Abstract
Introduction
Intracavernosal injection (ICI) therapy is widely used for the treatment of erectile dysfunction (ED). Its use in practice is largely empirical and has not been validated with evidence-based approaches.
Aim
To compare two strategies for ICI, specifically a risk-based approach and an empiric-based approach, and assess the efficacy, patient satisfaction, and complication rates of the two treatment approaches.
Methods
After obtaining approval from the institutional review board, a prospective database of patients enrolled in the ICI program at the Johns Hopkins Hospital (Baltimore, MD, USA) from May 2012 through May 2014 was amassed. Demographic information, treatment outcomes, and subjective patient evaluations of sexual function (International Index of Erectile Function erectile function domain [IIEF-EF], Quality of Erection Questionnaire [QEQ], Sexual Quality of Life [SQoL], and Erectile Dysfunction Inventory of Treatment Satisfaction [EDITS]) were obtained at baseline and at 3 and 6 months. Two approaches were compared. Group 1 received empiric ICI treatment initially with prostaglandin E1 (PGE1) 10 μg irrespective of ED etiology or severity. After initial dosing with PGE1 in the clinic, adjustments were made to titrate or change formulations pending on patient results. Group 2 received a risk-based approach, in which an algorithm that factored in ED etiology and number of ED risk factors was used for a bimix (papaverine 30 mg/mL, phentolamine 1 mg/mL), a low-dose trimix (papaverine 30 mg/mL, phentolamine 1 mg/mL, PGE1 10 μg/mL), or a high-dose trimix (papaverine 30 mg/mL, phentolamine 2 mg/mL, PGE1 40 μg/mL). Dose titration was permitted in the two groups. Statistical analysis was carried out using t-test and χ2 analysis.
Main Outcome Measures
The study design was powered for a non-inferiority comparison of the two approaches, in which the primary end point was a 15-point difference on the EDITS score or a 20% difference in the IIEF-EF score.
Results
One hundred seventy-five patients were enrolled (57 in group 1, 118 in group 2) with 3- and 6-month follow-up at 57% and 35%, respectively, and similar between groups. Baseline patient characteristics and sexual function questionnaire responses were similar between groups 1 and 2, although group 1 reported higher-quality erections at baseline (QEQ score = 14.3 vs 7.3, P = .05) and had a smaller proportion of patients with prostatectomy (54.4% vs 74.6%, P = .02). In the two groups, QEQ score (mean = 10.78 vs 56.76, P < .05), SQoL score (mean = 38.41 vs 50.25, P < .05), and IIEF-EF score (mean = 7.51 vs 18.48, P < .05) improved with treatment. However, at 3 and 6 months, there were no statistically significant differences in responses for IIEF, QEQ, SQoL, or EDITS scores and no difference in failure or medication switch rates between groups. There were no significant differences in complication rates, although at 3 months group 2 reported a higher incidence of priapism and pain (23% vs 7.4%, P = .08).
Conclusion
Empiric and risk-based strategies for ICI therapy resulted in significant improvements across multiple domains of sexual function. Complication rates, satisfaction, and efficacy overall were similar between the two approaches. Clinicians can be reassured that no one approach to ICI therapy for ED management appears inferior to another.
Key Words: Intracavernosal Injection Therapy, Phosphodiesterase Type 5 Inhibitor, Erectile Dysfunction, Treatment, Algorithm
Introduction
Erectile dysfunction (ED) affects roughly 20 million men in the United States and is predicted to affect more than 300 million men worldwide by 2025.1, 2 Various forms of therapy have been developed to treat ED, including oral pharmacotherapy,3, 4 transurethral suppositories, vacuum constriction devices, intracavernosal injection (ICI) therapy, and implantation of an inflatable penile prosthesis.5, 6 Traditional first-line treatment for ED includes oral phosphodiesterase type 5 inhibitors (PDE5-Is).4, 5, 6 Although these agents have a proved track record for enhancing erectile function, many patients will have failed treatment or will discontinue treatment, often requiring a second-line option.3, 6, 7, 8 In addition, patients with ED and diabetes or after radical prostatectomy are considered hard to treat and might be true non-responders to PDE5-I therapy.
