Introduction
Ventilator-associated pneumonia (VAP) is a significant cause of morbidity and mortality in critically ill and injured patients.1 VAP is one of the most common intensive care unit (ICU)-acquired nosocomial infection, affecting 4.8 – 7.5% of patients intubated > 24 hours with an estimated overall attributable mortality of 9%. VAP is associated with longer hospital stays with a resultant attributable cost of approximately $40,000 per case.1–3 Several studies have demonstrated the effectiveness of oral chlorhexidine in preventing pneumonia among intubated patients, and in 2010 the Institute for Healthcare Improvement recommended routine chlorhexidine prophylaxis to prevent VAP.4–10 Patients who are critically ill and intubated emergently have the highest risk of developing pneumonia,5,10–13 and in a recent trial, a single dose of chlorhexidine early in the care of trauma patients significantly reduced subsequent VAP.14 Interestingly, pre-intubation chlorhexidine has not demonstrated a reduction in VAP.15
Oral care varies across intensive care units (ICUs).12,16 Although some authors have advocated for routine application of chlorhexidine prior to ICU admission to reduce VAP,4 little is known about the importance of prophylaxis timing on clinical outcomes. This study was conducted to test the association between timing of chlorhexidine prophylaxis and VAP incidence.
Methods
Design, Setting and Sample
This retrospective cohort study was conducted in a 711-bed university hospital and involved all intubated adult patients (age ≥18 years) transferred to a 36-bed Surgical ICU by an air ambulance service between July 2011 and April 2013. Patients were excluded if they (1) died within 72 hours of hospital arrival, (2) presented with a diagnosis of pneumonia or infiltrates on chest imaging, or (3) were admitted to a transferring hospital prior to definitive transfer. This study is reported in accordance with the STROBE Statement,17 and was approved by the local Institutional Review Board under waiver of informed consent.
Procedures
The primary exposure was time to chlorhexidine (if given), and the primary outcome was early pneumonia (diagnosed within 5 days of admission).18,19 Application of oral chlorhexidine is the standard procedure in this ICU, however no protocol exists for prehospital, ED nor pre-intubation administration of chlorhexidine. Time to chlorhexidine was defined as the time from helicopter departure from the scene or transferring hospital to chlorhexidine administration in the ICU. The definition of early prophylaxis was derived from the median time to chlorhexidine administration, but quartiles were used for sensitivity analysis.
Pneumonia was defined as a clinical suspicion for pneumonia by a board-certified intensivist with initiation of antibiotic treatment and with subsequent respiratory culture indicating a pathogenic organism. Statistical tests are reported using standard descriptive and comparative analyses, and significance was defined as p < 0.05 for two-tailed tests.
Results
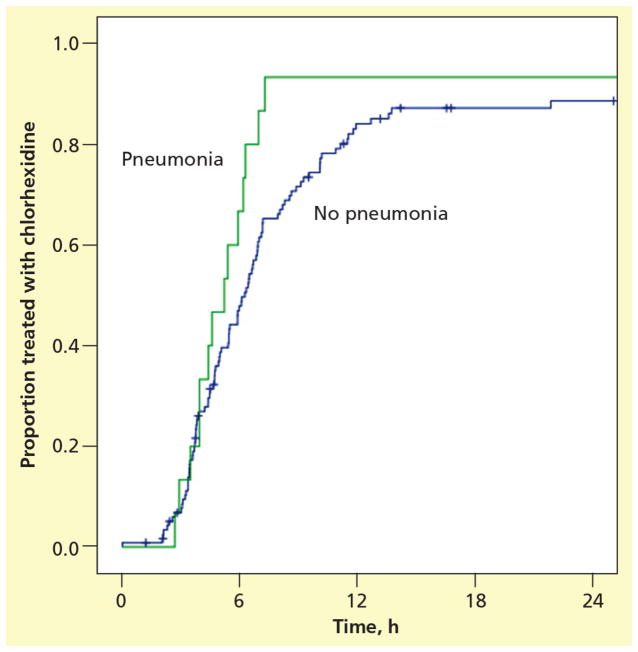
There were 134 intubated patients included and 128 (95.5%) were treated with chlorhexidine, with 84% (n=113) treated prior to 12 hours (Table 1). Most were male (61.2%) who presented through inter-hospital transfer (89.6%), with 94.8% of these transfers through the receiving hospital emergency department (ED). The most common diagnostic category was trauma (26.1%). Median APACHE-II score was 22 and was not associated with VAP diagnosis (p = 0.117). Pneumonia was treated before 5 days in 11.2% of patients. The median time to chlorhexidine was not associated with early VAP diagnosis (6.1 hours vs. 5.2 hours, p = 0.232, Figure 1). Multivariate logistic regression failed to demonstrate APACHE II scores as a confounder on the relationship between time to chlorhexidine and VAP. Chlorhexidine prior to 6 hours was not associated with a decreased risk of VAP (15.2% vs. 8.1%, p = 0.213), and no significant difference was observed in sensitivity analysis for 3 hours or 9 hours (p = 0.617 and p = 0.188, respectively). There was no difference in baseline characteristics nor outcome when the six patients (4.5%) not treated with chlorhexidine were compared to patients receiving chlorhexidine; none of the patients who were not treated with chlorhexidine developed pneumonia.
