Abstract
Background:
There are clear indications for benefits of stance control orthoses compared to locked knee ankle foot orthoses. However, stance control orthoses still have limited function compared with a sound human leg.
Objectives:
The aim of this study was to evaluate the potential benefits of a microprocessor stance and swing control orthosis compared to stance control orthoses and locked knee ankle foot orthoses in activities of daily living.
Study design:
Survey of lower limb orthosis users before and after fitting of a microprocessor stance and swing control orthosis.
Methods:
Thirteen patients with various lower limb pareses completed a baseline survey for their current orthotic device (locked knee ankle foot orthosis or stance control orthosis) and a follow-up for the microprocessor stance and swing control orthosis with the Orthosis Evaluation Questionnaire, a new self-reported outcome measure devised by modifying the Prosthesis Evaluation Questionnaire for use in lower limb orthotics and the Activities of Daily Living Questionnaire.
Results:
The Orthosis Evaluation Questionnaire results demonstrated significant improvements by microprocessor stance and swing control orthosis use in the total score and the domains of ambulation (p = .001), paretic limb health (p = .04), sounds (p = .02), and well-being (p = .01). Activities of Daily Living Questionnaire results showed significant improvements with the microprocessor stance and swing control orthosis with regard to perceived safety and difficulty of activities of daily living.
Conclusion:
The microprocessor stance and swing control orthosis may facilitate an easier, more physiological, and safer execution of many activities of daily living compared to traditional leg orthosis technologies.
Clinical relevance
This study compared patient-reported outcomes of a microprocessor stance and swing control orthosis (C-Brace) to those with traditional knee ankle foot orthosis and stance control orthosis devices. The C-Brace offers new functions including controlled knee flexion during weight bearing and dynamic swing control, resulting in significant improvements in perceived orthotic mobility and safety.
Keywords: Lower limb orthotics, rehabilitation of orthoses users
Background
For centuries, patients suffering from paralysis or weakness of the muscles that stabilize the knee, (e.g. after acute poliomyelitis, incomplete spinal cord injury, or femoral nerve lesions), have been prescribed knee ankle foot orthoses (KAFO) with locked or posterior off-set orthotic knee joints to prevent the paretic or paralyzed leg from collapsing. Since 1978,1 stance control orthoses (SCOs) have been an orthotic option as well. SCOs are KAFOs which enable the user to freely swing their orthotic leg during swing phase and lock it for stance phase.2 The mechanisms of action3 and the benefits to patients4–10 differ remarkably between the commercially available KAFO systems. Table 1 shows the mechanisms and respective functions of the different types of KAFOs. Aside from these technical differences, the physical abilities of the patients in need of a KAFO vary widely depending on the remaining muscle functions and compensatory movement patterns.
Table 1.
Mechanisms of action of the different types of knee ankle foot orthoses with resulting technical knee controls, possible functions of the orthotic knee joint (left), and technically supported walking terrains and situations (right).
| Mechanism of action | Knee control |
Knee flexion |
Walking |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| During stance | During swing | Under weight bearing (yielding) | During swing | On level ground | On uneven ground | With different velocities | Alternating ramp/stair descent | |||||
| Locked KAFOs | The orthotic knee is locked during stance and swing. It can be manually unlocked for sitting | Locked | Locked | Not possible | Not possible | Supported | Not supported | Not supported | Not supported | |||
| KAFO with a posterior off-set knee joint | The orthotic knee is off-set posteriorly to the center of rotation of the physiological knee center in order to relocate it behind the vector of the ground reaction force at early stance phase. The dorsiflexion stop in the orthotic ankle joint prevents ventral movement of the calf during mid and terminal stance as well as dorsiflexion of the foot. Therefore, the posterior off-set of the orthotic knee joint and the dorsiflexion stop in the orthotic ankle joint result in a premature extension of the orthotic leg during stance. Moreover, the patient must develop elevated muscle forces to overcome the stabilizing knee extension moment to initiate swing | Geo-metrically locked | Free | Not possible | Possible | Supported | Not supported | Not supported | Not supported | |||
| SCOs | Weight activated | The orthotic knee is locked as soon as there is a weight load on the foot. The orthotic knee is unlocked for swing phase when the foot is unloaded, or the weight load falls short of a pre-defined threshold, or the orthosis detects a shift in weight loads from heel to forefoot that can be attributed to walking | Locked | Free | Not possible | Possible | SCOs may also be differentiated by knee angles in which they are able to lock the orthotic knee for stance | Full extension only | Supported | Not supported | Not supported | Not supported |
| Position sensor activated | The orthotic knee is locked for stance phase when it reaches full extension at the end of swing and unlocks at the end of stance when it reaches a pre-set angle relative to the ground or hip of the patient | |||||||||||
| Flexed position although | Supported | Supported | Not supported | Not supported | ||||||||
| Ankle activated | The orthosis is controlled by movements of the tibia relative to the foot resulting in unlocking the orthotic knee at the end of stance for swing. It is locked for stance when the unloaded orthosis reaches full extension | |||||||||||
| MP-SSCO C-Brace® | The C-Brace is a microprocessor stance and swing control knee ankle foot orthosis (MP-SSCO). It is designed with a carbon fiber strut with integrated ankle moment sensor and a monocentric microprocessor-controlled knee joint. A knee angle sensor provides feedback on knee angle and knee angle velocity. Extension and flexion damping are adjusted at a frequency of 50 Hz by a microprocessor with the ankle moment, the knee angle, the knee angle velocity, and the temperature of the hydraulic as input signals | Hydraulically damped and microprocessor controlled | Possible | Possible | Supported | Supported | Supported | Supported | ||||
KAFO: knee ankle foot orthosis; SCO: stance control orthosis; MP-SSCO: microprocessor stance and swing control orthosis.
A systematic review of the scientific literature on SCOs found that there are clear indications for benefits of SCOs compared to locked knee ankle foot orthoses11 (LKAFOs). However, these are mostly limited to walking on level surfaces, having resulted in only limited health insurance coverage. As most patients also have to negotiate non-level surfaces on a daily basis, the use of SCOs has not prevailed over traditional LKAFOs. Therefore, standard orthotic devices provide much less function to a patient with leg paresis than current advanced lower limb prostheses do to an individual with an amputation above the knee.
A microprocessor stance and swing control orthosis (MP-SSCO), the C-Brace (Otto Bock HealthCare GmbH, D), has been engineered to overcome the technological limitations of traditional KAFOs and SCOs, making the benefits of advanced exoprosthetic technology12–17 available to orthotic patients.
