Abstract
Background:
Uncertainty is common in advanced illness but is infrequently studied in this context. If poorly addressed, uncertainty can lead to adverse patient outcomes.
Aim:
We aimed to understand patient experiences of uncertainty in advanced illness and develop a typology of patients’ responses and preferences to inform practice.
Design:
Secondary analysis of qualitative interview transcripts. Studies were assessed for inclusion and interviews were sampled using maximum-variation sampling. Analysis used a thematic approach with 10% of coding cross-checked to enhance reliability.
Setting/participants:
Qualitative interviews from six studies including patients with heart failure, chronic obstructive pulmonary disease, renal disease, cancer and liver failure.
Results:
A total of 30 transcripts were analysed. Median age was 75 (range, 43–95), 12 patients were women. The impact of uncertainty was frequently discussed: the main related themes were engagement with illness, information needs, patient priorities and the period of time that patients mainly focused their attention on (temporal focus). A typology of patient responses to uncertainty was developed from these themes.
Conclusion:
Uncertainty influences patient experience in advanced illness through affecting patients’ information needs, preferences and future priorities for care. Our typology aids understanding of how patients with advanced illness respond to uncertainty. Assessment of these three factors may be a useful starting point to guide clinical assessment and shared decision making.
Keywords: Uncertainty, palliative care, terminal care, qualitative research, comorbidity, communication
What is already known about the topic?
Patients with life-limiting illness commonly experience considerable uncertainty, yet uncertainty is under-researched in the context of life-limiting illness.
Much of this uncertainty cannot be eliminated, yet clinicians are often reluctant to discuss uncertainty with their patients.
If poorly addressed, uncertainty can result in poorer psychological outcomes for patients and increase use of healthcare resources.
What this paper adds?
In-depth analysis of the experience of uncertainty for patients with a range of advanced illnesses.
Information needs, temporal focus and engagement with illness are key concerns for patients.
A typology of patient responses to uncertainty based on these three factors is developed to inform clinical practice.
Implications for practice, theory or policy
When managing patients with advanced illness and an uncertain prognosis, professionals should realise that uncertainty is often a central feature of patients’ illness experience.
Our typology provides professionals with a framework to consider an individual patient’s preferences in terms of temporal focus, information needs and engagement with illness.
This may help to tailor discussions with patients so that patients’ priorities are addressed and information and support are provided according to their preferences.
Introduction
In our ageing population, an increasing number of people are living with advanced, life life-limiting illness.1 Their care and treatment are further complicated by multi-morbidity and interactions between medical conditions. Patients can struggle with the complex healthcare system of which they become a part2 and may experience a great deal of uncertainty regarding what treatments are best, the nature of their illness and the future.3
The concept of uncertainty in illness has been widely studied3–7 and can be understood to consist of uncertainty in relation to medical, personal and social domains.8 Most definitions agree that, in essence, uncertainty comprises the inability to attribute meaning to events.3,9 In her theory of uncertainty in illness, subsequently expanded to include chronic illness, Mishel4,5 argues that disease complexity, poor information provision and the unpredictability or ambiguity of events interfere with patients’ ability to confer meaning, thereby increasing uncertainty. Uncertainty is not necessarily a negative entity: it is patients’ appraisal and response to uncertainty that mediates its impact.5,7,10 For example, some patients will find prognostic uncertainty protective, as it allows them to ‘look on the bright side’, while others find not knowing what will happen distressing.
Research has mapped illness trajectories in several conditions,11,12 and much work has been undertaken in the field of prognostication.13,14 However, prognostication is based on professional judgement and inherently focuses on the clinician’s perspective,2,15 and there has been little attention to how patients themselves experience and cope with uncertainty in relation to prognosis. While experience of uncertainty has been investigated in some conditions,16 there is limited evidence related to patient experiences of uncertainty in advanced illnesses, in which trajectories are difficult to determine. Since uncertainty as to future illness course cannot be eliminated, it is crucial to understand how patients with advanced illness cope with uncertainty and how uncertainty affects their support needs and preferences for communication with healthcare providers.
We know that if uncertainty is poorly addressed and managed, it can lead to negative emotional and psychological states for patients17–19 and affect care delivery.20 Unaddressed uncertainty may result in poor adaptation to illness,21 adverse coping strategies, such as searching unrealistically for medical certainty, and conflict with health professionals.22 Unresolved emotional issues related to poor communication have been associated with higher use of healthcare services23 and poor communication of the uncertainties of cancer treatment with increased costs and higher risk of staff burnout.18 Despite these effects, we know clinicians can be reluctant to raise uncertainty with patients,24–27 and this may be a reflection of current limits to medical education.
To address these negative outcomes and inform professionals’ training needs, we need greater understanding of how patients experience and respond to uncertainty in advanced illness. This study aimed to understand experiences of uncertainty in patients with different advanced illnesses and develop a typology of their responses to uncertainty to inform future practice.