Table 1.
Demographics and baseline characteristics, stratified by VAP
| VAP (n = 15) | No VAP (n = 119) | p | |
|---|---|---|---|
| Baseline characteristics | |||
| Male | 11 (73.3%) | 71 (59.6%) | 0.404 |
| Age (mean ± SD) | 47.9 ± 21.4 | 51.8 ± 19.6 | 0.474 |
| APACHE II score (mean ± SD) | 25.6 ± 8.9 | 22.3 ± 10.2 | 0.242 |
| BMI (mean ± SD) | 27.5 ± 6.4 | 28.1 ± 5.6 | 0.729 |
| Scene flight | 0 (0%) | 13 (10.9%) | 0.373 |
| Inter-facility transfer | 15 (100%) | 105 (88.2%) | |
| Diagnoses (not mutually exclusive) | |||
| Trauma, n (%) | 6 (40%) | 45 (37.8%) | 0.999 |
| Cerebral Hemorrhage | 5 (33%) | 49 (41.2%) | 0.781 |
| Brain Injury | 4 (26.6%) | 33 (27.7%) | 0.999 |
| Respiratory failure | 3 (20%) | 18 (15.2%) | 0.705 |
| Pulmonary contusion, n (%) | 3 (20%) | 7 (5.9%) | 0.085 |
| Spinal cord injury, n (%) | 2 (13.3%) | 12 (15.9%) | 0.657 |
| Rib fracture, n (%) | 2 (13.3%) | 13 (10.9%) | 0.676 |
| Sepsis, n (%) | 1 (6.6%) | 3 (2.5%) | 0.382 |
| Timing of chlorhexidine amongst recipients | |||
| Median time to chlorhexidine (IQR)* | 5.2 (3.0, 6.3) hours | 6.1 (3.8, 9) hours | 0.232 |
| < 3 hours | 2 (13.3%) | 8 (6.7%) | 0.310 |
| <6 hours | 10 (66.7%) | 56 (47.1%) | 0.179 |
| <12 hours | 14 (93.3%) | 98 (82.4%) | 0.464 |
| <24 hours | 14 (93.3%) | 104 (87.4%) | 0.999 |
| ≥24 hours | 1 (6.7%) | 9 (7.6%) | |
| No chlorhexidine** | 0 (0%) | 6 (5.0%) | 0.999 |
| Outcomes | |||
| Hospital Days (LOS) (mean ± SD) | 19.5 ± 10.4 days | 11.1 ± 9.3 days | 0.002 |
| Death, n (%) | 3 (20%) | 13 (10.9%) | 0.389 |
P values derived from t-tests or Mann-Whitney U-tests for continuous variables and Chi square tests for categorical variables.
IQR: intra quartile range, 25th, 75th percentile
No difference in baseline characteristics, diagnoses, nor outcome in recipients vs non-recipients of chlorhexidine
Figure 1.
