Abstract
Background
Glioblastoma (GBM) is one of the most lethal tumors with a poor prognosis. Its inevitable recurrence is frequently explained by the presence of cancer stem cells. We aimed to show that human GBM cells with stemness features are more sensitive to natural killer (NK) cells than GBM cells without stemness characteristics.
Methods
Natural killer cell cytotoxicity was measured using flow cytometry in neurosphere-forming U87 GBM cells cultured with neurobasal media (NBE condition) and compared with that in serum-cultured U87 GBM cells (serum condition). Cytotoxicity was examined after addition of blocking NKG2D monoclonal antibodies. The expression profile of NK ligands of NK cells were investigated by reverse transcription polymerase chain reaction and western blot analysis in the U87 GBM cells in both conditions.
Results
NBE U87 cells showed higher cytotoxicity to NK cells than serum U87 cells did (55 vs 35% at an effector to target cell ratio of 5:1). The increased cytotoxicity was diminished in NBE U87 cells by a larger gap than in serum U87 cells by adding NKG2D blocking antibodies. Of the NKG2D ligands, the expression of ULBP1 and ULBP3 was relatively increased in NBE U87 cells compared to serum U87 cells.
Conclusions
U87 GBM cells with stemness features demonstrate increased cytotoxicity to NK cells in association with altered NKG2D ligand expression of NK cell activating receptor. Applying immune modulation to GBM treatment may be a promising adjuvant therapy in patients with intractable GBM.
Keywords: Cancer stem cells, Glioblastoma, Immunotherapy, Natural killer cell, U87
Background
Gliomas comprise a group of central nervous system (CNS) tumors with characteristics of neuroglial cells, such as astrocytes and oligodendrocytes. Glioblastoma (GBM), the most malignant type of glioma [World Health Organization (WHO) grade IV], are lethal neoplasms with a poor prognosis despite extensive treatments involving surgical resection with various combinations of radiotherapy, chemotherapy, and possible immunotherapy [1]. The existence of cancer stem cells in gliomas has been pointed out as one of culprits of the resistance of the conventional therapies that preludes their metastatic spread and recurrence [2]. Many efforts are being made to target cancer stem cells, particularly by improving immunotherapy using natural killer (NK) cell cytotoxicity against the tumors [3].
Natural killer cells can directly kill target cells via the perforin-granzyme pathway, antibody-dependent cellular toxicity, and death receptor ligand-induced apoptosis [3]. These mechanisms are tightly regulated by a balance between activating and inhibitory signals; NK cells can attack cells with decreased inhibitory signals, increased activating receptors, or both. Among them, the interaction between NK receptor group 2, membrane D (NKG2D) activating receptor and its ligand, such as MHC I-related chain (MIC) A/B and UL16 binding protein (ULBP) 1–5, seem to play a vital role in NK cell cytotoxicity [4] against cancer cells as ‘induced self’, although the tumors can secret these ligands as a soluble form to evade the immune surveillance.
Natural killer cell-mediated immunotherapy appears to be a promising approach to target various origins of cancer stem cells. GBM stem-like cells are sensitive to activated NK cells [5, 6]. NK cells activation has also been studied to enhance its efficacy by co-culture of genetically engineered K562 feeder cells in cytokine-containing medium [7, 8]. Additionally, the U87 GBM cell line has been extensively characterized immunologically [9].
The collective evidence indicates the merit of maximizing NK cell cytotoxicity against GBM with stem cell characteristics. However, the mechanism of NK cell cytotoxicity difference between GBM cells with stem cell-like features and serum-cultured GBM cells is not clear. In this study, we compared NK cell cytotoxicity against neurosphere-forming U87 cells (NBE U87) and serum-cultured U87 cells (serum U87). The mechanism that leads to the differential NK cell cytotoxicity between NBE U87 and serum U87 cells was explored in terms of NK cell degranulation and NKG2D–NKG2D ligand (NKG2DL) interaction.
Methods
Cell lines and cell cultures
The U87 human GBM cell line, as reported as isocitrate dehydrogenase (IDH)-wild type and O6-methylguanine-DNA methyltransferase (MGMT) promoter methylated [10, 11], was obtained from the Korean Cell Line Bank (Seoul, Korea). U87 cells were cultured in Dulbecco’s modified Eagle’s medium (DMEM; GibcoBRL, Gaithersburg, MD., USA) supplemented with 10% fetal bovine serum (FBS; GibcoBRL) at 37 °C in a humidified 95% air and 5% CO2 atmosphere, termed here ‘serum’ conditions. U87 cell line was also cultured with serum-free neurobasal medium (Invitrogen, Carlsbad, CA, USA) containing 50 ng/mL of both basic fibroblast growth factor (FGF; PeproTech, Rocky Hill, NJ, USA) and epidermal growth factor (EGF; PeproTech) supplemented with N2 and B27 supplement without vitamin A and l-glutamine, which are termed ‘NBE’ conditions.
