Abstract
Pathologic angiogenesis appears to be intrinsically associated with the fibrogenic progression of chronic liver diseases, which eventually leads to the development of cirrhosis and related complications, including hepatocellular carcinoma. Several laboratories have suggested that this association is relevant for chronic liver disease progression, with angiogenesis proposed to sustain fibrogenesis. This minireview offers a synthesis of relevant findings and opinions that have emerged in the last few years relating liver angiogenesis to fibrogenesis. We discuss liver angiogenesis in normal and pathophysiologic conditions with a focus on the role of hypoxia and hypoxia-inducible factors and assess the evidence supporting a clear relationship between angiogenesis and fibrogenesis. A section is dedicated to the critical interactions between liver sinusoidal endothelial cells and either quiescent hepatic stellate cells or myofibroblast-like stellate cells. Finally, we introduce the unusual, dual (profibrogenic and proangiogenic) role of hepatic myofibroblasts and emerging evidence supporting a role for specific mediators like vasohibin and microparticles and microvesicles.
Keywords: Hypoxia, Liver Angiogenesis, Liver Fibrogenesis, Myofibroblasts
Abbreviations used in this paper: Akt, protein kinase B; Ang-1, angiopoietin-1; ANGPTL3, angiopoietin-like-3 peptide; CCL2, chemokine ligand 2; CCR, chemokine receptor; CLD, chronic liver disease; eNOS, endothelial nitric oxide synthase; ET-1, endothelin 1; HCC, hepatocellular carcinoma; Hh, Hedgehog; HIF, hypoxia-inducible factor; HSC, hepatic stellate cell; HSC/MFs, myofibroblast-like cells from activated hepatic stellate cells; LSEC, liver sinusoidal endothelial cell; MF, myofibroblast; MP, microparticle; NAFLD, nonalcoholic fatty liver disease; NASH, nonalcoholic steatohepatitis; NO, nitric oxide; PDGF, platelet-derived growth factor; ROS, reactive oxygen species; α-SMA, α-smooth muscle actin; VEGF, vascular endothelial growth factor; VEGF-R2, vascular endothelial growth factor receptor type 2
Summary.
Pathologic angiogenesis is intrinsically associated with the fibrogenic progression of chronic liver diseases. Hypoxia, hypoxia-inducible factors, and other signals and mediators released by various cells of the liver drive and modulate the critical profibrogenic and proangiogenic role of hepatic myofibroblasts.
Angiogenesis and Liver Fibrogenesis
Fibrogenic progression of chronic liver diseases (CLDs), eventually leading to the development of liver cirrhosis and related complications including hepatocellular carcinoma (HCC), is intimately associated with pathologic angiogenesis and sinusoidal remodeling.1, 2, 3, 4, 5, 6 This is not surprising because angiogenesis is a major feature of any wound healing response and chronic activation of wound healing is a general mechanism involved in the progression of CLDs.7, 8, 9, 10 Some researchers, including the authors of this review, go further2, 3, 4, 9, 10, 11, 12, 13, 14, 15 in suggesting additionally that 1) hypoxia (the most obvious stimulus for angiogenesis, commonly detected in progressive CLDs1, 2, 3, 4, 5, 6, 16), hypoxia-inducible factors (HIFs), and angiogenesis may have a major role in sustaining and potentially driving liver fibrogenesis; 2) hepatic myofibroblasts (MFs), regardless of origin, are critical cells in governing and modulating the interactions between inflammation, angiogenesis, and fibrogenesis; 3) liver angiogenesis has a role in the genesis of portal hypertension and related complications in advanced stages of CLDs; and 4) microparticles/microvesicles released by either fat-laden hepatocytes or portal MFs have an emerging role in mediating angiogenesis and vascular remodeling. This review offers a synthesis of the most relevant recent data and opinions regarding the close relationship between liver angiogenesis and fibrogenesis. Established concepts about mechanisms of liver angiogenesis, liver fibrogenesis, and CLD progression will not be addressed. Moreover, in this review, the relationship between angiogenesis and portal hypertension and related complications are not discussed; readers interested in this specific topic should refer to a recent authoritative review.13
Angiogenesis in the Liver: General Considerations
Liver angiogenesis occurs in both physiologic (ie, liver regeneration) and pathologic conditions, including ischemia, progressive CLDs, hepatocellular carcinoma, and metastatic liver cancer.1, 2, 3, 4, 5 Angiogenesis in the liver is similar to angiogenesis in other tissues and organs; however, as suggested by several groups,1, 2, 3, 4, 5, 10, 11, 12 pathologic angiogenesis occurring during the progression of CLDs can be significantly affected by liver-specific events, interactions between different hepatic cell populations, and the involvement of atypical proangiogenic mediators.
From a general point of view, the pattern of fibrosis that predominates in a specific CLD is relevant to angiogenesis. Although pathologic liver angiogenesis has been described in all CLDs irrespective of etiology, it is much more prominent under conditions of bridging or postnecrotic fibrosis (eg, in chronic viral infection or, to a lesser extent, in autoimmune diseases) than in conditions characterized by pericellular or perisinusoidal fibrosis (as in non-alcoholic fatty liver disease or alcoholic liver disease) or by biliary fibrosis.3, 9, 10 This suggests an inverse correlation between angiogenesis and the potential for fibrosis reversibility, which is more evident in conditions characterized by pericellular or perisinusoidal fibrosis and biliary fibrosis than in those associated with bridging fibrosis.9 This may be related to the unique tissue localization, phenotypic profile, and functional role of hepatic stellate cells (HSCs).
HSCs, which in physiologic conditions synthesize extracellular matrix components in the space of Disse, store retinoids and possibly contract in response to vasoactive mediators to modulate sinusoidal blood flux, are also liver-specific pericytes. During the progression of CLDs, HSCs are the most relevant myofibroblast precursors and profibrogenic hepatic cells.2, 17, 18, 19, 20, 21 HSCs, particularly in their activated and MF-like phenotype (HSC/MFs), modulate angiogenesis in a way that, as we will describe, relates to the role attributed to them as microcapillary pericytes. Hepatic MFs, a heterogenous population of profibrogenic, highly proliferative, and contractile cells, can also originate from portal MFs and bone marrow-derived stem cells recruited into the injured liver, and these may also play a role in angiogenesis.17, 18, 19, 20, 21, 22
The relevance of intense cross-talk between hepatic cell populations in pathologic angiogenesis is strongly supported by the knowledge that major proangiogenic mediators such as vascular endothelial growth factor (VEGF) and platelet-derived growth factor (PDGF), are produced and released by several liver cell types involved in CLD progression, including hypoxic hepatocytes and hypoxia-responsive macrophages and MFs.1, 2, 3, 9, 10, 11, 12 The role of liver-specific proangiogenic mediators such as angiopoietin-like-3 peptide (ANGPTL3)23 is controversial. ANGPTL3, which belongs to a family of mediators described as playing major roles in the trafficking and metabolism of lipids, was reported to induce haptotactic endothelial cell adhesion and migration, possibly by binding to αvβ3 integrin.23 However, no further studies have been published on the role of this mediator in either physiologic or pathologic liver angiogenesis. As we will discuss, a more interesting role is attributed to the antiangiogenic protein vasohibin, which may have a dual role in inhibiting not only angiogenesis but also fibrogenesis, likely by deactivating HSCs.24
Hypoxia, Pathologic Angiogenesis, and Liver Fibrogenesis: Interconnected Events
Angiogenesis is best defined as a dynamic, hypoxia-stimulated, and growth factor-dependent process leading to the formation of new blood vessels from preexisting ones.25, 26 Hypoxia and HIFs are critical in sustaining the fibrogenic progression of CLDs, representing a persistent driving force able to directly affect the behavior of hepatic cell populations, including profibrogenic and proangiogenic MFs.1, 2, 3, 4, 5, 10, 11, 12, 13, 16
Detection of hypoxic areas is a common finding at any stage of CLD, increasing progressively from early injury to the development of cirrhosis, with hypoxia and HIFs serving throughout as proangiogenic stimuli in the overall, etiology-independent scenario of chronic wound healing. CLD progression itself is a major contributor to hypoxia due to the formation of regenerative nodules of parenchyma surrounded by evolving fibrotic septa and vascular remodeling that, along with progressive capillarization of the sinusoids, leads to an impairment of oxygen diffusion. A vicious circle between fibrosis and pathologic angiogenesis is likely to occur10, 12, 27 in which parenchymal hypoxia, through the action of HIFs, up-regulates expression of wound healing-related factors and mediators that should facilitate liver repair and revascularization. However, pathologic angiogenesis can be inefficient due to the immaturity and permeability of VEGF-induced neovessels and, as a result, may be unable to correct liver hypoxia. Pathologic angiogenesis and hypoxia may act synergistically in disrupting normal tissue repair, thereby promoting the development of liver fibrosis.27
The connection between pathologic angiogenesis and fibrogenesis in progressive CLDs is strongly suggested by their parallel development in all major human forms of CLD and animal models of CLDs, with several laboratories describing high numbers of endothelial cells and microvascular structures within fibrotic septae and in expanded portal areas.1, 2, 3, 4, 5, 10, 11, 12, 13, 16, 28, 29, 30 The response to hypoxia and VEGF (the major proangiogenic target gene) expression can be seen in liver sinusoidal endothelial cells (LSECs) and in hepatocytes1, 3, 4, 10, 28 and HSC/MFs of developing septa and at the borders of more mature and larger fibrotic septa.29, 30
Studies performed in HIF-1α liver conditional knockout mice provided the first definitive in vivo evidence for hypoxia-dependent induction of fibrogenesis.31 However, the most convincing evidence relating angiogenesis and fibrogenesis came through in vivo studies indicating that experimental antiangiogenic therapy was highly effective in significantly reducing fibrogenic progression. As summarized in Table 1, whatever the specific molecule or tool employed, experimental antiangiogenic therapy always resulted in a significant reduction not only of angiogenesis but also of the inflammatory infiltrate, the number of α-smooth muscle actin (α-SMA)-positive MFs and the extent of fibrosis.32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42 In some studies, experimental antiangiogenic therapy also resulted in a significant reduction of portal pressure and collateral vessel formation, as reported with sorafenib in cirrhotic animals34, 43 and with different molecules and tools in portal hypertensive animals.9, 24, 44, 45, 46, 47, 48, 49
Table 1.
