Abstract
Objectives
The aim of this study was to systematically review the literature on measurement of muscle strength in patients with femoroacetabular impingement (FAI) and other pathologies and to suggest guidelines to standardise protocols for future research in the field.
Methods
The Cochrane and PubMed libraries were searched for any publications using the terms ‘hip’, ‘muscle’, ‘strength’, and ‘measurement’ in the ‘Title, Abstract, Keywords’ field. A further search was performed using the terms ‘femoroacetabular’ or ‘impingement’. The search was limited to recent literature only.
Results
A total of 29 articles were reviewed to obtain information on a number of variables. These comprised the type of device used for measurement, rater standardisation, the type of movements tested, body positioning and comparative studies of muscle strength in FAI versus normal controls. The studies found that hip muscle strength is lower in patients with FAI; this is also true for the asymptomatic hip in patients with FAI.
Conclusions
Current literature on this subject is limited and examines multiple variables. Our recommendations for achieving reproducible results include stabilising the patient, measuring isometric movements and maximising standardisation by using a single tester and familiarising the participants with the protocol. Further work must be done to demonstrate the reliability of any new testing method.
Cite this article: E. Mayne, A. Memarzadeh, P. Raut, A. Arora, V. Khanduja. Measuring hip muscle strength in patients with femoroacetabular impingement and other hip pathologies: A systematic review. Bone Joint Res 2017;6:66–72. DOI: 10.1302/2046-3758.61.BJR-2016-0081.
Keywords: FAI, Muscle strength, Measurement
Article focus
A review of the literature on methods of muscle strength measurement
A closer focus on measuring muscle strength in patients with femoroacetabular impingement
To identify key variables in measuring muscle strength, with the aim of standardising future research into the subject
Key messages
Hip girdle muscles are weaker in patients with femoroacetabular impingement; this is the case in both hips, regardless of whether the hip is symptomatic or otherwise.
Motor driven and hand held dynamometry are both reliable methods of muscle strength measurement, and should be used with make tests.
Attempts should be made to standardise future research in muscle strength testing to ensure the ability to compare results across different studies. This includes employing the same tester for all measurements, stabilising the patient and identifying whether isometric or isokinetic results have been obtained.
Strengths and limitations
Strengths:
A comprehensive review of all literature relating to muscle strength measurement
An attempt to unify future research into measuring muscle strength
Limitation:
The review is limited by the quantity and quality of the articles previously published. There were only two studies on the effect of FAI on hip muscle strength
Introduction
Femoroacetabular impingement (FAI) is a morphological osseous abnormality, which results in a physical conflict between the femoral head-neck junction and the acetabular rim.1 The abnormality may be of the proximal femur (cam) or the acetabulum (pincer) or, most commonly, a mixture of both. This can result in, amongst other things, a chondrolabral lesion, which manifests as hip pain, and if not addressed can lead to osteoarthritis of the hip.2,3 Hip arthroscopy has become a common procedure to treat the different aetiologies causing FAI.4,5
The diagnosis of FAI is becoming more common and although the exact incidence is unclear, a study on asymptomatic individuals6 found an incidence of cam deformities of 24.7% in men and 5.4% in women. This is clearly a large proportion of the population who are at risk of developing the sequelae of the disease such as labral tears. More importantly, if FAI remains untreated, patients can suffer lifelong consequences in the form of osteoarthritis,2,3 functional disabilities and risk of injury secondary to hip muscle weakness.7 Changes associated with an arthritic gait have been seen in patients affected with FAI.8
At presentation, patients with FAI are typically young adults who are healthy, active and classically partake in athletic activity.2 They most commonly present with anterior groin pain but also experience limitations when performing activities of daily living and sport.2,9
It has been shown that patients with FAI also present with hip muscle weakness,7 although currently data on this are limited. It is generally well known that patients with FAI have a reduced range of movement,10 however, to date only two studies have compared hip muscle strength in patients with FAI versus normal controls.7,11 Both of these studies found reduced strength in patients with FAI compared with controls. It follows that, in accordance with current guidelines,12,13 measuring hip muscle strength in patients with FAI could be of certain benefit.
