Abstract
Background:
Medial patellofemoral ligament (MPFL) reconstruction is a procedure aimed to reestablish the checkrein to lateral patellar translation in patients with symptomatic patellofemoral instability. Correct femoral tunnel position is thought to be crucial to successful MPFL reconstruction, but the accuracy of this statement in terms of patient outcomes has not been tested.
Purpose:
To assess the accuracy of femoral tunnel placement in an MPFL reconstruction cohort and to determine the correlation between tunnel accuracy and a validated disease-specific, patient-reported quality-of-life outcome measure.
Study Design:
Case series; Level of evidence, 4.
Methods:
Between June 2008 and February 2014, a total of 206 subjects underwent an MPFL reconstruction. Lateral radiographs were measured to determine the accuracy of the femoral tunnel by measuring the distance from the center of the femoral tunnel to the Schöttle point. Banff Patella Instability Instrument (BPII) scores were collected a mean 24 months postoperatively.
Results:
A total of 155 (79.5%) subjects had adequate postoperative lateral radiographs and complete BPII scores. The mean duration of follow-up (±SD) was 24.4 ± 8.2 months (range, 12-74 months). Measurement from the center of the femoral tunnel to the Schöttle point resulted in 143 (92.3%) tunnels being categorized as “good” or “ideal.” There were 8 failures in the cohort, none of which occurred in malpositioned tunnels. The mean distance from the center of the MPFL tunnel to the center of the Schöttle point was 5.9 ± 4.2 mm (range, 0.5-25.9 mm). The mean postoperative BPII score was 65.2 ± 22.5 (range, 9.2-100). Pearson r correlation demonstrated no statistically significant relationship between accuracy of femoral tunnel position and BPII score (r = –0.08; 95% CI, –0.24 to 0.08).
Conclusion:
There was no evidence of a correlation between the accuracy of MPFL reconstruction femoral tunnel in relation to the Schöttle point and disease-specific quality-of-life scores. Graft failure was not related to femoral tunnel placement. The patellofemoral instability population is complex, and patients present with multiple risk factors that, in addition to the accuracy of femoral tunnel position, contribute to quality of life and warrant further investigation.
Keywords: patellofemoral instability, patellofemoral stabilization, patellar dislocation, patellar instability, quality of life, MPFL reconstruction
Patellofemoral instability is a common knee problem that is frequently associated with pain, decreased activity, reduced quality of life, and long-term osteoarthritis.10,13,23,25 Medial patellofemoral ligament (MPFL) reconstruction is an accepted procedure to stabilize the patella and has demonstrated excellent results.8,9,17,21,29,42 Correct femoral tunnel position is crucial to successful MPFL reconstruction.4,27,34,43,44 Biomechanical studies have demonstrated that the femoral tunnel position is the most important factor affecting isometric behavior of the MPFL ligament.¶ These studies have demonstrated that malpositioning of the femoral tunnel changes the isometry of the ligament graft and increases patellofemoral contact pressures.31,39,40
In 2007, Schöttle et al33 described the fluoroscopic landmarks for MPFL reconstruction femoral tunnel position using a lateral view. In this study of 8 cadaveric specimens, a radiopaque marker placed in the femoral insertion of the MPFL was within a 5-mm area that is now widely known as the “Schöttle point.” The Schöttle point is located 1.3 ± 1.7 mm anterior to the posterior cortical line and between 2 perpendicular lines to this extension line. Of these perpendicular lines, 1 intersects the contact of the posterior femoral condyle with the posterior cortex and 1 intersects the posterior point of the Blumensaat line. The Schöttle point has been used as a reference standard to assess the accuracy of MPFL femoral tunnel placement after reconstructive surgery.2,11,18,22,28,46
The Banff Patella Instability Instrument (BPII) was published in 2013 and is the only disease-specific, patient-reported quality-of-life outcome measure validated specifically for patients with patellofemoral instability.12–14,19 It is a 32-question, self-administered quality-of-life outcome measure. Questions are answered on a 100-mm visual analog scale, and the sum total of all items is converted to a score out of 100. The BPII is designed to capture a holistic view of the quality of life of patients with patellofemoral instability by assessing a broad range of constructs, including symptoms and physical complaints, work-related concerns, recreation- and sport-related concerns, lifestyle concerns, and social and emotional concerns. The BPII has demonstrated content validity, strong internal consistency, excellent reliability, and a statistically significant level of construct validity in both unstable and surgically stabilized patellofemoral instability patients.13,14
The purpose of this study was to assess the accuracy of femoral tunnel placement in an MPFL reconstruction cohort and to determine the correlation between femoral tunnel accuracy and a validated disease-specific patient-reported quality-of-life outcome measure.
