Abstract
Objective
We examined the effect of functional disability on all-cause mortality and cause-specific deaths among community-dwelling US adults.
Methods
We used data from 142,636 adults who participated in the 1994–1995 National Health Interview Survey-Disability Supplement eligible for linkage to National Death Index records from 1994 to 2006 to estimate the effects of disability on mortality and leading causes of death.
Results
Adults with any disability were more likely to die than adults without disability (19.92% vs. 10.94%; hazard ratio = 1.51, 95% confidence interval, 1.45–1.57). This association was statistically significant for most causes of death and for most types of disability studied. The leading cause of death for adults with and without disability differed (heart disease and malignant neoplasms, respectively).
Conclusions
Our results suggest that all-cause mortality rates are higher among adults with disabilities than among adults without disabilities and that significant associations exist between several types of disability and cause-specific mortality. Interventions are needed that effectively address the poorer health status of people with disabilities and reduce the risk of death.
Keywords: disability, mortality, cause of death
Functional disability affects large numbers of Americans. In 2010, 56.7 million people (18.7% of the community-dwelling population) had some level of disability, and 38.3 million (12.6% of the same population) had a severe disability.1
The concept of health should be the same for people with and without such disabilities.2 However, people with disabilities experience poorer health and functioning than those without disabilities.3–10 In particular, people with disabilities are at greater risk for secondary conditions, such as cardiovascular disease, diabetes, urinary tract infection, and pressure sores, each of which adversely affect overall health.2,11 These associations suggest that people with disabilities may have increased risk of mortality, although the mechanism is unclear.
A complication of the disability-mortality association is that people with disabilities are prone to higher behavioral health risks that affect morbidity and mortality. For example, people with disabilities are more likely to be obese,12–14 to smoke,14 and to be physically inactive,15 all risk factors for premature mortality. Additional studies have shown that protective lifestyle behaviors, such as exercise, may delay both the onset of disability and subsequent mortality.16
Prior studies of the association between disability and death have been limited by inadequate covariate adjustment or control for disability severity or functional limitations,6,9,17 low generalizability due to the use of clinic samples or focus only on older adults,3,5,6,8,17–19 and samples that do not include comparison adults without disability.20,21 Most studies have only focused on a single type of disability18,20,22–25 or disability in general,21 or only on all-cause mortality.3,5,6,8,9,17,19,24,25 Understanding differential mortality by disability type is necessary because different groups may need tailored interventions to reduce their mortality risk. Design of interventions to reduce mortality risk faced by people with disabilities also may require knowledge of their causes of death.
We used data on community-dwelling US adults to assess the association between disability (and disability type) on all-cause mortality and on cause-specific deaths. Disability types included sensory, mental/substance use impairment, cognitive, movement, and employment disability. Cause-specific deaths included heart disease, malignant neoplasms, chronic lower respiratory diseases, cerebrovascular diseases (stroke), unintentional accidents, and suicides/assaults. We used Cox proportional hazard regression models to estimate the likelihood of mortality, incorporating both time to death as well as adjustment for number of functional limitations and demographic and socioeconomic characteristics. We also examined the rank-ordered causes of death for adults with and without a disability at baseline who later died.
METHODS
Data Sources
We used data from the 1994 and 1995 National Health Interview Survey (NHIS) public use files and the NHIS-Disability Supplement (NHIS-D) fielded during the same years, linked to the restricted use files for the National Death Index (NDI) for the years 1994–2006.26 The NHIS-D data provide detailed information on disability, and the NDI provides detailed death information including date and cause of death.
Sample
For the 1994–1995 NHIS-D surveys, the total number of adult respondent records aged 18 or older was 145,007. Of these records, 2371 (1.64%) were ineligible for an NDI record linkage because of missing linkage information (eg, name, social security number, date of birth). Of the remaining 142,636 adult respondents, 19,283 (13.5%) died during the follow-up period, that is, between their interview date and December 31, 2006. Of the 142,636 adult respondents included in the descriptive analyses, the any disability measure was missing for 7093 (4.97%) adults, resulting in an analytical sample of 135,543 adult respondents for regression analyses. We found no difference on a range of characteristics between those dropped and included in regression analyses.
Disability Definition and Categories
Disability status was ascertained at the NHIS-D interview and defined by having any activity limitation or the use of special equipment (eg, a cane, wheelchair, or special bed or telephone). For the full list of NHIS questions used to code disability constructs, please see SDC, Table 1, Supplemental Digital Content 1, http://links.lww.com/MLR/A869). The “any disability” measure was defined as having one or more of the all-inclusive disability categories listed below for at least 12 months before interview. Some single disability types were combined into broader categories to increase sample sizes for analysis. The 5 categories were (1) sensory (impairment in sight or hearing); (2) mental/substance use impairment (schizophrenia, paranoid/delusional disorders, bipolar disorder, major depression, severe personality disorder, alcohol abuse, drug abuse, and other mental or emotional conditions); (3) cognitive impairment (problems with learning, communication, and/or understanding, Down Syndrome, mental retardation, autism, Alzheimer disease, or other senile disorders); (4) movement (difficulty with lifting 10 pounds, walking up 10 steps, walking a quarter mile, standing for 20 minutes, bending down from a standing position, reaching over the head, using the fingers to grasp or handle something, or holding a pen or pencil or reporting the use of a cane, crutches, walker, wheelchair, or scooter to get around), and, for analyses performed on adults aged 18–64 only; (5) employment (unable to work or limited in work because of impairment or health problem or currently receiving Supplemental Security Income). Each disability category was a dichotomous variable coded as 1 or 0, as was the overall variable of any disability.
TABLE 1.
