Abstract
Background
Self-injurious behaviors (SIBs) are devastating traits in autism spectrum disorder (ASD). Although deficits in pain sensation might be one of the contributing factors underlying the development of SIBs, the mechanisms have yet to be addressed. Recently, the Shank2 synaptic protein has been considered to be a key component in ASD, and mutations of SHANK2 gene induce the dysfunction of N-methyl-D-aspartate (NMDA) receptors, suggesting a link between Shank2 and NMDA receptors in ASD. Given that spinal NMDA receptors play a pivotal role in pain hypersensitivity, we investigated the possible role of Shank2 in nociceptive hypersensitivity by examining changes in spontaneous pain following intrathecal NMDA injection in Shank2−/− (Shank2 knock-out, KO) mice.
Results
Intrathecal NMDA injection evoked spontaneous nociceptive behaviors. These NMDA-induced nociceptive responses were significantly reduced in Shank2 KO mice. We also observed a significant decrease of NMDA currents in the spinal dorsal horn of Shank2 KO mice. Subsequently, we examined whether mitogen-activated protein kinase or AKT signaling is involved in this reduced pain behavior in Shank2 KO mice because the NMDA receptor is closely related to these signaling molecules. Western blotting and immunohistochemistry revealed that spinally administered NMDA increased the expression of a phosphorylated form of extracellular signal-regulated kinase (p-ERK) which was significantly reduced in Shank2 KO mice. However, p38, JNK, or AKT were not changed by NMDA administration. The ERK inhibitor, PD98059, decreased NMDA-induced spontaneous pain behaviors in a dose-dependent manner in wild-type mice. Moreover, it was found that the NMDA-induced increase in p-ERK was primarily colocalized with Shank2 proteins in the spinal cord dorsal horn.
Conclusion
Shank2 protein is involved in spinal NMDA receptor-mediated pain, and mutations of Shank2 may suppress NMDA-ERK signaling in spinal pain transmission. This study provides new clues into the mechanisms underlying pain deficits associated with SIB and deserves further study in patients with ASD.
Keywords: Shank2, N-methyl-D-aspartate receptor, pain, spinal cord, extracellular signal-regulated kinase
Background
Autism Spectrum Disorder (ASD) has drawn much attention from researchers, clinicians, and the general population during the past several decades. ASD is a group of conditions that shares common characteristics including a deficit in social interaction and communication, and repetitive behavior.1 Self-injurious behaviors (SIBs) are a key area of concern in patients with ASD.2 These SIBs include head banging, self-biting, or excessive self-rubbing that may cause physical harm, thus requiring immediate intervention in order to avoid injury. Sensory abnormality is an important feature of ASD, and in particular, ASD individuals experience pain in unusual ways, which appears to contribute to SIBs.3 Thus, it is important to investigate the mechanisms of decreased pain sensitivity in ASD patients.
Several lines of evidence suggest that the etiology of ASD may be linked to a genetic cause.4,5 Among the many genetic factors, the SHANK2 gene has been identified as an important causative candidate of ASD.6 Shank proteins, encoded by the three genes SHANK1, SHANK2, and SHANK3, are master scaffolding proteins highly enriched in the post-synaptic density (PSD) of the excitatory synapse.7 They form a mesh-like polymer matrix structure that is required for the structural integrity of dendritic spines, are essential for synaptic development, and function as central organizers.8 It has been reported that mutations in the SHANK genes cause autism-like phenotypes in human and mice providing strong support for the hypothesis that Shank proteins are associated with ASD.6,9,10 Recently, Shank2-mutant (Shank2−/−) transgenic mice carrying a mutation identical to the microdeletion (exons 6 and 7 deletions and a frame shift) in the SHANK2 gene of ASD patients have been shown to display autistic-like behaviors.11 Moreover, these transgenic Shank2−/− mice have decreased nociceptive sensitivity under normal as well as chronic pain conditions,12 leading us to hypothesize that the SHANK2 gene is associated with the deficits in pain sensation in ASD individuals that may underlie SIBs. However, the exact molecular mechanisms involved remain to be elucidated.
N-methyl-D-aspartate (NMDA) receptors in the spinal cord play a key role in the generation and maintenance of central sensitization during pain states.13 Therefore, dysfunction of spinal NMDA receptors can cause deficits in pain responses.14 It has been reported that NMDA receptors directly or indirectly bind to Shank proteins located at synapses in the central nervous system.15 Moreover, a study using Shank2 knock-out (KO) mice showed that NMDA receptor-mediated excitatory currents were significantly altered at hippocampal synapses.11,16 Based on these studies, we hypothesized that Shank2 mutations would affect pain sensation via dysfunction of spinal NMDA receptor-mediated synaptic transmission.
This study was designed to test this hypothesis using the followings experimental paradigm. First, behavioral tests were performed to determine the effects of a Shank2 mutation on NMDA-induced spontaneous nociceptive behaviors. Then, the downstream mechanisms underlying these Shank2/NMDA receptor interaction in the spinal cord were determined by investigating the possible involvement of the mitogen-activated protein kinase (MAPK) family and the serine/threonine-specific protein kinase (AKT) signaling pathway.
