Abstract
African American neighborhoods have been historically targeted for urban renewal projects, which impact social composition and resident’s health. The Hill District in Pittsburgh, PA is such a neighborhood. This research sought to investigate the extent to which social networks and perceived neighborhood social cohesion and safety were associated with psychological distress among residents in an African American neighborhood undergoing urban renewal, before the implementation of major neighborhood changes. Findings revealed a modest, significant inverse association between social network size and psychological distress (β=−0.006, p<0.01), even after controlling for age, employment, education and income. Perceived neighborhood safety predicted decreased psychological distress (β=−1.438, p<0.01), but not social cohesion, which is consistent with past research. Findings suggest that social networks protect against psychological distress, but neighborhood perceptions are also paramount.
Keywords: Psychological distress; African-Americans; perceived neighborhood social cohesion; perceived neighborhood safety; Pittsburgh, PA
Introduction
United States urban renewal efforts, or initiatives focused on revitalization or regeneration of urban areas, experienced a major shift in focus during the 1950s as a result of the Housing Act which targeted federal funds to areas within large urban cities perceived as “blighted” (Johnstone, 1958). Many of these blighted areas slated for renewal involved business relocation, structure demolition, relocation of residents, and use of eminent domain, or the government purchase of property for public purpose (Sutton, 2008). Urban scholars identified these efforts as a critical force that shaped many African American communities across the country; many of the neighborhoods facing urban renewal were once vibrant hubs of African American life (Fullilove, 2001). One such community is the Hill District in Pittsburgh, PA, once considered Pittsburgh’s cultural center of African-American life in the area. Historical accounts of the Hill District prior to urban renewal policies enacted in the 1950s depict a strong community, with high levels of social cohesion and trust; neighbors knew one another and it was common for children to run through street blocks and play at neighborhood playgrounds unattended (Fullilove, 2004). Reciprocity between neighbors and strong social networks were also prevalent features of this neighborhood’s social environment (Fullilove, 2004). However, starting in the 1950s, revitalization efforts included construction of the Pittsburgh civic arena which displaced over 8,000 Hill District residents and resulted in a substantial loss of economic infrastructure and a depletion of the population (Damewood & Young-Laing, 2011). Today, the Hill District is one of the most distressed neighborhoods in Pittsburgh, with 41% of residents with household incomes below the poverty line (Rebuilding Together).
In addition to economic devastation, recent scholarship on the impact of such activity in the Hill District reveals a traumatic stress reaction upon those who experienced displacement, with themes of grief and social isolation evident in residents’ narratives (Fullilove, 2005). Indeed, prior research indicates that there are associations between characteristics of the neighborhoods in which people live and adverse psychological outcomes (Mair, Diez Roux, & Galea, 2008; Mair, Kaplan, & Everson-Rose, 2012; Pickett & Pearl, 2001). However, there is a paucity of evidence on neighborhood features that are most relevant to the trajectory of psychological outcomes among low-income African American adults—a segment of the population that is disproportionately exposed to such noxious neighborhood features. An exception is qualitative evidence from Flint Michigan which highlighted the impact of the physical environment on residents’ perceptions of fears and decreased sense of security (Johansen, Neal, & Gasteyer, 2015). Other work assessing neighborhood effects on mental health among African Americans mostly focuses on children and adolescents (Caughy, O'Campo, & Muntaner, 2003; Fitzpatrick, Piko, Wright, & LaGory, 2005; Forehand & Jones, 2003; Simons et al., 2002; Stevenson, 1998), and other studies of adult populations exclude men (Cutrona et al., 2005; Cutrona, Russell, Hessling, Brown, & Murry, 2000). Studies among African American women show that lower levels of social cohesion and economic disadvantage are associated with psychological distress and depression (Cutrona, et al., 2005; Cutrona, et al., 2000). Longitudinal studies such as the Detroit Neighborhood Health Study (DNHS), and randomized control trials such as the Moving to Opportunity study suggest neighborhood characteristics (e.g., poverty levels) are associated with a number of mental health outcomes (e.g., posttraumatic stress disorder, depressive symptoms, and distress/anxiety) thus providing critical evidence for a causal relationship between neighborhoods and mental health (Johns et al., 2012; Leventhal & Brooks-Gunn, 2003).
On the other hand, research on social and family ties--and social networks more generally-- demonstrate their importance for African Americans’ ability to cope and adapt in the face of social stressors (e.g., social stigma, discrimination) (Chatters, Taylor, Woodward, & Nicklett, 2015; Levine, Taylor, Nguyen, Chatters, & Himle, 2015; Taylor, Chae, Lincoln, & Chatters, 2015). Indeed, research on a large representative sample of African Americans and White adults found that African Americans demonstrated a higher degree of social embeddedness compared to their White counterparts (Snowden, 2001). Specifically, relative to white men and women, African American men and women were more likely to be visited by friends per week, and African American women were more likely to attend churches, clubs, and other groups than their white counterparts. Compared with whites, African American men whose friends visited frequently were also less likely to report psychological symptoms of distress (Snowden, 2001). Other studies report more frequent contact between social network members among African Americans compared to whites; however, their network size was smaller and composition tends to be more homogenous (Ajrouch, Antonucci, & Janevic, 2001). Sizes of network and homogeneity, in turn, have been found to be key predictors of a myriad of mental outcomes among racially diverse samples (Levine, et al., 2015; Taylor, et al., 2015). Finally, social networks and perceived features of neighborhood cohesion are shown to have health implications (Boessen et al., 2014; De Jesus, Puleo, Shelton, & Emmons, 2010; Moore et al., 2011).