Published Studies Examining Antiangiogenic Therapy in Rodent Models of Chronic Liver Disease
| Antiangiogenic Molecule | Mode of Action | Major Findings | References |
|---|---|---|---|
| Sunitinib (SU11248) | Inhibition of multitargeted receptor tyrosine kinase | Decrease in hepatic vascular density, inflammatory infiltrate, α-SMA abundance, collagen expression, and portal pressure in cirrhotic rats | 32 |
| Sorafenib | Inhibition of VEGF-R2, PDGF-Rβ and RAF/MEK/ERK pathway | Decrease in splanchnic neovascularization, hyperdynamic splanchnic and systemic circulations, extent of portosystemic collaterals, portal pressure; improvement in liver damage and intrahepatic fibrosis, inflammation, and angiogenesis in cirrhotic rats | 34, 43 |
| Neutralizing monoclonal antibodies for VEGF-R2 | Neutralization of VEGF-R2 | Reduction in fibrosis and suppression of hepatic neovascularization | 35 |
| Neutralizing monoclonal antibodies for PlGF | Neutralization of PIGF | Reduction in angiogenesis, arteriogenesis, inflammation, fibrosis, and portal hypertension in cirrhotic mice | 36 |
| Adenovirus expressing soluble Tie2 (AdsTie2) | Binds angiopoietin 1 and blocks angiopoietin signaling | Inhibition of liver fibrosis both induced by CCl4 and BDL in mice; reduction in collagen and number of activated myofibroblasts | 37 |
| Cxcl9 | Reduction in VEGF-R2, phospholipase Cγ and ERK phosphorylation | Inhibition of proliferation and migration of VEGF-stimulated endothelial cells and stellate cells; attenuation of neoangiogenesis and experimental liver fibrosis in mice | 38 |
| Cannabinoid receptor 2 agonist | Stimulation of cannabinoid signalling | Improvement of portal hypertension, portosystemic collaterals, and mesenteric and intrahepatic angiogenesis as well as fibrosis in cirrhotic rats | 39 |
| AM1241 and F13A | Stimulation of CB2 receptor (AM1241) and apelin receptor blockade (F13A) | Reduction in fibrosis, improvement of portal pressure, improved cell viability, reduction in angiogenesis and cell infiltration in cirrhotic rats | 40 |
| Largazole | Inhibition of histone deacetylase | Inhibition of HSCs activation, TGF-β and VEGF signaling and induction of HSCs apoptosis; inhibition of fibrosis, angiogenesis, and inflammation in cirrhotic mice | 41 |
| Rifaximin | Inhibition of TLR4 dependent fibronectin-mediated cross-talk between HSCs and endothelial cells | Decrease in portal pressure, fibrosis, angiogenesis and fibronectin deposition in BDL mice | 42 |
| Monoclonal antibody against VEGF-R2 and inhibitor of VEGF-R2 autophosphorylation | Neutralization of VEGF-R2 or block of VEGF-R2 phosphorylation | Inhibition in the formation of portal-systemic collateral vessels in partial portal vein-ligated mice and rats | 44 |
| SU5416 | Inhibition of VEGF-R2 | Decrease in hyperdynamic splanchnic circulation, and portal-systemic collateral vessels in portal hypertensive rats | 45 |
| Rapamycin and Gleevec | VEGF signaling inhibition (rapamycin), PDGF signaling inhibition (Gleevec) | Reduction in splanchnic neovascularization and pericyte coverage of neovessels; decrease in portal pressure and portosystemic collateralization in portal vein-ligated rats | 46 |
| Octreotide | Inhibition of cell proliferation and neovascularization | Decrease in splanchnic neovascularization, VEGF expression at early stages, but not in advanced stages, of portal hypertension in cirrhotic rats | 47 |
| F13A | APJ receptor blockade (F13A or apelin receptor antagonist) | Decrease in splanchnic neovascularization, expression of the proangiogenic factors VEGF, PDGF, and ang-2, reduction in formation of portosystemic collateral vessels in portal hypertensive rats | 48 |
| Pigment epithelium-derived factor (PEDF) | Cleavage of VEGF-R1 transmembrane domain, interference with VEGF signaling | Attenuation of portal hypertension-associated pathological neovascularization; decrease in liver fibrosis, portosystemic collateralization and portal pressure in BDL rats | 49 |
| Vasohibin (VASH) | Reversal of VASH-induced negative feedback loop of VEGF angiogenesis | VASH overexpression results in reduction of pathologic angiogenesis, attenuation of liver fibrosis, decreases in portocollateralization, splanchnic blood flow, portohepatic resistance, and portal pressure | 24 |
Note: AM1241, (2-iodo-5-nitrophenyl)-[1-[(1-methylpiperidin-2-yl)methyl]indol-3-yl]methanone; BDL, bile duct ligation; CB2, cannabinoid type 2 receptor; CCl4, carbon tetrachloride; Cxcl9 chemokine (C-X-C motif) ligand 9; F13A, Gln-Arg-Pro-Arg-Leu-Ser-His-Lys-Gly-Pro-Met-Pro-Ala; HSCs, hepatic stellate cells; PDGF, platelet-derived growth factor; PIGF, placental growth factor; RAF/MEK/ERK, Raf/mitogen-activated protein (MAP) kinase kinase/extracellular signal-regulated kinase; α-SMA, α-smooth muscle actin; SU5416, semaxanib; TGF-β, transforming growth factor-β; TLR4, Toll-like receptor 4; VASH, vasohibin; VEGF, vascular endothelial growth factor; VEGF-R2, vascular endothelial growth factor receptor type 2.
To our knowledge, only two studies have been published that represent exceptions to this general finding. The first one was published in 2009 by Patsenker et al,50 who reported that pharmacologic inhibition of integrin ανβ3 by cilengitide, although able to suppress liver angiogenesis, significantly worsened experimental liver fibrosis. A second experimental and clinical study suggested that the development of liver fibrosis was associated with decreased expression of VEGF and sinusoidal rarefication of the fibrotic scar.51 These investigators reported that experimental resolution of fibrosis was accompanied by an increase in hepatic VEGF levels and revascularization of fibrotic septa, events that were prevented by ablating VEGF in myeloid cells or through pharmacologic inhibition of vascular endothelial growth factor receptor type 2 (VEGF-R2) signaling.