The biomechanical benefits of this MP-SSCO to patients with weakness of the leg muscles in terms of more physiologic movement patterns on various terrains have been reported recently for a part of the sample of this study.18 This article describes the results of the first patient-reported outcomes of its use in daily activities.
Methods
The device—technical description of the C-Brace
The C-Brace (Figure 1) is designed with custom carbon fiber thigh and calf shells connected by a monocentric knee joint with a microprocessor-controlled linear hydraulic damper. The orthotic knee is equipped with a sensor that detects the knee angle and knee angle velocity.19 A carbon fiber strut with an integrated ankle moment sensor connects the calf shell with the foot part.
Figure 1.
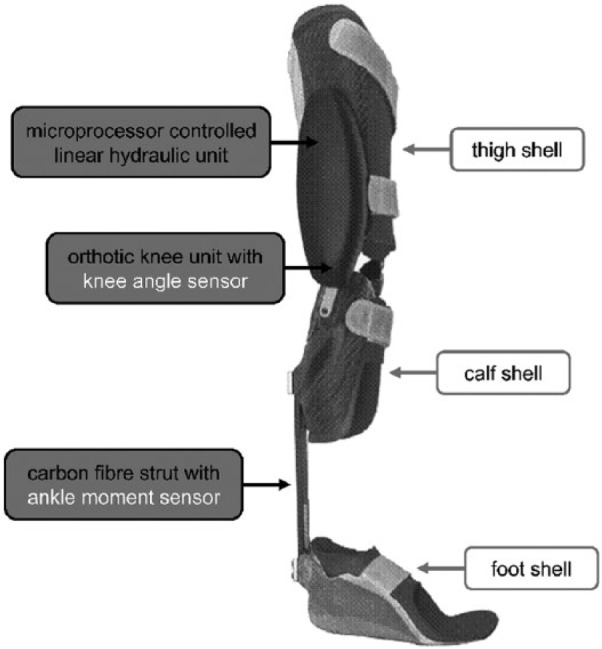
C-Brace with its components.
The microprocessor controls extension and flexion dampening of the hydraulic knee joint separately by adjusting two valves with the help of servomotors and a planetary gear set. In this way, the entire gait cycle is controlled in real time.19
The C-Brace is a default stance orthosis that switches into low flexion resistance for swing when a pre-set, customizable ankle moment is exceeded, while the knee is simultaneously extended, followed by significant knee flexion. It switches back to high flexion resistance for stance as early at the initiation of knee extension.19
The C-Brace offers controlled stance knee flexion, knee flexion during weight bearing, and dynamic control of the swing phase. Knee flexion during weight bearing makes it possible to reciprocally descend ramps and stairs and to sit down with both legs loaded.
Patient sample
Thirteen patients were enrolled in the study (9 males, 4 females, mean age 57.4 ± 14.4 years). Eight patients were poliomyelitis survivors, two of which were affected bilaterally. Three patients suffered from an incomplete spinal cord injury, one patient had a peripheral lesion of the femoral nerve, and one patient had a leg paralysis after stroke. Manual muscle testing20 demonstrated a variety of paretic or even paralytic patterns of hip and knee muscles. All patients were dependent on KAFOs. Only one patient (patient 11) needed orthoses for both legs. Five patients were using LKAFOs and eight patients used an SCO. Of the SCO patients, two had a NEURO MATIC (Fior & Gentz, Germany) and one patient used a Horton SCO (Horton’s Orthotic & Prosthetic Lab, USA)3 that can both lock in all flexed positions of the knee joint. The SPL-2 (Basko Healthcare, NL), which can only lock in full extension or 15° flexion, was used by one patient. Three patients used the E-MAG Active (Otto Bock HealthCare GmbH, D) and one used the Free Walk (Otto Bock HealthCare GmbH, D) which can both lock in full extension only. An inclusion criterion was that patients had to have used their previous orthoses for at least 6 months prior to enrollment in this study. As determined by the attending physicians of the patients, all previous orthoses had an optimal fit and the patients had received appropriate gait training at the time of fitting.
The average overall orthosis (LKAFO and/or SCO) use of the study sample was 24.3 ± 19.8 years.
Detailed information on the patients is given in Table 2.
Table 2.
Patient demographics and manual muscle test results.20
| Patient no. | Gender (female/male) | Age (years) | Underlying condition | Muscle strength |
Previous orthosis | |||
|---|---|---|---|---|---|---|---|---|
 Hip extensor |
 Hip flexor |
 Knee extensor |
 Knee flexor |
|||||
| 1 | Male | 61 | Poliomyelitis | 5 | 4–5 | 0 | 4–5 | E-MAG Active (Otto Bock, D) |
| 2 | Male | 70 | Disk herniation | 3 | 3 | 0 | 0 | E-MAG Active (Otto Bock, D) |
| 3 | Female | 32 | Incomplete spinal cord injury | 2 | 3 | 0 | 0 | E-MAG Active (Otto Bock, D) |
| 4 | Male | 56 | Incomplete femoral nerve lesion after tumor resection | 4 | 2 | 0 | 3 | NEURO MATIC (Fior & Gentz, D) |
| 5 | Male | 80 | Poliomyelitis | 3 | 4 | 3 | 3 | KAFO SPL (Basko Healthcare, NL) |
| 6 | Male | 67 | Poliomyelitis | 0 | 2 | 2 | 1 | Horton SCO (Horton’s Orthotic & Prosthetic Lab, USA) |
| 7 | Male | 46 | Stroke | 3 | 3 | 3 | 2 | NEURO MATIC (Fior & Gentz, D) |
| 8 | Male | 62 | Poliomyelitis | 2 | 1 | 1 | 0 | Free Walk (Otto Bock, D) |
| 9 | Female | 59 | Poliomyelitis | 0 | 0 | 0 | 1–2 | Locked KAFO |
| 10 | Female | 57 | Incomplete spinal cord injury | 1 | 0 | 1 | 1 | Locked KAFOs |
| bs | ||||||||
| 11 | Male | 29 | Poliomyelitis | 3 | 3 | 0 | 0 | Locked KAFO |
| 12 | Male | 68 | Poliomyelitis | 2 | 1 | 2 | 3 | Locked KAFO |
| 13 | Female | 59 | Poliomyelitis | 0 | 4 | 0 | 0 | Locked KAFO |
bs: on both sides; KAFO: knee ankle foot orthosis.