Proportion of patients treated with chlorhexidine by time, stratified by early pneumonia status.
Discussion
Hospital-acquired infection has gained importance as a marker of health care quality, yet many recognize that patient-oriented factors predispose some patients to infection. The effects of prehospital intubation on subsequent pneumonia are controversial,33–35 but most agree that severity of illness is associated with developing pneumonia.19,36,37
Administration of oral chlorhexidine to intubated patients has been shown to prevent VAP4,6,8,9,12,14, but few studies have defined a clear goal for treatment initiation time. Munro et al have recently shown that treatment with chlorhexidine immediately prior to endotracheal intubation does not reduce CPIS scores.15 Ours is now the second study demonstrating that early prophylaxis does not decrease the incidence of VAP, in our study using a different, clinical definition of VAP.
The CPIS score has been criticized for its test characteristics,20–26 perhaps due to the lack of a true gold-standard diagnosis of VAP. The Centers for Disease Control and Prevention definition of VAP has also been criticized as too insensitive for clinical practice.27–29 Stringency of diagnosis for VAP is highly variable among published diagnostic criteria for VAP; in one group, the diagnosis of VAP varied between 4–42%, depending on which of six diagnostic criteria (including CDC and CPIS) was utilized, with resultant 4–8 days of delay in diagnosis of VAP.30 Not surprisingly, the more stringent the diagnostic algorithm, the higher the mortality, which ranged from 50–80%. A clinical outcome as used in our analysis may capture a more meaningful patient-oriented event and the importance of early antibiotic initiation has been shown to reduce mortality.31,32
In addition to early chlorhexidine prophylaxis, our institution has standardized oral care including elevation of the head of bed ≥30 degrees, tooth brushing and subglottic suctioning twice daily, and chlorhexidine and oral suction every 4 hours. Similar oral care has demonstrated a 46% decrease in VAP at other institutions.38 It is challenging to separate the effect of chlorhexidine from standard oral care, so for institutions striving for early VAP prophylaxis, nursing education should stress chlorhexidine as a component of overall oral care.
Our study has several limitations. First, as a retrospective study only data recorded in the medical record is available. We selected variables that are likely recorded accurately and utilized standardized data abstraction. Second, it is challenging to divorce oral chlorhexidine from other prophylactic oral care delivered in the ICU. Third, our center has relatively short times to ICU admission, and most (84%) patients were treated with chlorhexidine within 12 hours of presentation. As such, the absence of effect in our cohort may not be replicated in centers where chlorhexidine treatment is less routine or rapid.
Finally, our clinical definition of VAP, which combined the treating clinician’s suspicion for pneumonia and bacteriologic evidence for diagnosis, differs from prior studies which utilized CPIS, making direct comparison difficult. Use of a retrospective dataset prevented our use of CPIS scores, however the test characteristics of the CPIS to predict VAP are not ideal. Use of our clinical diagnosis of VAP, however, has shown similar lack of protective effects of early chlorhexidine against VAP to very recent studies using CPIS as an outcome.15
Conclusions
Oral chlorhexidine prophylaxis administered within the initial 12 hours of treatment is not associated with a decreased incidence of early VAP in mechanically ventilated surgical ICU patients. The role of VAP prevention, with respect to timing of interventions and the interventions themselves, should be explored further.
Acknowledgments
Grant/Financial Support: This project was funded by the University of Iowa Carver College of Medicine and the Department of Emergency Medicine. Dr. Mohr is supported by a grant from the Emergency Medicine Foundation. Dr. Fuller is supported by the KL2 Career Development Award from the Washington University Institute of Clinical and Translational Sciences grants UL1 TR000448 and KL2 TR000450 from the National Center for Advancing Translational Sciences.
Contributor Information
Terrence Wong, Medical Student, Department of Emergency Medicine, University of Iowa Carver College of Medicine, Iowa City, IA.
Adam B. Schlichting, Clinical Assistant Professor, Department of Emergency Medicine, Department of Internal Medicine, Division of Pulmonary, Critical Care and Occupational Medicine, University of Iowa Carver College of Medicine, Iowa City, IA.
