Abstract
Introduction:
This study assessed whether patient portals influence patients’ ability for self-management, improve their perception of health state, improve their experience with primary care practices, and reduce healthcare utilization.
Methods:
Patients participating in a nurse-led care coordination program received personalized training to use the portal to communicate with the care team. Data analysis included pre-post comparison of self-efficacy (CDSES), health state (EQVAS), functional status (PROMIS®), experience with the provider/practice (CG-CAHPS), and healthcare utilization (admissions and ED visits).
Results:
A total of 94 patients were enrolled, and 92 (Intent to Treat) were followed up for 7 months to assess their experience, and for 12 months to assess healthcare utilization. Seventy four (mean age 60+13 years) used the portal (Users). Comparison between baseline and 7-month follow-up showed no statistically significant improvements in self-efficacy, perception of health state or experience with the primary care practice. Only functional status improved significantly. ED visits/1000 patients were reduced by 26% and 21% in the Intent to Treat and Users groups, respectively. Hospital admissions/1000 patients were reduced by 46% in the Intent to Treat group and by 38% in the Users group.
Discussion:
For patients in care coordination, having access to patient portals may improve access to providers and health data that lead to improvements in patients’ functional status and reduce high-cost healthcare utilization, but it does not seem to improve self-efficacy, perception of health state, or experience with primary care practices.
Conclusion:
In this study, the use of patient portals improved functional status and reduced high-cost healthcare utilization in patients with chronic conditions.
Keywords: Delivery of Health Care, Patient-Centered Care, Patient Care Management, Meaningful Use, Patient Portal, Electronic Health Record
Introduction
The diseases that contribute most heavily to death, illness, and disability among Americans have changed dramatically over the past century. Seven of every ten deaths in the United States are due to chronic diseases,1 and recent data suggest that the proportion of Americans with these diseases is increasing, with over half of the nation’s adults suffering from at least one chronic condition.2 The medical care costs of people with chronic diseases accounted for more than 86 percent of the nation’s total health care costs in 20101,3 due to complications resulting in hospitalizations and unnecessary provider visits, many of which were potentially preventable with appropriate care. Studies have indicated that chronic disease patients have many barriers to care, leading to poor management of such diseases,4,5 and that part of the solution includes increasing access to evidence-based programs and promoting patient self-management.5
Self-management of chronic disease has been recognized as a vital method to reduce health care utilization and to prevent disability.13–15 By teaching patients to take responsibility for their own health and coaching them on how to do it, the quality of health care for chronic condition patients can improve. Care coordination has been demonstrated to be effective in improving patient care, especially for those with chronic disease.6–8 Care coordination programs embedded in primary care practices are looking to increase self-management, improve the quality of care of patients, and reduce unnecessary health care utilization.6 Providing patients with a dedicated nurse care coordinator helps facilitate the delivery of care. This individual acts as a support for patients and families who need it most, encouraging and teaching patient self-management, and linking them to services that address the full range of needs and concerns related to their health care. Many primary care practices are adding nurse care coordinators in their offices to help patients develop goals and health care plans and to assist them in navigating through the different care transitions; however, their capacity to reach and coordinate a higher number of patients is limited.9
Health Information Technology (HIT), including patient portals, has the potential to assist care coordination programs in their goal to improve patients’ self-management and ultimately their care.10–13 HIT integrated in the new environment of nurse-led care coordination in primary care could be used as a resource to improve medical care by the following: (1) increasing patients’ self-efficacy for managing their conditions, (2) improving patient health outcomes, (3) reducing unnecessary high-cost health care visits, and (4) reducing administrative costs and time for health care providers.14–16 HIT could potentially help improve outcomes for chronic disease patients by expanding access to primary care and care coordination delivered through web-based patient portals, and could assist care coordination as a sustainable resource. Patient portals allow exchange of health information between health care providers, patients and caregivers, and also have the capacity to provide screening and decision tools necessary for care coordination.16–19 Kobb et al. found that patients with chronic conditions, including the elderly and their caregivers, may be more interested in using this technology than others,7 and that further studies are required in order to understand patient experience and satisfaction with the type and format of information provided and its accessibility and convenience.20 Currently, many health care organizations offer features of a patient portal, but their use is limited and the potential of patient portals to maintain the effect of care coordination and to improve health and patient experience has not been determined conclusively.16,21,22
The Meaningful Use Criteria are a set of requirements related to the adoption of HIT by eligible professionals (EPs) and hospitals that health care organizations must meet in order to qualify for financial incentives from the Center for Medicare and Medicaid Services (CMS) incentive program. Some of the objectives created for the criteria include the following: (1) the use of secure electronic messaging to communicate with patients on relevant health information, and (2) providing patients with the ability to view online, download, and transmit their health information.23 Despite the potential benefits of the use of patient portals to patients, caregivers, and providers and the reimbursement from the U.S. government for patient-centered care, the evidence for the impact of HIT-based programs for chronic disease on outcomes is scarce.24
The purpose of this study was to evaluate whether the use of patient portals by patients with chronic conditions who are participating in a care coordination program can influence patients’ perception of health state, patients’ self-efficacy, patients’ functional status, their experience with the primary care practice, and their health care utilization.