Methods
We undertook secondary analysis of in-depth qualitative interview data from studies including patients with a range of advanced illnesses. Available to us were interviews from six studies of patients with: heart failure, chronic obstructive pulmonary disease (COPD), motor neurone disease (MND), renal disease, liver disease and metastatic cancer and patients in intensive care. All studies investigated illness experience from a patient perspective. We followed the consolidated criteria for reporting qualitative research (COREQ) guidelines for reporting qualitative analyses as far as these apply to secondary analysis.28
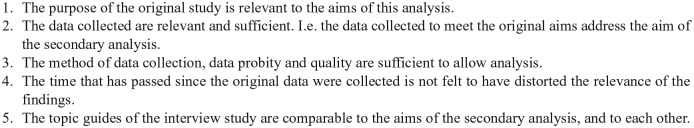
Assessment for inclusion
Data from different studies must be carefully assessed and found to be comparable if they are to be analysed together. We used criteria adapted from Stewart and Kamins29 to assess whether it was reasonable to compare the studies based on study aim, data collection method, interview topic guide, data quality and timing of data collection (Figure 1). Suitability for inclusion was discussed within the multidisciplinary research group. Following this process, two datasets were excluded: transcripts from the study in intensive care were not sufficiently relevant to the aims of this analysis (criterion 1) and data from patients with MND did not contain sufficient detail (criterion 2).
Figure 1.
Inclusion criteria – assessment of comparability of qualitative data for secondary analysis.
Source: Adapted from Stewart and Kamins.29
Sampling/selection
Five datasets30–35 containing 98 interview transcripts were eligible for inclusion (Table 1). We screened all transcripts to identify those with content particularly relevant to the experience of uncertainty. This resulted in 73 transcripts with highly relevant or relevant content. We used purposive, maximum-variation sampling to select a sample of 30 interviews from these 73 transcripts. Sampling was based on patients’ age, sex and diagnosis, with a preference for ‘highly relevant’ over ‘relevant’ content.
Table 1.
Details of included studies.
| Study | Population + sample | Sample size |
|---|---|---|
| Renal study 132 | Patients with advanced renal disease on conservative non dialytic pathway | 16 |
| Renal study 233 | Patients with end-stage renal disease on haemodialysis | 20 |
| Heart failure study30,31 | Patients with heart failure | 20 |
| AMBER care bundle evaluation35 | Patients with uncertain recovery who are supported by the AMBER care bundle (cancer, renal disease, liver disease) | 11 |
| Breathlessness study34 | Patients with cancer, COPD, MND and heart failure experiencing breathlessness | 48 (31 suitable for inclusion) |
COPD: chronic obstructive pulmonary disease; MND: motor neurone disease.
Analysis
Interview transcripts were analysed thematically using a combination of inductive and deductive coding.36 Thematic analysis was selected as the most appropriate approach to identify patterns and broad themes from the data.37 Following familiarisation with the data, one researcher (S.N.E.) developed the coding frame, with input from researchers who had conducted the analyses in the primary studies (K.B., L.E.S., F.E.M.M.) to finalise the coding frame. The researcher (S.N.E.) then applied the coding frame to the transcripts. During analysis, another researcher (K.Ba.) independently applied the coding frame to 10% of the transcripts. Discrepancies were resolved by discussion, with minor amendments to the coding frame. During analysis we recorded the new codes identified as each interview was analysed and considered that we had reached data saturation when no additional codes were identified. The final stage of analysis investigated the themes to identify a typology of patient responses to uncertainty.36 This was verified by applying the typology to the raw data and checking for fit.
Ethics
The secondary analysis was in line with the aims of the primary research studies and the original ethical approvals obtained. Additional approval for the secondary analysis was obtained from King’s College London Research and Development Service.
Results
Demographic characteristics
Interviews with 30 patients were analysed. A total of 12 patients were women; median age was 75 years (range, 43–95 years). The interviews included patients with heart failure (n = 10), COPD (n = 4), renal disease (n = 10), cancer (n = 5) and liver disease (n = 1) (Table 2)
Table 2.
Demographic characteristics of sample.
| Overall | Patients with heart failure | Patients with renal disease | Patients with COPD | Patients with cancer | Patients with liver disease | |
|---|---|---|---|---|---|---|
| n | 30 | 10a | 10b | 4 | 5c | 1 |
| % female | 40 | 20 | 40 | 75 | 50 | 0 |
| Age (median) | 75 | 72 | 83 | 69 | 62 | 43 |
| Age (range) | 43–95 | 57–80 | 59–95 | 54–75 | 52–84 | – |
COPD: chronic obstructive pulmonary disease.
All from heart failure study.
Seven from renal study 1 and three from renal study 2.
All from AMBER care bundle evaluation.