Summary Statistics of Baseline Sociodemographic Characteristics, Disability Type, and Number of Deaths During Follow-up Among Eligible Adults Aged 18 or Older
| Baseline Characteristics | Unweighted N | Weighted N (in 1000s) | Weighted % |
|---|---|---|---|
| Total | 187,287 | 100.00 | |
| Year of interview (n = 142,636) | |||
| 1994 | 76,146 | 93,223 | 49.78 |
| 1995 | 66,490 | 94,064 | 50.22 |
| Demographic | |||
| Age (n = 142,636) | |||
| 18–44 | 78,781 | 106,256 | 56.73 |
| 45–64 | 39,422 | 50,250 | 26.83 |
| 65–74 | 14,470 | 18,059 | 9.64 |
| 75+ | 9963 | 12,722 | 6.79 |
| Sex (n = 142,636) | |||
| Male | 66,180 | 89,589 | 47.84 |
| Female | 76,456 | 97,697 | 52.16 |
| Race (n = 142,636) | |||
| White, not Hispanic or Latino | 119,272 | 157,700 | 84.20 |
| Black, not Hispanic or Latino | 17,491 | 21,283 | 11.36 |
| Other, including Hispanic | 5873 | 8304 | 4.43 |
| Marital status (n = 142,414) | |||
| Currently married | 91,565 | 119,839 | 64.09 |
| Separated/divorced | 14,276 | 18,271 | 9.77 |
| Widowed | 10,390 | 12,920 | 6.91 |
| Never married | 26,183 | 35,969 | 19.23 |
| Socioeconomic | |||
| Education (n = 141,563) | |||
| < High school | 13,277 | 14,983 | 8.06 |
| High school graduate/some college | 68,853 | 89,790 | 48.28 |
| College graduate | 59,433 | 81,221 | 43.67 |
| Work/employment status (n = 142,636) | |||
| Currently employed | 91,113 | 121,863 | 65.07 |
| Unemployed | 4169 | 5516 | 2.95 |
| Not in the work force | 47,354 | 59,907 | 31.99 |
| Family income level (n = 142,636) | |||
| < 200% Federal poverty level | 43,428 | 54,467 | 29.08 |
| 200% Federal poverty level+ | 99,208 | 132,820 | 70.92 |
| Insurance coverage (n = 142,636) | |||
| Yes | 116,461 | 154,037 | 82.25 |
| No | 26,175 | 33,250 | 17.75 |
| Behavioral risk | |||
| Weight category (n = 142,635) | |||
| Underweight ≤ 19 | 16,077 | 21,412 | 11.43 |
| Normal 19 ≤ BMI < 25 | 56,471 | 75,226 | 40.17 |
| Overweight 25 ≤ BMI < 30 | 47,064 | 61,489 | 32.83 |
| Obese BMI ≥ 30 | 23,023 | 29,158 | 15.57 |
| Disability type | |||
| Any disability (N = 135,543) | 22,181 | 28,619 | 16.07 |
| Multiple disabilities (N = 135,543) | 5776 | 7380 | 4.14 |
| Single disability (N = 135,543) | 16,405 | 21,239 | 11.93 |
| Sensory* (n = 139,923) | 9285 | 11,877 | 6.46 |
| Mental/substance use impairment (n = 139,992) | 5941 | 7821 | 4.25 |
| Cognitive impairment (n = 141,445) | 3483 | 4634 | 2.51 |
| Movement (n = 138,688) | 10,788 | 13,619 | 7.48 |
| Employment (SSI) disability† (N = 112,296) | 10,058 | 12,960 | 8.71 |
| ADL difficulty >1 y (N = 141,958) | 3450 | 4424 | 2.37 |
| Mortality through December 31, 2006 (n = 142,636) | |||
| Yes | 19,283 | 24,400 | 13.03 |
| No | 123,353 | 162,887 | 86.97 |
Sight or hearing.
Assessed only for adults aged 18–64 years; defined as self-reported employment disability or receiving SSI.
ADL indicates activities of daily living; BMI, body mass index; SSI, Supplemental Security Income.
Sources: 1994–1995 National Health Interview Survey on Disability; 1994–2006 National Death Index.
Because the disability types were not mutually exclusive, a 3-level variable was created to designate whether the respondent had 1 disability or multiple disabilities with the referent group being no disability. Any disability, multiple/single/no disability, and each disability category were alternately the main predictor variables of interest in our analyses. We also created a count variable to measure difficulties with activities of daily living (ADLs), which included bathing, dressing, eating, getting in or out of bed or a chair, or using the toilet (range, 0–6), to serve as an indicator of the degree/level of disability experienced regardless of disability type. Finally, in models that assess the association between mortality and disability type, because respondents can have >1 type of disability we created a variable that indicates multiple disabilities (yes vs. no, with no including those with either one or no disabilities).
Death
All-cause mortality was indicated by having a death record in the linked NDI file (yes/no). We also coded causes of death using the underlying-cause-of-death International Classification of Diseases (ICD-10) codes,27 a set of variables representing the 113 mutually exclusive causes of death. The ICD-10 codes are based on the underlying cause of death, which is defined by the World Health Organization as the disease or injury that initiated the train of events leading directly to death, or the circumstances of the accident or violence that produced the fatal injury. For this analysis, we focused on 6 leading causes of death: (1) heart diseases (ICD-10 codes I00–I09, I11, I13, and I20–I51); (2) malignant neoplasms (eg, cancer and malignant tumors) (ICD-10 codes C00–C97); (3) chronic lower respiratory diseases (ICD-10 codes J40–J47); (4) cerebrovascular diseases (eg, stroke) (ICD-10 codes I60–I69); (5) unintentional accidents (ICD-10 codes V01–X59 and Y85–Y86); and (6) intentional—suicides/assaults (ICD-10 codes U01–U03, X60–X84–Y09,Y87.0, and Y87.1). We created a survival time variable based on the number of days between the date of the NHIS-D interview and the date of death for use in the Cox proportional hazard models. Adults who did not die during the follow-up period were censored in the analyses, with the survival time variable computed in days between the date of interview through December 31, 2006, the last date of the follow-up period when the person was last known to be alive.
