Abstract
Background
Using various models of behavior change, a number of studies in the area of nutrition education have confirmed that nutrition habits and behaviors can be improved.
Objectives
This study sought to determine the effects of education on patterns of dietary consumption among medical students at the military university of Tehran, with a view to correcting those patterns.
Methods
In this quasi-experimental study, 242 medical students from the Military University of Tehran were chosen by convenience sampling and then divided into control (n = 107) and intervention groups (n = 135) by block randomization. The self-administered questionnaire involving six categories of item (knowledge, perceived benefits, perceived barriers, perceived threats, self-efficacy and behavior) has been validated (Cronbach alpha > 0.7 for each).
Results
Following the educational intervention, the mean score of knowledge, health belief model (HBM) structure, and behavior of students in relation to healthy patterns of food intake increased significantly (P < 0.05). The mean pre-intervention knowledge score was 6.76 (1.452), referring to threats to HBM constructs including perceived threat 2.93 (1.147), perceived benefits 7.28 (1.07), perceived barriers 5.44 (1.831), self- efficacy 4.28 (1.479), and behavior 8.84 (2.527). The post-intervention scores all improved as follows: knowledge 8.3 (1.503), perceived threats 3.29 (1.196), perceived benefits 7.71 (0.762), perceived barriers 5.9 (1.719), self- efficacy 4.6 (1.472), and behavior 9.45 (2.324). This difference in mean scores for knowledge, health belief structures and employee behavior before and after educational intervention was significant (P ≤ 0.05).
Conclusions
The significant improvement in the experimental group’s mean knowledge, HBM structures , and behavior scores indicates the positive effect of the intervention.
Keywords: Health, Education, Nutrition Status, Students
1. Background
The association between diet and chronic diseases such as cancer, heart disease, and diabetes is well established (1, 2). Dietary habits and factors have also been shown to be associated with increased risk of gastric cancer (3, 4). Changes in dietary patterns globally have led to widespread increase in body weight and obesity. While this change has occurred more rapidly in developing countries (5), nutrition-related health issues have become more prevalent in the Middle East during the last two decades, causing changes that include increases in obesity and risk factors for chronic disease (6).
In Iran, more than 39% of deaths are related to circulatory system diseases. At present, Iran is witnessing a trend toward chronic diseases like obesity and metabolic syndromes (7), and chronic diseases (especially heart disease) are seen as a principal cause of death and disability (8). It is predicted that, with increased urbanization and mechanization, the occurrence of such diseases will rise in the near future (9, 10). One underlying cause is the consumption of rice and bread in the Iranian diet, which are considered the main sources of energy (11).
A review of studies of dietary pattern and meal courses among Iranian people revealed defects in the daily nutritional intake in various social groups (12, 13). A national health survey found that Iranians’ consumption of saturated fatty acids and the received energy exceed standard recommended amounts (14). That study focused mainly on elderly and middle-aged people, but less attention has been devoted to the unhealthy lifestyles of younger people (15). Nojomi and Najambadi (2006) found that 12.4 % of medical students in Tehran city had a BMI of more than 25 (16), and other reputable studies have emphasized the importance of consumption of fruits, vegetables, and milk among students (17).
There is evidence that nutrition education in schools and universities affects the behavior of teenagers and young people (18, 19). Given the high prevalence of obesity, more research is needed to improve lifestyle and dietary habits (20, 21). The first step in any such education program is to select an appropriate health education model (22, 23).
The health belief model (HBM) is a comprehensive framework that has proved effective in preventing disease. HBM reveals the relationship between beliefs and behaviors and assumes that preventive behavior is based on personal beliefs (24). The model holds that people will follow health recommendations when they become sufficiently motivated and believe that they are vulnerable to the disease; that this may seriously affect their life; that following the health recommendations may decrease their level of vulnerability; and that the benefits may outweigh the harms (25). The success of this approach to dietary behavior change and its ability to predict dietary habits has been demonstrated by various studies (26-28). HBM addresses the following issues: 1, perceived threats (severity and susceptibility); 2, perceived benefits; 3, perceived barriers; 4, self-efficacy.