Outcome measures
To our knowledge, there are no validated outcome measures for KAFO use. Therefore, we modified the Prosthesis Evaluation Questionnaire (PEQ), a validated self-reported outcome measure in lower limb prosthetics,21 for use with lower limb orthosis users. Most of the modifications were semantic. In the questions, “prosthesis” was replaced by “orthosis,” “residual limb” by “paretic limb,” and “amputation” by “indisposition.” In addition, all seven questions on phantom pain and the two questions on the prosthetic cover were removed as they do not apply to orthoses users. The resulting Orthosis Evaluation Questionnaire (OEQ) consists of 72 questions as compared to 81 questions in the PEQ to be answered by the patients on a 100-mm visual analogue scale (VAS) with higher values representing better function.21 In addition to the total score and in analogy to the PEQ, the OEQ may be divided into nine domains of ambulation, appearance, frustration, perceived response, paretic limb health, social burden, sounds, utility, and well-being.21,22 The OEQ was analyzed in accordance with the respective guideline for the PEQ.22 The total score was computed as the mean rating of all 72 questions. The scores for the domains are calculated as the mean ratings of certain sets of questions stipulated by the guideline for the analysis of the PEQ. As not all questions are assigned to a certain domain, the removal of the nine questions on phantom pain and the prosthetic cover only affected the domain of appearance that was reduced from five to four questions.
Because of the minimal modifications and the basic comparability of mobility restrictions to amputees and leg orthosis users, the high validity of the PEQ21 was assumed to also apply to the OEQ.
Perceived difficulty of executing activities of daily living (ADLs) with both orthoses was evaluated with the Activities of Daily Living Questionnaire (ADL-Q)23 that has also previously been used in a prosthetic study. It asks the patients to rate the importance (3-point scale: 1 = not important, 2 = somewhat important, 3 = very important) and difficulty (6-point scale from 1 = very difficult to 6 = very easy) to perform 45 ADLs with the prosthesis/orthosis they are currently using. The ADLs are grouped into five activity categories: personal hygiene and dressing (4 activities), family and social life (12 activities), mobility and transportation (19 activities), sports (4 activities), and other activities (6 activities). For these categories, a mean score was calculated for all questions answered. If an activity was not done and therefore not answered, it did not contribute to the score. The individual ADLs are listed in Table 3. In addition, the patients were asked to rate the comparative perceived safety and difficulty of each of the ADLs as “safer/easier with the previous orthosis,” “no difference between the two orthoses,” or “safer/easier with the C-Brace” at the end of the study.
Table 3.
Mean ratings of difficulty of the single ADLs of the Orthotic ADLs Questionnaire (ADL-Q) for all patients (left column), SCO as previous orthosis (middle column), and LKAFO as previous orthosis (right column).
| Activity | All patients (n = 13) |
Previous orthosis: SCO (n = 8) |
Previous orthosis: LKAFO (n = 5) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Previous orthosis | C-Brace | p value | Previous orthosis | C-Brace | p value | Previous orthosis | C-Brace | p value | |||||
| Personal hygiene and dressing | Putting on pants or skirts | 4.2 | 4.1 | .67 | ns | 4.0 | 3.8 | .59 | ns | 4.6 | 4.6 | 1.00 | ns |
| 1.5 | 1.7 | 1.5 | 2.0 | 1.5 | 1.1 | ||||||||
| Putting on socks, shoes, tie shoelaces | 4.2 | 4.5 | .40 | ns | 3.6 | 4.1 | .29 | ns | 5.0 | 5.0 | 1.00 | ns | |
| 1.7 | 1.4 | 1.8 | 1.6 | 1.2 | 0.7 | ||||||||
| Using the toilet | 4.5 | 4.8 | .18 | ns | 4.4 | 4.5 | .32 | ns | 4.6 | 5.2 | .27 | ns | |
| 1.8 | 1.7 | 2.1 | 2.1 | 1.5 | 0.8 | ||||||||
| Shaving, brushing teeth, putting on make-up | 5.3 | 5.7 | .24 | ns | 5.5 | 5.6 | .59 | ns | 5.0 | 5.8 | .27 | ns | |
| .9 | .6 | .8 | .7 | 1.2 | .4 | ||||||||
| Family and social life | Carrying a child | 3.1 | 3.5 | .55 | ns | 3.4 | 3.6 | .59 | ns | 2.8 | 3.4 | .72 | ns |