Cytokines and antibodies
Recombinant human interleukin (IL)-2, IL-15 and IL-21 (PeproTech) were used to expand NK cells. Fuorescein isothiocyanate (FITC)-conjugated anti-human CD3 and phycoerythrin (PE)-Cy5-conjugated antihuman CD56 antibodies were used to evaluate the purity of expanded NK cells. Anti-human NKG2D antibody was used to block the NK cell receptor. PE-conjugated anti-human CD107a antibody was used as a surrogate marker of degranulation. All the antibodies were from BD Biosciences (San Jose, CA, USA).
Flow cytometry-based NK cytotoxicity assay
Flow cytometric cytotoxicity assay using calcein acetoxymethyl ester (CAM)-stained expanded NK cells were performed as previously described [12]. U87 target (T) cells were prepared in serum and NBE conditions. Propidium iodide (PI) was added to detect target cell death. The generation of ex vivo expanded NK cells was performed as described previously, with a slight modification [8, 13, 14]. Peripheral blood mononuclear cells (PBMCs) were co-cultured with 100 Gy gamma-ray irradiated K562 (ATCC), in a 24-well tissue culture plate in the presence of IL-2 and IL-15 (PeproTech) in complete RPMI (Roswell Park Memorial Institute) 1640 medium. The target cells and effector cells were co-cultured at effector-to-target (E:T) ratios of 10:1, 5:1, and 1:1 for 4 h at 37 °C in a humidified incubator containing 5% CO2. Cells were acquired by means of FACSCalibur (BD Biosciences) and the data were analyzed by BD CellQuest™ Pro Software (BD Biosciences). This study was approved by the institutional review board of the Chonnam National University Hwasun Hospital (CNUHH-2016-074).
CD107a degranulation assay
Degranulation of expanded NK cells against target GBM cells was assessed as previously described [14]. Enhanced NK cells were incubated with serum U87 and NBE U87 at an effector/target ratio of 10:1 and 5:1 for 1 h in a 96-well plate in the presence of 5 µL/mL PE-conjugated anti-human CD107a. After 1 h, monensin and brefeldin A (BD Biosciences) were added and the plate was incubated for an additional 4 h. After co-culture with target GBM cells, expanded NK cells were washed and stained with FITC-conjugated anti-human CD3 antibody and PE-Cy5-conjugated antihuman CD56 antibody on ice for 15 min. The cells were washed, fixed and then analyzed with the use of a FACSCalibur instrument.
Cytotoxicity assay after anti-NKG2D antibody treatment
Anti-human NKG2D antibody was used to block the activating receptor NKG2D on NK cells. In blocking experiments, anti-NKG2D antibodies were added to the NK cell suspension at 10 μg/mL and incubated at 37 °C for 30 min before the addition of target cells. The number of dead cells was estimated by measuring the fluorescence intensity in medium. The fluorescence intensity in medium released spontaneously from target cells and the total maximum fluorescence intensity released from all target cells by treatment with 1% Triton X-100 were also determined.
Reverse transcription polymerase chain reaction (RT-PCR)
Reverse transcription polymerase chain reaction was performed as previously described on 23 NK ligands [15]. Briefly, total RNA from cells was extracted using Trizol reagent (Invitrogen, Carlsbad, CA, USA). An adequate amount of RNA was reverse transcribed using LeGene Express 1st Strand cDNA Synthesis System Kit (LeGene Biosciences, San Diego, CA, USA). Primer sequences used in this study are listed in Table 1 [16]. PCR amplification of cDNA was performed using gene-specific primers and h-Taq DNA Polymerase (SolGent, Daejeon, South Korea) under the following conditions: 15 min of denaturation at 95 °C, followed by 35 cycles of denaturation for 30 s at 95 °C, annealing for 40 s at 54 °C, and extension for 40 s at 72 °C, followed by a final extension for 7 min at 72 °C. PCR cycles were limited to 35. Primers for endogenous reference gene (glyceraldehyde-3-phosphate dehydrogenase, GAPDH) were used as internal controls. PCR products were analyzed by electrophoresis on agarose gels containing ethidium bromide. The intensity of the bands were quantified by the Labworks Image Acquisition (UVP, Upland, CA).
Table 1.