2. Objectives
The present study sought to establish whether HBM-based education can correct the knowledge, beliefs, and behaviors informing the dietary habits of university students of medical sciences at the military university in Tehran.
3. Methods
This quasi-experimental study of 242 university students was conducted between October and December 2011. Participants were aged 18 - 32 and had no record of heart disease or other chronic diseases. Students who were maimed or disabled were also excluded from study, along with those who were not interested in participating.
The inclusion criteria specified current university students; those who were absent at that point in time were excluded. All subjects participated in the study’s educational meetings.
Sample size was obtained using the formula:
| Equation 1. |
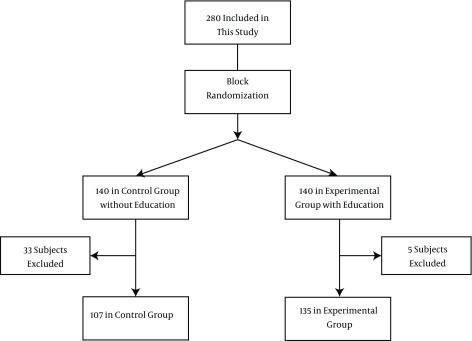
Where (∆ = PA-PB);α = 0.05, β = 0.2; Z(1-α/2) = 1.96, Z(1-β) = 0.85; PA = 0.65; and PB = 0.43 (29, 30). This yielded a sample of 101; allowing for a 40% loss, 140 subjects were selected for each group. In the end, there were 135 subjects in the intervention group and 107 control subjects. Convenience sampling was used, with allocation by block randomization (Figure 1).
Figure 1. Diagram of the Sampling Protocol for HBM-Based Educational Intervention.
Data were collected by means of a questionnaire, which included four sections: demographic features (age, marital status, field 4 items); knowledge about meal courses, ways of synthesizing nutrients, and recommended serving sizes 11 items); HBM constructs (including self-efficacy regarding correction of dietary habits 6 items; perceived benefits of consuming proper meal courses 8 items; perceived barriers to consumption and healthy food 10 items; and perceived threat of heart disease and obesity 5 items); and behavior informing dietary habits (including amounts consumed and portion sizes at breakfast, lunch, and dinner 19 items). A final question asked about the preferred type of education method (31).
To determine content validity, the questionnaire was first distributed to 10 specialists in health education, social medicine, nutrition, nursing, and epidemiology, whose views and suggestions were taken into account in producing the final questionnaire. Additionally, for finalization and internal cohesion, the questionnaire was piloted with 30 students, yielding the following Cronbach alpha coefficients: knowledge (0.79), perceived benefits (0.72), perceived barriers (0.786), perceived threat (0.783), self-efficacy (0.728) and behavior (0.718). As a Cronbach alpha of more than 0.7 indicates good internal consistency, these were considered statistically acceptable and valid (32).
3.1. Scoring
In the case of the knowledge questionnaire, each correct answer was assigned a score of 1; incorrect and don’t know responses were scored 0, yielding a range of 0 - 11. In the behavior section, investigating weekly frequency of different nutrition, mean scores were divided into three ranks: weak (below 50%), moderate (50% - 75%), or good (above 76%).
Each item on the HBM questionnaire was structured as a 3-point Likert range of responses: agree, neither agree nor disagree, and disagree. The most desirable state was assigned a score of 1 while the worst state was scored 0. In the case of self-efficacy (5 items), the maximum score was 5, and the minimum was 0. For perceived benefits (8 items), the maximum score was 8 and the minimum was 0. For perceived barriers (10 items), the maximum was 10 and the minimum was 0. For perceived threat (5 items), the maximum was 5, and the minimum was 0. Means of the HBM sections were categorized as weak (below 50%), moderate (50% - 75%), or good (above 76%). Prior to the intervention, subjects completed the questionnaire in the presence of the second author. Students’ educational needs were defined on the basis of this pre-test data collection and analysis.
