Abstract
Fibroblast-like synoviocytes (FLSs) contribute to synovial hyperplasia in rheumatoid arthritis (RA). Smoothened (Smo) is a key component of sonic hedgehog (Shh) signaling and contributes to tumor cell proliferation. The objective of this study was to investigate the role of Smo in RA synoviocyte proliferation. FLSs were isolated from RA synovium. Shh signaling was studied using a Smo antagonist (GDC-0449) and small interfering RNA (siRNA) targeting the Smo gene in FLSs. Cell proliferation was quantified by using kit-8 assay and cell cycle distribution and apoptosis were evaluated by flow cytometry. Cell cycle-related genes and proteins were detected by real-time PCR and western blot. FLSs treated with GDC-0449 or Smo-siRNA showed significantly decreased proliferation compared to controls (P < 0.05). Incubation with GDC-0449 or transfection with Smo-siRNA resulted in a significant increase of G1 phase cells compared to controls (P < 0.05). Cell cycle arrest was validated by the significant increase in cyclin D1 and E1 mRNA expression, decrease in cyclin-dependent kinase p21 mRNA expression in Smo-siRNA transfected cells (P < 0.05). Protein expression of cyclin D1 was also downregulated after Smo gene knockdown (P < 0.05). The results suggest that Shh signaling plays an important role in RA-FLSs proliferation in a Smo-dependent manner and may contribute to synovial hyperplasia. Targeting Shh signaling may help control joint damage in patients with RA.
Keywords: cell proliferation, rheumatoid arthritis, smoothened protein, sonic hedgehog signaling, synoviocyte
Introduction
Rheumatoid arthritis (RA) manifests histologically as synovial hyperplasia, neoangiogenesis and inflammatory cell infiltration.1 Activated fibroblast-like synoviocytes (FLSs), which comprise the major cell population of the hyperplastic synovial lining, play a central role in the pathogenesis of RA. Similar to cancer cells, FLSs show dysregulated proliferation and apoptosis, contributing to synovial hypertrophy, formation of invasive pannus tissue, and ultimately leading to joint destruction.2 Therefore, inhibition of synovial proliferation and induction of FLSs apoptosis are potential therapeutic strategies for RA.
Previous studies have demonstrated that overexpression of proto-oncogenes including c-Myc, c-Ras, and c-jun, and mutations in the p53 tumor suppressor gene contribute to the aberrant repression in apoptosis and increase in cell cycle activity of RA-FLSs.3 In addition, cyclin-dependent kinase inhibitors and FLS apoptosis inducers such as anti-Fas monoclonal antibodies have shown anti-arthritic effects and could inhibit joint destruction.4 However, the exact molecular mechanisms contributing to the aberrant tumor-like behavior of FLSs in RA remains unknown.
Signaling pathways involved in cell proliferation and survival, including sonic hedgehog (Shh), have recently been identified as key factors in human cancers. As a morphogen, Shh is essential in pattern formation and progenitor-cell proliferation during embryogenesis.5 During post-embryonic development and in adult tissues, this morphogenetic signaling pathway is quiescent. Canonical Shh signaling is mediated through two transmembrane receptors, patched (Ptch1) and smoothened (Smo).6 In the absence of the Shh ligand, Ptch1 exerts an inhibitory effect on Smo, which consequently prevents activation of downstream signals. When the ligand binds to Ptch1, inhibition of Smo is reversed, thus triggering expression of a panel of downstream target genes via activation of Gli transcription factors (Gli1-3).6
Aberrant activation and dysregulation of Shh signaling has been reported to contribute to various cancers, either by directly regulating cellular growth and survival7 or indirectly by influencing the tumor stroma.8,9 Suppression of Shh signaling using small molecules has been suggested as a promising strategy for anti-cancer treatment. GDC-0449 is a novel, small-molecule inhibitor of Smo. Clinical studies have revealed that inhibition of the Shh signaling pathway using GDC-0449 results in antitumor activity in patients with basal-cell carcinoma, with one of the main mechanisms underlying the effect being the decrease of tumor cell proliferation.10
Despite the critical role of Shh signaling in various cancers, its role in the pathogenesis of RA has not yet been elucidated. Earlier studies have described the aberrant expression of fetal morphogenesis genes, including wingless (Wnt) and bone morphogenetic proteins 2 and 6 in RA synovial tissue.11,12 Recently, we identified overexpression of Shh in synovium from RA patients.13,14 Moreover, we found that selective blockage of Smo attenuates the expression of Shh signaling components in FLSs.14 In this study, we further demonstrate that upregulation and suppression of Shh signaling regulates FLSs proliferation, and that the effect may be mediated by modulating G1 phase progression and G1/S transition.
Materials and methods
Ethics and samples
Han Chinese patients with active RA, including four males and six females (mean age 48.2 ± 9.2 years) were recruited from the Third Affiliated Hospital of Sun Yat-sen University in Guangzhou, China, from September 2012 to December 2013. Synovial tissues were obtained during knee arthroscopy. RA patients were classified according to the 1987 American College of Rheumatology revised classification criteria15 and exhibited moderate to severe disease activity (Disease Activity Score of 28 joint counts >3.2). This study was approved by the Medical Ethics Committee of the Third Affiliated Hospital of Sun Yat-sen University. All patients provided written informed consent.