Methods
This is a prospective, quasi-experimental pre-post study design, including an Intent to Treat analysis25,26 to determine the impact of patient portals on enhancing patient experience and improving quality of care. This was accomplished by assessing patient self-efficacy, functional status and health state, experience with the primary care practice, and the potential effects on health care service utilization. Due to the fact that the patient portal was available to all active patients from primary care practices, a randomized design was not possible.
The study was conducted at five primary care practices, certified as Patient-Centered Medical Home practices. Each primary care practice had an established nurse-led care coordination program with one coordinator per primary care practice. Each nurse had a panel of 100–150 chronic-condition patients at any given time. The goals of the care coordination program were the following: (1) to provide efficient, high quality, and cost effective care; (2) to improve outcomes and patients’ experiences of care by providing patient-centered, evidence-based holistic care to the Individuals; (3) to coordinate care of patients across care settings; and (4) to provide education to assist the patients with self-management of their chronic disease.27
All active chronic-condition patients participating in the care coordination program were invited to be enrolled in the study by their assigned nurse care coordinator. Eligible patients were those above the age of 18 years. Caregivers with written release to patient medical information were also eligible to participate in this project. All participants needed to have internet access through either a private or public computer. Care coordination services were defined as those that facilitate treatment of acute and chronically ill patients based on utilization and risks. They are focused on all chronic disease states with an emphasis on high-risk high-cost patients, and on the following chronic conditions: chronic obstructive pulmonary disease (COPD) and asthma, congestive heart failure (CHF) and coronary artery disease (CAD), diabetes, depression in conjunction with any of the previous diagnoses, end stage renal disease (ESRD), and frail or elderly.
Once enrolled, all participants were shown how to access and navigate the portal through one-on-one training by the study staff, and were provided with a self-guided instruction manual. The training lasted approximately 60 minutes, after which participants were directed to call the study staff if they had questions or encountered problems with the portal. All participants were encouraged to communicate with providers, care coordinators, and other office staff by using the portal for nonurgent health issues, scheduling appointments, requesting prescription renewals, obtaining referrals, and asking billing-related questions. Participants were also informed about electronic access to their medical record to find their problem list, medication list, laboratory and radiology reports, and to add pertinent information to their Patient Health Record.
Participants were followed up on 7 months (±1 month) after being introduced to the patient portal, to assess their experience with the portal by collecting all patient-reported metrics. They were asked to complete the study questionnaire, which included the following: Stanford Self-Efficacy for Self-Management of Chronic Disease (CDSES),28 Patient-Reported Outcomes measurement information system (PROMIS) for functional status,29 and EuroQol Group’s EQ 5D EQ visual analogue scale (EQ VAS)30 for health state, as part of a regular wellness questionnaire. The wellness questionnaire took approximately 15 to 20 minutes to complete. Patients completed the questionnaire via the portal at two different time points: enrollment (baseline), and 7 months (± 1 month) post enrollment.
Participants were also followed up on for 12 months after being introduced to the portal to collect health care utilization, including emergency department (ED) visits and hospital admissions using the statewide Health Information Exchange (HIE). This study was approved by the Institutional Review Board, and participants were enrolled after informed consent was obtained. Enrollment occurred between June 2013 and January 2015.
For the purpose of the study, data collection included the following.
Demographic Characteristics at the Date of Enrollment: gender, age, Medicare Part B enrollment, marital status, smoking status, and retiree status.
Portal Use and Adoption: adoption rate, number of days when patients access the portal, and type of use during the study period. Portal use was defined and assessed by using the portal package electronic report (number of days when participants access the portal) and electronic health record (EHR) documentation (number of days participants used the portal for relevant clinical criteria that include all secure email messages sent by the patient to the provider from the date of consent to the date of completion of the follow-up wellness questionnaire).
Health Care Utilization: number of hospital admissions and number of ED visits, obtained from the statewide HIE. This was assessed by examining the number of ED visits and hospital admissions 12 months before and 12 months after the date of study consent.
Patient-Reported Outcomes:
Patient self-efficacy: Chronic Disease Self-Efficacy Efficacy (CDSE) was assessed by utilizing a six-item questionnaire developed by Lorig et al.28 Participants rated their confidence in managing their chronic condition on a score of 1= not confident at all to 10 = totally confident. The overall CDSE score was the mean of all scores in the six items.