A greater understanding of hip muscle strength could achieve a number of goals. Firstly, understanding the muscle strength changes associated with FAI will give a better understanding of the condition’s pathophysiology and will help to guide the development of future treatments. This is vital for a condition where 34% of patients have reported weakness that greatly limits activity.8 Secondly, at an individual level, measuring hip muscle strength could help guide and monitor patients’ individual treatment and its efficacy. Finally, if a specific pattern of muscle weakness associated with FAI is identified, measuring patient hip muscle strength could help with diagnosis. Philippon et al9 highlighted that the equivocal presentation of FAI leads to a risk of incorrect diagnosis which in turn can result in inappropriate tests and interventions.
There are currently multiple methods of measuring muscle strength described in the literature, with many variables. These variables include:
The strength measuring device:
Manual muscle testing (MMT) – a subjective ‘grade’ of strength is given by an assessor for a given direction of joint movement, using a 5 point grading scale;14
Hand-held dynamometry (HHD) – a calibrated pressure sensor is used by an assessor to measure the strength of a particular joint movement;
Motor-driven dynamometry (MDD) – a calibrated pressure sensor is used to measure strength of movement; the sensor is held in position by a mechanical device (Fig. 1).
The individual rater measuring strength;
- The types of movements performed;
- Isokinetic – muscle contraction causing joint movement at constant speed;
- Isometric – muscle contraction against resistance resulting in no movement;
Body positioning and stability.
Fig. 1.

Cybex dynamometer (a MDD) showing a participant during testing of hip flexors
The different variables in the methodology of measurement of muscle strength have different advantages and disadvantages, making them more or less suitable in specific situations and difficult to be used uniformly. The aim of this study, therefore, was to review the current literature available on this subject and to suggest guidelines on measuring muscle strength in patients with FAI, which would allow standardisation of the results available on this subject.
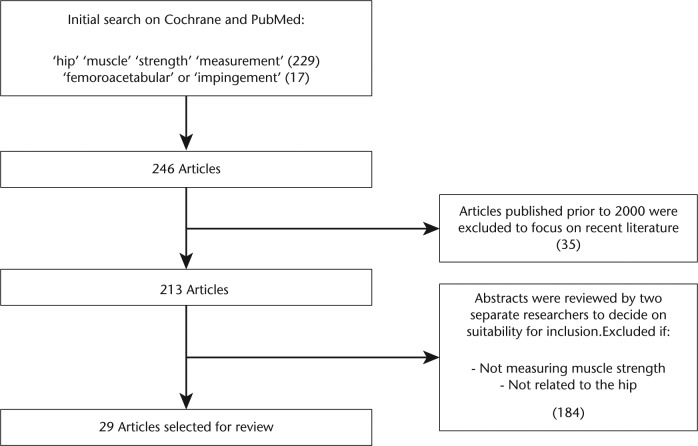
Materials and Methods
The Cochrane and PubMed databases were searched using the terms ‘hip’, ‘muscle’, ‘strength’ and ‘measurement’ in the ‘All Terms’ field and this produced 229 results. A further search using the terms ‘femoroacetabular’ or ‘impingement’ yielded 17 additional studies. It was decided to focus the review on recent literature and therefore the search was narrowed to papers published from 2000 onwards. This yielded 213 results. The abstracts were then reviewed by two medical researchers (EM and AM) independently to determine suitability for inclusion in the review. Articles were excluded if the abstract did not include any measurement of muscle strength. A total of 29 articles were deemed relevant to the study. The PRISMA chart is summarised in Figure 2.
Fig. 2.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow chart
All papers were individually assessed for strengths and weaknesses, both in terms of reliability and applicability to measuring muscle strength. Of particular interest were the methodology of hip muscle strength measurement used and the reliability of the results produced, measured by most papers as the intraclass correlation coefficients (ICC). This is a measure of correlation applied to quantitative data arranged into groups and is the standard method of assessing reliability of strength testing in the literature. The key conclusions drawn from the papers were then compared in order to produce the final conclusions of this review.