Cell culture
FLSs were isolated and cultured from RA synovium. Briefly, tissue biopsies were finely minced into pieces and transferred to a tissue culture flask in Dulbecco's modified Eagle's medium (DMEM) (Hyclone Laboratories, Logan, UT, USA) supplemented with 10% fetal bovine serum (FBS) (Hyclone Laboratories). Within 14 days, FLSs migrated out from the tissue explant and were grown to approximately 95% confluency. FLSs were subsequently trypsinized, collected, re-suspended, and planted for proliferation. FLSs from passages 3–5 were used for each experiment after being confirmed as being FLSs by morphology and purity analysis.
RNA interference
At 40% confluency, FLSs were transfected with small interfering RNA (siRNA) against human Smo (Smo-homo-1542, Smo-homo-1292, Smo-homo-1732, Gene Pharma Co., Shanghai, China) using the X-treme GENE siRNA transfection reagent (Roche, Mannheim, Germany) according to the manufacturer's protocol. A glyceraldehyde-3-phosphate dehydrogenase (GAPDH) positive control, a negative control (NC-siRNA group) and mock transfection (blank group) were used for the studies. The siRNA sequences were as follows (Forward, Reverse): Smo-homo-1542: 5′-GGAGUCAUGACUCUGUUCUTT-3′, 5′-AGAACAGAGUCAUGACUCCTT-3′, Smo-homo-1292: 5′-CUGGCACACUUCCUUCAAATT 3′, 5′-UUUGAAGGAAGUGUGCCAGTT-3′, Smo-homo-1732: 5′-GGGACUAUGUGCUAUGUCATT-3′, 5′-UGACAUAGCACAUAGUCCCTT-3′, GAPDH: 5′-GGATATTGTTGCCATCATTdTdT-3′, 5′-AATGATGGCAACAATATCCdTdT-3′, Negative control: 5′-UUCUCCGAACGUGUCACGUTT-3′, 5′-ACGUGACACGUCGGAGAATT-3′. The transfection efficiency was assessed by fluorescence microscopy six hours after transfection with fluoroscein isothiocyanate-conjugated control siRNA. Gene knockdown of Smo was confirmed 48 hours post-transfection by western blotting, which was performed as described in the subsequent section.
Cell proliferation
FLSs were seeded at a density of 2.5 × 104 mL−1 in 96-well plates. 24 hours later, cells were treated with different doses of Smo antagonist (GDC-0449, Selleckchem, Houston, TX, USA) (5 μM and 25 μM) or Smo agonist (purmorphamine, Cayman Chemical, Ann Arbor, MI, USA) (5 μM and 25 μM), or transfected with siRNA and cultured for another 48 hours. To antagonize the Smo receptor, GDC-0449 (5 μM) was added 30 minutes prior to application of purmorphamine (5 μM). Cell proliferation rates were subsequently assessed using the cell counting kit-8 (CCK-8) (Dojindo, Tokyo, Japan) according to the manufacturer's instructions. GDC-0449 and purmorphamine were dissolved at 10 mM in dimethyl sulfoxide (DMSO) and the solution was diluted to the final concentration in DMEM supplemented with 10% FBS. Cells in the control group were treated with vehicle (DMSO in DMEM supplemented with 10% FBS).
Cell cycle analysis
For cell cycle phase analysis, FLSs were plated at a density of 5 × 104 mL−1 in 6-well plates for 24 hours and transfected with siRNA as described in the previous section. FLSs were serum-starved for 18 hours before incubation with GDC-0449 (5 μM) or purmorphamine (5 μM). After treated for 48 hours, FLSs were harvested and fixed in 70% cold ethanol overnight at −20°C. Fixed cells were subsequently washed in phosphate-buffered saline (pH 7.4) and incubated with RNase A (100 μg mL−1) (Invitrogen, Carlsbad, CA, USA) for 30minutes at 37 °C. For staining of nuclei, cells were incubated with propidium iodide (50 μg mL−1) (Sigma-Aldrich, St. Louis, MO, USA) in the dark for 30 minutes at 4°C. Stained cells were subsequently analyzed using a FACSCalibur Flow Cytometer (Becton Dickinson, Franklin Lakes, NJ, USA). For each analysis, 10 000 events were evaluated with the software ModFit LT (Verity Software House, Topsham, ME, USA).
Apoptosis assay
For apoptosis analysis, FLSs were seeded at a density of 7 × 104 mL−1 in 6-well plates, then incubated with GDC-0449 (5 μM) or purmorphamine (5 μM) or transfected with siRNA for 48 hours. Apoptotic cells were determined using an Alexa Fluor 488 annexin V/Dead Cell Apoptosis kit (Invitrogen, Carlsbad, CA, USA) according to the manufacturer's instructions. Stained cells were analyzed by a FACSCalibur flow cytometer (Becton Dickinson). FACS data were analyzed by FlowJo software (Tree Star, Ashland, OR, USA). Viable cells were defined as Annexin V and PI negative, while early apoptotic cells were Annexin V positive and PI negative. Viable cells and cells undergoing early apoptosis were in the lower-left and lower-right quadrant of graph, respectively. Percentages in the two quadrants of each flow cytometric graph were calculated.