ICI therapy is a widely used second-line treatment for ED, although using it in practice is largely empirical and has not been validated with evidence-based approaches. Although there is a variety of literature on the efficacy and long-term outcomes of patients using ICI therapy, a standard approach to medication selection and dosing has never been investigated.9 In addition, data on patient satisfaction with this treatment are lacking. Patients with failed first-line therapies often have various risk factors contributing to the development of ED, such as medical comorbidities (diabetes, peripheral vascular disease, hypertension, dyslipidemia, or cardiovascular disease), lifestyle factors such as smoking, a history of pelvic surgery for the prostate, bladder, or colon or rectum, and radiation therapy for pelvic malignancies.10, 11, 12, 13 It is unclear whether accounting for such risk factors would help with the initial agent choice and dose selection when using ICI therapy and whether a risk-based approach would help define maximal efficacy and patient satisfaction.
The purpose of this study was to compare two strategies for ICI therapy to determine whether a risk-based approach differs in efficacy, satisfaction, or complication rate compared with an empiric approach.
Methods
After obtaining approval from the institutional review board, a prospective database of patients enrolled in the ICI program at the Johns Hopkins Hospital (Baltimore, MD, USA) from May 2012 through May 2014 was amassed. Baseline demographic information (Table 1), comorbidities (Table 2), treatment outcomes, and subjective patient self-evaluations of sexual function using the International Index of Erectile Function erectile function domain (IIEF-EF), Quality of Erection Questionnaire (QEQ), Sexual Quality of Life (SQoL), and Erectile Dysfunction Inventory of Treatment Satisfaction (EDITS) were obtained at baseline and 3 and 6 months after initiation of ICI therapy.
Table 1.
Baseline characteristics of patients
| Group 1, empiric | Group 2, risk based | P value | |
|---|---|---|---|
| Men, n | 57 | 118 | N/A |
| Age (y), mean (SEM) | 61.9 (1.4) | 61.3 (0.7) | .66 |
| QEQ score, mean (SEM) | 14.3 (3.5) | 7.3 (1.8) | .05 |
| SQoL score, mean (SEM) | 37.7 (3.3) | 39.2 (2.2) | .71 |
| IIEF-EF score, mean (SEM) | 8.1 (0.9) | 6.9 (0.6) | .28 |
IIEF-EF = International Index of Erectile Function erectile function domain; N/A = not applicable; QEQ = Quality of Erection Questionnaire; SEM = standard error of the mean; SQoL = Sexual Quality of Life.
Table 2.
Baseline characteristics and comorbidities of patients
| Characteristics | Group 1, empiric (n = 47), n (%) | Group 2, risk based (n = 90), n (%) | P value |
|---|---|---|---|
| Smoking history | 8 (17.0) | 30 (33.3) | .047 |
| EtOH abuse | 1 (2.1) | 6 (6.7) | .42 |
| DM2 | 6 (12.8) | 16 (17.8) | .62 |
| Atherosclerosis | 7 (14.9) | 12 (13.3) | .80 |
| HTN | 22 (46.8) | 48 (53.3) | .48 |
| Dyslipidemia | 22 (46.8) | 39 (43.3) | .72 |
| OSA | 3 (6.4) | 9 (10) | .54 |
| Renal failure | 1 (2.1) | 7 (7.8) | .26 |
| Renal transplantation | 1 (2.1) | 3 (3.3) | 1.0 |
| Prostate cancer | 32 (68.1) | 65 (72.2) | .69 |
| Prostatectomy | 26 (55.3) | 66 (73.3) | .037 |
| Radiation | 7 (14.1) | 6 (6.7) | .13 |
| Cryotherapy | 1 (2.1) | 0 (0) | .34 |
| ADT | 0 (0) | 0 (0) | 1.0 |
| Priapism | 1 (2.1) | 0 (0) | .34 |
| Peyronie disease | 0 (0) | 2 (2.2) | .54 |
| Pelvic trauma | 0 (0) | 0 (0) | 1.0 |
| Penile trauma | 0 (0) | 0 (0) | 1.0 |
| Spinal cord injury | 1 (2.1) | 1 (1.1) | 1.0 |
| Depression | 2 (4.2) | 4 (4.4) | 1.0 |
| Hypogonadism | 6 (12.8) | 6 (6.7) | .34 |
ADT = androgen deprivation therapy; DM2 = type 2 diabetes mellitus; EtOH = ethanol; HTN = hypertension; OSA = obstructive sleep apnea.