The question of whether available antiangiogenic drugs might be useful in treating patients with cirrhosis and portal hypertension remains unanswered, with some positive data reported in cirrhotic patients with HCC;52 however, several significant concerns were raised53 related to the known severe side effects of these drugs (eg, sorafenib) as well as the increased risk of bleeding reported in cirrhotic patients with HCC.54 On the other hand, although VEGF is unequivocally a critical profibrogenic mediator and has a well-established role in endothelial cell survival and proliferation, it may have also a role in fibrosis resolution.55 While blocking the interaction between VEGF and VEGF-R2 does not result (as hypothesized) in an improvement or acceleration of fibrosis resolution, the availability of VEGF is critical in chemokine (C-X-C motif) ligand 9 (CXCL9)- and matrix metalloprotease 13 (MMP13)-dependent fibrosis resolution in different murine models of fibrosis. This apparent paradox is explained by the fact that blocking VEGF-R2 effectively blocks VEGF-dependent recruitment of mononuclear cells and changes in vascular permeability. Blocking VEGF-R2 thereby potentially reduces the recruitment of “resolution” macrophages, which have an important role in fibrosis reversal. Indeed, in that study, the degree of impairment of fibrosis resolution obtained by blocking VEGF-R2 was nearly identical to that seen with macrophage depletion.55
Macrophages and Inflammation in Relation to Angiogenesis
Chronic liver inflammation is a key requirement for the progression of liver fibrosis, but there is little known about its role in promoting fibrosis-associated angiogenesis. Although inflammation-associated angiogenesis may contribute to both initiation of CLDs and their progression toward cirrhosis and HCC, the available data refer primarily to HCC and to macrophages in the tumor microenvironment.56, 57, 58, 59 Studies performed using specimens from CLD patients and from mouse models have shown that chemokine-dependent accumulation of monocyte-derived macrophages represents a relevant mechanism for perpetuating hepatic inflammation and promoting fibrogenesis.60 In particular, the chemokine receptor 2 (CCR2) and its ligand CCL2 have a key role in promoting the accumulation of certain monocyte subsets in the liver, in particular Ly6C+ (Gr1+) monocytes. Macrophages derived from these monocytes release proinflammatory cytokines and can directly activate profibrogenic hepatic MFs.60
Accordingly, CCL2-dependent infiltrating macrophages are critical in sustaining angiogenesis in experimental models of CLDs. A study has shown that these cells promote angiogenic vessel sprouting, particularly in the portal vein system, by releasing VEGF-A and other potential proangiogenic factors such as matrix metalloprotease 9 (MMP9).61 This study convincingly demonstrated that angiogenesis is induced even at the initial stages of liver fibrosis and that hepatic neovascularization correlates with fibrosis stage. Infiltrating and CCL2-dependent inflammatory cells mediate induction of fibrosis-associated pathologic angiogenesis, and, accordingly, pharmacologic inhibition of CCL2 blocks angiogenesis in experimental fibrosis by inhibiting the infiltration of CCL2-dependent monocyte/macrophages.61
Hepatic MFs in CLD Progression: The Cells That Drive Both Angiogenesis and Fibrogenesis
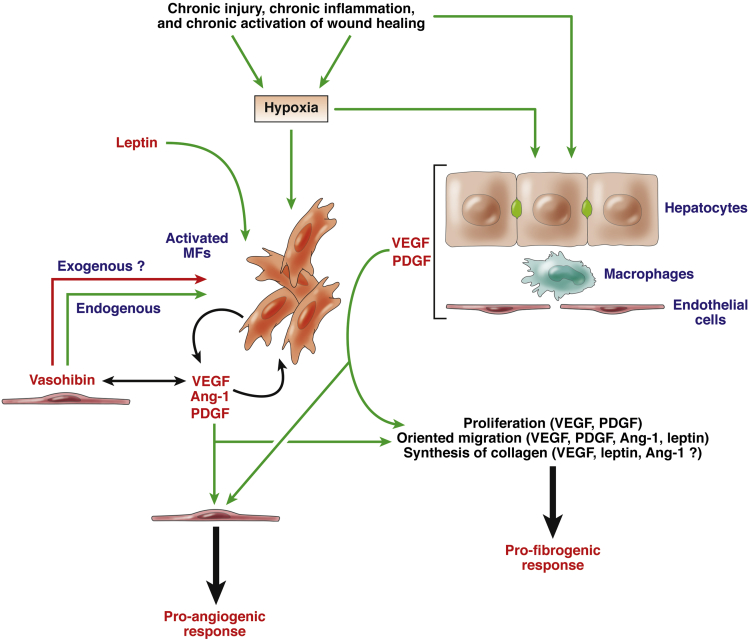
Hepatic MFs, particularly HSC/MFs, play a critical role in CLD progression through their unique ability to act as hypoxia-sensitive and cytokine- and chemokine-modulated cellular mediators at the crossroads between chronic liver injury, inflammation, pathologic angiogenesis, and fibrogenesis.1, 2, 3, 4, 5, 10 MFs are critical target cells, able to integrate signals from the microenvironment (including from hypoxia, contact with altered extracellular matrix, and plasma proteins) and from surrounding liver cells, acting as both profibrogenic and proangiogenic effector cells (see Figure 1). We propose that the overall proangiogenic role of MFs is the result of their interactions with surrounding hepatic cells and their exposure to the altered hepatic microenvironment during CLD progression. In the next sections, we focus particularly on LSECs and the relevance of the interactions between LSECs, HSC, and HSC/MFs, as well as on both hypoxia-dependent and hypoxia-independent responses of activated MFs.11
Figure 1.
Schematic representation of the critical role of activated myofibroblasts (MFs) in the scenario of a progressive chronic liver disease with the direct response to hypoxic conditions and the response to mediators released by other hepatic cell populations (under hypoxia or after chronic injury) or available in the microenvironment and being able to sustain both proangiogenic and profibrogenic role of MFs. Chronic conditions of injury as well as hypoxic conditions operate as efficient events/stimuli able to up-regulate transcription and release of critical proangiogenic mediators (with some also able to sustain fibrogenesis) by hepatocytes, endothelial cells, macrophages, or activated MFs (the latter cells being stimulated to produce proangiogenic cytokines also by leptin). Endogenous vasohibin 1 production is regulated by VEGF in a spatially and temporally coordinated way that operates a negative-feedback loop, driving pathologic angiogenesis through an overall positive effect on activation of HSCs and fibrogenic progression. However, it has been suggested that ectopic overexpression of this antiangiogenic protein (resulting in inhibition of fibrogenesis), being not regulated by VEGF, can disrupt the negative-feedback loop, thus generating constant but lower levels of VEGF synthesis, which are believed to be sufficient to maintain vascular homeostasis but not to sustain pathologic angiogenesis. Green and red arrows in the figure indicate stimulating or inhibitory effects, respectively.
Liver Sinusoidal Endothelial Cells and Their Interactions with Hepatic Stellate Cells or Myofibroblast-Like Cells From Activated Hepatic Stellate Cells
Under physiologic conditions, the intrahepatic vascular system is composed of different kinds of vessels, including liver sinusoids, portal venules, hepatic arterioles, central venules, and lymphatic vessels. These vessels are composed of endothelial cells and smooth muscle cells as well as, for liver sinusoids, HSCs, which act as liver specific pericytes. All these cells, plus resident Kupffer cells and other blood-derived cells, interact with each other. Signaling between these cells maintains sinusoidal homeostasis and is significantly altered in pathophysiologic conditions.62
LSECs represent the majority of liver endothelial cells and have a morphologic and functional phenotype that is strikingly different from that of endothelial cells of other vascular units in the liver and elsewhere. Fenestration and a lack of a typical basement membrane are predominant features of the LSEC phenotype but are lost in CLDs.62, 63 Under physiologic conditions, quiescent HSCs, which reside in the space of Disse and interact through their multiple processes with hepatocytes and LSECs, contribute to vitamin A and retinoid metabolism as well as to deposition and remodeling of the extracellular matrix in the space of Disse.64 Quiescent HSCs, which also interact with the axonal processes of autonomic nerve fibers, are liver-specific pericytes,65 able to respond to a variety of vasoactive mediators and may regulate sinusoidal blood flow through their perisinusoidal processes.62, 63, 64, 65, 66
The literature suggests that human HSCs contract mainly in response to endothelin-1 (ET-1), thrombin, and angiotensin-II, and relax in response to nitric oxide (NO) and NO donors, prostaglandin E2, somatostatin, and adrenomedullin.64, 65 There is considerable support for the paradigm that under conditions of chronic liver injury two features predominate: 1) overproduction of ET-1 by activated HSCs; and 2) a significant reduction in NO release by LSECs.62, 63, 64, 65
HSCs, which are a major source of ET-1, also represent a target for this vasoactive molecule during liver injury, with ET-1 (either from LSECs or activated HSCs, acting in a paracrine or autocrine way) exerting a prominent contractile effect on HSCs and MFs, and likely contributing to portal hypertension in the cirrhotic liver67, 68, 69 as well as having a growth inhibitory effect on HSC/MFs.70 During CLD progression, this results in an imbalance in vasoactive mediators and leads to abnormal sinusoids, with remodeling and constriction of the intrahepatic sinusoidal vasculature and a resulting increase in hepatic vascular resistance early in intrahepatic portal hypertension.62 As highlighted by Iwakiri et al,62 this differs from events in the mesenteric vascular bed, which are characterized by vasodilation and reduced resistance from up-regulation of vasodilators such as NO; this in turn leads to increased flow to the portal vein. The combined result of changes in the intrahepatic and mesenteric vasculature is an increase in intrahepatic resistance and portal blood flow from the splanchnic circulation, leading to increased portal pressure and portal hypertension.