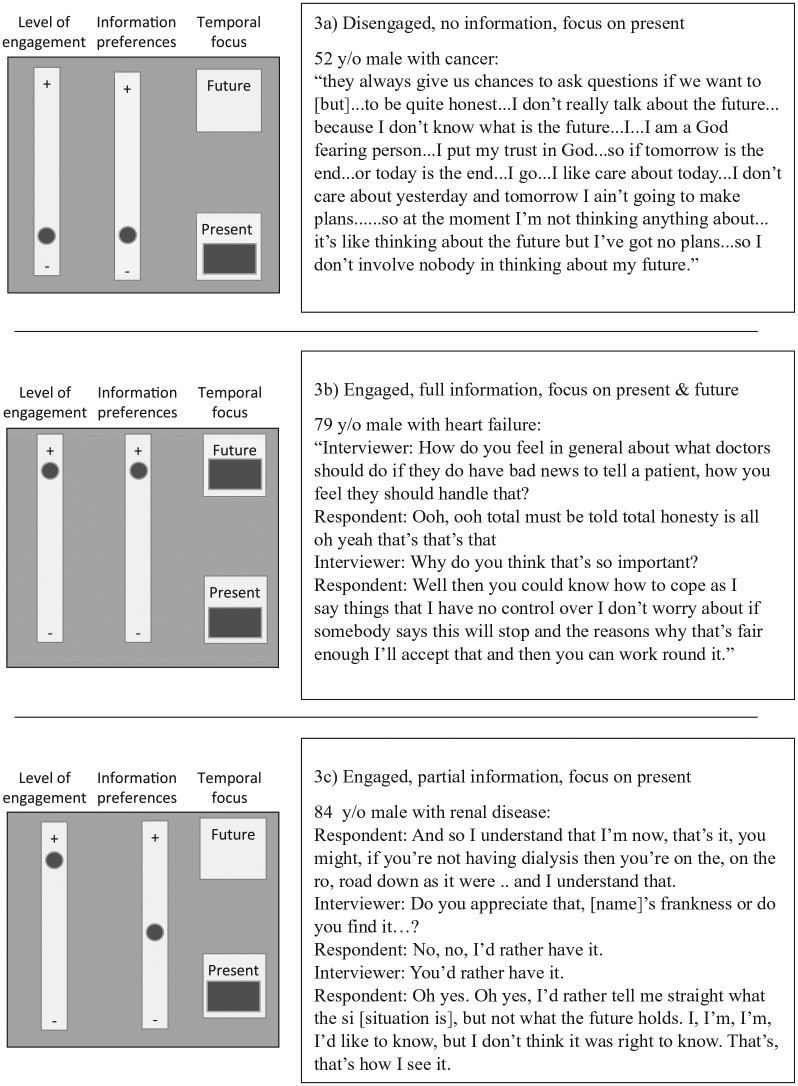
Main themes
Four main themes emerged from the analysis, relating to: (a) patients’ engagement with the illness process, (b) the period of time which patients mainly focused their attention on (denoted as ‘temporal focus’), (c) patients’ understanding of illness and information preferences and (d) patients’ priorities in the context of an uncertain future (see Figure 2). All four main themes were expressed by patients across the different disease groups.
Figure 2.
List of themes and sub-themes. Four main themes with list of sub-themes.
Patients’ engagement with the illness process: control and loss of control
The theme of engagement relates to how involved patients wanted to be in illness decisions when prognosis was uncertain. In particular, some patients sought control over these decisions, and others ceded control to health professionals and/or family members. Some patients preferred to be strongly engaged with their care, either at a general or specific level:
Yes … really involved … they give me enough time to decide if I want … yes or no … they give me enough time … don’t know about anybody else but of myself … I’ve got enough time … they will even come back to ask me … but um … I can think about what they have said and so I’m happy with that. (A5CP3, 52-year-old male patient with cancer)
Others preferred to cede control over their treatment to health professionals. Several patients felt that it was inappropriate for them to be involved with treatment decisions:
They give me the tablets, I take the tablets, I go away, I’m quite happy if they’re working, I’m quite happy. It’s when they’re not working then I have to go and see a doctor – then you have to accept what the doctor’s going to do. (HF2a, 59-year-old male patient with heart failure)
In addition to engaging with treatment decisions, some patients felt that maintaining independence in an uncertain future was a priority:
You know erm as long as, as long as I stay well and out of hospital and I can remain as independent as I can, keeping my indepen-, once my independence goes that will be me finished. I wouldn’t, I wouldn’t want people coming in here to wash me, dress me and that sort of thing … Once I’ve lost my independence that would be me. I would want, I would want the end stage to come quickly. (KP015, 72-year-old female patient with COPD)
Conversely, others were more concerned about areas where they had lost control over their lives due to illness. Some patients found it difficult to be limited by their illness:
Respondent: When I walked out on the river front a couple of hours, stay out there, no problems at all! Now I, I have to, no, I ain’t going, I got that fear of going through that door, just in case something might happen between going down there and coming back again.
Interviewer: So that’s a change for you … you’re quite anxious about -
Respondent: I’m wary, very, very wary about goin’. (HF2a, 59-year-old male patient with heart failure)
Temporal focus: facing an uncertain future
This theme describes the period of time that patients were most focused on and in particular patients’ thoughts and feelings about their future. While some patients focused mainly on their current health status, others focused on future possibilities. This was partly determined by clinical events; for example, patients receiving ongoing complex treatment tended to focus more on the present. Conversely, a recent serious illness event was associated with patients thinking more about the future; this was particularly apparent in the interviews with patients with heart failure. Some patients were attentive to both the present and the future. This is well illustrated in the interviews with patients with renal disease, where those receiving haemodialysis tended to be more focused on the present, while those receiving conservative care focused more on possible future events:
Interviewer: Do you feel the staff give you enough opportunity to talk about your care in the future?