RNA isolation and real-time PCR analysis
To measure the effects of Smo agonist and antagonist on Shh signaling, Gli1 expression was determined by real-time PCR analysis. FLSs were treated with different doses of GDC-0449 (5 μM and 25 μM) or purmorphamine (5 μM and 25 μM) for 48 hours as previously described. For the detection of cell cycle-related genes expression, FLSs were transfected with siRNAs for 48 hours. Total RNA was isolated using Trizol reagent (Invitrogen Life Technologies, Santa Clara, CA, USA) and cDNAs were synthesized using the Prime Script RT Reagent kit (Takara Biotechnology, Dalian, China) according to the manufacturer's instructions. Quantification of expressions of human Gli1, cyclin D1, cyclin E1, p21, and GAPDH mRNAs was determined using SYBR Premix Ex TaqTM kit (Takara Biotechnology) on an ABI-7500 Thermal Cycler (Applied Biosystems Inc., Foster City, CA, USA) according to the manufacturer's instructions. All experiments were examined in triplicate and positive and negative controls were included. Relative levels were quantified by the comparative delta Ct method. Primers for amplification were as follows (forward, reverse): Gli1: (5′-AGGGAGTGCAGCCAATACAG-3′, 5′-CCGGAGTTGATGTAGCTGGT-3′), cyclin D1: (5′-GCTGCGAAGTGGAAACCATC-3′, 5′-CCTCCTTCTGCACACATTTGAA-3′), cyclin E1: (5′-GCCAGCCTTGGGACAATAATG-3′, 5′-AGTTTGGGTAAACCCGGTCAT-3′), p21: (5′-CGATGGAACTTCGACTTTGTCA-3′, 5′-GCACAAGGGTACAAGACAGTG-3′), GAPDH: (5′-GGATATTGTTGCCATCATTdTdT-3′, 5′-AATGATGGCAACAATATCCdTdT-3′).
Western blot analysis
Briefly, total protein was extracted using a lysis buffer (Cell Signaling Technology, Beverly, MA, USA). Cell lysates (35 μg protein) were loaded and separated using 8% sodium dodecyl sulfate–-polyacrylamide gel electrophoresis, and then blotted onto a polyvinylidene fluoride membrane. Membranes were blocked at room temperature for two hours and incubated overnight at 4°C with primary antibodies. Primary antibodies included mouse anti-cyclin D1 (1:2000, Cell Signaling Technology) and rabbit anti-Smo (1:2500, Abcam, Cambridge, UK). Subsequently membranes were incubated for one hour at room temperature with secondary antibodies conjugated with horseradish peroxidase. The expression of GAPDH was used as an internal standard.
Statistical analysis
SPSS statistical software, version 17.0 (Chicago, IL, USA), was used for all statistical analyses. Values are presented as means ± standard deviation (S.D.). Comparisons of data between groups were performed by independent sample Student's t-test. Statistical differences among groups were tested by one-way analysis of variance (ANOVA) or the Kruskal–Wallis test. The Dunnett's t-test was used for multiple comparisons. A P-value of <0.05 was considered statistically significant.
Results
Smo agonist and antagonist regulate FLSs proliferation and cell cycle distribution
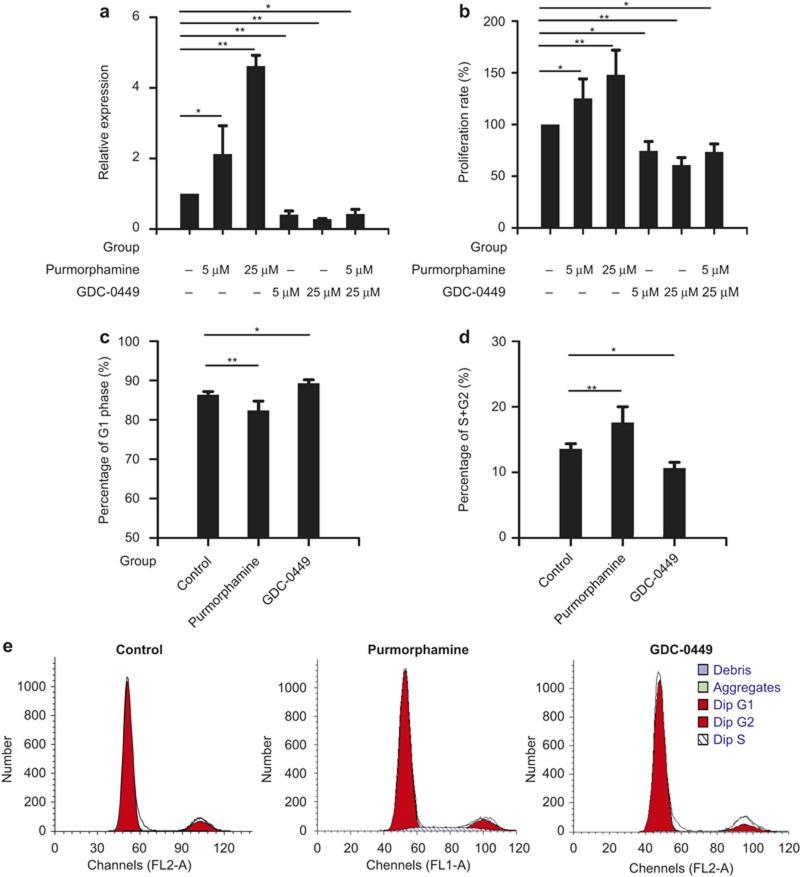
To investigate the effect of small molecules on Shh signaling, Gli1 mRNA levels were examined in FLSs. As shown in Figure 1a, Gli1 mRNA was significantly decreased after incubation with Smo antagonist, GDC-0449 and increased after treatment with different doses of purmorphamine. And the effect of Gli1 upregulation by purmorphamine was abolished by GDC-0449.
Figure 1.
Smo agonist and antagonist regulate FLSs proliferation and cell cycle distribution. (a–e) FLSs were treated with GDC-0449 or purmorphamine at different concentrations (5 μM and 25 μM). After 48 hours of incubation, real-time PCR was used to determine Gli1 expression (a), and cell counting kit-8 (CCK-8) assay was performed to examine the proliferation rate of FLSs (b), and flow cytometry was used to analyze cells in different cycle phases (c, d, e). Data are represented as means ± S.D. of three independent experiments. *P <0.05 versus control group. **P <0.01 versus control group.