Regulation of the phenotype of LSECs can be viewed as the net result of the action of different signals that include soluble factors (mainly VEGF, angiopoietins, ephrins, and fibroblast growth factors) and mechanical forces such as those due to shear stress. These signals are critical in modulating endothelial NO synthase (eNOS) activity in LSECs, resulting in the regulation of flow and vascular tone in the liver sinusoids.62, 71 LSECs release in a paracrine way several mediators that are involved in maintaining a “physiological” LSEC phenotype but also affect the early response of HSCs. For example, LSECs can produce the cellular isoform of fibronectin in response to injury; fibronectin has been reported to stimulate HSC synthesis of ET-1.72 ET-1, in turn, may differentially affect proliferation of HSCs, promoting proliferation in transiently activated HSCs but inhibiting it in fully activated HSCs.70, 73
During CLD progression, LSEC phenotype changes dramatically during the so-called capillarization of sinusoids in association with a reduction in eNOS activity and NO synthesis.62 This is possibly due to extensive posttranslational dysregulation of eNOS as a consequence of changes in phosphorylation or interactions with proteins such as calmodulin, caveolin-1, and protein kinase B (Akt).74, 75 The reduction in NO release by LSECs is believed to have a more direct role in sustaining fibrogenesis because NO contributes to the maintenance of quiescence of HSCs and may induce apoptosis or reversal of phenotype of activated HSCs, with reduced levels of NO facilitating HSC activation.76, 77 The scenario may be even more complex because HSCs can produce NO after injury,78 possibly in response to up-regulation of inducible NOS activity induced by proinflammatory cytokines or endotoxemia.62
LSECs produce mediators and factors that regulate both regeneration and fibrosis. LSECs, through interactions between VEGF and VEGF-R2, can release Wnt2 and hepatocyte growth factor, which sustain proliferation of hepatocytes;79 moreover, a significant amount of hepatocyte growth factor is also released by bone marrow-derived LSEC progenitor cells.80 LSECs from the livers of mice with biliary fibrosis have been reported to release profibrogenic mediators such as transforming growth factor β, bone morphogenetic protein 2, and PDGF-C and to decrease the release of putative antifibrotic factors such as follistatin and apelin.81
Hypoxia-Dependent Proangiogenic Response of Myofibroblasts
Increased expression of VEGF in specimens from fibrotic or cirrhotic patients colocalizes with areas of hypoxia and is mostly limited to hepatocytes and MFs.28, 29, 30 MFs respond to hypoxic conditions through HIF-1α-dependent up-regulation of VEGF and angiopoietin-1 (Ang-1) and of their respective receptors VEGF-R2 and Tie2.29, 80, 81, 82, 83, 84, 85 Exposure of HSC/MF to hypoxic conditions also results in HIF-1α-dependent up-regulation of CCR1, CCR5, macrophage migration inhibitory factor, interleukin-13 receptor-α1, prolyl-4-hydroxylase-α2, and (in part) placental growth factor, and HIF-1α-independent increased expression of angiopoietin-like 4 and prolyl-4-hydroxylase-α1.85 MFs can also directly respond to VEGF and Ang-1, with VEGF reported to elicit increased proliferation as well as increased synthesis of extracellular matrix components,28 and both VEGF and Ang-1 reported to stimulate oriented migration of HSC/MFs and MF-like cells from bone marrow-derived mesenchymal stem cells.30, 86, 87
Hypoxia alone is able to induce oriented migration of either HSC/MFs or MF-like cells by eliciting a biphasic mechanism involving 1) an early phase of migration, switched on by mitochondria-released reactive oxygen species (ROS) and requiring redox-dependent activation of extracellular-signal-regulated kinase and c-Jun-NH2-terminal kinase isoforms; and 2) a delayed and sustained phase of migration requiring the HIF-1α-mediated, ROS-stabilized increased synthesis and release of VEGF.29, 30, 86, 87 Overall these data fit well with morphologic evidence from both experimental rodent models of fibrosis and specimens from hepatitis C virus cirrhotic patients.29, 30
Positive staining for both HIF-2α and heme oxygenase-1 has been reported in α-SMA positive MFs in developing septa and at the border of more mature and larger fibrotic septa.30 This scenario is similar to the previously described finding that expression of VEGF, Ang-1, and related receptors VEGF-R2 and Tie229 was found at the leading edge of tiny and incomplete developing septa, but not in larger bridging septa. This suggests that pathologic angiogenesis during the fibrogenic progression of CLDs proceeds through two different phases: 1) an early phase, occurring in developing septa, in which fibrogenesis and angiogenesis are driven or modulated by HSC/MFs and by hypoxia itself; and 2) a later phase, occurring in larger and more mature fibrotic septa, where chronic wound healing is likely to be less active and fibrogenic progression more established. Morphologic analyses indicate that in the late setting proangiogenic factors, particularly receptors like VEGF-R2 or Tie2, are expressed only by endothelial cells, a feature that should favor stabilization of the newly formed vessels.29
After exposure to hypoxia and proangiogenic mediators released by other hepatic cells, including hepatocytes, MFs may then migrate and align with the leading edge of developing fibrotic septa to drive at the same time fibrogenesis and pathologic angiogenesis, an attractive concept that fits well in the scenario of pathologic angiogenesis.88, 89, 90 Angiogenesis is controlled by the balance between proangiogenic mediators (eg, VEGF) and endogenous inhibitors of angiogenesis. Pathologic angiogenesis can result from up-regulation of angiogenic stimuli and concurrent down-regulation of endogenous inhibitors, with a shift of the balance in favor of proangiogenic stimuli.88, 89, 90 This general view has been recently integrated, particularly for angiogenesis in CLDs, by an elegant study investigating the role of vasohibin.24
Vasohibin is a natural antiangiogenic protein that is selectively induced in endothelial cells by VEGF and appears to operate as an intrinsic, highly specific feedback inhibitor of activated endothelial cells engaged in the process of angiogenesis.91, 92 Expression profiling of vasohibin-1 and its relationship with VEGF expression, angiogenesis, and fibrogenesis in animal models of cirrhosis and portal hypertension as well as in human cirrhotic liver specimens showed that vasohibin-1 and VEGF are up-regulated in mesentery and liver in cirrhotic and precirrhotic portal hypertensive rats and cirrhotic patients. This suggests that vasohibin-1/VEGF cascades are spatially and temporally coordinated through a negative-feedback loop driving pathologic angiogenesis through an overall positive effect on the activation of HSCs and fibrogenic progression.24, 92
Paradoxically, the overexpression of vasohibin-1 by adenoviral gene transfer resulted in a significant reduction in pathologic angiogenesis, portal system collateralization, splanchnic blood flow, portohepatic resistance, and portal pressure as well as an attenuation in liver fibrogenesis that was attributed, at least in part, to a vasohibin-1-mediated inhibition of HSC activation.24, 92 The investigators suggested that ectopic overexpression of vasohibin-1, unlike endogenous expression of the protein, is not regulated by VEGF and therefore can disrupt the negative-feedback loop, resulting in constant but lower levels of VEGF synthesis; this is believed to be sufficient to maintain vascular homeostasis but not pathologic angiogenesis.24, 92 Although several questions remain unanswered,92 this study is extremely promising particularly because overexpression of vasohibin-1 appeared to affect pathologic angiogenesis without acting on the normal liver vasculature.24
Hypoxia-Independent Modulation of Proangiogenic Role of Myofibroblasts
Although hypoxia represents the most obvious proangiogenic environmental condition, the proangiogenic role of MFs is regulated and modulated by a number of other mediators and events typical of conditions of chronic injury and CLD progression, including growth factors, oncogenes, cytokines, chemokines, metabolic or mitochondrial stress, and ROS. Most if not all of these mediators, although theoretically hypoxia-independent, result in either increased transcription of HIF-1α mRNA levels or (as described for any condition leading to increased intracellular levels of ROS) increased stabilization of HIF-1.