3.2. Interventions
The educational methods used for the purposes of the study included a combination of lectures, question-and-answer sessions, and brainstorming. The content included an introduction to nutritional concepts, the food pyramid, the role of nutrition in lifestyle, and information about nutrition-related diseases. The first of two 60-minute sessions focused on knowledge constructs (perceived threats and perceived benefits) while the second addressed behavior constructs (perceived barriers and self-efficacy).
The first session discussed nutrition style, how to use nutrition in different meals, and food quality and value. Recent statistics were presented to alert the participants to nutrition-related diseases, the health risks of malnutrition, and cancers and coronary heart disease (CHD) (perceived threats). The quality of nutrition in different meals and their real value were explained, and students were then asked to recall their food and nutritional intake to internalize the benefits of a healthy food routine: maintaining a balanced weight, preventing CHD, and so on. The benefits of specific food items and nutritional differences were also discussed (perceived benefits).
The second session discussed barriers to a healthy food routine, such as time, expense, and friends. To modify or eradicate these perceived barriers, a list of food items was presented, along with their real calorie and energy value and the food pyramid, using flow of thought and a list of existing barriers. Self-efficacy and trusting a healthy food pattern were also discussed. The religious Hadiths (Islamic statements) were used to improve individuals’ sense of capability and responsibility (self-efficacy). At the end of each session, students’ questions were addressed. Four weeks after the end of the education intervention, the questionnaires were again administered and the new data were analyzed.
3.3. Ethical Issues
This study was informed by the declaration of Helsinki. All information remained confidential, and the requisite information was subsequently offered to the control group. The study was approved by the health research center of Baqiyatallah University of Medical Sciences (code no. MHRC_361 and registration number 57-17-5). Informed consent was obtained from all participants.
3.4. Statistical Analysis
All statistical analyses were carried out using SPSS version 18 (SPSS Inc., Chicago IL). For continuous variables, data were expressed as mean ± SD if normally distributed or as median (percentiles 25 - 75) for non-normal distributions. Categorical variables were recorded as frequency (percentage). Normality distributions of numeric variables were assessed using the Kolmogorov-Smirnov test. Paired and independent sample t-tests, Mann-Whitney U tests, Wilcoxon Signed Ranks tests and chi square tests were applied to compare two groups. A P-value of less than 0.05 was considered significant.
4. Results
In total, 242 students aged 18 - 32 years from three faculties (medical, paramedical, and nursing) at A.D., undergraduate, and PhD levels participated in the intervention. Of these, 135 were assigned to the case (experimental) group, and 107 were assigned to the control group. Table 1 summarizes their demographic and pretest data.
Table 1. Socio-Demographic Baseline Data for the Two Groupsa.
| Variables | Group | P Value | |
|---|---|---|---|
| Control | Experimental | ||
| Categorical Variables | No. (%) | No. (%) | |
| Marital Status | 0.735 | ||
| Single | 103 (97.2) | 128 (95.5) | |
| Married | 3 (2.8) | 6 (4.5) | |
| Education | 0.336 | ||
| Associated Degree | 14 (13.1) | 10 (7.4) | |
| License | 57 (53.3) | 78 (57.8) | |
| MA or Upper | 36 (33.6) | 47 (34.8) | |
| Continuous Variables | Mean (SD) | Mean (SD) | |
| Age | 20.53 (1.18) | 20.51 (1.73) | 0.912 |
| Weight | 71.14 (9.59) | 71.75 (9.95) | 0.633 |
| Knowledge | 7.11 (1.40) | 6.76 (1.45) | 0.083 |
| Behavior | 9.64 (2.30) | 8.84 (2.53) | 0.05 |
| Self-efficacy | 4.67 (1.36) | 4.28 (1.48) | 0.054 |
| Perceived benefits | 7.41 (1.12) | 7.28 (1.08) | 0.360 |
| Perceived barriers | 5.61 (1.99) | 5.44 (1.83) | 0.509 |
| Perceived threat | 3.05 (1.30) | 2.93 (1.15) | 0.472 |
aP-values based on chi square test, t-test or Mann-Whitney U test; SD = standard deviation.