Patient functional status: PROMIS Functional Status was assessed by utilizing PROMIS global items. The Global Physical Health score was generated by summing the scores on four physical health items (physical health, physical activities, pain, and fatigue). The Global Mental Health score was generated by summing responses to four mental health related items (quality of life, mental health, social activities, and emotional problems). The simple raw scores were converted to T-scores on each individual. T-score distributions are standardized such that a 50 score represents the average (mean) for the U.S. general population, and the standard deviation around that mean is 10 points. The T-score ranges from 16.2 to 67.7 for physical health and 21.2 to 67.6 for mental health.
Patient self-rated health state: EQ VAS was measured using a single item EuroQol Visual Analogue Scale. The scale ranges from 0 (worst imaginable health) to 100 (best imaginable health).
Patient Experience with the Primary Care Practice: evaluated using AHRQ’s Clinician & Group Survey of Adult Primary Care 1.0 (CG-CAHPS) survey. Participants took the CG CAHPS survey at baseline (at the time of enrollment) and at the 7 months (± 1 month) follow-up. The CG-CAHPS survey can be analyzed by calculating the six composite scores to assess: (1) getting timely appointments, care, and information; (2) how well providers communicate with patients; (3) how helpful, courteous, and respectful the office staff were; (4) patients’ rating of the provider; (5) whether provider’s office followed up with test results; and (6) patients’ willingness to recommend the provider. The CG-CAHPS also produces top box scores (proportion of patients responding with an “always” for each item on the composites). All items, except the overall provider rating question on the CG-CAHPS survey, were rated on a four-point Likert scale as Never, Sometimes, Usually, or Always. The overall provider rating was scored on a scale of 1–10 with 0 being the worst and 10 being the best.
For the analysis, the following Patient-Reported Outcomes related to self-management and quality of care were used as primary endpoints: (1) self-efficacy (CDSES),28 (2) functional status (PROMIS),29 and (3) health state (EQ VAS).30 Secondary endpoints included the following: (1) patient experience with the primary care practice using the CG-CAHPS,31 and (2) health care utilization including hospital admissions and ED visits.
Portal “Users” were defined as “those patients participating in the care coordination program who signed up to use the portal, accessed it, completed the protocol assessments through the portal, and communicated with their provider or care coordinator through the portal, as identified by the portal software report.” “Nonusers” were defined as “patients participating in care coordination who signed up to use the portal, but neither completed the assessments nor communicated with the care provider through the portal.” The Intent to Treat group included both Users and Nonusers. Analysis was conducted using data collected from participants in the Users and Intent to Treat groups. Due to small sample size among the Nonusers group, data on this group were not included.
Data were obtained from the following: (1) the electronic medical records reports on the forms filled by participants using the portal, (2) patient experience surveys, and (3) the statewide HIE. All data were transferred to SPSS version 2132 for analysis. Analysis was dedicated to pre-post comparisons of Intent to Treat and Users groups. Paired t-tests were used to compare pre- and post means of the composites score on CDSES, PROMIS, and Self Health Rating variables. To draw meaningful interpretations from the health care utilization measures that did not show normal distribution, ED visits and hospital admissions were reported as the following (1) pre-post difference in the proportion of patients requiring ED visits and hospital admissions for all causes, and (2) the number of ED visits and hospital admissions per 1,000 patients. For patient experience, all five composite scores on CG-CAHPS were not calculated due to the responses to individual items in each of the composites having highly unequal and small sample sizes. Hence, we decided to focus the assessment on item-by-item analysis of top-box scores. Top-box scores were used to measure pre-post differences in proportion of responses on each of the 18 items on CG-CAHPS (outcome: binomial percentage who responded as “always” versus “not always”). McNemar’s test for paired proportions was used to assess the difference between before and after in the item analysis of the CG-CAHPS survey to assess patient satisfaction. Results are reported as confidence intervals of the difference in proportions. Lower and upper limits of the 95 percent confidence interval were estimated for a proportion difference, without a correction for continuity.