Andrew J. Stoltze, Resident Physician, Department of Emergency Medicine, University of Iowa Carver College of Medicine, Iowa City, IA.
Brian M. Fuller, Division of Emergency Medicine, Division of Critical Care, Department of Anesthesiology, Washington University School of Medicine, St. Louis, MO.
Amanda Peacock, Advanced Registered Nurse Practitioner, Department of Anesthesia, Division of Critical Care, University of Iowa Carver College of Medicine, Iowa City, IA.
Kari K. Harland, Biostatistician, Department of Emergency Medicine, University of Iowa Carver College of Medicine, Iowa City, IA.
Azeemuddin Ahmed, Clinical Professor, Department of Emergency Medicine, University of Iowa Carver College of Medicine, Iowa City, IA.
Nicholas Mohr, Clinical Assistant Professor, Department of Emergency Medicine, Department of Anesthesia, Division of Critical Care, University of Iowa Carver College of Medicine, Iowa City, IA.
References
- 1.Eom JS, Lee MS, Chun HK, et al. The impact of a ventilator bundle on preventing ventilator-associated pneumonia: a multicenter study. American journal of infection control. 2014;42(1):34–37. doi: 10.1016/j.ajic.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 2.To KB, Napolitano LM. Common complications in the critically ill patient. The Surgical clinics of North America. 2012;92(6):1519–1557. doi: 10.1016/j.suc.2012.08.018. [DOI] [PubMed] [Google Scholar]
- 3.Cutler LR, Sluman P. Reducing ventilator associated pneumonia in adult patients through high standards of oral care: a historical control study. Intensive & critical care nursing : the official journal of the British Association of Critical Care Nurses. 2014;30(2):61–68. doi: 10.1016/j.iccn.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 4.Chan EY. Oral decontamination with chlorhexidine reduced ventilator associated pneumonia in patients needing mechanical ventilation for >/=48 hours. Evidence-based nursing. 2007;10(1):19. doi: 10.1136/ebn.10.1.19. [DOI] [PubMed] [Google Scholar]
- 5.Kollef MH. Ventilator-associated pneumonia. A multivariate analysis. JAMA : the journal of the American Medical Association. 1993;270(16):1965–1970. [PubMed] [Google Scholar]
- 6.Labeau SO, Van de Vyver K, Brusselaers N, Vogelaers D, Blot SI. Prevention of ventilator-associated pneumonia with oral antiseptics: a systematic review and meta-analysis. The Lancet infectious diseases. 2011;11(11):845–854. doi: 10.1016/S1473-3099(11)70127-X. [DOI] [PubMed] [Google Scholar]
- 7.Ibrahim EH, Tracy L, Hill C, Fraser VJ, Kollef MH. The occurrence of ventilator-associated pneumonia in a community hospital: risk factors and clinical outcomes. Chest. 2001;120(2):555–561. doi: 10.1378/chest.120.2.555. [DOI] [PubMed] [Google Scholar]
- 8.DeRiso AJ, 2nd, Ladowski JS, Dillon TA, Justice JW, Peterson AC. Chlorhexidine gluconate 0.12% oral rinse reduces the incidence of total nosocomial respiratory infection and nonprophylactic systemic antibiotic use in patients undergoing heart surgery. Chest. 1996;109(6):1556–1561. doi: 10.1378/chest.109.6.1556. [DOI] [PubMed] [Google Scholar]
- 9.Chlebicki MP, Safdar N. Topical chlorhexidine for prevention of ventilator-associated pneumonia: a meta-analysis. Critical care medicine. 2007;35(2):595–602. doi: 10.1097/01.CCM.0000253395.70708.AC. [DOI] [PubMed] [Google Scholar]
- 10.Berenholtz SM, Pham JC, Thompson DA, et al. Collaborative cohort study of an intervention to reduce ventilator-associated pneumonia in the intensive care unit. Infection control and hospital epidemiology : the official journal of the Society of Hospital Epidemiologists of America. 2011;32(4):305–314. doi: 10.1086/658938. [DOI] [PubMed] [Google Scholar]