In brief, these surveys assess the following aspects of patient satisfaction and sexual function. The IIEF survey is a 15-item questionnaire designed to assess for ED. It is broken down into domains to include erectile function, orgasmic function, sexual desire and intercourse, and overall satisfaction.14 The QEQ is a six-item patient-report measurement that solely evaluates the satisfaction of men with the quality of their erection.15 The SQoL domain from the Sexual Life Quality Questionnaire consists of 10 questions comparing patients' current sexual experience with their experience before the onset of ED.16 The EDITS is an 11-item survey that assesses patient satisfaction with treatment for ED.17
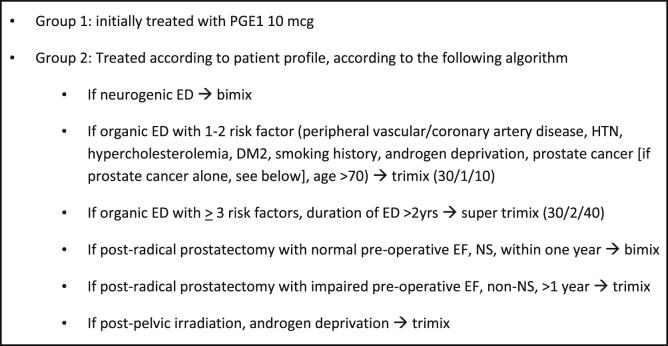
Using these validated surveys, two approaches were compared. Group 1 consisted of an empiric ICI treatment used by one sexual medicine provider (A.B.). Patients were treated with prostaglandin E1 (PGE1) 10 μg irrespective of ED etiology or severity and only if poor response was noted at test injection and then initiated on a bimix (papaverine 30 mg/mL and phentolamine 1 mg/mL, usual starting dose = 0.1–0.2 mL) or a low-dose trimix (papaverine 30 mg/mL, phentolamine 1 mg/mL, and PGE1 10 μg/mL, usual starting dose = 0.1–0.2 mL). Group 2 consisted of a risk-based approach used by another sexual medicine provider (T.J.B.), in which patients were treated with a bimix (papaverine 30 mg/mL and phentolamine 1 mg/mL), a low-dose trimix (papaverine 30 mg/mL, phentolamine 1 mg/mL, and PGE1 10 μg/mL), or a high-dose trimix (papaverine 30 mg/mL, phentolamine 2 mg/mL, and PGE1 40 μg/mL) using an algorithm that factored in ED etiology (vasculogenic vs neurogenic) and presence of ED risk factors (Figure 1). The presence of at least three risk factors was used as the cutoff for “difficult-to-manage ED,” which designated patients for high-dose trimix. Dose titration to 1 mL was permitted in the two groups. All patients in this study had failed PDE5-I therapy initially and thus were started on ICI therapy. No patients took combined therapy during the study.
Figure 1.
Treatment algorithm for selection of intracavernosalinjection agent. DM2 = type 2 diabetes mellitus; ED = erectile dysfunction; EF = erectile function; HTN = hypertension; NS = nerve sparing; PGE1 = prostaglandin E1.
Patients were counseled about the side effects and adverse events of using ICI therapy, including prolonged and/or painful erections, and instructed to seek medical attention if an erection lasted longer than 4 hours. During initial ICI treatment in the office, patients with a painful erection 2 hours after injection received phenylephrine in the office. After the initial office ICI therapy, priapic episodes were self-reported by the patient.
The study design was powered for a non-inferiority comparison of the two approaches, in which the primary end point was a 15-point difference on the EDITS score or a 20% difference in the IIEF-EF score. Statistical analysis was carried out using paired t-tests to assess for differences between survey scores on the QEQ, SQOL, IIEF, and EDITS at individual time points. The χ2 analysis was used to compare differences between rates of complications.
Results
One hundred seventy-five patients were enrolled (57 in group 1 with the empiric approach, 118 in group 2 with the risk-based approach) with 3- and 6-month follow-up at 57% and 35%, respectively. Baseline patient characteristics (Table 2) and sexual function questionnaire responses (Table 3, Table 4, Table 5, Table 6) were similar between groups 1 and 2, although group 1 reported higher-quality erections at baseline (QEQ score = 14.3 vs 7.3, P = .05) and had a smaller proportion of patients with prostatectomy (55.3% vs 73.3%, P = .037).