Materials and methods
Animals
Mice had a C57BL/6J genetic background. Female adult (10 weeks old) or juvenile (3.5 to 4 weeks old, Supplementary Figure 1) Shank2 KO (−/−) and Shank2 wild-type (+/+, WT) littermate mice were obtained by mating the parental strains female Shank2+/− and male Shank2+/−. Control C57BL/6J mice (female, 10 weeks old) for Figure 1(a) were obtained from Daehan Biolink (Eumseong, Korea). They were housed in colony cages with free access to food and water and maintained in temperature- and light-controlled rooms (22 ± 2℃, 12/12-h light/dark cycle with lights on at 08:00). All procedures for animal use were reviewed and approved by the Institutional Animal Care and Use Committee of the School of Dentistry, Seoul National University prior to the experiments and conform to NIH guidelines (NIH publication No. 86-23, revised 1985). All algesiometric assays were conducted in accordance with the ethical guidelines established by the International Association for the Study of Pain.
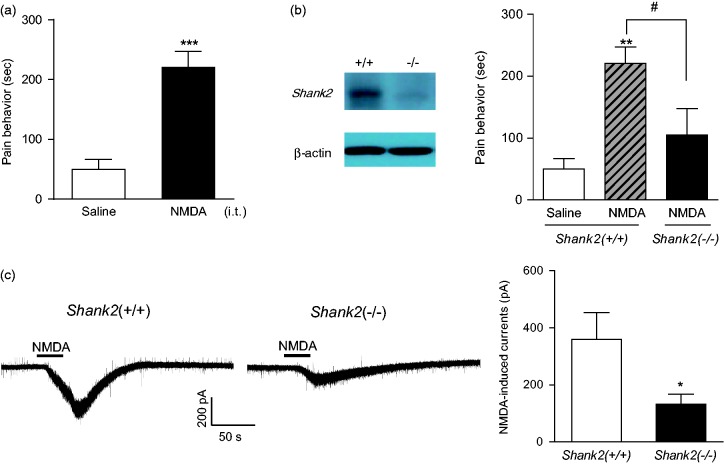
Figure 1.
Graph illustrating the effect of genetic depletion of Shank2 on i.t. NMDA-induced spontaneous pain responses. (a) NMDA-treated mice showed significant spontaneous nociceptive behaviors compared to saline-treated mice. ***p < 0.001: significantly different from the value of the saline-treated group (b) Representative Western blot image showing that Shank2 proteins are not detected in Shank2 KO (Shank2−/−) mice compared with WT (Shank2+/+). A bar graph demonstrating that NMDA-induced nociceptive behaviors are significantly reduced in Shank2 KO compared than WT mice. **p < 0.01: significantly different from the value of the saline-treated group. #p < 0.05: for the groups connected by a straight line. n = 7–8 mice per group. (c) Traces of NMDA (50 μM)-induced currents in the spinal cord lamina II neurons from WT (Shank2 +/+) and Shank2 KO (Shank2 −/−) mice. Right, amplitude of NMDA currents in the spinal cord lamina II neurons. *p < 0.05, unpaired Student’s t-test, n = 7–8 neurons per group.
Intrathecal drug administration
Drugs were dissolved in 5 µl of the vehicle. Intrathecal injections were made into the L5–L6 intervertebral space of unanaesthetized mice using a 50 -µl Hamilton syringe connected to a 30-gauge needle as previously described by Hylden and Wilcox.17 The flick of the tail was considered as an indicator of a successful i.t. administration.
NMDA-induced nociceptive behavior
Each mouse was acclimated to an acrylic observation chamber for at least 30 min before this experiment. NMDA (0.4 nmol in 5 μl sterile saline) was injected intrathecally in order to produce spinally mediated NMDA-induced pain-like nociceptive behaviors including biting, scratching, and licking behavior at the hind limb, gluteal region, and base of the tail.18 Following injection, animals were immediately placed in an observation chamber, and nociceptive behaviors were recorded for a 10-min period. The cumulative response time (s) of these behaviors was measured. To evaluate a possible role of extracellular signal-regulated kinase (ERK) or p38 signaling in NMDA-induced nociception, PD98059 (0, 10, or 30 nmol; Tocris, Bristol, UK) or SB203580 (0, 3, 10 nmol; Sigma, St. Louis, MO, USA) was intrathecally injected 10 min prior to NMDA injection, respectively. During the tests, the behavioral investigators were blind to both mouse genotype and drug treatment. The doses of drugs were selected based on previously published work.19–22 At the termination of the NMDA test, the mice were deeply anaesthetized with 3% isoflurane and euthanized by decapitation (for Western blot analysis) or transcardial perfusion (for immunohistochemistry studies).