In the baseline condition, experimental and control groups were compared by t-test or Mann-Whitney U test. The results indicate no statistically significant differences between the groups on HBM structures, knowledge, and behavior (P ≥ 0.05) (Table 1).
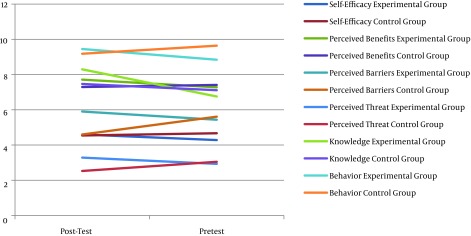
Following the educational intervention, the experimental group’s mean scores on knowledge, HBM structure, and behavior in terms of food intake increased significantly as follows. Pre-intervention: mean knowledge = 6.76 (1.452); perceived threat = 2.93 (1.147); perceived benefits = 7.28 (1.07); perceived barriers = 5.44 (1.831); self- efficacy = 4.28 (1.479); and behavior = 8.84 (2.527). Post-intervention: mean knowledge = 8.3 (1.503); perceived threats = 3.29 (1.196); perceived benefits = 7.71 (0.762); perceived barriers = 5.9 (1.719); self-efficacy = 4.6 (1.472); and behavior = 9.45 (2.324). In summary, the differences in mean scores for knowledge, health belief structures, and employee behavior before and after intervention were significant (P ≤ 0.05) (Figure 2, Table 2).
Figure 2. Pre- and Post-Intervention Comparison by Variable for Experimental and Control Groups.
Table 2. Means and Standard Deviations Before and After Educational Interventiona,b,c.
| Experimental | Case Group | Control Group | |||||
|---|---|---|---|---|---|---|---|
| Variable | Pre-Test | Post-Test | P-Value 1 | Pre-Test | Post-Test | P-Value 1 | P-Value 2 |
| Self-efficacy | 4.28 (1.479) | 4.6 (1.472) | 0.001 | 4.67 (1.358) | 4.54 (1.423) | 0.214 | P < 0.001 |
| Perceived benefits | 7.28 (1.077) | 7.71 (0.762) | 0.001 | 7.41 (1.116) | 7.29 (1.492) | 0.362 | P < 0.001 |
| Perceived barriers | 5.44 (1.831) | 5.9 (1.719) | 0.001 | 5.61 (1.994) | 4.6 (1.985) | 0.001 | P < 0.001 |
| Perceived threat | 2.93 (1.147) | 3.29 (1.196) | 0.001 | 3.05 (1.147) | 2.53 (1.196) | 0.001 | P < 0.001 |
| Knowledge | 6.76 (1.452) | 8.3 (1.503) | 0.001 | 7.11 (1.403) | 7.47 (2.129) | 0.067 | P < 0.001 |
| Behavior | 8.84 (2.527) | 9.45 (2.324) | 0.001 | 9.64 (2.300) | 9.18 (2.616) | 0.017 | P < 0.001 |
aValues are expressed as Mean (SD).
bP-value 1: based on paired sample t-test or Wilcoxon signed ranks test.
cP-value 2: based on independent sample t test or Mann-Whitney U test.
In the control group, differences before and after training between the means of knowledge, behavior, self-efficacy, perceived benefits, perceived barriers and perceived threats were analyzed by paired sample t-test or Wilcoxon Signed Ranks test. Differences in behavior, perceived barriers and perceived threat were significant (P ≤ 0.05), but differences in knowledge, self-efficacy and perceived benefits were not considered statistically significant (P ≥ 0.05) (Table 2).
5. Discussion
In the present study, the knowledge level and dietary behavior of most participants was found to be moderate, with health beliefs at a desirable level. This aligns with the findings of Xie et al. and Tan et al. (31, 33). However, in the study conducted by Nazni et al. on athletes, who pay more attention to their nutrition, the level of knowledge was found to be high (34).
