Abstract
Background
One-lung ventilation (OLV) anesthesia intubation route is often used in patients undergoing thoracoscopic-esophagectomy in semi-prone position. Recently, the two-lung ventilation (TLV) approach becomes popular. However, limited studies have compared the two ventilation approaches in parallel. Here, we report a single-center, retrospective study of comparing TLV and OLV approach in patients undergoing thoracoscopic-esophagectomy in semi-prone position.
Methods
From January 2013 to November 2014, 147 patients were enrolled into the current study and were given thoracoscopic-esophagectomy in semi-prone position either by OLV or TLV. Intraoperative respiratory functional data and perioperative surgical parameters of the two approaches were collected and analyzed.
Results
Of the 147 patients, 64 patients received OLV and 83 patients received TLV, and all of them were successfully under gone thoracoscopic procedures without conversion to open thoracotomy. There was no incidence of major intraoperative complications or perioperative death. There were no statistically different in postoperative respiratory complications, either. However, TLV approach resulted in better intraoperative respiratory function (PaCO2, PaO2, SaO2), shorter preparation time for anesthesia induction, less blood loss, shorter thoracoscopic operating time and less postoperative hospital stay (P<0.05). The incidence of postoperative respiratory complications and quantity of the resected thoracic lymph node showed no difference between the two ventilation approach (P>0.05).
Conclusion
This study demonstrated that TLV intubation approach is superior to OLV approach during the thoracoscopic-esophagectomy in semi-prone position. According to this, TLV approach is a technically feasible, convenient and safe anesthesia induction approach for esophageal cancer surgery.
Keywords: Esophageal cancer, thoracoscopic-esophagectomy, semi-prone position, two-lung ventilation (TLV), one-lung ventilation (OLV), perioperative period
Introduction
Despite the great progress in surgical technology, esophagectomy remains the most complex surgical procedure with significant perioperative morbidity and mortality rate (1,2). Following the first report on thoracoscopic-esophagectomy by Cuschieri in 1992 (3), the minimally invasive esophagectomy (MIE) method for esophageal cancer was accepted as the optimal approach (4-6), with the popular way of anesthesia intubation of one-lung ventilation (OLV) (7).
However, OLV way of anesthesia intubation has several disadvantages including high rate of respiratory complications and difficulties of anesthesia induction and maintenance. Thus, it has been a continuing quest to search for better method with convenience, safe and least-trauma in managing anesthesia intubation for thoracoscopic-esophagectomy (8).
In 2006, Palanivelu reported an approach of the anesthesia intubation, known as two-lung ventilation (TLV) approach, in thoracoscopic-esophagectomy in prone position (9). The TLV with a single-lumen endotracheal tube has rapidly gained popularity and seems to be a promising option for MIE (10,11). However, limited studies have compared the TLV and OLV in patients undergoing thoracoscopic-esophagectomy in a position of semi-prone. Thus, in this study, we examined safety and feasibility of the TLV in semi-prone position during surgery of esophageal cancer through thoracoscopic-esophagectomy by single-center retrospective study.
Methods
Candidate patients, OLV Group (left-lung ventilation by double-lumen tube intubation) (n=64, 43.5%) and TLV group (by using single-lumen endotracheal tube) (TVL group; n=84, 57.1%), who underwent thoracoscopic-esophagectomy for esophageal squamous carcinoma in semi-prone position in Division One of Xijing Digestive Hospital between January 2013 and November 2014, were enrolled in the study in chronological order. All patients were evaluated carefully for the safety of anesthesia and operation. This retrospective study was approved by the Ethics Committee of Xijing Hospital and all aspects of the study comply with the Declaration of Helsinki. A written informed consent was obtained from all the patients at the time of admission, with which the blood, tissue and other sample were authorized to scientific purpose.
Surgical procedures
Each patient was given anesthesia induction individually in supine position. The OLV group was performed using a bronchial blocker tube. And the TLV group was intubated with a single-lumen endotracheal tube in the standard conventional procedure.
Then, all patients were turned to a semi-prone position with the right arm was abducted about 100 degrees above the head. The head was well supported and fixed with a soft cushion in order to prevent tube displacement (Figure 1).
Figure 1.

Photograph of a patient by TLV in semi-prone position.