Western blot study
Spinal cord samples were collected from saline or NMDA-treated mice. The spinal dorsal horns from spinal cord segments L3 to 6 were dissected and quickly frozen in liquid nitrogen and stored at −80℃ until processed. Spinal cord tissues were homogenized by sonication in RIPA lysis buffer (50 mM Tris-HCl pH 7.4, 1% NP-40, 0.25% Na− deoxycholate, 150 mM NaCl, 1 mM EDTA) containing protease and phosphatase inhibitor cocktails (Sigma, St. Louis, MO, USA). The sonicated dorsal horn tissue was incubated at 4℃ for 1 h on a rotator and centrifuged for 15 min at 15,000 rotations per minute at 4℃. The protein concentration of the resulting supernatant was determined using a Lowry protein assay (Bio-Rad, Hercules, CA, USA). Protein samples (30 µg) were heated to 95℃ for 5 min, separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis, and transferred to a polyvinylidene fluoride membrane using a Transblot SD apparatus (Bio-Rad). After the blots had been washed with tris-buffered saline containing Tween-20 (TBST, 10 mM Tris-HCl (pH 7.6), 150 mM NaCl, 0.05% Tween-20), the membranes were blocked with 5% skim milk/TBST at room temperature (RT) for 30 min and incubated at 4℃ overnight with primary antibodies, followed by horseradish peroxidase-conjugated secondary antibodies at RT for 1 h. Primary antibodies included rabbit anti-Shank2 (#1136, kindly provided by Dr. Eunjoon Kim, Department of Biological Sciences, KAIST, Daejeon, Korea), rabbit anti-phospho-p44/42 MAPK (p-ERK1/2, 1:1000, Cell Signaling Technology, Beverly, MA), rabbit anti-ERK 1/2 (1:1000, Cell Signaling), rabbit anti-phospho-p38 MAPK (p-p38, 1:1000, Cell Signaling), rabbit anti-p38 (1:1000, Cell Signaling), rabbit anti-phospho-JNK (p-JNK, 1:1000, Cell Signaling), rabbit anti-JNK (1:1000, Cell Signaling), rabbit anti-phospho-Akt (p-AKT, 1:1000, Cell Signaling), or rabbit anti-AKT (1:1000, Cell Signaling) antibody. β-actin was used as a loading control (1:10000, Sigma). The proper bands were detected and visualized using an enhanced chemiluminescence system (Amersham Pharmacia Biotech, Little Chalfont, UK). Western blot analysis was performed by measuring band intensity with ImageJ 1.50i software (National Institutes of Health, Bethesda, MD, USA).
Immunohistochemistry
Mice were perfused transcardially with fixative containing 4% paraformaldehyde in 0.1 M phosphate buffer (pH 6.9), and the spinal cord was removed and sectioned based on the methods detailed in previous reports.19,23 Transverse spinal cord sections were incubated in blocking solution for 1 h at RT and then incubated for 48 h at 4℃ with one of the following primary antibodies: rabbit anti-phospho-p44/42 MAPK (p-ERK1/2, 1:500; Cell Signaling) and rabbit anti-Shank 2 (1:500; Synaptic Systems). Since anti-p-ERK and anti-Shank2 were derived from the same host species, donkey anti-rabbit IgG (H + L) Fab fragment (1:200; Jackson Immunoresearch) was used for blocking the visualization of the first primary antibody.24,25 The first primary antibody (anti-p-ERK1/2) was applied overnight at RT, then Alexa555-conjugated donkey anti-rabbit IgG (1:400; Invitrogen) was used as the secondary antibody. Next, according to the manufacturer’s instructions, we incubated the tissue with 5% normal rabbit serum and Fab anti-rabbit IgG (1:200) at RT for 20 min before incubation with the second primary antibody (anti-Shank, overnight at RT). Alexa488-conjugated donkey anti-rabbit IgG (1:400, Invitrogen Life Technologies, Carlsbad, CA, USA) was used as the secondary antibody for detecting the Shank2 protein.
Slice preparation of mouse spinal cord
We used adult (5 to 6 weeks old) male mice. Mice were deeply anesthetized with excess isoflurane, and the spinal cord including lumbosacral enlargement was exposed by a dorsal laminectomy. Dissected tissue blocks were placed into ice-cold cutting solution containing (in mM): 245 sucrose; 3 KCl; 6.0 MgCl2; 0.5 CaCl2; 26 NaHCO3; 1.25 NaH2PO4; 11 glucose; 5 HEPES; 1.0 Kynurenic acid (pH 7.4, when bubbled with 95% O2/5% CO2). Transverse slices (300 µm) were prepared using vibroslicer (Leica VT1000 Plus, Leica Microsystems GmbH, Germany). The slices were collected in a slice chamber containing recording artificial cerebrospinal fluid (aCSF) composed of (in mM): 126 NaCl; 3 KCl; 1.3 MgCl2; 2.5 CaCl2; 26 NaHCO3; 1.25 NaH2PO4; 11 glucose; 5 HEPES (pH 7.4, when bubbled with 95% O2 and 5% CO2 and had osmolarity of 305—310 mOsmol). The slices were initially maintained for 1 h to recover and transferred to the slice chamber kept at RT (25 ± 1℃) until used.