In a study entitled Study of knowledge, attitude and behavior of a military population regarding healthy food routine by Tavakoli et al., most participants exhibited moderate knowledge and low behaviors. While the findings on knowledge align with the present study, those related to behavior level do not. Most participants in the present study exhibited moderate behavior, probably because of improved behavior with the passage of time as military men (9). Additionally, our subjects were young military students and therefore differ from those in military units.
The aim of this study was to investigate the effect of an intervention based on HBM in correcting the dietary pattern of medical students in a military organization during the period 2011 - 2012. The results indicate that the designed intervention had a positive effect on dietary knowledge; the control group showed no significant difference. The results of the present study echo the findings of Gammage et al., Hazavehei et al., Abbasi et al., and Gupta et al., all of whom confirmed the positive impacts of education in increasing knowledge (35-38).
The designed intervention also had a positive influence on the behavior of the experimental group, which differed significantly from the declining behavior of the control group. This decline was probably due to environmental intervention and living conditions in a military social environment; responding to behavioral and food function questionnaires may also contribute. Nevertheless, the changes in the experimental group probably reflect the positive effects of education. In general, the control group’s behavior score in the pre-test was better (higher) than that of the experimental group.
Effective education must result in behavior change, which was the case here and in other studies. For instance, Hassan et al. showed that education led to desirable nutrition behavior (39). Liu et al. showed that education improved dietary behaviors such as consumption of fruit, vegetables, and soybean products (40). However, other studies have returned different results. For example, Poddar et al. found that theory-based education did not improve dairy consumption (41), and Brown et al. showed that education did not change intake of prescribed amounts of energy, carbohydrates, protein, and lipids (42).
Given that any change in dietary behavior depends on the passage of time and on environmental issues like access to food, family nutritional habits, financial status, accommodation, and so on, interventions should consider socio-environmental issues if they are to be successful. Some studies have found that education can lead to a decrease in intake of calories, lipids, saturated lipids, and cholesterol (26), as well as impacting on appropriate weight gain (43). These differences may be due to differences of cultural background and associated nutritional habits.
Following the educational intervention, the experimental group showed a significant improvement in relation to HBM constructs (perceived benefits, perceived barriers, perceived threat, and self-efficacy). In the control group, a significant decrease was observed in relation to perceived threat and perceived barriers. This may be a consequence of their sensitivity to the questions about perceived barriers, and of thinking more about barriers to a healthy diet. That is probably because of twice answering the questionnaire in which the control group had answered the questions with speculation and concentration for the second time so they were more well-known with the questions. Moreover, their youthfulness may in part explain the decrease in perceived threat, as they may have felt more secure about chronic diseases, and there may also have been a practice effect. In summary, education improved self-efficacy, perceived threat, and perceived barriers. This positive effect of HBM-based education on diet-related health beliefs has been shown in a number of studies, including Ghaffari et al.’s study of a population of students (44) and a study by Mardani et al. of patients with diabetes, focusing on dietary adherence (45).
The improvement in mean knowledge, HBM constructs, and behavior scores in the experimental group indicates the positive effect and success of the intervention; this improvement is noteworthy, as the control group means were higher than those of the experimental group in the pre-test a mere coincidence, which is reversed after the intervention. In defining the questions, an effort was made to employ religious and Islamic questions, and the positive effects of the teaching can be attributed to these cultural questions.
Strengths of this study included the method of intervention, and the use of case and control groups. Weaknesses included the use of convenience sampling and the cross-sectional design. As the study was performed in a military context, results cannot be generalized to non- military university students. Other weaknesses include the use of a self-report questionnaire and the lack of observation of nutrition-related behavioral habits. In future research, it would be preferable to use a standardized scale of nutrition.
Acknowledgments
The authors would like to thank all the participants, who made this study possible.
Footnotes
Authors’ Contribution:Hossein Dini-Talatappeh, investigator; Hamid Reza Tavakoli, supervisor; Fatemeh Rahmati Najarkolaei, advisor and study/paper designer; Mohammad Gholami Fesharaki, statistical advisor.