Results
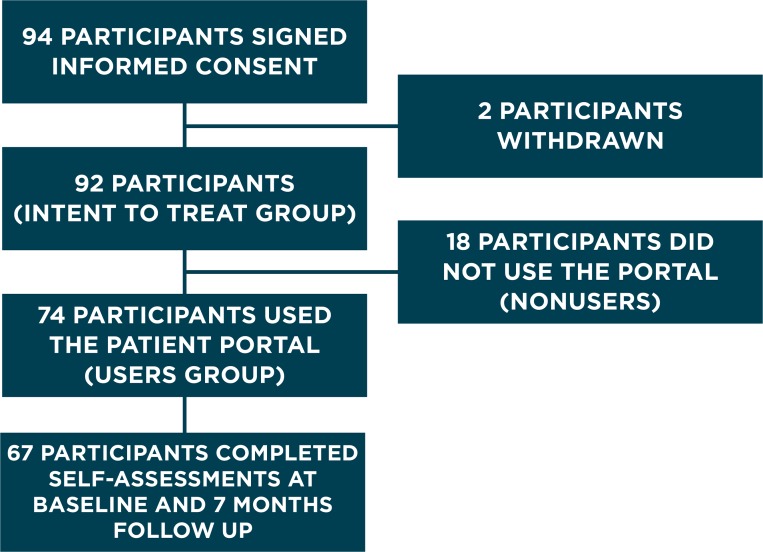
A total of 94 patients provided informed consent to participate in the study. Two withdrew at the beginning of the study due to concerns about privacy and connections with the Affordable Care Act. Ninety-two participants were included in the analysis and were defined as the Intent to Treat group (Figure 1). The mean age was 60±13 years, 99 percent were white or non-Hispanic, and 71 percent were female. As shown in Table 1, 70 percent of participants reported having some college or technical education, 59 percent were retired at the time of enrollment, and 64 percent were enrolled in Medicare. Although Table 1 showed apparent differences between Intent to Treat and Users groups for Medicare Part B enrollees, the sample is not large enough to demonstrate statistically significant differences between Users and Nonusers. All participants were primary care patients who were in active care coordination for an average of 15 months, with a range between 1 to 70 months. Participants were in care coordination primarily with the following chronic illnesses: diabetes (41 percent), asthma (15 percent), depression (13 percent), chronic obstructive pulmonary disease (11 percent), heart failure (11 percent), and coronary artery disease (5 percent). Before enrollment, 70 percent of the participants did not use the portal. After enrollment, approximately 80 percent of the enrolled participants accessed the portal, and most of the usage was related to sending secure messages (48 percent), requesting medication refills (34 percent), checking laboratory results (23 percent), and changing appointments (15 percent).
Figure 1.
Enrollment of Study Participants
Table 1.
Demographic Characteristics of Intent to Treat and Users of the Portal
| INTENT TO TREAT (n=92) | USERS (n=74) | |
|---|---|---|
| Females (%) | 71 | 72 |
| Age (Mean ± SD) | 59.6 ± 13.1 | 59.9± 12.6 |
| Medicare Part B (%) | 64 | 49 |
| Married (%) | 49 | 51 |
| Smokers (%) | 57 | 53 |
| Retired (%) | 59 | 55 |
| College Education (%) | 70 | 77 |
| White (race) (%) | 99 | 99 |
| Non-Hispanic/Latino (%) | 100 | 100 |
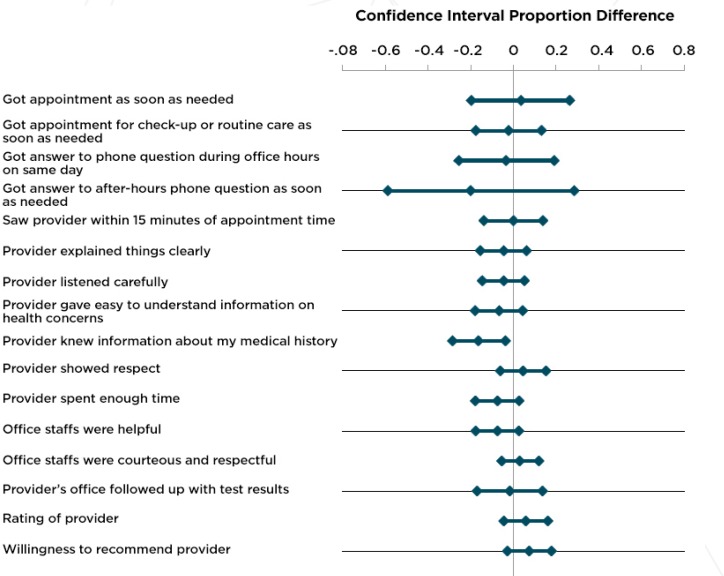
Of the 92 participants in the Intent to Treat group, 74 were Users (80 percent) and only 18 (20 percent) were Nonusers (Figure 1). While the Intent to Treat group showed improvements in all Patient-Reported Outcomes, only the unadjusted mental health component of the participants’ Global functional status improved significantly (49.2 ± 7.6 versus 50.9 ± 8.0, p= 0.035). There were no significant differences in self-efficacy and self-health state rating (Table 2), or in patient experience with primary care practices (Figure 2). Similar results were seen in the pre-post analysis for the Users group, where all Patient-Reported Outcomes improved slightly, but only statistically significant improvements were seen for both components of the functional status, Global mental health component (49.1 ± 7.8 versus 51.1 ± 8.2, p= 0.027) and physical health component (45.1 ± 7.3 versus 46.5 ± 7.6, p= 0.046) (Table 2).
Table 2.