Methods
Between June 2008 and February 2014, a total of 206 patients underwent an MPFL reconstruction by a single fellowship-trained sport medicine and arthroscopy knee surgeon (L.A.H.). The diagnosis of patellar instability was confirmed via subjective, clinical, and diagnostic imaging assessment. The MPFL reconstruction procedures were performed using a consistent surgical technique. After appropriate anesthesia, the limb was prepped and draped in a sterile fashion. A thorough examination under anesthesia was completed, and the diagnosis of patellofemoral instability was confirmed. The semitendinosus or gracilis tendon was harvested. A diagnostic and therapeutic knee arthroscopy was performed. The graft was attached to the superomedial border of the patella using two 3.3 Poplok suture anchors (ConMed Linvatec) around a prepared bleeding bone bed. The graft was passed to the femoral insertion point through layer 2 of the knee, below the vastus medialis fascia in an extra-articular position. Approximate femoral tunnel placement was assessed using the palpation method to determine anatomic landmarks,32 placing the guide pin in the saddle between the medial epicondyle and the adductor tubercle. Femoral tunnel placement was then finalized by assessment of graft biomechanics using sutures from the suture anchors. The sutures were required to be the most taut in full extension of the knee and loosen with knee flexion. If this did not occur, the guide pin was repositioned accordingly. The graft was then docked into an appropriately sized tunnel at the femoral attachment and fixed using a biocomposite screw (Genesys Matrix; ConMed Linvatec or BioSure; Smith & Nephew).
Postoperative rehabilitation included early weightbearing as tolerated, with crutches used to facilitate a normal gait pattern. A short period of immobilization in a range of motion knee brace (up to 48 hours postoperative) was followed by unrestricted range of motion of the knee. The phase-based rehabilitation protocol emphasized quadriceps activation, including the use of electrical muscle stimulation and functional exercises. In cases where a tibial tubercle osteotomy (TTO) was performed in conjunction with the MPFL reconstruction, knee range of motion was initiated at 2 weeks postoperatively.
Lateral radiographs were taken postoperatively and were measured to determine the accuracy of the femoral tunnel in relation to the Schöttle point. Radiographs were determined to be adequate by evaluating the overlap of the medial and lateral condyles on the true lateral view. Rotation in any direction of less than 7 mm was considered acceptable.3 The femoral tunnel had to be readily identified on the lateral radiograph to be considered for the study. Radiographs were evaluated using IMPAX Software (Agfa Healthcare). The posterior border of the cortex of the femur was marked (line 1). The superior border of the notch was marked perpendicular to line 1 (line 2). The superior border of the femoral condyle was marked parallel to line 2 (line 3). The anterior to posterior width of the femur was measured at line 2. The Schöttle point was then marked 1.3 mm anterior to line 1, halfway between lines 2 and 3. The center of the femoral tunnel (T) from the MPFL reconstruction was then marked. The distance from the center of the femoral tunnel to the Schöttle point (A) was then determined (A-T distance) (Figure 1). Rating categories and criteria for tunnel position were standardized and defined a priori as ideal (0-6 mm), good (>6-12 mm), or poor (>12 mm). An ideal or good femoral tunnel position was considered accurate.
Figure 1.
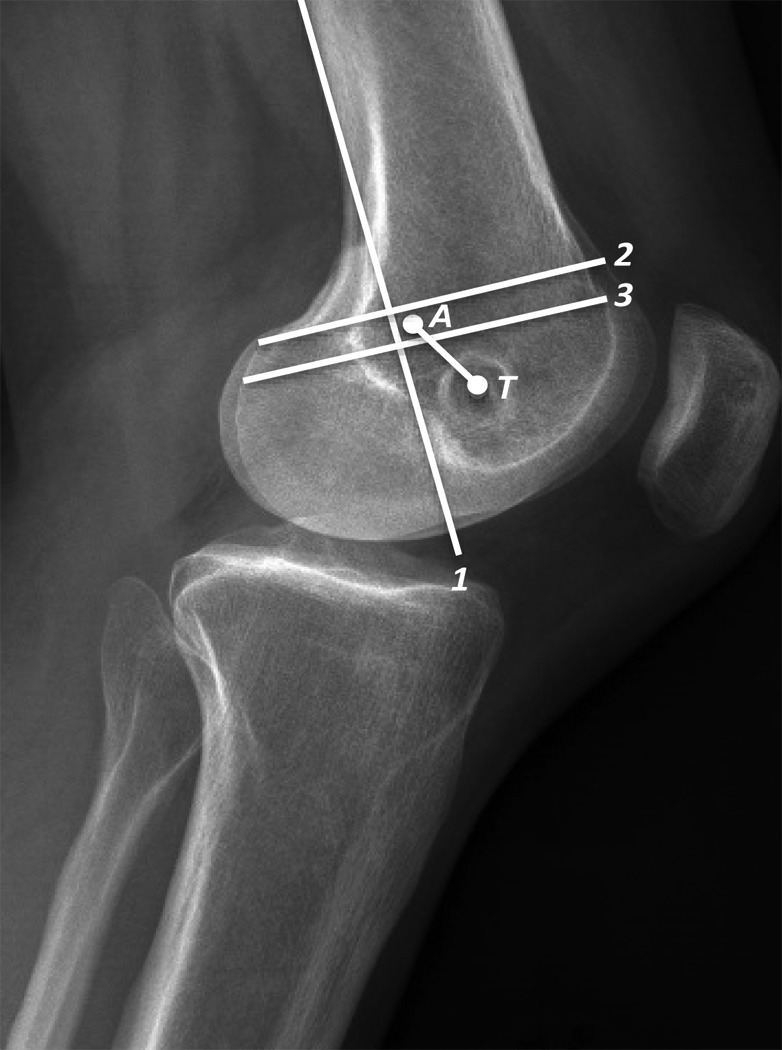
Identification of the femoral tunnel. Line 1, posterior border of the cortex of the femur; line 2, superior border of the notch, perpendicular to line 1; line 3, superior border of the femoral condyle, parallel to line 2; T, center of the femoral tunnel. The Schöttle point (A) is centered 1.3 mm anterior to line 1 and midway between lines 2 and 3.
