor cells were strongly positive for CD99. Molecular studies using a PCR confirmed the chromosomal translocation of FLI1 (exon 6). These findings were considered diagnostic for Ewing's sarcoma. Postoperatively, the patient was treated with combined chemotherapy and radiotherapy. Adjuvant chemotherapy consisting of vincristine, doxorubicin, and cyclophosphamide alternating with ifosfamide and etoposide (total: 7 cycles) was commenced. He also received radiation therapy for local control (total dose: 50.4 Gy). The patient is currently alive without any evidence of recurrence or metastasis.
Keywords: Ewing's sarcoma, Sinonasal tract, VDC-IE, Chemotherapy, Radiation therapy
Introduction
Ewing's sarcoma (EWS) is a highly malignant, small, round cell tumor that originated from the primitive neuroectodermal cells, as first described by James Ewing in 1921 [1]. EWS of the bone, which most commonly occurs in children and young adults, accounts for approximately 3% of all pediatric cancers and most cases arise in the long bones or the pelvis [2]. Primary EWS of the head and neck region is extremely rare, accounting for only 4–9% of all EWSs [3, 4, 5, 6]. Furthermore, sinonasal lesions are uncommon. Only 14 cases of EWS involving the nasal cavity or the paranasal sinuses have been reported in the world's otolaryngology literature [7, 8, 9]. We herein present a case of EWS arising in the left ethmoid sinus.
Case Report
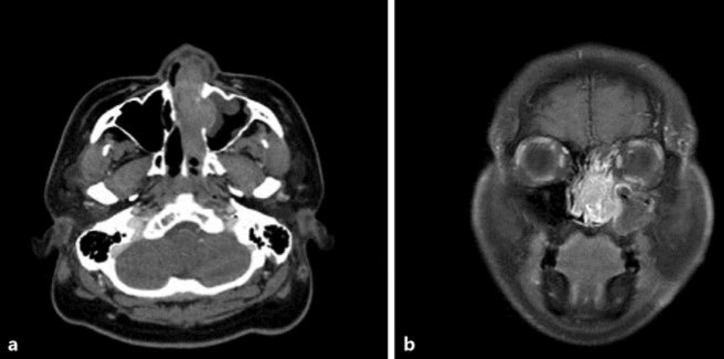
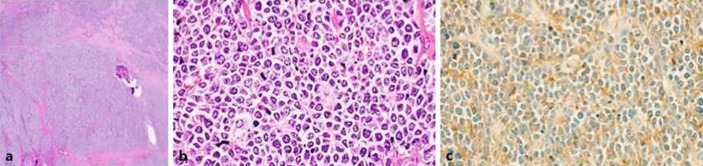
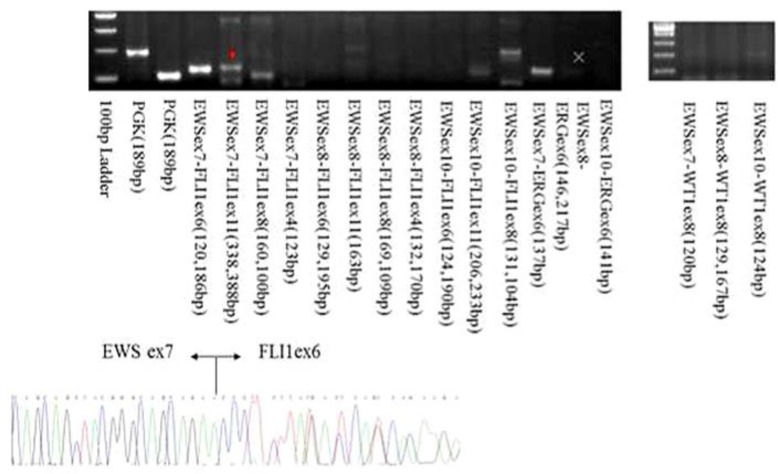
A 23-year-old male visited the otorhinolaryngology department for left purulent rhinorrhea and progressive nasal obstruction for 3 months. His past history was unremarkable. At the endoscopic examination, a large vascular polypoid mass was found to completely fill the left nasal cavity and the nasal septum was excluded to the right side (Fig. 1a, b). CT and MRI images showed a large hypervascular mass involving the left nasal airway, maxillary antrum, and anterior ethmoid cells. There was no bony erosion or contiguous spread, and the remaining sinuses, orbit, and cranial fossa were uninvolved (Fig. 2a, b). We embolized the mass (Fig. 3a) and subsequently performed surgical resection. Angiography of the left maxillary artery showed deep dyeing of the mass and gelatin was injected into the artery (Fig. 3b). A lateral rhinotomy approach was utilized to gain access to the tumor, followed by dissection along the medial wall of the orbit and around the tumor (Fig. 3c). A microscopic analysis revealed an undifferentiated tumor consisting of a solid sheet of small, round blue cells (Fig. 4a, b). Immunohistochemically, the tumor cells were strongly positive for CD99 (Fig. 4c). Molecular studies using PCR confirmed the chromosomal translocation of FLI1 (exon 6) (Fig. 5). These findings led to a diagnosis of EWS. Adjuvant chemotherapy consisting of vincristine, doxorubicin, and cyclophosphamide alternating with ifosfamide and etoposide (total: 7 cycles) was commenced. Radiation therapy was also administered for local control (total dose: 50.4 Gy) (Fig. 6). The patient has remained alive without evidence of recurrence or metastasis for 2½ years.