Patient-Reported Outcomes: before and after Portal Use in the Intent to Treat and Users Groups
| OUTCOME MEASURES | n | AT BASELINE MEAN ± SD | AT 7-MONTHS MEAN ± SD | MEAN DIFFERENCE 95% CI | P-VALUE* |
|---|---|---|---|---|---|
| INTENT TO TREAT | |||||
| Self-Efficacy€ | 72 | 7.59 ± 2.1 | 7.68 ± 2.0 | +0.09 (−0.54, 0.35) | 0.665 |
|
| |||||
| Physical Health☼ | 72 | 45.16 ± 7.3 | 46.2 ± 7.8 | +1.1 (−2.5, 0.26) | 0.124 |
|
| |||||
| Mental Health¥ | 72 | 49.2 ± 7.6 | 50.9 ± 8.0 | +1.7 (−3.4, −0.13) | 0.035 |
|
| |||||
| EQVAS£ | 72 | 75.3 ± 16.5 | 76.1 ± 17.7 | +0.84 (−4.7, 3.0) | 0.666 |
| USERS | |||||
| Self-Efficacy€ | 67 | 7.63 ± 2.1 | 7.66 ± 2.1 | +0.03 (−0.49, 0.42) | 0.880 |
|
| |||||
| Physical Health☼ | 67 | 45.1 ± 7.3 | 46.5 ± 7.6 | +1.4 (−2.8, −0.02) | 0.046 |
|
| |||||
| Mental Health¥ | 67 | 49.1 ± 7.8 | 51.1 ± 8.2 | +1.9 (−3.7, −0.23) | 0.027 |
|
| |||||
| EQVAS£ | 67 | 74.2 ± 16.5 | 75.9 ± 17.7 | +1.7 (−5.7, 2.3) | 0.406 |
Notes:
Paired samples t-test;
Chronic Disease Self-efficacy (1–10, higher = better);
PROMIS Global Physical Health T-score (16.2–67.7, higher = better);
PROMIS Global Mental Health T-score (21.2–67.6, higher = better);
EQVAS: Self Health State (1–100, higher = better).
Figure 2.
Patient Experience from CG-CAHPS Survey: Top Box Scores of Participants Responding “Always” for the Users Group (n=68)
The data source for health care utilization was the statewide HIE. The percentage of patients with more than 1 ED visit between the 12 months prior to using the portal and the 12 months after using the portal was reduced by 25 percent in the Intent to Treat group, and 20 percent in the Users group (Table 3). The number of ED visits per 1,000 patients was reduced by 26 percent among the Intent to Treat group (from 1,034 to 764), and 21 percent among the Users group (from 770 to 609). The percentage of patients with one or more hospital admissions was reduced by 32 percent and 30 percent among the Intent to Treat and Users groups, respectively. Hospital admissions per 1,000 patients were reduced in both groups by 46 percent and 38 percent, respectively (Table 3).
Table 3.
Health Care Utilization by Different Participant Groups: Intent to Treat and Users Groups. Changes over 12 Month Period
| INTENT TO TREAT (n= 92) | |||
|---|---|---|---|
| ED VISITS | 12 MONTHS BEFORE PORTAL USE | 12 MONTHS AFTER PORTAL USE | CHANGE |
| Patients with 1 or more ED Visit | 60% | 35% | −25% |
|
| |||
| Number of ED Visits per 1,000 Patients | 1032 | 764 | −268 |
| HOSPITAL ADMISSIONS | |||
| Patients with 1 or more Hospital Admission | 58% | 29% | −32% |
|
| |||
| Number of Hospital Admissions per 1,000 Patients | 891 | 480 | −411 |
| USERS (n=74) | |||
|---|---|---|---|
| ED VISITS | BEFORE | AFTER | CHANGE |
| Patients with 1 or more ED Visits | 47% | 27% | −20% |
|
| |||
| Number of ED visits per 1,000 Patients | 770 | 609 | −161 |
| HOSPITAL ADMISSIONS | |||
| Patients with 1 or more Hospital Admissions | 61% | 31% | −30% |
|
| |||
| Number of Hospital Admissions per 1,000 Patients | 783 | 487 | −296 |
Conclusion
In this study, the use of a patient portal among patients with chronic conditions enrolled in a care coordination program did not demonstrate a statistically significant improvement in self-efficacy, perception of health status, or patients’ experience with their primary care practice after 7 months of patient portal use. Self-reported functional status was the only outcome measure to improve significantly. The study also showed an overall reduction of annual health care utilization, ED visits, and overall hospital admissions, when compared with the year prior to enrollment. More research is needed to address the potential effects of patient portals on high-cost health care utilization and to better understand their effect on functional status.
Discussion
Over the past several years, health care organizations have implemented targeted efforts to facilitate physician practice change. These include new HIT and care coordination programs in primary care practices designed to improve the quality of care, enhance the patient experience, and ultimately reduce the cost of care by reducing unnecessary high-cost health care utilization. In this project, Patient-Reported Outcomes (self-efficacy, functional status, and self-rated health state) were used as proxies to measure improvements in quality of care. Moreover, CG-CAHPS was used as a proxy for patient experience, and health care utilization (reduction of hospital admissions and ED visits) was used as a proxy for reduction of health care cost. It was hypothesized that the use of HIT, specifically patient portals, could increase patient self-efficacy and subsequently leads to improvements in quality of care, patient experience, and health care utilization. In this study, the use of the patient portal did not influence Patient-Reported Outcomes—with the exception of small changes in functional status. These changes could be attributable to the length of time the participants were in care coordination and to the continuity of care the participants experienced.