Our study sought to build upon this previous scholarship during a period in which the Hill District is at a pivotal time, on the cusp of experiencing dramatic neighborhood changes in its redevelopment. In contrast to past efforts, the Hill District is part of a large community development planning process coordinated by the City of Pittsburgh and the Pittsburgh Urban Redevelopment Authority with goals to revitalize and redevelop the neighborhood while enabling residents to help with decision-making, planning, and implementation of the renovation. Plans have included opening a new full-service supermarket (October 2013), renovation of 4 playgrounds and a $160 million redevelopment project that involves replacing a large public housing project with mixed-income housing; commercial development of “Main Street”; and community-wide neighborhood clean-up projects (e.g., removal of graffiti, reclamation of vacant properties). Our team had the opportunity to measure network size and diversity, perceptions of neighborhood, and psychological distress prior to the start of these dramatic neighborhood changes. Based on the literature above, we hypothesized that social network features (i.e., size, diversity) would be inversely associated with psychological distress among residents (hypothesis 1). Further, we hypothesize that social networks and cohesion would be most relevant for those with perceived lack of neighborhood safety (hypothesis 2), as others have found an interaction effect between social cohesion and perceived neighborhood conditions (Bjornstrom, Ralston, & Kuhl, 2013).
Methods
Study design and sample
This analysis uses baseline data from the Pittsburgh Hill/Homewood Research on Eating, Shopping and Health (PHRESH) and the Pittsburgh Hill/Homewood Research on Neighborhood Exercise and Health (PHRESH-Plus) studies, both of which focused on a randomly selected cohort of low-income, predominantly African American residents living two very similar low-income predominantly African American neighborhoods: the Hill District and Homewood neighborhoods. Homewood, approximately the same geographic size as the Hill District, is located about four miles from the Hill District, and was selected so that for measures over time – we could distinguish between the impact of secular changes (i.e., changes that may have occurred over time, but unrelated to the specific renovations such as the new full-service supermarket) at the neighborhood-level. The study will have measures of psychological distress from the cohort before and after the neighborhood renovations, however, this analysis only uses the measurement at baseline because follow-up is currently ongoing.
Study participants were recruited from a random sample of households drawn from a complete list of residential addresses generated by the Pittsburgh Neighborhood and Community Information System in both communities (see Dubowitz et al., 2015, for a detailed description of sampling procedures). Eighteen trained data collectors who themselves were neighborhood residents went door-to-door to enroll households following local publicity in church bulletins, community-based organizations and groups, posters in businesses, and postcards that were mailed to each of the randomly selected addresses. This analysis uses data collected from 2013 where 1,321 households were re-contacted (they had been interviewed in 2011) and asked to participate in another in-person survey interview. Of those households, 1,190 were eligible to participate, and 1,253 (84%) households completed questionnaires. All study protocols were approved by the RAND Human Subjects Protection Committee.
Measures
Predictor: Social Network Size
To assess the size of participants’ social networks, we asked them to think of all the people whom they know, and who know them, and whom they have had regular contact with in the past six months. The contact could be face-to-face, by phone or mail, or on the Internet. Based on these criteria for defining members of their social network, participants were asked to enumerate the number of social network members they had in each of the following categories: (1) Family members (immediate family, birth family, spouse, in-laws) (2) close friends (3) Co-workers (4) Neighbors (5) People who are in your religious community or attend the same place of worship (e.g., church) (6) Others (e.g., people you know through recreational activities, etc.). The number of people in each category was summed to compute each participant’s social network size. Finally, we used frequencies to recode implausible values within each category (n=9 for family; n=1 for close friends; n=1 for co-workers; n=1 for neighbors; n=0 for religious community; n=1 for others). For example, for the “close friends” category we recoded 1 individual from 150 to 110 given that all other respondents reported up to 110 friends.
Predictor: Social Network Diversity
To measure the extent to which participants’ social networks were comprised of diverse role categories of network members (i.e., diverse mix of family, friends, coworkers etc.) we used the formula in Blau’s index of diversity (Blau, 1977) (also known as Simpson’s Diversity Index) (Simpson, 1949), which has been recently applied to diverse, ethnic, urban populations (Negrón, 2014). Specifically, the index is calculated by , where p is the proportion of network members in a given category and i is the number of different categories of network member roles (i = 6). Higher levels of diversity of network member roles result in scores approaching, 1 whereas scores approaching 0 denote low levels of diversity in roles. However, when i=6, the maximum possible value of this measure is 0.833.
Outcome: Psychological Distress
Psychological distress was measured with the K6, a validated six-item scale developed to efficiently predict serious mental illness as determined by a fully structured clinical diagnostic interview, the Structured Clinical Interview for DSM-IV (SCID) (Kessler et al., 2003). Questions asked respondents to report how frequently they experienced symptoms of psychological distress in the past 30 days, such as “feeling so depressed that nothing can cheer you up” and feeling “that everything was an effort.” Responses are recorded using a 5-point Likert scale, with 1=none of the time and 5=all of the time. Compared with other measures of psychological distress such as the 12-question General Health Questionnaire (GHQ-12), the K6 is more precise in detecting DSM-IV depressive and anxiety disorders (Furukawa, Kessler, Slade, & Andrews, 2003). The K6 has also been shown to have high concordance with blinded clinical diagnoses of Serious Mental Illness (SMI) in the general population samples in the United States (Kessler et al., 2002). The unweighted summary scale has values in the range of 0–24. We followed previously validated scoring rules that classify respondents as follows 1–5=No mental distress; 6–12=Psychological distress; 13–24=Severe Mental Illness. The K6 has been found to be a valid and reliable measure in other health studies with African Americans (Bratter & Eschbach, 2005), and in our sample, the scale exhibited acceptable reliability (Cronbach's α=0.86).