The thoracoscopic procedure was conducted by two surgeons, the operator and the scopist, who were standing at the right side of the patient and a video monitor system on the opposite side (Figure 2). The anesthesia parameters during thoracoscope were as follows: tidal volume was 350 mL for TVL and 400 mL for OVL at the beginning and adjusted according the changes of airway pressure; PEEP was 5 cmH2O; FiO2 was 100% and RR was 16 times/min.
Figure 2.
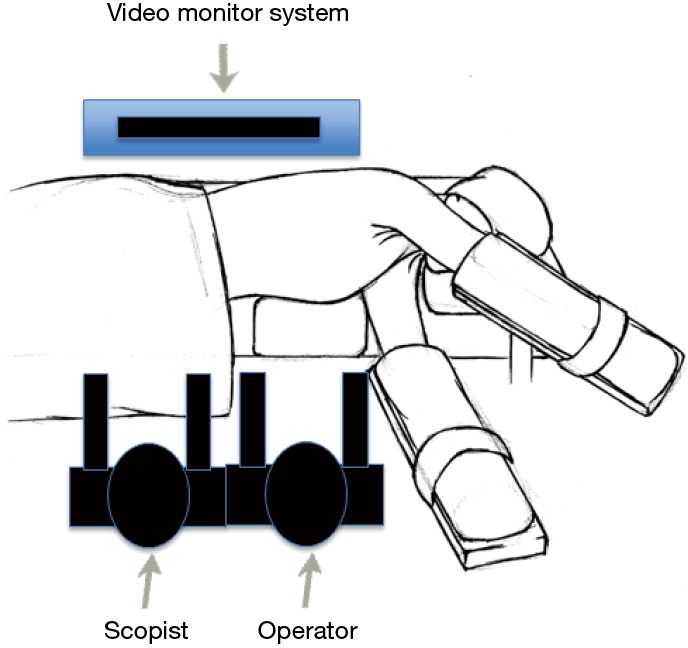
Schematic illustration of surgeons’ standing position and a video monitor location.
A three-port thoracoscopy technique was used as following: the observation port was placed at the fifth intercostal space on the mid-axillary line with a 10-mm scope; two 12-mm ports were placed at the fourth and eighth intercostal space, respectively, on the posterior axillary line for intra-thoracic procedure (dots shown in Figure 1). A carbon dioxide pneumothorax was created with a start pressure of 8–10 mmHg to deflate the lung partially or fully for a better exposure of operative field.
The following parameters were recorded at 1 and 2 hours, respectively, after initializing thoracoscopic-esophagectomy: partial pressure of oxygen in arterial blood (PaO2), partial pressure of carbon dioxide in the blood (PaCO2), oxygen saturation (SaO2). Subsequently, the artificial pneumothorax was stopped at the accomplishment of intra-thoracic procedure. Then, patients were changed to supine for conventional scopic procedure of intra-abdominal underwent Laparoscopy procedure and cervical procedures were followed by standard procedures.
Perioperative surgical parameters in the two groups (preparation time for anesthesia induction, blood loss, thoracoscopic operating time, respiratory complications, postoperative hospital stay and quantity of resection lymph node) were carefully collected and assessed.
Statistical analysis
Data were analyzed using SPSS 21.0 for Windows (SPSS Inc., Chicago, IL, USA). Numerical variables were expressed as the mean ± SD unless otherwise stated. The P values were considered to be statistically significant at the 5% level.
Results
Of 147 patients, 64 patients underwent OLV, and 83 patients were given TLV. There was no significant difference in the following clinical characteristics between the two groups: gender, age, smoking habit, neoadjuvant treatment, preoperative tumor staging, pre-operative respiratory parameters (Table 1).