To elucidate the effects of GDC-0449 and purmorphamine on FLSs proliferation, the CCK-8 assay was performed. We found that GDC-0449 decreased cell proliferation in a dose-dependent manner. The proliferation rates for cells treated with GDC-0449 (5 μM and 25μM) were 74.60% ± 9.01% and 60.80% ± 7.25%, respectively, compared with controls (100.00% ± 0.00%). We also observed that FLSs proliferation was effectively increased by purmorphamine. The proliferation rates for cells treated with purmorphamine (5 μM and 25μM) were 125.20% ± 18.83% and 148.00% ± 23.88%, respectively. And the effect of purmorphamine (5 μM) on cell proliferation was abolished by GDC-0449 (5 μM) pretreatment, with cell proliferation rate 73.62% ± 7.63% (Figure 1b).
The effect of GDC-0449 and purmorphamine on cell cycle distribution was assessed by flow cytometry. Incubation with GDC-0449 (5 μM) for 48 hours resulted in a significant increase of cells in the G1 phase to 89.32% ± 0.86% compared to controls (86.41% ± 0.77%, P < 0.05) (Figure 1c). The percentages of cells in the S and G2 phase were significantly decreased in the presence of GDC-0449 (10.68% ± 0.86% in the presence of GDC-0449 compared to 13.59% ± 0.76% in the absence of GDC-0449, P < 0.05) (Figure 1d). In addition, incubation of FLSs with purmorphamine (5 μM) decreased the percentage of cells in the G1 phase (82.39% ± 2.39%, P <0.01) and increased cells in the S and G2 phase (17.61% ± 2.39%, P <0.01). These results demonstrate that a compound known to suppress Shh signaling through Smo inhibition can decrease the proliferation of FLSs.
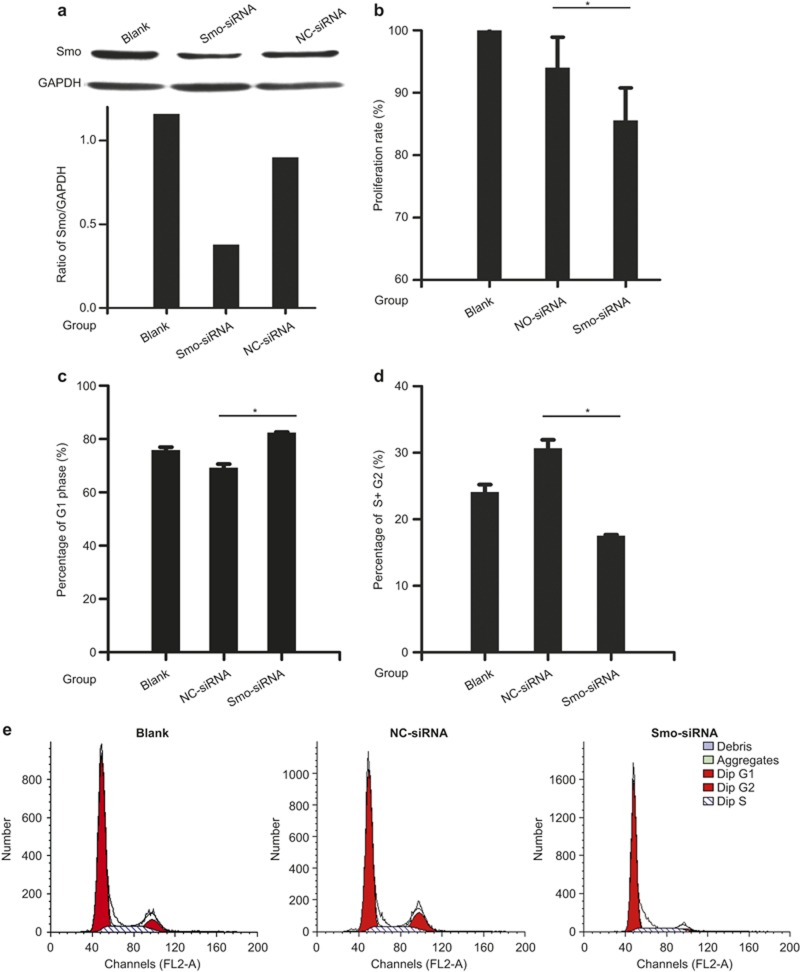
Knockdown of Smo mediated by siRNA decreases FLSs proliferation and induces G1 cell cycle arrest
Based on the above findings, we utilized RNA interference as an alternative approach to further investigate the role of Shh signaling in FLSs proliferation. FLSs were transfected with a NC-siRNA and a siRNA directed against Smo. After 48 hours of incubation with siRNAs, western blot analysis was performed. Relative Smo expression was evaluated and normalized to GAPDH, and the results revealed that the expression of Smo is predominantly inhibited in Smo-targeted siRNA-transfected cells versus NC-siRNA-transfected cells (Figure 2a). Cell proliferation was monitored using the CCK-8 assay and cell cycle distribution was performed using flow cytometry. The results of the CCK-8 assay showed that suppression of Smo decreases the proliferation of FLSs, with a cell proliferation rate of 85.64% ± 5.26%, compared to that of the NC-siRNA group (94.04% ± 4.95%, P < 0.05)(Figure 2b). The results of flow cytometry showed that transfection of Smo-siRNA contributes to accumulation of cells in the G1 phase (82.45% ± 0.15%), when compared to NC-siRNA controls (69.33% ± 1.3%, P <0.05) (Figure 2c). The percentages of cells in the S and G2 phase were significantly decreased after Smo-siRNA transfection (17.55% ± 0.15% versus 30.67% ± 1.28%, P < 0.05) (Figure 2d).