Perceived neighborhood crime/safety
Based on the work of others who have investigated the extent to which threat and occurrence of crime and perceptions of social disorder serve to disrupt the residential environment in diverse ethnic samples (Martinez, Black, & Starr, 2002), we used a 4-item measure that asked participants to rate on a Likert scale their level of agreement with the following statements: (1) “You feel safe walking in your neighborhood during the day,” (2) “You feel safe walking in your neighborhood during the evening,” (3) “Your neighborhood is safe from crime,” (4) “Violence is a problem in your neighborhood.” The last item was reversed coded, and all four items were scored from 1–5, with higher scores indicating greater perceived neighborhood safety. The scale had a reliability of Cronbach's α=0.71.
Perceived neighborhood social cohesion
Based on the work of Sampson and colleagues focused on neighborhoods and collective efficacy among Latinos and African Americans in Chicago (Sampson, Morenoff, & Earls, 1999; Sampson & Raudenbush, 1999), but recently utilize by another study with a larger sample size of residents throughout low-income neighborhoods in the U.S.(Collins, Neal, & Neal, 2014), this 6-item measure asked participants the extent to which they agreed that: (1) “people in this neighborhood are willing to help their neighbors,” (2) “this is a close-knit neighborhood,” (3) “people in this neighborhood can be trusted,” (4) “People in this neighborhood look out for one another,” (5) “People in this neighborhood generally don’t get along with each other,” and (6) “People in this neighborhood do not share the same values.” The last two items were reverse coded. Scores ranged from 1 to 5 with higher scores indicating greater perceived neighborhood social cohesion. The scale had a reliability of Cronbach's α=0.84.
Sociodemographic characteristics
These included sex, age (measured in years and entered into the model as a continuous variable), and a count of all children in the household (children defined as ≤18). Educational attainment was coded as less than high school, high school graduate or diploma, some college, and 4 years of college or more. Income was measured with a single question (“What was your total household income in the past year? Household income means the combined income of everyone who lives in the house and who shares expenses and earnings.”). Household income was then adjusted for number of people living inside the household and treated as a categorical variable (i.e., <$5,000; $5,000–$9,999; $10,000–$19,999; $20,000+). Years lived in neighborhood was also included. Missing values were imputed using single imputation methods in SAS software 9.4.
Data Analysis
First, descriptive statistics were calculated (means and percentages) to examine the distribution of sociodemographic factors, social network size and characteristics, perceived neighborhood features, and psychological distress. Next, we used robust regression to estimate the association between the social network characteristics (i.e., size, diversity, and composition) and perceived neighborhood characteristics (i.e., safety and social cohesion) with psychological distress, while controlling for sociodemographic factors. This regression approach was carefully chosen after performing a series of residual diagnostics to check for model assumptions (i.e., normality, linearity, and homoscedasticity). The process for choosing covariates included using a conceptual model and previous study results. Statistical significance was set at p < .05, and analyses were conducted using SAS statistical analysis software (version 9.4, 2014, SAS Institute Inc.).
Results
Table 1 shows the distribution of sociodemographic characteristics (age, sex, education, employment status, income, marital status, and years lived in neighborhood), social network characteristics (total network size, and split by group; network diversity), perceptions of neighborhood (social cohesion, safety), and psychological distress. In general, the cohort was comprised of mostly middle-aged and older adults, who were female, had a high school or some college education, were unemployed, and had low incomes. Over 20% were married and had almost 30 years living in their respective neighborhood. Mean network size was 46, and family (13.5) and religious affiliations (10.9) comprised the biggest share of their social network members, for an average person in this cohort. Social network diversity scores are 0.65, meaning that their social network composition tended towards diversity more so than homogeneity in the types of network members.
Table 1.