Covariates
In addition to year of interview, NHIS data provided information on covariates including demographic factors [age (y), sex, race/ethnicity, and marital status] and socioeconomic factors (education, employment status, family income level, and insurance coverage). In addition, NHIS data contained self-reported height and weight information that enabled the calculation of body mass index and classification of overweight/obese status.
Descriptive Analyses
Weighted population estimates (in 1000s) and weighted percentages of NHIS-D adults were reported for each predictor (disability) and outcome (death) variable of interest, as well as for each covariate level. In bivariate analyses, the relationship between disability at the time of the interview and death during the follow-up period was examined by computing the proportion of respondents who died by disability status and type for all causes of mortality and for 6 leading causes of death. Both unadjusted and age-adjusted percentages are presented. Age adjustment was performed using direct standardization to the age distribution of the 1994 and 1995 NHIS-D samples (categorized as 18–44, 45–64, 65–74, and 75+), thereby removing the confounding effect of age when comparing the proportion of adults who died across categories. For those who died during follow-up, leading causes of death were examined for adults with and without disability.
Proportional Hazard Models
Three Cox proportional hazard28 regression models were estimated on 2 different age groups (respondents aged 18–64 y and 65 y or older), as well as on all adults aged 18 years or older, adjusting for covariates and the number of functional limitations. First, we focused on the mortality effects of reporting any disability. Second, we estimated the mortality effects of having various disability levels (having no, single, or multiple disabilities). Third, we estimated the effect of each disability category (sensory, mental/substance use impairment, cognitive, movement, and employment (employment disability was assessed only for those adults aged 18–64 y) adjusting for presence of overlapping disabilities (multiple disabilities vs. single or no disability). Fourth, we estimated the effect of disability (any levels and categories) on each cause-specific death. Finally, we conducted a sensitivity analysis for the disability categories analyses where each model contained only 1 specific disability category rather than entering all categories into the model simultaneously, adjusting for the same covariates listed above to assess the robustness of the estimates in the model with all disability types included. Multicollinearity analyses did not reveal significant associations between variables. The proportional hazards assumption was met for each of the main independent variables of interest (ie, each of the disability variables in each model).
All statistical analyses were performed using SUDAAN release 11.029 to account for weighting and the complex sample design. A pooled analysis weight was created based on the combined 1994 and 1995 NHIS-D phase 1 data files and was applied to estimate population parameters permitting generalization to the US civilian, noninstitutionalized adult population. For all statistical tests, a P value of <0.05 was considered statistically significant.
RESULTS
Baseline characteristics of the 142,636 adults in descriptive analyses were representative of the 1994–1995 US noninstitutional population. A majority were aged 18–45 years, female, white, not Hispanic or Latino, married, high school graduates, currently employed, had family incomes over 200% of the federal poverty level, and had health insurance coverage (Table 1).
More than 16% of our sample had a disability at baseline. About one quarter of those with a disability had multiple disabilities. Movement disabilities were the most common (7.48% of our sample), followed by 6.46% with sensory disabilities, 4.25% with mental/substance use impairment, 2.51% with cognitive impairment, and 8.71% of adults aged 18–64 with an employment disability.
Overall, 18,236 respondents (13.5%) in our analytic sample [ie, those with nonmissing disability data (n = 135,543)] died of any cause during the follow-up period (1994–2006). Adults with any disability at baseline were more likely to die during follow-up than adults without a disability at baseline [age-adjusted percentages: 19.92% vs. 10.94%; hazard ratio (HR) = 1.51; 95% confidence interval (CI), 1.45–1.57, Table 2]. Those with multiple disabilities were most likely to die, followed by those with a single disability and those with no disability (age-adjusted percentages: 26.01% vs. 17.97% vs. 10.94%). Both adults with multiple disabilities and with a single disability were more likely to die than adults without a disability at baseline (HR = 1.70; 95% CI, 1.60–1.81 and HR = 1.45; 95% CI, 1.39–1.51, respectively). The magnitude of the coefficients (not shown) describing the association between any disability and death and between multiple disabilities and death for adults aged 18–64 years are larger than coefficients for adults aged 65 or older, suggesting a stronger association in young and middle-aged adults.
TABLE 2.