Table 1. Demographic characteristics of the 147 patients.
| Characteristics | OLV (%) (n=64) | TLV (%) (n=83) | P value |
|---|---|---|---|
| Gender | 0.411 | ||
| Male | 39 (60.94) | 56 (79.52) | |
| Female | 25 (39.06) | 27 (20.48) | 0.903 |
| Mean age | 57.83±8.145 | 57.66±8.139 | |
| Smoking | 0.385 | ||
| No | 37 (57.81) | 42 (50.60) | |
| Yes | 27 (42.19) | 41 (49.40) | |
| Neoadjuvant radiotherapy | 0.723 | ||
| No | 61 (95.31) | 78 (93.98) | |
| Yes | 3 (4.69) | 5 (6.02) | |
| Neoadjuvant chemotherapy | 0.957 | ||
| No | 58 (90.63) | 75 (90.36) | |
| Yes | 6 (9.37) | 8 (9.64) | |
| Pre T stage | 0.281 | ||
| 1 | 7 (11.29) | 9 (11.11) | |
| 2 | 21 (33.87) | 36 (44.44) | |
| 3 | 30 (48.39) | 27 (33.33) | |
| 4 | 4 (6.45) | 9 (11.11) | |
OLV, one-lung ventilation; TLV, two-lung ventilation.
All thoracic procedures were successfully accomplished under thoracoscopy and there was no incidence of conversion to open thoracotomy or major complications, such as tracheal and lung injury, aorta bleeding and or perioperative death.
Compared with OLV group, the TLV group had significantly better outcomes in intra-operative lung function, blood gas analysis, anesthesia induction period, blood loss, thoracoscopic operating time, and postoperative hospital stay (Tables 2,3).
Table 2. Comparison of the intraoperative blood gas analysis and perioperative surgical parameters between the two-intubation approaches.
| Intra-operative blood gas analysis | OLV | TLV | P value |
|---|---|---|---|
| Pre-PCO2 | 39.25 (4.6) | 37.50 (5.2) | 0.371 |
| 1 hr PCO2 | 48.20±7.83 | 47.44±7.71 | 0.662 |
| 2 hr PCO2 | 43.99±6.96 | 43.57±6.60 | 0.756 |
| Pre-PO2 | 74.65 (10.5) | 75.50 (11.4) | 0.209 |
| 1 hr PO2 | 124.45 (106) | 207.10 (283.0) | 0.002 |
| 2 hr PO2 | 296.90 (290.7) | 382.20 (205.7) | 0.035 |
| Pre-SO2 | 96.50 (2.0) | 96.30 (2.0) | 0.376 |
| 1 hr SO2 | 99.00 (3.0) | 100.00 (1.0) | 0.001 |
| 2 hr SO2 | 100.00 (0.0) | 100.00 (0.0) | 0.086 |
Data shown as mean ± SD or numeric value. OLV, one-lung ventilation; TLV, two-lung ventilation.
Table 3. Comparison of the perioperative surgical parameters between the two-intubation approaches.
| Parameters | OLV | TLV | P value |
|---|---|---|---|
| Preparation time (min) | 89.06±12.595 | 81.71±9.749 | 0.000 |
| Thoracic operating time (min) | 155.08±44.441 | 128.83±36.561 | 0.000 |
| Blood loss (mL) | 235.16±142.171 | 194.88±89.391 | 0.037 |
| Hospital stay (D) | 11.41±5.233 | 9.9±1.500 | 0.003 |
| Lymph node | 10.98±9.361 | 12.71±7.784 | 0.087 |
Data shown as mean ± SD or numeric value. OLV, one-lung ventilation; TLV, two-lung ventilation.
Moreover, there was no difference in the incidence of post-operative respiratory complications and quantity of thoracic lymph node resection between the two groups (Tables 3,4).
Table 4. Comparison of the postoperative respiratory complications between the two groups.
| Parameters | OLV | TLV | χ2 | P value |
|---|---|---|---|---|
| Respiratory complications | 7 | 5 | 1.164 | 0.366 |
| Pulmonary infection | 1 | 0 | Fisher | 0.435 |
| Left pleural effusion | 1 | 1 | Fisher | 1.000 |
| Right pleural effusion | 0 | 1 | Fisher | 1.000 |
| Right pneumothorax | 1 | 0 | Fisher | 0.435 |
| Right pyothorax | 1 | 0 | Fisher | 0.435 |
| Respiratory failure | 1 | 0 | Fisher | 0.435 |
| Chylothorax | 0 | 1 | Fisher | 1.000 |
OLV, one-lung ventilation; TLV, two-lung ventilation.
Discussion
Currently, surgical resection remains debate about the predominant treatment for resectable esophageal cancer (12). Regardless of whether squamous carcinoma or adenocarcinoma, perioperative mortality is high (8,9,13), and respiratory complication is one of the most significant factors that impacts the perioperative outcomes (8,14).