To ensure the A-T measure was reliable, an intraclass correlation coefficient, ICC(2,k), was employed to assess interrater reliability. For the first 73 subjects, 2 orthopaedic surgeons measured the A-T distance on each radiograph blinded to each other and to each patient’s identity. The ICC(2,k) was chosen since the raters were considered random and it is intended for the results of this research to be generalizable to a wider population. The ICC was assessed as 0.89 and confirmed the interrater reliability of this method of measurement. The anterior to posterior diameter of the distal femoral condyles was measured to normalize the A-T distance (Schöttle point to femoral tunnel) to femur size. To normalize the tunnel position, the A-T distance was divided by the anterior to posterior diameter of the femoral condyle (mm).
The BPII was completed by patients preoperatively and at the 1- and 2-year follow-up visits, as well as at any subsequent appointments. Demographic information was collected, including age at time of surgery, sex, body mass index, side of surgery, and whether the patient had unilateral or bilateral patellofemoral instability.
Statistical Considerations
The pre- and postoperative BPII scores were compared using a paired t test to evaluate the responsiveness of the BPII as well as the effectiveness of the surgical intervention. A Pearson r correlation coefficient (95% CI) was calculated to assess the relationship between the femoral tunnel position and the quality-of-life measure (BPII). In addition, Pearson r correlation was calculated for the femoral tunnel rating category (ideal, good, poor) to the BPII score. A Pearson r correlation coefficient was also calculated using the value of the A-T distance normalized to the size of the femur. All data were analyzed using SPSS version 22 (IBM Corp).
Results
Of the 206 patients who underwent MPFL reconstruction procedures, 11 were excluded from the cohort. Seven of these patients had subsequent significant procedures within 2 years such as a femoral or tibial osteotomy or fresh osteochondral transplant of the patella, 1 patient had no femoral tunnel as the procedure was performed with open physes and therefore a different surgical technique was employed, 2 patients were excluded due to significant psychiatric or chronic pain issues, and 1 patient was excluded due to a workers’ compensation claim. The remaining cohort of 195 patients was evaluated. Six patients (3.1%) were lost to follow-up and had no postoperative imaging and no BPII score. Thirty-four patients (17.4%) had partial data: 15 with no adequate postoperative imaging and 19 with no complete BPII score. Therefore 155 (79.5%) patients were included in the correlation, with adequate tunnel position radiographs and complete BPII scores a minimum of 1 year postoperatively. Due to surgical timing in relation to publication of the BPII, 133 patients had both pre- and postoperative BPII scores for t test comparison.
There were 36 male and 119 female patients. The mean (±SD) duration of follow-up was 24.4 ± 8.2 months (range, 12-74 months), with 148 patients completing follow-up to at least 2 years. There were 62 right knees and 93 left knees. The mean patient age was 25.4 ± 8.9 years (range, 13.4-50.4 years), with a mean body mass index of 23.8 ± 3.7 kg/m2 (range, 16-38 kg/m2). At the time of final assessment, 90 patients had unilateral patellofemoral instability, and 65 patients had bilateral instability. High-grade trochlear dysplasia was present in 73 patients, low-grade trochlear dysplasia was present in 58 patients, and 24 patients had no evidence of trochlear dysplasia. Patella alta, measured as a Caton-Deschamps ratio ≥1.3, was positive in 21 patients. Femoral anteversion was present in 34 patients. A tibial tubercle–trochlear groove (TT-TG) distance of ≥15 mm was present in 51 patients, with 23 patients demonstrating a TT-TG of ≥20 mm. A TTO to correct alignment was performed in 36 of 155 surgeries.