Association Between Disability and All-Cause Death Among Adults Aged 18 or Older
| Estimated n Died (in 1000s) | % Died | % Died Age Adjusted) | Adjusted Cox Regression Model HR (95% CI) | |
|---|---|---|---|---|
| Adults aged 18–64 | ||||
| Model 1* | ||||
| Any disability | ||||
| Yes | 3166 | 13.62 | 10.92 | 1.89 (1.77–2.02) |
| No | 4184 | 3.44 | 3.62 | 1.00 |
| Model 2* | ||||
| Disability | ||||
| Multiple | 1770 | 19.75 | 15.49 | 2.36 (2.15–2.58) |
| Single | 1397 | 9.77 | 7.98 | 1.66 (1.51–1.79) |
| None | 4184 | 3.44 | 3.62 | 1.00 |
| Model 3† | ||||
| Sensory disability | 892 | 14.00 | 9.96 | 1.13 (1.02–1.25) |
| Mental/substance use impairment disability | 856 | 13.02 | 12.55 | 1.20 (1.06–1.36) |
| Cognitive impairment disability | 340 | 10.33 | 10.68 | 0.74 (0.62–0.88) |
| Movement disability | 1457 | 21.03 | 15.18 | 1.32 (1.17–1.50) |
| Employment (SSI) disability‡ | 2345 | 18.09 | 14.04 | 1.93 (1.73–2.16) |
| No disability | 4184 | 3.44 | 3.62 | 1.00 |
| Adults aged 65 or older | ||||
| Model 1* | ||||
| Any disability | ||||
| Yes | 7371 | 69.70 | 65.28 | 1.47 (1.41–1.53) |
| No | 7936 | 42.95 | 45.51 | 1.00 |
| Model 2* | ||||
| Disability | ||||
| Multiple | 2607 | 79.14 | 73.52 | 1.64 (1.54–1.75) |
| Single | 4764 | 65.43 | 62.09 | 1.42 (1.35–1.49) |
| None | 7936 | 42.95 | 45.51 | 1.00 |
| Model 3† | ||||
| Sensory disability | 3704 | 67.26 | 61.78 | 1.08 (1.01–1.15) |
| Mental/substance use impairment disability | 946 | 75.86 | 72.40 | 1.41 (1.24–1.59) |
| Cognitive impairment disability | 1019 | 76.06 | 68.89 | 1.13 (1.00–1.28) |
| Movement disability | 5093 | 76.12 | 71.53 | 1.65 (1.55–1.75) |
| No disability | 7936 | 42.95 | 45.51 | 1.00 |
| Adults aged 18 or older | ||||
| Model 1* | ||||
| Any disability | ||||
| Yes | 9809 | 34.27 | 19.92 | 1.51 (1.45–1.57) |
| No | 13,262 | 8.87 | 10.94 | 1.00 |
| Model 2* | ||||
| Disability | ||||
| Multiple | 3470 | 47.02 | 26.01 | 1.70 (1.60–1.81) |
| Single | 6339 | 29.85 | 17.97 | 1.45 (1.39–1.51) |
| None | 13,262 | 8.87 | 10.94 | 1.00 |
| Model 3† | ||||
| Sensory disability | 4596 | 38.70 | 18.46 | 1.09 (1.03–1.16) |
| Mental/substance use impairment disability | 1082 | 23.04 | 22.37 | 1.51 (1.30–1.66) |
| Cognitive impairment disability | 1359 | 29.32 | 20.23 | 1.03 (0.93–1.15) |
| Movement disability | 6550 | 48.10 | 24.44 | 1.64 (1.56–1.73) |
All estimates are weighted. Age adjustment was performed using direct standardization to the age distribution of the 1994 and 1995 NHIS-D samples (categorized as 18–44, 45–64, 65–74, and 75+).
Model adjusted for covariates including year of interview, age, sex, race, marital status, education, employment status, income, insurance coverage, BMI, and disability severity (eg, # ADLs).
Model adjusted for covariates including year of interview, age, sex, race, marital status, education, employment status, income, insurance coverage, BMI, disability severity (eg, #ADLs), and multiple disabilities.
Assessed only for adults aged 18–64 years; defined as self-reported employment disability or receiving SSI.
CI indicates confidence interval; HR, hazard ratio; SSI, Supplemental Security Income.
Sources: 1994–1995 National Health Interview Survey on Disability and 1994–2006 National Death Index.
Among adults aged 65 or older, those with each type of disability were more likely to die than those with no disability in a model that contained all disability types and covariates. Findings were similar among younger adults aged 18–64 and all adults aged 18 or older, however, there was no association between having cognitive impairment and death. Sensitivity models among adults of these age groups that included just cognitive impairment adjusted for covariates and the number of functional limitations also showed the lack of association. In the model for adults aged 18–64 years that also contained the employment disability variable, adults with cognitive impairment were less likely to die as compared with those with no disability (HR=0.74; 95% CI, 0.62–0.88). Odds ratios for the covariates included in each all-cause mortality model are displayed in SDC, Table 2 (Supplemental Digital Content 2, http://links.lww.com/MLR/A870).
Among all adults who died (regardless of disability status), the leading cause of death was heart disease (29.76%), followed by malignant neoplasm (24.76%), stroke (cerebrovascular diseases, 6.40%), and chronic lower respiratory diseases (5.34%). In addition, 3.19% of all adults died of unintentional accidents and 1.47% died from suicide or assaults (Table 3). The leading causes of death were the same among adults with a disability at baseline, but the difference between heart disease and malignant neoplasms was considerably larger (32.83% and 17.84%, respectively). In contrast, the leading cause of death for adults with no disability at baseline was malignant neoplasm (29.68%), followed by heart disease (27.54%).
TABLE 3.
Proportion of Each Leading Cause of Death Among Eligible Adults Aged 18 or Older at Baseline Who Died During the Follow-up Period, by Disability Status at Baseline (n = 19,233)
| Primary Underlying Cause of Death | Total (95% CI) | Any Disability (95% CI) | No Disability (95% CI) |
|---|---|---|---|
| Heart disease | 29.76 (29.00–30.53) | 32.83 (31.79–33.90) | 27.54 (26.47–28.63) |
| Malignant neoplasm | 24.76 (24.07–25.47) | 17.84 (16.98–18.73) | 29.68 (28.68–30.71) |
| Stroke (cerebrovascular diseases) | 6.40 (6.04–6.78) | 7.59 (6.95–8.29) | 5.58 (5.12–6.07) |
| Chronic lower respiratory diseases | 5.34 (4.99–5.72) | 6.39 (5.80–7.03) | 4.45 (4.05–4.89) |
| Unintentional—accidents | 3.19 (2.92–3.48) | 2.18 (1.84–2.58) | 3.91 (3.52–4.33) |
| Intentional—suicide/assault | 1.47 (1.28–1.69) | 0.84 (0.64–1.10) | 1.97 (1.67–2.32) |
| Other | 29.07 (28.36–29.79) | 32.32 (31.20–33.47) | 26.88 (25.98–27.79) |
| Total (%) | 100 | 100 | 100 |
CI indicates confidence interval.