Cuschieri reported the first thoracoscopic-esophagectomy in 1992 (3). Afterwards, a variety of MIE approach procedures were reported with better surgical outcomes, for example, laparoscopic transhiatal esophagectomy (15,16), Ivor-Lewis esophagectomy in laparoscopic and/or laparoscopic technique (17,18), laparoscopic and/or laparoscopic McKewon esophagectomy (14,19,20-22). In 1994, Cuschieri reported a new approach of MIE in prone position with satisfactory outcomes, compared to procedures in left lateral decubitus position (23). Seven patients underwent thoracoscopic-esophagectomy in prone with OLV by Watson in 2000 (24). Currently, standard way of intubation is double-lumen endotracheal tubing with OLV (left lung only) (4,25). However, this way of intubation may has following disadvantage: complexity of anesthesia intubation, dissatisfactory exposure for thoracic operative field, difficulty to excise the left recurrent laryngeal nerve lymph node because of double-lumen endotracheal tube, the propensity of tracheal tube displacement and unsafety for re-intubation. Thus, optimal option for intra-operative management of thoracoscopic-esophagectomy is controversial, and surgeons are searching for a safer and more effective intubation approach for adequate exposure and convenient operation.
In 2006, a new way of anesthesia intubation followed by TLV was performed in 130 patients undergone thoracoscopic-esophagectomy in prone position, and the incidence of ARDS and pneumonia was 0.77% and 1.54%, respectively (9). Recently, researchers from Japan reported a result of thoracoscopic-esophagectomy for 14 patients in prone position with TLV and artificial pneumothorax, in which they showed a stable perioperative hemodynamics and oxygenation (10). And Bonavina indicated the thoracoscopic esophagectomy in prone position with TLV was a safer and more effective operation procedure by compared to the Ivor Lewis operation (26,27). Here, we report the result of thoracoscopic-esophagectomy performed on 147 patients in semi-prone position, with 83 patients of TLV and 64 patients of OLV. All patients underwent thoracoscopic procedures successfully without conversion to open thoracotomy or major complications, such as tracheal and lung injury, aorta bleeding, and perioperative mortality. Compared to patients of OLV group, patients in the TLV group had less preparation time for intubation, better intra-operative oxygenation status, less intra-thoracic operation time, less blood loss and postoperative hospital stay. There was no statistical difference in postoperative respiratory complications and quantity of resected thoracic lymph node between the two groups.
The current study demonstrated that TLV application could simplify anesthesia intubation, obtain sufficient exposure operative field (especially the left recurrent laryngeal nerve lymph node) (Figure 3), and perioperative respiratory complications showed no difference between the two groups Therefore, thoracoscopic-esophagectomy under semi-prone position followed by TLV could result in better perioperative outcomes than that by OLV with the accumulation of enrolled patients.
Figure 3.
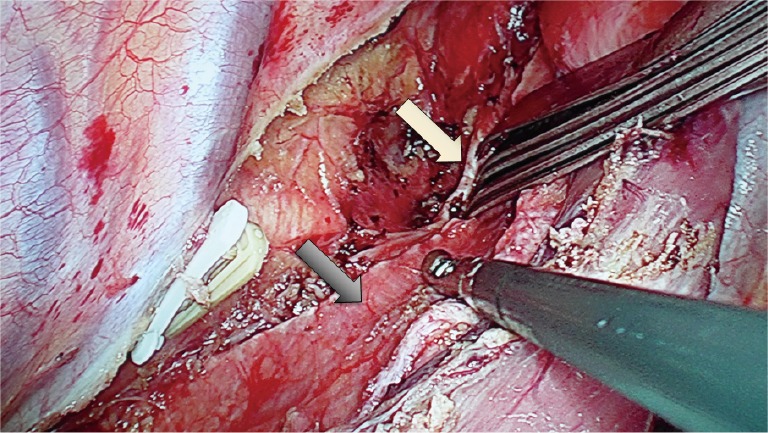
Exposure of left recurrent laryngeal nerve during thoracoscopic procedures. (White arrow: the left recurrent laryngeal nerve; black arrow: trachea with a single-lumen endotracheal tube).