Measurement from the center of the femoral tunnel to the center of the Schöttle point resulted in 143 (92.3%) tunnels being categorized as “ideal” or “good.” The mean A-T distance for the cohort was 5.9 ± 4.1 mm (range, 0.5-25.9 mm) from the center of the MPFL tunnel to the center of the Schöttle point. The mean preoperative BPII score was 23.1 ± 12.6 (range, 0.72-86.8; n = 132), and the mean postoperative BPII score was 65.2 ± 22.5 (range, 9.2-100; n = 155). For the 34 cases with partial data, the 19 patients with adequate radiographs but no BPII score demonstrated a mean A-T distance of 5.8 mm, and the 15 patients with no adequate postoperative imaging demonstrated a mean BPII score of 70.8. The mean BPII score was 61.8 ± 23.6 (range, 9.2-100; n = 102) for the tunnels categorized as “ideal,” 63.4 ± 21.4 (range, 26.3-98.9; n = 40) for tunnels categorized as “good,” and 62.1 ± 17.2 (range, 33.1-92.1; n = 13) for tunnels categorized as “poor.” There was a significant difference between the preoperative (mean ± SD, 23.5 ± 12.5) and postoperative (65.2 ± 22.5) BPII scores, t(131) = 19.7, P < .001. The effect size of this difference (r = 0.86) was classified as large.
High-grade trochlear dysplasia was present in 48 of 102 (47%) patients with ideal tunnels, 19 of 40 (48%) patients with good tunnels, and 6 of 13 (46%) patients with poor tunnels. In the group assessed as having ideal tunnels, 27 of 102 (26.5%) patients had a TTO performed in addition to their MPFL reconstruction. A TTO was performed in 7 of 40 (17.5%) patients in the good tunnel group and 2 of 13 (15.4%) patients in the poor tunnel group.
Pearson r correlation demonstrated no statistically significant relationship between accuracy of tunnel position (A-T distance) and BPII score (r = –0.08; 95% CI, –0.24 to 0.08). The Pearson r correlation coefficient between the BPII score and tunnel category (ideal, good, or poor) was also not significant (r = 0.02; 95% CI, –0.14 to 0.18). The Pearson r correlation demonstrated no significant correlation between the normalized femoral tunnel position based on femoral diameter and the A-T distance (femoral tunnel accuracy) (r = –0.08; 95% CI, –0.24 to 0.08).
There were 8 failures in the cohort (4.1%). Four failures occurred in patients with an ideal tunnel position and 4 occurred in patients with good tunnel position. The mean A-T distance for the failed MPFL reconstructions was 5.4 mm (range, 1.6-9.3 mm).
Discussion
In this patient cohort, accurate femoral tunnels were placed greater than 92% of the time in relation to the Schöttle point during MPFL reconstruction. The assessment of tunnel position on the lateral radiographs demonstrated a very high level of interrater reliability. There was no difference in mean postoperative BPII scores for ideal, good, and poor tunnels. There was no evidence of a correlation between the accuracy of the femoral tunnel in relation to the Schöttle point and the disease-specific quality-of-life score. The failures in this cohort were not related to the femoral tunnel position.
A number of studies have assessed MPFL reconstruction femoral tunnel position and have reported mixed results with respect to clinical outcomes. Servien et al34 were the first to analyze femoral tunnel position after MPFL reconstruction. This study assessed 29 patients using plain radiography and magnetic resonance imaging as well as clinical results, including the subjective International Knee Documentation Committee (IKDC) score, knee range of motion, apprehension test, and joint hypermobility. These authors found no correlation between the femoral tunnel position and the subjective IKDC score or range of motion. As noted by these authors, this study comprised a small cohort, making it difficult to draw concrete conclusions between MPFL tunnel accuracy and outcomes. Some more recent studies have reported an association between inaccurate femoral tunnel placement and outcomes after surgery.16,20 In addition, 2 case series publications have described complications after MPFL reconstruction and ascribed these to poor femoral tunnel position.24,26 Unfortunately, all these studies contained a limited number of patients, which limits the ability to draw robust conclusions regarding the influence of tunnel position on patient-reported outcome.