- 11.Fuller BM, Mohr NM, Drewry AM, Carpenter CR. Lower tidal volume at initiation of mechanical ventilation may reduce progression to acute respiratory distress syndrome: a systematic review. Critical care. 2013;17(1):R11. doi: 10.1186/cc11936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Par M, Badovinac A, Plancak D. Oral hygiene is an important factor for prevention of ventilator-associated pneumonia. Acta clinica Croatica. 2014;53(1):72–78. [PubMed] [Google Scholar]
- 13.Cook A, Norwood S, Berne J. Ventilator-associated pneumonia is more common and of less consequence in trauma patients compared with other critically ill patients. The Journal of trauma. 2010;69(5):1083–1091. doi: 10.1097/TA.0b013e3181f9fb51. [DOI] [PubMed] [Google Scholar]
- 14.Grap MJ, Munro CL, Hamilton VA, Elswick RK, Jr, Sessler CN, Ward KR. Early, single chlorhexidine application reduces ventilator-associated pneumonia in trauma patients. Heart & lung : the journal of critical care. 2011;40(5):e115–122. doi: 10.1016/j.hrtlng.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 15.Munro CL, Grap MJ, Sessler CN, et al. Pre-Intubation application of oral chlorhexidine does not provide additional benefit in prevention of early onset ventilator-associated pneumonia. Chest. 2014 doi: 10.1378/chest.14-0692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Caserta RA, Marra AR, Durao MS, et al. A program for sustained improvement in preventing ventilator associated pneumonia in an intensive care setting. BMC infectious diseases. 2012;12:234. doi: 10.1186/1471-2334-12-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 18.Shi Z, Xie H, Wang P, et al. Oral hygiene care for critically ill patients to prevent ventilator-associated pneumonia. The Cochrane database of systematic reviews. 2013;8:CD008367. doi: 10.1002/14651858.CD008367.pub2. [DOI] [PubMed] [Google Scholar]
- 19.Mohr NM, Harland KK, Skeete D, Pearson K, Choi K. Duration of prehospital intubation is not a risk factor for development of early ventilator-associated pneumonia. Journal of critical care. 2014;29(4):539–544. doi: 10.1016/j.jcrc.2014.03.030. [DOI] [PubMed] [Google Scholar]
- 20.Croce MA, Swanson JM, Magnotti LJ, et al. The futility of the clinical pulmonary infection score in trauma patients. The Journal of trauma. 2006;60(3):523–527. doi: 10.1097/01.ta.0000204033.78125.1b. discussion 527–528. [DOI] [PubMed] [Google Scholar]
- 21.Fabregas N, Ewig S, Torres A, et al. Clinical diagnosis of ventilator associated pneumonia revisited: comparative validation using immediate post-mortem lung biopsies. Thorax. 1999;54(10):867–873. doi: 10.1136/thx.54.10.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Papazian L, Thomas P, Garbe L, et al. Bronchoscopic or blind sampling techniques for the diagnosis of ventilator-associated pneumonia. American journal of respiratory and critical care medicine. 1995;152(6 Pt 1):1982–1991. doi: 10.1164/ajrccm.152.6.8520766. [DOI] [PubMed] [Google Scholar]
- 23.Pham TN, Neff MJ, Simmons JM, Gibran NS, Heimbach DM, Klein MB. The clinical pulmonary infection score poorly predicts pneumonia in patients with burns. Journal of burn care & research : official publication of the American Burn Association. 2007;28(1):76–79. doi: 10.1097/BCR.0b013E31802C88DB. [DOI] [PubMed] [Google Scholar]
- 24.Fartoukh M, Maitre B, Honore S, Cerf C, Zahar JR, Brun-Buisson C. Diagnosing pneumonia during mechanical ventilation: the clinical pulmonary infection score revisited. American journal of respiratory and critical care medicine. 2003;168(2):173–179. doi: 10.1164/rccm.200212-1449OC. [DOI] [PubMed] [Google Scholar]