Figure 2.
Knockdown of Smo by siRNA decreases FLSs proliferation and induces G1 cell cycle arrest. FLSs were transfected with a negative control siRNA (NC-siRNA) and siRNA directed against Smo for 48 hours. The expression of Smo was measured by western blot analyses and Smo expression was evaluated and normalized to GAPDH (ratio of Smo/GAPDH) (a). Cell proliferation (b) and cell cycle progression (c, d, e) were determined by CCK-8 assay and flow cytometry, respectively. Data are presented as means ± S.D. of three independent experiments. *P < 0.05 versus NC-siRNA group.
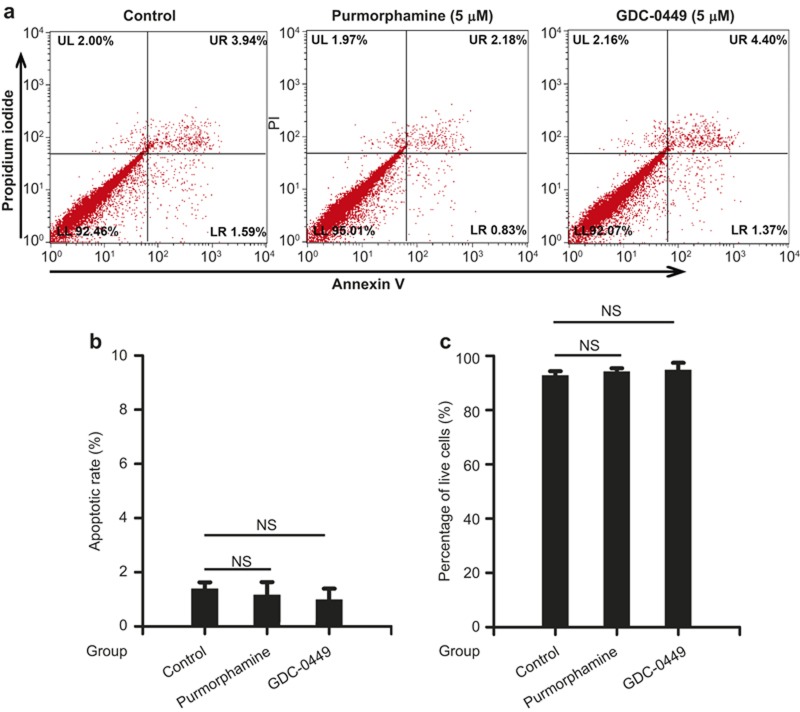
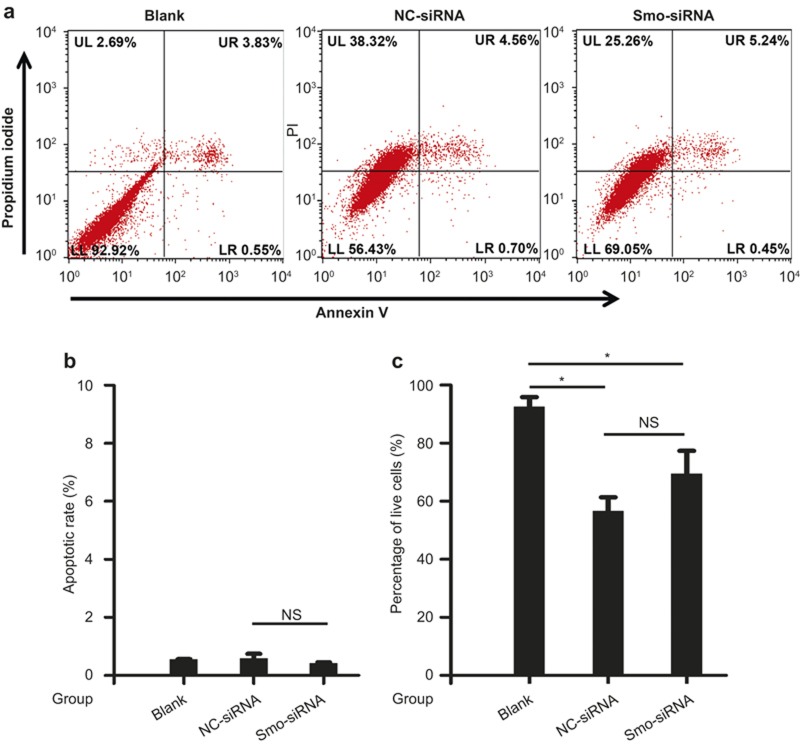
Smo antagonist and knockdown of Smo mediated by siRNA do not affect FLSs apoptosis
To investigate whether the decrease in proliferation seen after GCD-0449 treatment and Smo silencing is associated with an increase in apoptosis, we utilized Annexin V and PI staining. We found that FLSs incubated with GCD-0449 showed a low level of apoptosis, with cell apoptotic rate of 0.99% ± 0.40%, compared to that of the control group (1.39% ± 0.23%, P > 0.05). Treatment of purmorphamine did not affect the apoptosis of FLSs (Figure 3b). As shown in Figure 4, FLSs treated with NC-siRNA and Smo-siRNA displayed enhanced PI staining compared to the blank group (P < 0.05), suggesting that siRNA transfection caused a non-specific cytotoxic effect in the apoptosis assay, while the percentages of early apoptotic cells (Annexin V positive and PI negative) were not statistically different between the Smo-siRNA group and negative control group (P > 0.05) (Figure 4b). These results suggest that Smo downregulation does not significantly affect apoptosis, and apoptosis does not significantly contribute to the inhibition of proliferation induced by Smo suppression.