Patient self-efficacy was introduced by Lorig et al., who have advanced knowledge about the benefits of self-management programs in improving the health care of chronic disease patients.28,33,34 Studies have shown that standardized self-management programs can significantly reduce health distress, disability, and health care utilization compared to usual care.35 A meta-analysis36 found that self-management programs can improve the health status of patients with chronic disease; for example, self-management was more effective than usual care in reducing HbA1c and blood pressure for patients with various chronic conditions.13 Based on this evidence, adding HIT, such as a patient portal, to current care coordination programs is a useful tool that has the potential to facilitate improvements not only in self-management, but also in quality of care, patient experience, and indirectly on cost by reducing high-cost health care utilization. Patient portals are also seen as viable tools to improve patient communication and experience with providers, and give patients and caregivers the opportunity to have access to more health information when needed.
Among the specific population of chronic-conditions patients currently using care coordination services who participated in this study, the findings suggest that having access to patient portals may not have a significant effect on self-efficacy, perception of health state, or patient experience with the primary care provider and the provider’s office. It does, however, appear to improve functional status and potentially reduce health care utilization. This could be due to the fact that, for patients in care coordination, a patient portal improves access to providers and health data at the time patients need it.
This study did not show the expected changes in self-efficacy and self-reported health state, and this may be attributable to the fact that the patient population scored very high on these outcomes at baseline.35 More than 63 percent of participants had been in care coordination 6 months or longer, which could explain the high self-efficacy observed at baseline. Although all metrics improved after 7 months, the follow-up was not long enough to identify statistically significant differences.
Another limitation of this study was that the portal was already available to all primary care patients, which made it impossible to use a randomization design. In addition, the interest in using the portal was lower than anticipated. In the community studied, patient portals for chronic condition patients, who tend to be an older population, may not be the preferred method of communication regarding their health care. Although communication between patients and health care providers represented the higher use of the portal among the studied group, the overall number of Users was very small across our health care system (1.4 percent). Another limitation that cannot be underestimated was attributable to the technology itself. Technical difficulties were encountered throughout this study during actual portal use. These difficulties occurred every time the portal system was upgraded, and resulted in study participants being unable to complete the study assessments. Overall limitations include the small sample size, the quasi-experimental design, and the lack of diversity in the population.
Further studies might assess the differences between Users and Nonusers of patient portals, with and without care coordination, as well as adding a mixed-methods evaluation design to assess specific aspects of portals and patients’ preferences for how portals are accessed and used. This would address the effect of any confounding factors, such as length of time in care coordination.
The study findings suggest that although patient portals might help to improve outcomes in patients in care coordination programs, they may not be suitable for all patients, and that there is still a need to make portals more user friendly for providers, office staff, and patients.37 Moreover, although we did not find statistically significant differences between users of the portal and those who are not using it, it is possible that portal use is based more on accessibility, i.e., the portal is only available to those patients who have greater resources. Use of portals has implications for office workflow, which could be an issue that limits their use in primary care practices, by providers and care coordinators, as described in our previous study.37
Patient experience with the health care provider and office staff did not differ significantly before using the portal and 7 months after using the portal among the Users and Intent to Treat groups. This could be attributed to sporadic use of the portal limiting the ability to identify differences at 7 months post enrollment, or that the use of the portal is not considered by patients as relevant to their care. A qualitative study will be appropriate to address this issue. Changes in all CG CAHPS questions were not expected, as some of them do not refer to any HIT or portal activity specifically. However, three trends that could be related to the use of the portal and improved access to health care information were identified. Although not statistically significant, the results showed the following: (1) an improvement in the overall rating of the provider, (2) an improvement in the willingness to recommend the provider, and (3) a decrease in patient perception that providers know important information about their medical history. Patients’ positive perception of their providers may be influenced by the patients’ experience using the portal to communicate with them. A previous study showed that patients were pleased with the rapid responses and support they received from their providers and care coordinators when using patient portals.37 However, expanding access to the portal may have increased patients’ expectations that providers would know their medical history and concerns in more detail than was perceived during their office visit. This expectation of more knowledge may have affected the lack of improvement of the patients’ experience, as shown in Figure 2.
Health care utilization decreased in both the Intent to Treat and Users groups. Access to the portal may improve access to health care providers and, in turn, reduce the need for unscheduled high-cost health care utilization. Although the Intent to Treat group had a greater decrease in ED visits than the Users group, their overall ED utilization was higher both before and after portal use, indicating that the Nonusers may have contributed to the greater utilization. However, a comparison analysis was not possible due to the low number of Nonusers. Further research is needed with a larger sample, in which a control group can be identified, and participants followed for a longer period.