Financial Disclosure:The main investigator has worked in the field of the study, which may have affected the results.
Funding/Support:The financial costs of the study were covered by the health research center, Baqiyatallah University of Medical Sciences, and military medical university students. This study forms part of the MPH thesis of second author, conducted in the health research center at Baqiyatallah University of Medical Sciences and originating from a health research center project.
References
- 1.Mirmiran P, Noori N, Zavareh M, Azizi F. Fruit and vegetable consumption and risk factors for cardiovascular disease. Metabolism. 2009;58(4):460–8. doi: 10.1016/j.metabol.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Nissinen A, Berrios X, Puska P. Community-based noncommunicable disease interventions: lessons from developed countries for developing ones. World Health Organization. 2001;79(10):963–70. [PMC free article] [PubMed] [Google Scholar]
- 3.Pourfarzi F, Whelan A, Kaldor J, Malekzadeh R. The role of diet and other environmental factors in the causation of gastric cancer in Iran—a population based study. Int J Care. 2009;125(8):1953–60. doi: 10.1002/ijc.24499. [DOI] [PubMed] [Google Scholar]
- 4.Anisi J, Tavakoli H, Rahmati Najarkolaei F. A Survey to the Connection between Nutrition and Mental Health of the Staff of a Medical Sciences University. Journal Mil Med. 2013 Jul 15;15(2):149–56. [Google Scholar]
- 5.Popkin BM. What can public health nutritionists do to curb the epidemic of nutrition‐related noncommunicable disease? Nutr Rev. 2009;67(s1):S79–82. doi: 10.1111/j.1753-4887.2009.00165.x. [DOI] [PubMed] [Google Scholar]
- 6.Rahmati-Najarkolaei F, Tavafian SS, Gholami Fesharaki M, Jafari MR. Factors predicting nutrition and physical activity behaviors due to cardiovascular disease in tehran university students: application of health belief model. Iran Red Crescent Med J. 2015;17(3):eee18879. doi: 10.5812/ircmj.18879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amani R, Noorizadeh M, Rahmanian S, Afzali N, Haghighizadeh MH. Nutritional related cardiovascular risk factors in patients with coronary artery disease in IRAN: A case-control study. Nutr J. 2010;9(70):21184687. doi: 10.1186/1475-2891-9-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Azizi F, Hatami H, Janghorbani M. Epidemiology and control of common diseases in Iran. Tehran: Eshtiagh; 2000. [Google Scholar]
- 9.Tavakoli H, Sanaei Nasab H, Karimi AA, Tavakoli R. Study of knowledge, attitude, and practice towards proper model of foods and nutrition by Military formal personnel. MilMed Journal. 2008;10(2):129–36. [Google Scholar]
- 10.Ghassemi H, Harrison G, Mohammad K. An accelerated nutrition transition in Iran. Public Health Nutr. 2002;5(1a):149–55. doi: 10.1079/PHN2001287. [DOI] [PubMed] [Google Scholar]
- 11.Sarraf-Zadegan N, Sayed-Tabatabaei FA, Bashardoost N, Maleki A, Totonchi M, Habibi HR, et al. The prevalence of coronary artery disease in an urban population in Isfahan, Iran. Acta cardiologica. 1999;54(5):257–63. [PubMed] [Google Scholar]
- 12.Salehi L, Eftekhar H, Mohammad K, Tavafian SS, Jazayery A, Montazeri A. Consumption of fruit and vegetables among elderly people: a cross sectional study from Iran. Nutr J. 2010;9(2):20070890. doi: 10.1186/1475-2891-9-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Esmaillzadeh A, Kimiagar M, Mehrabi Y, Azadbakht L, Hu FB, Willett WC. Fruit and vegetable intakes, C-reactive protein, and the metabolic syndrome. Am J Clin Nutr. 2006;84(6):1489–97. doi: 10.1093/ajcn/84.6.1489. [DOI] [PubMed] [Google Scholar]