Multiple biomechanical studies have demonstrated that the femoral tunnel position for MPFL reconstruction is the most important factor that affects the isometric behavior of the ligament.# Given the detrimental effect that poor tunnel position has on patellofemoral force production in the laboratory, the lack of clinical studies corroborating these findings is concerning. The inability of clinical studies to confirm the results of biomechanical studies may be due to small sample sizes in both fields of literature. In addition, the published clinical studies have a relatively short duration of follow-up, and poor femoral tunnel position may have a greater effect on longer term outcomes. If excessive patellofemoral forces occur as a result of poor tunnel position, then it may require longer follow-up to demonstrate the sequelae of this overload. If cartilage overload is the result of poor tunnel position, it could take many years for the clinical repercussions to develop sufficiently to be measurable.
Another reason that clinical study outcomes may not align with biomechanical studies is because the primary outcome measure used may not be sufficiently robust or sensitive to detect a clinically important change. Multiple studies have been conducted to ascertain the clinical outcomes after MPFL reconstruction for patellofemoral instability.8,9,17,21,37 These studies were performed prior to the development of any disease-specific outcome measure designed for patellofemoral instability. The majority of these studies utilize the Kujala, IKDC, or Lysholm score as the outcome, and none of these measures have been extensively assessed for clinimetric and psychometric soundness in patients with patellofemoral instability.36 The current study is the first to utilize a disease-specific patient-reported outcome measure to assess the influence of femoral tunnel position after MPFL reconstruction. As a quality-of-life measure, the BPII assesses a broad range of constructs including symptoms and physical complaints, work-related concerns, recreation- and sport-related concerns, lifestyle concerns, and social and emotional concerns. By including these domains, the BPII is designed to capture a more holistic view of the quality of life of patients with patellofemoral instability. The significant improvement in BPII score from pre- to postoperative in this cohort also indicates the responsiveness to change of this outcome measure. The BPII has demonstrated validity, reliability, and responsiveness to change, providing a patient-reported outcome measure that can be used for correlation to clinical and functional outcomes in this challenging patient population.12,13,19
Variability in measuring the ideal femoral tunnel position radiologically may be a reason that the literature has been unable to demonstrate a relationship between femoral tunnel position and clinical outcomes. The Schöttle point is the most frequently employed reference standard for femoral tunnel position in MPFL reconstruction. The study by Schöttle et al33 was performed on 8 normal knees and therefore may not reflect the anatomic insertion point of the MPFL in knees with a dysplastic distal femur. This concept is consistent with recent research demonstrating that the Schöttle point did not correlate with the anatomic insertion of the MPFL in dysplastic femurs relative to the adductor tubercle.32 Despite the widespread use of the Schöttle point, the radiographic parameters for the anatomic insertion points of the MPFL have not been entirely consistent in the literature. Although the work by Schöttle et al33 is widely quoted, other studies have shown there may be more variability in the radiographic insertion point of the MPFL.3,6,30,48
The current study attempted to mitigate the challenges of assessing femoral tunnel position by assessing interrater reliability of the femoral tunnel accuracy measurement technique and by also using normalization of femur size as an alternate method to assess the relationship between tunnel accuracy and outcomes. Normalization was performed to adjust for the fact that a tunnel that is 10 mm from the Schöttle point in a large femur may have less influence on patient-reported outcomes than the same distance in a small femur. This calculation did not yield any significant correlation between femoral tunnel accuracy and patient-reported quality of life.
Limitations of this study include the relatively short follow-up time, with a mean of 24.4 months postoperative. Based on this follow-up timeline, all sequelae secondary to femoral tunnel positioning may not yet be evident in terms of affecting disease-specific outcome scores, and further long-term follow-up of this patient cohort will be required. This consecutive cohort of patients is a convenience sample of patients with patellofemoral instability that presented to a tertiary orthopaedic sports medicine clinic. Therefore, the sample may not represent the entire spectrum of patients with this disorder. The lack of objective outcome measures in this population could be considered a limitation; however, given the paucity of information on the natural history of poor tunnel position after MPFL reconstruction, selecting an appropriate measure is difficult.
The currently accepted gold standard of the Schöttle point may not represent a true gold standard for the ideal tunnel position for MPFL reconstruction. It remains, however, the most widely used and reproducible radiographic landmark, and therefore, it was adopted as the most appropriate reference standard for this study. The use of lateral radiographs may also be considered a limitation of this study, especially given recent criticism of the use of radiologic measures due to their inherent risk of error.50 Although 3-dimensional imaging may provide a more accurate measure of the exact location of the femoral tunnel, this was not a feasible test on this large clinical cohort, and valid and reliable measurement methods have not been reported. The low number of poor tunnels assessed in the cohort may influence the statistical power of this group’s correlation to the BPII. However, it should also be noted that no graft failures occurred in the group of patients with poor tunnels. Finally, the heterogeneity of this cohort with respect to the different pathoanatomies could be considered a limitation. However, the surgical correction of significant pathoanatomies using an à la carte approach attempts to create homogeneity in this complex population by correcting anatomic or biomechanical pathologies.5 The entire cohort was treated according to presenting pathologies, and the placement of the femoral tunnel was independent of these comorbidities. Patients with patellofemoral instability are a diverse group. Given the paucity of information on the contribution of pathoanatomic risk factors on the results of MPFL reconstruction, the analysis of the entire patient cohort was a logical initial step to identify patterns with respect to outcomes.