Respondent: As I said, I don’t even think about that, I just take it day to day (HDMar, 59-year-old female patient with renal disease on haemodialysis)
They said ‘Well you, you’ve got a bit of a kidney problem’. I don’t think it was very severe at that stage … but, but it, it’s gradually got worse since I’ve gone on, and now I’m told that I’m just on the borderline, if anything happens it won’t be very pleasant as it were … I accept that. (RG29, 84-year-old male patient with renal disease on conservative pathway)
Patients who considered their future did so in different ways. Some patients contemplated possible future scenarios such as deterioration or what might happen at the end of their lives. Others were more practical and considered in detail what might happen to their families or finances in future.
Information needs and preferences
Patients’ understanding of illness
Most patients understood the ‘big picture’ of their likely prognosis. Several patients stated ‘I’m going to die’ when asked what the future held. However, patients expressed uncertainty about the illness journey ahead of them and the complexities of their treatment. Most patients described complexity in their illness course. Many had multiple illnesses and were looked after by more than one healthcare team. Complexity frequently resulted in patients having poor understanding of their illness:
Interviewer: Yeah … and do you feel they … they understand your concerns?
Respondent: Yeah … oh yeah they’re very understanding … I say when you’re in here they’re very, very good, very understanding, very helpful … it uh … it’s me that doesn’t understand. (ACPt4, 84-year-old male patient with cancer)
Some patients responded to this complexity by seeking information and engaging with their illness, whereas others disengaged from their illness entirely. Another group experienced frustration at the complexities of illness, and this was sometimes expressed as concerns about continuity of care:
I always get confused when I go to hospital as to who is actually looking after me – you have a series of consultants or whatever they are, house you know, which … all very informative, they go round in a team and then one day one disappears one evening and I wonder who he was. (HF15a, 75-year-old male patient with heart failure)
Information preferences
There was considerable variation in patients’ information preferences. At one end of the spectrum were patients who wished to be informed fully:
I’ve always find that if I ask them something they’ve told me straight forward! I’m not frightened of bad news. You know, and I’m not frightened. (HF9a, 69-year-old male patient with heart failure)
Others preferred to have no information about their illness, even if having more information might change their behaviour.
Interviewer: Would you rather have not heard?
Respondent: Yes (emphatic) … But mind you, I heard, [and] it is going to prolong my life because I [will] be more careful … but I would have preferred not to have heard.
Interviewer: So there are advantages to hearing about it …
Respondent: There are advantages, yes, because I am more careful.
Interviewer: But also disadvantages?
Respondent: Disadvantages, that’s it.
Interviewer: So on balance …?
Respondent: On balance, not to tell me. [Very definite here] (RK21, 82-year-old male patient with renal disease)
Patient priorities in the context of an uncertain future
Patients were appreciative when their priorities were addressed by healthcare professionals. Patient priorities related to four areas: appropriate communication, quality versus quantity of life, social factors and co-morbidities. Patients wanted to get the amount of information about their illness that was right for them, communicated in the right way and with the right people present. There were consequences if this procedure wasn’t followed:
Respondent: and then one of the other ones of the team came in and out the blue he said we’re going to do a biopsy and if it’s um … malignant we can’t do anything
Interviewer: Mmm …
Respondent: So me son’s gone mad, he says he’s no right to say that to me without speaking to him first and he’s had a word with them … told them er what he thought and he said in future you contact me first … they came in the following day and did the same thing and it’s like nobody had anything positive, you know, it was all um gloom and doom. Well, of course you’ll have more bad days than good days … don’t want to be told that. (A3Cp1, 67-year-old female patient with cancer)
Most patients prioritised quality of life when making decisions about their care. Some were happy to sacrifice quantity of life for quality:
So that … I felt, in general, it wouldn’t alter my … I wouldn’t get such a, a good quality of life as I’m now getting. Now I understand that not having dialysis may reduce my life by … I don’t know, maybe six months or may even be a year, but I would have had all this time … good quality, I’ve got a very good quality, well you can see the cards, birthday. So I’ve got a very good quality of life. (RG29, 84-year-old male with renal disease on conservative pathway)
Several patients prioritised others over themselves when considering the future. For example, patients who were breadwinners for their family (in this sample, generally male) prioritised ensuring that their family were provided for after their death:
No it’s not really, it’s erm one of these questions that come up before in your mind but they’re not as medical er make sure the missus has enough money to survive on (laughs) erm or at least the children are erm (pause) come and see their mum more often than they do. (HF21a, 67-year-old male patient with heart failure)
Another, smaller group of patients felt that avoidance of isolation was vital and considered social contact a priority:
I’m not one to give in, I am not one to give in. I’ll fight it to the last but I just want that little bit of confidence … especially when you’re on your own, you’ve got no one to sort of tell people how you feel. (KP018, 75-year-old female with COPD)
A number of patients, predominantly with heart failure or on dialysis, prioritised health issues unrelated to their primary diagnosis, or features of living with illness they thought professionals considered unimportant. These priorities were less likely to have been addressed than issues that were of more concern to professionals:
Respondent: I can’t go out shopping
Interviewer: So your kidney trouble stops you being able to … to do that.