| 1.6 | 2.0 | 1.5 | 2.1 | 1.8 | 2.1 | ||||||||
| Chasing with a child | 3.1 | 3.7 | .15 | ns | 3.2 | 3.5 | .58 | ns | 3.0 | 4.0 | .11 | ns | |
| 1.9 | 2.0 | 1.7 | 2.1 | 2.3 | 2.1 | ||||||||
| Pushing a stroller | 4.1 | 4.6 | .42 | ns | 4.3 | 4.3 | 1.00 | ns | 3.8 | 5.0 | .11 | ns | |
| 1.7 | 1.7 | 1.9 | 1.9 | 1.6 | 1.7 | ||||||||
| Standing in a line | 3.6 | 4.5 | .08 | ns | 3.9 | 4.5 | .24 | ns | 3.2 | 4.6 | .18 | ns | |
| 1.6 | 1.7 | 1.5 | 1.8 | 1.9 | 1.7 | ||||||||
| Walking in a crowd | 3.8 | 4.6 | .05 | * | 4.0 | 4.6 | .18 | ns | 3.4 | 4.6 | .18 | ns | |
| 1.4 | 1.4 | 1.3 | 1.6 | 1.7 | 1.3 | ||||||||
| Walking on uneven terrain | 2.7 | 4.2 | .01 | ** | 2.9 | 4.0 | .04 | * | 2.4 | 4.6 | .07 | ns | |
| 1.5 | 1.4 | 1.6 | 1.5 | 1.5 | 1.1 | ||||||||
| Walking with a dog | 3.7 | 4.4 | .24 | ns | 3.8 | 4.5 | .50 | ns | 3.3 | 4.3 | .18 | ns | |
| 1.4 | 2.2 | 1.2 | 2.1 | 2.1 | 2.9 | ||||||||
| Going for a walk | 3.3 | 4.8 | .01 | ** | 3.5 | 4.6 | .06 | ns | 3.0 | 5.0 | .04 | * | |
| 1.5 | 1.2 | 1.6 | 1.3 | 1.4 | 1.2 | ||||||||
| Pushing or pulling a shopping trolley | 4.2 | 4.8 | .01 | ** | 4.4 | 4.9 | .07 | ns | 3.8 | 4.8 | .07 | ns | |
| 1.2 | 1.2 | 1.2 | 1.1 | 1.3 | 1.6 | ||||||||
| Pulling open a heavy door | 3.5 | 4.3 | .07 | ns | 3.7 | 4.1 | .35 | ns | 3.2 | 4.6 | .11 | ns | |
| 1.5 | 1.6 | 1.4 | 1.6 | 1.8 | 1.7 | ||||||||
| Loading or unloading the trunk of a car | 3.6 | 4.5 | .09 | ns | 4.1 | 4.4 | .60 | ns | 2.8 | 4.6 | .07 | ns | |
| 1.6 | 1.4 | 1.0 | 1.3 | 2.0 | 1.7 | ||||||||
| Carrying a heavy object | 3.2 | 3.7 | .02 | * | 3.3 | 3.6 | .11 | ns | 3.0 | 3.8 | .07 | ns | |
| 1.3 | 1.4 | .9 | 1.1 | 1.9 | 2.0 | ||||||||
| Mobility and transportation | Standing up from the floor | 3.2 | 3.8 | .04 | * | 3.0 | 3.6 | .14 | ns | 3.4 | 4.0 | .11 | ns |
| 1.3 | 1.5 | 1.2 | 1.5 | 1.5 | 1.6 | ||||||||
| Stepping in a sidewalk curb | 3.6 | 4.5 | .01 | ** | 3.6 | 4.3 | .09 | ns | 3.6 | 5.0 | .04 | * | |
| 1.3 | 1.2 | 1.4 | 1.2 | 1.1 | 1.2 | ||||||||
| Stepping over minor obstacles | 3.2 | 4.3 | .01 | ** | 3.4 | 4.0 | .09 | ns | 2.8 | 4.8 | .04 | * | |
| 1.4 | 1.1 | 1.3 | .9 | 1.6 | 1.3 | ||||||||
| Stepping on minor obstacles like rocks | 2.6 | 4.1 | .01 | ** | 3.0 | 3.6 | .07 | ns | 2.0 | 4.8 | .04 | * | |
| 1.8 | 1.6 | 1.8 | 1.6 | 1.7 | 1.3 | ||||||||
| Walking with different shoes | 2.6 | 3.4 | .09 | ns | 3.0 | 3.1 | .72 | ns | 2.0 | 3.8 | .07 | ns | |
| 1.7 | 2.0 | 1.7 | 1.9 | 1.7 | 2.3 | ||||||||
| Walking up stairs | 2.9 | 4.1 | .02 | * | 3.0 | 3.5 | .11 | ns | 2.8 | 5.0 | .07 | ns | |
| 1.3 | 1.2 | 1.4 | 1.1 | 1.3 | .7 | ||||||||
| Walking down stairs | 2.5 | 4.7 | .00 | ** | 2.4 | 4.3 | .02 | * | 2.6 | 5.4 | .04 | * | |
| 1.3 | 1.3 | 1.5 | 1.3 | 1.1 | .9 | ||||||||
| Walking up ramps | 3.0 | 4.8 | .00 | ** | 3.4 | 4.6 | .04 | * | 2.4 | 5.2 | .04 | * | |
| 1.5 | 1.3 | 1.7 | 1.5 | 1.1 | .8 | ||||||||
| Walking down ramps | 2.4 | 4.4 | .00 | ** | 2.5 | 4.4 | .02 | * | 2.2 | 4.4 | .08 | ns | |
| 1.1 | 1.6 | 1.3 | 1.7 | .8 | 1.5 | ||||||||
| Walking on unknown terrain | 2.7 | 4.3 | .01 | ** | 3.0 | 4.1 | .06 | ns | 2.2 | 4.6 | .04 | * | |
| 1.3 | 1.0 | 1.5 | 1.0 | 0.8 | 1.1 | ||||||||
| Walking with different speeds | 2.9 | 4.4 | .01 | ** | 3.3 | 4.6 | .02 | * | 2.4 | 4.0 | .11 | ns | |
| 1.6 | 1.6 | 1.8 | 1.3 | 1.1 | 2.0 | ||||||||
| Walking backward | 3.3 | 3.4 | .67 | ns | 3.7 | 4.1 | .47 | ns | 2.6 | 2.4 | 1.00 | ns | |
| 1.6 | 1.8 | 1.5 | 1.3 | 1.7 | 1.9 | ||||||||
| Carrying heavy objects | 2.4 | 3.6 | .01 | ** | 3.0 | 3.6 | .07 | ns | 1.6 | 3.6 | .07 | ns | |
| 1.3 | 1.8 | 1.3 | 1.5 | .9 | 2.3 | ||||||||
| Walking outside in bad weather | 2.6 | 4.3 | .01 | ** | 3.1 | 3.9 | .07 | ns | 1.8 | 4.8 | .04 | * | |
| 1.7 | 1.5 | 2.0 | 1.9 | .8 | .8 | ||||||||
| Getting into public transportation | 3.2 | 3.8 | .08 | ns | 3.3 | 3.5 | .36 | ns | 3.2 | 4.4 | .07 | ns | |
| 1.4 | 1.6 | 1.6 | 1.8 | 1.1 | 1.1 | ||||||||
| Standing in a crowded bus | 2.5 | 3.8 | .04 | * | 2.9 | 3.5 | .29 | ns | 2.0 | 4.4 | .04 | * | |
| 1.7 | 2.0 | 1.9 | 2.2 | 1.4 | 1.5 | ||||||||
| Driving a car | 4.9 | 4.8 | .75 | ns | 4.6 | 4.4 | .72 | ns | 5.5 | 5.5 | 1.00 | ns | |
| .9 | 1.6 | 1.0 | 1.9 | .6 | .6 | ||||||||