- 14.Kimiagar SM, Ghaffarpour M, Houshiar-Rad A, Hormozdyari H, Zellipour L. Food consumption pattern in the Islamic Republic of Iran and its relation to coronary heart disease. Relation. 1998;4(3):539–47. [Google Scholar]
- 15.Borah S. Food habit of rural and urban people-a case study of jorhat district of assam. IJCMS. 2013;4(1) [Google Scholar]
- 16.Nojomi M, Najambadi S. Obesity among university students, Tehran, Iran. J Clin Nutr. 2006;15(4) [PubMed] [Google Scholar]
- 17.Aberoumand A. Studies on energy and nutrients in students diet of shehid chamran university of ahvaz, iran. Middle East J Sci Res. 2010;6(2):162–5. [Google Scholar]
- 18.Shah P, Misra A, Gupta N, Hazra D, Gupta R, Seth P, et al. Improvement in nutrition-related knowledge and behaviour of urban Asian Indian school children: findings from the ‘Medical education for children/Adolescents for Realistic prevention of obesity and diabetes and for healthy aGeing’(MARG) intervention study. Br J Nutr. 2010;104(03):427–36. doi: 10.1017/S0007114510000681. [DOI] [PubMed] [Google Scholar]
- 19.Freedman MR, Connors R. Point-of-purchase nutrition information influences food-purchasing behaviors of college students: a pilot study. J Am Diet Assoc. 2011;111(5):S42–6. doi: 10.1016/j.jada.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 20.Mohebbi I, Saadat S, Aghassi M, Shekari M, Matinkhah M, Sehat S. Prevalence of metabolic syndrome in Iranian professional drivers: results from a population based study of 12,138 men. PloS one. 2012;7(2):eee31790. doi: 10.1371/journal.pone.0031790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heshmat R, Fakhrzadeh H, Pourebrahim R, Nouri M, Pajouhi M. Evaluation of obesity and overweight and their changes pattern among 25-64 aged inhabitants of Tehran University of Medical Sciences population lab region. IJDLD. 2004;3:63–70. [Google Scholar]
- 22.Nouri K, Shojaeezadeh D. Health education and change behavior. 1 ed. Tehran: Neshaneh; 2004. [Google Scholar]
- 23.Ghaffari M, Niknami S, Kazemnejad A, Mirzae E, Ghofranipour F. Designing and validating 10 conceptual scales to prevent HIV among adolescents. J Kermanshah Univ Med Sci. 2007;11(1) [Google Scholar]
- 24.Janz NK, Becker MH. The health belief model: A decade later. Health Edu Behav. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 25.Rosenstock IM. The health belief model and nutrition education. Can J Diet Pract Res. 1982;43(3):184–92. [PubMed] [Google Scholar]
- 26.Abood DA, Black DR, Feral D. Nutrition education worksite intervention for university staff: application of the health belief model. J Nutr Educ Behav. 2003;35(5):260–7. doi: 10.1016/s1499-4046(06)60057-2. [DOI] [PubMed] [Google Scholar]
- 27.Kloeblen AS, Batish SS. Understanding the intention to permanently follow a high folate diet among a sample of low-income pregnant women according to the health belief model. Health Edu Res. 1999;14(3):327–38. doi: 10.1093/her/14.3.327. [DOI] [PubMed] [Google Scholar]
- 28.Deshpande S, Basil MD, Basil DZ. Factors influencing healthy eating habits among college students: An application of the health belief model. Health Mar Q. 2009;26(2):145–64. doi: 10.1080/07359680802619834. [DOI] [PubMed] [Google Scholar]
- 29.Tavakoli H, Nasab H, Tavakoli R, Karimi AA, editors. Study effects of education on nutritional behaviors in Iranian military personnel.; The first international and 4th national congress on health education and promotion.; 2011; Tabtiz university of medical sciences; [Google Scholar]
- 30.Dini Talatappeh H, Tavakoli HR, Rahmati Najarkolaei F, Dabbagh Moghadam A, Khoshdel A. Knowledge, Beliefs and Behavior of Food Consumption among Students of Military University: The Application of Health Belief Model (HBM). Iran J Mil Med. 2012;14(3):192–9. [Google Scholar]