Table 3.
Comparison of mean Erectile Dysfunction Inventory of Treatment Satisfaction scores at different time points after treatment
| Months after treatment | Group 1, empiric (n = 57) |
Group 2, risk based (n = 118) |
P value | ||
|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | ||
| 0 (baseline) | N/A | N/A | N/A | N/A | N/A |
| 3 | 24 | 62.5 (27.9) | 39 | 66.2 (23.0) | .570 |
| 6 | 14 | 65.2 (23.3) | 22 | 63.4 (26.3) | .833 |
N/A = not applicable.
Table 4.
Comparison of mean Quality of Erection Questionnaire scores at different time points after treatment
| Months after treatment | Group 1, empiric (n = 57) |
Group 2, risk based (n = 118) |
P value | ||
|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | ||
| 0 (baseline) | 54 | 14.2 (25.3) | 111 | 7.2 (19.4) | .077 |
| 3 | 25 | 49.7 (39.4) | 37 | 61.1 (37.7) | .253 |
| 6 | 13 | 59.0 (35.4) | 23 | 54.9 (40.1) | .762 |
Table 5.
Comparison of mean Sexual Quality of Life scores at different time points after treatment
| Months after treatment | Group 1, empiric (n = 57) |
Group 2, risk based (n = 118) |
P value | ||
|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | ||
| 0 (baseline) | 56 | 37.3 (25.0) | 110 | 39.2 (24.0) | .650 |
| 3 | 22 | 45.9 (26.2) | 34 | 53.8 (27.1) | .283 |
| 6 | 14 | 44.3 (25.6) | 24 | 57.4 (28.2) | .161 |
Table 6.
Comparison of mean International Index of Erectile Function scores at different time points after treatment
| Months after treatment | Group 1, empiric (n = 57) |
Group 2, risk based (n = 118) |
P value | ||
|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | ||
| 0 (baseline) | 57 | 8.1 (6.9) | 117 | 7.0 (6.3) | .299 |
| 3 | 25 | 18.2 (9.9) | 37 | 18.5 (9.9) | .915 |
| 6 | 13 | 18.1 (9.9) | 24 | 19.2 (9.7) | .730 |
In the two groups, QEQ score (mean = 10.78 vs 56.76, P < .05), SQoL score (mean = 38.41 vs 50.25, P < .05), and IIEF-EF score (mean = 7.51 vs 18.48, P < .05) improved with treatment from baseline to 6 months. When comparing groups, there was no statistically significant difference in responses for the empiric group or the risk-based group at 3 months for QEQ score (49.7% vs 61.1%, P = .253), IIEF-EF score (18.2% vs 18.5%, P = .92), SQoL score (45.9% vs 53.8%, P = .28), and EDITS score (62.5% vs 66.2%, P = .57). At the 6-month mark, there was no statistically significant difference in responses between groups for QEQ score (59% vs 54.9%, P = .76), IIEF-EF score (18.1% vs 19.2%, P = .73), SQoL score (44.3% vs 57.4%, P = .2), or EDITS score (65.2% vs 63.4%, P = .83; Table 3, Table 4, Table 5, Table 6). Three-month failure rates, defined as patient-reported failure and discontinuation of ICI therapy, were similar, with 40% reporting failure of treatment and 20% then switching to another ICI medication. There also was no difference noted in failure or medication switch rates between the two approaches. There were no significant differences in complication rates between the two treatment approaches. At 3 months, group 2 reported a non-statistically significant higher incidence of priapism and pain than group 1 (23% vs 7.4%, P = .08).