Respondent: Well it’s, no, it’s not the kidney trouble … it’s the arthritis. To be truthful I don’t even know I’ve got kidney trouble. [Patient receiving haemodialysis during interview] (RDAu, 82-year-old female patient on haemodialysis)
Other patients reported that health professionals prioritised unimportant issues and were often distressed by the conflict in priorities and lack of communication about this:
… the only problem is, they keep poking me and I know there’s no blood … well there’s blood left, but they don’t seem to realise I’ve got nowhere for them to poke anymore … so that’s the only thing I would say … leave me arms alone. (A10AP1, 56-year-old female with cancer)
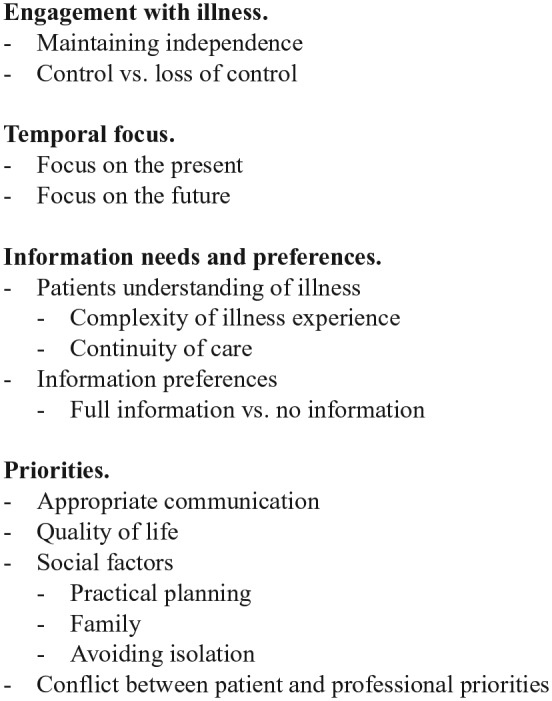
Typology of patient responses to uncertainty
Based on the themes in our data, we developed a typology of patient responses to uncertainty in advanced illness. Three factors determined patients’ response. First, patients had varying levels of engagement with their illness, treatment and the future, ranging from complete disengagement and delegation to medical professionals to close attention to all aspects of care. Second, in facing the future, patients’ temporal focus was on the present, on possible future events, or, for some patients, on both. Finally, patients’ information preferences ranged from wanting to know all the facts to not wanting any information.
Three main types were seen: (a) patients who were disengaged did not want information and focused on the present, (b) patients who were fully engaged wanted full information and considered the present and future and (c) patients who expressed intermediate views on one or all of these scales (Figure 3).
Figure 3.
Typology of patient responses to uncertainty with three examples (3 a,b,c). ‘Level of engagement’ describes the extent to which patients are actively involved in thinking about and making decisions about their illness. ‘Information preferences’ describes patient information preferences, ranging from preferring no information about illness to preferring full and detailed information. ‘Temporal focus’ describes whether patients are focused on the future or on current events.
Discussion
In this study, the first to explore patient experiences of uncertainty in depth across a range of advanced illnesses, we found that patients’ level of engagement with their illness, information preferences and temporal focus when facing the future are key factors in determining their response to uncertainty.
We found that patients’ experiences of uncertainty and the priorities they expressed were remarkably similar across the disease groups. There were exceptions to this: in particular patients with heart failure or COPD more frequently described being affected by unpredictability (in line with the organ failure disease trajectory12). Patients with heart failure more commonly described a previous serious event and its impact. Finally, patients with renal failure who were receiving dialysis and patients with heart failure described more experiences of conflict between their own priorities and those of their medical team. These differences warrant further investigation in primary qualitative research studies. As the experience of uncertainty is not unique to patients, further research into caregiver experiences of uncertainty is also needed to shed light on how uncertainty affects caregivers.
Our findings are largely supportive of Mishel’s5 established theory of uncertainty in illness, which specifies four underlying factors: complexity, unpredictability, lack of information and ambiguity. We have found complexity and unpredictability of illness to be a major part of the uncertainty experience for patients with advanced illness. Communication was a major theme, and this relates to the ‘lack of information’ aspect of Mishel’s theory. The final aspect in Mishel’s classification, ‘ambiguity concerning the state of the illness’, occurs when patients are unclear as to the meaning of illness-related events, due to unfamiliarity or complexity of events. This concept was considered less frequently by our patients and the reason for this is unclear. It may be that our secondary analysis design was insufficient to isolate ambiguity. Alternatively, it may be that once illness becomes advanced, there is less ambiguity about the illness course itself, though other uncertainties remain. Patients may also find it difficult to express their views on ambiguity or may attempt to attribute their own meanings to illness events to ‘cover up’ ambiguity.38 There is some evidence that ambiguity in the context of advanced disease is an immobiliser – that it prevents understanding and hence limits expression and decision making.39,40 Further research investigating patient responses to ambiguity will help to clarify this.