Acknowledgments
This project was supported by grant number R21HS021005 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. We thank the implementation and operational team who made this project possible. Special thanks to Michael Rocque and Sharon LaBrie for initial data design and project management, Lori Newcomb and the care coordinators from EMHS Beacon Health for participating in the project and using the portal, the IS departments at EMMC and EMHS, Matthew Ferrante from Instant Medical History™ for creating the interfaces, and all the staff at the EMMC Clinical Research Center for their dedication and assistance during the project design and implementation.
Footnotes
Disciplines
Health and Medical Administration | Health Information Technology
References
- 1.Centers for Disease Control and Prevention Chronic Disease Prevention and Health Promotion 2015 [updated August 24, 2015. cited 2015 August 26]. Available from: http://www.cdc.gov/chronicdisease/index.htm.
- 2.Centers for Disease Control and Prevention Chronic Diseases: The Leading Causes of Death and Disability in the United States 2015 [updated May 18, 2015. cited 2015 August 26]. Available from: http://www.cdc.gov/chronicdisease/overview/.
- 3.Gerteis J, Izrael D, Deitz D, LeRoy L, Ricciardi R, Miller T, et al. Multiple Chronic Conditions Chartbook[PDF-1062 MB] AHRQ Publications No, Q14-0038. Rockville, MD: Agency for Healthcare Research and Quality; 2014. [Google Scholar]
- 4.Wagner E. Managed Care and Chronic Illness: Health Services Research Needs. Health Serv Res. 1997;32(5):702. [PMC free article] [PubMed] [Google Scholar]
- 5.Wagner EH. Chronic Disease Management: What Will it Take to Improve Care for Chronic Illness? Effective Clinical Practice: ECP. 1997;1(1):2–4. [PubMed] [Google Scholar]
- 6.Peters SG, Bunkers KS. Chronic Care Coordination. Chest Journal. 2015 doi: 10.1378/chest.15-0704. [DOI] [PubMed] [Google Scholar]
- 7.Kobb R, Hoffman N, Lodge R, Kline S. Enhancing Elder Chronic Care through Technology and Care Coordination: Report from a Pilot. Telemed J E Health. 2003;9(2):189–95. doi: 10.1089/153056203766437525. [DOI] [PubMed] [Google Scholar]
- 8.Bayliss EA, Balasubramianian BA, Gill JM, Stange KC. Perspectives in Primary Care: Implementing Patient-Centered Care Coordination for Individuals with Multiple Chronic Medical Conditions. Annals of Family Medicine. 2014 Nov-Dec;12(6):500–3. doi: 10.1370/afm.1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laughlin CB, Beisel M. Evolution of the Chronic Care Role of the Registered Nurse in Primary Care. Nurs Econ. 2010;28(6):409. [PubMed] [Google Scholar]
- 10.Tulu B, Trudel J, Strong DM, Johnson SA, Sundaresan D, Garber L. Patient Portals: An Underutilized Resource for Improving Patient Engagement. Chest. 2015 Jun 11; doi: 10.1378/chest.14-2559. [DOI] [PubMed] [Google Scholar]
- 11.Turner A, Osterhage K, Joe J, Hartzler A, Lin L, Demiris G. Use of Patient Portals: Personal Health Information Management in Older Adults. Stud Health Technol Inform. 2015;216:978. [PubMed] [Google Scholar]
- 12.Kruse CS, Argueta DA, Lopez L, Nair A. Patient and Provider Attitudes toward the Use of Patient Portals for the Management of Chronic Disease: A Systematic Review. J Med Internet Res. 2015;17(2):e40. doi: 10.2196/jmir.3703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Irizarry T, DeVito Dabbs A, Curran CR. Patient Portals and Patient Engagement: A State of the Science Review. J Med Internet Res. 2015;17(6):e148. doi: 10.2196/jmir.4255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dorr D, Bonner LM, Cohen AN, Shoai RS, Perrin R, Chaney E, et al. Informatics Systems to Promote Improved Care for Chronic Illness: A Literature Review. J Am Med Inform Assoc. 2007;14(2):156–63. doi: 10.1197/jamia.M2255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Allen A, Des Jardins TR, Heider A, Kanger CR, Lobach DF, McWilliams L, et al. Making It Local: Beacon Communities Use Health Information Technology to Optimize Care Management. Population Health Management. 2014;17(3):149–58. doi: 10.1089/pop.2013.0084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rigby M, Georgiou A, Hypponen H, Ammenwerth E, de Keizer N, Magrabi F, et al. Patient Portals as a Means of Information and Communication Technology Support to Patient-Centric Care Coordination - the Missing Evidence and the Challenges of Evaluation. A joint contribution of IMIA WG EVAL and EFMI WG EVAL. Yearb Med Inform. 2015 Aug 13;10(1):148–59. doi: 10.15265/IY-2015-007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Casalino L, Gillies RR, Shortell SM, Schmittdiel JA, Bodenheimer T, Robinson JC, et al. External Incentives, Information Technology, and Organized Processes to Improve Health Care Quality for Patients with Chronic Diseases. JAMA. 2003;289(4):434–41. doi: 10.1001/jama.289.4.434. [DOI] [PubMed] [Google Scholar]