One example of a hypoxia-independent mediator is apelin, the endogenous ligand of angiotensin-like-receptor 1 (APJ; AGTRL1). Apelin is significantly increased in the serum of cirrhotic patients and cirrhotic animals.93 Apelin and APJ are expressed by MFs in cirrhotic animals and have been also detected in the splanchnic vasculature of portal hypertensive rats.48, 93, 94 Interestingly, apelin synthesis by HSC/MFs is hypoxia-independent and up-regulated by angiotensin II and ET-1; moreover, recombinant apelin can directly stimulate collagen-I and PDGF receptor β (PDGF-Rβ) expression in MF-like cells.95 As a proof of principle, experimental therapy based on the use of apelin receptor antagonists resulted in a significant reduction in liver angiogenesis and fibrosis as well as splanchnic angiogenesis and portosystemic collateral vessel formation.40, 48, 93, 94, 95
Two other examples of hypoxia-independent mediators are leptin and PDGF (particularly PDGF-BB). Leptin is an adipocytokine that exerts a profibrogenic effect during the progression from nonalcoholic fatty liver disease (NAFLD) to nonalcoholic steatohepatitis (NASH).7, 8, 9, 10, 11, 12 In human HSC/MFs, leptin up-regulates the expression of VEGF and Ang-1 as well as the proinflammatory chemokine CCL2.84 The action of leptin on HSC/MFs is mediated through its binding to its receptors (obesity receptor, ObR) and activation of several signaling pathways, including extracellular-signal-regulated kinase, Akt, and nuclear factor-κB, the latter relevant to chemokine expression. Leptin also operates as a proangiogenic mediator through the recruitment and stabilization of HIF-1α and the nuclear translocation of HIF-1.84 In vivo experiments confirmed that the obesity receptor colocalizes with VEGF and α-SMA after induction of fibrosis. The proangiogenic role of leptin in NAFLD and NASH was also confirmed by a study performed on Zucker rats (animals carrying leptin receptor mutations) receiving the steatogenic choline-deficient and amino acid-defined diet.96
The role of PDGF (known to stimulate proliferation and chemotaxis of MFs, particularly HSC/MFs) as a proangiogenic mediator was first described by Semela et al.97 PDGF was reported to promote an “angiogenic” phenotype in HSCs by modulating HSC-driven vascular tube formation in vitro and enhanced coverage of sinusoids in vivo, with resulting effects on vascular permeability and pressure regulation. Proangiogenic signaling by PDGF required the involvement of the multifunctional ephrin-B2 receptor tyrosine kinase. PDGF and leptin have more recently been described as playing a proangiogenic role in human HSC/MFs by sharing a common signaling pathway that leads to up-regulation of VEGF expression and release of the protein into the extracellular medium.98 This common signaling pathway involves activation of the mammalian target of rapamycin (mTOR) pathway and generation of intracellular ROS by nicotinamide adenine dinucleotide phosphate (NADPH)-oxidase, the latter event being relevant for increased HIF-1α stabilization but not for the mammalian target of rapamycin (mTOR) activation. Finally, another potential role for PDGF was suggested by a study performed in myeloid cell-specific HIF-1α or HIF-1β knockout mice subjected to bile duct ligation, which suggested that a significant amount of PDGF produced in this experimental model was dependent on the activation of HIFs in macrophages.99
Emerging Role of Microparticles in Mediating Angiogenesis and Vascular Remodeling
Microparticles (MPs) are small plasma membrane vesicles surrounded by a phospholipid bilayer that are released by apoptotic or stressed cells and usually contain proteins derived from the parental cells. MP shedding is a highly regulated process that occurs in several cell types. MPs have been detected in various biological fluids, including peripheral blood and urine. In recent years, it has become clear that MPs have important biological functions, including the horizontal transfer of bioactive molecules such as receptors, integrins, growth factors, RNAs, and microRNAs.100, 101 Circulating MPs are increased in animal models of biliary cirrhosis and human cirrhosis and NASH, and at least three different studies have linked the release of MPs from hepatic cells to a proangiogenic effect in the setting of CLD.102, 103, 104, 105 Although the cells releasing these proangiogenic MPs were different depending on the form of liver disease, MPs released by damaged or activated cells contributed significantly to pathologic angiogenesis regardless of their cell of origin.
One study provided evidence that cholangiocytes and HSC/MFs can produce and then release (mainly in response to PDGF) MPs containing Hedgehog (Hh) ligands. Hh ligands activate Hh signaling in endothelial cells, causing significant effects in the bile duct ligation model of fibrosis. This study found that in the normal liver the low levels of Hh ligands released by immature ductular-type progenitors are efficiently counteracted by the expression of Hh interacting protein (HIP) expressed by either quiescent HSCs or fenestrated LSECs. In conditions of chronic injury to biliary structures, however, Hh interacting protein–expression is repressed, and the activation of ductular-type progenitor cells results in PDGF-BB up-regulation and release. PDGF-BB, in turn, induces HSC/MFs and ductular cells to produce and release Hh ligands in MPs; these promote proliferation and survival of cholangiocytes and HSC/MFs as well as induce changes in LSEC gene expression. Overall, this results in capillarization of the sinusoids and the release of vasoactive factors such as NO, contributing to vascular remodeling in cirrhosis.103
A second study, focused on the role of MPs in NAFLD and NASH, showed that hepatocytes exposed to conditions mimicking the lipid accumulation and lipotoxicity that occurs in the liver during forms of steatohepatitis can also release MPs. These MPs from fat-laden hepatocytes were found to act on endothelial cells and, after their internalization, to promote pathologic angiogenesis as shown in vitro and in vivo in mice exposed to a murine model of NAFLD/NASH.105 The release of these MPs was caspase-3 dependent. Of interest, large numbers of hepatocyte-derived MPs were detected in the blood of mice with diet-induced steatohepatitis, and MPs levels correlated with disease severity. Genetic ablation of caspase-3 or RNA interference directed against vanin-1 (expressed on MPs and mediating contact with lipid rafts of endothelial cells) protected mice from steatohepatitis-induced pathologic angiogenesis and resulted in a loss of the proangiogenic effects of MPs by reducing the extent of fibrosis.
Finally, a third study suggested that portal MFs release proangiogenic MPs that contribute to the vascular changes leading to cirrhosis.15 Expression of collagen, type XV, α1 (COL15A1) by portal MFs was markedly increased in human and rat liver tissue at advanced stages of fibrosis caused by either biliary or hepatocellular injury. In the cirrhotic liver, COL15A1-expressing portal MFs were detected in an unusual perivascular distribution outlining vascular capillaries proximal to reactive ductules, within large fibrotic septa. Portal MFs were found to release MPs containing VEGF-A; this led to increased migration and tubulogenesis of LSECs and human umbilical vein endothelial cells and was able to trigger angiogenesis in matrigel plugs in mice. Cholangiocytes potentiated the angiogenic properties of portal MFs by increasing VEGF-A expression and MP shedding. This suggests that portal MFs have a significant role in angiogenesis and vascular remodeling, releasing VEGF-A containing MP, acting as mural cells for newly formed vessels, and driving angiogenesis and scar progression from portal tracts into the parenchyma.
Summary
The literature over the last decade has provided an unequivocal mechanistic link between liver angiogenesis and fibrogenesis. In the complex scenario of a progressive CLD, several major issues predominate in the relationship between angiogenesis and fibrogenesis: 1) tissue hypoxia and cellular responses mediated by HIFs significantly modulate the phenotype as well as migration and functional responses of all liver cells involved in CLD progression; 2) the interactions (both direct or mediated through the release of several mediators or signals) between hepatic cells are critical to both angiogenesis and fibrogenesis, with myofibroblasts serving a critical function integrating a variety of cell-derived signals; and 3) MPs have an important and increasingly appreciated role in mediating angiogenesis and vascular remodeling. Future studies are needed to further unravel the molecular, cell, and tissue mechanisms linking angiogenesis and fibrogenesis; ultimately, this has the potential to identify new targets for more selective and effective antifibrotic therapies.
Footnotes
Conflicts of interest The authors disclose no conflicts.