Figure 3.
Smo agonist and antagonist do not affect FLSs apoptosis. FLSs were cultured and serum-starved for 18 hours before incubation with GDC-0449 (5 μM) or purmorphamine (5 μM) for 48 hours. Cell apoptosis was determined by Annexin V and PI staining. Populations in the lower-right quadrant of the flow cytometric graph represented early apoptotic cells (a). The percentage of apoptotic cells (b) and live cells (c) was quantified. Data are represented as means ± S.D. of three independent experiments. NS: not significant.
Figure 4.
Knockdown of Smo by siRNA does not affect FLSs apoptosis. FLSs were cultured and transfected with small interfering RNAs (NC, Smo) for 48 hours. Cell apoptosis was determined by Annexin V and PI staining. Populations in the lower-right quadrant of the flow cytometric graph represented early apoptotic cells (a). The percentage of apoptotic cells (b) and live cells (c) was quantified. Data are represented as means ± S.D. of three independent experiments. *P < 0.05 versus control group. NS: not significant.
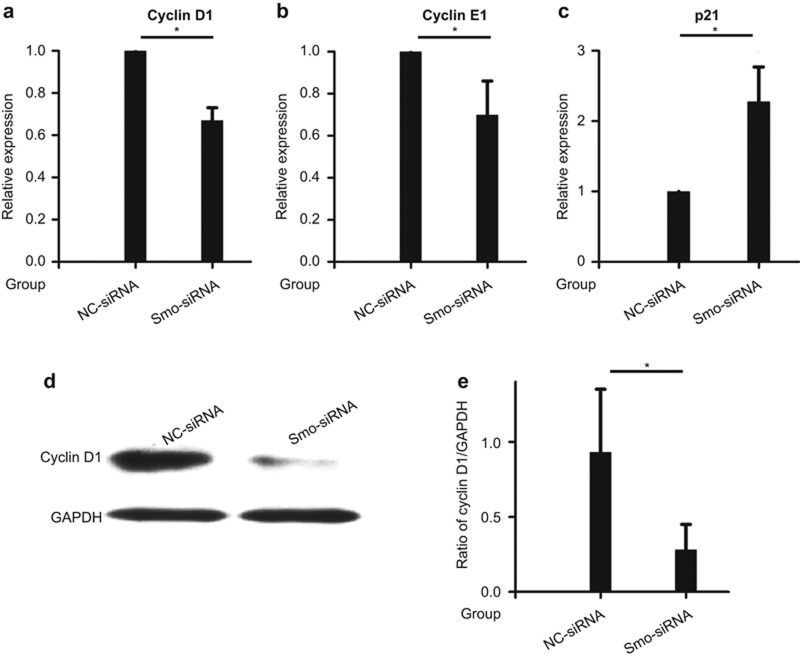
Knockdown of Smo mediated by siRNA affects the mRNA and protein expression of cell cycle-related genes
To further investigate how the Smo silencing impacts FLSs proliferation and cell cycle activity, we determined their impact on the expression of key cell cycle markers using real-time PCR and western blot analyses. Suppression of cyclin D1 and cyclin E1 mRNA expression was evident following Smo-siRNA transfection (Figure 5a and 5b), while this treatment induced an increase of cyclin-dependent kinase inhibitor p21 mRNA (Figure 5c). Smo-targeted siRNA also significantly inhibited the protein expression of cyclin D1 in FLSs (Figure 5d and 5e). These results indicate that the anti-proliferative effects of Smo silencing may be mediated by inhibiting G1 phase progression and G1/S transition through regulating the expression of cell cycle-related genes.
Figure 5.
Knockdown of Smo by siRNA affects the mRNA and protein expression of cell cycle-related genes. The level of mRNA expression of cyclin D1 (a), cyclin E1 (b), and p21/CIP1 (c) were evaluated using real time-PCR. Relative quantification of gene expression was performed by the 2−ΔΔCt method. The level of protein expression of cyclin D1 (d) was estimated using western blot analysis. Expression of cyclin D1 protein was quantified using GAPDH as an internal control (e). Data are represented as means ± S.D. of three independent experiments. *P < 0.05 versus NC-siRNA group. p21/CIP1: p21/cyclin-dependent kinase-interacting protein 1.
Discussion
Excessive proliferation of FLSs and synovial angiogenesis are the most important contributors to the progression of RA synovitis. In our previous study, we found that Shh signaling components including Shh, Smo, and Gli1 are overexpressed in RA synovium.14 Given the tumor-like behavior of FLSs, we hypothesize that Shh might function to induce FLSs proliferation and contribute to hyperplasia of RA synovium.
In the present study, we showed that upregulation of Smo promotes proliferation of FLSs, whereas inhibition of Smo induces growth suppression of FLSs, indicating that Shh signaling is involved in the proliferation of FLSs, and that Smo may play a critical role in the regulation of FLSs growth. However, it remains unclear how Shh signaling promotes FLSs proliferation, and its role in the pathogenesis of RA. It has been reported that pro-inflammatory cytokines promote synovitis and play key roles in the pathogenesis of RA. Studies have shown that tumor-necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6) can upregulate Shh expression and promote cell proliferation, contributing to tumor growth.16,17 Suppression of Shh signaling by pharmacologically targeting the Smo receptor resulted in downregulation of TNF-α and IL-1β mRNA expression in cholestatic rat liver.18 Heller et al. showed that knockdown of the Shh ligand decreases IL-6 production in tumor–stromal cells, revealing a paracrine role for Shh signaling in tumor–stromal cell interactions.19 Our results showed that FLSs are directly responsive to Shh signaling. Whether synovium-derived Shh ligands can stimulate synovial hyperplasia via the microenvironment, as well as the connection between the cytokines TNF-α and IL-6 and the Shh pathway in RA remains to be further investigated.