Our typology of uncertainty also links well with existing theoretical positions. In their concept analysis of uncertainty, McCormick3 identified temporality as one of the key aspects of uncertainty, which corresponds to the temporal focus aspect of our typology. Research in renal disease has also highlighted the importance of temporality to patients with advanced illness and an uncertain trajectory.33 Mishel5 noted that lack of information was one key contributor to the appraisal of uncertainty, which is reflected in our model’s information needs factor. McCormick and Mishel identified other aspects of the construct of uncertainty in illness: complexity, unpredictability, ambiguity and the probability of events occurring. We found that patients engaged to different degrees with these aspects, resulting in level of engagement as the third factor in our typology.
Our findings are highly relevant to clinical practice. Our typology provides professionals with a framework to gauge an individual patient’s preferences in three key areas. This may help to structure discussions with patients so that information and support are tailored to patients’ priorities. By providing patients with appropriate levels of information, involving them in decision making according to their level of engagement, and discussing present and/or future care according to their temporal focus, clinicians may be able to better individualise the care of patients with uncertain prognosis. Considerable evidence exists regarding communication and management of information preferences in advanced illness, particularly in cancer care.41–43 But there is less evidence regarding management of patient engagement. Shared decision-making approaches have proven effective,44 and patient activation approaches which aim to improve engagement have shown promise in other settings.45 Adaptation of these approaches to the context of uncertain prognosis may help to shape practice. However, it is unclear whether we should aim to increase engagement or manage the existing level of patient engagement. In future, the typology we propose here could be used to undertake a mixed-methods evaluation of the impact of considering these aspects of uncertainty on clinical assessment and patient care.
Evidence suggests that professionals vary in their acknowledgement and recognition of uncertainty20,26,46 and are often reluctant to discuss prognostic uncertainty.25,26 Some have argued that this reflects inadequate training of healthcare professionals to deal with uncertainty.47 Our findings concur with those of other studies demonstrating that patients frequently do want uncertainty to be made explicit.24,25 However, each patient’s priorities will be different, requiring an individually tailored approach. There are multiple factors involved in patients’ responses to uncertainty, which can be protective as well as harmful, and it is likely that professionals require more extensive training to enable them to effectively manage uncertainty. Future research should investigate professionals’ training needs in this area.
This study has both strengths and weaknesses. The secondary analysis design of this study allowed us to investigate the experience of uncertainty in a wide range of advanced illnesses and in a group of mixed age and gender. This increases the transferability of our findings and allows us to comment to some extent on the effects of different aspects of illness on the experience of uncertainty. We were able to pursue a maximum-variation sampling strategy while selecting transcripts containing the richest data relevant to our research questions. The input of authors of the primary studies ensured that the data were used appropriately and resulted in a more robust coding frame. The secondary design is a limitation, in that using data from different studies inevitably means differences between the transcripts analysed, despite our care to ensure the included studies were comparable. The secondary analysis approach means that we lacked control over what questions were asked; differences in probing between interviews resulted in richer data in some studies compared to others. We were particularly aware during analysis that data from the heart failure study were very rich, while interviews with COPD patients included less probing and fewer follow-up questions.
Our sample included more male than female patients with heart failure, while the cancer patients formed a younger demographic. This, along with the absence of advanced neurological illness, means that our data are not representative of all patients with advanced illness, though the disease groups included were fairly well represented. Finally, the coding frame was applied by a single researcher with only 10% cross checking of coding; full dual coding would have increased rigour further.
Conclusion
Uncertainty is a key component of the illness experience for patients with advanced illness. The evidence-based typology we present allows us to better understand patient responses in situations of uncertainty and develop strategies to address it in clinical practice. Better understanding and communication around uncertainty in the clinical setting can improve information provision, help to engage and empower patients and facilitate patient-centred care.
Acknowledgments
The Collaboration for Leadership in Applied Health Research and Care (CLAHRC) South London is part of the National Institute for Health Research (NIHR) and is a partnership between King’s Health Partners, St. George’s, University London and St George’s Healthcare NHS Trust. This report is funded by the National Institute for Health Research Collaboration for Leadership in Applied Health Research & Care Funding scheme. The authors would like to thank the C-CHANGE PPI group for their contributions.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: Simon Noah Etkind is funded as an Academic Clinical Fellow by the National Institute for Health Research. This article presents independent research funded by the National Institute for Health Research (NIHR) under the Programme Grants for Applied Research programme (RP-PG-1210-12015 – C-CHANGE: Delivering high quality and cost-effective care across the range of complexity for those with advanced conditions in the last year of life). Further information is available at http://www.csi.kcl.ac.uk/c-change1.html. The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, CCF, NETSCC, the NIHR Programme Grants for Applied Research or the Department of Health.