NK ligand primers used for RT-PCR
| NK receptor | Ligands | Forward primer | Reverse primer | Amplicon size (bp) |
|---|---|---|---|---|
| NKG2D | MICA | TCTACTACGATGGGGAGCTCTT | ACTGGGGCATTGTCCATTC | 66 |
| MICB | CTGAGAAGGTGGCGACGTA | CGAAGACTGTGGGGCTCA | 111 | |
| ULBP-1 | TGGGGGATTGTAAGATGTGG | GGCCAGAGAGGGTGGTTT | 83 | |
| ULBP-2 | CCGCTACCAAGATCCTTCTG | TGACGGTGATGTCATAGCAAA | 105 | |
| ULBP-3 | AGGAAGAAGAGGCTGGAACC | CTATGGCTTTGGGTTGAGCTA | 70 | |
| ULBP-4 | GGGAGAATTGACCCAAACG | CTTGCAGAGTGGAAGGATCAC | 104 | |
| NKG2A/C/E/H | HLA-E | GGAGTGGCTCCACAAATACC | GTCAGAGATGGGGTGGTGAG | 94 |
| 2DL4 | HLA-G | CTGGAGAACGGGAAGGAGAT | GGGTGGCCTCATAGTCAAAG | 88 |
| 2B4 | CD48 | CCTACATCATGAGGGTGTTGAA | ATGACAGGCTTGGGTACAGG | 91 |
| NTBA | NTBA | CCACAATTAATCATTCCAAAGAGA | TGTCATTCCCGAATTCCTCT | 107 |
| LIR2 | HLA-F | ATCACCCAGCGCTTCTATGA | CTGGGGAGACTGCTCTGC | 138 |
| NKR-P1A | LLT-1 | GTTCAGGGCCAGTGCATATT | GACTCTGCACCTTCCTTCACA | 61 |
| DNAM-1 | PVR-1 | CAACGTCACCAATGCCCTA | CTGAGTGCTCACTGGGAGGT | 80 |
| PVR-2 | GATATCTGGCTCCGAGTGCT | TCCAGTGAGCTGGACCTTCT | 69 | |
| Nectin2-1 | GGCAGAGGAGGACGAAGAC | GAGCTGGGAGGGCATCTC | 94 | |
| Nectin2-2 | GAGGACGAGGGCAACTACAC | GGCCTCAGCTTGGTTCTTG | 108 | |
| CD100 | CD72 | TTCTTCACATGCGGCTCA | AGCAGCTTTTCTGATGCATTATC | 67 |
| CD28 | CD80 | TCCTGGGCCATTACCTTAATC | CATCTTGGGGCAAAGCAG | 77 |
| LFA-1 | ICAM-1 | CCTTCCTCACCGTGTACTGG | AGCGTAGGGTAAGGTTCTTGC | 90 |
| LFA-2 | LFA-3 | CATGTATTGTGCTGTATATGAATGGT | TCTGGCTTCCCAAGTAATGG | 141 |
| CRACC | CRACC | TCTACTATGTGGGGATATACAGCTCA | TTTAGGCTTTGACAGGTGCTC | 92 |
| FasL | Fas | GTGGACCCGCTCAGTACG | TCTAGCAACAGACGTAAGAACGA | 112 |
| TRAIL | DR4 | GGGTCCACAAGACCTTCAAGT | GGGTCCACAAGACCTTCAAGT | 68 |
| DR5-1 | GTGTGTCAGTGCGAAGAAGG | GACCATCCCTCTGGGACA | 90 | |
| DR5-2 | GCACCAGGTGTGATTCAGG | CCCTCTGGGACACCCTGT | 143 | |
| TNF | TNFR1 | CTCTCCACCGTGCCTGAC | CCAGTCCAATAACCCCTGAG | 85 |
CRACC CD2-like receptor activating cytotoxic cell, DNAM-1 DNAX accessory molecule-1, ICAM-1 intercellular adhesion molecule 1, LFA lymphocyte function-associated antigen, MIC MHC I-related chain, NK natural killer, NKG2D NK receptor group 2; membrane D, PVR-1 poliovirus receptor-1, RT-PCR real-time quantitative polymerase chain reaction, TNF tumor necrosis factor, TRAIL tumor necrosis factor-related apoptosis-inducing ligand, ULBP UL16 binding protein
Western blotting
Total cellular proteins were extracted from cultured cells using RIPA Buffer (Biosolution, Korea) supplemented with protease inhibitor Cocktail (Roche, Germany). Briefly, lysates were cleared by centrifugation at 12,000 rpm for 30 min at 4 °C. Supernatant containing proteins were collected for immunoblotting, extracted proteins (20–40 μg) were separated by SDS-PAGE (6–15%) gel and then electroblotted onto Polyvinylidene Fluoride (PVDF) membranes (Amersham Hybond-P, GE-Healthcare Life Science, Pittsburgh, PA, USA). Followed by transfer membranes were blocked with 5% w/v skim milk in TBST (TBS; 0.05 M Tris, 0.15 M NaCl, pH 7.6 and 0.1% Tween20) for 1 h and then probed with primary antibodies diluted in 3% BSA in TBST for overnight. Membranes were washed in TBST and then incubated with HRP-conjugated anti-mouse or anti rabbit secondary antibodies. Membranes were detected with an electrochemiluminescence (ECL) system (Millipore). The bands were visualized by Luminescent image analyzer (FUJIFILM, LAS-4000). The following antibodies were used: ULBP1 (1:500, sc-33564, Santa cruz biotechnology, Dallas, TX, USA), ULBP3 (1:300, sc-390844, Santa cruz biotechnology).