Pannus formation in RA may stem from an imbalance between proliferation and apoptosis of FLSs. An earlier study reported that FLSs from RA patients expand in a monoclonal fashion and display enhanced growth ability compared to synoviocytes in osteoarthritis (OA).20 Moreover, the protein levels of cell cycle-related genes, cyclin A and B1 were significantly higher in synovial tissues of RA patients than in those of OA patients or patients with traumatic arthritis.21 Experiments using adjuvant arthritis in rats have shown that gene therapy with p21/cyclin-dependent kinase-interacting protein 1 (CIP1) inhibits the growth of FLSs and exerts anti-inflammatory effects.22 It is possible that the deregulation of cell cycle progression involves multiple pathways and molecules ultimately leading to overgrowth of FLSs. Here, we demonstrated that suppression of Shh signaling by targeting Smo downregulation results in loss of cell cycle progression and G1/S transition in FLSs.
Several studies have shown that the distinct ability of Shh to induce cell proliferation may be due to its direct connection with the principal G1 cell-cycle regulator, cyclins.23,24 Furthermore, the Ptch1 protein is reported to cause cell cycle arrest by inhibiting the translocation of cyclin B1 from the cytoplasm to the nucleus.25 In addition, Shh signaling has been described to negatively regulate p21/CIP1, a suppressor of the G1/S transition.26 We now demonstrate that the disruption of Smo by siRNA negatively regulated the expression of cyclin D1 and E1 while increasing p21/CIP1 expression in FLSs, further validating observations previously reported in other cell types. Thus, our results suggest that Shh signaling promotes cell cycle progression in FLSs through interactions with G1 cyclins and a cyclin-dependent kinase inhibitor, providing further support for the role of Shh in the proliferation of FLSs. However, whether suppression of Shh signaling has anti-inflammatory effects via upregulation of p21/CIP1 is still not known.
Reduced apoptosis of FLSs is another important mechanism associated with synovial hyperplasia of RA. However, we found that inhibition of Smo does not induce apoptosis in FLSs. Previous studies have indicated that Shh signaling exerts its anti-apoptotic effect in a Smo-independent manner.27,28 Therefore, it will be necessary to further explore the effects of Ptch1 and Gli1 in the regulation of apoptosis to gain a better understanding of Shh signaling in the pathogenesis of RA.
Conclusion
In the current investigation, we elucidated the impact of the Shh signaling pathway in FLS proliferation and advanced the understanding of the molecular mechanisms by which the Shh pathway is linked to cell cycle regulation. These findings may provide important insights into the pathogenesis of RA and implicate a potential therapeutic strategy to control hyperplasia of synovium in RA.
Acknowledgments
This work was supported in part by grants from the National Natural Science Foundation of China (81072480), from the Natural Science Foundation of Guangdong Province (S2012020010927), and from the Science and Technology Program of Guangdong Province (2013B021800076) (Jian-lin Huang); the major projects from Science and Technology Program of Guangzhou City, from the National Natural Science Foundation of Guangdong Province, from the Department of Education of Guangdong Province, and grants from NIH AR059103 and NIH AI084359 (Song Guo Zheng).
References
- Tak PP, Bresnihan B. The pathogenesis and prevention of joint damage in rheumatoid arthritis: advances from synovial biopsy and tissue analysis. Arthritis Rheum 2000; 43: 2619–2633. [DOI] [PubMed] [Google Scholar]
- Mor A, Abramson SB, Pillinger MH. The fibroblast-like synovial cell in rheumatoid arthritis: a key player in inflammation and joint destruction. Clin Immunol 2005; 115: 118–128. [DOI] [PubMed] [Google Scholar]
- Pap T, Nawrath M, Heinrich J, Bosse M, Baier A, Hummel KM et al. Cooperation of Ras- and c-Myc-dependent pathways in regulating the growth and invasiveness of synovial fibroblasts in rheumatoid arthritis. Arthritis Rheum 2004; 50: 2794–2802. [DOI] [PubMed] [Google Scholar]
- Nasu K, Kohsaka H, Nonomura Y, Terada Y, Ito H, Hirokawa K et al. Adenoviral transfer of cyclin-dependent kinase inhibitor genes suppresses collagen-induced arthritis in mice. J Immunol 2000; 165: 7246–7252. [DOI] [PubMed] [Google Scholar]
- Chiang C, Litingtung Y, Lee E, Young KE, Corden JL, Westphal H et al. Cyclopia and defective axial patterning in mice lacking sonic hedgehog gene function. Nature 1996; 383: 407–413. [DOI] [PubMed] [Google Scholar]
- Ryan KE, Chiang C. Hedgehog secretion and signal transduction in vertebrates. J Biol Chem 2012; 287: 17905–17913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson CW, Chuang PT. Mechanism and evolution of cytosolic hedgehog signal transduction. Development 2010; 137: 2079–2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varjosalo M, Taipale J. Hedgehog: functions and mechanisms. Genes Dev 2008; 22: 2454–2472. [DOI] [PubMed] [Google Scholar]