However, the limitation of this approach for an aesthesia intubation is that it may cause difficulties in intraoperative converting the procedure to open thoracotomy, which could be settled by an endobronchial blocker tube, and that it is plausible to affect function of left thoracic cavity if the pleura is broken during the procedure (8).
There are limitations in this study. Firstly, a single hospital-based design might lead to an uncertain amount of selection bias. Secondly, this present study is a retrospective analysis and a well-designed randomized clinical trial should be carried out in order to avoid statistical bias. Thirdly, the lack of long-time follow-up in our study which would be solved by the time.
In conclusion, the current study demonstrated that there were no increased perioperative respiratory complications when the patients receiving thoracoscopic-esophagectomy in semi-prone position and TLV approach, suggesting that the simplified anesthesia intubation approach of TLV is technically feasible and safe for thoracoscopic-esophagectomy in semi-prone position. Still, the results of our study still need bulk data and a long period follow-up.
Acknowledgements
Funding: This work was supported by Natural Science Foundation of China Grants: No.81300301, 31570907, 81572306; Shaanxi Province Social Development Research Foundation of China: No. 2014SF2-14; Xijing Zhu-Tui Project of the Fourth Military Medical University: No. XJZT12Z03.
Ethical Statement: All patients were evaluated carefully for the safety of anesthesia and operation. This retrospective study was approved by the Ethics Committee of Xijing Hospital and all aspects of the study comply with the Declaration of Helsinki. The number of the Ethics Approval is KY20163378-1. A written informed consent was obtained from all the patients at the time of admission, with which the blood, tissue and other sample were authorized to scientific purpose.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Yatabe T, Kitagawa H, Yamashita K, et al. Better postoperative oxygenation in thoracoscopic esophagectomy in prone positioning. J Anesth 2010;24:803-6. 10.1007/s00540-010-0968-4 [DOI] [PubMed] [Google Scholar]
- 2.Perry Y, Fernando HC. Three-field minimally invasive esophagectomy: current results and technique. J Thorac Cardiovasc Surg 2012;144:S63-6. 10.1016/j.jtcvs.2012.06.002 [DOI] [PubMed] [Google Scholar]
- 3.Cuschieri A, Shimi S, Banting S, et al. Technical aspects of laparoscopic splenectomy: hilar segmental devascularization and instrumentation. J R Coll Surg Edinb 1992;37:414-6. [PubMed] [Google Scholar]
- 4.D'Journo XB, Thomas PA. Current management of esophageal cancer. J Thorac Dis 2014;6 Suppl 2:S253-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anderegg MC, Gisbertz SS, van Berge Henegouwen MI. Minimally invasive surgery for oesophageal cancer. Best Pract Res Clin Gastroenterol 2014;28:41-52. 10.1016/j.bpg.2013.11.002 [DOI] [PubMed] [Google Scholar]
- 6.Bussières JS. Open or minimally invasive esophagectomy: are the outcomes different? Curr Opin Anaesthesiol 2009;22:56-60. 10.1097/ACO.0b013e32831cef4b [DOI] [PubMed] [Google Scholar]
- 7.Ng JM. Update on anesthetic management for esophagectomy. Curr Opin Anaesthesiol 2011;24:37-43. 10.1097/ACO.0b013e32834141f7 [DOI] [PubMed] [Google Scholar]
- 8.Noshiro H, Miyake S. Thoracoscopic esophagectomy using prone positioning. Ann Thorac Cardiovasc Surg 2013;19:399-408. 10.5761/atcs.ra.13-00262 [DOI] [PubMed] [Google Scholar]
- 9.Palanivelu C, Prakash A, Senthilkumar R, et al. Minimally invasive esophagectomy: thoracoscopic mobilization of the esophagus and mediastinal lymphadenectomy in prone position--experience of 130 patients. J Am Coll Surg 2006;203:7-16. 10.1016/j.jamcollsurg.2006.03.016 [DOI] [PubMed] [Google Scholar]