Statistics
GraphPad Prism version 6.00 software program for Windows (GraphPad, La Jolla, CA, USA) was used to analyze the experiments, with the data presented as the mean ± the standard error of the mean (SEM). Statistical significance was defined at P < 0.05.
Results
NK cell cytotoxicity to NBE and serum U87 GBM cells
To determine whether GBM cells with stem cell characteristics (NBE U87) were more susceptible to NK cell cytotoxicity than serum U87 cells, we co-cultured effector NK cells with each corresponding NBE U87 and serum U87 cell lines (Fig. 1a). Assays were performed in triplicate under serum and NBE conditions with E:T ratios from 10:1, 5:1, to 1:1 for expanded NK cells (Fig. 1b, c). Both cell lines showed increasing cell lysis proportional to increasing amount of effector NK cells. NBE U87 cells were, however, more sensitive than serum U87 cells to enhanced NK cells, with median cytotoxicity at 5:1 effector/target ratio of 56.1 and 34.5%, respectively (P < 0.001).
Fig. 1.
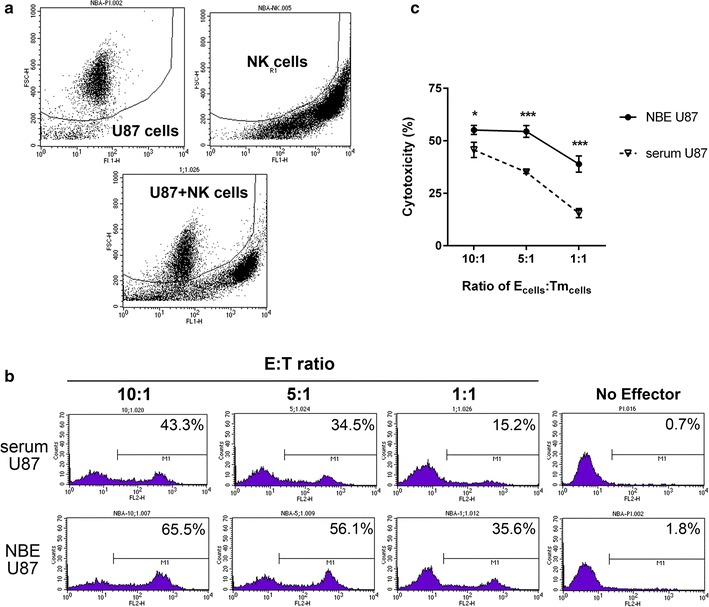
Representative flow cytometry view and cell compartment. a Forward scatter profiles were used to discriminate target and effector cells before (upper panels) and after (lower panel) co-culture of effector cells (NK cells) and target cells (U87 GBM cells). b Effector NK cells enhanced lysed target cell compartments in neurobasal medium-cultured NBE U87 cells (NBE U87) compared to serum-cultured U87 cells (serum U87) proportionally according to decreasing order of E:T ratio. c The average cytotoxicity levels are shown in decreasing order of E:T ratio, representing increased cytotoxicity of NK cells in NBE U87 cells compared to serum U87 cells. Bar graphs show the mean ± the standard error of the mean (SEM). (*P < 0.05, ***P < 0.001)
NK cells cytotoxicity with regard to CD107a degranulation
We investigated the relationship between CD107a-mediated degranulation and NK cell cytotoxicity to U87 tumor cells in each group. Using flow cytometry, we differentiated subsets of NK cells with CD56+CD3− then those with CD107a+ in each co-cultured cell lines (Fig. 2a). However, the lower fraction of the CD107a+ NK cells was observed in NBE U87 than in serum U87, 19.7 and 24.9% respectively at a 5:1 effector/target ratio (Fig. 2b, P < 0.05). CD107a+ was not increased with a higher effector/target ratio. Contrary to the hypothetical expectation, fractions of CD107a+ NK cells with degranulation did not appear to explain the differential cytotoxicity between NBE U87 cells and serum U87 cells.
Fig. 2.