Discussion
ICI therapy is an effective treatment alternative for men with ED. It is well tolerated in most patients, with high patient satisfaction rates.9, 18, 19 In our study, ICI therapy improved erectile function as measured by multiple validated questionnaires assessing different aspects of sexual function (IIEF, QEQ, and SQoL). Patient satisfaction with treatment was no different between the empiric and the risk-based approaches. The EDITS, specifically designed to assess patient satisfaction with treatment received, noted no difference at 3 or 6 months for either approach. Even subgroup analysis looking exclusively at the post-prostatectomy population showed no significant differences between approaches, but numbers were small and underpowered. This is in concordance with other studies that compared different ICI therapies and found no difference in patient satisfaction between different therapeutic groups.19 These results suggest that successful erectile response likely translates to patient satisfaction irrespective of initial ICI therapy used. Furthermore, although we might expect that risk-based selection of an initial ICI agent would lead to higher satisfaction rates through a fast and early response, our data suggest that empirically selecting an agent irrespective of ED etiology produces similar satisfaction rates and erectile responses.
This study also highlights the patient's perspective on ICI therapy. Similar satisfaction rates were noted in the two arms, and the use of validated questionnaires helped quantify the magnitude of the improvement in erectile function, sexual quality of life, and satisfaction rates. It demonstrated non-inferiority of one approach over another, suggesting that simple regimens might be equally efficacious from a patient's perspective.
ICI therapy is well known to induce side effects, in particular hematoma, priapism, and penile pain. A multicenter study evaluating a bimix in 157 men demonstrated an efficacy rate of 94% with a side effect incidence of 0.9% to 2.6% for priapism, pain, or hematoma.20 Another study comparing trimix with PGE1 found that Trimix produced a longer-lasting erection than PGE1 but increased the risk of priapism.19 Although not statistically significant, our study also showed an increased incidence of priapism in the risk-based treatment group at 3-month follow-up. This was not evident at the 6-month follow-up. Because the increased incidence of priapism occurred only at the 3-month timeframe in the group using the higher dose titration, this could represent a learning curve with dose escalation and indicate how further education at initial start-up might decrease the occurrence of priapism. In addition, providing further in-office education and follow-up during a patient's first three to six injections at home, to monitor their response, and to help with dose-appropriate titrations might decrease the incidence of priapism during the initial 3-month interval.
An obvious limitation to our study is that priapic episodes were self-reported and we do not have information on the duration of prolonged erection, although patients were instructed to seek medical attention if an erection lasted longer than 4 hours. All self-reported events required intervention to decrease the priapism. Another limitation is that we did not assess testosterone levels in this cohort, unless they specifically had signs and symptoms of low testosterone. This information might have been useful for the study.
Despite the efficacy and patient satisfaction seen with ICI therapy, cost and convenience could be limiting factors for many. ICI therapy can be costly, with most insurance companies not covering bimix or trimix, and typically requiring preparation in specialty compounding pharmacies. PGE1 is the only intracavernosal pharmacotherapy approved by the Food and Drug Administration.21 Although PGE1 might be covered, the common commercial formulas are not easily titrated and this can become cumbersome to many patients. In a survey of 301 physicians on practice patterns and opinions regarding post-prostatectomy ED and penile rehabilitation, although the vast majority (75%) used ICI as part of their rehabilitation regimen, for those who did not, 50% reported cost as being the primary reason.22
This study has several strengths. It represents the first study to our knowledge that prospectively evaluated two different treatment approaches for ICI therapy in men with failed first-line treatment for ED. In addition, validated patient-report questionnaires were used to assess treatment outcome and patient satisfaction. Although objective evaluation of erectile responses by clinicians might have been of interest, subjective patient outcomes were deemed more important and relevant to capture. This study has several limitations. The sample size, although comparable to other published studies, was relatively small and might have been underpowered to detect subtle differences in outcomes between groups. A high patient dropout rate also was noted. There are several possible explanations for this, including successful therapy, which might make follow-up superfluous for the patient. Measures were taken to limit dropout, including calling patients who did not show up for follow-up visits and allowing for returning the questionnaires by email. Another reason for dropout might be treatment dissatisfaction and failure, which could result in patient frustration and possibly abandoning therapy for ED altogether, which has been reported previously.23 Furthermore, if patients are no longer engaging in sexual relations, then this could relate to partner issues, which were not accounted for in this study. The dropout rates seen in this study appear to correlate with those reported in other studies examining patients undergoing ICI therapy9, 18, 19, 22 and have been reported as high as 80%.24
The purpose of this study was not to define the optimal strategy for ICI but to identify treatment regimens that are successful for the patient and the clinician and are easily reproducible. This is especially important because most ICI therapy clinics are often run by mid-level providers who will need guidance and a rationale therapy algorithm. The other aim was to assess whether, of the two approaches used at the Johns Hopkins Hospital, one was more successful than the other in optimizing outcomes and limiting complications. Given the similar efficacy and patient satisfaction rates of the two approaches, this article serves as a guide whereby the final decision can safely and effectively be made at the discretion of the practitioner. With the paucity of literature available on ICI therapy and lack of a standardized approach to administration, this article serves as a guide for sexual medicine specialists and physicians starting an ICI program. More research is necessary to compare other injection combinations and treatment strategies to further delineate the optimal approach to ICI therapy.