This study represents a large patellofemoral instability cohort with assessment of femoral tunnel accuracy and clinical outcomes after MPFL reconstruction. The study analysis did not identify an association between femoral tunnel position and patient-reported quality-of-life outcome. The study was methodologically sound and has reported confidence intervals or effect size in the statistical analysis, and therefore, the influence of sample size on the results. This is also the only study to use a disease-specific, patient-reported quality-of-life measure to assess clinical outcome. This study also included a range of tunnel position placements and a strong degree of follow-up to allow for accurate correlation assessment.
Conclusion
In this study, there was no evidence of a correlation between the accuracy of the MPFL reconstruction femoral tunnel in relation to the Schöttle point and disease-specific quality-of-life scores. Graft failure was not related to femoral tunnel placement. The patellofemoral instability population is complex, and patients present with multiple risk factors that, in addition to the accuracy of femoral tunnel position, contribute to quality of life and warrant further investigation.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: L.A.H. has completed educational consulting teaching for ConMed Linvatec.
Ethical approval for this study was obtained from the Conjoint Health Research Ethics Board of the Faculties of Medicine, Nursing, and Kinesiology, University of Calgary, Calgary, Alberta, Canada.
References
- 1. Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10:215–220. [DOI] [PubMed] [Google Scholar]
- 2. Balcarek P, Walde TA. Accuracy of femoral tunnel placement in medial patellofemoral ligament reconstruction: the effect of a nearly true-lateral fluoroscopic view. Am J Sports Med. 2015;43:2228–2232. [DOI] [PubMed] [Google Scholar]
- 3. Barnett AJ, Howells NR, Burston BJ, Ansari A, Clark D, Eldridge JD. Radiographic landmarks for tunnel placement in reconstruction of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2012;20:2380–2384. [DOI] [PubMed] [Google Scholar]
- 4. Bicos J, Fulkerson JP, Amis A. Current concepts review: the medial patellofemoral ligament. Am J Sports Med. 2007;35:484–492. [DOI] [PubMed] [Google Scholar]
- 5. Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc. 2007;15:39–46. [DOI] [PubMed] [Google Scholar]
- 6. Dirim B, Haghighi P, Trudell D, Portes G, Resnick D. Medial patellofemoral ligament: cadaveric investigation of anatomy with MRI, MR arthrography, and histologic correlation. AJR Am J Roentgenol. 2008;191:490–498. [DOI] [PubMed] [Google Scholar]
- 7. Elias JJ, Cosgarea AJ. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med. 2006;34:1478–1485. [DOI] [PubMed] [Google Scholar]
- 8. Enderlein D, Nielsen T, Christiansen SE, Fauno P, Lind M. Clinical outcome after reconstruction of the medial patellofemoral ligament in patients with recurrent patella instability. Knee Surg Sports Traumatol Arthrosc. 2014;22:2458–2464. [DOI] [PubMed] [Google Scholar]
- 9. Feller JA, Richmond AK, Wasiak J. Medial patellofemoral ligament reconstruction as an isolated or combined procedure for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22:2470–2476. [DOI] [PubMed] [Google Scholar]
- 10. Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32:1114–1121. [DOI] [PubMed] [Google Scholar]
- 11. Herschel R, Hasler A, Tscholl PM, Fucentese SF. Visual-palpatory versus fluoroscopic intraoperative determination of the femoral entry point in medial patellofemoral ligament reconstruction [published online March 12, 2016]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-016-4057-6. [DOI] [PubMed] [Google Scholar]
- 12. Hiemstra LA, Kerslake S, Lafave M, Mohtadi NG. Concurrent validation of the Banff Patella Instability Instrument to the Norwich Patellar Instability Score and the Kujala Score in patients with patellofemoral instability. Orthop J Sports Med. 2016;4:2325967116646085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hiemstra LA, Kerslake S, Lafave MR, Heard SM, Buchko GM, Mohtadi NG. Initial validity and reliability of the Banff Patella Instability Instrument. Am J Sports Med. 2013;41:1629–1635. [DOI] [PubMed] [Google Scholar]