Comparison of the percentage of NK cells characterized by CD107a+ phenotype. a The purity of expanded NK cells were evaluated upon immunostaining as CD3−CD56+ cells and the percentage of CD107a+ NK cells were assessed by flow cytometry in both NBE U87 cells and serum U87 cells. b Serum U87 cells showed higher fraction of CD107a+ NK cells than NBE U87 cells did. Bar graphs show the mean ± the standard error of the mean (SEM). (*P < 0.05)
NK cells cytotoxicity via NKG2D–NKG2DL interaction
Next, we measured NK cell cytotoxicity to tumor cell lines by directly neutralizing NKG2D receptor by NKG2D antibody. It was apparent that NKG2D blocking decreased NK cell cytotoxicity in both cell lines, but with a larger decrease in NBE U87 than serum U87 (Fig. 3a). The reduction of cytotoxicity was higher in NBE U87 than serum U87 with blocking NKG2D receptor with statistical significance at 1:1 of E:T ratios (Fig. 3b, P < 0.05).
Fig. 3.
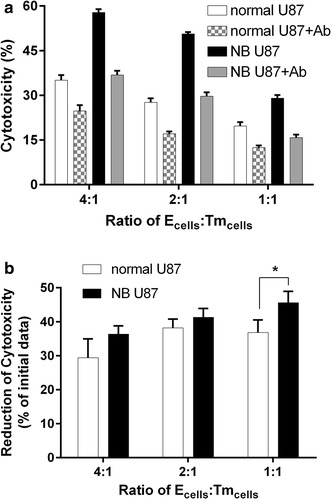
GBM cell sensitivity to NK cell lysis that occurs via NKG2D–NKG2DL interactions. a Cytotoxicity assays showing that GBM cells are sensitive to NK-mediated cell elimination using NKG2D blocking antibody at different E:T ratio. b Comparison of reduction rate between NBE U87 cells and serum U87 cells. The result showed that NK-mediated cell elimination effect using NKG2D blocking antibody is greater in NBE U87 cells, suggesting that the different cytotoxicity is mediated by NKG2D–NKG2DL interactions
Expression of NK ligands by RT-PCR and western blot
Since the cytotoxicity was decreased by a larger gap in NBE U87 cells than in serum U87 cells after applying NKG2D blocking antibodies, the expression of causal NKG2D ligands and other K cell ligands on the tumor cell surfaces were explored. Serum U87 and NBE U87 cell lines exhibited different RNA profiles of NK ligands (Fig. 4). In NBE U87, the expression of NKG2D ligands including ULBP1 and ULBP3 were relatively increased (Fig. 5a, P < 0.01 in ULBP1 and P < 0.05 in ULBP3). FAS expression was also increased with marginal statistical significance. In contrast, the level of DNAX accessory molecule-1 (DNAM-1) ligands of poliovirus receptor (PVR)-1, PVR-2, Nectin 2-1, and Nectin 2-2 were decreased in NBE cells (Fig. 4). The enhanced protein levels of ULBP1 and ULBP3 were also confirmed (Fig. 5b, P < 0.05 in both ligands).
Fig. 4.

Expression of NKG2D ligands in serum U87 and NBE U87 GBM cells by RT-PCR. Increased expression levels are shown in ULBP1, ULBP3, and FAS (in bold italic). In comparison, the expression levels reduced in PVR-1, PVR-2, Nectin 2-1, and Nectin 2-2 (in gray bold italic)
Fig. 5.

Quantification of NKG2D ligands in serum U87 and NBE U87 GBM cells. a ULBP1 and ULBP3 mRNA was increased in NBE U87 GBM cells. Increase of FAS mRNA was not statistical significant. b ULBP1 and ULBP3 protein expression was also enhanced. Bar graphs show the mean ± the standard error of the mean (SEM). (*P < 0.05, **P < 0.01)
Discussion
In the present study, human GBM cells with stem cell-like features (NBE U87) showed increased cytotoxicity to enhanced NK cells compared to serum-cultured GBM cells (serum U87). It was also suggested that increased cytotoxicity was mediated by NKG2D–NKG2DL interaction supported by different NK cell cytotoxicity in each groups after applying NKG2D blocking antibodies. In addition, NKG2DL expression in NBE U87 was altered in comparison of that in serum U87. Interestingly, we observed that the mechanism of different NK cell cytotoxicity with regard to stem cell-like features was not due to degranulation. As previously reported characteristics of U87 cell line, this study is focused on IDH-wild type GBM.
Activated NK cells are capable of killing different types of cancer cells including glioma cells [5–7]. Once NK cells are activated by various means including IL-2, IL-15, or PHA, they can overcome immune escape of glioma, such as HLA class I molecules, by overwhelming the activating signals [5, 6]. We used K562 cells in the presence of IL-2 and IL-15 to activate NK cells [7]. A previous study demonstrated that GBM cells with stem cell-like features were susceptible to lysis by lymphokine-activated NK cells [6], in contrast to the NK cell resistance caused by use of glioma cells cultured under non-stem cell conditions or freshly isolated NK cells [6].