Fig. 1.
a A large vascular polypoid mass completely filling the left nasal cavity. b The nasal septum is excluded to the right side.
Fig. 2.
a, b CT and MRI (T1) showed a large hypervascular mass involving the left nasal airway, maxillary antrum, and anterior ethmoid cells. There was no bony erosion or contiguous spread, and the remaining sinuses, orbit, and cranial fossa were uninvolved.
Fig. 3.
a Angiography of left maxillary artery. b Gelatin was injected into the left maxillary artery. c A lateral rhinotomy approach was performed to remove the tumor.
Fig. 4.
Microscopic analysis revealed an undifferentiated tumor consisting of a solid sheet of small, round blue cells (a 10 × 2, b 10 × 40). c Immunohistochemically, tumor cells showed strongly positive staining with CD99.
Fig. 5.
Molecular studies using PCR analysis confirmed the chromosomal translocation of FLI1 (exon 6).
Fig. 6.
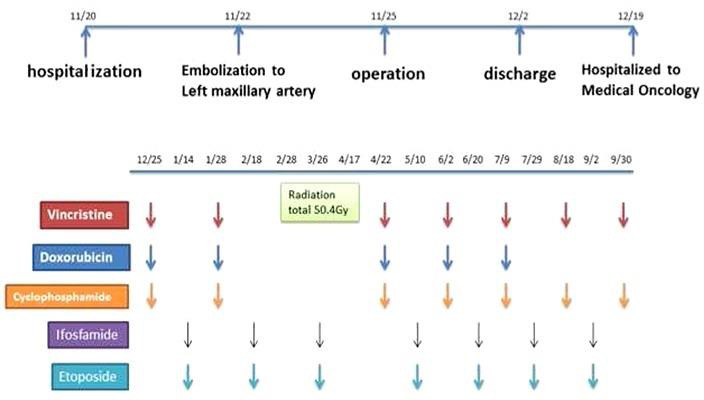
Adjuvant chemotherapy consisting of vincristine, doxorubicin, and cyclophosphamide alternating with ifosfamide and etoposide (7 cycles total) was commenced. He also received radiation therapy for local control (total dose of 50.4 Gy). The patient is alive without evidence of recurrence or metastasis.
Discussion
EWS is a highly malignant, small, round cell tumor that originates from the primitive neuroectodermal cells. It was first described by James Ewing in 1921 [1]. Primary EWS commonly occurs in early childhood or adolescence and rarely occurs in adulthood. There is a slightly male predominance with a male-to-female ratio of 1.5: 1 [7, 10, 11]. Primary EWS of the head and neck region is extremely rare and accounts for only 4–9% of all EWSs [3, 4, 5, 6]. In general, approximately 20–30% of EWS patients present with metastases at the time of their diagnosis [12, 13, 14, 15, 16]. Patients with EWS of the head and neck region less frequently have metastases at diagnosis [3, 4, 9, 17, 18, 19, 20]. In our case, the patient did not have metastasis. Microscopically, these tumors are composed of uniform small round cells with round nuclei containing fine chromatin and scant clear or eosinophilic cytoplasm. In the sinonasal tract, the differential diagnosis includes all tumors that are composed of small round cells, such as olfactory neuroblastoma and undifferentiated carcinoma [21]. The diagnosis requires a histopathological examination, immunohistochemistry, and a cytogenetic analysis. The essential diagnostic examination to differentiate EWS from the many small round neoplasms is the CD99 marker, which can be detected in a specific immunohistochemical examination. In addition, molecular studies using PCR to detect the characteristics of chromosomal translocation are definitive for the diagnosis of EWS. A gene sequence, t(11;22)(q24;q12), which results in the fusion of the EWS gene with the FLI gene, is a specific genetic hallmark of EWS [22, 23, 24]. In our case, the patient was positive for the CD99 marker and the FLI gene. In general, the treatment of EWS consists of induction chemotherapy, followed by local control, which usually involves surgical resection, possibly followed by radiotherapy, and subsequent adjuvant chemotherapy. Aside from the patient characteristics, local control also affects outcome [13, 25]. In EWS of the extremities, surgical resection (with or without radiotherapy) has been shown to be superior to radiotherapy alone [26]. Generally, EWS treatment begins with induction chemotherapy followed by local control. Adequate surgical removal with radical resection is desirable. Surgery should be combined with additional radiotherapy in cases involving a marginal resection and/or poor histological response. Local control is followed by adjuvant chemotherapy. In many cases, this approach is not practical for patients with EWS of the head and neck [27]. In our case, the patient was treated with postoperative combined chemotherapy and radiotherapy. Adjuvant chemotherapy was commenced. The patient also received radiation therapy for local control (total dose: 50.4 Gy). The patient remains alive without evidence of recurrence or metastasis at 3 years since the first examination.