References
- 1.Medina J., Arroyo A.G., Sánchez-Madrid F., Moreno-Otero R. Angiogenesis in chronic inflammatory liver disease. Hepatology. 2004;39:1185–1195. doi: 10.1002/hep.20193. [DOI] [PubMed] [Google Scholar]
- 2.Lee J.S., Semela D., Iredale J. Sinusoidal remodeling and angiogenesis: a new function for the liver-specific pericyte? Hepatology. 2007;45:817–825. doi: 10.1002/hep.21564. [DOI] [PubMed] [Google Scholar]
- 3.Fernández M., Semela D., Bruix J. Angiogenesis in liver disease. J Hepatol. 2009;50:604–620. doi: 10.1016/j.jhep.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 4.Valfrè di Bonzo L., Novo E., Cannito S. Angiogenesis and liver fibrogenesis. Histol Histopathol. 2009;23:1324–1341. doi: 10.14670/HH-24.1323. [DOI] [PubMed] [Google Scholar]
- 5.Elpek GÖ. Angiogenesis and liver fibrosis. World J Hepatol. 2015;7:377–391. doi: 10.4254/wjh.v7.i3.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bosch J., Abraldes J.G., Fernández M. Hepatic endothelial dysfunction and abnormal angiogenesis: new targets in the treatment of portal hypertension. J Hepatol. 2010;53:558–567. doi: 10.1016/j.jhep.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 7.Zhang D.Y., Friedman S.L. Fibrosis-dependent mechanisms of hepatocarcinogenesis. Hepatology. 2012;56:769–775. doi: 10.1002/hep.25670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kocabayoglu P., Friedman S.L. Cellular basis of hepatic fibrosis and its role in inflammation and cancer. Front Biosci (Schol Ed) 2013;5:217–230. doi: 10.2741/s368. [DOI] [PubMed] [Google Scholar]
- 9.Parola M., Marra F., Pinzani M. Myofibroblast-like cells and liver fibrogenesis: emerging concepts in a rapidly moving scenario. Mol Asp Med. 2008;29:59–67. doi: 10.1016/j.mam.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 10.Rosmorduc O., Housset C. Hypoxia: a link between fibrogenesis, angiogenesis, and carcinogenesis in liver disease. Semin Liver Dis. 2010;30:258–270. doi: 10.1055/s-0030-1255355. [DOI] [PubMed] [Google Scholar]
- 11.Novo E., Cannito S., Paternostro C. Cellular and molecular mechanisms in liver fibrogenesis. Arch Biochem Biophys. 2014;548:20–37. doi: 10.1016/j.abb.2014.02.015. [DOI] [PubMed] [Google Scholar]
- 12.Cannito S., Paternostro C., Busletta C. Hypoxia, hypoxia-inducible factors and fibrogenesis in chronic liver diseases. Histol Histopathol. 2014;29:33–44. doi: 10.14670/HH-29.33. [DOI] [PubMed] [Google Scholar]
- 13.Fernandez M. Molecular pathophysiology of portal hypertension. Hepatology. 2015;61:1406–1415. doi: 10.1002/hep.27343. [DOI] [PubMed] [Google Scholar]
- 14.Povero D., Eguchi A., Niesman I.R. Lipid-induced toxicity stimulates hepatocytes to release angiogenic microparticles that require Vanin-1 for uptake by endothelial cells. Sci Signal. 2013;6:ra88. doi: 10.1126/scisignal.2004512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lemoinne S., Cadoret A., Rautou P.E. Portal myofibroblasts promote vascular remodeling underlying cirrhosis formation through the release of microparticles. Hepatology. 2015;61:1041–1055. doi: 10.1002/hep.27318. [DOI] [PubMed] [Google Scholar]
- 16.Nath B., Szabo G. Hypoxia and hypoxia inducible factors: diverse roles in liver diseases. Hepatology. 2012;55:622–633. doi: 10.1002/hep.25497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Friedman S.L. Hepatic stellate cells: protean, multifunctional, and enigmatic cells of the liver. Physiol Rev. 2008;88:125–172. doi: 10.1152/physrev.00013.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kisseleva T., Brenner D.A. The phenotypic fate and functional role for bone marrow-derived stem cells in liver fibrosis. J Hepatol. 2012;56:965–972. doi: 10.1016/j.jhep.2011.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee U.E., Friedman S.L. Mechanisms of hepatic fibrogenesis. Best Pract Res Clin Gastroenterol. 2011;25:195–206. doi: 10.1016/j.bpg.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Forbes S.J., Parola M. Liver fibrogenic cells. Best Pract Res Clin Gastroenterol. 2011;25:207–218. doi: 10.1016/j.bpg.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 21.Mederacke I., Hsu C.C., Troeger J.S. Fate tracing reveals hepatic stellate cells as dominant contributors to liver fibrosis independent of its aetiology. Nature Commun. 2013;4:2823. doi: 10.1038/ncomms3823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dranoff J.A., Wells R.G. Portal fibroblasts: Underappreciated mediators of biliary fibrosis. Hepatology. 2010;51:1438–1444. doi: 10.1002/hep.23405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Camenisch G., Pisabarro M.T., Sherman D. ANGPTL3 stimulates endothelial cell adhesion and migration via integrin avβ3 and induces blood vessel formation in vivo. J Biol Chem. 2002;277:17281–17290. doi: 10.1074/jbc.M109768200. [DOI] [PubMed] [Google Scholar]
- 24.Coch L., Mejias M., Berzigotti A. Disruption of negative feedback loop between vasohibin-1 and vascular endothelial growth factor decreases portal pressure, angiogenesis, and fibrosis in cirrhotic rats. Hepatology. 2014;60:633–647. doi: 10.1002/hep.26995. [DOI] [PubMed] [Google Scholar]
- 25.Semenza G.L. Oxygen sensing, homeostasis and disease. N Engl J Med. 2011;365:537–547. doi: 10.1056/NEJMra1011165. [DOI] [PubMed] [Google Scholar]
- 26.Semenza G.L. Hypoxia inducible factors in physiology and medicine. Cell. 2012;148:399–408. doi: 10.1016/j.cell.2012.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang Z., Zhang F., Lu Y., Zheng S. Update on implications and mechanisms of angiogenesis in liver fibrosis. Hepatol Res. 2015;45:162–178. doi: 10.1111/hepr.12415. [DOI] [PubMed] [Google Scholar]
- 28.Corpechot C., Barbu V., Wendum D. Hypoxia-induced VEGF and collagen I expressions are associated with angiogenesis and fibrogenesis in experimental cirrhosis. Hepatology. 2002;35:1010–1021. doi: 10.1053/jhep.2002.32524. [DOI] [PubMed] [Google Scholar]
- 29.Novo E., Cannito S., Zamara E. Proangiogenic cytokines as hypoxia-dependent factors stimulating migration of human hepatic stellate cells. Am J Pathol. 2007;170:1942–1953. doi: 10.2353/ajpath.2007.060887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Novo E., Povero D., Busletta C. The biphasic nature of hypoxia-induced directional migration of activated human hepatic stellate cells. J Pathol. 2012;226:588–597. doi: 10.1002/path.3005. [DOI] [PubMed] [Google Scholar]
- 31.Moon J.O., Welch T.P., Gonzalez F.J. Reduced liver fibrosis in hypoxia-inducible factor-1 alpha-deficient mice. Am J Physiol Gastrointest Liver Physiol. 2009;296:G582–G592. doi: 10.1152/ajpgi.90368.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tugues S., Fernandez-Varo G., Muñoz-Luque J. Antiangiogenic treatment with sunitinib ameliorates inflammatory infiltrate, fibrosis, and portal pressure in cirrhotic rats. Hepatology. 2007;46:1919–1926. doi: 10.1002/hep.21921. [DOI] [PubMed] [Google Scholar]
- 33.Majumder S., Piguet A.C., Dufour J.F., Chatterjee S. Study of the cellular mechanism of Sunitinib mediated inactivation of activated hepatic stellate cells and its implications in angiogenesis. Eur J Pharmacol. 2013;705:86–95. doi: 10.1016/j.ejphar.2013.02.026. [DOI] [PubMed] [Google Scholar]
- 34.Mejias M., Garcia-Pras E., Tiani C. Beneficial effects of sorafenib on splanchnic, intrahepatic, and portocollateral circulations in portal hypertensive and cirrhotic rats. Hepatology. 2009;49:1245–1256. doi: 10.1002/hep.22758. [DOI] [PubMed] [Google Scholar]
- 35.Yoshiji H., Kuriyama S., Yoshii J. Vascular endothelial growth factor and receptor interaction is a prerequisite for murine hepatic fibrogenesis. Gut. 2003;52:1347–1354. doi: 10.1136/gut.52.9.1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Van Steenkiste C., Ribera J., Geerts A. Inhibition of placental growth factor activity reduces the severity of fibrosis, inflammation, and portal hypertension in cirrhotic mice. Hepatology. 2011;53:1629–1640. doi: 10.1002/hep.24238. [DOI] [PubMed] [Google Scholar]
- 37.Taura K., De Minicis S., Seki E. Hepatic stellate cells secrete angiopoietin 1 that induces angiogenesis in liver fibrosis. Gastroenterology. 2008;135:1729–1738. doi: 10.1053/j.gastro.2008.07.065. [DOI] [PubMed] [Google Scholar]