In the current study, NKG2D–NKG2DL interaction played a significant role in enhanced NK cytotoxicity against glioma cell lines. Prior studies reported controversial results on the mechanistic cause of increased cytotoxicity of tumor cells with stem cell features compared to serum-cultured tumor cells. Glioma is vulnerable to NK cells via NKp44, NKp46 [5], or DNAM-1 receptors [6] and their cytotoxicity is considered minimal or to be minor via NKG2D. Proneuronal GBM cancer stem cell lines were reported to downregulate NKG2D expression on NK cells through transforming growth factor-beta-dependent suppression, providing an explanation for the reduced immune infiltration [17]. The level of NKG2DL expression in tumor cells does not appear to correlate with increasing cytotoxicity [9]. The discrepancy between the current study and previous reports can be speculated as previously pointed out [5]; the target cells used (U87 immortalized GBM cell line vs. primary cultured cell lines from GBM patients); methodological modification in generating enhanced NK cells (use of K562 feeder cells), cytokine concentration, duration of cytokine treatment); or the effector cells used (polyclonal MelanA specificT cell lines vs. enhanced NK cells after separation from PBMCs of healthy donors).
However, there have been some subtle points that suggest a mechanistic possibility similar to our results. Jung et al. [9] demonstrated the increased expression levels of NKG2D ligands in NBE U87 cells, similar to our results. Avril et al. showed mRNA analysis results that displayed expression of NKG2D ligands [5] and Di Tomaso et al. [18] also reported more commonly detectable MICA, ULBP-2, ULBP-3, and ULBP-4, although at a low levels. Also, the interaction between NKG2D and DNAM-1 on the surface of NK cells with their ligands on tumor cells was designated to be critical for NK cell cytotoxicity against sarcoma cells as well [7].
Presently, we discovered that the ligands of activating receptors of NK cells differ from NBE U87 to serum U87. Although the level of NKG2DL does not necessarily affect NKG2D mediated cytotoxicity with enhanced NK cells [9], NBE U87 showed increased cell lysis compared to serum U87. High expression of MICA and ULBP2 in both cell lines could result in basal cytotoxicity, whereas the increment of ULBP1 and 3 may contribute to relatively higher cytotoxicitiy in stem cell-like GBM.
Additionally, stem cell-like glioma may display heterogeneous NK cell ligands depending on different subtypes. NBE U87 GBM cell line used in this study showed different RNA profile compared to other studies. Castriconi et al. [6] showed increased expression of DNAM-1 ligands, PVR and nectin-2, in GBM grown in neurobasal medium whereas we observed decreased amounts of these ligands in NBE U87. In this sense, the various types of glioma could make it difficult to exploit uniformly enhanced NK cells and individualized immunotherapy is much desired.
It is interesting to note that NK cell cytotoxicity did not attribute to the degree of degranulation. Low level of CD107a+ fraction in degranulation assay reflects the fact that enhanced NK cell cytotoxicity does not result from perforin granzyme release. This result implies that NK cell activation with NKG2D provides different mechanisms to lyse target cells, such as inducing apoptosis or mediating other cytokines.
Enhanced NK cells provided promising results in eliminating many different tumor cell lines [7, 8]. Although NK cell cytotoxicity is lower in glioma cell lines than other types of tumors, it is still necessary to show improved cytotoxicity compared to conventional methods [5, 6]. Whether the different cytotoxicities among various tumor types are due to different NK cell ligands expression is uncertain. However, many experiments have shown that NKG2D ligands induction in different tumors including glioma cell lines give a rise in increased cell lysis [19–22], indicating that enhanced NK cell ligands in tumor cells do play role in increasing cytotoxicity.
Recent emerging evidence has supported the potential synergistic effects of therapeutic combinations against solid tumors [3]. Examples include combining NK cell therapy with radiation therapy or with monoclonal antibody therapy. Radiation-induced tissue injury increases the expression of NK activating ligands, such as NKG2D, and monoclonal antibody therapy allows NK cells to kill antibody-coated target cells through antibody-dependent cellular cytotoxicity.
Conclusion
The results indicate that enhanced NK cell cytotoxicity against GBM stem cell populations in combination with other conventional anti-cancer therapy may be a promising treatment option in the near future. Further investigation is needed to elucidate the true nature of the enhanced sensitivity to GBM cell with stemness features by enhanced NK cells.