Visualized whole-cell patch clamp recordings
The slices were transferred to a recording chamber mounted on the stage of a BX50WI microscope (Olympus, Tokyo, Japan) fitted with fluorescence optics and a 40× water immersion objective. Slices were continuously superfused (∼5 ml/min) with recording aCSF. The data were recorded and acquired using an Axopatch 200B Amplifier (Molecular Devices, USA) and pClamp10.0 software (Molecular Devices, USA). Identified substantia gelatinosa (SG) neurons in translucent area of lamina II were recorded using microelectrodes of 4–5 MΩ pulled from borosilicate capillaries (World Precision Instruments). Whole-cell patch clamp recordings were performed at RT (25 ± 1℃). NMDA-induced currents were recorded using an internal solution containing (mM); 136 K-gluconate; 10 NaCl; 1 MgCl2; 10 EGTA; 10 HEPES; 2 Mg-ATP; 0.1 Na-GTP (pH 7.33 with KOH, 291 mOsmol); and recording aCSF. To prevent nonselective synaptic activity, a cocktail of neurotransmission inhibitors were added (in µM): 10 CNQX; 10 picrotoxin; 2 strychnine. Total NMDA currents were recorded in IIo neurons by perfusing spinal cord slices with 50 µM NMDA for 30 s.
Statistical analysis
All values are expressed as the mean ± SEM. Statistical analysis was performed using Prism 6.0 (Graph Pad Software, San Diego, USA). Results are expressed as means ± SEM. Comparison between two groups was made using the Student’s t-test. For multiple comparisons, ANOVA followed by post hoc Tukey’s test was performed. Differences with a p < 0.05 were considered significant.
Results
The effect of genetic depletion of Shank2 on i.t. NMDA-induced spontaneous pain responses
First, we investigated the effect of spinally injected NMDA in C57BL/6 control mice. Intrathecal administration of NMDA (0.4 nmol, 5 μl) produced spontaneous pain-like nociceptive behaviors (licking, scratching, and biting directed toward the hind limb, gluteal region, and base of the tail) compared with saline injection (Figure 1(a), ***p < 0.001 as compared to vehicle-treated mice), which is consistent with previous studies from our laboratories.26,27 Next, the potential role of the Shank2 protein in NMDA-induced spontaneous pain was examined in Shank2 KO mice. We verified that there was no Shank2 protein expression in the spinal dorsal horn of Shank2 KO with Western blot analysis (Figure 1(b), left panel). In saline-treated groups, there were no significant differences between WT and Shank2 KO mice (data not shown). However, following i.t. NMDA injection, Shank2 KO mice showed significantly reduced pain behaviors compared with Shank2 WT mice (Figure 1(b), right panel, #p < 0.05 as compared to NMDA injected WT mice), suggesting that the spinal Shank2 protein is involved in NMDA-induced pain transmission. Given symptoms of ASD are known to emerge early in childhood, we also observed this suppressed pain in response to i.t. NMDA injection in juvenile Shank2 KO mice (Supplementary Figure 1). To further determine the regulation of GluN2A and 2B function by Shank2 in spinal cord interneurons, we recorded NMDA-induced currents in lamina II neurons in spinal cord slices. NMDA (50 mM)-induced currents were significantly decreased from 410.2 ± 92.3 pA in WT mice to 131.7 ± 35.8 pA in Shank2 KO mice (Figure 1(c)).
The effect of i.t. injection of NMDA on phosphorylation of ERK in the spinal cord dorsal horn of the WT or Shank2 KO mice
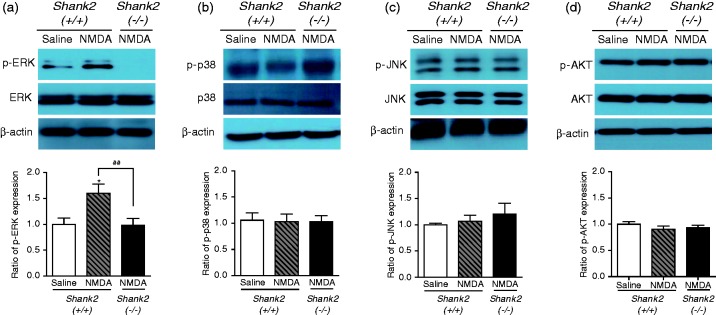
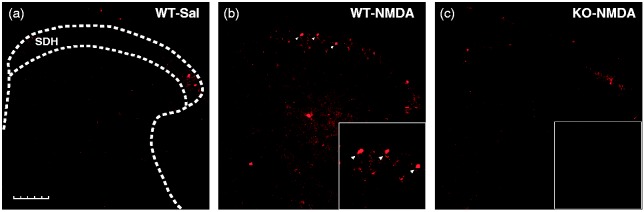
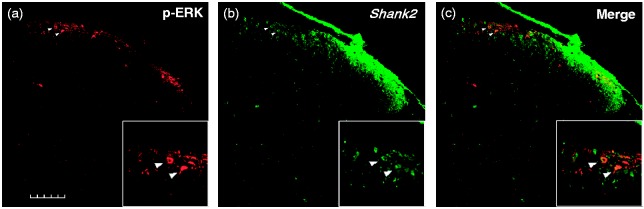
MAPKs and AKT play crucial roles in regulating NMDARs including their physiologic and biochemical/biophysical properties as well as their potential role in pathophysiology.28,29 Therefore, we examined whether MAPK or AKT signaling is activated in response to i.t. NMDA injection in WT and in Shank2 KO mice. In Western blot assays, we found that the ratio of p-ERK to MAPK/ERK expression was significantly increased in the spinal dorsal horn of NMDA-treated WT mice (Figure 2(a), *p < 0.05 as compared to saline-treated group). This NMDA-induced increase in spinal p-ERK expression was significantly reduced in Shank2 KO mice (Figure 2(a), ##p < 0.01 as compared to NMDA-treated WT mice). Moreover, in immunohistochemistry experiments, the number of p-ERK positive cells was significantly increased after NMDA injection and this increase occurred mainly in the superficial dorsal horn (Figure 3(a) and (b), the arrowheads indicate representative immunopositive p-ERK cells). A reduction in the NMDA-induced increase in p-ERK expression was also observed in Shank2 KO mice with immunohistochemistry (see Figure 3). Moreover, double immunohistochemistry indicated that many p-ERK positive cells were colocalized with Shank2 protein expressing cells in the dorsal horn (Figure 4(a)–(c)). On the other hand, the ratio of p-p38 to p38, p-JNK to JNK, or p-AKT to AKT expression was not changed by NMDA administration. These results suggest that the reduction in NMDA-induced spontaneous pain behaviors in Shank2 KO mice may be due to modulation of spinal ERK signaling.