Results
A total of 29 articles were assessed, of which only three related to strength in FAI. A total of 14 further studies assessed hip muscle strength (six in hip pathology other than FAI, three in healthy adults and five in a paediatric population). A total of 12 studies assessed the reliability of the muscle testing protocol (the equipment or other aspects of the protocol). Some of these studies are summarised in Tables I and II15-24 (the remaining studies can be found in the supplementary material).
Table I.
Summary of the findings of the articles identified for inclusion (muscle strength in femoroacetabular impingement (FAI))
| Authors | Journal (yr) | Title | Level of evidence | Methodology | Key results |
|---|---|---|---|---|---|
| Muscle strength in FAI (adults) | |||||
| Casartelli et al7 | Osteoarthritis Cartilage 2011 | Hip muscle weakness in patients with symptomatic femoroacetabular impingement | 2 | FAI patients vs controls; 22 participants in each arm; HHD and MDD measures; EMG (rectus femoris and tensor fasciae latae) | FAI patients had significantly lower strength than controls for hip adduction (28%), flexion (26%), external rotation (18%) and abduction (11%); EMG activity was significantly lower in FAI; Reduced power except internal rotators and extensors. |
| Diamond et al10 | Br J SportsMed 2015 | Physical impairments and activity limitations in people with femoroacetabular impingement: a systematic review | 2 | Systematic review of physical impairment in FAI (range of movement and strength) | 16 studies found, all except Casartelli 2011 paper compared ROM; No new information regarding muscle strength |
| Harris-Heyes et al11 | J Orthop Sports Phys Ther 2014 | Persons with chronic hip joint pain exhibit reduced hip muscle strength | 3 | Young adults with chronic hip joint pain (CHJP) 35 participants and 35 controls; Age 18-40 years; Side lying, HHD used for break tests | All muscle groups weak in affected hip in chronic pain (p < 0.01); ER & abductors weak in unaffected hip of chronic pain participants (p<0.05) |
Table II.
Summary of the findings of the articles identified for inclusion (assessment of reliability)
| Authors | Journal (yr) | Title | Level of evidence | Methodology | Key results |
|---|---|---|---|---|---|
| Assessment of reliability of testing protocols or devices | |||||
| MDD | |||||
| Click Fenter et al15 | Br J Sports Med 2003 | Reliability of stabilised commercial dynamometers for measuring hip abduction strength: a pilot study. | 4 | Hip abductor strength with dynamometer (three commonly used MDD); 10 women over 3 days, different device each day | ICCs: Inter-rater: 0.90 to 0.95 (across three devices); Intra-rater: 0.88 to 0.96 (across 2 raters and three devices) |
| Ford-Smith et al16 | Arch Phys Med Rehabil 2001 | Reliability of stationary dynamometer muscle strength testing in community-dwelling older adults. | 4 | 1 wk test, retest reliability; MDD used with a single assessor; n = 25 (age 70 to 87) | ICC: Hip flexors: 0.86; Extensors (sitting): 0.73 |
| Traina et al17 | Hip Int 2010 | A reproducible and inexpensive method of measuring hip abductor strength | 4 | Reproducibility of a make-shift MDD machine created from pads and supports in clinic; Abductor strength tested twice by two examiners; n = 10 (mean age 28 yrs) | Intrarater ICC: 0.85 to 0.98; Interrater ICC: 0.81 to 0.96; High reliability for ‘MDD’ |
| HHD | |||||
| Seko et al18 | J Phys Ther Sci 2015 | Measuring seated hip extensor strength using a handheld dynamometer: an examination of the reliability and validity of the protocol. | 4 | Measuring HHD reliability; Hip extension in sitting, prone and standing; n = 20 healthy men | Higher strength and reliability in sitting and standing positions (criterion related validity 0.81); Poor reliability in prone position (CRV 0.53) |
| Kim and Lee19 | J Phys Ther Sci 2015 | The intra-and inter-rater reliabilities of lower extremity muscle strength assessment of healthy adults using a hand held dynamometer | 4 | Measuring HHD reliability (inter and intra); Two assessors; measured muscle strength of hip, knee and ankle flexion and extension; n = 55 healthy students (age 18 to 20 yrs) | High reliability; Intra-rater (> 0.9); Inter-rater (> 0.8) |