Sources: 1994–1995 National Health Interview Survey on Disability and National Death Index 1994–2006.
Compared with adults without a disability, adults with a disability at baseline were more likely to die of heart disease (5.93% vs. 3.14%; HR = 1.55; 95% CI, 1.44–1.68), malignant neoplasms (3.97% vs. 3.06%; HR = 1.18; 95% CI, 1.09–1.27), stroke (1.25% vs. 0.67%; HR = 1.62; 95% CI, 1.40–1.87), chronic lower respiratory diseases (1.24% vs. 0.50%; HR = 2.05; 95% CI, 1.75–2.39), unintentional accidents (0.59% vs. 0.38%; HR = 1.43; 95% CI, 1.14–1.78), and intentional accidents such as suicides and assaults (0.33% vs. 0.17%; HR = 1.64; 95% CI, 1.15–2.34) (Table 4 and Fig. 1). People with multiple disabilities and those with single disabilities were more likely to die of each leading cause of death compared with those with no disability (except intentional suicides or assaults, in which estimates were suppressed because of small sample sizes); the magnitude of the HR was higher among those with multiple disabilities than those with a single disability.
TABLE 4.
Association Between Disability and Cause-Specific Death Among Adults Aged 18 or Older
| Cause of Death |
Any Disability* |
Multiple Disability* |
Single Disability* |
No Disability |
Sensory Disability† |
Mental/Substance Use Impairment Disability† |
Cognitive Impairment Disability† |
Movement Disability† |
|---|---|---|---|---|---|---|---|---|
| Heart diseases | ||||||||
| % died | 11.25 | 15.95 | 9.62 | 2.44 | 12.91 | 6.56 | 9.38 | 16.68 |
| % died (age adjusted) | 5.93 | 7.44 | 5.40 | 3.14 | 5.36 | 6.23 | 6.02 | 7.32 |
| Adjusted Cox model HR (95% CI) | 1.55 (1.44–1.68) | 1.77 (1.58–1.97) | 1.49 1.37–1.61) | 1.00 | 1.04 (0.95–1.15) | 1.42 (1.21–1.66) | 1.03 (0.86–1.23) | 1.82 (1.66–2.00) |
| Malignant neoplasms | ||||||||
| % died | 6.11 | 6.83 | 5.86 | 2.63 | 7.23 | 3.99 | 3.87 | 7.54 |
| % died (age adjusted) | 3.97 | 4.62 | 3.81 | 3.06 | 3.73 | 3.97 | 3.26 | 4.48 |
| Adjusted Cox model HR (95% CI) | 1.18 (1.09–1.27) | 1.22 (1.07–1.39) | 1.17 (1.07–1.27) | 1.00 | 1.02 (0.91–1.15) | 1.43 (1.20–1.70) | 0.78 (0.62–0.98) | 1.27 (1.14–1.43) |
| Stroke (cerebrovascular diseases) | ||||||||
| % died | 2.60 | 3.77 | 2.20 | 0.50 | 3.02 | 2.34 | 1.41 | 3.86 |
| % died (age adjusted) | 1.25 | 1.72 | 1.10 | 0.67 | 1.19 | 1.38 | 1.41 | 1.54 |
| Adjusted Cox model HR (95% CI) | 1.62 (1.40–1.87) | 1.80 (1.45–2.24) | 1.56 (1.34–1.81) | 1.00 | 1.12 (0.90–1.39) | 1.30 (0.97–1.76) | 1.15 (0.84–1.57) | 1.76 (1.44–2.13) |
| Chronic lower respiratory diseases | ||||||||
| % died | 2.19 | 2.70 | 2.01 | 0.39 | 2.42 | 1.37 | 1.40 | 3.08 |
| % died (age adjusted) | 1.24 | 1.44 | 1.18 | 0.50 | 1.08 | 1.40 | 0.97 | 1.53 |
| Adjusted Cox model HR (95% CI) | 2.05 (1.75–2.39) | 1.98 (1.58–2.48) | 2.07 (1.76–2.48) | 1.00 | 1.48 (1.20–1.84) | 1.83 (1.36–2.47) | 0.88 (0.60–1.28) | 2.31 (1.86–2.86) |
| Unintentional accidents | ||||||||
| % died | 0.75 | 0.98 | 0.67 | 0.35 | 0.78 | 0.60 | 0.71 | 0.94 |
| % died (age adjusted) | 0.59 | 0.71 | 0.55 | 0.38 | 0.49 | 0.62 | 0.56 | 0.70 |
| Adjusted Cox model HR (95% CI) | 1.43 (1.14–1.78) | 1.70 (1.23–2.34) | 1.35 (1.07–1.71) | 1.00 | 1.12 (0.79–1.59) | 1.16 (0.77–1.73) | 0.80 (0.46–1.37) | 1.67 (1.14–2.45) |
| Suicides/assaults | ||||||||
| % died | 0.29 | ‡ | ‡ | 0.17 | ‡ | 0.55 | ‡ | 0.23 |
| % died (age adjusted) | 0.33 | ‡ | ‡ | 0.17 | ‡ | 0.56 | ‡ | 0.20 |
| Adjusted Cox model HR (95% CI) | 1.64 (1.15–2.34) | ‡ | ‡ | 1.00 | 0.71 (0.36–1.39) | 3.58 (2.13–6.00) | ‡ | 0.93 (0.43–2.01) |
Rates based on <20 deaths are considered unreliable and noted with a double dagger (‡). All estimates are weighted. Age adjustment was performed using direct standardization to the age distribution of the 1994 and 1995 NHIS-D samples (categorized as 18–44, 45–64, 65–74, and 75+).