Figure 2.
Graph illustrating the effect of intrathecal NMDA injection on the activity of spinal ERK, p38, JNK, and AKT, in Shank2 KO (Shank2 −/−) or WT (Shank2 +/+) mice. (a) A Western blot assay indicates that the ratio of p-ERK to ERK MAPK expression is significantly increased in the spinal cord dorsal horn of NMDA-treated WT mice. This NMDA-induced increase in spinal p-ERK expression is significantly reduced in Shank2 KO mice. *p < 0.05: significantly different from the value of the saline-treated group. ##p < 0.01: for the groups connected by a straight line. On the other hand, the ratio of (b) p-p38 to p38, (c) p-JNK to JNK, and (d) p-AKT to AKT expression did not change following NMDA administration in either Shank2 KO or WT mice. n = 7–8 mice per group.
Figure 3.
Photomicrographs showing representative immunohistochemistry images of phosphorylation of ERK (p-ERK) protein in the dorsal horn from spinal cord sections from Shank2 KO (Shank2 −/−) or WT (Shank2 +/+) mice that were intrathecally treated with saline or NMDA. In WT mice, (b) NMDA treatment increased p-ERK expression in the superficial dorsal horn (SDH) as compared to (a) saline treatment. (c) This NMDA-induced increase in p-ERK expression is suppressed in Shank2 KO mice. The lower boxes (outlined in white) are magnified images of the superficial dorsal horn from each image. Scale bar = 200 µm.
Figure 4.
Representative immunohistochemistry photomicrographs illustrating images of double-labeled cells that were double-positive for phosphorylated ERK (p-ERK) and Shank2 proteins in the spinal dorsal horn from intrathecal NMDA-treated WT (Shank2 +/+) mice. Each column represents an image from (a) p-ERK, (b) Shank2, or (c) double labeling of p-ERK with Shank2, respectively. NMDA treatment-induced p-ERK immunoreactive neurons co-contain Shank2 immunoreactivity. The lower boxes (outlined in white) are magnified images of the superficial dorsal horn from each image. Scale bar = 200µm.
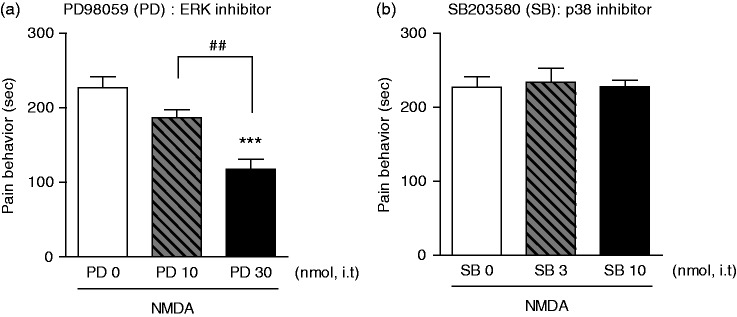
Analgesic effect of the ERK inhibitor, PD98059, on NMDA-induced spontaneous pain behaviors
In an attempt to determine a potential direct action of spinal ERK signaling on NMDA-induced spontaneous pain behaviors, we performed pharmacological blockade of ERK activation by pre-treatment with PD98059 prior to NMDA injection. Intrathecal injection of PD98059 dose-dependently reduced NMDA-induced pain behaviors. In this regard, a high dose of PD98059 (PD, 30 nmol) significantly blocked NMDA-induced spontaneous pain behaviors (Figure 5(a), *** p < 0.001 as compared to vehicle-treated mice, ##p < 0.01 as compared to PD 10 nmol treated mice). We further investigated the possible involvement of p38 MAPK signaling on NMDA-induced spontaneous pain behaviors. Intrathecal pre-injection of the selective p38 MAPK inhibitor, SB203580, did not affect NMDA-induced spontaneous pain behaviors (Figure 5(b)). Neither the 3 nmol nor the 10 mol doses of SB203580 produced an analgesic effect in NMDA-treated mice. Collectively, these results suggest that the ERK pathway, but not p38 MAPK, is involved in spinal NMDA-mediated pain sensation.