| Bloom and Cornbleet20 | PM R 2014 | Hip rotator strength in healthy young adults measured in hip flexion and extension by using a hand-held dynamometer. | 4 | Hip girdle strength measurement using HHD; 34 healthy participants; Hip rotation strength measured in flexion and extension | External rotators: no difference in flexion vs extension; Internal Rotators: significantly stronger in flexion (p < 0.01) |
| Thorborg at al21 | Scand J Med Sci Sports 2013 | Hip strength assessment using handheld dynamometry is subject to intertester bias when testers are of different sex and strength | 3 | Isometric test performed by one male and one female physiotherapy student; Ab/adduction, flexion, extension; HHD used; n = 50 (age 20 to 30 yrs) | Intra-rater ICC 0.76 to 0.95 across different muscle groups; Female rater consistently produced lower values (p < 0.05) |
| Lu et al22 | J Strength Cond Res 2011 | The Relative And Absolute Reliability Of Leg Muscle Strength Testing By A Handheld Dynamometer | 4 | Hip and knee muscle groups; HHD used for break tests; Maximal voluntary contractions; n = 16 | Excellent relative reliabilities; (ICC 0.83 to 0.92); Knee extensors least reliable |
| Youdas et al23 | Physiother Theory Pract 2008 | Determining meaningful changes in hip abductor muscle strength obtained by handheld dynamometry. | 4 | HHD used to measure bilateral hip abductor strength in healthy participants; Make test in the supine position; One tester (female); n = 90 (age 22 to 70 yrs) | Intra-rater: ICC 0.96; Minimal detectable change measured; 5.4% in men; 5.3% in women |
| Nadler et al24 | Arch Phys Med Rehabil 2000 | Portable dynamometer anchoring station for measuring strength of the hip extensors and abductors. | 4 | Specially designed dynamometer used in measuring hip extension and abduction; n = 10 (age 25 to 35) | ICC: Hip extension (prone): 0.98; Hip abduction (lateral): 0.98 |
HHD, hand-held dynamometry; MDD, motor-driven dynamometry
Muscle strength in FAI
Throughout our literature search, we found only two studies which compared hip muscle strength in patients with FAI with normal controls.7,11 Casartelli et al7 measured muscle strength and contraction using HHD, MDD and electromyography (EMG) in 22 participants with FAI and compared them with 22 healthy controls. The results revealed significantly lower muscle strength in all hip movements except for internal rotation and extension. No reason for this was suggested in the article. In addition, EMG results revealed lower activity in the tensor fascia lata in patients with FAI but no difference in rectus femoris activity between the two groups. In another study, Harris-Heyes et al11 compared hip muscle strength in normal controls with participants suffering with chronic hip joint pain (CHJP), which is an umbrella term to describe a number of conditions such as femoroacetabular impingement, labral tears and structural instability. There were 35 participants in each arm (aged 18 to 40 years). HHD was used to measure muscle strength and the results revealed that all muscle groups in the affected hip of patients with CHJP were weaker than those of the controls (p < 0.01). Furthermore, external rotators and abductors in the unaffected hip of participants with CHJP were also weaker compared with those of the controls (p < 0.05). This is an interesting finding, which has not been reported previously. Diamond et al10 conducted a review of the literature focusing on the ‘physical impairment’ in FAI. Other than Casartelli et al,7 all of the studies included in the review assessed range of movement rather than muscle strength.
Muscle strength in other hip pathology
Six studies25-30 assessed the reliability of assessment of hip muscle strength. The device used was HHD and a number of testing positions were used. The sample sizes ranged from 22 to 100 and the ICC range for HHD measurement in pathology varied from 0.38 to 0.99. There was no significant difference in the ICC values of different muscle groups. Thorborg et al26 suggested that an abduction/adduction ratio can be used as a marker of a return to normal function after hip injury in elite athletes.
Muscle strength in normal adults
Three recent studies31-33 assessed the reliability of HHD and MDD in normal adults. Although the sample sizes were small,22,34,35 the ICC values for MDD and HHD were > 0.7 and 0.87 to 0.99, respectively. Schmidt et al31 found that make tests were more reliable than break tests, and Meyer et al32 found adduction and extension strength the least reliable to measure.