- 38.Sahin H., Borkham-Kamphorst E., Kuppe C. Chemokine Cxcl9 attenuates liver fibrosis-associated angiogenesis in mice. Hepatology. 2012;55:1610–1619. doi: 10.1002/hep.25545. [DOI] [PubMed] [Google Scholar]
- 39.Huang H.C., Wang S.S., Hsin I.F. Cannabinoid receptor 2 agonist ameliorates mesenteric angiogenesis and portosystemic collaterals in cirrhotic rats. Hepatology. 2012;56:248–258. doi: 10.1002/hep.25625. [DOI] [PubMed] [Google Scholar]
- 40.Reichenbach V., Ros J., Fernández-Varo G. Prevention of fibrosis progression in CCl4-treated rats: role of the hepatic endocannabinoid and apelin systems. J Pharmacol Exp Ther. 2012;340:629–637. doi: 10.1124/jpet.111.188078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu Y., Wang Z., Wang J. A histone deacetylase inhibitor, largazole, decreases liver fibrosis and angiogenesis by inhibiting transforming growth factor-β and vascular endothelial growth factor signalling. Liver Int. 2013;33:504–515. doi: 10.1111/liv.12034. [DOI] [PubMed] [Google Scholar]
- 42.Zhu Q., Zou L., Jagavelu K. Intestinal decontamination inhibits TLR4 dependent fibronectin-mediated cross-talk between stellate cells and endothelial cells in liver fibrosis in mice. J Hepatol. 2012;56:893–899. doi: 10.1016/j.jhep.2011.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thabut D., Routray C., Lomberk G. Complementary vascular and matrix regulatory pathways underlie the beneficial mechanism of action of sorafenib in liver fibrosis. Hepatology. 2011;54:573–585. doi: 10.1002/hep.24427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fernandez M., Vizzutti F., Garcia-Pagan J.C. Anti-VEGF receptor-2 monoclonal antibody prevents portal-systemic collateral vessel formation in portal hypertensive mice. Gastroenterology. 2004;126:886–894. doi: 10.1053/j.gastro.2003.12.012. [DOI] [PubMed] [Google Scholar]
- 45.Fernandez M., Mejias M., Angermayr B. Inhibition of VEGF receptor-2 decreases the development of hyperdynamic splanchnic circulation and portal-systemic collateral vessels in portal hypertensive rats. J Hepatol. 2005;43:98–103. doi: 10.1016/j.jhep.2005.02.022. [DOI] [PubMed] [Google Scholar]
- 46.Fernandez M., Mejias M., Garcia-Pras E. Reversal of portal hypertension and hyperdynamic splanchnic circulation by combined vascular endothelial growth factor and platelet-derived growth factor blockade in rats. Hepatology. 2007;46:1208–1217. doi: 10.1002/hep.21785. [DOI] [PubMed] [Google Scholar]
- 47.Mejias M., Garcia-Pras E., Tiani C. The somatostatin analogue octreotide inhibits angiogenesis in the earliest, but not in advanced, stages of portal hypertension in rats. J Cell Mol Med. 2008;12:1690–1699. doi: 10.1111/j.1582-4934.2008.00218.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tiani C., Garcia-Pras E., Mejias M. Apelin signaling modulates splanchnic angiogenesis and portosystemic collateral vessel formation in rats with portal hypertension. J Hepatol. 2009;50:296–305. doi: 10.1016/j.jhep.2008.09.019. [DOI] [PubMed] [Google Scholar]
- 49.Mejias M., Coch L., Berzigotti A. Antiangiogenic and antifibrogenic activity of pigment epithelium-derived factor (PEDF) in bile duct-ligated portal hypertensive rats. Gut. 2015;64:657–666. doi: 10.1136/gutjnl-2014-307138. [DOI] [PubMed] [Google Scholar]
- 50.Patsenker E., Popov Y., Stickel F. Pharmacological inhibition of integrin αvβ3 aggravates experimental liver fibrosis and suppresses hepatic angiogenesis. Hepatology. 2009;50:1501–1511. doi: 10.1002/hep.23144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kantari-Mimoun C., Castells M., Klose R. Resolution of liver fibrosis requires myeloid cell-driven sinusoidal angiogenesis. Hepatology. 2015;61:2042–2055. doi: 10.1002/hep.27635. [DOI] [PubMed] [Google Scholar]
- 52.Coriat R., Gouya H., Mir O. Reversible decrease of portal venous flow in cirrhotic patients: a positive side effect of sorafenib. PLoS One. 2011;6:e16978. doi: 10.1371/journal.pone.0016978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shah V.H., Bruix J. Antiangiogenic therapy: not just for cancer anymore? Hepatology. 2009;49:1066–1068. doi: 10.1002/hep.22872. [DOI] [PubMed] [Google Scholar]
- 54.Duffy A., Wilkerson J., Greten T.F. Hemorrhagic events in hepatocellular carcinoma patients treated with antiangiogenic therapies. Hepatology. 2013;57:1068–1077. doi: 10.1002/hep.26120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yang L., Kwon J., Popov Y. Vascular endothelial growth factor promotes fibrosis resolution and repair in mice. Gastroenterology. 2014;146:1339–1350. doi: 10.1053/j.gastro.2014.01.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Coulon S., Heindryckx F., Geerts A. Angiogenesis in chronic liver disease and its complications. Liver Int. 2011;31:146–162. doi: 10.1111/j.1478-3231.2010.02369.x. [DOI] [PubMed] [Google Scholar]
- 57.Capece D., Fischietti M., Verzella D. The inflammatory microenvironment in hepatocellular carcinoma: a pivotal role for tumor-associated macrophages. Biomed Res Int. 2013;2013:187–204. doi: 10.1155/2013/187204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Matsubara T., Kanto T., Kuroda S. TIE2-expressing monocytes as a diagnostic marker for hepatocellular carcinoma correlates with angiogenesis. Hepatology. 2013;57:1416–1425. doi: 10.1002/hep.25965. [DOI] [PubMed] [Google Scholar]
- 59.Solinas G., Germano G., Mantovani A. Tumor-associated macrophages (TAM) as major players of the cancer-related inflammation. J Leukoc Biol. 2009;86:1065–1073. doi: 10.1189/jlb.0609385. [DOI] [PubMed] [Google Scholar]
- 60.Tacke F. Functional role of intrahepatic monocyte subsets for the progression of liver inflammation and liver fibrosis in vivo. Fibrogenesis Tissue Repair. 2012;5(Suppl 1):S27. doi: 10.1186/1755-1536-5-S1-S27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ehling J., Bartneck M., Wei X. CCL2-dependent infiltrating macrophages promote angiogenesis in progressive liver fibrosis. Gut. 2014;63:1960–1971. doi: 10.1136/gutjnl-2013-306294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Iwakiri Y., Grisham M., Shah V. Vascular biology and pathobiology of the liver: report of a single-topic symposium. Hepatology. 2008;47:1754–1763. doi: 10.1002/hep.22203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Iwakiri Y., Shah V., Rockey D.C. Vascular pathobiology in chronic liver disease and cirrhosis—current status and future directions. J Hepatol. 2014;61:912–924. doi: 10.1016/j.jhep.2014.05.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Geerts A. History, heterogeneity, developmental biology and functions of quiescent hepatic stellate cells. Semin Liver Dis. 2001;21:311–335. doi: 10.1055/s-2001-17550. [DOI] [PubMed] [Google Scholar]
- 65.Pinzani M., Failli P., Ruocco C. Fat-storing cells as liver-specific pericytes. Spatial dynamics of agonist-stimulated intracellular calcium transients. J Clin Invest. 1992;90:642–646. doi: 10.1172/JCI115905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Clemens M.G., Zhang J.X. Regulation of sinusoidal perfusion: in vivo methodology and control by endothelins. Semin Liver Dis. 1999;19:383–393. doi: 10.1055/s-2007-1007127. [DOI] [PubMed] [Google Scholar]
- 67.Kawada N., Kuroki T., Kobayashi K. Action of endothelins on hepatic stellate cells. J Gastroenterol. 1995;30:731–738. doi: 10.1007/BF02349639. [DOI] [PubMed] [Google Scholar]
- 68.Pinzani M., Milani S., De Franco R. Endothelin 1 is overexpressed in human cirrhotic liver and exerts multiple effects on activated hepatic stellate cells. Gastroenterology. 1996;110:534–548. doi: 10.1053/gast.1996.v110.pm8566602. [DOI] [PubMed] [Google Scholar]
- 69.Rockey D.C., Weisiger R.A. Endothelin induced contractility of stellate cells from normal and cirrhotic rat liver: implications for regulation of portal pressure and resistance. Hepatology. 1996;24:233–240. doi: 10.1002/hep.510240137. [DOI] [PubMed] [Google Scholar]