Statement of authorship
Category 1
-
(a)Conception and Design
- Helen Levey Bernie; Robert Segal; Brian Le; Arthur Burnett; Trinity J. Bivalacqua
-
(b)Acquisition of Data
- Helen Levey Bernie; Robert Segal; Brian Le; Arthur Burnett; Trinity J. Bivalacqua
-
(c)Analysis and Interpretation of Data
- Helen Levey Bernie; Robert Segal; Brian Le; Arthur Burnett; Trinity J. Bivalacqua
Category 2
-
(a)Drafting the Article
- Helen Levey Bernie; Robert Segal; Brian Le; Arthur Burnett; Trinity J. Bivalacqua
-
(b)Revising It for Intellectual Content
- Helen Levey Bernie; Robert Segal; Brian Le; Arthur Burnett; Trinity J. Bivalacqua
Category 3
-
(a)Final Approval of the Completed Article
- Helen Levey Bernie; Robert Segal; Brian Le; Arthur Burnett; Trinity J. Bivalacqua
Footnotes
Conflicts of Interest: Authors report no conflicts of interest.
Funding: None.
References
- 1.Fang S.C., Rosen R.C., Vita J.A. Changes in erectile dysfunction over time in relation to Framingham cardiovascular risk in the Boston Area Community Health (BACH) survey. J Sex Med. 2015;12:100–108. doi: 10.1111/jsm.12715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ayta I.A., McKinlay J.B., Krane R.J. The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU Int. 1999;84:50–56. doi: 10.1046/j.1464-410x.1999.00142.x. [DOI] [PubMed] [Google Scholar]
- 3.Goldstein I., Lue T.F., Padma-Nathan H. Oral sildenafil in the treatment of erectile dysfunction. Sildenafil Study Group. N Engl J Med. 1998;338:1397–1404. doi: 10.1056/NEJM199805143382001. [DOI] [PubMed] [Google Scholar]
- 4.Yuan J., Zhang R., Yang Z. Comparative effectiveness and safety of oral phosphodiesterase type 5 inhibitors for erectile dysfunction: a systematic review and network meta-analysis. Eur Urol. 2013;63:902–912. doi: 10.1016/j.eururo.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 5.Montague D.K., Jarow J.P., Broderick G.A. Chapter 1: the management of erectile dysfunction: an AUA update. J Urol. 2005;174:230–239. doi: 10.1097/01.ju.0000164463.19239.19. [DOI] [PubMed] [Google Scholar]
- 6.Wespes E., Amar E., Hatzichristou D. EAU guidelines on erectile dysfunction: an update. Eur Urol. 2006;49:806–815. doi: 10.1016/j.eururo.2006.01.028. [DOI] [PubMed] [Google Scholar]
- 7.Carson C.C., Burnett A.L., Levine L.A. The efficacy of sildenafil citrate (Viagra) in clinical populations: an update. Urology. 2002;60(Suppl 2):12–27. doi: 10.1016/s0090-4295(02)01687-4. [DOI] [PubMed] [Google Scholar]
- 8.Brotzman M.L., Trock B.J., Geringer A.M. Clinical efficacy of sildenafil citrate and predictors of long-term response. J Urol. 2003;170:503–506. doi: 10.1097/01.ju.0000071478.69480.fd. [DOI] [PubMed] [Google Scholar]
- 9.Coombs P.G., Heck M., Guhring P. A review of outcomes of an intracavernosal injection therapy programme. BJU Int. 2012;110:1787–1791. doi: 10.1111/j.1464-410X.2012.11080.x. [DOI] [PubMed] [Google Scholar]
- 10.Carvalheira A.A., Pereira N.M., Maroco J. Dropout in the treatment of erectile dysfunction with PDE5: a study on predictors and a qualitative analysis of reasons for discontinuation. J Sex Med. 2012;9:2361–2369. doi: 10.1111/j.1743-6109.2012.02787.x. [DOI] [PubMed] [Google Scholar]