Model adjusted for covariates including year of interview, age, sex, race, marital status, education, employment status, income, insurance coverage, BMI, and disability severity (eg, number of difficulties with activities of daily living).
Model adjusted for covariates including year of interview, age, sex, race, marital status, education, employment status, income, insurance coverage, BMI, disability severity (eg, number of ADLs), and multiple disabilities.
CI indicates confidence interval; HR, hazard ratio.
Sources: 1994–1995 National Health Interview Survey on Disability and National Death Index.
FIGURE 1.
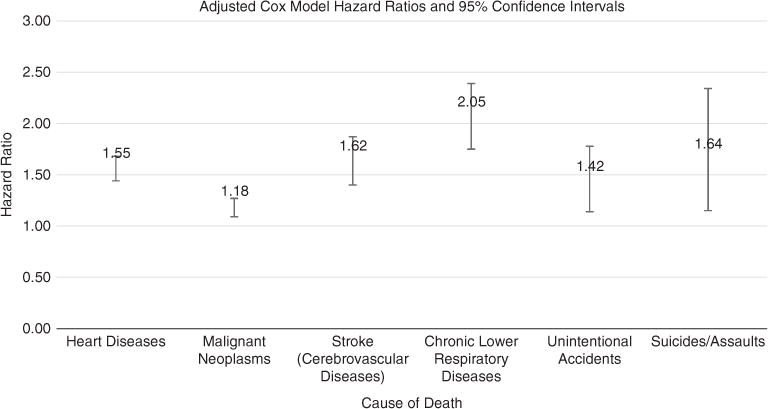
Association between disability and cause-specific mortality. Adjusted Cox model hazard ratios and 95% confidence intervals.
In models that included all disability types, adults in each of the specific disability categories had increased risk of death as compared with adults with no disability at baseline. For example, adults with mental/substance use impairment or movement disability were more likely to die of heart diseases and of malignant neoplasms than adults with no disability. Adults with movement disability were more likely to die of stroke, and adults within each disability category except cognitive were more likely to die of chronic lower respiratory disease than adults without a disability. Adults with mental/substance use impairment were approximately 3 and a half times as likely as adults without a disability to die of suicide/assaults (HR = 3.58; 95% CI, 2.13–6.00). Odds ratios for the covariates included in each cause-specific mortality model are displayed in SDC, Table 3 (Supplemental Digital Content 3, http://links.lww.com/MLR/A871).
DISCUSSION
This study found that all-cause mortality rates were higher among adults with disabilities than among adults without disabilities. In addition, the study found significant associations between several types of disability and cause-specific mortality. For example, adults with mental/substance use impairment were over 3 and a half times as likely to die of suicide or assault as those without disability, a finding that suggests targeting interventions for those experiencing mental illness or substance use disorders. Prior studies have shown significant associations between mental/substance use impairment and mortality from heart diseases,30 and malignant neoplasms.31 Overall, this study’s results are generalizable to community-dwelling adults in the United States.
The rank-ordered causes of death for adults with disability at baseline mirrored that of the general population, with heart disease as the leading cause of death, followed by malignant neoplasms. However, those without disability at baseline were most likely to die of malignant neoplasms, followed by heart disease. In contrast, heart disease is the leading cause of death in the United States among adults with disability, but not among adults without disability. Thus, public policies to lower heart disease may have a disproportionate effect in lowering mortality rates among people with disabilities.
Consistent with previous studies, this study found associations between disability, functional status, and mental illness and mortality.3,5,6,8,9,17–25 In addition, we found that most disability categories (all categories among adults aged 65 or older; all categories but cognitive impairment among adults aged 18–64 and among adults 18 or older) significantly increased the risk of mortality. Adults in both the single disability category and the multiple disabilities category had higher risks of mortality than adults without disability. Even though the working age population was less likely to report any disability, the magnitude of the effect of disability on mortality is greater when restricted to the 18–64 age group. Additional research to understand this difference in magnitude may help identify potential policies (eg, more timely access to care or better care coordination) to reduce mortality in the working age population.
In terms of disability categories, movement disability had the strongest association with mortality, followed by mental/substance use impairment, and sensory disability. The only disability category that we did not find to be associated with increased mortality was cognitive impairment among the younger (and overall adult) age groups; in fact, adults aged 18–64 years with cognitive impairment were less likely to die during follow-up. Although other studies have shown an increased risk of mortality among those with cognitive impairment, most sampled older adult populations or sampled patients with a particular medical disorder.32 Although our analysis did include younger adults, the NHIS did not sample some populations with high levels of cognitive impairment (eg, people in institutions, people without homes) and also excluded adults living in the community who had severe cognitive impairment for whom proxies may not have been available.33 Thus, future research is needed to investigate whether this finding of no effect for cognitive impairment would continue if other, perhaps more severely impaired, subpopulations with cognitive impairment were included.
The overall results suggest that, in addition to their long-term care needs, people with disabilities have acute care needs that need to be addressed to reduce mortality risk. In particular, disparities in behavioral health risks, preventive service use (eg, mammograms), and the quality of care34,35 experienced by people with disabilities may be associated with this differential mortality risk. In addition, persons with disabilities may have unique situations that require special consideration in determining ways to best modify some risk factors for mortality (eg, efforts to increase physical activity may require environmental accommodations or specific assistance in exercising safely). Improvements in the availability of and access to preventive services and inclusion in behavioral health interventions may reduce this mortality risk differential. In addition, once people with disabilities become seriously ill, additional focus on care and case management to aid in timely and appropriate receipt of acute care may help delay or reduce mortality.