Sociodemographic, Neighborhood Characteristics and Psychological Distress of Participants living in Pittsburgh, PA (N =1,040)
| No. (%) or Mean (SD; Min-Max) | |
|---|---|
| Age (in years) | |
| 18–34 | 137 (13.2%) |
| 35–44 | 119 (11.4%) |
| 45–54 | 227 (21.8%) |
| 55–64 | 242 (23.3%) |
| 65–74 | 176 (16.9%) |
| 75+ | 139 (13.4%) |
| Sex | |
| Female | 794 (76.4%) |
| Male | 246 (23.6%) |
| Education | |
| <High School | 142 (13.7%) |
| High School | 430 (41.4%) |
| Some college | 320 (30.8%) |
| ≥College | 148 (14.2%) |
| Employment status | |
| Full/Part Time Employed | 383 (36.8%) |
| Unemployed | 657 (63.2%) |
| Adjusted Annual Household Income | |
| < $5,000 | 272 (26.2%) |
| $5,000–$9,999 | 267 (25.7%) |
| $10,000–$19,999 | 314 (30.2%) |
| $20,000+ | 187 (18.0%) |
| Marital Status | |
| Married | 211 (20.3%) |
| Years lived in neighborhood | 29.8 (23.3) |
| Social Network Characteristics | |
| Total Social Network Size | 46.4 (53.1; 0–415) |
| M Number of Family | 13.5 (17.2; 0–100) |
| M Number of Friends | 6.4 (10.5; 0–110) |
| M Number of Co-Workers | 4.4 (11.3; 0–100) |
| M Number of Neighbors | 6.1 (11.8; 0–125) |
| M Number of Religious affiliations | 10.9 (27.1; 0–200) |
| M Number of Others | 5.3 (11.7; 0–100) |
| Social Network Diversity | 0.7 (0.2; 0–1) |
| Perceptions of Neighborhood Social Cohesion |
3.1 (0.8) |
| Perceptions of Neighborhood Safety | 2.9 (0.8) |
| Psychological distress (continuous) | 4.4 (4.6) |
| Psychological distress (categorical) | |
| None (k6=1–5) | 719 (69.1%) |
| Distress (k6=6–12) | 246 (23.7%) |
| Illness (k6 ≥13) | 75 (7.2%) |
Within the total cohort, 70% exhibited no symptomology (K6 ≤5) whereas 30% exhibited some psychological distress. Only about 7% had scores of 13 or higher, which means that the vast majority of this sample did not fall within the range of non-clinically significant psychological distress, or a diagnosable mental or emotional disorder that resulted in functional impairment that substantially interfered with or limited one or more major life activities. However, the mean for the cohort was 4.4 (SE=4.6), which is higher than the estimates for the general population of African Americans (2.41) in the National Health and Interview Survey (Bratter & Eschbach, 2005).
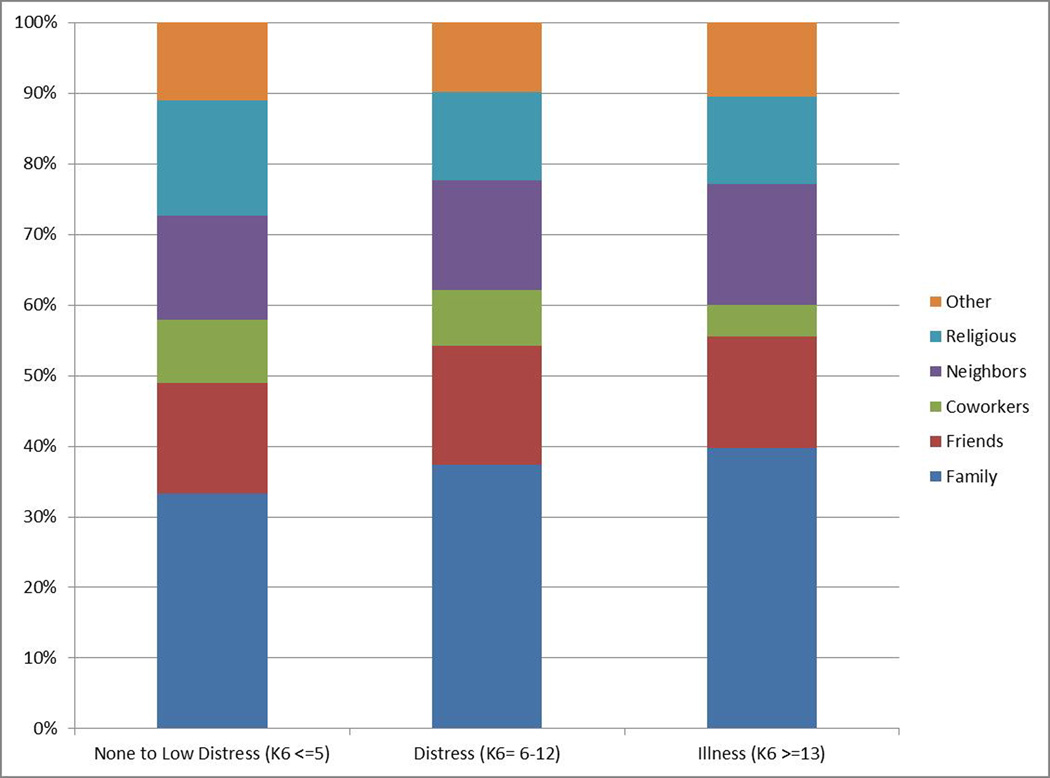
In Figure 1, we show social network composition at three levels of psychological distress: none/low, ‘distress,’ and ‘illness.’ Those individuals with no psychological distress had social networks that were comprised mostly of family (33.4%), religious affiliations (16.4%) and friends (15.6%). The social network composition of participants exhibiting some distress (i.e., K6 scores=6–12) were largely the same as those with no psychological distress, except that they had a slightly higher proportion of family members (37.1%) and friends (16.8%) in their social network, but a lower proportion of people from religious affiliations (12.4%). Individuals with scores within the illness range (i.e., K6 scores ≥13) had networks that were mostly comprised of family (39.8%) and neighbors (17.2%). They had similar proportion of friends (15.9%), those with religious affiliations (12.4%), and “other” category (10.5%) compared to the other two groups. Interestingly, it was the proportion of network members who were coworkers that differed most between the three groups of participants: among those with no distress coworkers comprised, on average, 9.0% of their network, while this proportion was 7.8% among participants with some distress, and 4.0% among participants with illness. Formal statistical tests reveal some several group differences, but mostly between group 1 (none to mild distress) compared to the two distressed groups (distressed and illness). Specifically, there were significant differences across K6 groups in total network size, as well as the size of coworkers, religious, and other network types. However, there were no differences for family, friends, or neighbors.