| Riding a motorcycle or bicycle | 2.9 | 4.3 | .11 | ns | 2.4 | 4.6 | .11 | ns | 3.7 | 3.7 | 1.00 | ns | |
| 1.7 | 1.4 | 1.9 | .5 | 1.2 | 2.3 | ||||||||
| Traveling by airplane | 3.9 | 4.8 | .04 | * | 4.2 | 5.4 | .07 | ns | 3.3 | 3.7 | .32 | ns | |
| 1.6 | 1.3 | 1.5 | .5 | 2.1 | 1.5 | ||||||||
| Sports and leisure activities | Walking on a treadmill | 2.7 | 3.7 | .04 | * | 2.9 | 3.4 | .20 | ns | 2.3 | 4.3 | .11 | ns |
| 1.6 | 1.3 | 1.3 | 1.3 | 2.3 | 1.5 | ||||||||
| Doing aerobic class | 2.7 | 2.9 | .46 | ns | 2.3 | 2.5 | .59 | ns | 3.3 | 3.7 | .59 | ns | |
| 1.5 | 1.6 | 1.2 | 1.4 | 2.1 | 2.1 | ||||||||
| Ride a bike | 2.4 | 3.9 | .04 | * | 2.2 | 3.3 | .11 | ns | 3.0 | 5.5 | .18 | ns | |
| 1.3 | 1.9 | 1.5 | 1.9 | .0 | .7 | ||||||||
| Sports in general | 2.4 | 3.0 | .11 | ns | 2.6 | 2.7 | .65 | ns | 2.0 | 3.5 | .11 | ns | |
| 1.3 | 1.7 | 1.4 | 1.4 | 1.2 | 2.4 | ||||||||
| Other activities | Standing still for a longer period of time | 3.2 | 3.8 | .09 | ns | 3.4 | 3.8 | .35 | ns | 2.8 | 3.8 | .07 | ns |
| 1.4 | 1.8 | 1.3 | 1.8 | 1.6 | 2.0 | ||||||||
| Moving around in a confined place | 3.3 | 4.0 | .17 | ns | 3.9 | 4.0 | .61 | ns | 2.4 | 3.8 | .11 | ns | |
| 1.4 | 1.8 | 1.2 | 1.8 | 1.1 | 2.0 | ||||||||
| Picking up an object from the floor | 3.8 | 4.2 | .16 | ns | 4.0 | 4.0 | 1.00 | ns | 3.4 | 4.6 | .11 | ns | |
| 1.5 | 1.6 | 1.9 | 1.8 | .9 | 1.5 | ||||||||
| Sitting for a longer period of time | 3.4 | 4.1 | .14 | ns | 3.9 | 3.5 | 1.00 | ns | 2.6 | 5.0 | .04 | * | |
| 1.6 | 1.9 | 1.9 | 2.1 | .5 | 1.4 | ||||||||
| Sitting on a low chair or sofa | 2.8 | 4.3 | .01 | ** | 3.0 | 4.0 | .11 | ns | 2.4 | 4.8 | .04 | * | |
| 1.6 | 1.1 | 2.1 | 1.1 | .5 | 1.1 | ||||||||
| Doing something else while walking | 3.2 | 4.2 | .07 | ns | 3.8 | 4.0 | .59 | ns | 2.4 | 4.4 | .04 | * | |
| 1.8 | 1.8 | 1.8 | 1.9 | 1.7 | 1.8 | ||||||||
SCO: stance control orthosis; LKAFO: locked knee ankle foot orthosis; ns: not significant.
The standard deviations added under the bold mean, and all significant differences between the previous orthosis and C-Brace are marked with gray background.
: .01<p<.05; **: p<.01.
Data collection
At baseline, the patients filled out the OEQ and the ADL-Q for their existing device. They were then fitted and trained to use the MP-SSCO (C-Brace) for daily ambulation. After 3 months of MP-SSCO use, they were asked to fill out the OEQ and the ADL-Q for the MP-SSCO as well as the questionnaire for comparative perceived safety and difficulty of both devices for the 45 ADLs.
Statistical analysis
The statistical analyses of the OEQ results and the separate ratings of the ADL-Q for the previous devices and the MP-SSCO were conducted using the Wilcoxon signed rank test with a power of 80% in WIN STAT for MS Excel. As SCOs have their main benefits over LKAFOs in level surface ambulation,11 we compared the results for the MP-SSCO to those for all previous orthoses combined as well as to the subgroups of LKAFO or SCO users, respectively.
The results of the comparative part of the ADL-Q could be subjected to a descriptive statistical analysis only, as only one value per patient and ADL was obtained for comparative difficulty and safety, respectively.
This survey accompanied regular fittings based on C-Brace prescriptions by the attending physicians of the patients. Under German law (§23b Medical Device Act), such survey was exempted from ethics committee review. Nevertheless, this study was conducted in accordance with the guidelines of the ethics committee of the Georg August University Göttingen, Germany. All investigations followed the ethical and human principles of research. Written informed consent of all participants for participation and publication was obtained.
Results
OEQ
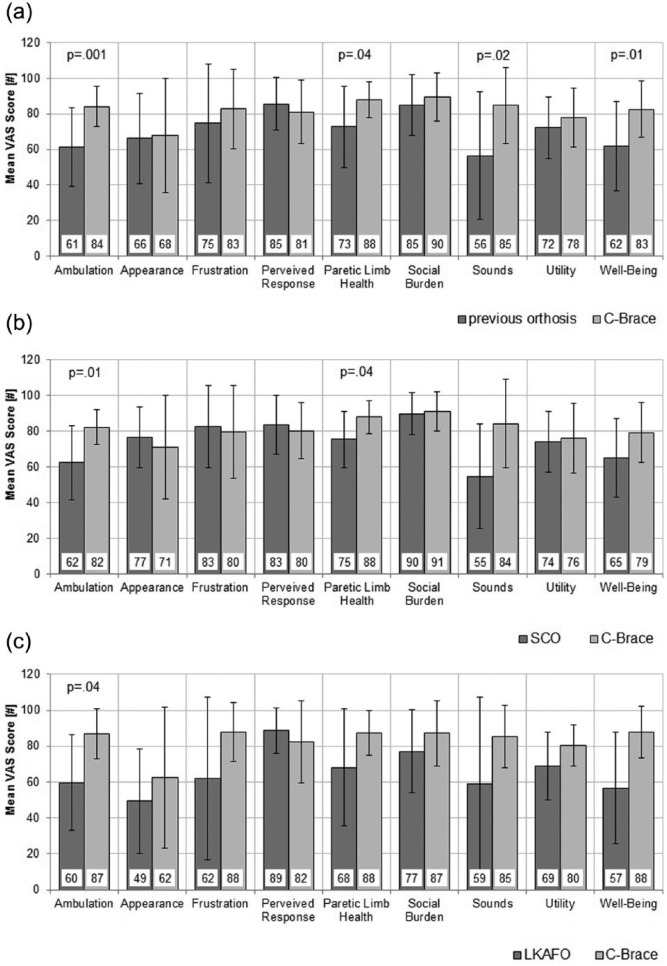
Compared to all previous orthoses combined, the results of the OEQ demonstrated significant improvements by MP-SSCO use in the total score (p = .03) and in the domains of ambulation (p = .001), paretic limb health (p = .04), sounds (p = .02), and well-being (p = .01). No differences were seen in the domains of appearance, perceived response, frustration, social burden, and utility (Figure 2(a)).