References
- 1. National population projections, 2012-based statistical bulletin. Office for National Statistics, 2013, http://webarchive.nationalarchives.gov.uk/20160105160709/http://www.ons.gov.uk/ons/dcp171778_334975.pdf
- 2. Oishi A, Murtagh FE. The challenges of uncertainty and interprofessional collaboration in palliative care for non-cancer patients in the community: a systematic review of views from patients, carers and health-care professionals. Palliat Med 2014; 28: 1081–1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McCormick KM. A concept analysis of uncertainty in illness. J Nurs Scholarsh 2002; 34: 127–131. [DOI] [PubMed] [Google Scholar]
- 4. Mishel MH. Reconceptualization of the uncertainty in illness theory. Image J Nurs Sch 1990; 22: 256–262. [DOI] [PubMed] [Google Scholar]
- 5. Mishel MH. Uncertainty in illness. Image J Nurs Sch 1988; 20: 225–232. [DOI] [PubMed] [Google Scholar]
- 6. Donovan EE, Brown LE, LeFebvre L, et al. ‘The uncertainty is what is driving me crazy’: the tripartite model of uncertainty in the adolescent and young adult cancer context. Health Commun 2015; 30: 702–713. [DOI] [PubMed] [Google Scholar]
- 7. Brashers DE. Communication and uncertainty management. J Commun 2001; 51: 477–497. [Google Scholar]
- 8. Brashers DE, Neidig JL, Russell JA, et al. The medical, personal, and social causes of uncertainty in HIV illness. Issues Ment Health Nurs 2003; 24: 497–522. [DOI] [PubMed] [Google Scholar]
- 9. Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer, 1984. [Google Scholar]
- 10. Nanton V, Munday D, Dale J, et al. The threatened self: considerations of time, place, and uncertainty in advanced illness. Br J Health Psychol 2016; 21: 351–373. [DOI] [PubMed] [Google Scholar]
- 11. Murray SA, Kendall M, Boyd K, et al. Illness trajectories and palliative care. BMJ 2005; 330: 1007–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lunney JR, Lynn J, Foley DJ, et al. Patterns of functional decline at the end of life. JAMA 2003; 289: 2387–2392. [DOI] [PubMed] [Google Scholar]
- 13. Christakis NA, Iwashyna TJ. Attitude and self-reported practice regarding prognostication in a national sample of internists. Arch Intern Med 1998; 158: 2389–2395. [DOI] [PubMed] [Google Scholar]
- 14. Davis F. Uncertainty in medical prognosis clinical and functional. Am J Sociol 1960; 66: 41–47. [Google Scholar]
- 15. Miller C. Medicine is not science: guessing the future, predicting the past. J Eval Clin Pract 2014; 20: 865–871. [DOI] [PubMed] [Google Scholar]
- 16. Hansen BS, Rørtveit K, Leiknes I, et al. Patient experiences of uncertainty – a synthesis to guide nursing practice and research. J Nurs Manag 2012; 20: 266–277. [DOI] [PubMed] [Google Scholar]
- 17. Han PKJ, Moser RP, Klein WMP. Perceived ambiguity about cancer prevention recommendations: relationship to perceptions of cancer preventability, risk, and worry. J Health Commun 2006; 11: 51–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Thorne SE, Bultz BD, Baile WF. Is there a cost to poor communication in cancer care? A critical review of the literature. Psychooncology 2005; 14: 875–884. [DOI] [PubMed] [Google Scholar]
- 19. Wright L, Afari N, Zautra A. The illness uncertainty concept: a review. Curr Pain Headache Rep 2009; 13: 133–138. [DOI] [PubMed] [Google Scholar]
- 20. Etkind S, Karno J, Edmonds PM, et al. Supporting patients with uncertain recovery: the use of the AMBER care bundle in an acute hospital. BMJ Support Palliat Care 2015; 5(1): 95–98. [DOI] [PubMed] [Google Scholar]
- 21. Lütze U, Archenholtz B. The impact of arthritis on daily life with the patient perspective in focus. Scand J Caring Sci 2007; 21: 64–70. [DOI] [PubMed] [Google Scholar]
- 22. Lillrank A. Back pain and the resolution of diagnostic uncertainty in illness narratives. Soc Sci Med 2003; 57: 1045–1054. [DOI] [PubMed] [Google Scholar]
- 23. Ashbury FD, Findlay H, Reynolds B, et al. A Canadian survey of cancer patients’ experiences: are their needs being met? J Pain Symptom Manage 1998; 16: 298–306. [DOI] [PubMed] [Google Scholar]
- 24. Barclay S, Momen N, Case-Upton S, et al. End-of-life care conversations with heart failure patients: a systematic literature review and narrative synthesis. Br J Gen Pract 2011; 61: e49–e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Momen N, Hadfield P, Kuhn I, et al. Discussing an uncertain future: end-of-life care conversations in chronic obstructive pulmonary disease. A systematic literature review and narrative synthesis. Thorax 2012; 67: 777–780. [DOI] [PubMed] [Google Scholar]