- 31.Tan C, Luo JY, Wang Z, Mou JS, Zhang LL, Fu CH, et al. Knowledge, attitude, practice and related determinants on nutrition among caregivers of rural stranded children under 7-year-olds in China. Zhonghua liuxingbingxue zazhi. 2009;30(6):588–91. [PubMed] [Google Scholar]
- 32.Najarkolaei FR, Niknami S, Shokravi FA, Tavafian SS, Fesharaki MG, Jafari MR. Sexual behavioral abstine HIV/AIDS questionnaire: Validation study of an Iranian questionnaire. J Educ Health Promot. 2014;3:10. doi: 10.4103/2277-9531.127564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xie B, Zhao X, Wu Q, Su Y. [Survey on nutritional knowledge, attitude and practice among the residents in Beijing, Guangzhou and Shanghai]. hygiene Res. 1997;26(5):343–8. [PubMed] [Google Scholar]
- 34.Nazni P, Vimala S. Nutrition knowkledge, attitude and practice of college sportsmen. Sports Med. 2010;1(2) doi: 10.5812/asjsm.34866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gammage KL, Francoeur C, Mack DE, Klentrou P. Osteoporosis health beliefs and knowledge in college students: the role of dietary restraint. Eating behav. 2009;10(1):65–7. doi: 10.1016/j.eatbeh.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 36.Hazavehei SM, Taghdisi MH, Saidi M. Application of the Health Belief Model for osteoporosis prevention among middle school girl students, Garmsar, Iran. Educ health. 2007;20(1):23. [PubMed] [Google Scholar]
- 37.Abbasi G, Hadian N, editors. The effects of education on knowledge: View and function of women aged 45-65 regarding menopause and osteoporosis.; The 17th international nursing research congress focusing on evidence-based practice..2006;
- 38.Gupta N, Kochar GK. Role of nutrition education in improving the nutritional awareness among adolescent girls. Internet J Nutr. 2009;7(1) [Google Scholar]
- 39.Hassan AE, Kamal MM, Fetohy EM, Turky GM. Health education program for mothers of children suffering from iron deficiency anemia in United Arab Emirates. J Egypt Public Health Assoc. 2004;80(5-6):525–45. [PubMed] [Google Scholar]
- 40.Liu N, Mao L, Sun X, Liu L, Yao P, Chen B. The effect of health and nutrition education intervention on women's postpartum beliefs and practices: a randomized controlled trial. BMC public health. 2009;9(1):45. doi: 10.1186/1471-2458-9-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Poddar KH, Hosig KW, Anderson ES, Nickols-Richardson S, Duncan SE. Web-based nutrition education intervention improves self-efficacy and self-regulation related to increased dairy intake in college students. J Egypt Public Health Assoc. 2010;110(11):1723–7. doi: 10.1016/j.jada.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 42.Brown LN. The effects of a 5-week nutrition education intervention on collegiate athletes' knowledge and dietary intake. Oklahoma State University; 2009. [Google Scholar]
- 43.Sharifirad G, Mohebi S, Matlabi M, Abasi M, Rajati F, Tol A, et al., editors. Effectiveness of nutrition education program based on health belief model compared with traditional training on the recommended weight gain in during pregnancy.; The first international and 4th national congress on health education and promotion.; 2011; Tabtiz university of medical sciences; [Google Scholar]
- 44.Ghaffari M, Tavassoli E, Esmaillzadeh A, Hasanzadeh A. The effect of education based on health belief model on the improvement of osteoporosis preventive nutritional behaviors of second grade middle school girls in Isfahan. J Health Res Sys. 2010;6(4):1–10. [Google Scholar]
- 45.Mardani M, Piri AR. Effects of education based on health belief model on dietary adherence in diabetic patients. Diabetes Metabol Dis. 2010;9 [Google Scholar]