- 18.Terry K. Patient Portals. Essential, but Underused by Physicians. Med Econ. 2015 May 10;92(9):43–7. [PubMed] [Google Scholar]
- 19.Drasnin J. With Patient Portals, Doctors Win Too. Health Manag Technol. 2015 Jul;36(7):21. [PubMed] [Google Scholar]
- 20.Barron J, Bedra M, Wood J, Finkelstein J. Exploring Three Perspectives on Feasibility of a Patient Portal for Older Adults. Integrating Information Technology and Management for Quality of Care. 2014;202:181. [PubMed] [Google Scholar]
- 21.Kruse CS, Bolton K, Freriks G. The Effect of Patient Portals on Quality Outcomes and Its Implications to Meaningful Use: A Systematic Review. J Med Internet Res. 2015;17(2):e44. doi: 10.2196/jmir.3171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ammenwerth E, Schnell-Inderst P, Hoerbst A. The Impact of Electronic Patient Portals on Patient Care: A Systematic Review of Controlled Trials. J Med Internet Res. 2012;14(6) doi: 10.2196/jmir.2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Office of the National Coordinator How to Attain Meaningful Use [updated January 15, 2013. cited 2015 August 26]. Available from: http://www.healthit.gov/providers-professionals/how-attain-meaningful-use.
- 24.Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, et al. Systematic Review: Impact of Health Information Technology on Quality, Efficiency, and Costs of Medical Care. Ann Intern Med. 2006;144(10):742–52. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 25.Gupta SK. Intention-to-Treat Concept: A Review. Perspect Clin Res. 2011;2(3):109. doi: 10.4103/2229-3485.83221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Newell DJ. Intention-to-treat analysis: implications for quantitative and qualitative research. Int J Epidemiol. 1992;21(5):837–41. doi: 10.1093/ije/21.5.837. [DOI] [PubMed] [Google Scholar]
- 27.Ehrlich C, Kendall E, Muenchberger H. Practice-based Chronic Condition Care Coordination: Challenges and Opportunities. Australian Journal of Primary Health. 2011;17(1):72–8. doi: 10.1071/PY10053. [DOI] [PubMed] [Google Scholar]
- 28.Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of A Self-management Program on Patients with Chronic Disease. Effective Clinical Practice: ECP. 2000;4(6):256–62. [PubMed] [Google Scholar]
- 29.Hays RD, Bjorner JB, Revicki DA, Spritzer KL, Cella D. Development of Physical and Mental Health Summary Scores from the Patient-reported Outcomes Measurement Information System (PROMIS) Global Items. Qual Life Res. 2009;18(7):873–80. doi: 10.1007/s11136-009-9496-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Group TE. EuroQol-A New Facility for The Measurement of Health-related Quality of Life. Health Policy. 1990;16(3):199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 31.U.S. Agency for Healthcare Research and Quality Clinician and Group- Consumer Assessment of Healthcare Providers and Systems (CG-CAHPS) Available from: https://www.cahps.ahrq.gov/surveys-guidance/cg/index.html.
- 32.IBM Corp . IBM SPSS Statistics for Windows. 21 ed. Armonk, NY: IBM Corp; 2012. [Google Scholar]
- 33.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient Self-management of Chronic Disease in Primary Care. JAMA. 2002;288(19):2469–75. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 34.Holman H, Lorig K. Patient Self-management: A Key to Effectiveness and Efficiency in Care of Chronic Disease. Public Health Rep. 2004;119(3):239. doi: 10.1016/j.phr.2004.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lorig KR, Ritter P, Stewart AL, Sobel DS, Brown BW, Jr, Bandura A, et al. Chronic disease Self-Management Program: 2-year Health Status and Health Care Utilization Outcomes. Med Care. 2001;39(11):1217–23. doi: 10.1097/00005650-200111000-00008. [DOI] [PubMed] [Google Scholar]
- 36.Chodosh J, Morton SC, Mojica W, Maglione M, Suttorp MJ, Hilton L, et al. Meta-analysis: Chronic Disease Self-management Programs for Older Adults. Ann Intern Med. 2005;143(6):427–38. doi: 10.7326/0003-4819-143-6-200509200-00007. [DOI] [PubMed] [Google Scholar]
- 37.Sorondo B, Allen A, Bayleran J, Doore S, Fathima S, Sabbagh I, et al. Using a Patient Portal to Transmit Patient Reported Health Information into the Electronic Record: Workflow Implications and User Experience. eGEMs. 2016;4(3) doi: 10.13063/2327-9214.1237. [DOI] [PMC free article] [PubMed] [Google Scholar]