Figure 1.
Social network composition by psychological distress categories
In unadjusted multivariate models (see Model 1, Table 2), a significant, small association was found between social network size and distress. Similarly in models adjusted for age, sex, employment status, income, education, marital status, and years lived in the neighborhood (Model 2, Table 2) larger social network size was associated with less psychological distress. Notwithstanding, the regression coefficient captures the effect of changing the social network size by one unit, which is very small relative to its full range (between 0—415). To explore a practically meaningful effect size, we obtained predicted means of the K6 by varying social network size from the 5th percentile value to its 95th percentile. We found that varying social network size corresponded to a change of 0.7 units in psychological distress. Despite adjusting for multiple strong individual predictors of distress such as age and income (p < .0001), employment and education (p<0.05), social network size had an additional protective association with psychological wellbeing. We also found that the association between social network size and K6 was twice the strength prior to adjusting for individual characteristics. In additional sensitivity analyses of various model specifications (i.e., using various modeling techniques such as negative binomial, ordered logistic, and logistic regression), we found the significant association between social network size and psychological distress was robust (results not shown). This was not the case for social network diversity, which was not significantly associated with psychological distress in the unadjusted or controlled models.
Table 2.
Multivariate Regression Predicting Psychological Distress (N=1040)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| Total Social Network Size | −0.010*** | −0.006* | −0.005* | −0.005* | −0.005* |
| Social Network Diversity | 0.309 | 0.591 | 0.667 | 0.683 | |
| Perceived Neighborhood Characteristics | |||||
| Perceived Neighborhood Safety | −0.578*** | −0.484** | −1.438* | ||
| Perceived Neighborhood Social Cohesion |
−0.206 | −1.081† | |||
| Safety X Cohesion | 0.310 | ||||
| Sociodemographic Variables | |||||
| Age | −0.044*** | −0.042*** | −0.040*** | −0.039*** | |
| Female | 0.094 | 0.075 | 0.082 | 0.085 | |
| Employed | −0.613* | −0.617* | −0.634* | −0.617* | |
| Adjusted Annual Household Income | −0.036*** | −0.035*** | −0.035*** | −0.035*** | |
| Married | −0.352 | −0.327 | −0.308 | −0.351 | |
| High School | −0.781* | −0.868* | −0.852* | −0.858* | |
| Some College/Technical | −1.347*** | −1.402*** | −1.373*** | −1.344*** | |
| College Graduate | −1.171* | −1.199* | −1.174* | −1.176* | |
| Years Lived in the Neighborhood | −0.013* | −0.011 | −0.011 | −0.011 |
p<0.10,
p<0.05,
p<0.01,
p<0.001
When we considered perceived neighborhood characteristics, only perceived neighborhood safety was associated with psychological distress. One unit increase in perceived safety was associated with a decrease in psychological distress (β=−1.438, p<.05). Both social cohesion, as well as the interaction term included to test whether cohesion would be most relevant for those with perceptions of lack of neighborhood safety, was not significantly associated with distress.
Discussion
Social network size, but not social network diversity, was found to have a small, protective effect on psychological distress in this cross-sectional study of an important cohort of African American adults in the historic Hill District in Pittsburgh, PA. This is interesting since historical accounts cite social networks as a major resource of this community (Fullilove, 2005), but no study had previously measured social network features and examined its association with mental health outcomes. Of note is that compared to studies using a similar measure of social networks, the average network total size for this cohort was much smaller (46.4 vs. 71.84) (Roberts, Dunbar, Pollet, & Kuppens, 2009). Social network composition also differed in this cohort compared to other studies, with the former having a smaller proportion of family, friends, coworkers, but higher proportion of people in their network with religious affiliation. Neighbors are the only category that was comparable, with an average of 6.1 neighbors in this cohort and 6.4 for those in other studies (Vardavas & Marcum, 2012).
Other studies utilizing different measures of social network among African Americans have found less frequent contact with relatives and friends (Pugliesi & Shook, 1998), but more frequent contact with members of the church/religious community (Kim & McKenry, 1998). Perhaps because this study’s social network elicitation measure required that people think about people whom they have had frequent contact with in the past six months, the results yielded this smaller proportion of family and friends in the network. The importance of people from church in this cohort’s social network index is consistent with historical accounts of this neighborhood, and in fact religious affiliations were described as a resource especially during periods in which the neighborhood was being transformed (Fullilove, 2005). Though this study was limited from further investigating the kinds of resources these network members provide, it would be important that future studies be able to elucidate the type of support (e.g., emotional, informational, instrumental) these network members provide and the extent to which these different types of support are associated with psychological distress. However, while our findings were consistently significant across multiple model specifications and held up with covariate adjustment, the effect size was consistently small. This may be due to the inclusion of several important individual-level predictors, with considerable influence on psychological distress. However, these effect sizes are similar to those of neighborhood-level or environment-level variables, which typically exhibit small effect sizes.