This study has several limitations. First, the study collects disability information only at the time of the 1994–1995 NHIS-D interview. Therefore, the analyses do not account for any changes in disability status during the follow-up period. Because the “no disability” category probably included adults who developed disability subsequent to the interview, our estimates of mortality serve as a lower-bound estimate of the effects of disability on mortality. Second, we were unable to adjust for certain behavioral characteristics known to be correlates of disability and also associated with increased risk of mortality, including physical activity, smoking, alcohol use, and presence of chronic health conditions36 because the NHIS-D did not collect these data on the full sample of participants. Thus, future research focused on exploring the impact of these covariates on the disability-mortality association is needed. Our findings, however, improve on previous studies examining the association between disability and death because relatively few earlier studies adjusted for covariates other than age and sex. Third, although we did attempt to adjust for disability severity by including ADLs as a covariate, our analyses may not have considered other types of heterogeneity not measured by ADLs. Finally, the NHIS-D samples only from noninstitutionalized adults living in the community. We thus were unable to examine the impact of disability on death among adults living in nursing homes, mental health facilities, institutions for persons with intellectual and developmental disabilities, and correctional facilities, or adults without homes—populations that are likely to have more severe forms of disability than noninstitutionalized adults.
Despite the limitations, our study goes beyond the prior evidence base in important ways. It is the first study using nationally representative data to examine the association between different types of disability and mortality, including specific causes of death among US adults. We used Cox proportional models rather than logistic regression, which enabled us to account for time until death rather than simply examining whether death occurred. Few prior studies that used nondisabled adults as their comparison group, were able to adjust for multiple covariates (eg, a measure of functional impairment and characteristics implicated in the disability-death association), and had sample sizes large enough to permit examination of specific causes of death associated with disability and particular types of disability.
This study underlines the fact that some people with disabilities have serious health problems in addition to needing long-term services and supports. To address this issue, policymakers might focus on initiatives that integrate medical care and long-term services and supports. In addition, interventions that reduce disparities in access to health services, behavioral risk factors, and the receipt of preventive services are needed to effectively address the poorer health status of people with disabilities and reduce the risk of death.
Supplementary Material
Acknowledgments
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention or RTI, International.
Footnotes
The authors declare no conflict of interest.
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Website, www.lww-medicalcare.com).
References
- 1.Brault MW. Current Population Reports. Washington, DC: US Census Bureau; 2012. Americans With Disabilities: 2010. [Google Scholar]
- 2.U.S. Department of Health and Human Services. The Surgeon General’s call to action to improve the health and wellness of persons with disabilities. 2005 Available at: http://www.cdc.gov/ncbddd/disabilityandhealth/pdf/whatitmeanstoyou508.pdf. Accessed January 30, 2015. [PubMed]
- 3.Bernard SL, Kincade JE, Konrad TR, et al. Predicting mortality from community surveys of older adults: the importance of self-rated functional ability. J Gerontol B Psychol Sci Soc Sci. 1997;52:S155–S163. doi: 10.1093/geronb/52b.3.s155. [DOI] [PubMed] [Google Scholar]
- 4.Dejong G, Palsbo SE, Beatty PW, et al. The organization and financing of health services for persons with disabilities. Milbank Q. 2002;80:261–301. doi: 10.1111/1468-0009.t01-1-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fried LP, Kronmal RA, Newman AB, et al. Risk factors for 5-year mortality in older adults: the Cardiovascular Health Study. JAMA. 1998;279:585–592. doi: 10.1001/jama.279.8.585. [DOI] [PubMed] [Google Scholar]
- 6.Greiner PA, Snowdon DA, Greiner LH. The relationship of self-rated function and self-rated health to concurrent functional ability, functional decline, and mortality: findings from the Nun Study. J Gerontol B Psychol Sci Soc Sci. 1996;51:S234–S241. doi: 10.1093/geronb/51b.5.s234. [DOI] [PubMed] [Google Scholar]
- 7.Krahn G, Drum C, Culley C, et al. Health Disparities and Disabilities: A Brief Report. Washington, DC: Rehabilitation Research and Training Centers Health and Wellness Consortium 2002 Policy Forum; 2002. [Google Scholar]
- 8.Scott WK, Macera CA, Cornman CB, et al. Functional health status as a predictor of mortality in men and women over 65. J Clin Epidemiol. 1997;50:291–296. doi: 10.1016/s0895-4356(96)00365-4. [DOI] [PubMed] [Google Scholar]
- 9.Tager IB, Haight TJ, Hollenberg M, et al. Physical functioning and mortality in older women: an assessment of energy costs and level of difficulty. J Clin Epidemiol. 2003;56:807–813. doi: 10.1016/s0895-4356(03)00149-5. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Racial/ethnic disparities in self-rated health status among adults with and without disabilities—United States, 2004–2006. MMWR Morb Mortal Wkly Rep. 2008;57:1069–1073. [PubMed] [Google Scholar]