Paediatric population
Five articles34,36-39 have assessed the muscle strength measurement in paediatric patients: three studies in children affected by cerebral palsy; one in children with traumatic brain injury; and another in normal participants. All except one used HHD to assess muscle strength, and the ICC values ranged from 0.67 to 0.99. Hébert et al34 discovered similar inter- and intra-rater reliability when HHD and MDD were used. Two studies34,37 found the lowest correlation values with hip extension.
Strength testing devices and protocols
Three studies15-17 measured hip muscle strength using MDD. Click Fenter et al15 compared three commercially available MDD devices when used on a population of ten participants over three separate days. They found high inter-and intra-observer reliability for all devices (ICC 0.88 to 0.95). Ford-Smith et al16 and Traina et al17 also found high ICC values for MDD devices (0.73 to 0.98).
Seven other studies18-23,30 used HHD to assess hip muscle strength in a number of positions. ICC values were again high (0.76 to 0.98), however, Seko et al18 found poor reliability when measuring hip extensor strength in the prone position (criterion-related validity = 0.53) compared with sitting or standing positions (criterion-related validity = 0.81). Thorborg et al21 also assessed the effect of the gender of the tester on the reliability of the measurement values. They found that female testers consistently produced lower values (p < 0.05) compared with their male counterparts. However, the intra-rater reliability was high (ICC 0.76 to 0.95) across all hip muscle groups. This suggests that the values recorded using HHD depend on the resistance offered by the assessor. Therefore, if a HHD is to be used to measure muscle strength, the same tester should be employed for the entire sample to avoid the significant inter-observer error.
The other significant finding was made by Bloom and Cornbleet.20 They discovered that the hip internal rotators were significantly stronger in hip flexion than in extension (p < 0.01) but no difference was seen in the strength of the external rotators in either position.
Body position and types of movement
The position of the hip joint can also affect the strength of the muscles acting on the region. Lue et al40 found that measuring hip extension was more reliable in the prone standing position (patient’s feet planted on the ground but hips flexed to 90° and the torso leaning on a flat surface) than in the prone sitting position (ICC 0.92 and 0.65, respectively).
The two main types of movements tested are isometric and isokinetic. Both have been shown to be reliable; isometric testing is possible with both HHD and MDD. It also has the advantage of producing less stress on the musculoskeletal system (important when pathology is present, as it is in FAI) than eccentric testing, thus minimising the risk of muscle injury and delayed onset muscle soreness.26 However, isokinetic testing can be standardised and is more representative of dynamic muscle action during daily life.32 Isokinetic testing can be accurately measured using MDD and the torque can be accurately measured throughout the range of movement. This is difficult to measure with HHD.
Comparisons have also been made between make and break tests. A make test is performed by the participant exerting a maximal force against a stationary dynamometer – HHD or MDD. In contrast, the break test involves a force being applied to a stationary joint until the joint gives way.41 Make tests are more reliable, more comfortable and carry a lower risk of injury than break tests.34 The choice between make and break tests was examined by Schmidt et al,31 who assessed the inter-rater reliability of hip abduction using HHD. They found that the make test was statistically more reliable but also noted that the break test was clinically more convenient.21,26,32,34,35
Discussion
There is currently no standardised protocol described in the literature for measurement of muscle strength. A number of methods of measuring muscle strength have been described such as MMT, HHD, MDD and EMG.17-22,25,26,31-35,40 This causes difficulty in comparing the different studies as there are, at times, major differences in research methodology.
The most suitable method to measure hip muscle strength in patients with FAI will depend on the priorities of the situation and the aim of the measurement. The following recommendations from our evaluation should help to guide the choice of options available:
MDD and HHD are both reliable methods of muscle strength measurement. However, the reliability of HHD depends on the consistency of the assessor and there is a high inter-observer error. In contrast, MDD eliminates this error and is therefore more reliable. However, HHD is more practical in the clinical setting. Both methods can be used reliably as long as these variations are accounted for.
Isometric results are more reliable but isokinetic results are more representative of muscle action in vivo.
Make tests should be used when feasible rather than break tests.
- It is important to standardise the measurement protocol, e.g. training of testers and verbal encouragement given to patients.
- The same tester should be used for all measurements if possible.