Authors’ contributions
LKH, DC and KSM designed this study. SJO and OK carried out the study. SJO, JIY, KHL, WDK and DC drafted the manuscript. EJA and KSM carried out the statistical analysis. KSM and JHL assisted with the manuscript preparation and data analysis. All authors read and approved the final manuscript.
Acknowledgements
We would like to thank Ms. Ju-Sun Kim for her assistance with the FACS analysis.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The data and material of this study are included in this published article.
Ethical approval
This study was approved by the institutional review board of the Chonnam National University Hwasun Hospital (CNUHH-2016-074), and all the patients provided written informed consent for the use of clinical specimens for medical research.
Funding
This work was supported by Chonnam National University Hospital Biomedical Research Institute (HCRI14024-1, HCRI15014-21), partly by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Minist (2016R1A2B1014597, 2016R1C1B2007494).
Abbreviations
- DNAM-1
DNAX accessory molecule-1
- GAPDH
glyceraldehyde-3-phosphate dehydrogenase
- GBM
glioblastoma
- MIC
MHC I-related chain
- NBE
neurobasal media
- NK
natural killer
- NKG2D
NK receptor group 2, membrane D
- PBMC
peripheral blood mononuclear cell
- PVR-1
poliovirus receptor-1
- RT-PCR
real-time quantitative polymerase chain reaction
- ULBP
UL16 binding protein
Contributor Information
Se-Jeong Oh, Email: ddalki7598@hanmail.net.
Jung-In Yang, Email: junginyangms@gmail.com.
Ok Kim, Email: oasis99k@daum.net.
Eun-Jung Ahn, Email: happybear33@naver.com.
Woo Dae Kang, Email: kangwd@chonnam.ac.kr.
Jae-Hyuk Lee, Email: jhlee@chonnam.ac.kr.
Kyung-Sub Moon, Phone: +82-61-379-7666, Email: moonks@chonnam.ac.kr.
Kyung-Hwa Lee, Phone: +82-61-379-7666, Email: mdkaylee@gmail.com.
Duck Cho, Phone: +82-2-3410-2403, Email: hasomii@hanmail.net.
References
- 1.Ostrom QT, Bauchet L, Davis FG, Deltour I, Fisher JL, Langer CE, Pekmezci M, Schwartzbaum JA, Turner MC, Walsh KM, et al. The epidemiology of glioma in adults: a “state of the science” review. Neuro Oncol. 2014;16(7):896–913. doi: 10.1093/neuonc/nou087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liebelt BD, Shingu T, Zhou X, Ren J, Shin SA, Hu J. Glioma stem cells: signaling, microenvironment, and therapy. Stem Cells Int. 2016;2016:7849890. doi: 10.1155/2016/7849890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cho D, Kim SK, Carson WE., 3rd NK cell-based immunotherapy for treating cancer: will it be promising? Korean J Hematol. 2011;46(1):3–5. doi: 10.5045/kjh.2011.46.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fujisaki H, Kakuda H, Shimasaki N, Imai C, Ma J, Lockey T, Eldridge P, Leung WH, Campana D. Expansion of highly cytotoxic human natural killer cells for cancer cell therapy. Cancer Res. 2009;69(9):4010–4017. doi: 10.1158/0008-5472.CAN-08-3712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Avril T, Vauleon E, Hamlat A, Saikali S, Etcheverry A, Delmas C, Diabira S, Mosser J, Quillien V. Human glioblastoma stem-like cells are more sensitive to allogeneic NK and T cell-mediated killing compared with serum-cultured glioblastoma cells. Brain Pathol. 2012;22(2):159–174. doi: 10.1111/j.1750-3639.2011.00515.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Castriconi R, Daga A, Dondero A, Zona G, Poliani PL, Melotti A, Griffero F, Marubbi D, Spaziante R, Bellora F, et al. NK cells recognize and kill human glioblastoma cells with stem cell-like properties. J Immunol. 2009;182(6):3530–3539. doi: 10.4049/jimmunol.0802845. [DOI] [PubMed] [Google Scholar]
- 7.Cho D, Shook DR, Shimasaki N, Chang YH, Fujisaki H, Campana D. Cytotoxicity of activated natural killer cells against pediatric solid tumors. Clin Cancer Res. 2010;16(15):3901–3909. doi: 10.1158/1078-0432.CCR-10-0735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Imai C, Iwamoto S, Campana D. Genetic modification of primary natural killer cells overcomes inhibitory signals and induces specific killing of leukemic cells. Blood. 2005;106(1):376–383. doi: 10.1182/blood-2004-12-4797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jung TY, Choi YD, Kim YH, Lee JJ, Kim HS, Kim JS, Kim SK, Jung S, Cho D. Immunological characterization of glioblastoma cells for immunotherapy. Anticancer Res. 2013;33(6):2525–2533. [PubMed] [Google Scholar]