Statement of Ethics
The authors have no ethical conflicts to disclose.
Disclosure Statement
The authors have no conflicts of interest to declare.
References
- 1.Ewing J. Diffuse endothelioma of bone. Pathol Soc. 1921;21:17–24. [Google Scholar]
- 2.Ludwig JA. Ewing sarcoma: historical perspectives, current state-of-the-art, and opportunities for targeted therapy in the future. Curr Opin Oncol. 2008;20:412–418. doi: 10.1097/CCO.0b013e328303ba1d. [DOI] [PubMed] [Google Scholar]
- 3.Siegal GP, Oliver WR, Reinus WR, Gilula LA, Foulkes MA, Kissane JM, Askin FB. Primary Ewing's sarcoma involving the bones of head and neck. Cancer. 1987;60:2829–2840. doi: 10.1002/1097-0142(19871201)60:11<2829::aid-cncr2820601139>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 4.Allam A, El-Husseinty G, Khafaga Y, Kandil A, Gray A, Ezzat A, Schultz H. Ewing's sarcoma of the head and neck: a retrospective analysis of 24 cases. Sarcoma. 1999;3:11–15. doi: 10.1080/13577149977811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carlotti CG, Jr, Drake JM, Hladky JP, Teshima I, Becker LE, Rutka JT. Primary Ewing's sarcoma of the skull in children. Utility of moleculer diagnostics surgery and adjuvant therapies. Pediatr Neurosurg. 1999;31:307–315. doi: 10.1159/000028881. [DOI] [PubMed] [Google Scholar]
- 6.Desai KI, Nadkarni TD, Goel A, Muzumdar DP, Naresh KN, Nair CN. Primary Ewing's sarcoma of the cranium. Neurosurgery. 2000;46:62–68. [PubMed] [Google Scholar]
- 7.Yeshvanth SK, Ninan K, Bhandary SK, Lakshinarayana KP, Shetty JK, Makannavar JH. Rare case of extraskeletal Ewings sarcoma of the sinonasal tract. J Cancer Res Ther. 2012;8:142–144. doi: 10.4103/0973-1482.95197. [DOI] [PubMed] [Google Scholar]
- 8.Coskun BU, Cinar U, Savk H, Basak T, Dadas B. Isolated maxillary sinus Ewing's sarcoma. Rhinology. 2005;43:225–228. [PubMed] [Google Scholar]
- 9.Gupta S, Gupta OP, Mehrotra S, Mehrotra D. Ewing sarcoma of the maxilla: a rare presentation. Quintessence Int. 2009;40:135–140. [PubMed] [Google Scholar]
- 10.Howarth KL, Khodaei I, Karkanevatos A, Clarke RW. A sinonasal primary Ewing's sarcoma. Int J Pediatr Otorhinolaryngol. 2004;68:221–224. doi: 10.1016/j.ijporl.2003.09.011. [DOI] [PubMed] [Google Scholar]
- 11.Csokonai LV, Liktor B, Arató G, Helffrich F. Ewing's sarcoma in the nasal cavity. Otolaryngol Head Neck Surg. 2001;125:665–667. doi: 10.1067/mhn.2001.119486. [DOI] [PubMed] [Google Scholar]
- 12.Cotterill SJ, Ahrens S, Paulussen M, Jürgens HF, Voûte PA, Gadner H, Craft AW. Prognostic factors in Ewing's tumor of bone: analysis of 975 patients from the European Intergroup Cooperative Ewing's Sarcoma Study Group. J Clin Oncol. 2000;18:3108–3114. doi: 10.1200/JCO.2000.18.17.3108. [DOI] [PubMed] [Google Scholar]
- 13.Bacci G, Longhi A, Ferrari S, Mercuri M, Versari M, Bertoni F. Prognostic factors in non-metastatic Ewing's sarcoma tumor of bone: an analysis of 579 patients treated at a single institution with adjuvant or neoadjuvant chemotherapy between 1972 and 1998. Acta Oncol. 2006;45:469–475. doi: 10.1080/02841860500519760. [DOI] [PubMed] [Google Scholar]