Our study is also unique in that it simultaneously examined perceived neighborhood stressors through perceptions of crime/safety, as well as neighborhood social support through measures of perceived social cohesion. Like Steptoe & colleagues, we found perceived safety to be associated with psychological distress independent of social cohesion (Steptoe & Feldman, 2001). This is likely due to the fact that perceptions of one’s neighborhood as unsafe can increase feelings of distress through increased feelings of powerlessness and fear (Mair, et al., 2012; Perkins & Taylor, 1996; Ross & Jang, 2000), and that the predictive value of perceived neighborhood safety in this study is due to the eminence of this construct for this neighborhood. Specifically, crime and violence have been cited as a crucial factor in the decline of this community (Fullilove, 2005), and neighborhood crime levels have been shown to increase the risk of experiencing psychological distress especially damage to the built environment (Astell-Burt, Feng, Kolt, & Jalaludin, 2015). Similarly, residents in Flint Michigan understood disordered physical environment (e.g., abandoned buildings) as a factor fomenting fear and crime, as well creating an impression that neighborhood authorities have lost control in the area (Johansen, et al., 2015). Taken together, these feelings of tension and fear could be the mechanism linking neighborhood safety to psychological distress. For example, living in a neighborhood where you hear gunshots or are worried for your safety can create a stress response—that over time (and with cumulative impact) could be relevant for mental health outcomes such as psychological distress. On the other hand, a sense of social cohesion could help dampen this response even in the face of concerns about neighborhood safety. Further examinations of the pathways linking neighborhood crime to psychological distress are warranted, especially as violence in the urban context is severely felt by African American communities.
Lastly, most studies of African Americans and psychological distress have been limited to a few sociodemographic correlates of distress (e.g., income, employment) (Lincoln & Chae, 2010). Of the few studies that include a wide array of sociodemographic predictors, our findings are consistent in that age, employment, income, and education were significantly associated with distress (Lincoln, Taylor, Chae, & Chatters, 2010; Lincoln, Taylor, Watkins, & Chatters, 2011). Age was a particularly robust predictor in this study, with older individuals having less psychological distress. Further, those between the ages of 55–64 had the largest social networks. Together, these age-related findings in this cohort support scholarship among African Americans that suggests there is a “healthy survivor effect” (Lincoln, et al., 2011; Strauss, Ojdana, Shavelle, & Rosenbloom, 2004) given the high rates of mortality among African Americans of all ages.
This study yielded important cross-sectional evidence regarding the protective role of social networks and perceived neighborhood safety among residents of this historic African American neighborhood in the cusp of major neighborhood changes. There are important methodological limitations; however, including the cross-sectional nature of the study that limits to fully assess the temporality of these associations. Other issues include reporting bias (e.g., asking participants about their psychological distress and perceptions of their neighborhood), as well as limits on generalizability of the findings. Despite these, our findings are an important contribution to our current understanding of psychological distress among African Americans, and highlights social networks and perceptions of neighborhood safety as important factors when devising effective and individualized interventions. Future work will assess the extent to which social networks and perceptions are affected by the neighborhood revitalization projects, and the extent to which these are associated with psychological distress.
Acknowledgments
Funding
Flórez received support from the University of California, Los Angeles (UCLA) and Charles Drew University (CDU), Resource Centers for Minority Aging Research Center for Health Improvement of Minority Elderly (RCMAR/CHIME) under NIH/NIA Grant P30-AG021684, and from the UCLA Clinical and Translational Science Institute (CTSI) under NIH/NCATS Grant Number UL1TR000124. Ghosh-Dastidar, Beckman and Dubowitz received support from the National Cancer Institute (Grant No.R01CA149105; Tamara Dubowitz, principal investigator). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
The authors express sincere appreciation and gratitude to La’Vette Wagner, field coordinator of the Pittsburgh Hill/Homewood Research on Eating, Shopping, and Health study; the data collection staff; and Shellae H. Versey for her valuable comments on a previous version of the manuscript.
References
- Ajrouch KJ, Antonucci TC, Janevic MR. Social networks among blacks and whites: the interaction between race and age. [Comparative Study Research Support, U.S. Gov't, P.H.S.] The journals of gerontology. Series B, Psychological sciences and social sciences. 2001;56(2):S112–S118. doi: 10.1093/geronb/56.2.s112. [DOI] [PubMed] [Google Scholar]
- Astell-Burt T, Feng XQ, Kolt GS, Jalaludin B. Does rising crime lead to increasing distress? Longitudinal analysis of a natural experiment with dynamic objective neighbourhood measures (vol 138, pg 68, 2015) Social science & medicine. 2015;139:70–70. doi: 10.1016/j.socscimed.2015.05.014. [DOI] [PubMed] [Google Scholar]
- Bjornstrom EE, Ralston ML, Kuhl DC. Social cohesion and self-rated health: The moderating effect of neighborhood physical disorder. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't] American journal of community psychology. 2013;52(3–4):302–312. doi: 10.1007/s10464-013-9595-1. [DOI] [PubMed] [Google Scholar]
- Blau PM. Inequality and Heterogeneity. New York, NY: Free Press; 1977. [Google Scholar]