- 25.Luyt CE, Chastre J, Fagon JY. Value of the clinical pulmonary infection score for the identification and management of ventilator-associated pneumonia. Intensive care medicine. 2004;30(5):844–852. doi: 10.1007/s00134-003-2125-0. [DOI] [PubMed] [Google Scholar]
- 26.Schurink CA, Van Nieuwenhoven CA, Jacobs JA, et al. Clinical pulmonary infection score for ventilator-associated pneumonia: accuracy and inter-observer variability. Intensive care medicine. 2004;30(2):217–224. doi: 10.1007/s00134-003-2018-2. [DOI] [PubMed] [Google Scholar]
- 27.Klompas M. Is a ventilator-associated pneumonia rate of zero really possible? Current opinion in infectious diseases. 2012;25(2):176–182. doi: 10.1097/QCO.0b013e3283502437. [DOI] [PubMed] [Google Scholar]
- 28.Nair GB, Niederman MS. Ventilator-associated pneumonia: present understanding and ongoing debates. Intensive care medicine. 2015;41(1):34–48. doi: 10.1007/s00134-014-3564-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Skrupky LP, McConnell K, Dallas J, Kollef MH. A comparison of ventilator-associated pneumonia rates as identified according to the National Healthcare Safety Network and American College of Chest Physicians criteria. Critical care medicine. 2012;40(1):281–284. doi: 10.1097/CCM.0b013e31822d7913. [DOI] [PubMed] [Google Scholar]
- 30.Ego A, Preiser JC, Vincent JL. Impact of diagnostic criteria on the incidence of ventilator-associated pneumonia. Chest. 2014 doi: 10.1378/chest.14-0610. [DOI] [PubMed] [Google Scholar]
- 31.Muscedere JG, McColl C, Shorr A, et al. Determinants of outcome in patients with a clinical suspicion of ventilator-associated pneumonia. Journal of critical care. 2008;23(1):41–49. doi: 10.1016/j.jcrc.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 32.Muscedere JG, Shorr AF, Jiang X, Day A, Heyland DK Canadian Critical Care Trials, G. The adequacy of timely empiric antibiotic therapy for ventilator-associated pneumonia: an important determinant of outcome. Journal of critical care. 2012;27(3):322 e327–314. doi: 10.1016/j.jcrc.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 33.Carr BG, Kaye AJ, Wiebe DJ, Gracias VH, Schwab CW, Reilly PM. Emergency department length of stay: a major risk factor for pneumonia in intubated blunt trauma patients. The Journal of trauma. 2007;63(1):9–12. doi: 10.1097/TA.0b013e31805d8f6b. [DOI] [PubMed] [Google Scholar]
- 34.Eckert MJ, Davis KA, Reed RL, 2nd, et al. Ventilator-associated pneumonia, like real estate: location really matters. The Journal of trauma. 2006;60(1):104–110. doi: 10.1097/01.ta.0000197376.98296.7c. discussion 110. [DOI] [PubMed] [Google Scholar]
- 35.Decelle L, Thys F, Zech F, Verschuren F. Ventilation-associated pneumonia after intubation in the prehospital or the emergency unit. European journal of emergency medicine : official journal of the European Society for Emergency Medicine. 2013;20(1):61–63. doi: 10.1097/MEJ.0b013e3283501677. [DOI] [PubMed] [Google Scholar]
- 36.Tseng CC, Liu SF, Wang CC, et al. Impact of clinical severity index, infective pathogens, and initial empiric antibiotic use on hospital mortality in patients with ventilator-associated pneumonia. American journal of infection control. 2012;40(7):648–652. doi: 10.1016/j.ajic.2011.08.017. [DOI] [PubMed] [Google Scholar]
- 37.Kasuya Y, Hargett JL, Lenhardt R, et al. Ventilator-associated pneumonia in critically ill stroke patients: frequency, risk factors, and outcomes. Journal of critical care. 2011;26(3):273–279. doi: 10.1016/j.jcrc.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 38.Babcock HM, Zack JE, Garrison T, et al. An educational intervention to reduce ventilator-associated pneumonia in an integrated health system: a comparison of effects. Chest. 2004;125(6):2224–2231. doi: 10.1378/chest.125.6.2224. [DOI] [PubMed] [Google Scholar]