- 70.Mallat A., Preaux A.M., Serradeil-Le G. Growth inhibitory properties of endothelin-A in activated human stellate cells: a cyclic adenosine monophosphate-mediated pathway. J Clin Invest. 1996;98:2771–2778. doi: 10.1172/JCI119103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shah V., Haddad F.G., Garcia-Cardena G. Liver sinusoidal endothelial cells are responsible for nitric oxide modulation of resistance in the hepatic sinusoids. J Clin Invest. 1997;100:2923–2930. doi: 10.1172/JCI119842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jarnagin W.R., Rockey D.C., Koteliansky V.E. Expression of variant fibronectins in wound healing: cellular source and biological activity of the EIIIA segment in rat hepatic fibrogenesis. J Cell Biol. 1994;127:2037–2048. doi: 10.1083/jcb.127.6.2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rockey D.C., Fouassier L., Chung J.J. Cellular localization of endothelin-1 and increased production in liver injury in the rat: potential for autocrine and paracrine effects on stellate cells. Hepatology. 1998;27:472–480. doi: 10.1002/hep.510270222. [DOI] [PubMed] [Google Scholar]
- 74.Michel J.B., Feron O., Sacks D., Michel T. Reciprocal regulation of endothelial nitric-oxide synthase by Ca2+-calmodulin and caveolin. J Biol Chem. 1997;272:15583–15586. doi: 10.1074/jbc.272.25.15583. [DOI] [PubMed] [Google Scholar]
- 75.Fulton D., Gratton J.P., McCabe T.J. Regulation of endothelium-derived nitric oxide production by the protein kinase Akt. Nature. 1999;399:597–601. doi: 10.1038/21218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Langer D.A., Das A., Semela D. Nitric oxide promotes caspase-independent hepatic stellate cell apoptosis through the generation of reactive oxygen species. Hepatology. 2008;47:1983–1993. doi: 10.1002/hep.22285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Deleve L.D., Wang X., Guo Y. Sinusoidal endothelial cells prevent rat stellate cell activation and promote reversion to quiescence. Hepatology. 2008;48:920–930. doi: 10.1002/hep.22351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Rockey D.C., Chung J. Inducible nitric oxide synthase in rat hepatic lipocytes and the effect of nitric oxide on lipocyte contractility. J Clin Invest. 1995;95:1199–1206. doi: 10.1172/JCI117769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ding B.S., Nolan D.J., Butler J.M. Inductive angiocrine signals from sinusoidal endothelium are required for liver regeneration. Nature. 2010;468:310–315. doi: 10.1038/nature09493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wang L., Wang X., Xie G. Liver sinusoidal endothelial cell progenitor cells promote liver regeneration in rats. J Clin Invest. 2012;122:1567–1573. doi: 10.1172/JCI58789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ding B.S., Cao Z., Lis R. Divergent angiocrine signals from vascular niche balance liver regeneration and fibrosis. Nature. 2014;505:97–102. doi: 10.1038/nature12681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ankoma-Sey V., Wang Y., Dai Z. Hypoxic stimulation of vascular endothelial growth factor expression in activated rat hepatic stellate cells. Hepatology. 2000;31:141–148. doi: 10.1002/hep.510310122. [DOI] [PubMed] [Google Scholar]
- 83.Wang Y.Q., Luk J.M., Ikeda K. Regulatory role of vHL/HIF-1α in hypoxia-induced VEGF production in hepatic stellate cells. Biochem Biophys Res Commun. 2004;317:358–362. doi: 10.1016/j.bbrc.2004.03.050. [DOI] [PubMed] [Google Scholar]
- 84.Aleffi S., Petrai I., Bertolani C. Upregulation of proinflammatory and proangiogenic cytokines by leptin in human hepatic stellate cells. Hepatology. 2005;42:1339–1348. doi: 10.1002/hep.20965. [DOI] [PubMed] [Google Scholar]
- 85.Copple B.L., Bai S., Burgoon L.D. Hypoxia-inducible factor-1α regulates the expression of genes in hypoxic hepatic stellate cells important for collagen deposition and angiogenesis. Liver Int. 2011;31:230–244. doi: 10.1111/j.1478-3231.2010.02347.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Novo E., Busletta C., Bonzo L.V. Intracellular reactive oxygen species are required for directional migration of resident and bone marrow-derived hepatic pro-fibrogenic cells. J Hepatol. 2011;54:964–974. doi: 10.1016/j.jhep.2010.09.022. [DOI] [PubMed] [Google Scholar]
- 87.Busletta C., Novo E., Valfrè Di Bonzo L. Dissection of the biphasic nature of hypoxia-induced motogenic action in bone marrow-derived human mesenchymal stem cells. Stem Cells. 2011;29:952–963. doi: 10.1002/stem.642. [DOI] [PubMed] [Google Scholar]
- 88.Ferrara N., Gerber H.P., LeCouter J. The biology of VEGF and its receptors. Nat Med. 2003;9:669–676. doi: 10.1038/nm0603-669. [DOI] [PubMed] [Google Scholar]
- 89.Carmeliet P., Jain R.K. Molecular mechanisms and clinical applications of angiogenesis. Nature. 2011;473:298–307. doi: 10.1038/nature10144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Nyberg P., Xie L., Kalluri R. Endogenous inhibitors of angiogenesis. Cancer Res. 2005;65:3967–3979. doi: 10.1158/0008-5472.CAN-04-2427. [DOI] [PubMed] [Google Scholar]
- 91.Watanabe K., Hasegawa Y., Yamashita H. Vasohibin as an endothelium-derived negative feedback regulator of angiogenesis. J Clin Invest. 2004;114:898–907. doi: 10.1172/JCI21152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chatterjee S. Reversal of vasohibin-driven negative feedback loop of vascular endothelial growth factor/angiogenesis axis promises a novel antifibrotic therapeutic strategy for liver diseases. Hepatology. 2014;60:458–460. doi: 10.1002/hep.27061. [DOI] [PubMed] [Google Scholar]
- 93.Principe A., Melgar-Lesmes P., Fernández-Varo G. The hepatic apelin system: a new therapeutic target for liver disease. Hepatology. 2008;48:1193–2001. doi: 10.1002/hep.22467. [DOI] [PubMed] [Google Scholar]
- 94.Yokomori H., Oda M., Yoshimura K. Overexpression of apelin receptor (APJ/AGTRL1) on hepatic stellate cells and sinusoidal angiogenesis in human cirrhotic liver. J Gastroenterol. 2011;46:222–231. doi: 10.1007/s00535-010-0296-3. [DOI] [PubMed] [Google Scholar]
- 95.Melgar-Lesmes P., Casals G., Pauta M. Apelin mediates the induction of profibrogenic genes in human hepatic stellate cells. Endocrinology. 2010;151:5306–5314. doi: 10.1210/en.2010-0754. [DOI] [PubMed] [Google Scholar]
- 96.Kitade M., Yoshiji H., Kojima H. Leptin-mediated neovascularization is a prerequisite for progression of non-alcoholic steatohepatitis in rats. Hepatology. 2006;44:983–991. doi: 10.1002/hep.21338. [DOI] [PubMed] [Google Scholar]
- 97.Semela D., Das A., Langer D. Platelet-derived growth factor signaling through ephrin-b2 regulates hepatic vascular structure and function. Gastroenterology. 2008;135:671–679. doi: 10.1053/j.gastro.2008.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Aleffi S., Navari N., Delogu W. Mammalian target of rapamycin mediates the angiogenic effects of leptin in human hepatic stellate cells. Am J Physiol Gastrointest Liver Physiol. 2011;301:G210–G219. doi: 10.1152/ajpgi.00047.2010. [DOI] [PubMed] [Google Scholar]
- 99.Copple B.L., Kaska S., Wentling C. Hypoxia-inducible factor activation in myeloid cells contributes to the development of liver fibrosis in cholestatic mice. J Pharmacol Exp Ther. 2012;341:307–316. doi: 10.1124/jpet.111.189340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Morel O., Morel N., Jesel L. Microparticles: A critical component in the nexus between inflammation, immunity, and thrombosis. Semin Immunopathol. 2011;33:469–486. doi: 10.1007/s00281-010-0239-3. [DOI] [PubMed] [Google Scholar]
- 101.Rautou P.E., Vion A.C., Amabile N. Microparticles, vascular function, and atherothrombosis. Circ Res. 2011;109:593–606. doi: 10.1161/CIRCRESAHA.110.233163. [DOI] [PubMed] [Google Scholar]
- 102.Rautou P.E., Bresson J., Sainte-Marie Y. Abnormal plasma microparticles impair vasoconstrictor responses in patients with cirrhosis. Gastroenterology. 2012;143:166–176. doi: 10.1053/j.gastro.2012.03.040. [DOI] [PubMed] [Google Scholar]
- 103.Witek R.P., Yang L., Liu R. Liver cell–derived microparticles activate hedgehog signaling and alter gene expression in hepatic endothelial cells. Gastroenterology. 2009;136:320–330. doi: 10.1053/j.gastro.2008.09.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kornek M., Lynch M., Mehta S.H. Circulating microparticles as disease-specific biomarkers of severity of inflammation in patients with hepatitis C or nonalcoholic steatohepatitis. Gastroenterology. 2012;143:448–458. doi: 10.1053/j.gastro.2012.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lemoinne S., Thabut D., Housset C. The emerging roles of microvesicles in liver diseases. Nat Rev Gastroenterol Hepatol. 2014;11:350–361. doi: 10.1038/nrgastro.2014.7. [DOI] [PubMed] [Google Scholar]