- 14. Hiemstra LA, Lafave M, Buchko G, Heard M. Banff Patellar Instability Instrument—responsiveness to change at 24 months post patellar stabilization. Knee Surg Sports Traumatol Arthrosc. 2014;22(suppl 1):S54–S55. [Google Scholar]
- 15. Higuchi T, Arai Y, Takamiya H, Miyamoto T, Tokunaga D, Kubo T. An analysis of the medial patellofemoral ligament length change pattern using open-MRI. Knee Surg Sports Traumatol Arthrosc. 2010;18:1470–1475. [DOI] [PubMed] [Google Scholar]
- 16. Hopper GP, Leach WJ, Rooney BP, Walker CR, Blyth MJ. Does degree of trochlear dysplasia and position of femoral tunnel influence outcome after medial patellofemoral ligament reconstruction? Am J Sports Med. 2014;42:716–722. [DOI] [PubMed] [Google Scholar]
- 17. Howells NR, Barnett AJ, Ahearn N, Ansari A, Eldridge JD. Medial patellofemoral ligament reconstruction. J Bone Joint Surg Br. 2012;94:1202–1208. [DOI] [PubMed] [Google Scholar]
- 18. Jaecker V, Brozat B, Banerjee M, Otchwemah R, Bouillon B, Shafizadeh S. Fluoroscopic control allows for precise tunnel positioning in MPFL reconstruction [published online May 10, 2015]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3613-9. [DOI] [PubMed] [Google Scholar]
- 19. Lafave MR, Hiemstra L, Kerslake S. Factor analysis and item reduction of the Banff Patella Instability Instrument (BPII): introduction of BPII 2.0. Am J Sports Med. 2016;44:2081–2086. [DOI] [PubMed] [Google Scholar]
- 20. Larson E, Edwards A, Albright J. Functional outcomes of MPFL reconstruction vs. graft tissue placement. Iowa Orthop J. 2014;34:38–43. [PMC free article] [PubMed] [Google Scholar]
- 21. Lippacher S, Dreyhaupt J, Williams SR, Reichel H, Nelitz M. Reconstruction of the medial patellofemoral ligament: clinical outcomes and return to sports. Am J Sports Med. 2014;42:1661–1668. [DOI] [PubMed] [Google Scholar]
- 22. McCarthy M, Ridley TJ, Bollier M, Wolf B, Albright J, Amendola A. Femoral tunnel placement in medial patellofemoral ligament reconstruction. Iowa Orthop J. 2013;33:58–63. [PMC free article] [PubMed] [Google Scholar]
- 23. Mehta VM, Inoue M, Nomura E, Fithian DC. An algorithm guiding the evaluation and treatment of acute primary patellar dislocations. Sports Med Arthrosc. 2007;15:78–81. [DOI] [PubMed] [Google Scholar]
- 24. Nelitz M, Theile M, Dornacher D, Wolfle J, Reichel H, Lippacher S. Analysis of failed surgery for patellar instability in children with open growth plates. Knee Surg Sports Traumatol Arthrosc. 2012;20:822–828. [DOI] [PubMed] [Google Scholar]
- 25. Nomura E, Inoue M. Second-look arthroscopy of cartilage changes of the patellofemoral joint, especially the patella, following acute and recurrent patellar dislocation. Osteoarthritis Cartilage. 2005;13:1029–1036. [DOI] [PubMed] [Google Scholar]
- 26. Parikh SN, Nathan ST, Wall EJ, Eismann EA. Complications of medial patellofemoral ligament reconstruction in young patients. Am J Sports Med. 2013;41:1030–1038. [DOI] [PubMed] [Google Scholar]
- 27. Philippot R, Chouteau J, Wegrzyn J, Testa R, Fessy MH, Moyen B. Medial patellofemoral ligament anatomy: implications for its surgical reconstruction. Knee Surg Sports Traumatol Arthrosc. 2009;17:475–479. [DOI] [PubMed] [Google Scholar]
- 28. Rammohan R, Kotwal RS, Chandratreya A. Intraoperative localisation of schottle’s point without fluoroscopy during medial patellofemoral ligament reconstruction. Ann R Coll Surg Engl. 2016;98:288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Reagan J, Kullar R, Burks R. MPFL reconstruction: technique and results. Clin Sports Med. 2014;33:501–516. [DOI] [PubMed] [Google Scholar]
- 30. Redfern J, Kamath G, Burks R. Anatomical confirmation of the use of radiographic landmarks in medial patellofemoral ligament reconstruction. Am J Sports Med. 2010;38:293–297. [DOI] [PubMed] [Google Scholar]
- 31. Rood A, Hannink G, Lenting A, et al. Patellofemoral pressure changes after static and dynamic medial patellofemoral ligament reconstructions. Am J Sports Med. 2015;43:2538–2544. [DOI] [PubMed] [Google Scholar]
- 32. Sanchis-Alfonso V, Ramirez-Fuentes C, Montesinos-Berry E, Aparisi-Rodriguez F, Marti-Bonmati L. Does radiographic location ensure precise anatomic location of the femoral fixation site in medial patellofemoral ligament surgery? Knee Surg Sports Traumatol Arthrosc. 2016;24:2838–2844. [DOI] [PubMed] [Google Scholar]