- 11.Braun M., Wassmer G., Klotz T. Epidemiology of erectile dysfunction: results of the ‘Cologne Male Survey’. Int J Impot Res. 2000;12:305–311. doi: 10.1038/sj.ijir.3900622. [DOI] [PubMed] [Google Scholar]
- 12.Goldstein I., Kim E., Steers W.D. Efficacy and safety of tadalafil in men with erectile dysfunction with a high prevalence of comorbid conditions: results from MOMENTUS: Multiple Observations in Men with Erectile Dysfunction in National Tadalafil Study in the US. J Sex Med. 2007;4:166–175. doi: 10.1111/j.1743-6109.2006.00402.x. [DOI] [PubMed] [Google Scholar]
- 13.Montorsi F., Salonia A., Deho F. Pharmacological management of erectile dysfunction. BJU Int. 2003;91:446–454. doi: 10.1046/j.1464-410x.2003.04093.x. [DOI] [PubMed] [Google Scholar]
- 14.Rosen R.C., Riley A., Wagner G. The International Index of Erectile Function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–830. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 15.Porst H., Gilbert C., Collins S. Development and validation of the quality of erection questionnaire. J Sex Med. 2007;4:372–381. doi: 10.1111/j.1743-6109.2006.00422.x. [DOI] [PubMed] [Google Scholar]
- 16.Woodward J.M., Hass S.L., Woodward P.J. Reliability and validity of the Sexual Life Quality Questionnaire (SLQQ) Qual Life Res. 2002;11:365–377. doi: 10.1023/a:1015513228469. [DOI] [PubMed] [Google Scholar]
- 17.Althof S.E., Corty E.W., Levine S.B. EDITS: development of questionnaires for evaluating satisfaction with treatments for erectile dysfunction. Urology. 1999;53:793–799. doi: 10.1016/s0090-4295(98)00582-2. [DOI] [PubMed] [Google Scholar]
- 18.Hsiao W., Bennett N., Guhring P. Satisfaction profiles in men using intracavernosal injection therapy. J Sex Med. 2011;8:512–517. doi: 10.1111/j.1743-6109.2010.02093.x. [DOI] [PubMed] [Google Scholar]
- 19.Seyam R., Mohamed K., Akhras A.A. A prospective randomized study to optimize the dosage of trimix ingredients and compare its efficacy and safety with prostaglandin E1. Int J Impot Res. 2005;17:346–353. doi: 10.1038/sj.ijir.3901313. [DOI] [PubMed] [Google Scholar]
- 20.Thon W.F., Hartmann U. [Effectiveness and safety of cavernous body auto-injection therapy with papaverine/phentolamine. Study group] Urologe A. 1993;32:466–469. [in German] [PubMed] [Google Scholar]
- 21.US Food and Drug Administration Drugs@FDA: FDA approved drug products. http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm?fuseaction=Search.Overview&DrugName=ALPROSTADIL Available at: Accessed August 3, 2015.
- 22.Teloken P., Mesquita G., Montorsi F. Post-radical prostatectomy pharmacological penile rehabilitation: practice patterns among the International Society for Sexual Medicine practitioners. J Sex Med. 2009;6:2032–2038. doi: 10.1111/j.1743-6109.2009.01269.x. [DOI] [PubMed] [Google Scholar]
- 23.Salonia A., Gallina A., Zanni G. Acceptance of and discontinuation rate from erectile dysfunction oral treatment in patients following bilateral nerve-sparing radical prostatectomy. Eur Urol. 2008;53:564–570. doi: 10.1016/j.eururo.2007.08.016. [DOI] [PubMed] [Google Scholar]
- 24.Sung H.H., Ahn J.S., Kim J.J. The role of intracavernosalinjectiontherapyand the reasons of withdrawal from therapy in patients with erectile dysfunction in the era of PDE5 inhibitors. Andrology. 2014;2:45–50. doi: 10.1111/j.2047-2927.2013.00155.x. [DOI] [PubMed] [Google Scholar]