- Boessen A, Hipp JR, Smith EJ, Butts CT, Nagle NN, Almquist Z. Networks, space, and residents' perception of cohesion. [Research Support, U.S. Gov't, Non-P.H.S.] American journal of community psychology. 2014;53(3–4):447–461. doi: 10.1007/s10464-014-9639-1. [DOI] [PubMed] [Google Scholar]
- Bratter JL, Eschbach K. Race/ethnic differences in nonspecific psychological distress: Evidence from the National Health Interview Survey. Social Science Quarterly. 2005;86(3):620–644. doi: [Google Scholar]
- Caughy MO, O'Campo PJ, Muntaner C. When being alone might be better: neighborhood poverty, social capital, and child mental health. [Research Support, Non-U.S. Gov't] Social science & medicine. 2003;57(2):227–237. doi: 10.1016/s0277-9536(02)00342-8. [DOI] [PubMed] [Google Scholar]
- Chatters LM, Taylor RJ, Woodward AT, Nicklett EJ. Social support from church and family members and depressive symptoms among older African Americans. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't] The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2015;23(6):559–567. doi: 10.1016/j.jagp.2014.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins CR, Neal JW, Neal ZP. Transforming individual civic engagement into community collective efficacy: the role of bonding social capital. American journal of community psychology. 2014;54(3–4):328–336. doi: 10.1007/s10464-014-9675-x. [DOI] [PubMed] [Google Scholar]
- Cutrona CE, Russell DW, Brown PA, Clark LA, Hessling RM, Gardner KA. Neighborhood context, personality, and stressful life events as predictors of depression among African American women. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.] Journal of abnormal psychology. 2005;114(1):3–15. doi: 10.1037/0021-843X.114.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutrona CE, Russell DW, Hessling RM, Brown PA, Murry V. Direct and moderating effects of community context on the psychological well-being of African American women. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.] Journal of personality and social psychology. 2000;79(6):1088–1101. doi: 10.1037//0022-3514.79.6.1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damewood R, Young-Laing B. Strategies to prevent displacement of residents and businesses in Pittsburgh's Hill District: Public Policy Institute of California. 2011 [Google Scholar]
- De Jesus M, Puleo E, Shelton RC, Emmons KM. Associations between perceived social environment and neighborhood safety: Health implications. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't] Health & place. 2010;16(5):1007–1013. doi: 10.1016/j.healthplace.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubowitz T, Ncube C, Leuschner K, Tharp-Gilliam S. A natural experiment opportunity in two low-income urban food desert communities: research design, community engagement methods, and baseline results. Health Educ Behav. 2015;42(1 Suppl):87S–96S. doi: 10.1177/1090198115570048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick KM, Piko BF, Wright DR, LaGory M. Depressive symptomatology, exposure to violence, and the role of social capital among African American adolescents. The American journal of orthopsychiatry. 2005;75(2):262–274. doi: 10.1037/0002-9432.75.2.262. [DOI] [PubMed] [Google Scholar]
- Forehand R, Jones DJ. Neighborhood violence and coparent conflict: interactive influence on child psychosocial adjustment. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.] Journal of abnormal child psychology. 2003;31(6):591–604. doi: 10.1023/a:1026206122470. [DOI] [PubMed] [Google Scholar]
- Fullilove MT. Root shock: the consequences of African American dispossession. Journal of urban health : bulletin of the New York Academy of Medicine. 2001;78(1):72–80. doi: 10.1093/jurban/78.1.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fullilove MT. Be It Ever So Humble. Vol. 138. National Housing Institute; 2004. [Google Scholar]
- Fullilove MT. Root Shock: How tearing Up City Neighborhoods Hurts America, and What We Can Do About It. New York: Ballante Books; 2005. [Google Scholar]
- Furukawa TA, Kessler RC, Slade T, Andrews G. The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S. Validation Studies] Psychological medicine. 2003;33(2):357–362. doi: 10.1017/s0033291702006700. [DOI] [PubMed] [Google Scholar]
- Johansen R, Neal ZP, Gasteyer S. The view from a broken window: How residents make sense of neighbourhood disorder in Flint. Urban Studies. 2015;52(16):3054–3069. [Google Scholar]
- Johns LE, Aiello AE, Cheng C, Galea S, Koenen KC, Uddin M. Neighborhood social cohesion and posttraumatic stress disorder in a community-based sample: findings from the Detroit Neighborhood Health Study. [Research Support, N.I.H., Extramural] Social psychiatry and psychiatric epidemiology. 2012;47(12):1899–1906. doi: 10.1007/s00127-012-0506-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnstone Q. Federal Urban Renewal Program. Faculty Scholarship Series. 1958;1958 [Google Scholar]
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, Zaslavsky AM. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. [Comparative Study Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.] Psychological medicine. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Zaslavsky AM. Screening for serious mental illness in the general population. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.] Archives of general psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Kim HK, McKenry PC. Social networks and support: A comparison of African Americans, Asian Americans, Caucasians, and Hispanics. Journal of Comparative Family Studies. 1998;29(2):313-+. [Google Scholar]
- Leventhal T, Brooks-Gunn J. Moving to opportunity: an experimental study of neighborhood effects on mental health. [Clinical Trial Randomized Controlled Trial Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S. Research Support, U.S. Gov't, P.H.S.] American journal of public health. 2003;93(9):1576–1582. doi: 10.2105/ajph.93.9.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine DS, Taylor RJ, Nguyen AW, Chatters LM, Himle JA. Family and friendship informal support networks and social anxiety disorder among African Americans and Black Caribbeans. Social psychiatry and psychiatric epidemiology. 2015;50(7):1121–1133. doi: 10.1007/s00127-015-1023-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lincoln KD, Chae DH. Stress, Marital Satisfaction, and Psychological Distress Among African Americans. Journal of Family Issues. 2010;31(8):1081–1105. [Google Scholar]