Figure 5.
Graphs illustrating the effects of pretreatment with an ERK (PD98059, PD) or p38 (SB203580, SB) inhibitor on intrathecal (i.t.) NMDA-induced spontaneous nociceptive behavioral responses. (a) I.t. injection of the ERK inhibitor dose-dependently suppressed NMDA-induced nociceptive responses compared with the vehicle-treated group (PD, 0 nmol). ***p < 0.001: significantly different from the value of the vehicle (PD, 0 nmol) treated group. ##p < 0.01: for the groups connected by a straight line. (b) Pretreatment with a p38 inhibitor did not affect nociceptive responses even at the high dose (SB, 10 nmol). n = 7–8 mice per group.
Discussion
In the present study, we have demonstrated that i.t. NMDA induces spontaneous pain behaviors that are significantly suppressed in Shank2 KO mice. These data suggest that the Shank2 protein is associated with NMDA-induced pain transmission in the spinal cord dorsal horn. Postsynaptic NMDA receptors are considered to be crucial molecules in central sensitization in the spinal cord.30 Activation of NMDA receptors leads to calcium influx, which causes spinal dorsal horn neurons to become more responsive to sensory inputs, resulting in central sensitization.13 Therefore, NMDA receptor dysfunction or modulation in the spinal cord can cause deficits in the synaptic transmission of nociceptive information.14 NMDA receptors at the synapse are physically associated with Shank2 proteins via its PDZ domain binding the PSD95-NMDA receptor complex.15,31,32 Moreover, dysfunction of NMDA receptors has been shown in mice lacking Shank2 proteins related to the ASD,11,16 and furthermore, the use of drugs to enhance NMDA receptor function leads to a significant recovery of ASD-like social deficits in Shank2-mutant mice.11 In addition to the behavioral data, we have also observed that NMDA-induced currents were dramatically reduced in shank2 KO mice compared with WT mice (Figure 1(c)). These results are in line with a previous study performed in the hippocampal synapses; NMDA receptor-dependent excitatory current and synaptic plasticity was impaired in Shank2 KO mice11. Collectively, the above results together with our data suggest that Shank2 mutations can lead to dysfunction of the NMDA receptor ultimately causing suppression of NMDA receptor-mediated pain transmission in the spinal cord.
Activation of MAPK and/or AKT are key biochemical events in the initiation and maintenance of peripheral and central neuronal sensitization.33–35 There is the strong evidence that phosphorylation of either MAPK or AKT can alter pain transmission via transcriptional and non-transcriptional signaling events.36,37 Thus, in the present study, we examined whether MAPK or AKT signaling is involved in NMDA-induced pain responses associated with Shank2 proteins. We demonstrated that p-ERK is increased in spinal superficial dorsal horn within 10 min following i.t. NMDA injection, while p38, JNK, and AKT signaling proteins are not changed by NMDA administration. The ERK1/2 pathway of mammals is probably the best-characterized MAPK system and our data in conjunction with information from other studies28,38 suggest that ERK is a specific signaling pathway associated with NMDA-induced pain transmission. In this regard, we show that i.t. injection of the ERK inhibitor, PD98059, suppresses the nociceptive behavioral responses induced by direct activation of NMDA receptors, indicating a significant link between NMDA receptor activation and the ERK pathway in the spinal cord dorsal horn. Because ERK was rapidly activated in a short timeframe (∼10 min), its regulation of neuronal excitability appears to be associated with non-transcriptional events, which may include phosphorylation of kinases, receptors, and ion channels, thus altering synaptic function.38
We next examined whether a Shank2 mutation would affect the NMDA-induced increase in ERK activity. Our data indicate that p-ERK-immunoreactivity is colocalized with Shank2 in many dorsal horn neurons following i.t. NMDA injection in WT mice. Moreover, NMDA-induced ERK activation is significantly suppressed in Shank2 KO mice. These results support our hypothesis that Shank2 mutation-induced dysfunction of NMDA receptors suppresses the normal NMDA-ERK pathway in the spinal dorsal horn, leading to a reduction in nociception. However, we cannot rule out the possibility that the Shank2 mutation also affects the synaptic function and plasticity at glutamatergic synapses in higher brain areas including the anterior cingulate cortex that is involved in pain perception. It has been reported that ERK signaling is disrupted in ASD, which results from a number of single gene mutations.5,39 However, it is unknown whether the SIBs observed in ASD are in fact related to dysfunction of NMDA-ERK signaling. Further study is required to better understand the detailed mechanisms associated with the Shank2 mutation-NMDA-ERK signaling that underlies SIBs.
Conclusions
We found in the present study that i.t. NMDA-induced spontaneous pain behaviors were significantly reduced in Shank2 mutation (KO) mice. These results suggest that Shank2 is involved in NMDA-mediated pain transmission in the spinal cord. Moreover, this decreased pain response in Shank KO mice appears to be mediated at least in part by suppression of p-ERK activity. This study provides insight into future investigations into the possibility that alterations in pain transmission may underlie the development of SIBs in ASD individuals and more importantly for the potential therapeutic use of NMDA or ERK specific drugs to treat SIBs or pain deficits in ASD patients.