- 33. Schöttle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:801–804. [DOI] [PubMed] [Google Scholar]
- 34. Servien E, Fritsch B, Lustig S, et al. In vivo positioning analysis of medial patellofemoral ligament reconstruction. Am J Sports Med. 2011;39:134–139. [DOI] [PubMed] [Google Scholar]
- 35. Smirk C, Morris H. The anatomy and reconstruction of the medial patellofemoral ligament. Knee. 2003;10:221–227. [DOI] [PubMed] [Google Scholar]
- 36. Smith TO, Davies L, O’Driscoll ML, Donell ST. An evaluation of the clinical tests and outcome measures used to assess patellar instability. Knee. 2008;15:255–262. [DOI] [PubMed] [Google Scholar]
- 37. Smith TO, Walker J, Russell N. Outcomes of medial patellofemoral ligament reconstruction for patellar instability: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2007;15:1301–1314. [DOI] [PubMed] [Google Scholar]
- 38. Steensen RN, Dopirak RM, McDonald WG., 3rd The anatomy and isometry of the medial patellofemoral ligament: implications for reconstruction. Am J Sports Med. 2004;32:1509–1513. [DOI] [PubMed] [Google Scholar]
- 39. Stephen JM, Kaider D, Lumpaopong P, Deehan DJ, Amis AA. The effect of femoral tunnel position and graft tension on patellar contact mechanics and kinematics after medial patellofemoral ligament reconstruction. Am J Sports Med. 2014;42:364–372. [DOI] [PubMed] [Google Scholar]
- 40. Stephen JM, Kittl C, Williams A, et al. Effect of medial patellofemoral ligament reconstruction method on patellofemoral contact pressures and kinematics. Am J Sports Med. 2016;44:1186–1194. [DOI] [PubMed] [Google Scholar]
- 41. Stephen JM, Lumpaopong P, Deehan DJ, Kader D, Amis AA. The medial patellofemoral ligament: location of femoral attachment and length change patterns resulting from anatomic and nonanatomic attachments. Am J Sports Med. 2012;40:1871–1879. [DOI] [PubMed] [Google Scholar]
- 42. Stupay KL, Swart E, Shubin Stein BE. Widespread implementation of medial patellofemoral ligament reconstruction for recurrent patellar instability maintains functional outcomes at midterm to long-term follow-up while decreasing complication rates: a systematic review. Arthroscopy. 2015;31:1372–1380. [DOI] [PubMed] [Google Scholar]
- 43. Tanaka MJ, Bollier MJ, Andrish JT, Fulkerson JP, Cosgarea AJ. Complications of medial patellofemoral ligament reconstruction: common technical errors and factors for success: AAOS exhibit selection. J Bone Joint Surg Am. 2012;94:e87. [DOI] [PubMed] [Google Scholar]
- 44. Tateishi T, Tsuchiya M, Motosugi N, et al. Graft length change and radiographic assessment of femoral drill hole position for medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:400–407. [DOI] [PubMed] [Google Scholar]
- 45. Thaunat M, Erasmus PJ. Management of overtight medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2009;17:480–483. [DOI] [PubMed] [Google Scholar]
- 46. Tischer T, Geier A, Lenz R, Woernle C, Bader R. Impact of the patella height on the strain pattern of the medial patellofemoral ligament after reconstruction: a computer model-based study [published online June 11, 2016]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-016-4190-2. [DOI] [PubMed] [Google Scholar]
- 47. Triantafillopoulos IK, Panagopoulos A, van Niekerk L. Isometric behavior of the reconstructed medial patellofemoral ligament using two different femoral pulleys: a cadaveric study. Med Sci Monit. 2007;13:BR181–BR187. [PubMed] [Google Scholar]
- 48. Wijdicks CA, Griffith CJ, LaPrade RF, et al. Radiographic identification of the primary medial knee structures. J Bone Joint Surg Am. 2009;91:521–529. [DOI] [PubMed] [Google Scholar]
- 49. Zaffagnini S, Colle F, Lopomo N, et al. The influence of medial patellofemoral ligament on patellofemoral joint kinematics and patellar stability. Knee Surg Sports Traumatol Arthrosc. 2013;21:2164–2171. [DOI] [PubMed] [Google Scholar]
- 50. Ziegler CG, Fulkerson JP, Edgar C. Radiographic reference points are inaccurate with and without a true lateral radiograph: the importance of anatomy in medial patellofemoral ligament reconstruction. Am J Sports Med. 2016;44:133–142. [DOI] [PubMed] [Google Scholar]