- The participants should be stabilised while measuring muscle strength.
- Specific muscle groups:
- Hip flexion should be measured in the standing or supine position.
- Hip extension is best measured in the standing or prone standing positions; the prone position is not recommended.
- Internal and external rotation are more reliably measured in hip flexion, e.g. sitting.
Future work therefore needs to focus on developing current methods and also isolating variables to examine their effect on the reliability of results. Ideally, this would allow the direct comparison of specific variables, for example HHD versus MDD, while keeping other variables as similar as possible. A consensus needs to be agreed among the research community to ensure that comparable conclusions can be drawn from future research.
As highlighted by the literature, some muscle group measurements are still less reliable than others.32,34 It is thought that this is due to poor stability and compensatory movements at the pelvis. Therefore, further work again needs to be done, focusing on these muscle groups, to improve the methodology with the aim of improving reliability. Another note on further work concerns the size of studies. The majority of studies involved a small number of participants, ranging from only two raters to 35 participants in comparative studies. Hébert et al34 correctly identified that for these to be clinically useful, larger samples must be used in the future. In addition, Poulsen et al25 suggested that to improve external validity, more than two clinicians should be used in future studies regarding inter-rater reliability. Finally, there are only two studies which have described muscle strength measurement and comparison in the context of FAI.7,11 These comparative studies included 22 and 35 participants in each arm, however, despite the relatively low numbers, the results have shown significantly weaker hip muscles in FAI compared with normal controls. In addition, Harris-Heyes et al11 identified weaker muscles in the unaffected hip of patients with FAI. This is surprising as patients with FAI are commonly athletic, and it merits further investigation. The paucity of research in this arena creates an exciting opportunity for future research. It must be highlighted that devising a standardised protocol for measuring hip muscle strength will improve the ability to compare future studies and enable a better understanding of the topic.
In conclusion, the most suitable method to measure hip muscle strength in patients with FAI will depend on the priorities of the situation and the aim of the measurement. There are a large number of variables in any situation; to be able to compare findings of different studies, it is pertinent to agree a set of ‘benchmarks’ in the measurement of hip muscle strength. Ideally, this should be in the form of a consensus between the centres where this research is undertaken.
From this review we would suggest that the following parameters are used in future research on the subject:
MDD and/or HHD could be used to record the measurements but the assessor should remain constant if HHD is to be used;
Make tests should be used and both isokinetic and isometric strength values should be recorded;
Hip flexion and extension should be measured in standing (not prone);
Hip rotation should be measured with hip in flexion (sitting position).
Acknowledgments
*E. Mayne and A. Memarzadeh are co-first authors
Footnotes
Author Contribution: E. Mayne: Writing the paper, Literature search, Co-first author
A. Memarzadeh: Writing the paper, Literature search, Final corrections, Co-first author
P. Raut: Literature search, Writing the paper
A. Arora: Literature search and analysis, Project support, Writing the paper
V. Khanduja: Writing the paper
ICMJE conflicts of intrest: None declared
Supplementary material
A table showing themes is available alongside the online version of this article at http://www.bjr.boneandjoint.org.uk
Funding Statement
None declared
References
- 1. Imam S, Khanduja V. Current concepts in the diagnosis and management of femoroacetabular impingement. Int Orthop 2011;35:1427-1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dooley PJ. Femoroacetabular impingement syndrome: nonarthritic hip pain in young adults. Can Fam Physician 2008;54:42-47. [PMC free article] [PubMed] [Google Scholar]