Author contributions
SBO conceived the idea, and S-YY and S-GK helped design and conduct the study, analyze and interpret the data, and write the manuscript. YHK and J-HY helped conduct the experiments, interpret the data, and write the manuscript. H-GK helped conduct the study. B-KK, D-HR, J-HL, and SBO supervised the experiments, participated in the interpretation of data, and wrote the manuscript. AJB assisted with data interpretation and manuscript revision. All authors read and approved the final manuscript. S-YY and S-GK contributed equally.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the grants of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (No. HI15C3077). This work also was supported by the National Research Foundation of Korea (NRF) grants funded by the Korea government (MSIP) (No. 2013R1A6A3A04065858, 2014R1A2A2A01007695, 2015R1D1A1A01059208 and 2016M3A9B6021209). H-GK and B-KK are supported by the National Honor Scientist program.
Supplemental Material
Supplementary material for this paper can be found at http://journals.sagepub.com/doi/suppl/10.1177/1744806916688902.
References
- 1.Gomot M, Wicker B. A challenging, unpredictable world for people with autism spectrum disorder. Int J Psychophysiol 2012; 83: 240–247. [DOI] [PubMed] [Google Scholar]
- 2.Minshawi NF, Hurwitz S, Fodstad JC, et al. The association between self-injurious behaviors and autism spectrum disorders. Psychol Res Behav Manag 2014; 7: 125–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yasuda Y, Hashimoto R, Nakae A, et al. Sensory cognitive abnormalities of pain in autism spectrum disorder: a case-control study. Ann Gen Psychiatry 2016; 15: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chung BH, Tao VQ, Tso WW. Copy number variation and autism: new insights and clinical implications. J Formos Med Assoc 2014; 113: 400–408. [DOI] [PubMed] [Google Scholar]
- 5.Levitt P, Campbell DB. The genetic and neurobiologic compass points toward common signaling dysfunctions in autism spectrum disorders. J Clin Invest 2009; 119: 747–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sala C, Vicidomini C, Bigi I, et al. Shank synaptic scaffold proteins: keys to understanding the pathogenesis of autism and other synaptic disorders. J Neurochem 2015; 135: 849–858. [DOI] [PubMed] [Google Scholar]
- 7.Sheng M, Kim E. The Shank family of scaffold proteins. J Cell Sci 2000; 113(Pt 11): 1851–1856. [DOI] [PubMed] [Google Scholar]
- 8.Grabrucker AM. A role for synaptic zinc in ProSAP/Shank PSD scaffold malformation in autism spectrum disorders. Dev Neurobiol 2014; 74: 136–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leblond CS, Nava C, Polge A, et al. Meta-analysis of SHANK Mutations in Autism Spectrum Disorders: a gradient of severity in cognitive impairments. PLoS Genet 2014; 10: e1004580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zatkova M, Bakos J, Hodosy J, et al. Synapse alterations in autism: review of animal model findings. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 2016; 160: 201–210. [DOI] [PubMed] [Google Scholar]
- 11.Won H, Lee HR, Gee HY, et al. Autistic-like social behaviour in Shank2-mutant mice improved by restoring NMDA receptor function. Nature 2012; 486: 261–265. [DOI] [PubMed] [Google Scholar]
- 12.Ko HG, Oh SB, Zhuo M, et al. Reduced acute nociception and chronic pain in Shank2−/− mice. Mol Pain 2016; 12: 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Petrenko AB, Yamakura T, Baba H, et al. The role of N-methyl-D-aspartate (NMDA) receptors in pain: a review. Anesth Analg 2003; 97: 1108–1116. [DOI] [PubMed] [Google Scholar]
- 14.Zhou Q, Sheng M. NMDA receptors in nervous system diseases. Neuropharmacology 2013; 74: 69–75. [DOI] [PubMed] [Google Scholar]
- 15.Naisbitt S, Kim E, Tu JC, et al. Shank, a novel family of postsynaptic density proteins that binds to the NMDA receptor/PSD-95/GKAP complex and cortactin. Neuron 1999; 23: 569–582. [DOI] [PubMed] [Google Scholar]
- 16.Schmeisser MJ, Ey E, Wegener S, et al. Autistic-like behaviours and hyperactivity in mice lacking ProSAP1/Shank2. Nature 2012; 486: 256–260. [DOI] [PubMed] [Google Scholar]
- 17.Hylden JL, Wilcox GL. Intrathecal morphine in mice: a new technique. Eur J Pharmacol 1980; 67: 313–316. [DOI] [PubMed] [Google Scholar]
- 18.Yajima Y, Narita M, Tsuda M, et al. Modulation of NMDA- and (+)TAN-67-induced nociception by GABA(B) receptors in the mouse spinal cord. Life Sci 2000; 68: 719–725. [DOI] [PubMed] [Google Scholar]