- 26. Tai-Seale M, Stults C, Zhang W, et al. Expressing uncertainty in clinical interactions between physicians and older patients: what matters? Patient Educ Couns 2012; 86: 322–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sturmberg JP. Variability, continuity and trust – towards an understanding of uncertainty in health and health care. J Eval Clin Pract 2010; 16: 401–402. [DOI] [PubMed] [Google Scholar]
- 28. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2008; 19: 349–357. [DOI] [PubMed] [Google Scholar]
- 29. Stewart DW, Kamins MA. Secondary research: information sources and methods. Newbury Park, CA: SAGE, 1993. [Google Scholar]
- 30. Harding R, Selman L, Beynon T, et al. Meeting the communication and information needs of chronic heart failure patients. J Pain Symptom Manage 2008; 36: 149–156. [DOI] [PubMed] [Google Scholar]
- 31. Selman L, Harding R, Beynon T, et al. Improving end-of-life care for patients with chronic heart failure: ‘let’s hope it’ll get better, when I know in my heart of hearts it won’t’. Heart 2007; 93: 963–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Murtagh FE, Sheerin NS, Addington-Hall J, et al. Trajectories of illness in stage 5 chronic kidney disease: a longitudinal study of patient symptoms and concerns in the last year of life. Clin J Am Soc Nephrol 2011; 6: 1580–1590. [DOI] [PubMed] [Google Scholar]
- 33. Bristowe K, Horsley HL, Shepherd K, et al. Thinking ahead – the need for early Advance Care Planning for people on haemodialysis: a qualitative interview study. Palliat Med. Epub ahead of print 19 December 2014. DOI: 10.1177/0269216314560209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bausewein C, Booth S, Gysels M, et al. Understanding breathlessness: cross-sectional comparison of symptom burden and palliative care needs in chronic obstructive pulmonary disease and cancer. J Palliat Med 2010; 13: 1109–1118. [DOI] [PubMed] [Google Scholar]
- 35. Bristowe K, Carey I, Hopper A, et al. Patient and carer experiences of clinical uncertainty and deterioration, in the face of limited reversibility: a comparative observational study of the AMBER care bundle. Palliat Med 2015; 29: 797–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ritchie J, Lewis J, Nicholls CM, et al. Qualitative research practice: a guide for social science students and researchers. Thousand Oaks, CA: SAGE, 2013. [Google Scholar]
- 37. Bristowe K, Selman L, Murtagh FEM. Qualitative research methods in renal medicine: an introduction. Nephrol Dial Transplant. Epub ahead of print 18 January 2015. DOI: 10.1093/ndt/gfu410. [DOI] [PubMed] [Google Scholar]
- 38. Gardner DS. Cancer in a dyadic context: older couples’ negotiation of ambiguity and search for meaning at the end of life. J Soc Work End Life Palliat Care 2008; 4: 135–159. [DOI] [PubMed] [Google Scholar]
- 39. Boss P, Couden BA. Ambiguous loss from chronic physical illness: clinical interventions with individuals, couples, and families. J Clin Psychol 2002; 58: 1351–1360. [DOI] [PubMed] [Google Scholar]
- 40. Hoth KF, Wamboldt FS, Strand M, et al. Prospective impact of illness uncertainty on outcomes in chronic lung disease. Health Psychol 2013; 32: 1170–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Fallowfield LJ, Jenkins VA, Beveridge HA. Truth may hurt but deceit hurts more: communication in palliative care. Palliat Med 2002; 16: 297–303. [DOI] [PubMed] [Google Scholar]
- 42. McCormack LA, Treiman K, Rupert D, et al. Measuring patient-centered communication in cancer care: a literature review and the development of a systematic approach. Soc Sci Med 2011; 72: 1085–1095. [DOI] [PubMed] [Google Scholar]
- 43. Parker SM, Clayton JM, Hancock K, et al. A systematic review of prognostic/end-of-life communication with adults in the advanced stages of a life-limiting illness: patient/caregiver preferences for the content, style, and timing of information. J Pain Symptom Manage 2007; 34: 81–93. [DOI] [PubMed] [Google Scholar]
- 44. Barry MJ, Edgman-Levitan S. Shared decision making – the pinnacle of patient-centered care. N Engl J Med 2012; 366: 780–781. [DOI] [PubMed] [Google Scholar]
- 45. Barlow J, Wright C, Sheasby J, et al. Self-management approaches for people with chronic conditions: a review. Patient Educ Couns 2002; 48: 177–187. [DOI] [PubMed] [Google Scholar]
- 46. Gordon GH, Joos SK, Byrne J. Physician expressions of uncertainty during patient encounters. Patient Educ Couns 2000; 40: 59–65. [DOI] [PubMed] [Google Scholar]
- 47. Hillman KM, Cardona-Morrell M. The ten barriers to appropriate management of patients at the end of their life. Intensive Care Med 2015; 41: 1700–1702. [DOI] [PubMed] [Google Scholar]