Figure 2.
Mean visual analogue scale (VAS) ratings and standard deviations of the nine subscales of (a) the Orthosis Evaluation Questionnaire (OEQ) for all patients, (b) SCO as previous orthosis, and (c) LKAFO as previous orthosis. The p value is given for all significant (p < .05) differences.
The results of the patients who entered the study using an SCO showed significant improvements with the MP-SSCO in two domains: ambulation (p = .01) and paretic limb health (p = .04) (Figure 2(b)).
The results of the patients who previously used a LKAFO demonstrated a trend toward improvement in almost all domains with MP-SSCO use, but attained significance only in ambulation (p = .04) (Figure 2(c)).
ADL-Q
Importance of the ADLs to the patients
Patients rated the importance of the 45 activities for their daily life at an average of 2.4 ± 0.4.
Difficulty of performing the ADLs with the different devices
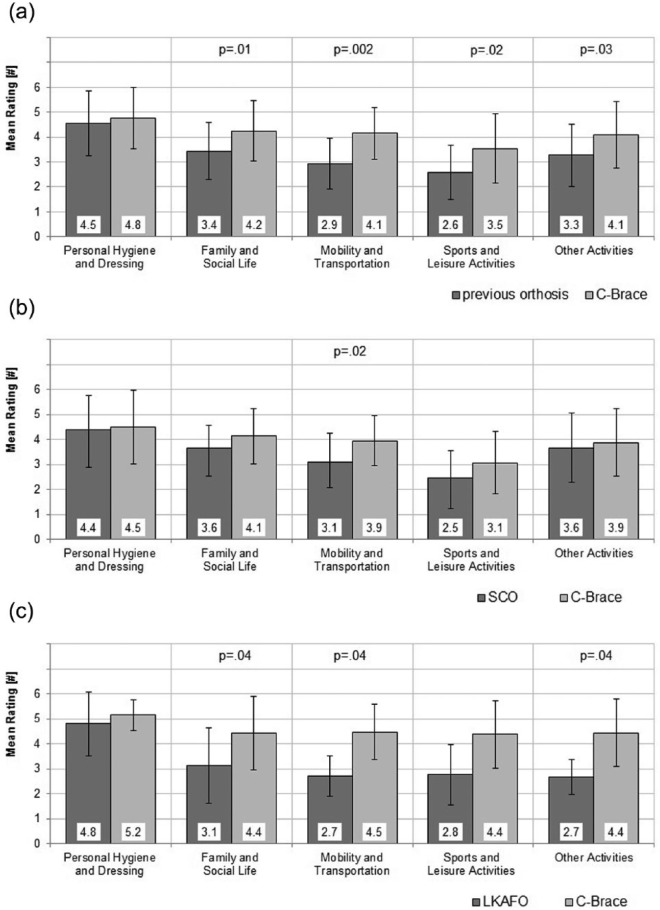
Compared to the results for all previous orthoses combined, the patients rated the activities in the domains of family and social life (p = .01) and mobility and transportation (p = .002) highly significantly easier to perform with the MP-SSCO. In the categories sports (p = .02) and other activities (p = .03), a significant improvement with the MP-SSCO could be detected. No significant difference was seen in the domain personal hygiene and dressing (Figure 3(a)).
Figure 3.
Mean ratings of difficulty of the five subscales of (a) the Orthotic ADLs Questionnaire (ADL-Q) for all patients, (b) SCO as previous orthosis, and (c) LKAFO as previous orthosis. The p value is given for all significant (p < .05) differences.
In the subgroup of previous SCO users, MP-SSCO use resulted in a significant improvement in the category of mobility and transportation (p = .02) (Figure 2(b)).
The subgroup of previous users of LKAFOs demonstrated significant improvements in the categories family and social life (p = .04), mobility and transportation (p = .04), and other activities (p = .04) when using the MP-SSCO (Figure 2(c)).
The analysis of the mean perceived difficulty of each of the 45 activities showed that 22 activities were rated significantly easier to perform with the MP-SSCO than with the previous devices combined (Table 3, left column). In the subgroup of previous SCO users, 5 activities were significantly easier to execute with the MP-SSCO and another 13 activities showed a trend toward easier execution with p values ⩽.09 (Table 3, middle column). The previous LKAFO users rated 12 activities as significantly easier to perform with the MP-SSCO, while another 9 activities presented a trend toward greater ease of execution with p values ⩽.09 (Table 3, right column).
Comparative perceived safety and difficulty of performing ADLs with the previous orthoses and the C-Brace
All 13 patients rated comparative safety and difficulty of the 45 ADLs, resulting in 585 responses for each of the two aspects of activity execution. The distributions of the answers are shown in Figure 4.
Figure 4.
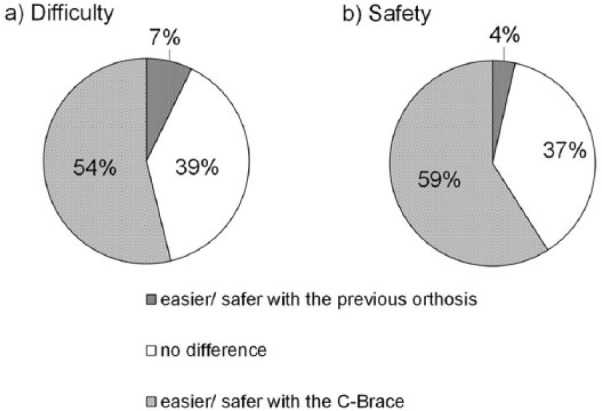
Distribution of the answers for the comparison of perceived (a) difficulty and (b) safety of the 45 activities of the Orthotic ADLs Questionnaire (ADL-Q) between the C-Brace and the previous orthoses.
Difficulty
Of the responses for perceived comparative difficulty, 54% showed a greater ease of ADL execution with the MP-SSCO, 39% no difference, and only 7% indicated an advantage of the previous orthoses (Figure 4(a)).
Safety
Of the responses for perceived comparative safety, 59% demonstrated a safer execution of ADLs with the MP-SSCO, 37% no difference, and only 4% indicated an advantage of the previous orthoses (Figure 4(b)).