- 3. Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003;417:112-120. [DOI] [PubMed] [Google Scholar]
- 4. Bedi A, Kelly BT, Khanduja V. Arthroscopic hip preservation surgery: current concepts and perspective. Bone Joint J 2013;95-B:10-19. [DOI] [PubMed] [Google Scholar]
- 5. Fontana A, de Girolamo L. Sustained five-year benefit of autologous matrix-induced chondrogenesis for femoral acetabular impingement-induced chondral lesions compared with microfracture treatment. Bone Joint J 2015;97-B:628-635. [DOI] [PubMed] [Google Scholar]
- 6. Hack K, Di Primio G, Rakhra K, Beaulé PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg [Am] 2010;92-A:2436-2444. [DOI] [PubMed] [Google Scholar]
- 7. Casartelli NC, Maffiuletti NA, Item-Glatthorn JF, et al. Hip muscle weakness in patients with symptomatic femoroacetabular impingement. Osteoarthritis Cartilage 2011;19:816-821. [DOI] [PubMed] [Google Scholar]
- 8. Alshameeri Z, Khanduja V. The effect of femoro-acetabular impingement on the kinematics and kinetics of the hip joint. Int Orthop 2014;38:1615-1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Philippon MJ, Maxwell RB, Johnston TL, Schenker M, Briggs KK. Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc 2007;15:1041-1047. [DOI] [PubMed] [Google Scholar]
- 10. Diamond LE, Dobson FL, Bennell KL, et al. Physical impairments and activity limitations in people with femoroacetabular impingement: asystematic review. Br J SportsMed 2015;49:230-242. [DOI] [PubMed] [Google Scholar]
- 11. Harris-Hayes M, Mueller MJ, Sahrmann SA, et al. Persons with chronic hip joint pain exhibit reduced hip muscle strength. J Orthop Sports Phys Ther 2014;44:890-898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cibulka MT, White DM, Woehrle J, et al. Hip pain and mobility deficits–hip osteoarthritis: clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the American Physical Therapy Association. J Orthop Sports Phys Ther 2009;39:A1-A25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kelly BT, Williams RJ, 3rd, Philippon MJ. Hip arthroscopy: current indications, treatment options, and management issues. Am J Sports Med 2003;31:1020-1037. [DOI] [PubMed] [Google Scholar]
- 14. Clarkson HM. Musculoskeletal Assessment: Joint Range of Motion and Manual Muscle Strength. Second ed. Philadelphia: Lippincott Williams & Wilkins, 2000. [Google Scholar]
- 15. Click Fenter P, Bellew JW, Pitts TA, Kay RE. Reliability of stabilised commercial dynamometers for measuring hip abduction strength: a pilot study. Br J Sports Med 2003;37:331-334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ford-Smith CD, Wyman JF, Elswick RK, Jr, Fernandez T. Reliability of stationary dynamometer muscle strength testing in community-dwelling older adults. Arch Phys Med Rehabil 2001;82:1128-1132. [DOI] [PubMed] [Google Scholar]
- 17. Traina F, Cristofolini L, De Fine M, et al. A reproducible and inexpensive method of measuring hip abductor strength. Hip Int 2010;20:512-517. [DOI] [PubMed] [Google Scholar]
- 18. Seko T, Kumamoto T, Miura S, et al. Measuring seated hip extensor strength using a handheld dynamometer: an examination of the reliability and validity of the protocol. J Phys Ther Sci 2015;27:2179-2182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kim S-G, Lee Y-S. The intra- and inter-rater reliabilities of lower extremity muscle strength assessment of healthy adults using a hand held dynamometer. J Phys Ther Sci 2015;27:1799-1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bloom N, Cornbleet SL. Hip rotator strength in healthy young adults measured in hip flexion and extension by using a hand-held dynamometer. PM R 2014;6:1137-1142. [DOI] [PubMed] [Google Scholar]
- 21. Thorborg K, Bandholm T, Schick M, Jensen J, Hölmich P. Hip strength assessment using handheld dynamometry is subject to intertester bias when testers are of different sex and strength. Scand J Med Sci Sports 2013;23:487-493. [DOI] [PubMed] [Google Scholar]