- 11.Campbell ML, Sheets D, Strong PS. Secondary health conditions among middle-aged individuals with chronic physical disabilities: implications for unmet needs for services. Assist Technol. 1999;11:105–122. doi: 10.1080/10400435.1999.10131995. [DOI] [PubMed] [Google Scholar]
- 12.Coyle CP, Santiago MC, Shank JW, et al. Secondary conditions and women with physical disabilities: a descriptive study. Arch Phys Med Rehabil. 2000;81:1380–1387. doi: 10.1053/apmr.2000.9169. [DOI] [PubMed] [Google Scholar]
- 13.Kinne S, Patrick DL, Doyle DL. Prevalence of secondary conditions among people with disabilities. Am J Public Health. 2004;94:443–445. doi: 10.2105/ajph.94.3.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Armour BS, Campbell VA, Crews JE, et al. State-level prevalence of cigarette smoking and treatment advice, by disability status, United States, 2004. Prev Chronic Dis. 2007;4:A86. [PMC free article] [PubMed] [Google Scholar]
- 15.Rantanen T, Guralnik JM, Sakari-Rantala R, et al. Disability, physical activity, and muscle strength in older women: the Women’s Health and Aging Study. Arch Phys Med Rehabil. 1999;80:130–135. doi: 10.1016/s0003-9993(99)90109-0. [DOI] [PubMed] [Google Scholar]
- 16.Chakravarty EF, Hubert HB, Lingala VB, et al. Reduced disability and mortality among aging runners: a 21-year longitudinal study. Arch Intern Med. 2008;168:1638–1646. doi: 10.1001/archinte.168.15.1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Newman AB, Simonsick EM, Naydeck BL, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA. 2006;295:2018–2026. doi: 10.1001/jama.295.17.2018. [DOI] [PubMed] [Google Scholar]
- 18.Dembling BP, Chen DT, Vachon L. Life expectancy and causes of death in a population treated for serious mental illness. Psychiatr Serv. 1999;50:1036–1042. doi: 10.1176/ps.50.8.1036. [DOI] [PubMed] [Google Scholar]
- 19.Corti MC, Guralnik JM, Salive ME, et al. Serum albumin level and physical disability as predictors of mortality in older persons. JAMA. 1994;272:1036–1042. [PubMed] [Google Scholar]
- 20.Esbensen AJ, Seltzer MM, Greenberg JS. Factors predicting mortality in midlife adults with and without Down syndrome living with family. J Intellect Disabil Res. 2007;51:1039–1050. doi: 10.1111/j.1365-2788.2007.01006.x. [DOI] [PubMed] [Google Scholar]
- 21.Zayatz T. Social Security Disability Insurance Program Worker Experience. Baltimore, MD: Social Security Administration Office of the Chief Actuary; 2011. [Google Scholar]
- 22.Dickey B, Dembling B, Azeni H, et al. Externally caused deaths for adults with substance use and mental disorders. J Behav Health Serv Res. 2004;31:75–85. doi: 10.1007/BF02287340. [DOI] [PubMed] [Google Scholar]
- 23.Druss BG, Zhao L, Von Esenwein S, et al. Understanding excess mortality in persons with mental illness: 17-year follow up of a nationally representative US survey. Med Care. 2011;49:599–604. doi: 10.1097/MLR.0b013e31820bf86e. [DOI] [PubMed] [Google Scholar]
- 24.Pratt LA. Serious psychological distress, as measured by the K6, and mortality. Ann Epidemiol. 2009;19:202–209. doi: 10.1016/j.annepidem.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 25.Zheng D, Macera CA, Croft JB, et al. Major depression and all-cause mortality among white adults in the United States. Ann Epidemiol. 1997;7:213–218. doi: 10.1016/s1047-2797(97)00014-8. [DOI] [PubMed] [Google Scholar]
- 26.National Center for Health Statistics. Office of Analysis and Epidemiology, The National Health Interview Survey (1986–2004) Linked Mortality Files, Mortality Follow-up Through 2006: Matching Methodology. 2009 Available at: http://www.cdc.gov/ncbddd/disabilityandhealth/pdf/whatitmeanstoyou508.pdf. Accessed January 30, 2015.
- 27.World Health Organization. International Classification of Diseases (ICD) classifications. 2012 Available at: http://www.who.int/classifications/icd/en/. Accessed December 4, 2013.
- 28.Cox DR. Regression models and life tables. J R Stat Soc B. 1972;34:187–220. [Google Scholar]
- 29.RTI International. SUDAAN® Language Manual, Release 110. Research Triangle Park, NC: RTI International; 2012. [Google Scholar]
- 30.Osborn DP, Levy G, Nazareth I, et al. Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom’s General Practice Rsearch Database. Arch Gen Psychiatry. 2007;64:242–249. doi: 10.1001/archpsyc.64.2.242. [DOI] [PubMed] [Google Scholar]
- 31.Lawrence D, Holman CD, Jablensky AV, et al. Excess cancer mortality in Western Australian psychiatric patients due to higher case fatality rates. Acta Psychiatr Scand. 2000;101:382–388. doi: 10.1034/j.1600-0447.2000.101005382.x. [DOI] [PubMed] [Google Scholar]
- 32.Dewey ME, Saz P. Dementia, cognitive impairment and mortality in persons aged 65 and over living in the community: a systematic review of the literature. Int J Geriatr Psychiatry. 2001;16:751–761. doi: 10.1002/gps.397. [DOI] [PubMed] [Google Scholar]
- 33.Gould E, Maslow K, Yuen P, et al. Providing Services for People With Dementia Who Live Alone. Research Triangle Park, NC: RTI International; 2010. [Google Scholar]
- 34.Lawthers AG, Pransky GS, Peterson LE, et al. Rethinking quality in the context of persons with disability. Int J Qual Health Care. 2003;15:287–299. doi: 10.1093/intqhc/mzg048. [DOI] [PubMed] [Google Scholar]
- 35.Armour BS, Ouyang L, Thibadeau J, et al. Hospitalization for urinary tract infections and the quality of preventive health care received by people with spina bifida. Disabil Health J. 2009;2:145–152. doi: 10.1016/j.dhjo.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 36.Altman B, Bernstein A. Disability and Health in the United States, 2001–2005. Hyattsville, MD: National Center for Health Statistics; 2008. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