Discussion
The purpose of this study was to investigate if patients perceive the MP-SSCO C-Brace useful for their everyday lives. The patients’ perception of orthotic function and difficulty to perform ADLs is of great importance for the acceptance and actual everyday use of a device.
SCOs have clear biomechanical and clinical benefits over LKAFOs,11 but these are largely limited to level walking. As soon as SCO users have to negotiate uneven ground, slopes, and stairs, the locking and unlocking mechanisms become difficult to control, resulting in many patients manually locking the knee joint for safe ambulation without free swing. This result of technical considerations of the control mechanisms is supported by the fact that in most of the 22 ADLs that showed significantly greater ease of execution with the MP-SSCO compared to all previous orthoses combined. The differences between the MP-SSCO and previous SCO or LKAFO use, respectively, were also either statistically significant or showed a statistical trend with p values ⩽.09. The biggest and statistically significant differences between the MP-SSCO and SCOs were seen in those activities that require knee flexion during weight bearing that mimics the eccentric action of the knee extensors muscles, such as walking on uneven terrain, slopes, and stairs. For most of the 22 activities, however, the subgroups of previous SCO and LKAFO users were just a little underpowered to also attain statistical significance in favor of the MP-SSCO. We therefore think that it is justified to focus the evaluation of the MP-SSCO on the comparison of the results of SCOs and LKAFOs combined.
The significant improvements in perceived orthotic function and ease of ADL execution can be explained by the technological differences between the MP-SSCO C-Brace and the standard orthoses. The mechanisms and supported functions of the standard orthotic knee joints have already been described in the introduction and summarized in Table 1. Adding the MP-SSCO C-Brace to this table makes the technological and functional differences obvious. Unlike the permanently locked (LKAFO) or locked for stance and free for swing (SCO) knees, the MP-SSCO provides continuous flexion and extension resistance in the knee during stance and swing that adjusts permanently to any ambulation requirement. This results in the orthosis mimicking the eccentric action of the knee extensor muscles supporting reciprocal slope and stair descent, which can even be utilized by long-term LKAFO or SCO users as has previously been demonstrated for a part of this study sample.18 That is the likely reason why all patients perceive it easier and safer to perform these ADLs with the MP-SSCO as observed especially in the category of mobility and transportation of the ADL-Q. These activities are an integral part of participation in family, social, and business life. Thus, improved safety and greater ease of these activities are a very good basis for reducing potential restrictions to mobility and participation. Furthermore, the improvements may also contribute to enhancing self-sufficiency and independence of the patients.
Another important aspect is the safety of the orthotic knee during swing. Based on their technology, all current types of SCOs immediately release the knee joint into free swing when the switching parameters are met.11 Once released, SCOs that lock in full extension cannot be loaded during swing before they reach full extension to relock for stance. If loaded during swing, these SCOs will collapse. SCOs that can lock in flexed position may be exposed to weight bearing as long as the knee flexion angle is smaller than their maximum locking angle.24 Therefore, the latter group of SCOs technically allows for somewhat safer walking on uneven ground.11,24 In case of stumbling with the knee joint flexed, the patient may be able to recover with this type of SCOs while it would inevitably result in a fall with the full-extension SCOs.3 The MP-SSCO, however, switches back to high stance flexion resistance as early as with the initiation of knee swing extension, to allow the patient to safely load the limb. This could be the reason why patients perceive walking on uneven terrain easier as confirmed by the results of the ADL-Q. This benefit may especially be recognized and appreciated by patients who previously used an SCO, as they no longer need to lock the knee or be prepared for a sudden knee collapse in case of locking failure or to compensate for missing knee flexion during stance phase. During slope ascent, SCOs technically do not allow for knee flexion, forcing the patient to walk with a stiff leg with reduced ground clearance. In turn, the MP-SSCO allows for knee flexion during slope ascent, resulting in improved ground clearance and greater ease of walking.
Patients who previously used an LKAFO also greatly benefit from the switching mechanism of the MP-SSCO. Most of these patients in this study were not able to safely operate an SCO18 but now have, for the first time, the chance to flex the knee during swing with the MP-SSCO. This makes many ADLs easier as it improves ground clearance (e.g. stepping on a sidewalk curb, stepping over minor obstacles, stepping on minor obstacles like rocks, and walking on unknown terrain) and makes the benefits of an unlocked KAFO11 available to these patients.
The MP-SSCO supports walking with a wide variety of gait speeds resulting in an easier execution of certain activities as seen in the ADL-Q category of mobility and transportation. Walking with different speeds seems to be especially easier for the patients who previously used an SCO that technically allows for free but uncontrolled swing. It can therefore be concluded that both SCO and LKAFO users may considerably improve perceived function and independence using the MP-SSCO, with LKAFO users benefitting on all kinds of walking terrains and SCO users mainly in non-level surface ambulation.
Limitations
With a convenience sample of 13 patients, the sample size is rather small, and the design was a pre-post survey with no crossover or randomization of the order of interventions. It should be considered, however, that, compared to other fields of medicine, the level of methodological quality and subject numbers in prosthetic and orthotic research are generally low to moderate. A systematic review of the patient benefits of SCOs11 found that most studies included only one to three patients, used no crossover or randomized order of interventions, and 40% of studies were conducted with SCOs that are not commercially available. Inasmuch, this study is among the bigger orthotic studies. Moreover, this study investigated only self-reported outcomes using two questionnaires that have not been subjected to prior validation in orthosis users. Unfortunately, we have not been able to identify any self-reported outcome measures that have been validated for use in KAFO or SCO users. Thus, every existing questionnaire validated to survey populations other than KAFO/SCO users would have presented the same limitation. Based on the comparable restrictions to mobility that amputees and leg orthosis users suffer, we assumed that questionnaires validated (PEQ) or previously used (ADL-Q) in individuals with lower limb amputations would probably best match the mobility needs of KAFO users. But, as a matter of fact, validity and reliability of the OEQ and ADL-Q for the population of leg orthosis users are still unknown.
Conclusion
The MP-SSCO may facilitate an easier, more physiological, and safer execution of many ADLs compared to traditional leg orthosis technologies. As the MP-SSCO allows for knee flexion during weight bearing, it enables leg orthosis users to perform many important ADLs such as descending ramps and stairs in a nearly physiologic and naturally reciprocal manner. Moreover, its control of knee flexion and extension during swing supports walking with a wide variety of gait speeds. The results of this study suggest that users of LKAFOs and SCOs may benefit from MP-SSCO use in terms of perceived safer and easier execution of many ADLs.