- 14.Daw NC, Mahmoud HH, Meyer WH, Jenkins JJ, Kaste SC, Poquette CA, Kun LE, Pratt CB, Rao BN. Bone sarcomas of the head and neck in children: the St Jude Children's Research Hospital experience. Cancer. 2000;88:2172–2180. doi: 10.1002/(sici)1097-0142(20000501)88:9<2172::aid-cncr25>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 15.Esiashvili N, Goodman M, Marcus RB., Jr Changes in incidence and survival of Ewing sarcoma patients over the past 3 decades: Surveillance Epidemiology and End Results data. J Pediatr Hematol Oncol. 2008;30:425–430. doi: 10.1097/MPH.0b013e31816e22f3. [DOI] [PubMed] [Google Scholar]
- 16.Krishnamani K, Kumar TN, Gandhi LV, Raghunadharao D, Sadashivudu G, Megha U. Pri- mary Ewing's sarcoma of the cranium: case series and review of literature. J Cancer Res Ther. 2014;10:377–380. doi: 10.4103/0973-1482.136663. [DOI] [PubMed] [Google Scholar]
- 17.Whaley JT, Indelicato DJ, Morris CG, Hinerman RW, Amdur RJ, Mendenhall WM, Keole SR, Marcus RB., Jr Ewing tumors of the head and neck. Am J Clin Oncol. 2010;33:321–326. doi: 10.1097/COC.0b013e3181aaca71. [DOI] [PubMed] [Google Scholar]
- 18.Salunke PS, Gupta K, Malik V, Kumar N, Henke LE, Cai C, Chen WS, Pfeifer JD. Primary Ewing's sarcoma of cranial bones: analysis of ten patients. Acta Neurochir (Wien) 2011;153:1477–1485. doi: 10.1007/s00701-011-1028-z. [DOI] [PubMed] [Google Scholar]
- 19.Zöllner S, Dirksen U, Jürgens H, Ranft A. Renal Ewing tumors. Ann Oncol. 2013;24:2455–2461. doi: 10.1093/annonc/mdt215. [DOI] [PubMed] [Google Scholar]
- 20.Jenkin RD, Al-Fawaz I, Al-Shabanah MO, Allam A, Ayas M, Memon M, Rifai S, Schultz HP. Metastatic Ewing sarcoma/PNET of bone at diagnosis: prognostic factors – a report from Saudi Arabia. Med Pediatr Oncol. 2001;37:383–389. doi: 10.1002/mpo.1214. [DOI] [PubMed] [Google Scholar]
- 21.Yeshvanth SK, Ninan K, Bhandary SK, Lakshinarayana KP, Shetty JK, Makannavar JH. Rare case of extraskeletal Ewings sarcoma of the sinonasal tract. J Cancer Res Ther. 2012;8:142–144. doi: 10.4103/0973-1482.95197. [DOI] [PubMed] [Google Scholar]
- 22.Kawabata M, Yoshifuku K, Sagara Y, Kurono Y. Ewing's sarcoma/primitive neuroectodermal tumour occurring in the maxillary sinus. Rhinology. 2008;46:75–78. [PubMed] [Google Scholar]
- 23.Gupta S, Gupta OP, Mehrotra S, Mehrotra D. Ewing sarcoma of the maxilla: a rare presentation. Quintessence Int. 2009;40:135–140. [PubMed] [Google Scholar]
- 24.Iezzoni JC, Mills SE. “Undifferentiated” small round cell tumors of the sinonasal tract: differential diagnosis update. Am J Clin Pathol. 2005;124(suppl):S110–S121. doi: 10.1309/59RBT2RK6LQE4YHB. [DOI] [PubMed] [Google Scholar]
- 25.Haeusler J, Ranft A, Boelling T, Gosheger G, Braun-Munzinger G, Vieth V, Burdach S, van den Berg H, Juergens H, Dirksen U. The value of local treatment in patients with primary, disseminated, multifocal Ewing sarcoma (PDMES) Cancer. 2010;116:443–450. doi: 10.1002/cncr.24740. [DOI] [PubMed] [Google Scholar]
- 26.Schuck A, Ahrens S, Paulussen M, Kuhlen M, Könemann S, Rübe C, Winkelmann W, Kotz R, Dunst J, Willich N, Jürgens H. Local therapy in localized Ewing tumors: results of 1,058 patients treated in the CESS 81, CESS 86, and EICESS 92 trials. Int J Radiat Oncol Biol Phys. 2003;55:168–177. doi: 10.1016/s0360-3016(02)03797-5. [DOI] [PubMed] [Google Scholar]
- 27.Grevener K, Haveman LM, Ranft A, van den Berg H, Jung S, Ladenstein R, Klco-Brosius S, Juergens H, Merks JH, Dirksen U. Management and outcome of Ewing sarcoma of the head and neck. Pediatr Blood Cancer. 2016;63:604–610. doi: 10.1002/pbc.25830. [DOI] [PubMed] [Google Scholar]