- Walter K, Omura N, Hong SM, Griffith M, Vincent A, Borges M et al. Overexpression of smoothened activates the sonic hedgehog signaling pathway in pancreatic cancer-associated fibroblasts. Clin Cancer Res 2010; 16: 1781–1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yauch RL, Gould SE, Scales SJ, Tang T, Tian H, Ahn CP et al. A paracrine requirement for hedgehog signalling in cancer. Nature 2008; 455: 406–410. [DOI] [PubMed] [Google Scholar]
- Sekulic A, Migden MR, Oro AE, Dirix L, Lewis KD, Hainsworth JD et al. Efficacy and safety of vismodegib in advanced basal-cell carcinoma. N Engl J Med 2012; 366: 2171–2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen M, Lauterbach K, El-Gabalawy H, Firestein GS, Corr M, Carson DA. Expression and function of wingless and frizzled homologs in rheumatoid arthritis. Proc Natl Acad Sci USA 2000; 97: 2791–2796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lories RJ, Derese I, Ceuppens JL, Luyten FP. Bone morphogenetic proteins 2 and 6, expressed in arthritic synovium, are regulated by proinflammatory cytokines and differentially modulate fibroblast-like synoviocyte apoptosis. Arthritis Rheum 2003; 48: 2807–2818. [DOI] [PubMed] [Google Scholar]
- Zhu SL, Luo MQ, Peng WX, Li QX, Feng ZY, Li ZX et al. Sonic hedgehog signalling pathway regulates apoptosis through Smo protein in human umbilical vein endothelial cells. Rheumatology (Oxford) 2015; 54: 1093–1102. [DOI] [PubMed] [Google Scholar]
- Wang M, Zhu S, Peng W, Li Q, Li Z, Luo M et al. Sonic hedgehog signaling drives proliferation of synoviocytes in rheumatoid arthritis: a possible novel therapeutic target. J Immunol Res 2014; 2014: 401903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988; 31: 315–324. [DOI] [PubMed] [Google Scholar]
- Kasperczyk H, Baumann B, Debatin KM, Fulda S. Characterization of sonic hedgehog as a novel NF-kappaB target gene that promotes NF-kappaB-mediated apoptosis resistance and tumor growth in vivo. FASEB J 2009; 23: 21–33. [DOI] [PubMed] [Google Scholar]
- Su YC, Li SC, Wu YC, Wang LM, Chao KS, Liao HF. Resveratrol downregulates interleukin-6-stimulated sonic hedgehog signaling in human acute myeloid leukemia. Evid Based Complement Alternat Med 2013; 2013: 547430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pratap A, Panakanti R, Yang N, Lakshmi R, Modanlou KA, Eason JD et al. Cyclopamine attenuates acute warm ischemia reperfusion injury in cholestatic rat liver: hope for marginal livers. Mol Pharm 2011; 8: 958–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heller E, Hurchla MA, Xiang J, Su X, Chen S, Schneider J et al. Hedgehog signaling inhibition blocks growth of resistant tumors through effects on tumor microenvironment. Cancer Res 2012; 72: 897–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imamura F, Aono H, Hasunuma T, Sumida T, Tateishi H, Maruo S et al. Monoclonal expansion of synoviocytes in rheumatoid arthritis. Arthritis Rheum 1998; 41: 1979–1986. [DOI] [PubMed] [Google Scholar]
- Takahashi TC, Yamakawa M, Murasawa A, Nakazono K, Ishikawa H. Local cell proliferation in rheumatoid synovial tissue: analysis by cyclin expression. Clin Rheumatol 2006; 25: 801–806. [DOI] [PubMed] [Google Scholar]
- Nonomura Y, Kohsaka H, Nagasaka K, Miyasaka N. Gene transfer of a cell cycle modulator exerts anti-inflammatory effects in the treatment of arthritis. J Immunol 2003; 171: 4913–4919. [DOI] [PubMed] [Google Scholar]
- Li F, Duman-Scheel M, Yang D, Du W, Zhang J, Zhao C et al. Sonic hedgehog signaling induces vascular smooth muscle cell proliferation via induction of the G1 cyclin-retinoblastoma axis. Arterioscler Thromb Vasc Biol 2010; 30: 1787–1794. [DOI] [PubMed] [Google Scholar]
- Duman-Scheel M, Weng L, Xin S, Du W. Hedgehog regulates cell growth and proliferation by inducing cyclin D and cyclin E. Nature 2002; 417: 299–304. [DOI] [PubMed] [Google Scholar]
- Barnes EA, Kong M, Ollendorff V, Donoghue DJ. Patched1 interacts with cyclin B1 to regulate cell cycle progression. EMBO J 2001; 20: 2214–2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohta M, Tateishi K, Kanai F, Watabe H, Kondo S, Guleng B et al. p53-independent negative regulation of p21/cyclin-dependent kinase-interacting protein 1 by the sonic hedgehog-glioma-associated oncogene 1 pathway in gastric carcinoma cells. Cancer Res 2005; 65: 10822–10829. [DOI] [PubMed] [Google Scholar]
- Chinchilla P, Xiao L, Kazanietz MG, Riobo NA. Hedgehog proteins activate pro-angiogenic responses in endothelial cells through non-canonical signaling pathways. Cell Cycle 2010; 9: 570–579. [DOI] [PubMed] [Google Scholar]
- Thibert C, Teillet MA, Lapointe F, Mazelin L, Le DNM, Mehlen P. Inhibition of neuroepithelial patched-induced apoptosis by sonic hedgehog. Science 2003; 301: 843–846. [DOI] [PubMed] [Google Scholar]