- 10.Saikawa D, Okushiba S, Kawata M, et al. Efficacy and safety of artificial pneumothorax under two-lung ventilation in thoracoscopic esophagectomy for esophageal cancer in the prone position. Gen Thorac Cardiovasc Surg 2014;62:163-70. 10.1007/s11748-013-0335-0 [DOI] [PubMed] [Google Scholar]
- 11.Xu WY, Wang N, Xu HT, et al. Effects of sevoflurane and propofol on right ventricular function and pulmonary circulation in patients undergone esophagectomy. Int J Clin Exp Pathol 2013;7:272-9. [PMC free article] [PubMed] [Google Scholar]
- 12.Hong L, Zhang Y, Zhang H, et al. The short-term outcome of three-field minimally invasive esophagectomy for Siewert type I esophagogastric junctional adenocarcinoma. Ann Thorac Surg 2013;96:1826-31. 10.1016/j.athoracsur.2013.06.058 [DOI] [PubMed] [Google Scholar]
- 13.Napier KJ, Scheerer M, Misra S. Esophageal cancer: A Review of epidemiology, pathogenesis, staging workup and treatment modalities. World J Gastrointest Oncol 2014;6:112-20. 10.4251/wjgo.v6.i5.112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levy RM, Wizorek J, Shende M, et al. Laparoscopic and thoracoscopic esophagectomy. Adv Surg 2010;44:101-16. 10.1016/j.yasu.2010.05.002 [DOI] [PubMed] [Google Scholar]
- 15.Verhage RJ, Hazebroek EJ, Boone J, et al. Minimally invasive surgery compared to open procedures in esophagectomy for cancer: a systematic review of the literature. Minerva Chir 2009;64:135-46. [PubMed] [Google Scholar]
- 16.Barreto JC, Posner MC. Transhiatal versus transthoracic esophagectomy for esophageal cancer. World J Gastroenterol 2010;16:3804-10. 10.3748/wjg.v16.i30.3804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang L, Onaitis M. Minimally invasive and robotic Ivor Lewis esophagectomy. J Thorac Dis 2014;6 Suppl 3:S314-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wee JO, Morse CR. Minimally invasive Ivor Lewis esophagectomy. J Thorac Cardiovasc Surg 2012;144:S60-2. 10.1016/j.jtcvs.2011.12.051 [DOI] [PubMed] [Google Scholar]
- 19.Kato H, Nakajima M. Treatments for esophageal cancer: a review. Gen Thorac Cardiovasc Surg 2013;61:330-5. 10.1007/s11748-013-0246-0 [DOI] [PubMed] [Google Scholar]
- 20.Berry MF. Esophageal cancer: staging system and guidelines for staging and treatment. J Thorac Dis 2014;6 Suppl 3:S289-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mallipeddi MK, Onaitis MW. The contemporary role of minimally invasive esophagectomy in esophageal cancer. Curr Oncol Rep 2014;16:374. 10.1007/s11912-013-0374-9 [DOI] [PubMed] [Google Scholar]
- 22.Biere SS, van Berge Henegouwen MI, Maas KW, et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 2012;379:1887-92. 10.1016/S0140-6736(12)60516-9 [DOI] [PubMed] [Google Scholar]
- 23.Cuschieri A. Thoracoscopic subtotal oesophagectomy. Endosc Surg Allied Technol 1994;2:21-5. [PubMed] [Google Scholar]
- 24.Watson DI, Jamieson GG, Devitt PG. Endoscopic cervico-thoraco-abdominal esophagectomy. J Am Coll Surg 2000;190:372-8. 10.1016/S1072-7515(99)00230-6 [DOI] [PubMed] [Google Scholar]
- 25.Jaeger JM, Collins SR, Blank RS. Anesthetic management for esophageal resection. Anesthesiol Clin 2012;30:731-47. 10.1016/j.anclin.2012.08.005 [DOI] [PubMed] [Google Scholar]
- 26.Bonavina L, Laface L, Abate E, et al. Comparison of ventilation and cardiovascular parameters between prone thoracoscopic and Ivor Lewis esophagectomy. Updates Surg 2012;64:81-5. 10.1007/s13304-012-0156-1 [DOI] [PubMed] [Google Scholar]
- 27.Bonavina L, Scolari F, Aiolfi A, et al. Early outcome of thoracoscopic and hybrid esophagectomy: Propensity-matched comparative analysis. Surgery 2016;159:1073-81. 10.1016/j.surg.2015.08.019 [DOI] [PubMed] [Google Scholar]