- 10.Yi GZ, Liu YW, Xiang W, Wang H, Chen ZY, Xie SD, Qi ST. Akt and β-catenin contribute to TMZ resistance and EMT of MGMT negative malignant glioma cell line. J Neurol Sci. 2016;367:101–106. doi: 10.1016/j.jns.2016.05.054. [DOI] [PubMed] [Google Scholar]
- 11.Ohba S, Mukherjee J, See WL, Pieper RO. Mutant IDH1-driven cellular transformation increases RAD51-mediated homologous recombination and temozolomide resistance. Cancer Res. 2014;74(17):4836–4844. doi: 10.1158/0008-5472.CAN-14-0924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jang YY, Cho D, Kim SK, Shin DJ, Park MH, Lee JJ, Shin MG, Shin JH, Suh SP, Ryang DW. An improved flow cytometry-based natural killer cytotoxicity assay involving calcein AM staining of effector cells. Ann Clin Lab Sci. 2012;42(1):42–49. [PubMed] [Google Scholar]
- 13.Phan MT, Lee SH, Kim SK, Cho D. Expansion of NK cells using genetically engineered K562 feeder cells. Methods Mol Biol. 2016;1441:167–174. doi: 10.1007/978-1-4939-3684-7_14. [DOI] [PubMed] [Google Scholar]
- 14.Lim DP, Jang YY, Kim S, Koh SS, Lee JJ, Kim JS, Thi Phan MT, Shin DJ, Shin MG, Lee SH, et al. Effect of exposure to interleukin-21 at various time points on human natural killer cell culture. Cytotherapy. 2014;16(10):1419–1430. doi: 10.1016/j.jcyt.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 15.Lee KH, Ahn EJ, Oh SJ, Kim O, Joo YE, Bae JA, Yoon S, Ryu HH, Jung S, Kim KK, et al. KITENIN promotes glioma invasiveness and progression, associated with the induction of EMT and stemness markers. Oncotarget. 2015;6(5):3240–3253. doi: 10.18632/oncotarget.3087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luo Y, Duan LN, Lu CR, Cai Q, Wang Z, Bao RF, Xiang PD. Detection of the expression of NK ligands in acute leukemia cell lines by real-time PCR. Zhonghua Xue Ye Xue Za Zhi. 2013;34(1):26–29. [PubMed] [Google Scholar]
- 17.Beier CP, Kumar P, Meyer K, Leukel P, Bruttel V, Aschenbrenner I, Riemenschneider MJ, Fragoulis A, Rummele P, Lamszus K, et al. The cancer stem cell subtype determines immune infiltration of glioblastoma. Stem Cells Dev. 2012;21(15):2753–2761. doi: 10.1089/scd.2011.0660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Di Tomaso T, Mazzoleni S, Wang E, Sovena G, Clavenna D, Franzin A, Mortini P, Ferrone S, Doglioni C, Marincola FM, et al. Immunobiological characterization of cancer stem cells isolated from glioblastoma patients. Clin Cancer Res. 2010;16(3):800–813. doi: 10.1158/1078-0432.CCR-09-2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Friese MA, Platten M, Lutz SZ, Naumann U, Aulwurm S, Bischof F, Buhring HJ, Dichgans J, Rammensee HG, Steinle A, et al. MICA/NKG2D-mediated immunogene therapy of experimental gliomas. Cancer Res. 2003;63(24):8996–9006. [PubMed] [Google Scholar]
- 20.Kim JY, Bae JH, Lee SH, Lee EY, Chung BS, Kim SH, Kang CD. Induction of NKG2D ligands and subsequent enhancement of NK cell-mediated lysis of cancer cells by arsenic trioxide. J Immunother. 2008;31(5):475–486. doi: 10.1097/CJI.0b013e3181755deb. [DOI] [PubMed] [Google Scholar]
- 21.Kim JY, Son YO, Park SW, Bae JH, Chung JS, Kim HH, Chung BS, Kim SH, Kang CD. Increase of NKG2D ligands and sensitivity to NK cell-mediated cytotoxicity of tumor cells by heat shock and ionizing radiation. Exp Mol Med. 2006;38(5):474–484. doi: 10.1038/emm.2006.56. [DOI] [PubMed] [Google Scholar]
- 22.Li K, Mandai M, Hamanishi J, Matsumura N, Suzuki A, Yagi H, Yamaguchi K, Baba T, Fujii S, Konishi I. Clinical significance of the NKG2D ligands, MICA/B and ULBP2 in ovarian cancer: high expression of ULBP2 is an indicator of poor prognosis. Cancer Immunol Immunother. 2009;58(5):641–652. doi: 10.1007/s00262-008-0585-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data and material of this study are included in this published article.