- 22. Lu YM, Lin JH, Hsiao SF, et al. The relative and absolute reliability of leg muscle strength testing by a handheld dynamometer. J Strength Cond Res 2011;25:1065-1071. [DOI] [PubMed] [Google Scholar]
- 23. Youdas JW, Mraz ST, Norstad BJ, Schinke JJ, Hollman JH. Determining meaningful changes in hip abductor muscle strength obtained by handheld dynamometry. Physiother Theory Pract 2008;24:215-220. [DOI] [PubMed] [Google Scholar]
- 24. Nadler SF, DePrince ML, Hauesien N, et al. Portable dynamometer anchoring station for measuring strength of the hip extensors and abductors. Arch Phys Med Rehabil 2000;81:1072-1076. [DOI] [PubMed] [Google Scholar]
- 25. Poulsen E, Christensen HW, Penny JØ, et al. Reproducibility of range of motion and muscle strength measurements in patients with hip osteoarthritis - an inter-rater study. BMC Musculoskelet Disord 2012;13:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Thorborg K, Serner A, Petersen J, et al. Hip adduction and abduction strength profiles in elite soccer players: implications for clinical evaluation of hip adductor muscle recovery after injury. Am J Sports Med 2011;39:121-126. [DOI] [PubMed] [Google Scholar]
- 27. Pua YH, Wrigley TV, Cowan SM, Bennell KL. Intrarater test-retest reliability of hip range of motion and hip muscle strength measurements in persons with hip osteoarthritis. Arch Phys Med Rehabil 2008;89:1146-1154. [DOI] [PubMed] [Google Scholar]
- 28. Sherrington C, Lord SR. Reliability of simple portable tests of physical performance in older people after hip fracture. Clin Rehabil 2005;19:496-504. [DOI] [PubMed] [Google Scholar]
- 29. Wang CY, Olson SL, Protas EJ. Test-retest strength reliability: hand-held dynamometry in community-dwelling elderly fallers. Arch Phys Med Rehabil 2002;83:811-815. [DOI] [PubMed] [Google Scholar]
- 30. Arokoski MH, Arokoski JP, Haara M, et al. Hip muscle strength and muscle cross sectional area in men with and without hip osteoarthritis. J Rheumatol 2002;29:2185-2195. [PubMed] [Google Scholar]
- 31. Schmidt J, Iverson J, Brown S, Thompson PA. Comparative reliability of the make and break tests for hip abduction assessment. Physiother Theory Pract 2013;29:648-657. [DOI] [PubMed] [Google Scholar]
- 32. Meyer C, Corten K, Wesseling M, et al. Test-Retest Reliability of Innovated Strength Tests for Hip Muscles. PLoS One 2010;8:e81149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lee SPPC, Powers C. Description of a weight-bearing method to assess hip abductor and external rotator muscle performance. J Orthop Sports Phys Ther 2013;43:392-397. [DOI] [PubMed] [Google Scholar]
- 34. Hébert LJ, Maltais DB, Lepage C, et al. Isometric muscle strength in youth assessed by hand-held dynamometry: a feasibility, reliability, and validity study. Pediatr Phys Ther 2011;23:289-299. [DOI] [PubMed] [Google Scholar]
- 35. Seo DI, Kim E, Fahs CA, et al. Reliability of the one-repetition maximum test based on muscle group and gender. J Sports Sci Med 2012;11:221-225. [PMC free article] [PubMed] [Google Scholar]
- 36. Katz-Leurer M, Rottem H, Meyer S. Hand-held dynamometry in children with traumatic brain jury: within-session reliability. Pediatr Phys Ther 2008;20:259-263. [DOI] [PubMed] [Google Scholar]
- 37. Crompton J, Galea MP, Phillips B. Hand-held dynamometry for muscle strength measurement in children with cerebral palsy. Dev Med Child Neurol 2007;49:106-111. [DOI] [PubMed] [Google Scholar]
- 38. van der Linden ML, Aitchison AM, Hazlewood ME, Hillman SJ, Robb JE. Test-Retest repeatability of gluteus maximus strength testing using a fixed digital dynamometer in children with cerebral palsy. Arch Phys Med Rehabil 2004;85:2058-2063. [DOI] [PubMed] [Google Scholar]
- 39. Taylor NF, Dodd KJ, Graham HK. Test-retest reliability of hand-held dynamometric strength testing in young people with cerebral palsy. Arch Phys Med Rehabil 2004;85:77-80. [DOI] [PubMed] [Google Scholar]
- 40. Lue YJ, Hsieh CL, Liu MF, et al. Influence of testing position on the reliability of hip extensor strength measured by a handheld dynamometer. Kaohsiung J Med Sci 2009;25:126-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bohannon RW. Make tests and break tests of elbow flexor muscle strength. Phys Ther 1988;68:193-194. [DOI] [PubMed] [Google Scholar]