- 19.Moon JY, Roh DH, Yoon SY, et al. sigma1 receptors activate astrocytes via p38 MAPK phosphorylation leading to the development of mechanical allodynia in a mouse model of neuropathic pain. Br J Pharmacol 2014; 171: 5881–5897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moon JY, Roh DH, Yoon SY, et al. Sigma-1 receptor-mediated increase in spinal p38 MAPK phosphorylation leads to the induction of mechanical allodynia in mice and neuropathic rats. Exp Neurol 2013; 247: 383–391. [DOI] [PubMed] [Google Scholar]
- 21.van den Heuvel I, Reichl S, Segelcke D, et al. Selective prevention of mechanical hyperalgesia after incision by spinal ERK1/2 inhibition. Eur J Pain 2015; 19: 225–235. [DOI] [PubMed] [Google Scholar]
- 22.Zhuang ZY, Gerner P, Woolf CJ, et al. ERK is sequentially activated in neurons, microglia, and astrocytes by spinal nerve ligation and contributes to mechanical allodynia in this neuropathic pain model. Pain 2005; 114: 149–159. [DOI] [PubMed] [Google Scholar]
- 23.Yoon SY, Robinson CR, Zhang H, et al. Spinal astrocyte gap junctions contribute to oxaliplatin-induced mechanical hypersensitivity. J Pain 2013; 14: 205–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lewis Carl SA, Gillete-Ferguson I, Ferguson DG. An indirect immunofluorescence procedure for staining the same cryosection with two mouse monoclonal primary antibodies. J Histochem Cytochem 1993; 41: 1273–1278. [DOI] [PubMed] [Google Scholar]
- 25.Negoescu A, Labat-Moleur F, Lorimier P, et al. F(ab) secondary antibodies: a general method for double immunolabeling with primary antisera from the same species. Efficiency control by chemiluminescence. J Histochem Cytochem 1994; 42: 433–437. [DOI] [PubMed] [Google Scholar]
- 26.Kim HW, Roh DH, Yoon SY, et al. Activation of the spinal sigma-1 receptor enhances NMDA-induced pain via PKC- and PKA-dependent phosphorylation of the NR1 subunit in mice. Br J Pharmacol 2008; 154: 1125–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yoon SY, Roh DH, Seo HS, et al. An increase in spinal dehydroepiandrosterone sulfate (DHEAS) enhances NMDA-induced pain via phosphorylation of the NR1 subunit in mice: involvement of the sigma-1 receptor. Neuropharmacology 2010; 59: 460–467. [DOI] [PubMed] [Google Scholar]
- 28.Haddad JJ. N-methyl-D-aspartate (NMDA) and the regulation of mitogen-activated protein kinase (MAPK) signaling pathways: a revolving neurochemical axis for therapeutic intervention? Prog Neurobiol 2005; 77: 252–282. [DOI] [PubMed] [Google Scholar]
- 29.Hetman M, Kharebava G. Survival signaling pathways activated by NMDA receptors. Curr Top Med Chem 2006; 6: 787–799. [DOI] [PubMed] [Google Scholar]
- 30.Millan MJ. The induction of pain: an integrative review. Prog Neurobiol 1999; 57: 1–164. [DOI] [PubMed] [Google Scholar]
- 31.Ehlers MD. Synapse structure: glutamate receptors connected by the shanks. Curr Biol 1999; 9: R848–R850. [DOI] [PubMed] [Google Scholar]
- 32.Tu JC, Xiao B, Naisbitt S, et al. Coupling of mGluR/Homer and PSD-95 complexes by the Shank family of postsynaptic density proteins. Neuron 1999; 23: 583–592. [DOI] [PubMed] [Google Scholar]
- 33.Obata K, Noguchi K. MAPK activation in nociceptive neurons and pain hypersensitivity. Life Sci 2004; 74: 2643–2653. [DOI] [PubMed] [Google Scholar]
- 34.Sun RQ, Tu YJ, Yan JY, et al. Activation of protein kinase B/Akt signaling pathway contributes to mechanical hypersensitivity induced by capsaicin. Pain 2006; 120: 86–96. [DOI] [PubMed] [Google Scholar]
- 35.Sweatt JD. The neuronal MAP kinase cascade: a biochemical signal integration system subserving synaptic plasticity and memory. J Neurochem 2001; 76: 1–10. [DOI] [PubMed] [Google Scholar]
- 36.Choi JI, Svensson CI, Koehrn FJ, et al. Peripheral inflammation induces tumor necrosis factor dependent AMPA receptor trafficking and Akt phosphorylation in spinal cord in addition to pain behavior. Pain 2010; 149: 243–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Edelmayer RM, Brederson JD, Jarvis MF, et al. Biochemical and pharmacological assessment of MAP-kinase signaling along pain pathways in experimental rodent models: a potential tool for the discovery of novel antinociceptive therapeutics. Biochem Pharmacol 2014; 87: 390–398. [DOI] [PubMed] [Google Scholar]
- 38.Ji RR, Baba H, Brenner GJ, et al. Nociceptive-specific activation of ERK in spinal neurons contributes to pain hypersensitivity. Nat Neurosci 1999; 2: 1114–1119. [DOI] [PubMed] [Google Scholar]
- 39.Kalkman HO. Potential opposite roles of the extracellular signal-regulated kinase (ERK) pathway in autism spectrum and bipolar disorders. Neurosci Biobehav Rev 2012; 36: 2206–2213. [DOI] [PubMed] [Google Scholar]