Footnotes
Author contribution: All authors contributed equally in the preparation of this manuscript.
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: All authors are employees of Otto Bock HealthCare, the manufacturer of the C-Brace.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Otto Bock HealthCare allowed the authors to work on the article during their regular working hours and use the company’s office equipment (computers, Internet access, etc).
References
- 1. Irby SE, Bernhardt KA, Kaufman KR. Gait changes over time in stance control orthosis users. Prosthet Orthot Int 2007; 31(4): 353–361. [DOI] [PubMed] [Google Scholar]
- 2. Bernhardt KA, Irby SE, Kaufman KR. Consumer opinions of a stance control knee orthosis. Prosthet Orthot Int 2006; 30(3): 246–256. [DOI] [PubMed] [Google Scholar]
- 3. Yakimovich T, Lemaire ED, Kofman J. Engineering design review of stance-control knee-ankle-foot orthoses. J Rehabil Res Dev 2009; 46(2): 257–268. [PubMed] [Google Scholar]
- 4. Davis PC, Bach TM, Pereira DM. The effect of stance control orthoses on gait characteristics and energy expenditure in knee-ankle-foot orthosis users. Prosthet Orthot Int 2010; 34(2): 206–215. [DOI] [PubMed] [Google Scholar]
- 5. Zissimopoulos A, Fatone S, Gard SA. Biomechanical and energetic effects of a stance-control orthotic knee joint. J Rehabil Res Dev 2007; 44(4): 503–514. [DOI] [PubMed] [Google Scholar]
- 6. Moreno JC, Brunetti F, Rocon E, et al. Immediate effects of a controllable knee ankle foot orthosis for functional compensation of gait in patients with proximal leg weakness. Med Biol Eng Comput 2008; 46(1): 43–53. [DOI] [PubMed] [Google Scholar]
- 7. Yakimovich T, Lemaire ED, Kofman J. Preliminary kinematic evaluation of a new stance-control knee-ankle-foot orthosis. Clin Biomech 2006; 21(10): 1081–1089. [DOI] [PubMed] [Google Scholar]
- 8. Hebert JS, Liggins AB. Gait evaluation of an automatic stance-control knee orthosis in a patient with postpoliomyelitis. Arch Phys Med Rehabil 2005; 86(8): 1676–1680. [DOI] [PubMed] [Google Scholar]
- 9. Hwang S, Kang S, Cho K, et al. Biomechanical effect of electromechanical knee-ankle-foot-orthosis on knee joint control in patients with poliomyelitis. Med Biol Eng Comput 2008; 46(6): 541–549. [DOI] [PubMed] [Google Scholar]
- 10. Schmalz T, Blumentritt S, Drewitz H. Gangphasenabhängig entriegelnde versus gesperrte Beinorthesen—biomechanische und metabolische Untersuchungen. Med Orthop Tech 2005; 125(3): 67–74. [Google Scholar]
- 11. Zacharias B, Kannenberg A. Clinical benefits of stance control orthosis systems: an analysis of the scientific literature. J Prosthet Orthot 2012; 24(1): 2–8. [Google Scholar]
- 12. Highsmith MJ, Kahle JT, Bongiorni DR, et al. Safety, energy efficiency, and cost-effectiveness of the C-leg for transfemoral amputees. Prosth Orthot Int 2010; 34(4): 362–377. [DOI] [PubMed] [Google Scholar]
- 13. Bellmann M, Schmalz T, Blumentritt S. Comparative biomechanical analysis of current microprocessor-controlled prosthetic knee joints. Arch Phys Med Rehabil 2010; 91(4): 644–652. [DOI] [PubMed] [Google Scholar]
- 14. Blumentritt S, Schmalz T, Jarasch R. The safety of C-leg: biomechanical tests. J Prosthet Orthot 2009; 21(1): 2–17. [Google Scholar]
- 15. Wetz HH, Hafkemeyer U, Drerup B. Einfluss des C-Leg-Kniegelenk-Passteiles der Fa. Otto Bock auf die Versorgungsqualität Oberschenkelamputierter. Orthopäde 2005; 34(4): 298–319. [DOI] [PubMed] [Google Scholar]
- 16. Drerup B, Wetz HH, Tiemeyer K, et al. Langzeitergebnisse mit dem C-Leg Kniegelenksystem: qualitätskontrolle der Indikationsstellung der Klinischen Prüfstellen. Med Orth Tech 2010; 130(2): 7–16. [Google Scholar]
- 17. Hafner BJ, Willingham LL, Buell NC, et al. Evaluation of function, performance, and preference as transfemoral amputees transition from mechanical to microprocessor control of the prosthetic knee. Arch Phys Med Rehabil 2007; 88(2): 207–217. [DOI] [PubMed] [Google Scholar]
- 18. Schmalz T, Proebsting E, Auberger R, et al. A functional comparison of conventional knee-ankle-foot orthoses and a microprocessor-controlled leg orthosis system based on biomechanical parameters. Prosthet Orthot Int 2016; 40(2): 277–286. [DOI] [PubMed] [Google Scholar]
- 19. Pahl E, Auberger R. Ganzbeinorthese mit kontrollierter Schwung- und Standphase. Orth Tech 2013; 64(1): 28–31. [Google Scholar]
- 20. Janda V. Manuelle Muskelfunktionsdiagnostik. 4th ed. München; Jena: Urban & Fischer, 2000. [Google Scholar]
- 21. Legro MW, Reiber GD, Smith DG, et al. Prosthesis evaluation questionnaire for persons with lower limb amputations: assessing prosthesis-related quality of life. Arch Phys Med Rehabil 1998; 79(8): 931–938. [DOI] [PubMed] [Google Scholar]
- 22. Prosthetic Research Study. Prosthesis Evaluation Questionnaire. Seattle, WA: Prosthetics Research Study, 1998, pp. 1–21, http://www.prs-research.org (accessed 29 April 2013). [Google Scholar]
- 23. Kannenberg A, Zacharias B, Mileusnic M. Activities of daily living: Genium Bionic Prosthetic knee compared with C-Leg. J Prosthet Orthot 2013; 25(3): 110–118. [Google Scholar]
- 24. McMillan AG, Kendrick K, Michael JW, et al. Preliminary evidence for effectiveness of a stance control orthosis. J Prosthet Orthot 2004; 16(1): 6–13. [Google Scholar]