- Lincoln KD, Taylor RJ, Chae DH, Chatters LM. Demographic Correlates of Psychological Well-Being and Distress Among Older African Americans and Caribbean Black Adults. Best practices in mental health. 2010;6(1):103–126. [PMC free article] [PubMed] [Google Scholar]
- Lincoln KD, Taylor RJ, Watkins DC, Chatters LM. Correlates of Psychological Distress and Major Depressive Disorder Among African American Men. Research on social work practice. 2011;21(3):278–288. doi: 10.1177/1049731510386122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mair C, Diez Roux AV, Galea S. Are neighbourhood characteristics associated with depressive symptoms? A review of evidence. [Research Support, N.I.H., Extramural Review] Journal of epidemiology and community health. 2008;62(11):940–946. doi: 10.1136/jech.2007.066605. 948 p following 946. [DOI] [PubMed] [Google Scholar]
- Mair C, Kaplan GA, Everson-Rose SA. Are there hopeless neighborhoods? An exploration of environmental associations between individual-level feelings of hopelessness and neighborhood characteristics. [Research Support, N.I.H., Extramural] Health & place. 2012;18(2):434–439. doi: 10.1016/j.healthplace.2011.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez ML, Black M, Starr RH. Factorial structure of the Perceived Neighborhood Scale (PNS): A test of longitudinal invariance. Journal of Community Psychology. 2002;30(1):23–43. doi: [Google Scholar]
- Moore S, Bockenholt U, Daniel M, Frohlich K, Kestens Y, Richard L. Social capital and core network ties: a validation study of individual-level social capital measures and their association with extra- and intra-neighborhood ties, and self-rated health. [Research Support, Non-U.S. Gov't Validation Studies] Health & place. 2011;17(2):536–544. doi: 10.1016/j.healthplace.2010.12.010. [DOI] [PubMed] [Google Scholar]
- Negrón RN. Diversity, Multiethnicity, and Latino Social Networks. Societies. 2014;4:222–239. [Google Scholar]
- Perkins DD, Taylor RB. Ecological assessments of community disorder: Their relationship to fear of crime and theoretical implications. American journal of community psychology. 1996;24(1):63–107. doi: 10.1007/BF02511883. doi: [DOI] [PubMed] [Google Scholar]
- Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. [Research Support, Non-U.S. Gov't Review] Journal of epidemiology and community health. 2001;55(2):111–122. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pugliesi K, Shook SL. Gender, ethnicity, and network characteristics: Variation in social support resources. Sex Roles. 1998;38(3–4):215–238. doi: [Google Scholar]
- Rebuilding Together. Hill District. [Retrieved August 25, 2015]; from http://www.rtpittsburgh.org/hill-district/ [Google Scholar]
- Roberts SGB, Dunbar RIM, Pollet TV, Kuppens T. Exploring variation in active network size: Constraints and ego characteristics. Social Networks. 2009;31(2):138–146. [Google Scholar]
- Ross CE, Jang SJ. Neighborhood disorder, fear, and mistrust: The buffering role of social ties with neighbors. American journal of community psychology. 2000;28(4):401–420. doi: 10.1023/a:1005137713332. doi: [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Morenoff JD, Earls F. Beyond social capital: Spatial dynamics of collective efficacy for children. American Sociological Review. 1999;64(5):633–660. doi: [Google Scholar]
- Sampson RJ, Raudenbush SW. Systematic social observation of public spaces: A new look at disorder in urban neighborhoods. American Journal of Sociology. 1999;105(3):603–651. doi: [Google Scholar]
- Simons RL, Murry V, McLoyd V, Lin KH, Cutrona C, Conger RD. Discrimination, crime, ethnic identity, and parenting as correlates of depressive symptoms among African American children: a multilevel analysis. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.] Development and psychopathology. 2002;14(2):371–393. doi: 10.1017/s0954579402002109. [DOI] [PubMed] [Google Scholar]
- Simpson EH. Measurement of diversity. Nature. 1949;163 [Google Scholar]
- Snowden LR. Social embeddedness and psychological well-being among African Americans and whites. [Comparative Study Research Support, U.S. Gov't, P.H.S.] American journal of community psychology. 2001;29(4):519–536. doi: 10.1023/A:1010480816822. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Feldman PJ. Neighborhood problems as sources of chronic stress: Development of a measure of neighborhood problems, and associations with socioeconomic status and health. Annals of Behavioral Medicine. 2001;23(3):177–185. doi: 10.1207/S15324796ABM2303_5. doi: [DOI] [PubMed] [Google Scholar]
- Stevenson H. Raising safe villages: Cultural-ecologial factors that influence the emotional adjustment of adolescents. Journal of Black Psychology. 1998;24:44–59. [Google Scholar]
- Strauss D, Ojdana K, Shavelle R, Rosenbloom L. Decline in function and life expectancy of older persons with cerebral palsy. NeuroRehabilitation. 2004;19(1):69–78. [PubMed] [Google Scholar]
- Sutton S. Urban revitalization in the United States: Policies and Practices. New York: Columbia University; 2008. [Google Scholar]
- Taylor RJ, Chae DH, Lincoln KD, Chatters LM. Extended family and friendship support networks are both protective and risk factors for major depressive disorder and depressive symptoms among African-Americans and black Caribbeans. [Research Support, N.I.H., Extramural] The Journal of nervous and mental disease. 2015;203(2):132–140. doi: 10.1097/NMD.0000000000000249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vardavas E, Marcum SC. Modeling Influenza Vaccination Behavior via Inductive REasoning Games. In: d'Onofrio A, Manfredi P, editors. Modeling the interplay between human behavior and spread of infectious disease. Springer; 2012. [Google Scholar]